Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Self Assesment Ulcer Prevention
Caricato da
yaniCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Self Assesment Ulcer Prevention
Caricato da
yaniCopyright:
Formati disponibili
Agency for Healthcare Research and Quality
Safety Program for Nursing Homes: On-Time Prevention
On-Time Pressure Ulcer Prevention
Self-Assessment Worksheet for Pressure Ulcer
The Self-Assessment Worksheet is designed to help staff review how they currently identify
residents who have experienced a change in pressure ulcer risk, how they determine if new
clinical interventions are needed, and how they determine what those interventions are. The selfassessment tool is intended to help identify the current processes and structures the nursing home
uses to prevent pressure ulcers and identify gaps and places for improvement. It is intended to
help staff think about ways to transform these processes and how to begin to use the pressure
ulcer prevention reports in clinical discussions. The self-assessment tool is an important first step
in implementing the reports into current workflow.
The team is expected to use the Self-Assessment Worksheet to help understand current pressure
ulcer prevention practices. This is the first step to help them determine how to transform their
current practices and to identify ways to incorporate the On-Time Reports into current practice. It
is expected that the facilitator will work with the change team to identify gaps in current pressure
ulcer prevention practices and help them see ways to incorporate the reports to improve these
practices and improve clinical interventions.
The Self-Assessment Worksheet shows how the nursing home:
Identifies how they identify which residents are at risk of pressure ulcers,
Identifies how they develop interventions to prevent pressure ulcer formation,
Identifies how they discuss at-risk residents and formulate changes in care plans, and
Identifies how they carry out root cause analysis when a pressure ulcer occurs.
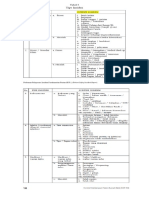
The Self-Assessment Worksheet has four sectons:
Section 1: Screening for Pressure Ulcer Risk
Section 2: Pressure Ulcer Prevention Plan
Section 3: Communication Practices
Section 4: Investigations/Root Cause Analysis of Pressure Ulcer Development
Self-Assessment Worksheet for Pressure Ulcer Prevention
Agency for Healthcare Research and Quality
Safety Program for Nursing Homes: On-Time Prevention
Self-Assessment Worksheet for Pressure Ulcer Prevention
Section 1: Screening for Pressure Ulcer Risk
In this section, we would like to learn more about your facilitys pressure ulcer risk activities.
1. Does your facility have a pressure ulcer risk policy?
Yes No If no, skip to Question 3.
2. If yes, does the policy include the following:
a.
Clinical areas to be covered
b.
Timing or frequency of assessments
c.
Documentation requirements
d.
Communication to care team
Yes
No
3. Does your facility provide training to nursing staff on how to accurately assess for pressure
ulcer risk?
Yes No
4. Does the pressure ulcer risk assessment use a standardized assessment tool (for example,
Braden score of Norton tool)?
Yes No If yes, skip to Question 6.
5. If not using a standardized tool, does the assessment tool that the facility uses cover the
following:
a.
Impaired mobility
b.
Incontinence
c.
Nutritional deficits
d.
Diabetes diagnosis
e.
Peripheral vascular disease diagnosis
f.
Contractures
g.
History of pressure ulcers
h.
Paralysis
Self-Assessment Worksheet for Pressure Ulcer Prevention
Yes
No
Agency for Healthcare Research and Quality
Safety Program for Nursing Homes: On-Time Prevention
6. How frequently is the risk assessment tool completed?
a. Monthly
b. Quarterly
c. Annually
d. Change of condition
e. Other (specify): _________________________________________________________
7. When are residents screened for pressure ulcer risk? Check all that apply.
a. Upon admission/readmission
b. With a change in condition
c. With each MDS assessment
d. When weight loss has occurred
e. Change in meal intake
f. Change in fluid intake
g. Change in mobility
h. Change in continence
i. Change in communication
8. Do your facilitys pressure ulcer risk assessment activities include a comprehensive skin
assessment/inspection*?
Yes No
*A comprehensive skin assessment is defined as a full head to toe and front and back
assessment of the skin, the bodys largest organ, for any breakdown or reddened areas. This
includes attention to all bony prominences, ears, scalp, in between toes, etc.
9. Who completes the skin assessment/inspection on admission?
a. Admitting nurse
b. Nursing assistant
c. Wound/skin care nurse
d. Nurse manager
e. Nursing supervisor
f. Director of nursing
g. Other (specify) __________________________________________________________
Self-Assessment Worksheet for Pressure Ulcer Prevention
Agency for Healthcare Research and Quality
Safety Program for Nursing Homes: On-Time Prevention
10. Who completes routine skin assessments/inspections?
a. Unit nurse
b. Nursing assistant
c. Wound care nurse
d. Other (specify): _________________________________________________________
11. How often are skin assessments/inspections completed?
a. Daily
b. Weekly
c. Monthly
d. Other (specify): _________________________________________________________
12. Where are skin assessments/inspections documented?
a. Medical record
b. Nursing assistant documentation
c. Skin assessment form
d. Other (specify): _________________________________________________________
13. Do you screen all residents for pressure ulcer risk at the following times:
a. Upon admission
Yes No
b. Upon readmission/reentry
Yes No
c. When there is a change in condition
Yes No
d. With each MDS assessment
Yes No
14. If the resident is not currently deemed at risk, is there a plan to rescreen at regular intervals?
Yes No
15. Do you screen residents for pressure ulcer risk with the following diagnoses?
a. Diabetes mellitus
Yes No
b. Peripheral vascular disease
Yes No
c. History of pressure ulcer
Yes No
d. Paralysis
Yes No
Self-Assessment Worksheet for Pressure Ulcer Prevention
Agency for Healthcare Research and Quality
Safety Program for Nursing Homes: On-Time Prevention
Section 2: Pressure Ulcer Prevention Plan
For residents at risk, we would like to learn what is included in your pressure ulcer prevention
care plan.
1. Do you develop a care plan for residents at risk of developing a pressure ulcer?
Yes No If not, skip to Section 3.
2. Does your plan include interventions for skin care?
Yes No
3. Does your plan include daily skin assessments of pressure points?
Yes No
3A. Does your daily assessment assess the following areas?
4.
a. Sacrum
Yes No
b. Ischium
Yes No
c. Trochanters
Yes No
d. Heels
Yes No
e. Elbows
Yes No
f. Back of the head
Yes No
g. Ears/nose
Yes No
Does your plan include interventions addressing nutrition and hydration?
Yes No
4A. Does your plan include interventions to address:
a. Feeding or swallowing difficulties
Yes No
b. Undernourishment (e.g., weight loss, decreased meal intake) Yes No
5. Does your plan include a nutritional screen for residents at risk of developing a pressure
ulcer?
Yes No
Self-Assessment Worksheet for Pressure Ulcer Prevention
Agency for Healthcare Research and Quality
5A
6.
Safety Program for Nursing Homes: On-Time Prevention
Does the screen include any of the following:
a. Estimation of nutritional requirements
Yes No
b. Comparison of nutrient intake with estimated requirements
Yes No
c. Recommendation for frequency of reassessment of
nutritional status
Yes No
d. Weight pattern change summary
Yes No
Does your plan include an assessment for pain?
Yes No
7.
Does your plan include an assessment for decreased mental status?
Yes No
8.
Does your plan include an assessment for incontinence?
Yes No
9.
Does your plan include an assessment for medical device-related pressure?
Yes No
9A. Do recommendations for positioning include the following?
a. Dealing with medical devices (oxygen tubing, catheters)
b. Guidance for avoiding friction and shear
c. Support surfaces
d. Frequency of repositioning
10.
Does your plan include an assessment for friction and shear?
Yes No
10a. Does your plan include an assessment for muscle spasms?
Yes No
11.
Does your plan include an assessment for immobility?
Yes No
12.
Does your plan include an assessment for contractures?
Yes No
Self-Assessment Worksheet for Pressure Ulcer Prevention
Self-Assessment Worksheet for Pressure Ulcer Prevention
Safety Program for Nursing Homes: On-Time Prevention
Meeting
Care plan review
Report or brief with CNAs
Report or brief with department heads
Medical staff
QAPI* or performance improvement
plan meeting
f. Skin or wound meeting
g. MD/APRN* rounds
h. Report or brief with Dietary
Department
i. Report or brief with Social Services
Department
j. Report or brief with Therapy
Department
k. Report or brief with Other
Meeting
Chair/Leader Name
and Discipline
Staff Invited
and in Attendance
(indicate A Always,
V- Varies as needed)
* QAPI = Quality Assessment and Performance Improvement; APRN = advanced practice registered nurse.
a.
b.
c.
d.
e.
Pressure Ulcer
Prevention
Discussed Yes/No
Frequency of
Meeting (Weekly,
Biweekly, Monthly,
Quarterly, Change in
Condition,
As Needed)
1. We are interested in how you communicate the pressure ulcer risk and prevention care plans to the interdisciplinary team. Please
review the following list of meetings. For every meeting that occurs at your facility, indicate how often it occurs, who leads the
meeting, and who attends.
Section 3: Communication Practices
Agency for Healthcare Research and Quality
Agency for Healthcare Research and Quality
On-Time Quality Improvement Program
2. Training
Indicate the date of the most recent training provided for the following:
a.
b.
c.
d.
e.
f.
g.
Topic
Conducting an accurate skin assessment
Conducting an accurate skin assessment
Effective positioning
Effective positioning
Skin care
Documentationmeal and fluid intake
Documentationpositioning
Self-Assessment Worksheet for Pressure Ulcer Prevention
Participants
Nurses
CNAs
Nurses
CNAs
CNAs
CNAs
CNAs
Date
Agency for Healthcare Research and Quality
On-Time Quality Improvement Program
Section 4: Investigations/Root Cause Analysis of Pressure Ulcer Development
1. Do you investigate each new in-house pressure ulcer according to your facilitys policies and
guidelines?
Yes No Not Sure
2. Do you investigate each new in-house pressure ulcer in a root cause framework?
Yes No Not Sure If no or not sure, stop here.
3. In the course of your root cause analysis, do you look at the most recent pressure ulcer
risk screen?
Yes No
If yes, how do you check the accuracy of that screen?
4. In the course of your root cause analysis, do you check to see if the risk status of the resident
has changed?
Yes No
If yes, would your investigation include any of the following factors as affecting risk for a
pressure ulcer? Check all that apply.
a. Change in condition
b. Weight loss
c. Change in meal intake
d. Change in fluid intake
e. Change in mobility
f. Change in continence
g. Change in ability to communicate pain
h. Other (specify): ________________________________________________________
i. Other (specify): ________________________________________________________
Self-Assessment Worksheet for Pressure Ulcer Prevention
Agency for Healthcare Research and Quality
On-Time Quality Improvement Program
5. Please review the following list of assessments to identify appropriate interventions to
address pressure ulcer risk. Check the one(s) that you would investigate as part of your root
cause analysis:
a. Nutrition assessment for a resident with decreased meal or fluid intake
b. Nutrition screen for a resident at risk of developing a pressure ulcer
c. Pain assessment
d. Cognitive assessment
e. Incontinence assessment
f. Medical device-related pressure assessment (e.g., oxygen tubing, catheters)
g. Assessment for friction and shear
h. Mobility assessment
i. Contracture assessment
j. Assessment for appropriate bed and chair support surfaces
k. Positioning assessment
l. Skin assessments per frequency designated by MD/NP
m. Other (specify): ________________________________________________________
n. Other (specify): ________________________________________________________
6. Assessments may reveal that a particular action should be taken (e.g., a toileting routine to
prevent incontinence, diet change to encourage increased intake, new cushion for
wheelchair). How would you find out if an intervention had been identified as necessary, but
not carried out?
7. Are there any particular obstacles or challenges to investigating the root cause of pressure
ulcers?
Self-Assessment Worksheet for Pressure Ulcer Prevention
10
Potrebbero piacerti anche
- DrentechSimple BrochureDocumento2 pagineDrentechSimple BrochureyaniNessuna valutazione finora
- Jenis InsidenDocumento5 pagineJenis InsidenyaniNessuna valutazione finora
- Collecting A Sputum Specimen Geisinger Medical Laboratory MicrobiologyDocumento43 pagineCollecting A Sputum Specimen Geisinger Medical Laboratory MicrobiologyyaniNessuna valutazione finora
- National Patient Safety GoalsDocumento7 pagineNational Patient Safety GoalsyaniNessuna valutazione finora
- Requestedfile Hfmea Abduction ChildDocumento78 pagineRequestedfile Hfmea Abduction Childyani0% (1)
- Student ExchangeDocumento1 paginaStudent ExchangeyaniNessuna valutazione finora
- Please Fill The Form by Typing: (If You Give More Than One, Please Indicate Which Is The Primary Address)Documento2 paginePlease Fill The Form by Typing: (If You Give More Than One, Please Indicate Which Is The Primary Address)yaniNessuna valutazione finora
- Tetanus: Information For Health Professionals.: HPA-CDSC November 2003Documento6 pagineTetanus: Information For Health Professionals.: HPA-CDSC November 2003yaniNessuna valutazione finora
- Summary FGD Mapping KE 2001Documento17 pagineSummary FGD Mapping KE 2001yaniNessuna valutazione finora
- Guideline For Disinfection and Sterilization in Healthcare FacilitiesDocumento6 pagineGuideline For Disinfection and Sterilization in Healthcare FacilitiesyaniNessuna valutazione finora
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Effects of Advanced Carbohydrate Counting On Glucose Control and QolDocumento9 pagineEffects of Advanced Carbohydrate Counting On Glucose Control and QollloplNessuna valutazione finora
- CLUBFOOT GuidelineDocumento111 pagineCLUBFOOT GuidelineNuhiat NahreenNessuna valutazione finora
- Malabsorption SyndromeDocumento7 pagineMalabsorption SyndromeHassan.shehri100% (4)
- Report 5 - Najihah - Group A1Documento8 pagineReport 5 - Najihah - Group A1nurul fatinajihahNessuna valutazione finora
- Contact Nummular (Discoid) Eczema From Depilating Cream: Case ReportDocumento2 pagineContact Nummular (Discoid) Eczema From Depilating Cream: Case ReportMorindaNessuna valutazione finora
- Vaccination Certificate 20435699572410Documento1 paginaVaccination Certificate 20435699572410MANOJ BHADANENessuna valutazione finora
- 3M Bair Hugger Gown SystemDocumento4 pagine3M Bair Hugger Gown SystemmochkurniawanNessuna valutazione finora
- Intrapartum HandoutDocumento29 pagineIntrapartum HandoutZahNessuna valutazione finora
- Legal and Ethical Aspects of Genetic Screening and Counseling Role of Nurse in Genetic CounselingDocumento41 pagineLegal and Ethical Aspects of Genetic Screening and Counseling Role of Nurse in Genetic CounselingAmy Lalringhluani67% (3)
- Compilation AnesthesiaDocumento5 pagineCompilation AnesthesiaNorjetalexis CabreraNessuna valutazione finora
- Home Visit PlanDocumento2 pagineHome Visit Planako at ang exoNessuna valutazione finora
- FC Derm (SA) Regulations 26-3-2014Documento13 pagineFC Derm (SA) Regulations 26-3-2014matentenNessuna valutazione finora
- 2012 OiteDocumento256 pagine2012 Oiteaddison wood100% (4)
- Emergency Report Thursday:, October 07 2021Documento21 pagineEmergency Report Thursday:, October 07 2021Wilson WijayaNessuna valutazione finora
- Unang Yakap DOH EINCDocumento20 pagineUnang Yakap DOH EINCLore Anne Mhae Santos100% (1)
- Colchicine Drug Study For Gouty ArthritisDocumento3 pagineColchicine Drug Study For Gouty ArthritisLeslie PaguioNessuna valutazione finora
- Punjab Public Service CommissionDocumento2 paginePunjab Public Service CommissionShehnila ShoukatNessuna valutazione finora
- Histological Comparison of Pulpal Inflamation in Primary Teeth With Occlusal or Proximal CariesDocumento8 pagineHistological Comparison of Pulpal Inflamation in Primary Teeth With Occlusal or Proximal CariesGilmer Solis SánchezNessuna valutazione finora
- Radiographic Aids in The Diagnosis of Periodontal Diseases: Presented By: DR: Abdullah AliDocumento27 pagineRadiographic Aids in The Diagnosis of Periodontal Diseases: Presented By: DR: Abdullah AliMugahed Abdo Al-gahdariNessuna valutazione finora
- بنك الأسئلةDocumento775 pagineبنك الأسئلةسماح صلاح100% (1)
- Slide Materi Dr. Kevin Triangto, SPKFR - Heart Failure - PMR4GP 2022Documento27 pagineSlide Materi Dr. Kevin Triangto, SPKFR - Heart Failure - PMR4GP 2022Maulia Wisda Era ChresiaNessuna valutazione finora
- International Journal of Cardiology May 2021 Issue 2Documento343 pagineInternational Journal of Cardiology May 2021 Issue 2Fareesha KhanNessuna valutazione finora
- Analisis Lama Waktu Pelayanan Laboratorium Di Rumah Sakit Umum Daerah Pasaman BaratDocumento8 pagineAnalisis Lama Waktu Pelayanan Laboratorium Di Rumah Sakit Umum Daerah Pasaman Baratdina filanNessuna valutazione finora
- Thesis Synopsis - Naveen ReddyDocumento16 pagineThesis Synopsis - Naveen ReddyNaveen ReddyNessuna valutazione finora
- (S-W5-Sun-Gen.S) (By Dr. Emad) Gall Bladder 1Documento28 pagine(S-W5-Sun-Gen.S) (By Dr. Emad) Gall Bladder 1Haider Nadhem AL-rubaiNessuna valutazione finora
- ADR Notes KINJAL S. GAMITDocumento13 pagineADR Notes KINJAL S. GAMITKinjal GamitNessuna valutazione finora
- Chandy C. John - Advances in The Diagnosis and Treatment of Pediatric Infectious Diseases - 2013Documento212 pagineChandy C. John - Advances in The Diagnosis and Treatment of Pediatric Infectious Diseases - 2013Alla AlkateebNessuna valutazione finora
- Triage Assessment of Psychiatric Patient LectureDocumento31 pagineTriage Assessment of Psychiatric Patient Lectureهشام عفانه100% (1)
- Gambaran Penemuan Kasus Tuberkulosis Paru Oleh Petugas Puskesmas Di Kabupaten SukoharjoDocumento8 pagineGambaran Penemuan Kasus Tuberkulosis Paru Oleh Petugas Puskesmas Di Kabupaten SukoharjoBenti Eka WatiNessuna valutazione finora
- Periop PhinmaaugustDocumento221 paginePeriop PhinmaaugustEna RodasNessuna valutazione finora