Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Pompholyx
Caricato da
Suci Dika UtariTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Pompholyx
Caricato da
Suci Dika UtariCopyright:
Formati disponibili
Research Article
www.enlivenarchive.org
Enliven: Pediatrics and Neonatal Biology
Dyshidrotic Eczema
Alexander K. C. Leung1*, Benjamin Barankin2, and Kam Lun Hon3
Clinical Professor of Pediatrics, University of Calgary, Pediatric Consultant, Alberta Childrens Hospital
Medical Director and Founder, Toronto Dermatology Centre
Professor of Pediatrics, Chinese University of Hong Kong
Corresponding author: Alexander K. C. Leung, MBBS, FRCPC, FRCP
(UK & Irel), FRCPCH, FAAP, Clinical Professor of Pediatrics, University
of Calgary, Pediatric Consultant, Alberta Childrens Hospital, Canada, Tel:
(403) 230-3322; Fax: (403) 230-3322; E-mail: aleung@ucalgary.ca
*
Received Date: 14th August 2014
Accepted Date: 10th September 2014
Published Date: 16th September 2014
Citation: Leung AK, Barankin B, Hon KL (2014) Dyshidrotic Eczema.
Enliven: Pediatr Neonatol Biol 1(1): 002.
Copyright:@ 2014 Dr. Alexander K. C. Leung. This is an Open Access
article published and distributed under the terms of the Creative Commons
Attribution License, which permits unrestricted use, distribution and
reproduction in any medium, provided the original author and source are
credited.
Abstract
Dyshidrotic eczema, also known as dyshidrotic dermatitis or pompholyx, is characterized by pruritic, tense, deep-seated vesicles mainly on the
palms and lateral surfaces of the fingers. In the chronic phase, scaling, desquamation, fissuring, and, sometimes, lichenification may be seen. The
peak age of onset is between 20 and 30 years of age. The sex incidence is approximately equal. Most cases are idiopathic. Predisposing factors
include atopy, contact allergens, contact irritants, dermatophyte infection, allergy to ingested metal, hyperhidrosis, prolonged use of protective gloves,
intravenous immunoglobulin, psychological stress, and smoking. Although the disease is benign, it tends to run a chronic and relapsing course.
Successful treatment requires a systemic multipronged approach that consists of avoidance of triggering factors, optimal skin care, pharmacotherapy
during acute exacerbations, and education of patients/caregivers. Ultrapotent topical corticosteroids are the mainstay of pharmacotherapy.
Keywords
Dyshidrotic eczema; Dyshidrotic dermatitis; Pompholyx; Pruritic vesicles; Palms; Fingers; Relapsing; Corticosteroids
Introduction
Dyshidrotic eczema, also known as dyshidrotic dermatitis or pompholyx,
is characterized by pruritic, tense, deep-seated vesicles mainly on the
palms and lateral surfaces of the fingers [1]. The term dyshidrosis (Greek,
hidrosis meaning sweat) was coined by Fox in 1873 to describe a blistering
disease of the palms and soles, presumably due to a disorder of the sweat
glands [2]. The term dyshidrosis is a misnomer as it is now recognized
that the condition has nothing to do with dysfunction of the sweat glands.
Enliven Archive | www.enlivenarchive.org
Epidemiology
The prevalence of hand dermatitis varies from 2 to 8.9% of the general
population [3]. Dyshidrotic eczema accounts for 5 to 20% of all cases of
hand dermatitis [4,5]. In one population study, the one-year prevalence
of dyshidrotic eczema was estimated to be 0.5% [6]. Although dyshidrotic
eczema occurs worldwide, it is less common among Asians [7,8]. The
condition is more common in hot weather [9]. The peak age of onset
is between 20 and 30 years of age [3]. Onset before 10 years of
age is unusual [5]. The sex incidence is approximately equal [5].
2014 | Volume 1 | Issue 1
Etiology and Pathogenesis
The exact etiology is not known. Most cases are idiopathic. Factors
that may predispose to the development of dyshidrotic eczema in a
susceptible individual include atopy, contact allergens, contact irritants,
dermatophyte infection, allergy to ingested metal (in particular, nickel and
cobalt), hyperhidrosis, prolonged use of protective gloves, intravenous
immunoglobulin, psychological stress, and smoking [4,8,10-12]. Most cases
are sporadic. Rarely, an autosomal dominant mode of inheritance has been
described [5]. A gene locus on chromosome 18q22.1-18q22.3 was identified
in a large Chinese family with 14 affected individuals through 4 generations [5].
Histopathology
In the acute phase, histologic features include intraepidermal spongiosis
with vesicle formation and a superficial perivascular inflammatory infiltrate
composed mainly of lymphocytes and histiocytes [3,4,11,12]. In the
more chronic phase, there are multiple foci of parakeratosis, acanthosis,
irregular epidermal hyperplasia with minimal or absent spongiosis [3,4,12].
The epidermis is thick and the overlying horny layer is even thicker [8].
Clinical Manifestations
Clinically, acute dyshidrotic eczema presents with a sudden outbreak of
deep-seated tapioca-like vesicles and, less commonly, bullae that affect
primarily the palms and lateral surfaces of the fingers [1,9]. The eruption
may also occur on the soles of the feet. In approximately 80% of cases,
only the hands are affected [4]. The eruption is usually symmetrical and
pruritic [1]. Some patients experience pain and/or a burning sensation
[1]. In the chronic phase, scaling, desquamation, fissuring, and,
sometimes, lichenification may be seen [1]. The condition is typically
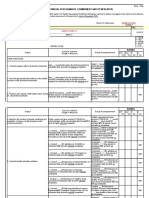
recurrent and both the acute and chronic phases can coexist (Figure 1).
Diagnosis and Differential Diagnosis
The diagnosis is mainly clinical based on a detailed history and the appearance
of the rash. Differential diagnosis includes allergic contact dermatitis (can be
determined by patch testing to various contactants), irritant contact dermatitis
(typically over-washing, using harsh soaps and/or insufficient moisturizing) ,
and atopic hand dermatitis (typically a family or personal history of eczema,
asthma, and/or hay fever) most commonly; much less commonly, the differential
would include epidermolysis bullosa simplex, bullous impetigo, herpes
infection, id reaction, linear IgA disease, dyshidrotic tinea, dyshidrosiform
pemphigoid, pemphigus vulgaris, fixed drug eruption, acropustulosis
of infancy, hand-foot-mouth disease, pustular psoriasis, palmoplantar
pustulosis, secondary syphilis, and acrodermatitis enteropathica [8,12].
Complications
Dyshidrotic eczema has a significant negative impact on the
quality of life due to the severe pruritus [5,9]. Secondary bacterial
infection, especially with Staphylococcus aureus, is not uncommon
[4]. Nail dystrophy may result if the nail matrix is affected [4].
Prognosis
Although the disease is benign, it tends to run a chronic and relapsing
course [3]. The condition tends to be less severe and recurs less often with
age [4]. Most patients eventually outgrow the condition [4].
Management
Dyshidrotic eczema is often difficult to treat, possibly because of the thick
epidermis with a compact stratum corneum and richness of the sweat glands
of the affected skin. Successful treatment requires a systemic multipronged
approach that consists of avoidance of triggering factors, optimal skin care,
pharmacotherapy during acute exacerbations, and education of patients/
caregivers.
Soaps and detergents should be avoided as much as possible [13]. The hands
should be washed with lukewarm (not hot) water and soap free cleansers.
Emotional stress often exacerbates the skin lesions of atopic dermatitis.
If avoidance is not possible, coping mechanisms should be tried [13].
Figure 1: A 3-year-old girl with dyshidrotic eczema presenting with
vesicles on the palms and scaling patches with crusts and fissures on
the fingers.
Enliven Archive | www.enlivenarchive.org
Hydration of the skin helps to improve the dryness and pruritus and restore
the disturbed skins barrier function. As such, hydration of the skin is of
paramount importance both in the prevention and management of dyshidrotic
eczema. A moisturizer or emollient should be applied as soon as possible after
hand-washing to prevent evaporation of water and to keep the skin soft and
flexible. In general, ointments are most effective but messy; creams are often
better tolerated. The type of moisturizer or emollient should be tailored to the
individual skin conditions as well as the childs needs and preferences [13].
2014 | Volume 1 | Issue 1
Ultrapotent topical corticosteroids are the mainstay of therapy. Topical
corticosteroids should not be applied more than twice a day; frequent
use does not improve efficacy and increase the risk of side effects [14].
Topical immunomodulators such as tacrolimus and pimecrolimus are not
as fast or effective as ultrapotent topical corticosteroids in the treatment of
this skin condition, although they can be considered in the maintenance
phase of treatment [4]. Both topical steroids and immunomodulators are
commonly and safely used in children [4]. Systemic corticosteroids should
be reserved for recalcitrant cases and used for the shortest time possible
(typically 1 week or so) while awaiting response to other therapies. Other
immunosuppressants such as cyclosporine, azathioprine, and methrotrexate
have occasionally be used for recalcitrant and severe cases unresponsive
to the above measures, but with variable success, and typically not in
children [8]. These immunosuppressants all have potential adverse effects,
requiring careful monitoring and restricting their clinical usefulness [13].
Psoralen plus ultraviolet A (PUVA), UVA1 and UVB have been shown to be
effective and may be considered in the treatment of refractory cases in older
children [8]. Narrow-band UVB is most commonly used. More recently, oral
alitretinoin has been shown to be effective for recurrent and refractory cases
of this condition in adults. The response rate is approximately 50% [15].
Intradermal botulinum toxin A has also been tried with some success in
patients with concomitant hyperhidrosis [16]. The medication has potent
antihidrotic activity [16]. Since hyperhidrosis is an aggravating factor,
treatment of hyperhidrosis may lead to regression of the disorder. The
drawback is the need for repeated injections approximately every 6
months. This is rarely used in children because of the pain involved.
Although pruritus in dyshidrotic eczema does not appear to be mediated by
histamine release, oral antihistamines can provide symptomatic relief because
of their sedative properties and may be effective for intense pruritus refractory
to moisturizers and conservative measures. Of the H1 antihistamines,
hydroxyzine is more effective than diphenhydramine and cyproheptadine [13].
Patient/caregivers education and support are vital in the management of
dyshidrotic eczema. Misinformation may be detrimental to disease control.
Steroid fear or phobia among patients/caregivers is common and is a
significant factor in suboptimal use or non-compliance to treatment [17]. Poor
compliance is a major reason for treatment failure. Patients and caregivers
should be reassured that topical corticosteroids are safe and effective with
their sensible use and they remain first-line treatment for acute flares [17].
4. Adams DR, Marks JG (2014) Acute palmplantar eczema (dyshidrotic
eczema). In: Post TW, ed. Up To Date. Waltham, MA.
5. Chen JJ, Liang YH, Zhou FS, Yang S, Wang J, et al. (2006) The gene
for a rare autosomal dominant form of pompholyx maps to chromosome
18q22.1-18q22.3. J Invest Dermatol 126: 300-304.
6. Meding B, Swanbeck G (1989) Epidemiology of different types of hand
eczema in an industrial city. Acta Derm Venereol 69: 227-233.
7. Lee CS, Lim HW (2003) Cutaneous diseases in Asians. Dermatol Clin
21: 668-677.
8. Wollina U (2010) Pompholyx: a review of clinical features, differential
diagnosis, and management. Am J Clin Dermatol 11: 305-314.
9. Abreu-Velez AM, Pinto FJ Jr, Howard MS (2009) Dyshidrotic eczema:
relevance to the immune response in situ. N Am J med Sci 1: 117-120.
10. Markantoni V, Kouris A, Armyra K, Vavouli C, Kontochristopoulos G
(2014) Remarkable improvement of relapsing dyshidrotic eczema after
treatment of coexistant hyperhidrosis with oxybutynin. Dermatol Ther
Doi: 10.1111/dth. 12514.
11. Shiraishi T, Yamamoto T (2013) Severe dyshidrotic eczema after
intravenous immunoglobulin therapy for Kawasaki syndrome. Pediatr
Dermatol 30: e30-e31.
12. Yoon SY, Park HS, Lee JH, Cho S (2013) Histological and differentiation
between palmplantar pustulosis and pompholyx. J Eur Acad Dermatol
Venereol 27: 889-893.
13. Leung AK, Hon KL (2011) Atopic Dermatitis: A Review for the Primary
Care Physician. New York: Nova Science Publishers 1-113.
14. Baumer JH (2008) Atopic eczema in children, NICE. Arch Dis Child
Educ Pract Ed 93: 93-97.
15. Ruzicka T, Lynde CW, Jemec GB, Diepgen T, Berth-Jones J, et
al. (2008) Efficacy and safety of oral alitretinoin (9-cis retinoic acid)
in patients with severe chronic hand eczema refractory to topical
corticosteroids: results of a randomized, double-blind, placebocontrolled, multicentre trial. Br J Dermatol 158: 808-817.
16. Kontochritopoulos G, Gregoriou S, Agiasofitou G, Nikolakis G,
Rigopoulos D, et al. (2007) Regression of relapsing dyshidrotic eczema
after treatment of concomitant hyperhidrosis with botulinum toxin-A.
Dermatol Surg 33:1289-1290.
17. Hon KL, Kam WY, Leung TF, Lam MC, Wong KY, et al. (2006) Steroid
fears in children with eczema. Acta Paediatr 95: 1451-1455.
Reference
1. Brazzelli V, Grassi S, Savasta S, Ruffinazzi G, Carugno A, et al. (2014)
Pompholyx of the hands after intravenous immunoglobulin therapy for
clinically isolated syndrome: a paediatric case. Int J Immunopathol
Pharmacol 27: 127-130.
2. Fox T (1873) Clinical lecture on Dyshidrosis: an undescribed eruption.
Br Med J 2: 365-366.
3. Nezafati KA, Cruz P (2014) Dyshidrotic dermatitis. In: Heyman
WR, Anderson BE, Hivnor C, et al, eds. Clinical Decision Support:
Dermatology. Wilmington, Delaware: Decision Support in Medicine,
LLC, electronic database.
Enliven Archive | www.enlivenarchive.org
Submit your manuscript at
http://enlivenarchive.org/submit-manuscript.php
New initiative of Enliven Archive
Apart from providing HTML, PDF versions; we also provide video
version and deposit the videos in about 15 freely accessible social
network sites that promote videos which in turn will aid in rapid
circulation of articles published with us.
2014 | Volume 1 | Issue 1
Potrebbero piacerti anche
- The Risk Factors in Children With Simple and Complex SeizureDocumento8 pagineThe Risk Factors in Children With Simple and Complex SeizureSuci Dika UtariNessuna valutazione finora
- Mastoiditis PDFDocumento4 pagineMastoiditis PDFMildred MontNessuna valutazione finora
- Prevalence of Pulmonary Embolism Among Patients Hospitalized For SyncopeDocumento8 paginePrevalence of Pulmonary Embolism Among Patients Hospitalized For Syncopeadan2010Nessuna valutazione finora
- MR EnglishDocumento27 pagineMR EnglishSuci Dika UtariNessuna valutazione finora
- Mastoiditis PDFDocumento4 pagineMastoiditis PDFMildred MontNessuna valutazione finora
- Volume 36 Number 2 Article6Documento11 pagineVolume 36 Number 2 Article6Kakak AdekNessuna valutazione finora
- Anestesi MRDocumento18 pagineAnestesi MRSuci Dika UtariNessuna valutazione finora
- Guideline Konjungtivitis CPG-11 PDFDocumento33 pagineGuideline Konjungtivitis CPG-11 PDFhanumzniiNessuna valutazione finora
- Fitzpatricks Derm8e Ref Ch114 PDFDocumento4 pagineFitzpatricks Derm8e Ref Ch114 PDFSuci Dika UtariNessuna valutazione finora
- Files 110711 Squ AmousDocumento4 pagineFiles 110711 Squ AmousReynalth Andrew SinagaNessuna valutazione finora
- A JCR 0000023Documento26 pagineA JCR 0000023feonajaparNessuna valutazione finora
- Fitzpatricks Derm8e Ref Ch114 PDFDocumento4 pagineFitzpatricks Derm8e Ref Ch114 PDFSuci Dika UtariNessuna valutazione finora
- Ecg Findings in Pulmonary Embolism: Acute Cor PulmonaleDocumento1 paginaEcg Findings in Pulmonary Embolism: Acute Cor PulmonaleSuci Dika UtariNessuna valutazione finora
- Ecg Findings in Pulmonary Embolism: Acute Cor PulmonaleDocumento1 paginaEcg Findings in Pulmonary Embolism: Acute Cor PulmonaleSuci Dika UtariNessuna valutazione finora
- Fever PDFDocumento6 pagineFever PDFSuci Dika UtariNessuna valutazione finora
- Varicella Dan Herpes Zoster 2Documento12 pagineVaricella Dan Herpes Zoster 2husenahNessuna valutazione finora
- Newly Developed Approaches For Studying Pathogenesis of Varicella Zoster Virus Jaa.1000065 PDFDocumento10 pagineNewly Developed Approaches For Studying Pathogenesis of Varicella Zoster Virus Jaa.1000065 PDFSuci Dika UtariNessuna valutazione finora
- Varicella Dan Herpes Zoster 2Documento12 pagineVaricella Dan Herpes Zoster 2husenahNessuna valutazione finora
- Expression of The T-Cell-Specific Adapter Protein in Oral EpitheliumDocumento10 pagineExpression of The T-Cell-Specific Adapter Protein in Oral EpitheliumSuci Dika UtariNessuna valutazione finora
- Healthy Neighborhoods GuidebookDocumento102 pagineHealthy Neighborhoods GuidebookSuci Dika UtariNessuna valutazione finora
- Jurnal Cardiovascular Dalam Al - Quran Dan HaditsDocumento5 pagineJurnal Cardiovascular Dalam Al - Quran Dan HaditsAdhitya Soewadji MartodimuljoNessuna valutazione finora
- Model Australian Public Health Policy 20101203 BackgroundDocumento47 pagineModel Australian Public Health Policy 20101203 BackgroundSuci Dika UtariNessuna valutazione finora
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Opalescence Boost Whitening PDFDocumento2 pagineOpalescence Boost Whitening PDFVikas AggarwalNessuna valutazione finora
- Current Cancer Treatment - Novel Beyond Conventional ApproachesDocumento826 pagineCurrent Cancer Treatment - Novel Beyond Conventional Approacheselenac67100% (1)
- Bleak House - Book ThreeDocumento36 pagineBleak House - Book ThreeNicklaus Adam Rhodes100% (1)
- Reflection Paper On Contagion DraftDocumento4 pagineReflection Paper On Contagion DraftSheena ChanNessuna valutazione finora
- Rubber Dam Isolation For Endodontic Treatment in Difficult Clinical SituationsDocumento8 pagineRubber Dam Isolation For Endodontic Treatment in Difficult Clinical SituationsDavid ColonNessuna valutazione finora
- Gwich'in EthnobotanyDocumento72 pagineGwich'in EthnobotanyNatalia Alexandra Bernal QuinteroNessuna valutazione finora
- Monograph On Lung Cancer July14Documento48 pagineMonograph On Lung Cancer July14PatNessuna valutazione finora
- 150 Years of PharmacovigilanceDocumento2 pagine150 Years of PharmacovigilanceCarlos José Lacava Fernández100% (1)
- Dysrhythmia Advance Content Outline A1 - 2020.1.2Documento3 pagineDysrhythmia Advance Content Outline A1 - 2020.1.2Kimberly Whiteside50% (2)
- Clinical Assessment of The Autonomic Nervous System PDFDocumento312 pagineClinical Assessment of The Autonomic Nervous System PDFAndrija100% (1)
- Primary Health Care Notes Health What Is Illness and Causes of Illness?Documento22 paginePrimary Health Care Notes Health What Is Illness and Causes of Illness?Nano KaNessuna valutazione finora
- Filipino Scientists: GE 07 Science, Technology and SocietyDocumento4 pagineFilipino Scientists: GE 07 Science, Technology and SocietyEvangeline EnocNessuna valutazione finora
- Big Data Final ReportDocumento34 pagineBig Data Final Reportclinfox100% (2)
- Individual Performance Commitment and Review (Ipcr) : Name of Employee: Approved By: Date Date FiledDocumento12 pagineIndividual Performance Commitment and Review (Ipcr) : Name of Employee: Approved By: Date Date FiledTiffanny Diane Agbayani RuedasNessuna valutazione finora
- Strabismus and Eye Muscle SurgeryDocumento68 pagineStrabismus and Eye Muscle SurgeryOpeyemi IdaeworNessuna valutazione finora
- Background: Abruptio PlacentaeDocumento6 pagineBackground: Abruptio PlacentaeEj ZGNessuna valutazione finora
- Case Presentation OF: Iron Deficiency AnemiaDocumento33 pagineCase Presentation OF: Iron Deficiency Anemiaitshurt_teardrops100% (1)
- Allergic Rhinitis in ChildrenDocumento39 pagineAllergic Rhinitis in ChildrenrinajackyNessuna valutazione finora
- RestorilDocumento1 paginaRestorilKatie McPeek100% (1)
- The Effects of Virus Variants On COVID-19 Vaccines: Inglés Nivel II Examen FinalDocumento4 pagineThe Effects of Virus Variants On COVID-19 Vaccines: Inglés Nivel II Examen FinalDIEGONessuna valutazione finora
- Meta Health Social Media Toolkit - EnglishDocumento18 pagineMeta Health Social Media Toolkit - EnglishAndri MayasariNessuna valutazione finora
- Emergency Nursing: By: Keverne Jhay P. ColasDocumento61 pagineEmergency Nursing: By: Keverne Jhay P. ColasGaras AnnaBerniceNessuna valutazione finora
- Cases and Doctrines On Legal MedicineDocumento44 pagineCases and Doctrines On Legal MedicineEliza MontemayorNessuna valutazione finora
- Psych Drugs Cheat SheetDocumento4 paginePsych Drugs Cheat SheetSunel100% (35)
- Clinical Findings and Management of PertussisDocumento10 pagineClinical Findings and Management of PertussisAGUS DE COLSANessuna valutazione finora
- Antibiotics, Misuse and ConsequencesDocumento67 pagineAntibiotics, Misuse and Consequencestummalapalli venkateswara raoNessuna valutazione finora
- Colonoscopy Is Mandatory AfterDocumento3 pagineColonoscopy Is Mandatory AfterLaurice BarronNessuna valutazione finora
- Claim IntimationDocumento2 pagineClaim IntimationSyed's Way PoolNessuna valutazione finora
- Kidney CancerDocumento6 pagineKidney CancerAKHILNessuna valutazione finora
- HerbsDocumento3 pagineHerbsUchihaLunaNessuna valutazione finora