Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Adenocarcinoma of The Pancreas
Caricato da
Stephanie Locsin0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
15 visualizzazioni4 pagine******
Titolo originale
Adenocarcinoma of the Pancreas
Copyright
© © All Rights Reserved
Formati disponibili
DOCX, PDF, TXT o leggi online da Scribd
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documento******
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato DOCX, PDF, TXT o leggi online su Scribd
0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
15 visualizzazioni4 pagineAdenocarcinoma of The Pancreas
Caricato da
Stephanie Locsin******
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato DOCX, PDF, TXT o leggi online su Scribd
Sei sulla pagina 1di 4
Adenocarcinoma of the Pancreas
Ductal adenocarcinoma arising in the exocrine part of pancreas,
account for 80-90% of pancreatic tumor. Cystadenocarcinoma and
endocrine tumour account for most of the remains of malignancy.
About two-thirds of pancreatic adenocarcinomas arise within the head
or uncinate process of the pancreas; 15% are in the body, and 10% in
the tail, with the remaining tumors demonstrating diffuse involvement
of the gland. The prevalence of the head in the surgical series result
from earlier detection and better resectability. The average size of
tumors of the head is about 2-3 cm and is smaller than tose of the
body and tail, about 5-7 cm (Gourtsoyiannis, 2005). Despite its
ubiquity, this disease is extremely difficult to treat, and its exact cause
is unknown. However, epidemiologic studies linking various
environmental and host factors provide some clues. The etiology of
pancreatic cancer likely involves a complex interaction of genetic and
environmental factors (Brunicardi, 2014).
Pancreatic cancer is more common in the elderly with most
patients being >60 years old. Peak incidence is in the 6th and 7th
decade. Pancreatic cancer is more common in men than women. The
risk of developing pancreatic cancer is two to three times higher if a
parent or sibling had the disease. Smoking increases the risk of
developing pancreatic cancer by at least twofold due to the
carcinogens in cigarette smoke. As in other GI cancers, diets high in fat
and low in fiber, fruits, and vegetables are thought to be associated
with an increased risk of pancreatic cancer. Diabetes has been known
to be associated with pancreatic cancer for many years. In fact,
glucose intolerance is present in 80% of patients with pancreatic
cancer, and approximately 50% have overt diabetes. Pre-existing type
2 diabetes increases the risk for development of pancreatic cancer by
about twofold. (Brunicardi, 2014).
Although exact pathophysiologic mechanism is unknown,
pancreatic cancer is related to mutation of K-ras oncogene in 90% of
pancreatic tumours. It s detected in DNA from serum, stool, pancreatic
juice, tissue aspirates. Another is overexpression of HER-2/neu
oncogene which is exaggeration of cellular proliferation. 10% of
pancreatic cancers: result of inherited genetic predisposition as
manifested by family history of pancreatic cancer increases the risk by
two-fold (Brunicardi, 2014).
Pancreatic cancer probably arises through a step-wise
progression of cellular changes, just as colon cancer progresses by
stages from hyperplastic polyp to invasive cancer. Systematic
histologic evaluation of areas surrounding pancreatic cancers has
revealed the presence of precursor lesions that have been named
pancreatic intraepithelial neoplasia.
Spread of pancreatic tumours is by local Invasion, lymphatic,
blood and via peritoneal & omental causing ascites. The diagnosis of
pancreatic cancer varies from the simple and clinically obvious to the
most difficult and almost impossible the initial symptoms and signs
depend on the site and extent of the pancreatic cancer.
Clinical manifestation includes weight loss, icteric skin, distented
gallbladder in 1/4 of patients, pain perceived in epigastrium,
experienced as mild and vague, jaundice, the most common and may
present as painless, steatorrhea, duodenal obstruction, a late event
and present in about 20% of patients, diabetes mellitus, acute
pancreatitis, malignant ascites, gastric outlet obstruction.
Approach to investigations include ultrasound scan especially for
patients with jaundice, CT scan, MRI scan, PET scan, ERCP, histology
and cytology, angiography of the celiac and superior mesenteric artery
and laparoscopy. CT Scan is the single most versatile and cost-effective
tool for diagnosis and staging of pancreatic cancer. It is done for
patients who present pain but with no jaundice. Accuracy of 90-95% in
unresectable diseases it is less accurate in resectable diseases. PET
Scan is used to distinguish chronic pancreatitis from pancreatic cancer.
The American Joint Committee on Cancer proposed TNM Staging
for Pancreatic Cancer as shown by the table below.
Over 90% of patient with pancreatic cancer present in the late
stage of their disease. At this time, there is no chance of cure. Only
palliation is an effective form of management. The factors responsible
for late diagnosis are tumor is asymptomatic in the early stage, patient
delay, physician delay and the patient may not have ready and easy
access to competent diagnostic center.
Refrence:
Brunicardi, F. (2014). Schwartz's principles of surgery (8th ed.). New
York: McGraw-Hill, Health Pub. Division.
Gourtsoyiannis, N. (2005). Radiologic-pathologic correlations from head
to toe: Understanding the manifestations of disease. Berlin: Springer.
Potrebbero piacerti anche
- Hypertensionin PregnancyDocumento100 pagineHypertensionin Pregnancyricky hutagalungNessuna valutazione finora
- Adenocrcinoma of The PancreasDocumento5 pagineAdenocrcinoma of The PancreasStephanie LocsinNessuna valutazione finora
- B Symptoms Fever Night Sweats Weight LossDocumento1 paginaB Symptoms Fever Night Sweats Weight LossStephanie LocsinNessuna valutazione finora
- Primary Lung CancerDocumento3 paginePrimary Lung CancerStephanie LocsinNessuna valutazione finora
- CholeraDocumento6 pagineCholeraStephanie LocsinNessuna valutazione finora
- Adenocarcinoma of The PancreasDocumento4 pagineAdenocarcinoma of The PancreasStephanie LocsinNessuna valutazione finora
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (119)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Common Disorders of The PancreasDocumento2 pagineCommon Disorders of The PancreasEli AyaseNessuna valutazione finora
- Apple Inc.: Presented by Lukas Caregorodcevas (TPML18)Documento20 pagineApple Inc.: Presented by Lukas Caregorodcevas (TPML18)Gabrielė GineikaitėNessuna valutazione finora
- KPC Mouse ModelDocumento16 pagineKPC Mouse Modeljoe smoNessuna valutazione finora
- YÖKDİL Sağlık 26 Şubat 2017Documento20 pagineYÖKDİL Sağlık 26 Şubat 2017SalmaanCadeXaajiNessuna valutazione finora
- American College of Gastroenterology Guideline .6Documento16 pagineAmerican College of Gastroenterology Guideline .6Alex Antony Fernandez QuisocalaNessuna valutazione finora
- AJR050569Documento15 pagineAJR050569Jorge SosaNessuna valutazione finora
- Crossroads Summer 08Documento99 pagineCrossroads Summer 08csatterwhiteNessuna valutazione finora
- ACG Guideline AcutePancreatitis September 2013Documento16 pagineACG Guideline AcutePancreatitis September 2013gorditomaloNessuna valutazione finora
- GemcitabineDocumento6 pagineGemcitabineCaballero X CaballeroNessuna valutazione finora
- Met Caz ClinicDocumento57 pagineMet Caz ClinicIndrecan AndreiNessuna valutazione finora
- 2005 AHPBA CONGRESS ABSTRACTS—FREE PAPERS AND VIDEOSDocumento100 pagine2005 AHPBA CONGRESS ABSTRACTS—FREE PAPERS AND VIDEOSDrAmmar MagdyNessuna valutazione finora
- Surgery 1Documento73 pagineSurgery 1Ong Kie80% (5)
- Pancreatic CancerDocumento6 paginePancreatic CancermillexaNessuna valutazione finora
- Anaesthesiology For Pancreatic CancerDocumento18 pagineAnaesthesiology For Pancreatic CancerAnggi CalapiNessuna valutazione finora
- Abdo Sepsis TabsDocumento15 pagineAbdo Sepsis TabsSantosh ParabNessuna valutazione finora
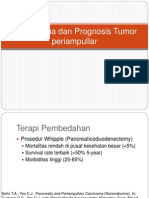
- Tatalaksana Tumor periampullarDocumento16 pagineTatalaksana Tumor periampullarVerico PratamaNessuna valutazione finora
- Application of Endoscopic Ultrasound Guided Fnac (Eus-Fnac) in Diagnosing Pancreatic Mass LesionsDocumento7 pagineApplication of Endoscopic Ultrasound Guided Fnac (Eus-Fnac) in Diagnosing Pancreatic Mass LesionsIJAR JOURNALNessuna valutazione finora
- Last Minute Revision Points SurgeryDocumento45 pagineLast Minute Revision Points Surgerysrikanth harinadhNessuna valutazione finora
- Bailey 28th Edtion - Spleen-GB-PancreasDocumento86 pagineBailey 28th Edtion - Spleen-GB-Pancreasnihal jainNessuna valutazione finora
- Ceo Health Disclosure at AppleDocumento3 pagineCeo Health Disclosure at AppleToral ShahNessuna valutazione finora
- Imir Studyguide2014Documento499 pagineImir Studyguide2014Sam GhaziNessuna valutazione finora
- Copying Music from One CD to AnotherDocumento17 pagineCopying Music from One CD to AnotherAurellia ShafitriNessuna valutazione finora
- Abraxane DetailDocumento7 pagineAbraxane DetailGoel VaibhavNessuna valutazione finora
- 2013 - Pancreaticoduodenectomy (Whipple Procedure) TechniquesDocumento11 pagine2013 - Pancreaticoduodenectomy (Whipple Procedure) TechniquesOlteanu IonutNessuna valutazione finora
- Volum de Rezumate Gastro Mamaia 2021Documento108 pagineVolum de Rezumate Gastro Mamaia 2021Mariana UngurNessuna valutazione finora
- Fat MalabsorbtionDocumento18 pagineFat MalabsorbtionDragosAurNessuna valutazione finora
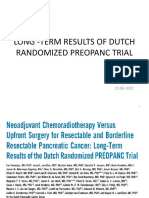
- Preopanc Trial - PancreasDocumento20 paginePreopanc Trial - PancreasRajalakshmi RadhakrishnanNessuna valutazione finora
- 2012-03 - Resection of Tumors of The Neck of The Pancreas With Venous Invasion - The "Whipple at The Splenic Artery (WATSA) " Procedure PDFDocumento7 pagine2012-03 - Resection of Tumors of The Neck of The Pancreas With Venous Invasion - The "Whipple at The Splenic Artery (WATSA) " Procedure PDFNawzad SulayvaniNessuna valutazione finora
- VRAY - Investor Presentation - October 2018Documento24 pagineVRAY - Investor Presentation - October 2018medtechyNessuna valutazione finora
- Un Bahasa Inggris Dear Customer 16 17 Damaged 20 22 PDFDocumento18 pagineUn Bahasa Inggris Dear Customer 16 17 Damaged 20 22 PDFAradila PriandoNessuna valutazione finora