Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Jurnal Bu Putri 6 PDF
Caricato da
PitoAdhiDescrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Jurnal Bu Putri 6 PDF
Caricato da
PitoAdhiCopyright:
Formati disponibili
Oral Ondansetron in Management of Dehydrating Diarrhea with Vomiting in
Children Aged 3 Months to 5 Years: A Randomized Controlled Trial
Arun Singh Danewa, MD1, Dheeraj Shah, MD, DNB, MNAMS, FIAP1, Prerna Batra, MD, FACEE1,
Swapan Kumar Bhattacharya, MD2, and Piyush Gupta, MD, FAMS, FIAP1
Objectives To evaluate the role of oral ondansetron in facilitating successful rehydration of under-5-year-old children suffering from acute diarrhea with vomiting and some dehydration.
Study design Children (n = 170) aged 3 months to 5 years with acute diarrhea with vomiting and some dehydration were enrolled in this double blind, randomized, placebo-controlled trial. The participants were randomized to
receive either single dose of oral ondansetron (n = 85) or placebo (n = 85) in addition to standard management of
dehydration according to World Health Organization guidelines. Failure of oral rehydration therapy (ORT), administration of unscheduled intravenous fluids, and amount of oral rehydration solution intake in 4 hours were the primary
outcomes. Secondary outcome measures included duration of dehydration correction, number of vomiting episodes, adverse effects, and caregiver satisfaction.
Results Failure of ORT was significantly less in children receiving ondansetron compared with those receiving placebo (31% vs 62%; P < .001; relative risk 0.50, 95% CI 0.35-0.72). Almost one-half of the children in the ondansetron group received intravenous fluids compared with those in the placebo group, but it was not statistically
significant (P = .074; relative risk 0.56, 95% CI 0.30-1.07). The oral rehydration solution consumption was significantly more in the ondansetron group (645 mL vs 554 mL; mean difference 91 mL; 95% CI: 35-148 mL). Patients
in the ondansetron group also showed faster rehydration, lesser number of vomiting episodes, and better caregiver
satisfaction.
Conclusion A single oral dose of ondansetron, given before starting ORT to children <5 years of age with acute
diarrhea and vomiting results in better oral rehydration. (J Pediatr 2015;-:---).
Trial registration Clinical Trial Registry of India: CTRI-2011/07/001916.
iarrheal illnesses are the leading cause of death beyond infancy in developing countries.1 Oral rehydration therapy
(ORT) with oral rehydration solution (ORS) remains the cornerstone of appropriate case management of diarrheal
dehydration but, unfortunately, is grossly underused.2-4 Data from periodic National Surveys from India report that
less than one-half of children use ORS during an episode of diarrhea.2-4 Many health care providers perceive vomiting a barrier
to success of ORT.3,5 Vomiting in children suffering from acute gastroenteritis may interfere with oral rehydration process, and
frustrates parents and health care providers.6 This prompts health care providers to use intravenous fluids even when these may
not be indicated. Trials in developed countries have suggested benefit of anti-emetics like domperidone, metoclopramide,
promethazine, and ondansetron in acute gastroenteritis, when vomiting is a major symptom.5-7 However, there is a paucity
of literature addressing functional outcomes such as failure of ORT and use of unscheduled intravenous fluids related to
anti-emetic use in these studies. As the etiological and clinical profile of diarrhea, caregivers expectations, and the management
practices differ significantly in developing countries, we planned this study to evaluate the role of oral ondansetron in successful
rehydration of under-5-year-old children suffering from acute dehydrating diarrhea in the setting of a hospital catering mainly
to urban poor population in Northern India.
Methods
This double-blind randomized placebo-controlled trial was carried out in the
emergency pediatric unit of a tertiary care hospital over a period of 1 year.
Approval was provided by the institutional ethical committee.
Study participants included children aged between 3 months and 5 years with a
clinical diagnosis of acute diarrhea (duration <14 days) with some dehydration
as per World Health Organization (WHO) criteria,8 and at least 2 reported
ORS
ORT
WHO
Oral rehydration solution
Oral rehydration therapy
World Health Organization
From the Departments of 1Pediatrics and
2
Pharmacology, University College of Medical Sciences
and Guru Teg Bahadur Hospital, Delhi, India
The drug (ondansetron) was supplied by Mankind
Pharma Ltd, and the placebo was prepared in the
Department of Pharmacology at University College of
Medical Sciences. Mankind Pharma Ltd had no role in (1)
study design; (2) the collection, analysis, and interpretation of data; (3) the writing of the report; or (4) the decision
to submit the paper for publication. The authors declare
no conflicts of interest.
0022-3476/$ - see front matter. Copyright 2015 Elsevier Inc. All
rights reserved.
http://dx.doi.org/10.1016/j.jpeds.2015.10.006
THE JOURNAL OF PEDIATRICS
episodes of non-bilious, non-bloody vomiting within the last
6 hours. Children having severe malnutrition (weight for
length/height < 3 SD of WHO standards), edema, unconsciousness, convulsions, or paralytic ileus were excluded.
Paralytic ileus was defined as presence of abdominal distension, not passing stools, and diminished or absent bowel
sounds. Children who had received any anti-emetic within
24 hour prior to enrollment, and those who received intravenous fluids before enrollment, were also excluded.
Computer-generated block randomization with variable
block sizes was used to assign patients to the ondansetron
or the placebo group. Bottles were coded with this randomization scheme by a person not directly involved with the
study. Drug was supplied by a pharmaceutical company,
and placebo (similar composition, except for the active ingredient) was prepared in the pharmacy of our hospital. Drug
and placebo were identical in appearance, taste, and odor.
Ten mL bottles were procured from the market, and drug
and placebo were repackaged and labeled for the purpose
of the study by the pharmacy of the hospital. Bottles were
given a unique identification number according to the
randomization scheme. Study subjects, their caregivers, person assigning intervention, doctors managing the patient,
and outcome assessors were blinded to the content of formulation given. The codes were broken only at the end of the
study after complete data entry and data cleaning.
Detailed clinical history, physical examination, and
anthropometry were recorded in all patients. The child was
assessed every 30 minutes for intake of amount of ORS, frequency of vomiting, frequency of loose stools, and hydration
status; findings were recorded in a predesigned case record
form. Hydration was assessed using WHO criteria and also
by dehydration score devised by Freedman et al.9
Syrup ondansetron (2 mg/5 mL) or placebo was given
orally in a dose of 0.5 mL/kg (providing 0.2 mg/kg of ondansetron in drug group) single dose at enrollment before start of
ORS therapy. Exact doses of drug/placebo were measured
with a syringe and administered to the patient with a spoon
by one of the investigators. Same dose of drug/placebo was
repeated once if the patients vomited within 30 minutes of
receiving first dose. After receiving drug or placebo, children
were given WHO ORS at the rate of 75 mL/kg in first 4 hours.
ORS was given with a spoon or small sips frequently. A repeat
course of 75 mL/kg of ORS over 4 hours was given to children
who continued to have features of some dehydration after
initial 4 hours of therapy. Children who had features of severe
dehydration or shock any time during assessment, persistence of signs of some dehydration even after 8 hours of
ORS therapy, or appearance of convulsions, altered sensorium, or paralytic ileus during ORS therapy were shifted to
intravenous fluid therapy. Breastfed infants continued to
breastfeed during oral rehydration. Other fluids were avoided
during treatment. The study participants were admitted for
at least 2 hours after dehydration correction. After dehydration correction, children were advised to take oral zinc (zinc
acetate) in the dose of 10 mg/d for 3 months to 6 months age
group and 20 mg/d in 2 divided doses for the 6 months to
2
Vol. -, No. -
www.jpeds.com
5 years age group. Oral zinc was advised to be continued
for a total duration of 14 days.
The primary outcome measures were failure of ORT
(features of some dehydration persisting after 4 hours of
ORT or severe dehydration at any time during assessment),
administration of unscheduled intravenous fluids and
amount of ORS intake in 4 hours. Secondary outcomes
were duration of dehydration correction, number of vomiting episodes in 4 hours, adverse effects (eg, rash, headache, diarrhea), and caregiver satisfaction as assessed on a
5-point Likert scale10 on the basis of mood, activity, alertness, comfort, number of vomiting, and fluid intake. Single
caregiver, which was either mother or the one who was present with the child at that time, was assessed for caregiver
satisfaction.
Sample size was calculated on the basis of study by
Freedman et al9 who documented 31% unscheduled intravenous fluid use in placebo group and a better ORS intake in
ondansetron groups. Also, our hospital data suggested that
almost 50% of under-5-year-old children with some dehydration require a second course of ORT (defined as failure
of ORT for this study). Assuming a 50% reduction in failure
of ORT in ondansetron group with 90% power and a of 0.05,
sample size calculated was 77 children in each group. A sample size of 82 in each group was calculated to be sufficient to
reduce the intravenous fluid use from an estimated 30%9 to
10%, with 90% power and a of 0.05. For ORS intake, a sample size of 72 in each group was required to demonstrate
50 mL difference in ORS intake between the two groups
with group SD of 92 mL9 with 90% power and a of 0.05.
We decided to enroll a total of 170 children (85 in each
group) so as to be sufficient for these 3 primary outcomes.
SPSS version 17.0 (IBM, Armonk, New York) was used for
data analysis. Frequencies of children who failed ORT, those
requiring intravenous fluids, and those having at least 1 point
to 2 points improvement in caregiver satisfaction scores were
compared by c2 test. Mean (SD) amount of ORS intake and
change in caregiver satisfaction scores after 4 hours were
compared in two groups by Student t test. The duration of
dehydration correction in each group was compared by
Kaplan-Meier survival analysis censoring the cases at 8 hours
if they fail to correct dehydration by that time. For children
who needed intravenous fluids earlier than 8 hours or for
subjects who withdrew from the study earlier, censoring
was done at the last observation period.
Results
A total of 204 eligible children were screened during the
study period (April 2011 to July 2011 was the initial period
of procurement and repackaging of the drug, development
of placebo, testing for similarity in color, taste, and smell,
and designing randomization; patient enrollment occurred
August 2011 to March 2012), out of which 34 were
excluded. Figure 1 (available at www.jpeds.com) shows
the flow diagram of study and reasons for exclusion from
study.
Danewa et al
- 2015
ORIGINAL ARTICLES
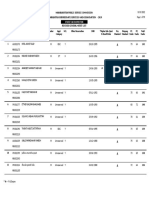
Table I. Comparison of baseline and anthropometric variables in ondansetron and placebo group
Total (N = 170)
Age (mo), mean (SD)
Sex, N (%)
Female
Male
Fever, N (%)
Duration of diarrhea before enrollment (d), Mean (SD)
Number of vomiting in last 6 h, mean (SD)
Dehydration score at admission (0 h)
Weight (kg), mean (SD)
Weight for age Z score, mean (SD)
Height/length (cm), mean (SD)
Height for age Z score, mean (SD)
Weight for height Z score, mean (SD)
Mid-arm circumference (cm), mean (SD)
Ondansetron (N = 85)
Placebo (N = 85)
15.3 (10.1)
15.5 (10.7)
15.0 (9.5)
71 (41.8)
99 (58.2)
61 (35.9)
2.2 (1.7)
6 (2.6)
12.8 (1.8)
8.6 (2.0)
1.30 (1.05)
74.3 (8.4)
1.23 (1.21)
0.88 (1.34)
13.06 (1.20)
31 (36.5)
54 (63.5)
25 (29.4)
2.0 (1.6)
6 (2.6)
12.5 (1.8)
8.7 (2.0)
1.29 (1.10)
74.5 (8.4)
1.23 (1.25)
0.95 (1.36)
13.03 (1.45)
40 (47.1)
45 (52.9)
36 (42.4)
2.3 (1.7)
6 (2.6)
13.1 (1.7)
8.6 (2.1)
1.30 (1.01)
74.2 (8.5)
1.24 (1.19)
0.81 (1.34)
13.08 (1.05)
Most of the study participants were infants (60%) and a
majority (93%) of them had watery diarrhea. The children
in both groups were comparable for baseline variables such
as anthropometry, duration of diarrhea, duration of vomiting, and dehydration score (Table I).
Table II shows the comparison of outcome variables
among the drug and placebo group. Failure of ORT was
almost one-half (30% absolute reduction) in children
receiving ondansetron in comparison with those receiving
placebo (P < .001, relative risk 0.50, 95% CI 0.35-0.72).
Around 20% of study subjects needed intravenous fluids;
the fluid requirement was seen in twice the number of
children in the placebo group in comparison with the drug
group. However, this did not reach statistical significance.
The amount of ORS consumed in 4 hours was significantly
more in children receiving ondansetron than those in the
placebo group. Figure 2 (available at www.jpeds.com)
depicts the survival function for the outcome of duration
of dehydration correction. Median duration of dehydration
correction was significantly less in children receiving
ondansetron than placebo (4 h vs 6 h, P < .001). The mean
number of vomiting episodes during 4 hours of observed
ORT was also significantly less in children receiving
ondansetron. Caregiver satisfaction in all fields (mood,
activity, alertness, comfort, number of vomiting episodes,
fluid intake) was better in the drug group compared with
the placebo group (Table III; available at www.jpeds.com).
Improvement by at least 2 points in score was seen in
almost twice the number of parents in the drug group
compared with the placebo group in all fields. The study
participants were observed for adverse effects like headache,
rash, or any other reported event, and no such adverse
effect was seen. No increase in diarrheal episodes was seen
with the use of anti-emetics.
Discussion
Diarrhea is one of the major causes of morbidity and mortality in children from the developing countries.1 Many healthcare providers perceive vomiting as a barrier to successful
execution of ORT. In our study, we found that a single oral
dose of ondansetron resulted in significantly fewer children
failing ORT, faster correction of dehydration, reduction of
vomiting episodes, and better caregiver satisfaction, without
any significant adverse event. The proportion of children
receiving intravenous fluids was, however, not statistically
different between the drug group and the placebo group.
The strength of the present study was the randomized,
double blind, placebo controlled design, and evaluation of
functional outcomes such as failure of ORT, receipt of intravenous fluids, duration of dehydration correction, and caregiver satisfaction. We did not limit ourselves to evaluation of
cessation of vomiting as was done in some previous studies.
The bias because of seasonal variation was minimized by
continuous enrollment throughout the year, and by block
randomization. We defined failure of ORT as persistence
of features of some dehydration after 4 hours of ORT. Varied definitions for failure of ORT have been used by different
researchers in different studies11,12; persistence of some level
of dehydration after completion of rehydration period is an
acceptable definition.11 As we used WHO guidelines for
rehydration, which recommend a duration of 4 hours for
Table II. Comparison of outcome variables in ondansetron and placebo group
Outcome variable
Ondansetron (N = 84)
Placebo (N = 83)
P value
Relative risk (95% CI)
Failure of ORT, N (%)
Intravenous fluid use, N (%)
ORS intake in 4 h (mL), mean (SD)
Number of vomiting in 4 h
26 (31.0)
12 (14.3)
645 (193)
1.8 (2.3)
51 (61.5)
21 (25.3)
554 (175)
3.6 (2.6)
<.001
.074
.002
<.001
0.50 (0.35, 0.72)
0.56 (0.30, 1.07)
91.3* (35.0, 147.6)
1.8* ( 2.6, 1.1)
*Mean difference and 95% CI for outcome of ORS intake and number of vomiting in 4 h.
Oral Ondansetron in Management of Dehydrating Diarrhea with Vomiting in Children Aged 3 Months to 5 Years:
A Randomized Controlled Trial
THE JOURNAL OF PEDIATRICS
rehydration, we defined treatment failure as some dehydration persisting after 4 hours of ORT. Receipt of intravenous
fluids was a composite definition that depended on the clinical indications of intravenous fluids. Although these 2 outcomes are inter-related, we believed that though persistence
of intravenous fluids after 1 full course (4 hours) of ORT
may not be an indication for using intravenous fluids, it is
an important functional outcome to be evaluated separately.
The main limitation of our study was the short duration of
monitoring and lack of follow-up to know the revisit rate. We
also did not investigate the etiology of diarrhea in our study.
Use of WHO definition for dehydration might have induced
some subjectivity; we utilized it for assessing the outcomes as
it is the most widely used definition for management of diarrhea in our and similar settings. We could document an increase in ORS intake, but the results related to intravenous
fluid use were not statistically significant. This could be
because of less proportion (than estimated) of children
requiring intravenous fluids, because of strict criteria used
for administration of intravenous fluids. Moreover, we
were looking at a larger difference in reduction of intravenous fluids use (30% to 10%), and our study may not be
powered enough to detect smaller (may still be clinically
meaningful) difference. The sample size was too small to
evaluate rare adverse effects due to drug.
The direction of the results of our study was comparable
with that reported in the Cochrane review13 on the role of
anti-emetics for reducing vomiting related to acute gastroenteritis in children and adolescents, where 60% reduction in
the use of intravenous therapy was shown in the ondansetron
group compared with controls. The drug was found to be
effective in reducing the number of vomiting episodes.
Yilmaz et al14 found a higher proportion of subjects in the
ondansetron group who were able to tolerate ORT compared
with the placebo group (relative risk 1.17; 95% CI: 0.99 to
1.38, P = .06). Higher ORS intake in initial 4 hours of ORT
in ondansetron group in our study was similar to results by
Freedman et al9 (239 mL vs 196 mL, P < .001). A study by
Mullarkey et al15 documented 19% reduction in intravenous
fluid administration on adding oral ondansetron to ORT
regimen. A systematic evaluation of all Cochrane reviews
evaluating commonly used interventions in developed countries by Freedman et al showed significant reduction in the
hospital admission and intravenous rehydration rates with
oral ondansetron.16 We documented faster correction of
dehydration after single dose of oral ondansetron and better
caregiver satisfaction. These outcomes, though important,
have not been evaluated in earlier studies.
In the present study, we did not find any adverse effect
during the initial 4 hours of observation. A systematic review
and meta-analysis by Decamp et al17 on use of antiemetic
agents in acute gastroenteritis reported that diarrheal episodes increased in ondansetron group. We did not observe
any increase in diarrhea with ondansetron use.
The Canadian Pediatric Society recommended considering
the use of a single dose of oral ondansetron in children aged
6 months to 12 years presenting with acute gastroenteritis
4
Vol. -, No. -
www.jpeds.com
and vomiting as a prominent symptom, mild to moderate
dehydration, or have failed ORT.18 Current WHO diarrhea
management guidelines and American Academy of Pediatrics
guidelines19 do not recommend the use of anti-emetics in
management of diarrheal dehydration. There are no definite
guidelines from other parts of the world, but the hospitallevel analysis from the US has documented a marked increase
in the use of ondansetron between 2002 and 2011.20 This,
however, did not result in reduction of intravenous fluid
use, probably because of improper use (not given timely,
not waiting for its effect before intravenous fluid administration) in real settings.21,22 Our results favored the use of ondansetron to overcome the barrier of vomiting in successful
implication of ORT therapy by reducing the proportion of
children who failed ORT. However, one needs to study the
metrics around failure of ORT other than vomiting and
decision to administer ondansetron. n
Submitted for publication Jun 8, 2015; last revision received Aug 25, 2015;
accepted Oct 2, 2015.
Reprint requests: Dheeraj Shah, MD, DNB, MNAMS, FIAP, Department of
Pediatrics, UCMS and GTB Hospital, Dilshad Garden, Delhi-110095, India.
E-mail: shahdheeraj@hotmail.com
References
1. Sample Registration System: Special Survey of Deaths. Report on Causes
of Death: 2001-03, Office of Registrar General, India.
2. International Institute of Population Sciences (IIPS) and Macro International. National Family Health Survey (NFHS-3), 2005-2006: India,
Volume I. Mumbai: IIPS; 2007.
3. Diarrhea: Why children are still dying and what should be done. http://
www.unicef.org/media/files/Final_Diarrhoea_Report_October_2009_
final.pdf. Accessed August 03, 2015.
4. Shah D, Choudhury P, Gupta P, Mathew JL, Gera T, Gogia S, et al. Promoting appropriate management of diarrhea: a systematic review of
literature for advocacy and action: UNICEF-PHFI series on newborn
and child health, India. Indian Pediatr 2012;49:627-49.
5. Ramsook C, Sahagun-Carreon I, Kozinetz CA, Moro-Sutherland D. A
randomized clinical trial comparing oral ondansetron with placebo in
children with vomiting from acute gastroenteritis. Ann Emerg Med
2002;39:397-403.
6. Van Eygen M, Dhondt F, Heck E, Ameryckx L, Van Ravensteyn H. A
double blind comparison of domperidone and metoclopramide suppositories in the treatment of nausea and vomiting in children. Postgrad
Med J 1979;55(Suppl 1):36-9.
7. Dhondt F, Traen S, VanEygen M, Baran D, Willaert H. Domperidone
(R-33812) suppositories: an effective antiemetic agent in diverse pediatric conditions: multicenter trial. Curr Ther Res Clin Exp 1978;24:912-23.
8. World Health Organization. The Treatment of Diarrhea: A Manual for
Physicians and Other Senior Healthcare Workers. Geneva: World Health
Organization; 2005.
9. Freedman SB, Adler M, Seshadri R, Powell EC. Oral ondansetron for
gastroenteritis in a pediatric emergency department. N Engl J Med
2006;354:1698-705.
10. Gupta H, Shah D, Gupta P, Sharma KK. Role of paracetamol in treatment of childhood fever: a double blind randomized placebo controlled
trial. Indian Pediatr 2007;44:903-11.
11. Bellemare S, Hartling L, Wiebe N, Russell K, Craig WR, McConnell D,
et al. Oral rehydration versus intravenous therapy for treating dehydration due to gastroenteritis in children: a meta-analysis of randomized
controlled trials. BMC Med 2004;2:11.
12. Hartling L, Bellemare S, Wiebe N, Russell KF, Klassen TP, Craig WR.
Oral versus intravenous rehydration for treating dehydration due to
Danewa et al
- 2015
13.
14.
15.
16.
17.
gastroenteritis in children (Review). Cochrane Database Syst Rev 2006;3:
CD004390.
Fedorowicz Z, Jagannath VA, Carter B. Anti-emetics for reducing vomiting related to acute gastroenteritis in children and adolescents. Cochrane Database Syst Rev 2011;9:CD005506.
Yilmaz HL, Yildizdas RD, Sertdemir Y. A randomized clinical trial: oral
ondansetron for reducing vomiting secondary to acute gastroenteritis in
children. Ann Emerg Med 2008;1:82-3.
Mullarkey C, Crowley E, Martin C. The addition of ondansetron to an
oral rehydration protocol for children with acute gastroenteritis. Ir
Med J 2013;106:66-8.
Freedman SB, Ali S, Oleszczuk M, Gouin S, Hartling L. Treatment of
acute gastroenteritis in children: an overview of systematic reviews of interventions commonly used in developed countries. Evid Based Child
Health 2013;8:1123-37.
DeCamp LR, Byerley JS, Doshi N, Steiner MJ. Use of anti-emetic agents
in acute gastroenteritis: a systematic review and meta-analysis. Arch Pediatr Adolesc Med 2008;162:858-65.
ORIGINAL ARTICLES
18. Cheng A. Canadian Pediatric Society, Acute Care Committee. Emergency department use of oral ondansetron for acute gastroenteritis
related vomiting in infants and children. Pediatr Child Health 2011;16:
177-9.
19. American Academy of Pediatrics, Provisional Committee on Quality
Improvement and Subcommittee on Acute Gastroenteritis. Practice
parameter: the management of acute gastroenteritis in young children.
American Academy of Pediatrics, Provisional Committee on Quality
Improvement, Subcommittee on Acute Gastroenteritis. Pediatrics
1996;97:424-35.
20. Freedman SB, Hall M, Shah SS, Kharbanda AB, Aronson PL,
Florin TA, et al. Impact of increasing ondansetron use on clinical
outcomes in children with gastroenteritis. JAMA Pediatr 2014;168:
321-9.
21. Keren R. Ondansetron for acute gastroenteritis: a failure of knowledge
translation. JAMA Pediatr 2014;168:308-9.
22. Is Ondansetron any use in gastroenteritis? Arch Dis Child 2015;100:
225.
Oral Ondansetron in Management of Dehydrating Diarrhea with Vomiting in Children Aged 3 Months to 5 Years:
A Randomized Controlled Trial
THE JOURNAL OF PEDIATRICS
www.jpeds.com
Vol. -, No. -
Figure 1. Flow of participants in the study.
5.e1
Danewa et al
- 2015
ORIGINAL ARTICLES
Figure 2. A, Kaplan-Meier survival and B, one minus survival
curves for duration of dehydration correction.
Oral Ondansetron in Management of Dehydrating Diarrhea with Vomiting in Children Aged 3 Months to 5 Years:
A Randomized Controlled Trial
5.e2
THE JOURNAL OF PEDIATRICS
Vol. -, No. -
www.jpeds.com
Table III. Comparison of caregiver satisfaction after 4 hours of ORT in ondansetron and placebo groups
Ondansetron (N = 84)
Placebo (N = 83)
P value*
1.2 (0.99)
68 (81.0)
42 (50)
0.6 (1.12)
51 (61.5)
20 (24.1)
.01
.005
<.001
1.1 (0.98)
69 (82.1)
32 (38.1)
0.6 (1.00)
51 (61.5)
13 (15.7)
.004
.003
.001
1.1 (0.94)
70 (83.3)
33 (39.3)
0.6 (1.06)
50 (60.2)
14 (16.9)
.001
<.001
.001
1.1 (0.98)
66 (78.6)
32 (38.1)
0.4 (1.11)
46 (55.4)
15 (18.1)
<.001
.001
.004
1.4 (1.18)
66 (78.6)
46 (54.8)
0.5 (1.15)
40 (48.2)
20 (24.1)
<.001
<.001
<.001
1.2 (0.91)
70 (83.3)
33 (39.3)
0.5 (1.12)
46 (55.4)
17 (20.5)
<.001
<.001
.008
Mood
Change in score from baseline, mean (SD)
Improvement by at least 1 score, N (%)
Improvement by at least 2 scores, N (%)
Activity
Change in score from baseline, mean (SD)
Improvement by at least 1 score, N (%)
Improvement by at least 2 scores, N (%)
Alertness
Change in score from baseline, mean (SD)
Improvement by at least 1 score, N (%)
Improvement by at least 2 scores, N (%)
Comfort
Change in score from baseline, mean (SD)
Improvement by at least 1 score, N (%)
Improvement by at least 2 scores, N (%)
Vomiting
Change in score from baseline, mean (SD)
Improvement by at least 1 score, N (%)
Improvement by at least 2 scores, N (%)
Fluid intake
Change in score from baseline, mean (SD)
Improvement by at least 1 score, N (%)
Improvement by at least 2 scores, N (%)
*By Student t test for comparing mean (SD) score and c2 test for comparing proportion.
5.e3
Danewa et al
Potrebbero piacerti anche
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Performing A Comprehensive Epicardial Echo ExamDocumento11 paginePerforming A Comprehensive Epicardial Echo ExamPitoAdhiNessuna valutazione finora
- Piba Rot 2000Documento11 paginePiba Rot 2000PitoAdhiNessuna valutazione finora
- Performance of A Comprehensive Intraoperative Epiaortic Ultrasonographic ExamDocumento9 paginePerformance of A Comprehensive Intraoperative Epiaortic Ultrasonographic ExamPitoAdhiNessuna valutazione finora
- 2008 Cardiac Resynchronization TherapyDocumento23 pagine2008 Cardiac Resynchronization TherapyPitoAdhiNessuna valutazione finora
- Use of Carotid US To ID Subclinical Vasc Disease and Eval Disease RiskDocumento19 pagineUse of Carotid US To ID Subclinical Vasc Disease and Eval Disease RiskPitoAdhiNessuna valutazione finora
- Athappan 2013Documento11 pagineAthappan 2013PitoAdhiNessuna valutazione finora
- HealthyforGood PhysicalActivity Adult Infographic FINAL PDFDocumento1 paginaHealthyforGood PhysicalActivity Adult Infographic FINAL PDFLuis DominguezNessuna valutazione finora
- Editorial TASC IIDocumento2 pagineEditorial TASC IIPitoAdhiNessuna valutazione finora
- Performance Interpretation and App of Stress EchoDocumento21 paginePerformance Interpretation and App of Stress EchoPitoAdhiNessuna valutazione finora
- D2-Excessive Endurance ExerciseDocumento9 pagineD2-Excessive Endurance ExerciseJad SoaiNessuna valutazione finora
- Inter Society Consensus For The Management of PAOD TASC II GuidelinesDocumento70 pagineInter Society Consensus For The Management of PAOD TASC II GuidelinesPitoAdhiNessuna valutazione finora
- Chest X Rays in Pediatric CardiologyDocumento35 pagineChest X Rays in Pediatric CardiologyPitoAdhiNessuna valutazione finora
- Tasc II 2015 Update On AliDocumento15 pagineTasc II 2015 Update On AliPitoAdhiNessuna valutazione finora
- Aetiology of Sudden Cardiac Death in SportDocumento7 pagineAetiology of Sudden Cardiac Death in SportPitoAdhiNessuna valutazione finora
- European Heart Journal - Cardiovascular Imaging Volume 17 Issue Suppl 2 2016 (Doi 10.1093 - Ehjci - Jew248.002) Jung, IH. Kurnicka, K. Enache, R. Nagy, AI. Martins, E. Cer - P569Diastolic DyssynDocumento26 pagineEuropean Heart Journal - Cardiovascular Imaging Volume 17 Issue Suppl 2 2016 (Doi 10.1093 - Ehjci - Jew248.002) Jung, IH. Kurnicka, K. Enache, R. Nagy, AI. Martins, E. Cer - P569Diastolic DyssynPitoAdhiNessuna valutazione finora
- Excercise Recommendations For Stroke Survivors Ucm - 463998Documento1 paginaExcercise Recommendations For Stroke Survivors Ucm - 463998PitoAdhiNessuna valutazione finora
- Exercise and The HeartDocumento25 pagineExercise and The HeartPitoAdhiNessuna valutazione finora
- 10 1 1 553 2590 PDFDocumento3 pagine10 1 1 553 2590 PDFPitoAdhiNessuna valutazione finora
- Cororanary Artery FistulaDocumento4 pagineCororanary Artery FistulaPitoAdhiNessuna valutazione finora
- Impact of Valve Prosthesis-PatientDocumento7 pagineImpact of Valve Prosthesis-PatientPitoAdhiNessuna valutazione finora
- 508 Hormone Therapy Supplemental 100311Documento6 pagine508 Hormone Therapy Supplemental 100311elisasusantiNessuna valutazione finora
- Such As Activation of The Extracellular SignalDocumento1 paginaSuch As Activation of The Extracellular SignalPitoAdhiNessuna valutazione finora
- Jurnal Mba Sari 1Documento44 pagineJurnal Mba Sari 1PitoAdhiNessuna valutazione finora
- Aetiology of Sudden Cardiac Death in SportDocumento7 pagineAetiology of Sudden Cardiac Death in SportPitoAdhiNessuna valutazione finora
- 10 1152@physiol 00030 2016Documento10 pagine10 1152@physiol 00030 2016PitoAdhiNessuna valutazione finora
- Rehabilitation European Journal of Cardiovascular PreventionDocumento7 pagineRehabilitation European Journal of Cardiovascular PreventionPitoAdhiNessuna valutazione finora
- Chest X Rays in Pediatric CardiologyDocumento35 pagineChest X Rays in Pediatric CardiologyPitoAdhiNessuna valutazione finora
- Ronde September10Documento22 pagineRonde September10PitoAdhiNessuna valutazione finora
- GPCR 1Documento70 pagineGPCR 1PitoAdhiNessuna valutazione finora
- Circulation 1990 Berger 401 11Documento12 pagineCirculation 1990 Berger 401 11PitoAdhiNessuna valutazione finora
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (120)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Drug Study 1Documento2 pagineDrug Study 1Hafza MacabatoNessuna valutazione finora
- Uti StudiesDocumento10 pagineUti Studiesapi-302840362Nessuna valutazione finora
- Maharashtra Public Service Commission Maharashtra Subordinate Services Main Examination - 2019Documento59 pagineMaharashtra Public Service Commission Maharashtra Subordinate Services Main Examination - 2019S KatyarmalNessuna valutazione finora
- Group1-FINAL-Chapter-1-2-3 (G1)Documento46 pagineGroup1-FINAL-Chapter-1-2-3 (G1)Sydney BautistaNessuna valutazione finora
- B Biokinetics 2023Documento10 pagineB Biokinetics 2023ZandileNessuna valutazione finora
- PsikosomatikDocumento65 paginePsikosomatikHengki Permana PutraNessuna valutazione finora
- ESI ER CompleteDocumento45 pagineESI ER Completetammy2121Nessuna valutazione finora
- Rachel Tucker Resume 2020Documento1 paginaRachel Tucker Resume 2020api-489845523Nessuna valutazione finora
- ADS Dec 27Documento1.946 pagineADS Dec 27Robert Andrew BaldadoNessuna valutazione finora
- Musculoskeletal Clinical Translation FrameworkDocumento1 paginaMusculoskeletal Clinical Translation FrameworkRafaelNessuna valutazione finora
- Inguinal Hernias: BMJ (Online) March 2008Documento5 pagineInguinal Hernias: BMJ (Online) March 2008Karl PinedaNessuna valutazione finora
- V-Gel Cleaning & User GuideDocumento3 pagineV-Gel Cleaning & User GuideInstrulife OostkampNessuna valutazione finora
- Polytechnic of Health Denpasar Is An Institution of Higher Education Official of The Department of Health Which Is The Technical Implementation UnitDocumento1 paginaPolytechnic of Health Denpasar Is An Institution of Higher Education Official of The Department of Health Which Is The Technical Implementation UnitDewi PradnyaniNessuna valutazione finora
- Pathophysiology of Neonatal Sepsis Secondary To Neonatal PneumoniaDocumento4 paginePathophysiology of Neonatal Sepsis Secondary To Neonatal Pneumoniapaul andrew laranjo asuncion80% (5)
- Students Sleep During Classes: The Amount of Time VariesDocumento7 pagineStudents Sleep During Classes: The Amount of Time Variesjason_aaNessuna valutazione finora
- Fragility of MarriageDocumento10 pagineFragility of MarriageMichelleNessuna valutazione finora
- Extend XT - Folleto ComercialDocumento6 pagineExtend XT - Folleto ComercialMuhamadZuhdiAlWaliNessuna valutazione finora
- Job Chart of Physical Education Teachers - AP GOVTDocumento3 pagineJob Chart of Physical Education Teachers - AP GOVTRamachandra Rao100% (1)
- 2020 HivDocumento1 pagina2020 HivhenkNessuna valutazione finora
- SAS Blank Monitoring Report 7Documento16 pagineSAS Blank Monitoring Report 7Rodjan Moscoso100% (1)
- 2021 IWBF Classification Rules Version 202110 1Documento108 pagine2021 IWBF Classification Rules Version 202110 1Sebastian Alfaro AlarconNessuna valutazione finora
- Lecture 1 Health, Safety & Environment (HSE)Documento23 pagineLecture 1 Health, Safety & Environment (HSE)A to z type videosNessuna valutazione finora
- Pecial Eature: Transitions in Pharmacy Practice, Part 3: Effecting Change-The Three-Ring CircusDocumento7 paginePecial Eature: Transitions in Pharmacy Practice, Part 3: Effecting Change-The Three-Ring CircusSean BlackmerNessuna valutazione finora
- Profile of Osteopathic Practice in Spain Results FDocumento11 pagineProfile of Osteopathic Practice in Spain Results FBerenice LimarkNessuna valutazione finora
- Interpretation: LPL - PSC Chandigarh Sector 19-D Booth No:-3, Sector:-19-D ChandigarhDocumento5 pagineInterpretation: LPL - PSC Chandigarh Sector 19-D Booth No:-3, Sector:-19-D ChandigarhSanNessuna valutazione finora
- Cerad Total ScoreDocumento6 pagineCerad Total ScorecoconitaNessuna valutazione finora
- Dr. Dan Siegel - Resources - Healthy Mind PlatterDocumento4 pagineDr. Dan Siegel - Resources - Healthy Mind PlatterInês Novais100% (4)
- 2018 MUSE Inspire Conference - Show and Tell SessionsDocumento13 pagine2018 MUSE Inspire Conference - Show and Tell SessionsMichele LambertNessuna valutazione finora
- Blood Testing For DioxinsDocumento2 pagineBlood Testing For DioxinstedmozbiNessuna valutazione finora
- Physiological Changes Postpartum PeriodDocumento2 paginePhysiological Changes Postpartum PeriodEurielle MioleNessuna valutazione finora