Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
The Red Eye The Swollen Eye and Acute Vision Loss Handling Non Traumatic Eye Disorders in The ED
Caricato da
Bimantoro SaputroTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
The Red Eye The Swollen Eye and Acute Vision Loss Handling Non Traumatic Eye Disorders in The ED
Caricato da
Bimantoro SaputroCopyright:
Formati disponibili
EMERGENCY MEDICINE PRACTICE
A N E V I D E N C E - B A S E D A P P ROAC H T O E M E RG E N C Y M E D I C I N E
June 2002
The Red Eye, The Swollen Eye,
And Acute Vision Loss:
Handling Non-Traumatic
Eye Disorders In The ED
Volume 4, Number 6
Authors
Janet G. Alteveer, MD, FACEP
Associate Professor of Emergency Medicine, Robert
Wood Johnson Medical SchoolCamden, University of
Medicine and Dentistry of New Jersey, Camden, NJ.
1:15 a.m.: A 55-year-old woman arrives in the ED complaining of headache and
vomiting. She felt fine when she went to bed but woke with a horrible frontal headache
and retching. She has never had a headache like this before and has no significant past
medical history. Although a quick neurologic exam is normal, you think, Ill get a head
CT, and then I suppose Ill have to tap her. Before she leaves the department, the nurse
cheerily asks, Why is her eye so red?
1:18 a.m.: Cancel CT.
YE problems are common in every ED. While the exact number of
emergency visits for eye complaints remains unknown, in the year 2000,
nearly 4 million patients presented to U.S. EDs with a complaint referable to the
ear or eye.1 The American Academy of Ophthalmology (AAO) estimates that
one-third of all Americans have some ocular abnormality. Of these, one-quarter
need corrective refraction to achieve normal vision. In all, 3 million Americans
have impaired vision despite correction, and 890,000 are legally blind.2
This article addresses three basic complaints: the red eye, visual problems,
and periorbital swelling. It addresses both common and unusual causes of eye
disorders as well as the approach to specific populations (neonates, children,
and the immunocompromised).
Clinical Guidelines
In the past several years, the AAO has published Preferred Practice Patterns
on a variety of subjects. Each subcommittee of the AAO reviews the medical
literature of the previous five years on a particular subject (e.g., conjunctivitis,
blepharitis, acute angle-closure glaucoma, etc.). The Committee recommendations are rated A to C with respect to clinical importance, A being most
important; B, moderately important; and C, relevant but not critical. The
Editor-in-Chief
Stephen A. Colucciello, MD, FACEP,
Assistant Chair, Department of
Emergency Medicine, Carolinas
Medical Center, Charlotte, NC;
Associate Clinical Professor,
Department of Emergency
Medicine, University of North
Carolina at Chapel Hill, Chapel
Hill, NC.
Associate Editor
Andy Jagoda, MD, FACEP, Professor
of Emergency Medicine; Director,
International Studies Program,
Mount Sinai School of Medicine,
New York, NY.
Editorial Board
Judith C. Brillman, MD, Residency
Director, Associate Professor,
Department of Emergency
Medicine, The University of
New Mexico Health Sciences
Center School of Medicine,
Albuquerque, NM.
W. Richard Bukata, MD, Assistant
Clinical Professor, Emergency
Medicine, Los Angeles County/
USC Medical Center, Los Angeles,
CA; Medical Director, Emergency
Department, San Gabriel Valley
Medical Center, San Gabriel, CA.
Francis M. Fesmire, MD, FACEP,
Director, Chest PainStroke
Center, Erlanger Medical Center;
Assistant Professor of Medicine,
UT College of Medicine,
Chattanooga, TN.
Valerio Gai, MD, Professor and Chair,
Department of Emergency
Medicine, University of Turin, Italy.
Michael J. Gerardi, MD, FACEP,
Clinical Assistant Professor,
Medicine, University of Medicine
and Dentistry of New Jersey;
Director, Pediatric Emergency
Medicine, Childrens Medical
Center, Atlantic Health System;
Vice-Chairman, Department of
Emergency Medicine, Morristown
Memorial Hospital.
Michael A. Gibbs, MD, FACEP,
Residency Program Director;
Medical Director, MedCenter Air,
Department of Emergency
Medicine, Carolinas Medical
Center; Associate Professor of
Emergency Medicine, University
of North Carolina at Chapel Hill,
Chapel Hill, NC.
Gregory L. Henry, MD, FACEP,
CEO, Medical Practice Risk
Assessment, Inc., Ann Arbor,
MI; Clinical Professor, Department
of Emergency Medicine,
University of Michigan Medical
School, Ann Arbor, MI; President,
American Physicians Assurance
Society, Ltd., Bridgetown,
Barbados, West Indies; Past
President, ACEP.
Jerome R. Hoffman, MA, MD, FACEP,
Professor of Medicine/Emergency
Medicine, UCLA School of
Medicine; Attending Physician,
UCLA Emergency Medicine Center;
Co-Director, The Doctoring
Program, UCLA School of Medicine,
Kathryn M. McCans, MD, FAAP
Assistant Professor of Emergency Medicine and
Pediatrics, Robert Wood Johnson Medical School
Camden, University of Medicine and Dentistry of New
Jersey, Camden, NJ.
Peer Reviewers
Robin R. Hemphill, MD
Associate Residency Director, Department of
Emergency Medicine, Vanderbilt University,
Nashville, TN.
Capt. Kevin J. Knoop, MD, MS, FACEP
Program Director, Emergency Medicine Residency,
Naval Medical Center, Portsmouth, VA.
Alfred Sacchetti, MD, FACEP
Associate Director Emergency Medicine, Our Lady
of Lourdes Medical Center, Camden, NJ.
CME Objectives
Upon completing this article, you should be able to:
1. explain both common and rare causes of the red
eye, swollen eye, and acute vision loss in children
and adults;
2. determine which causes of non-traumatic eye
disorders require ophthalmologic consultation;
3. list eye disorders that can threaten vision; and
4. describe treatment strategies for common
eye disorders.
Date of original release: June 1, 2002.
Date of most recent review: May 7, 2002.
See Physician CME Information on back page.
Los Angeles, CA.
Francis P. Kohrs, MD, MSPH, Associate
Professor and Chief of the Division
of Family Medicine, Mount Sinai
School of Medicine, New York, NY.
John A. Marx, MD, Chair and Chief,
Department of Emergency
Medicine, Carolinas Medical
Center, Charlotte, NC; Clinical
Professor, Department of
Emergency Medicine, University
of North Carolina at Chapel Hill,
Chapel Hill, NC.
Michael S. Radeos, MD, MPH,
Attending Physician, Department
of Emergency Medicine,
Lincoln Medical and Mental
Health Center, Bronx, NY;
Assistant Professor in Emergency
Medicine, Weill College of
Medicine, Cornell University,
New York, NY.
Steven G. Rothrock, MD, FACEP, FAAP,
Associate Professor
of Emergency Medicine, University
of Florida; Orlando Regional
Medical Center; Medical Director of
Orange County Emergency
Medical Service, Orlando, FL.
Alfred Sacchetti, MD, FACEP,
Research Director, Our Lady of
Lourdes Medical Center, Camden,
NJ; Assistant Clinical Professor
of Emergency Medicine,
Thomas Jefferson University,
Philadelphia, PA.
Corey M. Slovis, MD, FACP, FACEP,
Professor of Emergency Medicine
and Chairman, Department of
Emergency Medicine, Vanderbilt
University Medical Center;
Medical Director, Metro Nashville
EMS, Nashville, TN.
Mark Smith, MD, Chairman,
Department of Emergency
Medicine, Washington Hospital
Center, Washington, DC.
Charles Stewart, MD, FACEP,
Colorado Springs, CO.
Thomas E. Terndrup, MD, Professor
and Chair, Department of
Emergency Medicine, University
of Alabama at Birmingham,
Birmingham, AL.
clinical evidence is also evaluated on a scale of I to III, with
Level I reflecting at least one well-designed randomized
clinical trial; Level II, non-randomized, case-controlled, or
multiple-time trials; and Level III, case reports, descriptive
studies, or expert opinion. These guidelines are discussed in
further detail in the subsequent sections of this article.
The eye is the jewel of the body.Henry David Thoreau
(1817-1862), U.S. essayist, poet, naturalist3
The Red Eye
While the red eye is a very frequent complaint in the ED,
there are no definite data on its overall prevalence.4 The
most common causes of the red eye include viral, bacterial,
and allergic conjunctivitis. While emergency physicians are
capable of treating the majority of patients who complain of
a red eye, it is important to differentiate benign and selflimited conditions from more serious processes. (See Table
1.) Such vision-threatening conditions include acute angleclosure glaucoma, scleritis, uveitis, and keratitis. (See Table 2
on page 3.)
Unilateral vs. bilateral
Character of the discharge: purulent vs. clear
Recent exposure to an infected individual
Trauma: mechanical (as in rubbing an irritated eye) or
foreign body, chemical, ultraviolet (UV) light (welders
flash, excessive sunlight, skiing without sunglasses,
tanning booth, etc.)
Contact lens wear: the type of lens, duration of wear,
hygiene, etc.
Associated symptoms that may be related to systemic
disease: genital discharge, dysuria, upper respiratory
infection (URI), skin and mucosal lesions, joint swelling
Allergy: any systemic complaints
Use of topical (especially ophthalmic) and/or
systemic medications
Previous episodes of conjunctivitis
Pregnancy status5
Family history of acute angle-closure glaucoma (this is
given a rating of A-II)6
The following are considered moderately important,
again with Level III evidence:
Use of personal care items (including eyeliners and
other cosmetics)
Previous ophthalmic surgery
Presence of immune dysfunction (e.g., HIV, chemotherapy, immunosuppression)
Prior allergic phenomena, such as atopy or StevensJohnson syndrome
History
The AAO categorizes the following elements of the history
as A, or most important; however, the evidence for these
is rated as Level III:
Symptoms and signs: itching, discharge, pain, photophobia, blurred vision,5 colored halos around lights,
headache, or brow pain6
Duration of symptoms
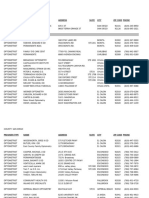
Table 1. Diagnostic Characteristics of Selected Disorders That Cause A Red Eye.
Characteristic
or Site
Angle-Closure
Glaucoma
Acute
Anterior Uveitis
Superficial
Keratitis
Focal or
diffuse
Diffuse; most
prominent
adjacent to
limbus
Diffuse; most
prominent
adjacent to
limbus
Diffuse
No
No
No
Minimal, if
present
Yes (if infectious
cause)
Not affected
Not affected
Constricted if
secondary uveitis
present;
otherwise
not affected
Moderately
dilated;
unreactive to
light
Constricted;
poor response
to light
Constricted if
secondary uveitis
present; otherwise
not affected
Ocular pain
Essentially none
Mild to
moderate
Moderate
to severe
Moderate to
severe (often
with headache
and vomiting)
Moderate
Moderate to
severe
Vision
Generally
not affected
Not affected
May be reduced
Severely
reduced
Mildly to
moderately
reduced
Moderately to
severely reduced
Cornea
Clear
Clear
Occasional
peripheral
opacity;
otherwise clear
Hazy
May be hazy (not Hazy
as prominently
as in angle-closure
glaucoma)
Conjunctivitis
Episcleritis
Scleritis
Hyperemia
Diffuse, more
prominent
toward fornices
Focal
Discharge
Yes
Pupil
Reproduced with permission: Leibowitz HM. The red eye. N Engl J Med 2000 Aug 3;343(5):345-351. Table 1. Copyright 2000 Massachusetts Medical
Society. All rights reserved.
Emergency Medicine Practice
www.empractice.net June 2002
The social history is considered relevant but not
critical, again with Level III evidence:
Alcohol and tobacco use
Occupation and hobbies (e.g., welding, skiing,
gardening)
Travel
Sexual activity1
If none of these methods are successful, grossly
estimate vision by asking the patient to count fingers at two
feet. If they cannot count fingers, try hand motion or, failing
that, light perception.
The External Eye Examination
Inspect the skin around the eyes as well as the lids and lid
margins for rashes, swelling, vesicles, discoloration, and
malposition of the lids. The character of the conjunctival
discharge should be noted: A purulent discharge almost
always means a bacterial infection (A-1).4,5 Also examine for
preauricular adenopathy (A-II),5 which often accompanies
viral conjunctivitis and chlamydial infections. One unusual
(and unsettling) finding is a lice infection of the lids.
Other relevant questions may include exposure to
metal hitting metal (hammering) or other foreign body
exposure (drilling, grinding, etc.).
The Physical Examination
Visual acuity and inspection of the external structures of the
eye and pupil must be part of any examination in patients
with eye-related complaints. Other aspects of the physical
examination will vary depending on the clinical presentation. Slit lamp, ophthalmoscopy, measurement of intraocular pressure (IOP), and fluorescein staining should be
considered if directed by the history or other facets of the
physical examination. The remainder of the HEENT
examination may also be revealing.
The Pupil
The size of the pupil and its response to light and accommodation may help narrow the differential diagnosis. In one
study of more than 300 consecutive patients presenting to
an eye clinic with a unilateral red eye, the presence of miosis
(small pupil) in the affected eye was a fairly reliable
indicator of iritis.8
Miosis is often secondary to spasm of the ciliary
muscle. While miosis is a nonspecific response to inflammation or injury, it generally indicates a disease process deep to
the cornea. Two simple maneuvers also suggest ciliary
muscle spasm. The first involves shining a bright light in the
unaffected eye. If the opposite eye has iritis, the consensual
response will elicit pain in the eye hidden from the light, a
phenomenon known as consensual photophobia.9 Pain in
response to accommodation may also indicate iritis. To
perform this test, have the patient look across the room and
then quickly look at your finger held a few inches in front
of their face. If they complain of pain with this test, iritis
is likely.10
A detailed discussion of the pupillary exam as well as
visual fields can be found in the section on acute vision loss.
Visual Acuity
Visual acuity is the vital sign of the eye. It is traditionally
quantified using the Snellen chart, with the patient standing
at a preset distance. The distance of the chart to the eye
should be recorded. If the patient is illiterate or pre-verbal,
use a picture chart or tumbling E chart (in which the
patient may indicate which way the E is facing with his or
her fingers). (See also the section on pediatric patients.) If
the patient is unable to stand, use a near chart consisting
of calibrated letters held at a preset distance from the eye.
It is important to test each eye separately to accurately
determine vision in the affected eye. If the patient is unable
to see either chart, walk the patient one half the distance to
the chart and attempt again. If the patient can read the chart,
the numerator of the visual acuity documented will be 10
instead of 20.
Another option is to ask the patient to look through a
pinhole. (Construct one simply by poking an 18-gauge
needle through a piece of thick paper.) The pinhole will
correct most refractive errors and thus compensate for
missing or forgotten glasses. An alternative to the pinhole is
to have the patient use a hand-held ophthalmoscope when
reading the chart. The patient can then dial up or down
with the lens until the image is clear. The correction can then
be recorded as, for example, 20/30 with a -8 lens.7
The Slit Lamp
The slit lamp provides magnification of structures anterior
to the iris, including the anterior chamber, cornea, and
conjunctiva. Subtle abnormalities or small foreign bodies
involving the cornea and palpebral conjunctiva are often
best visualized with the slit lamp. The device provides a
better assessment of corneal defects or infiltrates than
ophthalmoscopy or visual inspection.
Some physicians routinely have trouble using the slit
lamp. Slit-lamp-aphobia can easily be overcome using the
following interventions. These include maintaining the
patients forehead against the restraining strap, using a
narrow, bright light at a very oblique angle, and moving the
joystick of the slit lamp forward and backward to focus on
various points between the cornea and iris. The presence of
cells (sparkles) and flare (searchlight in the fog) suggests
inflammation or trauma to the eye.11 (See the subsequent
section on uveitis for specific findings.) While gross
hypopyon (a meniscus of white cells in the anterior chamber) and hyphema (red cells) can often be visualized with an
ophthalmoscope, smaller collections are seen more clearly
Table 2. Glossary Of Terms.
Blepharitis: inflammation of the eyelids
Conjunctivitis: inflammation of the conjunctiva
Keratitis: inflammation of the cornea
Episcleritis: inflammation of the subconjunctival
connective tissue and the blood vessels that course
between the sclera and conjunctiva
Scleritis: inflammation of the sclera
Anterior uveitis: inflammation of the iris and ciliary body
(also called iritis or iridocyclitis)
Posterior uveitis: inflammation of the choroid
June 2002 www.empractice.net
Emergency Medicine Practice
with the slit lamp.
Slit lamp examinations are probably not necessary
for all ophthalmic complaints. Limit them to patients in
whom iritis or small foreign bodies are suspected. In one
study, two separate, blinded ophthalmologists examined 98
successive patients presenting with a red eye to an emergency ophthalmology service; their findings were recorded
independently. The physician limited to the ophthalmoscope was asked to indicate if a slit lamp examination was
indicated (an effort to mimic the general practitioner
requesting an eye consult). There was a 71% agreement in
diagnosis between the slit lamp and ophthalmoscope group.
An incorrect diagnosis was made in four of the non-slitlamp patients (three had anterior uveitis); however, in each
case, the examining physician had clinical suspicion of a
potentially serious problem. Each of these patients had findings
consistent with iritisphotophobia or deep, aching pain made
worse on accommodation.12
the lids. Simply ask the patient to look down while you
place a small, cotton-tipped applicator at the midpoint of
the upper lidthen firmly grasp the eyelashes and pull
them gently over the applicator. The undersurface of the lid
containing the palpebral or tarsal conjunctiva can now be
examined for foreign bodies or other abnormalities. (A
paperclip bent at 90 can also be used to evert the lid,18
although some suggest that this may expose the patient to
fine metal particles that flake off the clip.)
Tonometry
Tonometry measures intraocular pressure. Normal IOP
ranges between 12 and 21 mmHg. Individuals with
pressures between 21 and 30 mmHg who have normal optic
discs are said to have ocular hypertension and are at risk of
open-angle glaucoma.19
There are many methods for measuring IOP; all involve
prior anesthesia of the cornea using topical drops. The
Goldmann-type applanation tonometer is considered a gold
standard. It is the tonometer preferred by the AAO (A-III);
however, it requires significant training in use and calibration.6 During the past 10 years, a small, highly portable
electronic device called the Tono-pen has appeared on the
market. It uses a strain gauge that converts the voltage
changes to a digital read-out. A disposable mini-condom
covers the tip to prevent cross-contamination. While it is
relatively easy to use, it remains quite expensive. The Tonopen is as accurate as the Goldmann tonometer in the usual
physiologic ranges (10-30 mmHg). However, it slightly
overestimates pressures in the low ranges and, more
importantly, underestimates pressures in the high ranges. It
is appropriate for general screening, but probably not in
glaucoma clinics, where fine-tuning of pressures at the high
end is needed.20,21
The Schiotz tonometer is still in use in many EDs and
outpatient clinics. It is a metallic tonometer that mechanically indents the cornea. The resultant deflection on the
scale must then be converted using a supplied chart to
arrive at the IOP reading. It is important to remember that
the lower the measurement on the Schiotz, the higher the
IOP. The Schiotz is somewhat cumbersome to use, can only
be used in cooperative patients in the supine position, and
must be cleaned thoroughly after each use. To use the
Schiotz to its best advantage, it is helpful to ask the patient
to look at a spot on the ceiling directly in front of their eye,
taking care not to apply pressure to the globe when the
eyelids are retracted.
Whichever tonometer is used, be sure to disinfect the
contact surface against viruses and bacteria properly if
disposable tips are not used. An effective solution is sodium
hypochlorite (bleach) at 500 ppm.22
While tonometry is the most objective means to determine
IOP, digital ballottement of the eye can provide important
information. Gentle palpation of the globe in the setting of
acute angle-closure glaucoma can confirm that the involved
eye is much harder than the unaffected side.4 (Do not
perform this maneuver in the setting of ocular trauma or
suspected corneal perforation, as this may herniate intraocular contents.)
Topical Anesthetics
Patients with acute eye irritation may require topical
anesthesia to cooperate with the examination. Topical
anesthetics such as proparacaine 0.5% (Opthane, Opthetic)
or tetracaine 0.5% are used to facilitate examination of the
eye and provide diagnostic information as well. These
agents facilitate lid eversion, tonometry, fluorescein staining,
and examination of the patient with severe eye pain. In
addition, topical anesthesia can help differentiate pain due
to simple corneal injury from pain due to iritis, glaucoma, or
other serious eye problems. In one study, eye pain relieved
by proparacaine was usually due to corneal injury (sensitivity, 80%; specificity, 86%).13
As to which agent to use, in one trial proparacaine
was less painful than tetracaine.14 Dilution of proparacaine
with a balanced salt solution (1:15 dilution) further decreases the burning sensation that many patients experience
with 0.5% proparacaine.15
Whichever anesthetic is used, it should be supplied
in unit doses in order to prevent the spread of infectious
agents. A 1987 study of an ophthalmology outpatient clinic
revealed some disturbing findings. The usual practice in
this clinic was to use one bottle of anesthetic drops for each
slit lamp for an entire day, after which the opened bottles
were discarded. Normally, the anesthetic is instilled prior
to the fluorescein, but for this study, it was instilled afterward. At the end of the day, every bottle of anesthetic
showed fluorescein contamination (i.e., the anesthetic bottle
was touched to the surface of the eye, thus facilitating
bacterial transmission).16
Topical anesthetics should never be prescribed for routine
or extended use, as they impair corneal healing. Persistent
corneal defects, corneal ulcers, and microbial infections
have all been reported with extended use of topical anesthetic drops.17
Why do you see the speck in your neighbors eye, but do not
notice the log in your own eye?Matthew 7:3
Eyelid Eversion
If the patient complains of a foreign body sensation, evert
Emergency Medicine Practice
www.empractice.net June 2002
Fluorescein Staining
spectrum topical antibiotic preparations. The decision of
which preparation to use is often based on cost, availability,
local resistance patterns, and local practice.24 For instance, in
the United Kingdom, the number-one medication prescribed by the National Health Service is chloramphenicol.
However, case reports of marrow hypoplasia and aplastic
anemia associated with chloramphenicol have made U.S.
physicians generally abandon its use.27 An old and inexpensive medication in the U.S., such as sulfacetamide (Bleph 10
or Sulf 10), which has good gram-positive activity, is an
acceptable first-line choice. While the fluoroquinolones are
generally effective, there is concern regarding cost and
emerging resistance of gram-positive organisms.27 In
general, adults prefer ophthalmic drops to ointments, which
can be messy and blur vision.
Most antibiotics are administered on a QID basis. A
French study found similar cure rates comparing a BID
quinolone, lomefloxacin (not available in the U.S.), with QID
norfloxacin, with no deleterious side effects.28 A smaller
American study compared BID ofloxacin 0.3% (Ocuflox)
with the usually prescribed QID regimen and found no
difference in resolution at either 3-5 days or 11 days.29
Patients are generally instructed to follow up in 3-4 days if
there is no resolution of symptoms.5 Neither topical steroids
nor combination steroid-antibiotic preparations are recommended for bacterial conjunctivitis.
The final step in the evaluation of the red eye, when
indicated, is fluorescein staining of the cornea. It can be
performed with or without topical anesthesia. The lower lid
is gently retracted, and the tip of a moistened fluorescein
strip is touched to the lower conjunctival sulcus. This
maneuver prevents accidental injury to the cornea by the
fluorescein strip. (Touching the strip to the cornea ensures a
corneal abrasion, providing every patient with a false
diagnosis). Alternatively, hold the strip above the eye and
apply a drop of sterile irrigant to it, allowing the florescent
drop to plop into the conjunctival sac. Shine a cobalt blue or
Woods light on the cornea in a darkened room. Fluorescein
is readily picked up by damaged superficial cells or exposed
deeper cells of the cornea. Absence of staining implies an
intact or undamaged cornea. The pattern of staining can be
helpful in pinpointing the diagnosis:
A superficial criss-cross of mostly vertical lines (ice-rink
sign) suggests a foreign body under the upper lid
(either still present or already dislodged)
A focal area of staining may indicate a corneal abrasion
A deep area of staining with raised or blurred margins
may indicate a corneal ulcer
Herpes virus infections (see Figure 1) produce a
characteristic pattern of dendrites, reminiscent of a
bunch of grapes, tree roots, or a jagged flash of lightning (if you have a vivid imagination)
Gonococcal Conjunctivitis
Funduscopy
Gonococcal conjunctivitis is particularly aggressive, with the
potential to spread quickly to deeper eye structures and
result in permanent visual impairment. The incubation
period is thought to be from a few hours to three days.
Rarely, the onset can be 1-2 weeks.30 The spread is probably
oculogenital, and patients should be questioned about
urethral or vaginal discharge or other symptoms of STDs.5
An important clue to the diagnosis is a discharge so
copious that it re-accumulates immediately, as soon as it is
wiped away. (Some have made the imaginative comparison
to a waterfall of pus.) The eye is angry, demonstrating
bloody scleral injection, and the lids are often swollen and
red. In one series, keratitis, anterior chamber inflammation,
periocular edema and tenderness, gaze restriction, and
preauricular lymphadenopathy were common.31 The initial
evaluation should look for evidence of corneal infiltrates or
ulcerations. A Grams stain showing gram-negative
diplococci is diagnostic, but a culture is generally obtained
to confirm the diagnosis.
Such patients need parenteral antibiotics, saline
Funduscopy rarely provides useful information in the red
eye, as most etiologies involve processes in the anterior
rather than posterior portion of the globe. In addition, the
fundus may be difficult to visualize because of photophobia
or defects in the cornea.
Common, Benign Causes Of A Red Eye
Bacterial Conjunctivitis
Emergency physicians recognize bacterial conjunctivitis as a
common affliction.23 The main pathogens in adults include
Staphylococcus species, Streptococcus pneumoniae, and
Haemophilus influenzaea microbiologic spectrum that
varies little worldwide.24 Patients report a rapid onset of
irritation as well as redness and a purulent discharge that
usually starts in one eye and then spreads to the other
within 48 hours. Patients with bacterial conjunctivitis often
give a history of morning crusting and difficulty opening
the eyelids.25 While patients complain of irritation, they are
spared deep orbital pain and suffer no visual loss. On examination, the eye is diffusely injected; the pupil, cornea, and
anterior chamber are normal; and the grossly purulent
discharge is unmistakable.
While bacterial conjunctivitis is considered a benign
and self-limited condition, several studies show that broadspectrum topical antibiotics shorten the duration of illness
by 2-3 days.23,26 A recent meta-analysis of three doubleblinded clinical trials proved comparable efficacy between
bacitracin plus polymixin, ciprofloxacin 0.3% (Ocuflox),
tobramycin 0.3% (Tobrex), and norfloxacin 0.3%
(Chibroxin).24 A number of other, less well-controlled trials
found similar clinical cure rates with many other broad-
June 2002 www.empractice.net
Figure 1. HSV dendrites.
Emergency Medicine Practice
lavages, and daily ophthalmologic evaluations. The current
recommendations are single-dose ceftriaxone (Rocephin)
250 mg IM, ocular saline washes, and optional topical
therapy.5,32 There are many regions of the world (Asia,
Africa, and parts of the Middle East and Europe) that have
high rates of quinolone resistance; thus, oral quinolones are
not recommended. Ensure daily follow-up with an ophthalmologist.4 The CDC recommends empiric treatment for
chlamydia infection, as well as screening for syphilis,
whenever the diagnosis of gonorrhea is made.
resolution occurs in the vast majority of cases; however,
occasional complications of superficial keratitis, membranous conjunctivitis, and conjunctival scarring occur.
In most cases of viral conjunctivitis, no specific
treatment is necessary. Topical steroids are used only when
severe keratitis is present (see the subsequent section on
keratitis). In patients with a conjunctival membrane
(membranous conjunctivitis), debridement of this casing
followed by topical steroids may hasten recovery.5 While
some authorities recommend topical antibiotics, ostensibly
to prevent secondary bacterial infection, there is little
evidence and no trials within the past 15 years to support
this practice. Some authors cite patient expectation to justify
prescribing topical antibiotics.4 (What? We always get
drops for pinkeye! The school nurse said you would give us
some.) Studies comparing topical ketorolac 0.5%,
trifluridine 1.0% (Viroptic), dexamethasone 0.5%, and
artificial tears (the placebo) found no statistical benefit in
any of the treatment arms.35,36
All cases are highly contagious for about seven days,
and families should be educated on proper hygiene
(separate towels, frequent hand-washing, avoiding touching
the nose or lips, and avoiding close contact). This needs to
be taken into account when advising healthcare or daycare
workers on when to return to work. Most adults who can
maintain careful hygienic measures can return to work
before the conjunctivitis has resolved.37 The emergency
physician should be acutely aware of potential patient-tophysician (and then to another patient) transmission. Use
disposable gloves during the examination and wash hands
vigorously after touching a patient with conjunctivitis.
Chlamydial Conjunctivitis
Although exceedingly rare in the U.S., trachoma (a type of
chlamydia ocular infection) is the number-one cause of
blindness throughout the world. Chlamydial conjunctivitis,
a less serious disease, is caused by different serovars than
trachoma. It appears to be on the rise, paralleling the
increase in genital chlamydial infections. Nearly 1% of
adults with genital chlamydia may develop ocular involvement.33 In adults, the infection is contracted through
oculogenital spread. The average incubation period is five
days, with a range of 2-19 days.34 Untreated chlamydial
conjunctivitis may persist for months.
Patients may appear to have a viral conjunctivitis, with
diffuse conjunctival injection, superficial punctate lesions of
the cornea, and preauricular lymphadenopathy. However,
the discharge is mucoid, not watery, as in the case with viral
infections. A distinctive finding in chlamydial conjunctivitis
is a pathognomonic enlargement of bulbar conjunctival
follicles.5 (Because these follicles develop between the
second and third week of infection, they may not be evident
at the time of the ED visit.34) The diagnosis can be made in
the laboratory with either a direct immunofluorescent
antibody test or by chlamydia culture. Treatment is systemic: either azithromycin 1 g (Zithromax) PO or doxycycline 100 mg BID for seven days.5 Patients should be
screened for syphilis, and sexual contacts should be treated
for chlamydia.
Allergic Conjunctivitis
Allergic conjunctivitis is often a seasonal phenomenon in
sensitive individuals. Vernal and atopic conjunctivitis are
chronic conditions that begin in childhood and wax and
wane for decades before recurrences finally cease. Some
patients develop ocular symptoms during a generalized
allergic flare, in response to a specific allergen such as cat
dander, or in response to certain ophthalmic preparations
(Neomycin being the classic). Up to 15% of soft contact lens
users may develop an allergic response to the lenses.38 Mast
cells, present in many eye structures, are involved in the
allergic response, with histamine being the culprit in the
actual symptom complex.
During the acute flare, the major complaint is itching,
accompanied by burning and tearing. The discharge is
mucoid or stringy. On physical exam, both eyes are usually
injected, and the bulbar conjunctiva is often strikingly
edematous (chemosis). Some patients may even have
bulging tissue protruding from their closed lids. In atopic
conjunctivitis, the eyelids may become thickened or scarred,
with loss of eyelashes. In atopic and vernal types, the tarsal
conjunctiva is often hypertrophied. In contact-lens-associated giant papillary conjunctivitis, large, square papillae
(often described as cobblestones) are present on the
palpebral conjunctivae, best seen by inverting the lower lid.
The treatment of allergic conjunctivitis depends on the
etiology. In mild cases, removing the allergen (such as the
Viral Conjunctivitis
Viral conjunctivitis is the leading cause of red eye, although
exact numbers remain obscure. There are many viruses
that produce conjunctivitis. Among the most important
are the adenoviruses, often associated with epidemic
keratoconjunctivitis. Transmission is most commonly
from hand to eye, but other vectors include contaminated
tonometers, improper hand-washing technique, and
contaminated swimming pools. Epidemics may occur in
densely populated habitats, such as military outposts or
school dormitories.
Viral conjunctivitis usually presents with diffuse
conjunctival redness, lid edema, and a copious, watery
discharge. Patients may find a puddle of clear ocular
discharge on their pillow each morning. A preauricular
lymph node, while characteristic (and also seen with
chlamydial infections), is not always present. Other
distinctive findings may include subconjunctival hemorrhage, corneal erosions, or punctate keratitis. The symptoms
may last a week, often spreading to the other eye.
There is no role for routine viral cultures.5 Spontaneous
Emergency Medicine Practice
www.empractice.net June 2002
warm the meibomian secretions, followed by brief, gentle
massage of the eyelids, then cleaning the lids with a
commercial preparation or baby shampoo diluted 1:10.
Erythromycin ophthalmic ointment is useful when staphylococcal blepharitis is suspected. Instruct the patient to
apply the ointment to the lid margins several times daily for
one or more weeks. For resistant and severe inflammation, a
one- to three-week course of topical steroids is often used.
Most patients with blepharitis need to be counseled about
the chronicity of the problem, the likelihood of recurrent
flare-ups, and the need for a regular regimen of lid hygiene.50 Patients with keratoconjunctivitis sicca are managed
initially with artificial tear supplements.
eyedrops), if possible, using warm compresses, and
avoiding eye-rubbing may be all that is needed. In catsensitive individuals, eye-rubbing in the presence of cat
dander causes a prolonged allergic response.39 Topical overthe-counter vasoactive drops that contain a combination
vasoconstrictor and antihistamine (such as Vasocon-A or
Naphcon-A) may provide temporary relief of itching,
swelling, and tearing.40 The topical nonsteroidal medications
ketorolac 0.5% and diclofenac 0.1%, one drop QID, have
both been shown to be effective in reducing symptoms at
seven days.41-43 Ketorolac is the only topical NSAID to have
an actual FDA indication for allergic conjunctivitis.44 Mast
cell stabilizers (sodium chromolyn [Crolom], lodoxamide
[Alomide], or nedocromil [Alacril]) have shown statistically
significant improvement in several trials.45-47 Patients need to
be aware that there is a lag time of two weeks before
improvement is noted.
A systematic review to evaluate the efficacy of these
preparations is currently under way but has not yet been
published.48 The ultimate anti-inflammatorythe steroid
preparationis generally reserved for ophthalmologists
treating severe cases. Steroid treatment is usually prolonged,
and the patient has to be monitored closely for complications such as glaucoma and cataract formation.5
Pinguecula And Pterygium
Pinguecula, a benign degeneration of the conjunctiva related
to UV light exposure and aging, appears as a fatty-looking
yellow spot, usually on the nasal aspect of the conjunctiva.
A pterygium develops over years in individuals who spend
a lot of time exposed to UV light (e.g., farmers and fishermen). It appears as a raised, yellowish, fleshy lesion, usually
on the nasal aspect of the bulbar conjunctiva. It usually
extends only to the peripheral cornea, seldom interfering
with vision.4 Occasionally these lesions become inflamed,
leading to complaints of eye irritation, foreign body
sensation, pain, or tearing. The erythema is usually confined
to the areas surrounding the lesions.
Topical indomethacin (not available in the U.S.) has
been shown to reduce the inflammatory symptoms of both
pinguecula and pterygium when used over a 14-day
period.52 It performed as well as topical dexamethasone in a
small prospective, randomized trial.53 Several nonsteroidal
ophthalmic preparations are available in the U.S.: ketorolac
0.5% (Acular), diclofenac 0.1% (Voltaren), flurbirofen 0.03%
(Ocufen), and suprofen 1% (Profenal). Most have an FDA
indication for ophthalmologic surgery and have been used
extensively and with good results in controlling postoperative inflammation.53 Such drugs may be useful in
treating an inflamed pinguecula or pterygium, but hard
data are slim.
Youre a parasite for sore eyes.actor Gregory Ratoff
Blepharitis
Blepharitis is an acute or chronic inflammation of the
eyelids, often accompanied by conjunctival irritation. It may
be caused by a variety of bacterial, viral, or parasitic
infections as well as allergic, systemic, or dermatological
diseases. Blepharitis is divided into three main categories:
staphylococcal or seborrheic (both of which involve the
anterior eyelid) and meibomian gland dysfunction (which
involves the posterior eyelid). These conditions may be
difficult to differentiate on initial examination.
Keratoconjunctivitis sicca, a condition of low tear
volume, is associated with up to 50% of staphylococcal
blepharitis cases. Patients with dry eyes often complain
of eye irritation, fluctuating vision, red eyes, and
sometimes photophobia, symptoms suggestive of an
unstable tear film.49 Keratoconjunctivitis sicca may be
diagnosed by the Shirmer test (a qualitative measurement
of tear production using filter paper placed in the lower
fornix) or observing the rate of dilution of fluorescein on
the surface of the cornea.50
Inspection of the eyelids in blepharitis may show
chronic scaling, erythema or edema of the lid margins,
abnormal direction of eyelashes, or peculiar apposition of
the lid margins (entropion or extropion). The staphylococcal
variety tends to have hard, crusty deposits at the lid
margins, whereas those of the seborrheic type are often oily
or greasy.51 The magnitude of the findings reflects the
severity and the chronicity of the disease. There are no
specific diagnostic tests for blepharitis. Cultures of the lid
margins may be done for recurrent, severe inflammation or
cases resistant to standard therapy.
Treatment of blepharitis involves a daily regimen of lid
hygiene: warm compresses to soften the encrustations and
June 2002 www.empractice.net
Corneal Abrasions
Corneal abrasions are defects of the normal corneal epithelium caused by trauma from small objects (often a fingernail, twig, hairbrush, or comb). They also occur after
removal of a foreign body. Corneal abrasions from contact
lenses represent a separate category with a unique set of
clinical problems. In a one-year survey of admissions to a
British emergency eye clinic, corneal abrasions accounted
for 10% of the visits.54
Corneal abrasions are quite painful, and most people
do not return to full functioning until the abrasion is healed.
Patients describe immediate, sharp pain followed rapidly by
tearing, photophobia, a decrease in visual acuity, and a
persistent foreign body sensation. The eye will appear
injected. Topical anesthetic drops will often significantly
improve the pain, reduce blepharospasm, and allow a full
examination. Fluorescein staining reveals the corneal defect.
The magnification provided by a slit lamp allows a detailed
Emergency Medicine Practice
favor bacterial replication. Follow-up within 24 hours
should be arranged, because suppuration of the abrasions
can occur rapidly. Contact lens use should not resume until
the abrasion is fully healed.59 The offending lenses should be
replaced or inspected carefully for evidence of damage.
quantification of the size as well as the depth of the lesion.
The natural history of most abrasions is full healing in 2-3
days. Except in the cases of abrasions associated with
contact lens use, infection occurs in fewer than 1% of cases.
Until the mid-1990s, accepted therapy involved
occlusive eye patches, antibiotic ointments (felt to be more
soothing than drops), oral analgesics, and optional
cycloplegics. The theory behind the occlusive patches was to
provide a stable corneal environment to promote rapid reepithelialization. Patches were also thought to reduce pain.
A meta-analysis by Flynn et al in 1998 that combined five
randomized clinical trials showed no statistical difference in
healing between patched and un-patched eyes, and no reduction in
pain in patients whose eyes were patched.55 These trials,
however, enrolled only patients with small- to moderatesized abrasions (< 10 mm2). Large abrasions seem to enjoy
improved healing if patched.56
Unlike eye patching, topical NSAID drops may
improve patient comfort. In one randomized, double-blind,
placebo-controlled trial of 100 patients with corneal
abrasions, topical ketorolac 0.5% (Acular) was shown to reduce
pain and photophobia significantly at the one-day mark. The
ketorolac group was also able to return to function one day
sooner, on average, than the placebo group. There was no
difference in rates of healing or complications.56 A smaller
study using diclofenac 0.3% (Voltaren) showed a small but
statistically significant improvement in pain scale at two
hours.57 The exact mechanism of action of these topical
NSAIDs has not yet been delineated. It is probably some
combination of reduction in pain sensation and antiinflammatory effect.56 For traumatic, non-contact lens
abrasions with significant pain, Kaiser et al recommend
ketorolac 0.3% QID for three days or until the patient is
comfortable, a broad-spectrum antibiotic ointment TID for
three days or until the abrasion is healed, an optional shortacting cycloplegic such as cyclopentolate, and no patch
(unless the abrasion is > 10 mm2).56 Many emergency
physicians prescribe narcotic pain medicines for patients
with corneal abrasions; these drugs are especially appreciated when the patient tries to go to sleep.
Corneal abrasions in contact lens users represent a
distinct problem. There are approximately 25 million contact
lens wearers in the U.S. They are all at increased risk of
developing infected abrasionsreferred to as ulcerative
keratitis. Overnight, extended-wear soft lenses carry a 10- to
15-fold risk of infection. The causative organism is most
often Pseudomonas species. The course can be fulminant,
leading to permanent vision loss from corneal scarring.
Do not patch corneal abrasions secondary to contact lens use.
In 1987, Clemons et al reported six cases of Pseudomonas
keratitis following pressure patching for contact-lensassociated corneal abrasions.58 The occlusive patch favors
bacterial replication by raising corneal temperature and
interfering in the normal protective effects of routine eye
blinking, tear exchange, and tear movement. The treatment
of contact-lens-associated abrasions should begin with an
antibiotic ointment that covers Pseudomonas (such as
gentamicin [Genoptic] or combination polymixin/bacitracin). Steroid combinations should be avoided, as they may
Emergency Medicine Practice
Superficial Keratitis
Superficial keratitis may be caused by UV light exposure
(Welders flash or snow blindness), use (or overuse) of
contact lenses, topical medications, dry eyes (keratoconjunctivitis sicca), blepharitis, as well as viral infections. Patients
present with eye pain, redness, tearing, and decreased
vision. In the case of UV keratitis, symptoms may not begin
until 8-12 hours after exposure, prompting a nighttime visit
to the ED. Both eyes are usually affected. Correlating the
history with the characteristic ocular findings provides
the diagnosis.
Fluorescein staining reveals multiple punctate lesions
of the cornea, some of which stain intensely, others of which
appear as tiny gray spots.4 Broad-spectrum topical antibiotics are prescribed to prevent infection, while cycloplegics
provide significant pain relief if there is associated iritis (a
full discussion of cycloplegics appears later). Oral pain
medications are often needed as adjunctive therapy. The
erosions of superficial keratitis generally resolve in 2-3 days.
Patients who complain of continued symptoms should be
referred to an ophthalmologist for follow-up.
Less Common (But More Serious) Causes
Of The Red Eye
The following conditions can threaten vision and should be
referred to an ophthalmologist. The majority of these
disorders present with eye pain and redness.
Corneal Ulcers
Approximately 30,000 cases of corneal ulcers or microbial
keratitis occur yearly in the U.S.60 The microbiology of
bacterial infections differs somewhat depending on the
geographic location, with staphylococci, streptococci, and
gram-negative organisms being the most common.
Pseudomonas species are the predominant organisms in
contact-lens-associated cases. Acanthamoeba, fungi, herpes
simplex virus (HSV), and herpes zoster (HZ) have also been
implicated. The normal cornea is quite resistant to infection,
due to the tight junctions between the top two layers of the
cornea. Some preceding injury or insult is usually necessary
for an infection to develop. The most common pre-existing
condition is prior corneal surgery, such as corneal transplant, radial keratotomy, or cataract surgery.61 Ocular
surface disease (e.g., keratoconjunctivitis sicca or blepharitis), systemic diseases with eye involvement (e.g., rheumatoid disease or sarcoidosis), trauma, cranial nerve VII palsy,
immunosuppression (including topical and systemic
steroids), and contact lens wear are also risk factors for
ulcerative keratitis.62
Most patients with bacterial corneal ulcers complain
of rapidly progressive eye pain, blurred vision (particularly
if the ulcer is in the central field of vision), and photophobia.
On occasion, a purulent discharge occurs. Parasitic, viral, or
fungal infections may present in a more indolent fashion.
www.empractice.net June 2002
Acute Anterior Uveitis
The presence of corneal abnormalities on physical examination differentiates ulcers from uncomplicated conjunctivitis. The
cornea will appear hazy to the naked eye. The raised
margins and crater of the ulcer can clearly be seen with the
slit lamp, and the ulcer will stain intensely with fluorescein.
The use of Grams stain, culture, and scrapings from
the ulcer margins remains controversial. A survey of
ophthalmologists in Southern California revealed that fewer
than half used culture prior to initiating antibiotic therapy.
The need for cultures is controversial because most ulcers
respond to empiric therapy63 and because bacterial sensitivity results do not seem to correlate with clinical response.61
The AAO recommends that cultures be done in the following settings: a large or deep infiltration, an ulcer that is
chronic or unresponsive to broad-spectrum antibiotics, or
when there is a suspicion of fungal, amoebic, or mycobacterial infection. Cultures are best done with both a specialized
platinum (Kimura) spatula and a dacron, calcium alginate,
or cotton swab that is then inoculated directly onto the
appropriate medium and transferred immediately to the
laboratory.62 The type of medium is dependent on the type
of infection suspected; consult with your microbiology lab.
Cultures of the patients contact lenses, lens case, or cleaning
solution may be useful when acanthamoeba infection
is suspected.62
Four to six percent of ulcers do not respond to initial
therapy. Because of the high potential for complications,
such as corneal scarring, decreased vision, endophthalmitis,
and ultimate enucleation, an ophthalmologist should be
involved early in the care of such patients. Two large trials
show that monotherapy with ofloxacin (Ocuflox) or
ciprofloxacin (Ciloxin) is as effective as combination
therapy.64,65 Some academic ophthalmologists are concerned
about emerging quinolone resistance to gram-positive
organisms and choose instead to use combinations of
fortified antibiotic solutions reconstituted from powdered
parenteral preparations and artificial tears.66 They often
have pharmacies willing and able to reconstitute these
solutions. The most common first-line choice is cefazolin
(Ancef) plus tobramycin or gentamicin. Specific directions
for reconstituting these preparations can be found in the
AAO Preferred Practice Pattern issue on bacterial keratitis.62
Loading doses of any of these medications are usually
begun on a 5- to 15-minute cycle followed by every hour
instillation for the first 24 hours. At this point, the eye is reexamined with a slit lamp. The regimen may be modified
depending on clinical response. If topical steroids were
being used, they should be discontinued, or at least reduced
to the minimum amount needed to control the underlying
condition. The initiation of topical steroids for corneal ulcers
is controversial and without conclusive scientific evidence.
Nevertheless, many ophthalmologists continue to use lowdose topical steroids for corneal ulcerations in the belief that
they will reduce inflammation.62
Many corneal ulcers may be managed on an outpatient
basis with daily re-examinations. Ensure that the patient is
able to comply with treatment. For instance, can an older or
arthritic patient actually administer the eye drops? Will the
patient actually return for next-day follow-up?
June 2002 www.empractice.net
Acute anterior uveitis, also called iritis or iridocyclitis, is an
inflammation of the anterior portions of the uvea. The
majority of cases are idiopathic; however, uveitis may
develop in association with viral infections, HSV, HZ, or
AIDS. Other implicated etiologies include Lyme disease,
syphilis, toxoplasmosis, brucellosis, intraocular foreign
bodies, and anterior segment ischemia.67
Acute iritis may also develop several days after blunt
trauma to the eye. Unless specifically questioned, patients
may not make the connection between the trauma and their
current eye pain (although a black eye is a powerful clue).
Patients complain of significant eye pain, tearing, and
photophobia. The eye is injected, with the most marked
hyperemia adjacent to the iris (the limbus); this is called limbal
injection or flush. The pupil may appear constricted or
irregular and may react poorly to light. Some patients
demonstrate a moderate-to-severe reduction in visual
acuity. As described in the section on the physical examination, testing for a consensual light reflex or accommodation
will cause significant pain in the affected eye. The hallmark
of anterior uveitis is the presence of inflammatory cells and
flare in the anterior chamber on slit lamp exam. The cells
(sparkle) are quantified in a 1x1 mm slit on a scale of 0-4,
such that +1 = 5-15 cells; +4 > 60 cells. The flare (smoke),
which represents protein in the anterior chamber, is also
quantified on a scale of 0-4, such that +1 = very slight,
+4 = intense. The flare may persist even after the cells are
gone.67 If the inflammation is severe, a layer of pus (hypopyon) will be evident on direct examination of the
anterior chamber.
Topical steroids, prescribed after consultation with an
ophthalmologist, are the cornerstones of therapy. Prednisolone (PredForte) is commonly prescribed, given every 1-2
hours initially, then slowly tapered over 3-4 weeks. A
response to steroids is usually noted by 3-4 weeks. Intermediate-acting cycloplegics, such as homatropine or scopolamine, are used to control the pain from ciliary spasm.
Sympathetic stimulants such as tropicamide (Mydriasil) are
inappropriate, as they have no affect on the ciliary constrictor muscle. Cyclopentolate (Cyclogyl) is not recommended
because it may aggravate the inflammation.67
Because of the significant potential for long-term
sequelae, such as glaucoma, pupillary abnormalities,
cataract formation, and macular dysfunction, an
ophthalmologist should be involved early in the care
of anterior uveitis.4
Why do you hasten to remove anything which hurts
your eye, while if something affects your soul you postpone
the cure until next year?Horace68
HSV Keratitis
As many as 500,000 cases of ocular herpes infections are
diagnosed in the U.S. each year.69 Primary HSV infections
are associated with ocular lesions in 2%-6% of cases,
whereas ocular lesions are present in 10%-30% of secondary
disease.70 Secondary infection represents reactivation of the
virus that has lain dormant, sometimes for decades, in the
trigeminal ganglion. Many factors have been implicated in
Emergency Medicine Practice
Herpes Zoster
reactivation: UV light, cold, wind, systemic illness, emotional stress, surgery, menstruation, minor local trauma, and
immunosuppression, either from disease or medication.
Recently, there have been case reports of HSV following
laser refractive surgery as well as laser glaucoma surgery.69
Primary ocular disease rarely results in vision loss; however,
each recurrence raises the risk of stromal immune response
and permanent morbidity. The cumulative risk of recurrence
is estimated at 30% per year.70
The most common presenting complaints are irritation,
tearing, photophobia, and blurred vision. Past medical
history should include questions regarding facial lesions,
such as cold sores or blisters, genital lesions, previous
episodes of corneal ulcers or iritis, recent topical or systemic
steroids, immunosuppressive diseases, or medications.69
Corneal sensation, which may be tested using thin wisps of
cotton from a sterile cotton-tipped applicator, is decreased in
80% of cases. When the herpes-infected eye is touched, the
corneal reflex may be depressed or the patient may notice
decreased sensation in the involved eye.
The best diagnostic test in the ED involves slit lamp
examination in combination with fluorescein staining. Using
the blue light on the slit lamp will illuminate the pathognomonic dendrites. Dendrites are single or multiple masses
that have linear branches that end in terminal bulbs.
However, depending on the time of presentation, these
dendrites may not be present. HSV begins as a punctate
keratitis, which then progresses to dendritic lesions that
then coalesce into geographic ulcerations. Iritis with a cell or
flare reaction on slit lamp exam occurs in 40% of cases.
Disease confined to the epithelium responds to topical
or oral antiviral agents in 90%-95% of cases. Forty percent of
cases resolve spontaneously without sequelae69 (but the ED
physician should still treat them). Three topical antivirals
(trifluridine [Viroptic], vidarabine [Vira A], and idoxuridine
[Stoxil]) and three oral preparations (acyclovir [Zovirax],
famcyclovir [Famvir], and valacyclovir [Valtrex]) are
available in the U.S. For disease limited to the epithelium,
any of the topical or oral preparations are used for 10-14
days. A topical antibiotic preparation is added when ulcers
are present.69 Acyclovir is the only oral agent to have been
studied in ocular clinical trials. The other agents are used
off-label based on genital infection trials.
Corticosteroids are sometimes used for HSV immune
keratitis and keratouveitis. Their beneficial effects include
inhibition of white cell infiltration, scar formation, and
neovascularization. However, they may promote the spread
of a superficial viral infection, increase the incidence of
bacterial or fungal infections, and result in steroid-induced
glaucoma or cataracts. They may also require a prolonged
taper to prevent inflammatory rebound. Consult an ophthalmologist before instituting steroids. When steroid drops are
used, a prophylactic antiviral preparation is added.69 A
series of clinical trials by the Herpetic Eye Disease Study
(HEDS) multicenter group did not show an improvement in
resolution with the addition of oral acyclovir to a topical
regimen. However, a subsequent HEDS trial showed that
prophylactic oral acyclovir reduces the rate of recurrent
HSV eye infections.71
Emergency Medicine Practice
Like HSV, HZ is a disease of recrudescence, the virus
emerging in specific nerve root distributions years after the
original infection. HZ of the ophthalmic division of the
trigeminal nerve (cranial nerve V) represents 10% of total
HZ infections. In the vast majority of cases, the characteristic
vesicular skin lesions precede ocular involvement.
A vesicular lesion on the tip of the nose (Hutchinsons
sign) is thought to be associated with a higher prevalence of
eye infection.72 There are case reports of ocular involvement
occurring prior to skin involvement and ocular lesions
without skin involvement.70 Although HZ may affect many
different areas of the eye, one-half of untreated ophthalmic
HZ involves the cornea. The corneal manifestations vary
from punctate keratitis to ulcers to pseudodendrites to
deeper stromal keratitis. The dendrites of HZ may be
difficult to differentiate from those of HSV. About 40%-60%
of immunocompetent patients develop an associated iritis.
These patients are at risk for ocular hypertension. The
characteristic skin lesions accompanied by corneal anesthesia are usually enough to make the diagnosis. A Tzanck
smear of vesicular lesions or epithelial scrapings may show
multinucleated giant cells but will not differentiate HZ from
HSV. Corneal cultures, while diagnostic, take 1-2 weeks.
PCR of tear film or corneal scrapings shows promise as a
rapid test in hard-to-diagnose cases.70
The skin lesions may be treated with a seven- to
10-day course of acyclovir (Zovirax, 800 mg 5 times a day),
famcyclovir (Famvir, 500 mg TID), or valacyclovir (Valtrex,
1 g TID). All of these preparations promote healing and
reduce pain if given within 72 hours of onsetbest if
within 48 hours. However, the incidence of post-herpetic
neuralgia, a particular problem in the elderly, is unaffected.73
Topical antivirals have not been shown to be effective in HZ.
Topical steroids should be reserved for cases of active
stromal keratitis and anterior uveitis, under the direction
of an ophthalmologist.70
Fungal Conjunctivitis
Fungal conjunctivitis is initially clinically indistinguishable
from bacterial infection. The diagnosis may be suggested by
a history of trauma from vegetation or work on a farm or
vegetable garden, but sometimes the initial trauma is so
mild as to have been forgotten. Contact lens users and
immunocompromised patients are also at risk. Corneal
scrapings and culture provide the diagnosis. Treatment,
requiring topical antifungals and sometimes subconjunctival injection, is best left to the ophthalmologist.74
Acute Angle-Closure Glaucoma
One in 50 Americans over 35 is at risk for glaucoma;
primary angle-closure glaucoma (PACG) represents about
10% of total cases. Risk factors for PACG include older age,
female sex, a history of hyperopia (farsightedness), a family
history of acute angle-closure glaucoma, Eskimo or Asian
extraction, and a prior history of anterior uveitis.6 The
pathophysiology of PACG involves obstruction of the
trabecular meshwork. When the entire circumference of the
anterior chamber angle is occluded, IOP increases and
10
www.empractice.net June 2002
pain without discharge.4 The eye is usually tender to palpation. In
some cases the sclera may be so thin that the bluish uvea is
seen shining through. Therapy with a nonsteroidal antiinflammatory agent can be started; however, steroid
preparations are usually needed to control the disease. If the
disease is non-necrotizing, topical steroids are often
prescribed initially. There is a high failure rate (47% in a
small descriptive Canadian study),80 so that approximately
60% of patients end up on oral steroids or other immunosuppressive drugs.81 Referral to an ophthalmologist should
be done promptly, because of the often chronic nature of the
disease, the potential to permanently impair vision, and to
rule out necrotizing scleritis.4,79
corneal edema occurs. Attacks may be precipitated in a
susceptible individual by anything that causes excessive
pupillary dilatation: low light, stress, fatigue, or medication
with sympathetic or parasympatholitic actions.75
Acute PACG classically presents as severe unilateral
eye or brow pain, decreased vision, and colored halos
around lights (due to corneal edema). Vagal stimulation
from severe pain may precipitate significant nausea and
vomiting. There are case reports of elderly patients presenting only with nausea and vomiting and generalized
headache or with abdominal pain, which results in an
extensive GI work-up or even laparotomy.76 While PACG
can affect both eyes, an acute attack usually presents
unilaterally with a red eye, hazy cornea, and a dilated,
minimally reactive pupil. IOPs are often in the 50-70 mmHg
range. The diagnosis is usually obvious by the combination
of history and tonometry. Using a slit lamp and goniometer,
an ophthalmologist can demonstrate that the peripheral iris
blocks the trabecular meshwork. If a hazy cornea impedes a
clear view of the angle, the other eye should be examined. If
a skilled observer or slit lamp is unavailable, an oblique
flashlight test may be used. In this test, a penlight or
flashlight is held off to the side and parallel to the iris with
the beam shining across the anterior chamber. If the whole
iris is illuminated, the angle is open. If a shadow appears on
the nasal aspect of the iris, the angle is narrow or closed.
This test has a sensitivity of 80% and specificity of 69%.77
If untreated, acute angle-closure glaucoma will result in
blindness within a few days. The initial treatment targets
lowering IOP in preparation for definitive surgery.6 Call an
ophthalmologist as soon as the diagnosis is made or
strongly suspected. Accepted components of acute medical
therapy include topical beta-blockers, a topical alphaadrenergic agent (such as apraclonidine), oral or intravenous acetazolamide, topical steroids, and low-dose pilocarpine.76 Intravenous osmotic agents, such as mannitol, are
effective in lowering IOP, but they need to be used with
great caution in the setting of congestive heart failure or
renal insufficiency. The miotic effect of pilocarpine is
blocked at IOPs over 60 mmHg; however, the action on the
ciliary muscle and the anterior movement of the lens
continue, so that IOP may be paradoxically increased with
aggressive use of pilocarpine. Many ophthalmologists have
their own established routine, and even the AAO does not
endorse one particular medical algorithm.6 (See Table 3.)
Episcleritis
Episcleritis is an inflammation of the blood vessels that
course between the conjunctiva and sclera. It is almost
always a benign condition that resolves spontaneously in
1-2 weeks, never to return again. It may recur in about 20%
of cases and can occasionally evolve into scleritis.79,82
Episcleritis usually presents as localized conjunctival
erythema associated with mild ocular pain. The blood
vessels are engorged in the affected region, and a nodule
may be present as well. Vision, cornea, and pupil are all
normal. Often, no therapy is required, but episcleritis often
responds to oral4 or topical82 anti-inflammatory medications.
Corneal Perforation
The most common cause of corneal perforation is infectious
breakdown of the corneal stroma. Perforations may also
occur as a result of blunt or penetrating trauma to the eye,
inflammatory conditions, environmental exposure (as in
cranial nerve VII nerve palsies), and degenerative diseases.
Presenting symptoms include pain, decreased visual acuity,
and increased tearing. There are three clinical findings
classic for perforation: a flat or shallow anterior chamber,
uveal prolapse, and a positive Seidel test. The Seidel test is
done as follows: After topical anesthesia, the area suspicious
for perforation is painted with a sterile fluorescein strip
dipped in some sterile saline. Using a slit lamp with a cobalt
Table 3. Treatment Of Acute Angle-Closure Glaucoma.
A beta-blocker such as timolol 0.5% (Timoptic), 1-2 drops
every 10-15 minutes times three, then one drop BID.
A parasympathomimetic such as pilocarpine 0.2%, one drop
every 30 minutes until the pupil constricts, and then q6h.
Prednisolone 1% (Pred-Forte), one drop every 30-60 minutes
to reduce inflammation.
Apraclonidine 0.5%, two drops, once; an alpha-2-agonist that
reduces aqueous humor production and acts additively with
the beta-blocker.
Acetazolamide (Diamox) 500 mg IV q12h or PO q6h. Because
of the possibility of metabolic and respiratory acidosis, this
medication should probably be avoided in patients with
serious respiratory disease.
Mannitol 20% 1-2 g/kg IV over 30-60 minutes. Mannitol
is a hyperosmotic agent that should be used with caution
(if at all) in patients with congestive heart or renal failure.
It may cause mental status changes, worsening headache,
and dehydration.75,78
Scleritis
Scleritis, or inflammation of the anterior or posterior sclera,
is an idiopathic disease that may represent the first sign of a
connective tissue or systemic disease. There are three types
of scleritis: diffuse, nodular, and necrotizing. The latter
carries a severe prognosis not only for the eye, but also for
the underlying disease. Scleritis has been associated with
rheumatoid arthritis (the most common), relapsing
polychondritis, systemic lupus erythematosus, Wegener
granulomatosis, Cogan syndrome, polyarteritis nodosa,
Takayasu disease, sarcoidosis, porphyria, syphilis, tuberculosis, brucellosis, Lyme disease, and HZ.79
Scleritis presents with a red eye, decreased vision, and eye
June 2002 www.empractice.net
11
Emergency Medicine Practice
Pediatric Considerations
blue light, the painted area is observed for clearing or
dilution of the fluorescein (sometimes an active swirling of
the dye is visible, representing the leaking aqueous).
Clearing or dilution represents a positive Seidel test and
confirms the perforation. Treatment is surgical. In patients
who are unable to undergo surgery, tissue adhesives are
sometimes used to seal the perforation.83 All perforations
should be rapidly referred to an ophthalmologist.
The history for children presenting with a red eye requires
some additional elements:
The age of the child
The presence or absence of fever
Ill contacts
Pre- or postnatal STD infections in the mother
The physical examination can be challenging and often
needs to be adapted to the age of the child. For a pre-reader,
the eye chart should have pictures or directional Es. The
extraocular muscle (EOM) examination can be accomplished using brightly colored objects to encourage the
infant or child to track the object. The retinal exam may
require that an assistant (or parent) distract the child over
the shoulder of the examining physician. Be sure to examine
the ears in young children with purulent eye discharge; they may
be suffering from the conjunctivitis-otitis syndrome and could
require oral, rather than topical, therapy.
Endophthalmitis
Endophthalmitis is the most dreaded ocular infection. As
the word implies, it is a deep infection of the eye and carries
a poor prognosis. Patients who have had recent ocular
surgery are at risk for developing endophthalmitis.106 It
occurs in 0.1%-0.77% of cases post penetrating keratoplasty
(e.g., cornea, cataract, lens surgeries). At other times, it is a
complication of severe bacterial keratitis or ulceration.
Signs and symptoms include pain beyond that
expected in the immediate post-operative period, marked
inflammation, hypopyon, and diminished red reflex.83
Intravenous as well as subconjunctival or intraorbital
antibiotics are used in an attempt to save the eye.83
Bacterial Conjunctivitis
Bacterial conjunctivitis presents as it does in adults with
Ten Pitfalls To Avoid
1. An eye patch never hurt anyone.
Au contraire! The patient with a corneal ulcer who gets an
eye patch is at risk for perforation. Do not patch corneal
abrasions secondary to contact lens use.
6. We dont do fluorescein exams in our ED.
Start. Fluorescein exams are essential in diagnosing
keratitis and corneal abrasions. They are also helpful in
detecting corneal ulcers and corneal perforations.
2. He just had some eye pain. Thats not an indication for
visual acuities.
Having an eye complaint (and some say having an eye) is
an indication for visual acuities. They are the vital sign of
the eye.
7. He was complaining of eye pain. I told him to take a few
days off his job as a machinist and it would get better.
Intraocular foreign bodies rarely get better without surgery.
A history of metal-on-metal exposure is key. Look for an
irregular pupil. A Seidel test (see text) may be positive for
leakage of aqueous humor.
3. I know he had a lot of pus leaking from the eye, but I
thought he would do fine with some Sulamyd.
This gentleman had gonococcal ophthalmia and was
admitted the next day. Clues to this diagnosis include
copious pus; an angry, often-hemorrhagic sclera;
preauricular adenopathy; and anterior chamber
inflammation. Grams stain of the discharge will reveal the
gram-negative diplococci within the leukocytes. Such
patients require admission and parenteral antibiotics.
8. She was just another elderly woman with conjunctivitis
who came to the ED in the middle of the night.
By the time the ophthalmologist saw her three days later,
her IOP was over 80. Conjunctivitis usually does not present
with severe eye pain, hazy cornea, and unreactive pupil.
Check IOPs in suspicious cases; at the very least, compare
the tension in each eye by fingertip assessment.
9. I looked in his eye and didnt see a foreign body. All he
had were a lot of vertical scratches to his cornea.
And a foreign body under the lid. Evert the lids when a
patient complains of a foreign body sensationespecially
when they demonstrate an ice rink sign.
4. Since the H. flu vaccine, Ive been sending all kids with
periorbital cellulitis home on oral antibiotics.
This child did not do well, even after decompressive
surgery to the orbit. While it is true that the fierceness of
this disease has relented in the past decade, the decision to
treat as an outpatient must be made on an individual basis.
Children who appear toxic, those with proptosis or
impairment of extraocular motions, and patients with
decreased vision need admission and parenteral antibiotics.
10. I thought she was malingering. She said she was almost
blind in her right eye, but she blinked when I pretended to
poke her in the eye. Besides, her pupil reacted to light.
She had optic neuritis, not hysteria. Patients with ON may
still have a light reflex; the swinging flashlight test would
have been abnormal (if it had been done). Blind patients
still blink when a threat is made to their eye secondary to
the corneal reflex in response to a rush of air. (Plus, there
was nothing wrong with this ladys other eye.)
5. It looked like he had fire ant bites to his eyelids. Heck,
they even bit him on the tip of his nose.
Hel-looofire ant bites!? Patients with herpes zoster need
acyclovir, not Benadryl.
Emergency Medicine Practice
12
www.empractice.net June 2002
injected conjunctivae and a purulent discharge. In
preschoolers, it is the major cause of a red eye.84 The predominant organisms are nontypeable H. influenzae and S.
pneumoniae, with Moraxella catarrhalis, Neisseria gonorrhoeae,
and Neisseria meningitides occurring less frequently. N.
gonorrhoeae may occur outside the neonatal population in a
sexually abused child.85
The syndrome of conjunctivitis/otitis begins as a lowgrade fever and mild URI, but then progresses to a painful
red eye with purulent discharge. Otitis media, either
symptomatic or asymptomatic, may be present initially or
develop later. It is usually due to nontypeable H. influenzae,
less commonly to S. pneumoniae.86 Children who are less
than 3 years old or who attend daycare are more likely to
develop this syndrome.84
Several prospective studies have demonstrated the
efficacy of topical antimicrobials in hastening a clinical and
bacteriologic cure.84 Trimethoprim-polymyxin B eradicated
H. influenzae better than gentamicin sulfate or sodium
sulfacetamide.87 One study demonstrated the efficacy and
safety of topically applied ciprofloxacin ophthalmic solution
when it was compared to tobramycin ophthalmic drops in
257 children with bacterial conjunctivitis.88
There is some evidence to suggest the utility of
systemic antibiotics effective against H. influenzae to treat
bacterial conjunctivitis in children less than 6 years of age
(whether or not they have an associated otitis media).
Topical therapy does not eradicate nasopharyngeal carriage
of H. influenzae or N. meningitides, nor does it prevent or treat
an associated otitis media. Topical therapy may also be
difficult for parents to apply successfully as directed. In the
young child, the use of an oral agent effective against H.
influenzae might be considered even in the absence of a
documented otitis media. A three- to five-day treatment
course of an agent such as amoxicillin/clavulanate results in
a clinical and bacteriologic cure of the conjunctivitis and
may be effective prophylaxis for the otitis. However, there is
currently only one small, randomized study to support this
approach.89 There is more supporting evidence for a 10-day
course of oral antibiotics for bacterial conjunctivitis.90,91 Systemic
antibiotics successfully treat the conjunctivitis and prevent
(or cure) the associated otitis media.
Viral Conjunctivitis
Viral conjunctivitis is the most common cause of conjunctivitis in school-aged children.85 Viral conjunctivitis ranks
second after bacteria as the cause of acute conjunctivitis in
preschoolers. Adenovirus predominates in the fall. Viral
conjunctivitis is more commonly associated with pharyngitis than bacterial conjunctivitis.85 Conjunctivitis caused by
adenovirus may be hemorrhagic, and some children can
demonstrate significant periorbital swelling.84 Presentation
and treatment (or lack thereof) are similar to adult viral
conjunctivitis. Unlike adults, who can be expected to follow
recommendations on hygiene and minimizing viral
transmission, children should probably be kept home from
school or daycare for approximately one week.34
You cant depend on your eyes when your imagination
is out of focus.Mark Twain (1835-1910)
Neonatal Conjunctivitis
Neonatal conjunctivitis is caused by N. gonorrhoeae, Chlamydia trachomatis, and, less commonly, HSV. Infection is
acquired during passage through an infected birth canal.
While neonatal ophthalmic prophylaxis is universal in the
United States, it is not 100% effective. The medications used
are 1% silver nitrate solution, 0.5% erythromycin ophthalmic ointment, or 1% tetracycline ophthalmic ointment.
Only silver nitrate is effective against penicillinase-producing gonococcus.
Ophthalmia neonatorum, or gonococcal conjunctivitis,
presents in the first week after birth, with fever and a
profuse and purulent discharge that rapidly re-accumulates.
Continued on page 17
Cost-Effective Strategies For Patients With Eye Disorders
gonococcal ophthalmia may benefit from culture and/or
Grams stain.
1. Do not patch corneal abrasions.
Multiple studies show that patches have no beneficial effect
on patients with small-to-moderate corneal abrasions. They
provide neither comfort nor healing. Never patch a lesion
caused by a contact lens, as pseudomonal overgrowth and
subsequent perforation may occur.
Caveat: The jury is still out regarding large corneal
abrasions. There are no data to support or refute their
use in this situation.
3. Consider the use of oral antibiotics for purulent
conjunctivitis in preschool children.
Young children with obvious bacterial conjunctivitis are liable to
have (or develop) concurrent otitis media. Oral antibiotics may
obviate a repeat visit for a complaint of ear pain.
4. Use older, cheaper topical antibiotics rather than the
latest, more expensive drops.
Most studies show that older topical antibiotics such as
tobramycin or sodium sulfacetamide are as effective as the
more expensive quinolones for simple bacterial
conjunctivitis. All topical antibiotics are equally ineffective
for viral conjunctivitis.
Caveat: Quinolones are useful as monotherapy for
corneal ulcers.
2. Do not obtain cultures on patients with conjunctivitis.
Most cases of conjunctivitis are viral, and cultures have no
impact on management (except to increase costs). Even
bacterial conjunctivitis responds quickly to topical antibiotics
without the need to tailor therapy to an organism obtained
by culture.
Caveat: Patients with corneal ulcers, those with refractory
infections, and patients suspected of fungal lesions or
June 2002 www.empractice.net
13
Emergency Medicine Practice
Clinical Pathway: Management Of The Red Eye
Obtain visual acuities (Class I)
Perform eye examination (Class I)
Evaluate for foreign body (lid eversion as indicated)
(Class I)
Fluorescein exam (Class I)
Significant pain?
Unreactive pupil?
Steamy cornea?
Yes
Measure intraocular pressure (Class I)
Treat for acute angle-closure glaucoma if present (see
Table 3) (Class I)
No
Photophobia?
Pain on accommodation?
Pain with consensual light response?
Yes
Evaluate for iritis (Class I)
Use slit lamp to look for cell or flare reaction in anterior
chamber. If positive:
Consult with ophthalmologist (Class I)
Pred-Forte if approved by consultant (Class I)
Homatropine drops (Class II)
No
Photophobia?
Pain?
Corneal ulcer?
Yes
Consult with ophthalmologist (Class I)
Determine need for corneal scraping (Class II)
Aggressive antibiotic therapy (see text) (Class I)
No
Go to top of next page
The evidence for recommendations is graded using the following scale. For complete definitions, see back page. Class I: Definitely recommended.
Definitive, excellent evidence provides support. Class II: Acceptable and useful. Good evidence provides support. Class III: May be acceptable,
possibly useful. Fair-to-good evidence provides support. Indeterminate: Continuing area of research.
This clinical pathway is intended to supplement, rather than substitute for, professional judgment and may be changed depending upon a
patients individual needs. Failure to comply with this pathway does not represent a breach of the standard of care.
Copyright 2002 EB Practice, LLC. 1-800-249-5770. No part of this publication may be reproduced in any format
without written consent of EB Practice, LLC.
Emergency Medicine Practice
14
www.empractice.net June 2002
Clinical Pathway: Management Of The Red Eye
Photophobia?
Decreased corneal sensation?
Dendrites on fluorescein staining?
Yes
(continued)
Consult with ophthalmologist (Class I)
Oral acyclovir or topical antivirals (Class I)
No
Photophobia?
Exposure to UV light?
Fluorescein exam demonstrating keratitis?
Yes
Topical mydriatic (cyclopentolate or homatropine)
(Class II)
PO narcotics (Class II)
Counseling regarding proper eye protection (sunglasses, welders mask) (Class I)
No
Exuberant, purulent discharge?
Angry or hemorrhagic conjunctivitis?
Preauricular adenopathy?
Keratitis?
Yes
Evaluate and treat for gonococcal conjunctivitis
(Class I)
Consider Grams stain and culture of discharge
(Class II)
No
Purulent discharge?
Normal vision?
No keratitis?
No iritis?
Yes
Age greater than 6: topical antibiotic drops (Class I)
Age less than 6: consider oral antibiotics (Class II)
No treatment necessary (Class I)
Give precautions regarding transmission of virus
(Class I)
No
Clear discharge?
Preauricular adenopathy?
Normal vision?
No keratitis?
No iritis?
Yes
The evidence for recommendations is graded using the following scale. For complete definitions, see back page. Class I: Definitely recommended.
Definitive, excellent evidence provides support. Class II: Acceptable and useful. Good evidence provides support. Class III: May be acceptable,
possibly useful. Fair-to-good evidence provides support. Indeterminate: Continuing area of research.
This clinical pathway is intended to supplement, rather than substitute for, professional judgment and may be changed depending upon a
patients individual needs. Failure to comply with this pathway does not represent a breach of the standard of care.
Copyright 2002 EB Practice, LLC. 1-800-249-5770. No part of this publication may be reproduced in any format
without written consent of EB Practice, LLC.
June 2002 www.empractice.net
15
Emergency Medicine Practice
Clinical Pathway: Diagnosing The Swollen Eye In Adults
Onset
Acute
Probable cause: infectious
Normal
host
Probable cause: bacterial
Immunocompromised
host
Gradual
Probable diagnoses:
Tumor
Thyroid-related ophthalmopathy
Idiopathic orbital inflammatory
syndrome
Probable cause: fungal
Extraocular eye muscle movement?
Normal
Probable diagnosis: periorbital cellulitis
Painful or abnormal
Probable diagnosis: orbital cellulitis
Clinical Pathway: Diagnosing Acute Vision Loss In Adults
Age of patient
Probable diagnosis: optic neuritis
Any age
< 50
Probable cause: vascular
Possible causes:
Retinal detachment
Infection
Tumor
> 60
Systemic symptoms?
No
Retinal exam
Probable diagnosis: central retinal
artery occlusion
Probable diagnosis: temporal
arteritis
Pale
Yes
Congested
Probable diagnosis: central retinal
vein occlusion
The evidence for recommendations is graded using the following scale. For complete definitions, see back page. Class I: Definitely recommended.
Definitive, excellent evidence provides support. Class II: Acceptable and useful. Good evidence provides support. Class III: May be acceptable,
possibly useful. Fair-to-good evidence provides support. Indeterminate: Continuing area of research.
This clinical pathway is intended to supplement, rather than substitute for, professional judgment and may be changed depending upon a
patients individual needs. Failure to comply with this pathway does not represent a breach of the standard of care.
Copyright 2002 EB Practice, LLC. 1-800-249-5770. No part of this publication may be reproduced in any format
without written consent of EB Practice, LLC.
Emergency Medicine Practice
16
www.empractice.net June 2002
Continued from page 13
Conclusion
There is also lid edema and erythema. Corneal ulceration
and perforation can occur.
Neonatal HSV infection occurs in up to 1/3000 live
births. A mother with primary infection poses the greatest
risk to her infant. HSV of the eye is part of the skin, eye,
mouth disease; however, skin and mouth lesions may be
absent at presentation. The conjunctivae are erythematous
and with characteristic dendrites on fluorescein staining of
the cornea.92
The incubation period for chlamydial conjunctivitis is
longer, and so infants may present up to several weeks after
birth. The conjunctiva is beefy red, with a watery or
mucopurulent discharge. The infant may be afebrile.
Among infants born to infected mothers, 12%-25% will
develop chlamydial conjunctivitis.
It is important to differentiate ophthalmia neonatorum
and HSV infection from chlamydia. The first two require a
full sepsis evaluation, including complete blood count,
chemistries, blood and eye cultures, lumbar puncture (LP),
admission, and IV antibiotics. Emergent ophthalmic
evaluation is mandatory because of the potential for
perforation with gonococcus and vision loss with HSV.92
Chlamydia, on the other hand, is largely an outpatient
disease. Oral antibiotics are given to these patients because
many of these infants will infect their respiratory tracts
through infected drainage via the nasolacrimal ducts. There
are no randomized clinical trials dealing with these diseases;
however, clinical experience and the potential severity of the
complications make aggressive treatment the current
standard of care. (See Table 4.)
Bacterial, viral, and allergic conjunctivitis are usually benign
causes of the red eye that present with a variable discharge,
redness, and, in some cases, itching or mild irritation. The
presence of significant pain with or without impairment of
visual acuity should alert the emergency physician to the
presence of a more serious condition. The character of the
pupil and the cornea and the presence or absence of any
lesions on fluorescein staining will further help to delineate
the etiology. Corneal ulcer, uveitis, and HSV keratitis,
among other conditions, need to be referred to an ophthalmologist for definitive care. (See Table 5 on page 18.)
In the pediatric population, ophthalmia neonatorum
and HSV infections need a full septic workup with admission for IV antibiotics or acyclovir. With the exception of
antibiotic drops for bacterial conjunctivitis (and possibly
systemic antibiotics for young children with this disease),
there are few extensive clinical trials to support what is
considered standard therapy for most of these conditions.
The Swollen Eye
Infections, inflammatory processes, or tumors may all
present as a swollen or protuberant eye. As the treatment
and outcome are different with each etiology, it is important
for the emergency physician to narrow the diagnostic
possibilities. Certain conditions are more prevalent in
certain age groups. (Intraocular neoplasms, for instance,
peak before the age of 10.) Immunosuppressed patients are
at risk for certain fungal diseases. In addition to a thorough
eye exam, a working knowledge of the anatomy of the orbit,
including the extraocular muscles, is essential to arrive at
the correct diagnosis. The CT scan is the test of choice for
evaluating the swollen eye.
Kawasaki Disease
Kawasaki disease, or mucocutaneous lymph node syndrome, is a multisystem disease, probably of infectious
origin, that presents with a bilateral, non-exudative conjunctivitis that spares the perilimbic area. It occurs primarily in
children under the age of 8. The development of coronary
artery aneurysms is a source of significant morbidity.
Recognition of the disease by the emergency physician and
resultant early treatment with intravenous immunoglobulin
(2 g/kg over 10 hours) and high-dose aspirin (100 mg/kg)
reduce both the duration of the disease and the incidence of
coronary artery aneurysms.
Bacterial Infections
The orbit is separated from the eyelids by a fascial layer that
attaches to the periosteum of the orbital bones (the orbital
septum; see Figure 2 on page 18). Periorbital cellulitis (POC)
(also known as pre-septal cellulitis) is defined as infection
anterior to the orbital septum (i.e., involving the tissue of the
lids). In contrast, orbital cellulitis (OC or post-septal
cellulitis) involves the orbit (and frequently tissues on both
sides of the orbital septum). Both POC and OC will present
Table 4. Therapy For Neonatal Conjunctivitis.
Disease
Medication
Other
Chlamydia trachomatis
Erythromycin 50 mg/kg/d PO divided QID for 14 days
Neisseria gonorrhoeae
Ceftriaxone 25-50 mg/kg IV or IM in a single dose,
not to exceed 125 mg*
Frequent saline eye irrigation;
ophthalmologic consult
Herpes simplex virus
Acyclovir 30-60 mg/kg/d IV divided q8h for 14-21 days
and 1% to 2% trifluridine, 1% iododeoxyuridine,
or 3% vidarabine, topically
Ophthalmologic consult
* Other acceptable regimens can be found in the 2000 Red Book: Report of the Committee on Infectious Diseases (see sources).
Sources: Centers for Disease Control and Prevention. 1998 guidelines for treatment of sexually transmitted diseases. MMWR Morb Mortal Wkly Rep
1998;47(No. RR-1); and The American Academy of Pediatrics. Chlamydial infections, gonococcal infections, herpes simplex infections, meningococcal
infections and Kawasaki Disease. In: Pickering LK, ed. 2000 Red Book: Report of the Committee on Infectious Diseases. 25th ed. Elk Grove Village, IL:
American Academy of Pediatrics: 1997; 208-212, 254-260, 309-313, 360-363,396-401, 650-656.
June 2002 www.empractice.net
17
Emergency Medicine Practice
sinusitis develops in patients with poor phagocytic function
and spreads contiguously to the orbit.
Fungal OC can be clinically indistinguishable from
bacterial disease. It also tends to be unilateral. The most
common clinical presentation is proptosis, decreased vision,
chemosis, ophthalmoplegia, and trigeminal anesthesia.
Treatment is with intravenous amphotericin B and
surgical debridement.93
Immunocompetent adults with chronic sinusitis
can develop a syndrome of allergic fungal sinusitis.
Seven percent of patients have some orbital involvement.
Treatment is surgical drainage of the sinuses and
oral antifungals.93
with significant pain, a tender and erythematous unilateral
swelling around the eye, conjunctival injection, and
chemosis. In POC, patients demonstrate full and painless
extraocular motions. Any impairment of extraocular movements
or pain on EOM testing should alert the emergency physician to
the possibility of OC.
In adults, the majority of cases of OC result from
contiguous spread of sinusitis, primarily the ethmoid
sinuses to the orbit. The initial pathogens are Staphylococcus
aureus, Streptococcus pneumoniae, and Haemophilus influenzae;
however, anaerobic bacteria soon predominate.93 Other
sources of OC are maxillary dental abscesses.94
A CT scan is indicated whenever there is suspicion that
the infection has spread beyond the septum, if the diagnosis
is unclear, or if the differential diagnosis includes noninfectious etiologies. It will delineate the extent of orbital
infection, presence of abscess collections, sinusitis, and
orbital osteomyelitis.
Treatment requires antibiotics covering Staphylococcus
and Streptococcus species as well as anaerobic organisms.
There are no controlled outcome studies. General recommendations include ampicillin/sulbactam or a thirdgeneration cephalosporin plus clindamycin. An orbital
abscess, osteomyelitis, or sinusitis usually requires adjunctive surgical drainage.93 Complications of OC include
cavernous sinus thrombosis, subdural empyema, and
meningitis or cerebritis.
Inflammatory Conditions
Idiopathic orbital inflammatory syndrome (formerly called
orbital pseudotumor) is thought to be an autoimmune
disorder (10% of cases are associated with diabetes, asthma,
rheumatoid arthritis, systemic lupus erythematosus, or
Crohns disease). Its presentation may be indistinguishable
from OC; however, a CT scan may show a diffuse infiltrate
that enhances with contrast, as opposed to an abscess with
or without sinusitis. Once systemic diseases such as
sarcoidosis, Wegeners granulomatosis, tuberculosis, or
syphillis are ruled out, treatment is usually begun with
corticosteroids.95 There are no large clinical trials; most
evidence is based on case series.
Thyroid-related ophthalmopathy (TRO) is diagnosed in
22% of patients before systemic hyperthyroidism develops.95
White females between 30 and 50 predominate, with a
female-to-male ratio of 6:1. TRO is generally bilateral and
gradual in onset, and usually it is not painful. The eyes are
generally proptotic due to collagen deposition, increased
retrobulbar fat, and orbital inflammation. A classic finding
Fungal Infections
Diabetics, patients with hematologic malignancies, those
treated with immunosuppressive drugs, and generally
debilitated patients are at risk for mucormycosis. Fungal
Table 5. Key Points In Managing The Red Eye.
1. Important historical data
Onsetgradual vs. rapid
Type of dischargeclear, mucoid, or purulent
Painpresence or absence
Itching
Changes in vision
Past medical historydiabetes, immunocompromise,
sexually transmitted diseases
Current medications
Figure 2. Sagittal section of orbit.
Bone
Orbital septum
2. Important physical findings
Condition of the eyelidscrusting, discharge, swelling
Visual acuitiesnormal or decreased
Location of rednessfocal or diffuse
Corneaclear or hazy
Anterior chambercells and flare, or visible hypopyon
Pupilnormal, constricted, or dilated
Fluorescein stainingulcer, punctate, dendrites
Upper eyelid
Cornea
3. Immediate referral to an ophthalmologist
Lack of response to presumed bacterial conjunctivitis
Hyperacute (gonococcal) bacterial conjunctivitis
Keratitis due to HSV infection
Acute angle-closure glaucoma
Scleritis
Uveitis
Pediatrics (ophthalmia neonatorum, HSV
neonatal conjunctivitis)
Emergency Medicine Practice
Lower eyelid
Orbital septum
Bony orbit
18
www.empractice.net June 2002
months, and without meningeal or focal neurologic
findings, vision loss, limitation of eye motion, eye malformation, or operation in the vicinity of the infection. These
children can be evaluated with blood culture and CBC
(what the CBC tells us is unclear, but it remains an accepted
ritual), without LP.99 Low-risk patients can be considered for
outpatient therapy; however, the parents should also be
willing and able to return at any sign of worsening. Daily
follow-up should be ensured.97 The American Academy of
Pediatrics issued a position statement that mild cases of
periorbital cellulitis (eyelid < 50% closed) may be treated
with appropriate oral antibiotic therapy as an outpatient
with daily patient encounters.100
As with adults, CT of the orbits and cranium is very
useful in defining the extent of the infection, sinusitis, or
abscess collection. A CT should be ordered on the suspicion
that the infection extends beyond the orbital septum. Any
orbital involvement mandates consultation with a surgical
specialist (ophthalmologist, ENT surgeon).
Parenteral antibiotics are standard for inpatient therapy
and are often administered as the first dose of an outpatient
regimen. There are no prospective trials comparing the
different regimens. Initial treatment is based on an estimation of the microbes involved and several clinical factors: the
severity of the process, the toxicity of the child, and the
suspicion of intracranial disease.
Inpatient regimens for OC/POC consist of:100
Ceftriaxone (100 mg/kg/d in 2 divided doses) or
Ampicillin-sulbactam (200 mg/kg/d in 4 divided
doses) plus
Vancomycin (60 mg/kg/d in 4 divided doses) if
infection is either known or likely to be caused by
highly resistant Streptococcus pneumoniae.
(present in 92% of patients) is upper and lower lid retraction. On downward gaze, the upper lid does not follow the
eyeball (lid lag). The autoimmune process also affects the
extraocular muscles, and patients may present with
extraocular motor paresis. TRO is considered an ophthalmologic emergency, as 22% of patients develop severe vision
loss if untreated.95 Treatment is begun with high-dose oral
steroids. Radiation therapy and surgical decompression are
reserved for non-responders.
Tumors
Both metastatic and primary orbital tumors generally
present unilaterally, after a gradual onset, and with mild
pain. There may be significant proptosis associated with
EOM dysfunction and significant visual loss. Primary
tumors tend to peak in childhood years, whereas metastatic
disease follows the general pattern of increasing incidence
of malignancies with aging. A CT scan of the orbit and
consultation are essential.
Pediatric Considerations
Periorbital Cellulitis/Orbital Cellulitis
The availability and widespread use of the H. influenzae type
B (HIB) vaccine between 1985 and 1990 has had a profound
effect on the microbiology, virulence, and treatment of
POC/OC. Standard management prior to 1990 included
aggressive evaluation with blood cultures and LP followed
by admission for IV antibiotics. Such aggressive interventions are rare in the current era. Today, the pathogenesis and
management of POC/OC more closely resembles adult
disease, with organisms associated with sinusitis predominating. If the sinusitis is acute, S. pneumoniae, nontypeable
H. influenzae, and Moraxella catarrhalis are most common.
With chronic sinusitis, S. aureus and anaerobes must also be
considered.96 If there is evidence of local trauma resulting in
a break in the dermis, skin flora are often causative agents.
Spread via the bloodstream may still occur in children
younger than 24 months of age, who are at risk for S.
pnemoniae bacteremia.97 In older children with bacteremia,
Group A Streptococcus predominates.97
It is important to differentiate soft-tissue swelling due
to an acute allergic reaction from POC. Children may also
present with erythema and edema of either eyelid secondary to an acute allergic reaction. In these instances, the child
is generally afebrile, looks well, and may complain of
itching in the area. In contrast to the violaceous color seen in
infectious causes, the erythema in allergic edema is less
prominent, and the edema has a lighter, watery type of
appearance. A trial dose of an oral antihistamine in the ED
may confirm allergic erythema if the symptoms resolve after
an hour of observation.
Children with POC/OC often present the day symptoms begin.98 There may be marked erythema, edema, fever,
proptosis, ophthalmoplegia, or pain with EOM motion.
Although the evidence comes exclusively from
retrospective chart reviews (the incidence of POC/OC is
probably too low for any successful prospective trial), a less
aggressive approach is likely safe in the HIB-vaccine era.
Low-risk patients are defined as nontoxic, older than 12
June 2002 www.empractice.net
If intracranial disease is suspected or known, consult
with a pediatric infectious disease specialist and a surgeon,
and consider adding metronidazole 15-35 mg/kg/d divided
q8h (maximum dose, 1-2 g/d) and nafcillin/vancomycin to
the third-generation cephalosporin.
The outpatient regimens for OC/POC are:
Ceftriaxone 50 mg/kg IM or IV (maximum, 1 g)
followed by either amoxicillin/clavulanate 45 mg/kg/d
divided twice daily PO for at least 10 days or
Azithromycin 12 mg/kg (maximum, 500 mg/d) for five
days in the penicillin-allergic child.101,102
When sinusitis is present or suspected, treatment
duration should be extended to reflect accepted courses for
this entity.
Dacryocystitis
Dacryocystitis (inflammation or infection of the nasolacrimal duct) may be acute or chronic. (See Figure 3 on page 20.)
Dacryocystitis occurs in children with congenital or
acquired nasolacrimal duct obstruction. Congenital
nasolacrimal duct obstruction (CNLDO) may occur in up to
70% of healthy newborns.103 It presents as eye watering,
crusting, and mucoid discharge without conjunctival
injection in a newborn that is otherwise well. As most cases
will resolve spontaneously by 1 year of age, conservative
19
Emergency Medicine Practice
topical ophthalmic antibiotics and elective nasolacrimal
duct probing by an ophthalmologist.105
management is generally the rule. Parents should massage
the lacrimal ducts several times a day. The duct is milked
by placing an clean index finger over the common canaliculus, thus preventing material from exiting from the lacrimal
punctum, and then applying gentle pressure in a downward
motion. Massage improves the chance for early resolution.103
Acquired nasolacrimal obstruction is usually the result of
trauma to the midface or orbit. Simple obstruction needs
to be differentiated from both chronic inflammation and
acute infection.
Acute dacryocystitis (AD) also presents with eye
discharge and crusting, but it is associated with lacrimal sac
or eyelid erythema and edema. It can occur as a complication of chronic dacryocystitis (CD) in neonates and older
infants and in older children in association with facial
trauma that disrupts the nasolacrimal duct. Some authorities believe neonates require a full sepsis evaluation,
including CBC, blood and urine cultures, and LP, due to
their relative immunosuppression. Such children should be
evaluated by ophthalmology or ENT, depending on the
practice in any given institution.87 Other authors recommend probing of the nasolacrimal duct by the specialist
with or without antibiotics.104 In older infants, an LP is not
necessary unless the child is ill-appearing or there are signs
of meningitis. All cases of acute dacryocystitis, no matter
what the age, are treated with intravenous antibiotics to
cover Staphylococcus and Streptococcus species, with early
probing of the duct by the consultant.105 In the case of
fracture-related AD, a stent may need to be placed in the
duct. POC/OC is a recognized complication of AD.105
Suggested antibiotic regimens include:
Cefotaxime 200 mg/kg/d, divided q8h plus nafcillin
100-200 mg/kg/d, divided q6h plus erythromycin
ophthalmic ointment
Ampicillin/sulbactam (Unasyn) 100-200 mg/kg/d
divided q6h (maximum, 6-12 g/d)
Tumors
Tumors that originate in the eye are far more common in
childhood than metastatic disease. They generally present
with vision loss and/or proptosis. These tumors may be
either benign or malignant. Clues to the presence of tumor
include proptosis, absence of light reflex, and decreased
visual acuity. CT scan and appropriate referral are crucial.
Conclusion
Infections, most often the sequelae of acute or chronic
sinusitis, are the most common causes of the unilateral
swollen eye. The emergency physician should be aware of
other etiologies, such as tumor or inflammation, the latter
especially if the proptosis is bilateral. Current therapy is
supported largely by small case series or retrospective
reviews.
Acute Vision Loss
In general, patients presenting to the ED with acute vision
loss should be referred quickly to an ophthalmologist. In
truly emergent conditions, minutes may count in preserving
vision. This section will not cover neurologic causes of
vision loss, such as aneurysms, TIAs (except to the retinal
artery), and strokes, nor does it address diseases of the optic
nerve beyond the orbit (optic chiasm, optic radiation, or
visual cortex).
History
Dividing patients by age and type of visual loss is the first
step in the approach to acute vision loss. Partial loss or
complaints of flashing lights or floaters often denote
retinal detachment. Non-traumatic vision loss under the age
of 50 is almost always due to optic neuritis (ON). Over the
age of 60, vascular causes predominate, with temporal
arteritis rarely occurring below 65 years of age.
Besides the age of the patient and the extent of visual
impairment, it is important to ask about perception of color,
central vs. peripheral vision loss, current medications, and
the presence of underlying medical conditions. Determine
how quickly the visual loss occurred and whether the
patient has pain.
Chronic dacryocystitis is a low-grade inflammation of
the lacrimal sac in the setting of nasolacrimal obstruction. It
can be difficult to differentiate from CNLDO. In CD, there is
a mucopurulent discharge from the lacrimal punctum and
crusting of the lashes, but with the absence of erythema in
either the lacrimal sac or the eyelid. Treatment consists of
Figure 3. Nasolacrimal apparatus.
Physical Examination
Superior lacrimal papilla and puncta
The examination should be systematic and is best approached in the following order.
Lacrimal canaliculi
Lacrimal sac
1. Visual Acuity And The Pinhole Test
Nasolacrimal duct
If visual acuity improves with looking through a pinhole,
the etiology of visual loss is likely to be optical (uncorrected
refractive error, lens or corneal opacity, or vitreous disease)
and not due to diseases of the CNS or the eye.107
Opening of nasolacrimal duct
2. Swinging Flashlight Test
Relative afferent pupillary defect (RAPD), formerly referred
to as the Marcus Gunn pupil sign, is detected by the
swinging flashlight test. This is performed by brisk alternat-
Inferior lacrimal papilla and puncta
Emergency Medicine Practice
20
www.empractice.net June 2002
rotated at rest (extorted). The sixth cranial nerve innervates
the lateral rectus muscle. An eye with a sixth nerve palsy
will be slightly adducted at rest and unable to abduct.108
ing stimulation of the eyes with a strong light source. The
normal response is constriction of the pupil when light is
shown directly in the eye. Paradoxical dilatation to direct
light is a positive RAPD test. The abnormal pupil will
initially dilate to direct light, but then constrict when the
light is shone in the opposite eye. This greater response to
consensual vs. direct stimulation establishes an afferent
defect in the eye with the positive test. This strongly suggests
disease of the optic nerve.107
6. Funduscopy
In early central retinal artery occlusion, funduscopy may
reveal the classic box car pattern of stagnant blood in the
arteries or veins. A pale retina with a spared fovea (the
cherry red spot) is pathognomonic of late retinal artery
occlusion. Venous congestion and hemorrhage may be
present in central retinal vein occlusion. Optic disc edema or
congestion may be evident in ON and pseudotumor cerebri.
3. Evaluation Of Pupil Size, Shape, And Response
To Light And Accommodation
The size of the pupil depends on a balance between
sympathetic and parasympathetic tone. The parasympathetic fibers travel in the oculomotor (III) nerve to the ciliary
ganglion. Postganglionic axons innervate the pupillary
constrictor muscle. The sympathetic fibers exit the spinal
cord at T1 to T2 and ascend in the sympathetic trunk to the
superior cervical ganglion. Postganglionic fibers then
ascend via the carotid plexuses and the nasociliary nerve to
innervate the pupillary dilator muscle.108 Significant pupil
findings include:
Adies tonic pupil: a dilated pupil that reacts poorly to
light, but better to accommodation. It is usually
unilateral. The defect is usually localized to the third
cranial nerve ciliary ganglion and is usually due to a
viral infection or inflammatory process.108
Argyll-Robertson pupil: a small, irregular pupil
associated with CNS syphilis.
Horners syndrome: a miotic pupil that reacts to light.
It is the result of sympathetic denervation of the pupil.
Causes include apical lung tumors, trauma to the spinal
cord, lateral brainstem vascular lesions, or syringomyelia. The pupil will usually dilate to instillation of
topical mydriatics. Patients may demonstrate ptosis of
the involved eye and inability to sweat on that side of
their face (anhydrosis).
7. Tests For Malingering
Emergency physicians are occasionally faced with patients
who claim sudden bilateral blindness. While such events
occur, they are quite rare, and several simple tests performed without sophisticated lenses or prisms can substantiate the impression of malingering. The first step is to know
how the truly blind eye responds to certain maneuvers.
Patients who are bilaterally blind cannot make eye contact,
nor will they have spontaneous accommodation and
convergence. However, when asked to look at their own
finger, malingerers will demonstrate accommodation and
convergence. A sudden bright light should not cause any
blinking or flinching. A menacing action, likewise, should
cause no response, although throwing a punch toward the
face can cause blinking if the air from the force of the blow
hits the patients cornea. (Besides, just in case the patient can
see, dont be too menacing.)
Unless the etiology of the blindness is cortical or
subcortical, the pupils will be moderately dilated and
unreactive to light. (However, the patient with cortical
blindness will still have a pupillary response.)
With unilateral blindness, there should be a positive
RAPD test in the affected eye (unless the lesion is cortical or
subcortical). The truly blind eye will deviate first when
following an object. If the good eye is suddenly covered,
the blind eye should not continue to follow the object.
Moving a mirror in front of the blind eye should not result
in any movement of the eye. Having a patient stare straight
ahead while passing a piece of paper with wide stripes in
front of the eyes will produce involuntary nystagmus in a
patient with intact vision. (Cardiac monitor paper with
alternating blackened wide blocks works well for this. )
Some patients may even place anticholinergic
preparations in their eye to create a blown pupil.
Unlike a neurologically dilated pupil, the pharmacologicblockaded eye will not constrict when 1% pilocarpine is
placed in the eye. If there is no structural abnormality of the
iris on slit-lamp examination and if the IOP is normal, then
it is likely that the dilated pupil is pharmacologically
induced. Only a few cases of an acute Adies pupil or
traumatic iritis will produce the same result.109
4. Visual Fields
Evaluating visual fields by direct confrontation is important
in ON. Patients with this condition may have central
scotoma with sparing of the periphery. Abnormalities of
visual fields may also detect optic chiasm or associated
neurologic disease. For instance, a pituitary tumor compressing the optic chiasm may present with a bitemporal
hemianopsia, whereas a large hemispheric stroke may result
in a homonymous hemianopsia.
5. Evaluation Of The Extraocular Muscles
Have patients hold their head still and use their eyes to
follow the examiners finger up and down and side to side.
The third cranial nerve innervates the medial, superior, and
inferior rectus muscles as well as the inferior oblique and
levator palpebri muscles. The parasympathetic fibers also
run with the third nerve. An eye with a third nerve palsy
will be deviated down and out due to unopposed actions of
the IVth and VIth nerves and will not move up or medially.
The fourth cranial nerve innervates the inferior oblique
muscle. An eye with a fourth nerve palsy will be externally
June 2002 www.empractice.net
Retinal Detachment
Retinal detachment may present as sudden onset of light
flashes or floaters, or with the classic description of a
shade coming down. It is most commonly idiopathic,
21
Emergency Medicine Practice
but it may be associated with inflammation, trauma,
surgery, or infections in immunocompromised patients. If
the detachment involves the macula, visual loss will be
severe. Many detachments are peripheral and thus difficult
to appreciate on direct funduscopy of the undilated eye
(indirect ophthalmoscopy being more accurate in diagnosis). Using a short-acting midriatic such as tropicamide
(Mydriasil) may aid in visualization of the fundus. If
visualized, the detachment will appear as an elevated gray
area.110 All retinal detachments should be referred to an
ophthalmologist for treatment.
There is an association between isolated ON and
multiple sclerosis (MS). ON can be the initial presentation
of MS in 20% of cases and will affect 50% of patients
who have MS sometime during their lifetime. IV methylprednisolone (250 mg IV QID x 3 days) improves short-term
visual outcome and may slow the progression of MS
over the subsequent two years. Consultation with an
ophthalmologist or neurologist should be done prior to
initiating treatment.
Other Causes
There are certain clinical findings not characteristic of ON
that should prompt a further workup: visual function that
worsens after two weeks or shows no improvement after
six weeks, bilateral ON (collagen vascular disease or
vasculitis), severe optic disc swelling or hemorrhage
(possible external compression of the optic nerve),
bitemporal hemianopsia (pituitary masses), and age
less than 18.115 Possible causes include:
Infections: Cat-scratch disease, Lyme disease, syphilis,
toxoplasmosis, toxocariasis, and histoplasmosis can
present with painless visual loss and optic disc edema.
Sarcoidosis generally affects the anterior chamber
(uveitis); however, the optic nerve is the second most
affected cranial nerve after the VIIth nerve. Ninety
percent of patients will have abnormalities on chest
radiography or CT scan.112
Acute methanol intoxication: Accidental or intentional
overdose with methanol presents with visual disturbances often described as being in a snow storm. The
visual complaints, abdominal pain, and accompanying
severe anion and osmolar gap acidosis should suggest
the diagnosis. Treatment involves bicarbonate and
fomepizole, followed by dialysis to remove the formic
acid that forms the basis for methanol toxicity.116,117
All seems infected that the infected spy / As all looks yellow
to the jaundicd eye.Alexander Pope (1688 - 1744),
English poet, An Essay on Criticism.
Double Vision
Double vision (diplopia) may be monocular or binocular. A
prospective survey of all patients presenting to an ophthalmologic ED (in the United Kingdom) over a nine-month
period found that monocular diplopia represented about
20% of cases.111 Monocular diplopia is almost always due to
abnormalities in the eyeball itself or to problems with
contact lenses or bifocal glasses. In contrast, binocular
diplopia is due to dysfunction of the extraocular muscles.
Most cases of binocular diplopia are due to abnormalities of
the cranial nerves (from systemic illnesses such as diabetes
or vasculitis), extraocular muscle pathology (either congenital or acquired), or trauma. The most frequent traumatic
cause is a blow-out fracture of the orbit with subsequent
entrapment of the inferior rectus muscle. A small percentage
of patients develop diplopia as a result of retro-orbital
tumors or inflammatory processes. Other rare causes
include from supra-nuclear palsies, brainstem ischemia, and
pituitary tumors.111
Acute Vision Loss Under The Age Of 50
Vision Loss Over The Age Of 60
Central Retinal Artery Occlusion
Optic neuritis is almost exclusively a disease affecting
individuals between 15 and 45, with a significant preponderance of white females. It has been reported in children;
however, less than 1% of cases occur in individuals over 50
years of age.112,113 The etiology is as yet undetermined.
Significant visual improvement will occur in the first 4-6
weeks, with 95% of patients having visual acuities of 20/40
twelve months after the episode.114
The onset of visual loss is often rapid (over hours), but
it may develop over days, with maximum visual loss at two
weeks. The amount of visual loss varies from mild to severe.
Many patients also complain of alterations in color vision.115
Almost all patients complain of periorbital pain that is
exacerbated by extraocular movements.112 In the majority of
patients, the disease is retrobulbar, so that the disc may
appear normal (the origin of the old saw regarding ONthe
patient doesnt see anything and the doctor doesnt see
anything). In the third of patients who have anterior ON,
the disc may appear edematous. The diagnosis is largely
clinical, relying on the presence of decreased vision (either
central or peripheral) and an afferent pupillary defect.
Routine lab tests to screen for etiologies other than ON, in
the absence of clinical findings, are of very little use.115
Emergency Medicine Practice
Central retinal artery occlusion (CRAO) may be caused by
atherosclerotic obstruction, vasospasm, embolism, or
systemic hypotension.118 It is associated with systemic
diseases such as hypertension, diabetes, atherosclerosis,
vasculitis, hypercoagulable states, and migraines.
The classic presentation is sudden, painless, and severe
visual loss. The classic funduscopic finding is a pale,
edematous retina with a cherry red spot representing the
unaffected choroidal vascular bed in the ischemic fovea.
When the cherry red spot is present, it implies ischemia of
three hours or longer.
The general prognosis is poor; however, there are case
reports of return of vision even after 72 hours of arterial
occlusion. Interventions of low and unproven efficacy are
generally recommended for the emergency physician more
on the basis of something is better than nothing. Interventions include placing the patient supine and performing
ocular massage. To do this, apply pressure five seconds on
then five seconds off, for 15-30 minutes. Because carbon
dioxide dilates cerebral vasculature (and could allow an
arterial clot to move downstream), have the patient
rebreathe CO2. If a mixture of 95% O2 5% CO2 is unavailable,
22
www.empractice.net June 2002
a paper bag may be used. Intravenous acetazolamide
(500 mg) may lower IOP.118 Paracentesis by an ophthalmologist is sometimes attempted, although it has a high complication rate and must be repeated every two hours to
maintain a low IOP. It is not recommended in recent
literature or textbooks.
Recently, intra-arterial urokinase has been investigated.
However, a recent meta-analysis has shown only a modest
improvement with this aggressive approach (27% vs. 18%21% with conservative treatment).118
are often the ones who note an abnormality with the eye
or with vision. Congenital cataracts and glaucoma are
usually discovered in the newborn nursery. Cataracts are
detected as an absent red reflex, or leukocoria, when an
ophthalmoscope is shone directly on the pupil. All cataracts
should be urgently referred to an ophthalmologist, as the
treatment of choice is surgical. Once the cataract is removed,
the ultimate prognosis is closely related to compliance with
amblyopia therapy.122
Congenital glaucoma (or infantile glaucoma), although
rare (less than 1/10,000 live births), is a significant cause
of childhood blindness.122 Infantile glaucoma should be
suspected when excessive tearing and photophobia
accompany an increase in corneal size or an enlarged
globe. Clouding of the cornea may also be evident. The
treatment of congenital glaucoma is primarily surgical, and
ophthalmologic referral should be rapid whenever the
diagnosis is suspected.
Central Retinal Vein Occlusion
Central retinal vein occlusion (CRVO) presents with either
abrupt or gradual decrease in vision. The pathogenesis of
CRVO is generally unknown, although in older individuals
it is associated with hypertension, atherosclerosis, diabetes,
cardiovascular disease, and hyperlipidemia.
Visual acuity may range from mild impairment to light
perception.119 Funduscopic examination early in the course
will usually reveal retinal hemorrhages, dilated veins, and a
swollen optic disc.
There is no generally effective medical therapy. Certain
subsets of patients (those with diabetes or glaucoma) are
candidates for specific laser techniques. Surgery and rTPA
are still considered experimental.119 Prognosis for recovery is
directly related to visual acuity at presentation: 65% of
patients with 20/40 maintained that vision at three-year
follow-up, whereas 80% of patients with 20/200 vision
remained at that level.120
Children
Amblyopia (or abnormal vision in a structurally normal
eye) occurs before the age of 10. It develops when an
unclear image falls on the retina and is then transmitted to
the immature visual cortex. Amblyopia may result from
strabismus (lazy eye) or from external obstruction to vision
(capillary hemangioma of the eyelid). It is diagnosed when
there is a large discrepancy in visual acuity between the two
eyes. Amblyopia should be referred to an ophthalmologist
for outpatient management.
Temporal Arteritis
Adolescents
Temporal arteritis (TA) is a granulomatous inflammation of
extracranial arteries that may lead to rapid or sudden visual
loss either by ischemic optic neuropathy (90% of cases) or
acute central retinal artery occlusion. It is a disease of the
elderly and rarely occurs before the age of 65. The majority
of cases occur in Caucasians, especially those of Scandinavian descent. The role of the emergency physician is the
identification of the patient with TA before visual loss occurs,
because when it does, it is often rapid and permanent. TA
may present in association with polymyalgia rheumatica, a
complex of anemia, elevated erythrocyte sedimentation rate
(ESR), proximal joint pain, fatigue, low-grade fever, and
weight loss.107
TA should be considered in any elderly patient who
presents with a headache and temporal tenderness. Jaw
claudication (pain in the masseter muscles with chewing)
and tender or indurated temporal arteries may also provide
clues to the diagnosis. The ESR is almost always elevated,
often greater than 100. Although there are isolated cases of
TA with a low or normal ESR, this is so rare that an alternative diagnosis should be sought.120,121 Temporal artery biopsy
is the gold standard for diagnosis; however, if the patient
has visual symptoms on presentation, IV methylprednisolone is recommended while awaiting the biopsy results.120
ON is an uncommon cause of vision loss in children. In
children, ON frequently presents with bilateral sudden
vision loss occurring after a recent viral illness.123 ON has
been associated with measles, mumps, chickenpox, pertussis, EBV infections, immunizations,124 and Lyme disease.123
Retrospective studies by Morales et al and Brady et al
provide conflicting data on visual prognosis. However,
there appears to be a significant risk of permanent and
considerably diminished vision (22% of patients in Brady et
al and 29% in Morales et al).125,126 Children are less likely to
develop MS than adults.123 Unilateral disease has a better
visual prognosis and an increased risk of subsequent MS vs.
bilateral disease.
There are no large, randomized, controlled studies on
its management. Current practice is based mainly on the
Optic Neuritis Treatment Trial (ONTT), a multicenter,
prospective, randomized trial that did not include pediatric
patients.123 Intravenous steroids and a slow taper are
recommended to treat ON (again, based exclusively on
adult clinical trials).124
Conclusion
The causes of acute vision loss are strongly tied to the age of
the patient. In the neonate, congenital cataracts, glaucoma,
and tumors are most frequent. In the child, refractive errors,
amblyopia, and tumors predominate. In the older child or
adolescent, the emergency physician must also consider the
diagnosis of optic neuritis. ON is the overwhelming cause of
Pediatric Considerations
Infants
Parents, especially with infants or pre-verbal children,
June 2002 www.empractice.net
23
Emergency Medicine Practice
13.
Sklar DP, Lauth JE, Johnson DR. Topical anesthesia of the eye as a
diagnostic test. Ann Emerg Med 1989 Nov;18(11):1209-1211.
(Convenience sample; 71 patients)
14. Bartfield JM, Holmes TJ, Raccio-Robak N. A comparison of
proparacaine and tetracaine eye anesthetics. Acad Emerg Med 1994
Jul;1(4):364-367. (Prospective, volunteer, randomized, controlled
trial; 23 subjects)
15. Brady MD, Hustead RR, Robinson RH, et al. Dilution of
proparacaine in balanced salt solution reduces pain of anesthetic
instillation in the eye. Reg Anesth 1994 May;19(3):196-198.
(Randomized, controlled trial; 42 adults)
16. Aylward GW, Wilson RS. Contamination of dropper bottles with
tear fluid in an ophthalmic outpatient clinic. Br Med J (Clin Res Ed)
1987 Jun 20;294(6587):1587. (Descriptive)
17. Hoffman CJ, Laibson PR. Corneal manifestations of local and
systemic therapy. In: Krachmer JH, Mannis MJ, Holland E, eds.
Cornea. St. Louis: Mosby; 1997:1023-1028. (Textbook chapter)
18. Bode DD, Manson RA. An expedient lid retracter. J Pediatr
Ophthalmol Strabismus 1978 Jan;15(1):54.
19.* Alward WLM. Medical management of glaucoma. N Engl Med
1998 Oct 29;339(18):1298-1307. (Review)
20. Hessemer V, Rossler R, Jacobi KW. Tono-pen, a new tonometer.
Internat Ophthal 1989 Jan;13(1-2):51-56. (2 studies comparing the
Tono-pen with the Goldmann tonometer)
21. Bafa M, Lambrinakis I, Dayan M, et al. Clinical comparison of the
measurement of the IOP with the ocular blood flow tonometer, the
Tono-pen XL and the Goldmann applanation tonometer. Acta
Ophthalmol Scand 2001 Feb;79(1):15-18. (Randomized, controlled
trial; 99 eyes)
22. Nagington J, Sutehall GM, Whipp P. Tonometer disinfection
and viruses. Br J Ophthalmol 1983 Oct;67(10):674-676. (Microbiologic study)
23. Chung CW, Cohen EJ. Eye disorders: bacterial conjunctivitis. West
J Med 2000 Sep;173(3):202-205. (Systematic review)
24. Sheikh A, Hurwitz B. Topical antibiotics for acute bacterial
conjunctivitis: a systematic review. Br J Gen Pract 2001
Jun;51(467):473-477. (Systematic review of six published
clinical trials)
25. Friedlaender MH. A review of the causes and treatment of
bacterial and allergic conjunctivitis. Clin Ther 1995 SepOct;17(5):800-810; discussion 779. (Review; 213 references)
26.* Sheik A, Hurwitz B, Cave J. Antibiotics versus placebo for
acute bacterial conjunctivitis. Cochrane Eyes and Vision
Group. Cochrane Database of Systematic Reviews. 2001; issue 4.
(Systematic review)
27. Adler AG, McElwain GE, Merli GJ, et al. Systemic effects of eye
drops. Arch Intern Med 1982 Dec;142(13):2293-2294. (Review)
28. Kettenmeyer A, Jauch A. The French Lomefloxacin Group. A
double-blind double-dummy multicenter equivalence study
comparing topical Lomefloxacin 0.3% twice daily with
Norfloxacin 0.3% four times daily in the treatment of acute
bacterial conjunctivitis. J Drug Assess 1998;1(1):69-80. (Multicenter,
double- blind clinical trial)
29. Friedlaender MH. Twice-a-day versus four-times-a-day ofloxacin
treatment of external ocular infection. CLAO J 1998 Jan;24(1):48-51.
(Prospective, randomized, controlled trial; 50 patients)
30. Soukiasian S, Baum J. Bacterial conjunctivitis. In: Krachmer JH,
Mannis MJ, Holland E, eds. Cornea. St. Louis: Mosby; 1997:758772. (Textbook chapter)
31. Wan WL, Farkas GC, May WN, et al. The clinical characteristics
and course of adult gonococcal conjunctivitis. Am J Ophthalmol
1986 Nov 15;102(5):575-583. (Retrospective; 21 cases)
32. Haimovici R, Roussel TJ. Treatment of gonococcal conjunctivitis
with single-dose intramuscular ceftriaxone. Am J Ophthalmol 1989
May 15;107(5):511-514. (Consecutive series; 13 patients)
33. Viswalingam ND, Darougar S, Yearsley P. Oral doxycycline in the
treatment of adult chlamydial ophthalmia. Br J Ophthalmol 1986
Apr;70(4):301-304. (Comparative; 93 patients)
34. Lindquist TD. Conjunctivitis: an overview and classification. In:
Krachmer JH, Mannis MJ, Holland E, eds. Cornea. St. Louis:
Mosby; 1997:745-757. (Textbook chapter)
35. Ward JB, Siojo LG, Waller SG. A prospective, masked clinical trial
of trifluridine, dexamethasone, and artificial tears in the treatment
of epidemic keratoconjunctivitis. Cornea 1993 May;12(3):216-221.
acute vision loss in patients under 50 years of age, while
vascular disease is the main culprit in patients over 60. The
emergency physician should also consider temporal arteritis
in the geriatric population, as rapid institution of therapy
can prevent further loss of vision.
The next best thing to being clever
is being able to quote someone who is.
Mary Pettibone Poole, A Glass Eye at a Keyhole, 1938.
General Conclusion
With a little detective work, a thorough exam, and an
understanding of the incidence and presentation of the most
common and most serious disorders, the ED physician
should be well-prepared to deal with non-traumatic eye
emergencies. We must recognize when urgent consultation
with an ophthalmologist is needed and when it can safely
be delayed.
References
Evidence-based medicine requires a critical appraisal of the
literature based upon study methodology and number of
subjects. Not all references are equally robust. The findings
of a large, prospective, randomized, and blinded trial
should carry more weight than a case report.
To help the reader judge the strength of each reference,
pertinent information about the study, such as the type of
study and the number of patients in the study, will be
included in bold type following the reference, where
available. In addition, the most informative references cited
in the paper, as determined by the authors, will be noted by
an asterisk (*) next to the number of the reference.
1.
McCaig LF, Ly N. National Hospital Ambulatory Medical Care
Survey: 2000 Emergency Department Summary. Advance Data
No. 326. April 22, 2002. Centers for Disease Control and
Prevention. (U.S. government data)
2.* Comprehensive Adult Medical Eye Evaluation. Preferred Practice
Pattern. American Academy of Ophthalmology 2000 Sept. (Clinical
practice guideline)
3.
As cited in: The Ultimate Success Quotations Library, 1997.
4.* Leibowitz HM. The red eye. N Engl Med 2000 Aug 3;343(5):345351. (Systematic review)
5.* Conjunctivitis. Preferred Practice Pattern. American Academy of
Ophthalmology 1998 Sept. (Clinical practice guideline)
6.
Primary Angle Closure. Preferred Practice Pattern. American
Academy of Ophthalmology 2000 Sept. (Clinical practice guideline)
7.
Powers DW, Meador SA. Testing visual acuity in the emergency
department: a simple method of correcting refractive error by
using the hand-held ophthalmoscope. Ann Emerg Med 1986
Jul;15(7):818-819. (Description of method)
8.
Rose GE, Pearson RV. Unequal pupil size in patients with
unilateral red eye. BMJ 1991 Mar 9;302(6776):571-572. (Consecutive series)
9.
Au YK, Henkind P. Pain elicited by consensual pupillary reflex: a
diagnostic test for acute iritis. Lancet 1981 Dec 5;2(8258):1254-1255.
(Consecutive series)
10.* Talbot EM. A simple test to diagnose iritis. BMJ 1987 Oct
3;295(6602):812. (Consecutive series)
11. Roberts JR, Hedges JR, eds. Clinical Procedures in Emergency
Medicine. Philadelphia; W.B. Saunders;1998. (Textbook)
12. Anderson DF, Sullivan PM, Luff AJ, et al. Direct ophthalmoscopy
versus slit lamp biomicroscopy in diagnosis of the acute red eye. J
R Soc Med 1998 Mar;91(3):127-128. (Prospective, controlled
clinical trial; 98 patients)
Emergency Medicine Practice
24
www.empractice.net June 2002
36.
37.
38.*
39.
40.
41.
42.
43.
44.
45.*
46.
47.
48.*
49.
50.*
51.*
52.
53.
54.
55.*
(Prospective, randomized, controlled trial; 74 patients)
Shiuey Y, Ambati BK, Adamis AP. A randomized, double-masked
trial of topical ketorolac versus artificial tears for treatment of viral
conjunctivitis. Ophthalmology 2000 Aug;107(8):1512-1517.
(Randomized, controlled trial; 117 patients)
Stamler JF. Viral conjunctivitis. In: Krachmer JH, Mannis MJ,
Holland E, eds. Cornea. St. Louis: Mosby; 1997;773-777.
(Textbook chapter)
Bielory L, Goodman PE, Fisher EM. Allergic ocular disease. A
review of pathophysiology and clinical presentations. Clin Rev
Allergy Immunol 2001 Apr;20(2):183-200. (Systematic review)
Raizman MB, Rothman JS, Maroun F, et al. Effect of eye rubbing
on signs and symptoms of allergic conjunctivitis in cat-sensitive
individuals. Ophthalmology 2000 Dec;107(12):2158-2161. (Two
comparative, controlled clinical trials; 13 patients in the first and
20 patients in the second)
Lanier BQ, Tremblay N, Smith JP, et al. A double-masked
comparison of ocular decongestants as therapy for allergic
conjunctivitis. Ann Allergy 1983 Mar;50(3):174-177. (Prospective,
randomized, double-blind trial; 89 patients)
Tauber J, Raizman MB, Ostrov CS, et al. A multicenter comparison
of the ocular efficacy and safety of diclofenac 0.1% solution with
that of ketorolac 0.5% solution in patients with acute seasonal
allergic conjunctivitis. J Ocul Pharmacol Ther 1998 Apr;14(2):137145. (Multicenter, prospective, randomized, controlled trial;
60 patients)
Laibovitz RA, Koester J, Schaich L, et al. Safety and efficacy of
diclofenac sodium 0.1% ophthalmic solution in acute seasonal
allergic conjunctivitis. J Ocul Pharmacol Ther 1995;11(3):361-368.
(Randomized, controlled trial; 20 patients)
Ballas Z, Blumenthal M, Tinkelman DG, et al. Clinical evaluation
of ketorolac tromethamine 0.5% ophthalmic solution for the
treatment of seasonal allergic conjunctivitis. Surv Ophthalmol 1993
Jul;38 Suppl:141-148. (Multicenter, randomized, controlled trial;
148 patients)
Physicians Desk Reference. Montvale, NJ: Medical Economics; 2002.
el Hennawi M. A double blind placebo controlled group
comparative study of ophthalmic sodium cromoglycate and
nedocromil sodium in the treatment of vernal keratoconjunctivitis.
Br J Ophthalmol 1994 May;78(5):365-369. (Randomized, controlled
trial; 138 patients)
Kray KT, Squire EN Jr, Tipton WR, et al. Cromolyn sodium in
seasonal allergic conjunctivitis. J Allergy Clin Immunol 1985
Oct;76(4):623-627. (Randomized, controlled trial; 58 patients)
Verin PH, Dicker ID, Mortemousque B. Nedocromil sodium eye
drops are more effective than sodium cromoglycate eye drops
for the long-term management of vernal keratoconjunctivitis.
Clin Exp Allergy 1999 Apr;29(4):529-536. (Randomized, controlled
trial; 34 children)
Henshaw K, Sheikh A, Smeeth L, et al. Mast cell stabilizers for
seasonal and perennial allergic conjunctivitis. Cochrane Review.
The Cochrane Library, Issue 3, 2001. (Systematic review)
Pflugfelder SC. Advances in the diagnosis and management
of keratoconjunctivitis sicca. Curr Opin Ophthalmol 1998
Aug;9(4):50-53. (Review)
Care of the Patient with Ocular Surface Disease. American
Optometric Association. 1995 (reviewed 1997). (Clinical
practice guideline)
Blepharitis. Preferred Practice Pattern. American Academy of
Ophthalmology. 1998 Sept. (Clinical practice guideline)
Frucht-Pery J, Solomon A, Siganos CS, et al. Treatment of inflamed
pterygium and pinguecula with topical indomethacin 0.1%
solution. Cornea 1997 Jan;16(1):42-47. (Randomized, controlled
trial; 51 patients)
Frucht-Pery J, Siganos CS, Solomon A, et al. Topical indomethacin
solution versus dexamethasone solution for treatment of inflamed
pterygium and pinguecula: a prospective randomized clinical
study. Am J Ophthalmol 1999 Feb;127(2):148-152. (Randomized,
controlled trial; 51 patients)
Chiapella AP, Rosenthal AR. One year in an eye casualty clinic.
Br J Ophthalmol 1985 Nov;69(11):865-870. (Observational;
6576 patients)
Flynn CA, DAmico F, Smith G. Should we patch corneal
abrasions? A meta-analysis. J Fam Pract 1998 Oct;47(4):264-270.
June 2002 www.empractice.net
56.
57.
58.*
59.*
60.
61.*
62.
63.
64.
65.
66.*
67.
68.
69.*
70.*
71.
72.
73.
74.*
75.
76.
77.
78.*
25
(Meta-analysis)
Kaiser PK, Pineda R 2nd. A study of topical nonsteroidal antiinflammatory drops and no pressure patching in the treatment of
corneal abrasions. Corneal Abrasion Patching Study Group.
Ophthalmology 1997 Aug;104(8):1353-1359. (Randomized, blinded,
placebo-controlled trial; 100 patients)
Szucs PA, Nashed AH, Allegra JR, et al. Safety and efficacy of
diclofenac ophthalmic solution in the treatment of corneal
abrasions. Ann Emerg Med 2000 Feb;35(2):131-137. (Randomized,
controlled trial; 49 patients)
Clemons CS, Cohen EJ, Arentsen JJ, et al. Pseudomonas ulcers
following patching of corneal abrasions associated with contact
lens wear. CLAO J 1987 May;13(3):161-164. (Retrospective,
case report)
Schein OD. Contact lens abrasions and the nonophthalmologist.
Am J Emerg Med 1993 Nov;11(6):606-608. (Case report)
Pepose JS, Wilhelmus KR. Divergent approaches to the
management of corneal ulcers. Am J Ophthalmol 1992;114:
630-632. (Review)
Cheung J, Slomovic AR. Microbial etiology and predisposing
factors among patients hospitalized for corneal ulceration. Can J
Ophthalmol 1995 Aug;30(5):251-255. (Case report)
Bacterial Keratitis. Preferred Practice Pattern. American Academy of
Ophthalmology. 2000 Sept. (Clinical practice guideline)
Benson WH, Lanier JD. Current diagnosis and treatment of
corneal ulcers. Curr Opin Ophthalmol 1998 Aug;9(4):45-49.
(Systematic review)
No authors listed. Ofloxacin monotherapy for the primary
treatment of microbial keratitis: a double-masked, randomized,
controlled trial with conventional dual therapy. The Ofloxacin
Study Group. Ophthalmology 1997 Nov;104(11):1902-1909.
(Multicenter, randomized, blinded, trial; 122 patients)
Hyndiuk RA, Eiferman RA, Caldwell DR, et al. Comparison of
ciprofloxacin ophthalmic solution 0.3% to fortified tobramycincefazolin in treating bacterial corneal ulcers. Ciprofloxacin
Bacterial Keratitis Study Group. Ophthalmology 1996
Nov;103(11):1854-1862; discussion 1862-1863. (Multicenter,
randomized, controlled trial; 324 patients)
Goldstein MH, Kowalski RP, Gordon YJ. Emerging
fluoroquinolone resistance in bacterial keratitis: a 5-year review.
Ophthalmology 1999;106:1313-1318. (Review)
Walton RC, Nussenblatt RB. Anterior uveitis. In: Krachmer JH,
Mannis MJ, Holland E, eds. Cornea. St. Louis: Mosby; 1997:14931503. (Textbook chapter)
As cited in: The Columbia World of Quotations, 1996.
Pavan-Langston D. Herpes simplex of the ocular anterior
segment. Curr Clin Top Infect Dis 2000;20:298-324. (Review)
Gaynor BD, Margolis TP, Cunningham ET Jr. Advances in
diagnosis and treatment of herpetic uveitis. Int Ophthalmol Clin
2000 Spring;40(2):85-109. (Systematic review)
No authors listed. Acyclovir for the prevention of recurrent herpes
simplex virus eye disease. Herpetic Eye Disease Study Group. N
Engl J Med 1998 Jul 30;339(5):300-306. (Multicenter, randomized,
controlled trial; 703 patients)
Harding SP, Lipton JR, Wells JC. Natural history of herpes zoster
ophthalmicus: predictors of postherpetic neuralgia and ocular
involvement. Br J Ophthalmol 1987;71:353-358. (Review)
Cobo LM, Foulks GN, Liesegang T, et al. Oral acyclovir in the
treatment of acute herpes zoster ophthalmicus. Ophthalmology
1986 Jun;93(6):763-770. (Randomized, controlled trial;
71 patients)
Klotz SA, Penn CC, Negvesky GJ, et al. Fungal and parasitic
infections of the eye. Clin Microbiol Rev 2000 Oct;13(4):
662-685. (Review)
Bozeman W. Acute angle-closure glaucoma. In: Harwood-Nuss A,
et al, eds. The Clinical Practice of Emergency Medicine. Philadelphia:
Lippincott Williams & Wilkins; 2000:67-71. (Textbook chapter)
Ritch R, Lowe RF, et al, eds. The Glaucomas. St. Louis: Mosby;
1989. (Textbook)
Coleman AL. Glaucoma. Lancet 1999 Nov 20;354(9192):
1803-1810. (Review)
Ritch R, Lowe RF. Angle-closure glaucoma: therapeutic overview.
In: Ritch R, et al, eds. The Glaucomas. St. Louis: Mosby; 1996.
Chapter 74. (Textbook chapter)
Emergency Medicine Practice
Nuss A, et al, eds. The Clinical Practice of Emergency Medicine. 3rd
ed. Philadelphia: Lippincott Williams & Wilkins; 2000:1246.
(Textbook chapter)
102. Personal communication with Deborah Meislich, MD, Pediatric
Infectious Disease, Cooper Hospital/UMC, Camden, NJ.
103. Sharma S. Ophthaproblem. Congenital nasolacrimal duct
obstruction. Can Fam Physician 1998 Oct;44:2085, 2095.
(Case report)
104.* Pollard ZF. Treatment of acute dacryocystitis in neonates. J Pediatr
Ophthalmol Strabismus 1991 Nov;28(6):341-343. (25 newborns)
105. Campolattaro BN, Lueder GT, Tychsen L. Spectrum of pediatric
dacryocystitis: medical and surgical management of 54 cases. J
Pediatr Ophthalmol Strabismus 1997 May;34(3):143-153. (Case
report; 54 patients)
106. Donahue SP, Khoury JM, Kowalski RP. Common ocular infections.
A prescribers guide. Drugs 1996 Oct;52(4):526-540. (Review)
107.* Laskowitz D, Liu GT, Galetta SL. Acute visual loss and other
disorders of the eyes. Neurol Clin 1998 May;16(2):323-353.
(Systematic review)
108. Young PA, Young PH. Basic Clinical Neuroanatomy. Baltimore:
Williams & Wilkins; 1997. (Textbook)
109. Burde RM, Savino PJ, Trobe JD. Clinical Decisions in NeuroOphthalmology. St Louis: Mosby; 1992. (Textbook)
110.* Morgan A, Hemphill RR. Acute visual change. Emerg Med Clin
North Am 1998 Nov;16(4):825-843, vii. (Review)
111. Morris RJ. Double vision as a presenting symptom in an
ophthalmic casualty department. Eye 1991;5(Pt 1):124-129.
(Prospective; 275 patients)
112. Eggenberger ER. Inflammatory optic neuropathies. Ophthalmol
Clin North Am 2001 Mar;14(1):73-82. (Systematic review)
113. Rodriguez M, Siva A, Cross SA, et al. Optic neuritis: a populationbased study in Olmsted County, Minnesota. Neurology 1995
Feb;45(2):244-250. (Retrospective; 156 patients)
114. Beck RW, Cleary PA, Trobe JD, et al. The effect of corticosteroids
for acute optic neuritis on the subsequent development of
multiple sclerosis. The Optic Neuritis Study Group. N Engl J Med
1993 Dec 9;329(24):1764-1769. (Multicenter, randomized,
controlled trial; 389 patients)
115.* Granadier RJ. Ophthalmology update for primary practitioners.
Part I. Update on optic neuritis. Dis Mon 2000 Aug;46(8):508532. (Review)
116. No authors listed. Acute methanol poisoning the blind drunk.
West J Med 1981 Aug;135(2):122-128. (Case report)
117. Jacobsen D. Methanol poisoning. In: Harwood-Nuss A, et al, eds.
The Clinical Practice of Emergency Medicine. 3rd ed. Philadelphia:
Lippincott Williams & Wilkins; 2000:1542. (Textbook chapter)
118.* Beatty S, Au Eong KG. Acute occlusion of the retinal arteries:
current concepts and recent advances in diagnosis and
management. J Accid Emerg Med 2000 Sep;17(5):324-329.
(Systematic review)
119. Cooney MJ, Fekrat S, Finkelstein D. Current concepts in the
management of central retinal vein occlusion. Curr Opin
Ophthalmol 1998 Jun;9(3):47-50. (Review)
120.* Bhagat N, Goldberg MF, Gascon P, et al. Central retinal vein
occlusion: review of management. Eur J Ophthalmol 1999
Jul;9(3):165-180. (Review)
121. Branum G, Massey EW, Rice J. Erythrocyte sedimentation rate in
temporal arteritis. South Med J 1987 Dec;80(12):1527-1528.
(Retrospective; 62 patients)
122.* Olitsky SE, Nelson LB. Common ophthalmologic concerns
in infants and children. Pediatr Clin North Am 1998;45(4):
993-1012. (Review)
123. The Pediatric Eye Diseases Investigation Group. A randomized
trial of Atropine versus patching for the treatment of moderate
amblyopia in children. Ophthalmology 2002 Mar;120(3):268-278.
(Multicenter, randomized, controlled trial)
124. Repka MX. Common pediatric neuro-ophthalmologic conditions.
Pediatr Clin North Am 1993;40(4):777-778. (Review)
125. Morales DS, Siatkowski RM, Howard CW, et al. Optic neuritis in
children. J Pediatr Ophthalmol Strabismus 2000 Sep;37(5):254-259.
(Retrospective; 15 patients)
126. Brady KM, Brar AS, Lee AG, et al. Optic neuritis in children:
clinical features and visual outcome. J AAPOS 1999 Apr;3(2):98103. (Retrospective; 25 patients)
79.
Pavesio CE, Meier FM. Systemic disorders associated
with episcleritis and scleritis. Ophthalmology 2001;12(6):
471-478. (Review)
80. McMullen M, Kovarik G, Hodge WG. Use of topical steroid
therapy in the management of nonnecrotizing anterior scleritis.
Can J Ophthalmol 1999 Jun;34(4):217-221. (Phase I/II descriptive
study; 32 patients)
81.* Jabs DA, Mudun A, Dunn JP, et al. Episcleritis and scleritis:
clinical features and treatment results. Am J Ophthalmol 2000
Oct;130(4):469-476. (Retrospective; 134 patients)
82. Akpek EK, Uy HS, Christen W, et al. Severity of episcleritis and
systemic disease association. Ophthalmology 1999 Apr;106(4):729731. (Retrospective; 100 patients)
83. Honig MA, Rapuano CJ. Management of corneal perforation. In:
Krachmer JH, Mannis MJ, Holland E, eds. Cornea. St. Louis:
Mosby; 1997:1817. (Textbook chapter)
84.* Wald ER. Conjunctivitis in infants and children. Pediatr Infect Dis J
1997;16(2 Suppl):S17-S20. (Review)
85. Weiss A. Acute conjunctivitis in childhood. Curr Probl Pediatr
1994;24(1):4-11. (Review)
86.* Bodor FF, Marchant CD, Shurin PA, et al. Bacterial etiology
of conjunctivitis-otitis media syndrome. Pediatrics 1985
Jul;76(1):26-28. (Prospective descriptive series, convenience
sample; 20 episodes)
87. Lueder GT. Neonatal dacryocystitis associated with nasolacrimal
duct cysts. J Pediatr Ophthalmol Strabismus 1995 Mar;32(2):102-106.
(Prospective, case report; 3 patients)
88. Gross RD, Hoffman RO, Lindsay RN. A comparison of
ciprofloxacin and tobramycin in bacterial conjunctivitis in
children. Clin Pediatr (Phila) 1997 Aug;36(8):435-444. (Randomized, controlled trial; 257 children)
89. Wald ER, Serdy C, Guerra N, et al. Short course: oral antibiotic
treatment of bacterial conjunctivitis [Abstract 727]. Program and
abstracts of the American Pediatric Society-The Society for
Pediatric Research Annual Meeting, Washington, DC, May 3 to 6,
1993. Pediatr Res 1993;33:124A.
90. Bodor FF. Systemic antibiotics for treatment of the conjunctivitisotitis media syndrome. Pediatr Infect Dis J 1989 May;8(5):287-290.
(114 episodes)
91. Harrison CJ, Hedrick JA, Block SL, et al. Relation of the outcome
of conjunctivitis and the conjunctivitis-otitis syndrome to
identifiable risk factors and oral antimicrobial therapy. Pediatr
Infect Dis J 1987 Jun;6(6):536-540. (Randomized, controlled trial;
83 patients)
92.* The American Academy of Pediatrics. Chlamydial infections,
gonococcal infections, herpes simplex infections, meningococcal
infections and Kawasaki disease. In: Pickering LK, ed.
2000 Red Book: Report of the Committee on Infectious Diseases,
25th ed. Elk Grove Village, IL: American Academy of
Pediatrics: 1997;208-212, 254-260, 309-313, 360-363, 396-401,
650-656. (Textbook)
93.* Shovlin JP. Orbital infections and inflammations. Curr Opin
Ophthalmol 1998 Oct;9(5):41-48. (Review)
94. Rumelt S, Rubin PA. Potential sources for orbital cellulitis. Int
Ophthalmol Clin 1996 Summer;36(3):207-221. (Review)
95. Phillips PH. The orbit. Ophthalmol Clin North Am 2001
Mar;14(1):109-127, viii. (Systematic review)
96.* Barone SR, Aiuto LT. Periorbital and orbital cellulitis in the
Haemophilus influenzae vaccine era. J Pediatr Ophthalmol Strabismus
1997 Sep;34(5):293-296. (Retrospective; 134 patients)
97. Schwartz GR, Wright SW. Changing bacteriology of periorbital
cellulitis. Ann Emerg Med 1996 Dec;28(6):617-620. (Retrospective;
49 patients)
98.* Powell KR. Orbital and periorbital cellulitis. Pediatr Rev
1995;16(5):163-167. (Review)
99.* Dudin A, Othman A. Acute periorbital swelling: evaluation of
management protocol. Pediatr Emerg Care 1996 Feb;12(1):16-20.
(Evaluation; 34 patients)
100.* No authors listed; American Academy of Pediatrics. Subcommittee on Management of Sinusitis and Committee on Quality
Improvement Clinical practice guideline: management of
sinusitis. Pediatrics 2001 Sep;108(3):798-808. (Clinical practice
guideline; 79 references)
101. Alteveer JG, McCans K. Pediatric eye disorders. In: Harwood-
Emergency Medicine Practice
26
www.empractice.net June 2002
Physician CME Questions
88. Fluorescein staining that reveals a superficial crisscross of mostly vertical lines suggests:
a. herpes infection.
b. corneal abrasion.
c. a foreign body under the upper lid.
d. a corneal ulcer.
81. Blepharitis is:
a. an inflammation of the eyelids.
b. an inflammation of the cornea.
c. an inflammation of the subconjunctival connective
tissue and the blood vessels that course between
the sclera and conjunctiva.
d. an inflammation of the iris and ciliary body (also
called iritis or iridocyclitis).
e. an inflammation of the choroid.
89. The slit lamp examination:
a. should be performed in all patients who present
with ocular complaints.
b. can be reserved for patients in whom iritis or
small foreign bodies are suspected.
c. can substitute for measuring a patients
visual acuity.
d. should not be performed in children.
82. Keratitis is:
a. an inflammation of the eyelids.
b. an inflammation of the cornea.
c. an inflammation of the subconjunctival connective
tissue and the blood vessels that course between
the sclera and conjunctiva.
d. an inflammation of the iris and ciliary body (also
called iritis or iridocyclitis).
e. an inflammation of the choroid.
90. All of the following about bacterial conjunctivitis are
true except:
a. It can cause deep orbital pain and vision loss.
b. Patients report a rapid onset of irritation, redness,
and a purulent discharge.
c. It is generally a benign and self-limited condition.
d. Broad-spectrum topical antibiotics can shorten the
duration of illness.
83. Episcleritis is:
a. an inflammation of the eyelids.
b. an inflammation of the cornea.
c. an inflammation of the subconjunctival connective
tissue and the blood vessels that course between
the sclera and conjunctiva.
d. an inflammation of the iris and ciliary body (also
called iritis or iridocyclitis).
e. an inflammation of the choroid.
91. Treatment of blepharitis involves:
a. a daily regimen of lid hygiene (warm compresses,
massage, cleaning the lids).
b. erythromycin ophthalmic ointment when staphylococcal blepharitis is suspected.
c. a one- to three-week course of topical steroids for
resistant and severe inflammation.
d. counseling the patient about the likelihood of
recurrent flare-ups and the need for a regular
regimen of lid hygiene.
e. all of the above.
84. Anterior uveitis is:
a. an inflammation of the eyelids.
b. an inflammation of the cornea.
c. an inflammation of the subconjunctival connective
tissue and the blood vessels that course between
the sclera and conjunctiva.
d. an inflammation of the iris and ciliary body (also
called iritis or iridocyclitis).
e. an inflammation of the choroid.
92. Which of the following concerning eye patches for
corneal abrasions is true?
a. They should only be used in contact lens wearers.
b. They should be used for all corneal abrasions.
c. They should only be used in patients with smallto moderate-sized abrasions.
d. A recent meta-analysis has shown that they
do not promote healing, nor do they help to
control pain.
85. Posterior uveitis is:
a. an inflammation of the eyelids.
b. an inflammation of the cornea.
c. an inflammation of the subconjunctival connective
tissue and the blood vessels that course between
the sclera and conjunctiva.
d. an inflammation of the iris and ciliary body (also
called iritis or iridocyclitis).
e. an inflammation of the choroid.
93. Which of the following conditions can threaten vision
and should be referred to an ophthalmologist?
a. Corneal ulcers
b. Acute anterior uveitis
c. Ocular herpes infections
d. Acute angle-closure glaucoma
e. All of the above
86. Visual acuity:
a. is the vital sign of the eye.
b. cannot be assessed in children.
c. should be measured in both eyes at once.
d. cannot be measured in patients without glasses.
94. Which of the following may present as a swollen eye?
a. Bacterial or fungal infections
b. Inflammatory conditions such as idiopathic orbital
inflammatory syndrome or thyroid-related
ophthalmopathy
c. Tumors
d. Periorbital cellulitis and orbital cellulitis
e. All of the above
87. Normal intraocular pressure:
a. is less than 12 mmHg.
b. ranges between 12 and 21 mmHg.
c. ranges between 21 and 30 mmHg.
d. is greater than 30 mmHg.
June 2002 www.empractice.net
27
Emergency Medicine Practice
Physician CME Information
95. Acute, non-traumatic vision loss in adults under the
age of 50 is most likely due to:
a. optic neuritis.
b. temporal arteritis.
c. central retinal artery occlusion.
d. glaucoma.
This CME enduring material is sponsored by Mount Sinai School of Medicine
and has been planned and implemented in accordance with the Essentials
and Standards of the Accreditation Council for Continuing Medical
Education. Credit may be obtained by reading each issue and completing
the printed post-tests administered in December and June or online singleissue post-tests administered at www.empractice.net.
Target Audience: This enduring material is designed for emergency
medicine physicians.
Needs Assessment: The need for this educational activity was
determined by a survey of medical staff, including the editorial board
of this publication; review of morbidity and mortality data from the
CDC, AHA, NCHS, and ACEP; and evaluation of prior activities for
emergency physicians.
Date of Original Release: This issue of Emergency Medicine Practice was
published June 1, 2002. This activity is eligible for CME credit through
June 1, 2005. The latest review of this material was May 7, 2002.
Discussion of Investigational Information: As part of the newsletter, faculty
may be presenting investigational information about pharmaceutical
products that is outside Food and Drug Administration approved labeling.
Information presented as part of this activity is intended solely as
continuing medical education and is not intended to promote off-label
use of any pharmaceutical product. Disclosure of Off-Label Usage: Off-label
uses mentioned in this article include topical nonsteroidal medications to
treat allergic conjunctivitis, pinguecula, pterygium, and corneal abrasions.
Other off-label uses include oral antivirals other than acyclovir to treat
herpes infections of the eye and the BID use of topical quinolones to treat
bacterial conjunctivitis. (See text.)
Faculty Disclosure: In compliance with all ACCME Essentials, Standards, and
Guidelines, all faculty for this CME activity were asked to complete a full
disclosure statement. The information received is as follows: Dr. Alteveer,
Dr. McCans, Dr. Hemphill, Dr. Knoop, and Dr. Sacchetti report no significant
financial interest or other relationship with the manufacturer(s) of any
commercial product(s) discussed in this educational presentation.
Accreditation: Mount Sinai School of Medicine is accredited by the
Accreditation Council for Continuing Medical Education to sponsor
continuing medical education for physicians.
Credit Designation: Mount Sinai School of Medicine designates this
educational activity for up to 4 hours of Category 1 credit toward the
AMA Physicians Recognition Award. Each physician should claim only
those hours of credit actually spent in the educational activity.
Emergency Medicine Practice is approved by the American College
of Emergency Physicians for 48 hours of ACEP Category 1 credit (per
annual subscription).
Earning Credit: Two Convenient Methods
Print Subscription Semester Program: Physicians with current and
valid licenses in the United States who read all CME articles during
each Emergency Medicine Practice six-month testing period, complete
the post-test and the CME Evaluation Form distributed with the
December and June issues, and return it according to the published
instructions are eligible for up to 4 hours of Category 1 credit toward
the AMA Physicians Recognition Award (PRA) for each issue. You must
complete both the post-test and CME Evaluation Form to receive
credit. Results will be kept confidential. CME certificates will be
delivered to each participant scoring higher than 70%.
Online Single-Issue Program: Physicians with current and valid
licenses in the United States who read this Emergency Medicine Practice
CME article and complete the online post-test and CME Evaluation
Form at www.empractice.net are eligible for up to 4 hours of Category
1 credit toward the AMA Physicians Recognition Award (PRA). You
must complete both the post-test and CME Evaluation Form to receive
credit. Results will be kept confidential. CME certificates may be printed
directly from the Web site to each participant scoring higher than 70%.
96. Acute, non-traumatic vision loss in patients over the
age of 60 is most likely due to:
a. vascular causes.
b. infections.
c. optic neuritis.
d. acute methanol intoxication.
This test concludes the January through June 2002 semester
testing period of Emergency Medicine Practice. The answer
form for this semester and a return envelope have been
included with this issue. All paid subscribers are eligible to
take this test. Please refer to the instructions printed on the
answer form.
Monthly online CME testing is now available
at no extra charge at www.empractice.net.
Class Of Evidence Definitions
Each action in the clinical pathways section of Emergency Medicine Practice
receives an alpha-numerical score based on the following definitions.
Class I
Always acceptable, safe
Definitely useful
Proven in both efficacy and
effectiveness
Level of Evidence:
One or more large prospective
studies are present (with
rare exceptions)
High-quality meta-analyses
Study results consistently
positive and compelling
Class II
Safe, acceptable
Probably useful
Level of Evidence:
Generally higher levels
of evidence
Non-randomized or retrospective studies: historic, cohort, or
case-control studies
Less robust RCTs
Results consistently positive
Class III
May be acceptable
Possibly useful
Considered optional or
alternative treatments
Level of Evidence:
Generally lower or intermediate
levels of evidence
Case series, animal studies,
consensus panels
Occasionally positive results
Indeterminate
Continuing area of research
No recommendations until
further research
Level of Evidence:
Evidence not available
Higher studies in progress
Results inconsistent,
contradictory
Results not compelling
Significantly modified from: The
Emergency Cardiovascular Care
Committees of the American Heart
Association and representatives
from the resuscitation councils of
ILCOR: How to Develop EvidenceBased Guidelines for Emergency
Cardiac Care: Quality of Evidence
and Classes of Recommendations;
also: Anonymous. Guidelines for
cardiopulmonary resuscitation and
emergency cardiac care. Emergency
Cardiac Care Committee and
Subcommittees, American Heart
Association. Part IX. Ensuring
effectiveness of community-wide
emergency cardiac care. JAMA
1992;268(16):2289-2295.
Emergency Medicine Practice is not affiliated with any
pharmaceutical firm or medical device manufacturer.
Publisher: Robert Williford. Executive Editor: Heidi Frost.
Direct all editorial or subscription-related questions to EB Practice, LLC: 1-800-249-5770 Fax: 1-770-500-1316 Non-U.S. subscribers, call: 1-678-366-7933
EB Practice, LLC 305 Windlake Court Alpharetta, GA 30022
E-mail: emp@empractice.net Web Site: http://www.empractice.net
Emergency Medicine Practice (ISSN 1524-1971) is published monthly (12 times per year) by EB Practice, LLC, 305 Windlake Court, Alpharetta, GA 30022. Opinions expressed are not necessarily
those of this publication. Mention of products or services does not constitute endorsement. This publication is intended as a general guide and is intended to supplement, rather than
substitute, professional judgment. It covers a highly technical and complex subject and should not be used for making specific medical decisions. The materials contained herein are not
intended to establish policy, procedure, or standard of care. Emergency Medicine Practice is a trademark of EB Practice, LLC. Copyright 2002 EB Practice, LLC. All rights reserved. No part of this
publication may be reproduced in any format without written consent of EB Practice, LLC. Subscription price: $249, U.S. funds. (Call for international shipping prices.)
Emergency Medicine Practice
28
www.empractice.net June 2002
Potrebbero piacerti anche
- Evaluation of The Painful EyeDocumento9 pagineEvaluation of The Painful EyeMuthia Farah AshmaNessuna valutazione finora
- State-of-the-art Treatment of Coronary Heart DiseaseDa EverandState-of-the-art Treatment of Coronary Heart DiseaseNessuna valutazione finora
- OSCE - Family MedicineDocumento1 paginaOSCE - Family MedicineDr-Sulaiman Bani Abdel-rahman100% (1)
- Eye Diseases Manual EngDocumento73 pagineEye Diseases Manual EngAbdul SohrabNessuna valutazione finora
- A Simple Guide to Pick Disease, Diagnosis, Treatment and Related ConditionsDa EverandA Simple Guide to Pick Disease, Diagnosis, Treatment and Related ConditionsValutazione: 5 su 5 stelle5/5 (1)
- Syncope - Approach To The Patient Dynamed 2020 PDFDocumento76 pagineSyncope - Approach To The Patient Dynamed 2020 PDFHeriberto Moreno HernandezNessuna valutazione finora
- Ventricular Septal Defect, A Simple Guide To The Condition, Treatment And Related ConditionsDa EverandVentricular Septal Defect, A Simple Guide To The Condition, Treatment And Related ConditionsNessuna valutazione finora
- Nbme 7 Block 1 AnswersDocumento20 pagineNbme 7 Block 1 AnswersVictoria BlentiranNessuna valutazione finora
- General Rules of Abdomenal ExaminationDocumento22 pagineGeneral Rules of Abdomenal ExaminationSamuel Sebastian SirapanjiNessuna valutazione finora
- Personal Statement - FinalDocumento2 paginePersonal Statement - Finalapi-383932502Nessuna valutazione finora
- Intern Survival Guide (UIC)Documento51 pagineIntern Survival Guide (UIC)medstick100% (1)
- Adya Ebook On Water and MineralsDocumento80 pagineAdya Ebook On Water and Mineralsapi-261829418Nessuna valutazione finora
- High Yield SurgeryDocumento77 pagineHigh Yield SurgeryDr.2020Nessuna valutazione finora
- Using The ACLS Primary Survey For A Patient in Respiratory ArrestDocumento34 pagineUsing The ACLS Primary Survey For A Patient in Respiratory Arrest강기연100% (1)
- Pediatrics - Neonatal Jaundice PDFDocumento2 paginePediatrics - Neonatal Jaundice PDFJasmine KangNessuna valutazione finora
- Unit Two Basic Examination of The Eye: 2.1. History TakingDocumento12 pagineUnit Two Basic Examination of The Eye: 2.1. History TakingiuytrerNessuna valutazione finora
- ONDOC Format & Guide To Oral PresentationsDocumento10 pagineONDOC Format & Guide To Oral PresentationsZainNessuna valutazione finora
- PCM Guidebook For History Taking and Physical Exam, Revised Final, 9-20-17Documento82 paginePCM Guidebook For History Taking and Physical Exam, Revised Final, 9-20-17anon_925247980Nessuna valutazione finora
- Personal Notes Excpetional StuffDocumento352 paginePersonal Notes Excpetional StuffYagyeshNessuna valutazione finora
- Megs History PhysicalDocumento1 paginaMegs History Physicalrmelendez001Nessuna valutazione finora
- Mnemonics For CsDocumento8 pagineMnemonics For CsManisanthosh KumarNessuna valutazione finora
- Synapses: and Their FunctionsDocumento14 pagineSynapses: and Their FunctionsPratibha MathivananNessuna valutazione finora
- Optic NeuritisDocumento31 pagineOptic NeuritisUsman ImtiazNessuna valutazione finora
- Facing Neu Ent Fearlessly: Ro AssessmDocumento7 pagineFacing Neu Ent Fearlessly: Ro AssessmokipashaNessuna valutazione finora
- Diagnostic Strategy in RheumatologyDocumento25 pagineDiagnostic Strategy in Rheumatologyaa031987Nessuna valutazione finora
- Parathyroid Disease Lecture SlidesDocumento50 pagineParathyroid Disease Lecture SlidesMaxwell PalSingh100% (1)
- Weakness A Systematic Approach To Acute Non-Traumatic NDocumento28 pagineWeakness A Systematic Approach To Acute Non-Traumatic Ncalmira3653Nessuna valutazione finora
- USMLEasy Psych Case01Documento10 pagineUSMLEasy Psych Case01Tanzeel Ur RehmanNessuna valutazione finora
- PAS 606 - TEXT HP Handbook PDFDocumento65 paginePAS 606 - TEXT HP Handbook PDFNick Malizia100% (1)
- Preventive Care Checklist Form ExplanationsDocumento3 paginePreventive Care Checklist Form ExplanationsKak KfgaNessuna valutazione finora
- PCDDocumento15 paginePCDana100% (1)
- Psychiatry: Ome + UworldDocumento92 paginePsychiatry: Ome + UworldIqra JabeenNessuna valutazione finora
- Word AssociationDocumento27 pagineWord AssociationMilan Kolovrat100% (1)
- Introduction To Internal Medicine - PPTMDocumento30 pagineIntroduction To Internal Medicine - PPTMAddyNessuna valutazione finora
- Chest Radiology For Dummies PDFDocumento6 pagineChest Radiology For Dummies PDF0395Nessuna valutazione finora
- IM Essentials Text Jan 5, 2015 1938921097 TheDocumento478 pagineIM Essentials Text Jan 5, 2015 1938921097 TheChu Thành HưngNessuna valutazione finora
- Hopkins Ortho Survival GuideDocumento37 pagineHopkins Ortho Survival GuideJayson Mac YowellNessuna valutazione finora
- Medex Exam Writeups PageDocumento9 pagineMedex Exam Writeups Pageaahmad87Nessuna valutazione finora
- Neurology Shelf Exam Review - Part 2.newDocumento14 pagineNeurology Shelf Exam Review - Part 2.newyogurtNessuna valutazione finora
- Mnemonics For CsDocumento7 pagineMnemonics For CsTony Menias100% (1)
- Child Neurology: Dr. Endang Mutiawati SP.SDocumento28 pagineChild Neurology: Dr. Endang Mutiawati SP.SacutdevyNessuna valutazione finora
- The Detailed Neurologic Examination in Adults - UpToDate PDFDocumento29 pagineThe Detailed Neurologic Examination in Adults - UpToDate PDFMiguel GarciaNessuna valutazione finora
- Amc Limb FractureDocumento10 pagineAmc Limb Fractureffaa100% (1)
- Step 1 REVIEWDocumento140 pagineStep 1 REVIEWRima HajjarNessuna valutazione finora
- 03-Spinal Cord Phys & AnatDocumento9 pagine03-Spinal Cord Phys & AnatAzwar Arsyad S SiNessuna valutazione finora
- Pediatrics 04: 8-Year-Old Male Well-Child Check: Learning ObjectivesDocumento8 paginePediatrics 04: 8-Year-Old Male Well-Child Check: Learning ObjectivesJeffNessuna valutazione finora
- Step 1 Physiology Flash CardsDocumento22 pagineStep 1 Physiology Flash CardsbobiomeNessuna valutazione finora
- Fluids&Lytes PediatricDocumento33 pagineFluids&Lytes Pediatricnugraha_esaNessuna valutazione finora
- Typhon Cases 2Documento7 pagineTyphon Cases 2api-483865455Nessuna valutazione finora
- Mock Record B-1-2-Well Child VisitsDocumento4 pagineMock Record B-1-2-Well Child VisitsaelteeNessuna valutazione finora
- AECP-Essentials of Ophthalmology PDFDocumento235 pagineAECP-Essentials of Ophthalmology PDFsandeepNessuna valutazione finora
- Practice Exam: Https://learnuw - Wisc.edu/ (Requires Log In) 2. Practice OSCE Scenarios (Below)Documento20 paginePractice Exam: Https://learnuw - Wisc.edu/ (Requires Log In) 2. Practice OSCE Scenarios (Below)chioNessuna valutazione finora
- The Yale Way - New Patient PresentationsDocumento9 pagineThe Yale Way - New Patient PresentationsAndrew McGowanNessuna valutazione finora
- Excited Delirium Task ForceDocumento22 pagineExcited Delirium Task ForceFrances CorreaNessuna valutazione finora
- Disease Activity Scoring in RheumatologyDocumento28 pagineDisease Activity Scoring in RheumatologyLeo FluxNessuna valutazione finora
- Pediatrics - Lower AirwayDocumento3 paginePediatrics - Lower AirwayJasmine KangNessuna valutazione finora
- 100 Commonly Tested Facts For MRCP Part 1Documento5 pagine100 Commonly Tested Facts For MRCP Part 1Khalid AbdelazizNessuna valutazione finora
- The Art of Presenting A Patient ByFalconDocumento15 pagineThe Art of Presenting A Patient ByFalconsapereaude11Nessuna valutazione finora
- Obat NarcolepsyDocumento10 pagineObat NarcolepsyBimantoro SaputroNessuna valutazione finora
- 1741 7015 11 171Documento6 pagine1741 7015 11 171Bimantoro SaputroNessuna valutazione finora
- 5Documento20 pagine5Bimantoro SaputroNessuna valutazione finora
- Viruses 04 03851Documento8 pagineViruses 04 03851Bimantoro SaputroNessuna valutazione finora
- BPJ59 GlaucomaDocumento10 pagineBPJ59 GlaucomaBimantoro SaputroNessuna valutazione finora
- Viruses 04 03851Documento8 pagineViruses 04 03851Bimantoro SaputroNessuna valutazione finora
- Narcolepsy: Autoimmunity or Secondary To Infection?: Adriano Fontana, Heidemarie Gast, and Thomas BirchlerDocumento9 pagineNarcolepsy: Autoimmunity or Secondary To Infection?: Adriano Fontana, Heidemarie Gast, and Thomas BirchlerBimantoro SaputroNessuna valutazione finora
- AngiographyDocumento11 pagineAngiographyBimantoro SaputroNessuna valutazione finora
- AdalimumabDocumento11 pagineAdalimumabBimantoro SaputroNessuna valutazione finora
- Anatomi Dan FisiologiDocumento60 pagineAnatomi Dan FisiologiBimantoro SaputroNessuna valutazione finora
- Mri GeneralDocumento48 pagineMri GeneralBimantoro SaputroNessuna valutazione finora
- A Guide To Coronary Angiogram and Angioplasties-Stents - Online Version EnglishDocumento12 pagineA Guide To Coronary Angiogram and Angioplasties-Stents - Online Version EnglishBimantoro SaputroNessuna valutazione finora
- Atlas of Contrast Enhanced AngiographyDocumento124 pagineAtlas of Contrast Enhanced AngiographyCardinosum100% (1)
- Brain 2010 Fontana 1300 11Documento12 pagineBrain 2010 Fontana 1300 11Bimantoro SaputroNessuna valutazione finora
- Angio CTDocumento8 pagineAngio CTBimantoro SaputroNessuna valutazione finora
- Review of Policies Programmes and GuidelinesDocumento46 pagineReview of Policies Programmes and GuidelinesBimantoro SaputroNessuna valutazione finora
- Angiogram Angioplasty and StentsDocumento8 pagineAngiogram Angioplasty and StentsBimantoro SaputroNessuna valutazione finora
- Peripartum and Amniotic Fluid EmbolismDocumento16 paginePeripartum and Amniotic Fluid EmbolismBimantoro SaputroNessuna valutazione finora
- M PL E: Hand-Foot-and-Mouth DiseaseDocumento2 pagineM PL E: Hand-Foot-and-Mouth DiseaseBimantoro SaputroNessuna valutazione finora
- Medical and Surgical Management of PriapismDocumento6 pagineMedical and Surgical Management of PriapismBimantoro SaputroNessuna valutazione finora
- Amniotic Fluid Embolism 2012Documento48 pagineAmniotic Fluid Embolism 2012Bimantoro SaputroNessuna valutazione finora
- Hand Foot MouthDocumento2 pagineHand Foot MouthBimantoro SaputroNessuna valutazione finora
- Jurnal JIA HighlightDocumento9 pagineJurnal JIA HighlightBimantoro SaputroNessuna valutazione finora
- Poster EWMA 2011-Treatment of Venous Ulcers (Ulcus Cruris Venosum)Documento1 paginaPoster EWMA 2011-Treatment of Venous Ulcers (Ulcus Cruris Venosum)Bimantoro SaputroNessuna valutazione finora
- 2011 CAP in ChildrenDocumento52 pagine2011 CAP in Childrenbebekdd22Nessuna valutazione finora
- Pneumonia The Forgotten Killer of ChildrenDocumento44 paginePneumonia The Forgotten Killer of ChildrenBimantoro SaputroNessuna valutazione finora
- 10 Testicular CancerDocumento56 pagine10 Testicular CancerRachhpal SinghNessuna valutazione finora
- Testicular CancerDocumento50 pagineTesticular CancerMuhammad Ikhwan ZainNessuna valutazione finora
- CME Bacterial TropicalDocumento20 pagineCME Bacterial Tropicalzul090Nessuna valutazione finora
- Anatomy of Angle of Anterior ChamberDocumento67 pagineAnatomy of Angle of Anterior ChamberRahnaNessuna valutazione finora
- Dialog General Assesment Vena Dan DyahDocumento4 pagineDialog General Assesment Vena Dan DyahVena HarminNessuna valutazione finora
- Standardization of Uveitis Nomenclature For Reporting Clinical D 2005Documento8 pagineStandardization of Uveitis Nomenclature For Reporting Clinical D 2005Stephanie PfengNessuna valutazione finora
- Eyes and Ears AssessmentDocumento20 pagineEyes and Ears AssessmentMonica JoyceNessuna valutazione finora
- gt0912 F4 LarocheDocumento3 paginegt0912 F4 LarocheMichael CraneNessuna valutazione finora
- BNS 200 Drugs and The EyeDocumento36 pagineBNS 200 Drugs and The EyeAnthony MoepengNessuna valutazione finora
- Anatomy of Anterior Chamber Angle and Physiology ofDocumento24 pagineAnatomy of Anterior Chamber Angle and Physiology ofAnumeha Jindal100% (1)
- The Tearing Patient: Diagnosis and Management: Ophthalmic PearlsDocumento3 pagineThe Tearing Patient: Diagnosis and Management: Ophthalmic PearlsAnonymous otk8ohj9Nessuna valutazione finora
- Anatomy & Physiology of The EyeDocumento37 pagineAnatomy & Physiology of The EyeRajakannan60% (5)
- 2013 Meeting Guide FINAL WebDocumento168 pagine2013 Meeting Guide FINAL Webmuhammad sharafNessuna valutazione finora
- Soal Infeksi Immunology 2019Documento7 pagineSoal Infeksi Immunology 2019Reinhard TuerahNessuna valutazione finora
- Florida Spots in Dogs and Cats. A Clinical Study in São PauloDocumento2 pagineFlorida Spots in Dogs and Cats. A Clinical Study in São PauloLuciana DieguesNessuna valutazione finora
- Chalazion PDFDocumento14 pagineChalazion PDFDaniel MehirutNessuna valutazione finora
- Sensory Function General ObservationsDocumento3 pagineSensory Function General ObservationsLeila Camille De SagunNessuna valutazione finora
- Glaucoma Part II - Dr. JusufDocumento73 pagineGlaucoma Part II - Dr. JusufChristine Andriana AmbaritaNessuna valutazione finora
- State and Federal Compliant Employee Handbook 03172022Documento32 pagineState and Federal Compliant Employee Handbook 03172022api-226085761Nessuna valutazione finora
- Practical Ophthalmology - Web - 2Documento104 paginePractical Ophthalmology - Web - 2Yellyasta Siusiu ImranNessuna valutazione finora
- Vision-SanDiego (1) - 231013 - 141100Documento10 pagineVision-SanDiego (1) - 231013 - 141100fernyz2886Nessuna valutazione finora
- Eye Pathology: Dr. Jusuf FantoniDocumento8 pagineEye Pathology: Dr. Jusuf Fantonitutor tujuhNessuna valutazione finora
- Retinal Diseases - 5Documento2 pagineRetinal Diseases - 5AkicaNessuna valutazione finora
- Optics, Refraction & Instruments: Instructions For CandidatesDocumento16 pagineOptics, Refraction & Instruments: Instructions For CandidatesAna-Maria CeausescuNessuna valutazione finora
- Ocular Complications of Diabetes MellitusDocumento18 pagineOcular Complications of Diabetes MellitusEllieNessuna valutazione finora
- Healthy Eyes - 11 March 2018Documento8 pagineHealthy Eyes - 11 March 2018Irfan AksariNessuna valutazione finora
- Block M2 EYE Distribution by MMCDocumento3 pagineBlock M2 EYE Distribution by MMCF ParikhNessuna valutazione finora
- GlaucomaDocumento25 pagineGlaucomaChris Paguio100% (2)
- Fundus Autofluorescence and Optical Coherence TomoDocumento4 pagineFundus Autofluorescence and Optical Coherence TomoAndi Tiara S. AdamNessuna valutazione finora
- Perceptual DisturbancesDocumento7 paginePerceptual DisturbancesVin SageNessuna valutazione finora
- Uveitis & Retinal DetachmentDocumento8 pagineUveitis & Retinal Detachmentjumi26Nessuna valutazione finora
- A Clinical Study To Correlate Visual Field Defects With Optic Disc Changes in 100 Patients With Primary Open Angle Glaucoma in A Tertiary Eye Care HospitalDocumento3 pagineA Clinical Study To Correlate Visual Field Defects With Optic Disc Changes in 100 Patients With Primary Open Angle Glaucoma in A Tertiary Eye Care HospitalIOSRjournalNessuna valutazione finora
- GlaucomaDocumento53 pagineGlaucomaLyNessuna valutazione finora
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDDa EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDValutazione: 5 su 5 stelle5/5 (2)
- The Age of Magical Overthinking: Notes on Modern IrrationalityDa EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityValutazione: 4 su 5 stelle4/5 (28)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionDa EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionValutazione: 4 su 5 stelle4/5 (404)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeDa EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeValutazione: 2 su 5 stelle2/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedDa EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedValutazione: 5 su 5 stelle5/5 (81)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaDa EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Gut: the new and revised Sunday Times bestsellerDa EverandGut: the new and revised Sunday Times bestsellerValutazione: 4 su 5 stelle4/5 (393)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsDa EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsValutazione: 5 su 5 stelle5/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisDa EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisValutazione: 4.5 su 5 stelle4.5/5 (42)
- The Obesity Code: Unlocking the Secrets of Weight LossDa EverandThe Obesity Code: Unlocking the Secrets of Weight LossValutazione: 4 su 5 stelle4/5 (6)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsDa EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNessuna valutazione finora
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsDa EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsValutazione: 3.5 su 5 stelle3.5/5 (3)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningDa EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningValutazione: 4 su 5 stelle4/5 (3)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Da EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Nessuna valutazione finora
- Why We Die: The New Science of Aging and the Quest for ImmortalityDa EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityValutazione: 4 su 5 stelle4/5 (4)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisDa EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisValutazione: 3.5 su 5 stelle3.5/5 (2)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryDa EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryValutazione: 4 su 5 stelle4/5 (44)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeDa EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeValutazione: 4.5 su 5 stelle4.5/5 (253)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Da EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Valutazione: 4.5 su 5 stelle4.5/5 (110)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisDa EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisValutazione: 4 su 5 stelle4/5 (1)
- The Marshmallow Test: Mastering Self-ControlDa EverandThe Marshmallow Test: Mastering Self-ControlValutazione: 4.5 su 5 stelle4.5/5 (58)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsDa EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsValutazione: 4.5 su 5 stelle4.5/5 (170)
- Dark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingDa EverandDark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingValutazione: 4 su 5 stelle4/5 (1138)