Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Comparative Study of Midazolam On The Characteristics of Intrathecal Bupivacaine - A Prospective Randomized Study
Caricato da
IOSRjournalTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Comparative Study of Midazolam On The Characteristics of Intrathecal Bupivacaine - A Prospective Randomized Study
Caricato da
IOSRjournalCopyright:
Formati disponibili
IOSR Journal of Dental and Medical Sciences (IOSR-JDMS)
e-ISSN: 2279-0853, p-ISSN: 2279-0861.Volume 14, Issue 10 Ver.III (Oct. 2015), PP 31-36
www.iosrjournals.org
Comparative Study of Midazolam on the Characteristics of
Intrathecal Bupivacaine A Prospective Randomized Study
Dr S.Anal Kumar.M.D.,
Assistant Professor, Department of Anaesthesiology, Siddhartha Medical College
Dr. Abhimanyu Singh. M.D.,
Associate Professor, Department of Anaesthesiology, Siddhartha Medical College
Dr. S. Vinay Kumar. M.D.,
Assistant Professor, Department of Anaesthesiology, Siddhartha Medical College
Dr.T. Suryashree M.D.,
Professor and H.O.D., Department of Anaesthesiology, Siddhartha Medical College
Abstract:
Introduction: Spinal Anaesthesia is the most commonly used technique for lower abdominal & lower limb
surgeries as it is very economical and easy to administer. A common problem during lower abdominal & lower
limb surgeries under spinal anaesthesia is visceral pain, nausea and vomiting. Local anaesthetic agents for
spinal anaesthesia are used have various side effects and less duration of action. In order to minimize the side
effects and maximize the duration of analgesia, various adjuvants have been used along with local anaesthetics.
A number of adjuvants like fentanyl, clonidine, dexmeditomide etc., have been used to improve the quality of
subarachnoid block. Midazolam a water soluble benzodiazepine is used to increase the duration of analgesia
and facilitate early ambulation and reducing hospital stay of the patient. The aim of the study was to compare
the subarachnoid block characteristics with Midazolam to intrathecal Bupivacaine.
Methodology: After Institutional ethics committee approved and written informed consent, 100 patients between
16-60 years belonging to ASA I&II were included in the study. Patients were randomly allocated into 2 groups
of 50 each. Group-1 received 3ml of 0.5% hyperbaric bupivacaine with 0.5ml of 0.9% Saline. Group-2 received
3ml of Hyperbaric Bupivacaine with 0.5m l (2.5mg) of preservative free midazolam. Total volume made upto
3.5ml to achieve subarachnoid block.
Sensory block characteristics, motor block characteristics, Haemodynamic characteristics, adverse
effects, duration of analgesia, statistical analysis and results were noted in all groups. Statistical analysis was
done with one way analysis of variants. Duration of sensory blockade was significantly longer in group-II than
in group-I. (P value < 0.001). Duration of Motor blockade was also higher in group-II only to some extent (P
value < 0.01). The first request of analgesia was significantly longer in group-II than group-I.
Conclusion: Addition of Midazolam to intrathecal bupivacaine produces better quality of analgesia and without
gross haemodynamic disturbances comparative to bupivacaine alone.
Key Words: Analgesia, Bupivacaine, midazolam, Postoperative, Subarachnoid blockade.
I.
Introduction
Spinal Anaesthesia is the most commonly used technique for lower abdominal surgeries including
orthopaedic surgeries, as it is very economical and easy to administer and safe. Howeverusing local anesthetics
alone for subarachnoid block associated with relatively short duration ofaction. Addition of adjuvants like
fentanyl, ketamine,clonidine etc, to intrathecal bupivacaine significantly prolongs the duration of spinal
anaesthesia and also improved quality of spinal blockade in various clinical studies1,2. A common problem
during lower abdominal and orthopaedic surgeries under spinal anaesthesia is visceral pain, nauseaand
vomiting3. This problem can be overcome by the addition of anti-emetics preoperatively and the addition of
adjuvants to improve the quality of block.
II.
Methodology
After institutional ethics committee approval written informed consent 100 patients of ASA Grade-I &
II belonging to both sexes were scheduled for lower abdominal andorthopaedic surgeries included in the
prospective randomized controlled study.
Exclusion Criteria:
1. ASA Grade >III
2. Patients below 16 years and above 60 years of age.
DOI: 10.9790/0853-141033136
www.iosrjournals.org
31 | Page
Comparative Study of Midazolam on the Characteristics of Intrathecal Bupivacaine
3.
Patients with H/O severe systemic diseases, metabolic disorders, neurological, congenital &
cardiovascular disorders.
Patients with H/O allergy to study drugs i.e., bupivacaine, midazolam.
Patients with H/O any contra indications to spinal anesthesia.
Pregnancy.
4.
5.
6.
Two investigators involved in the study. The observer and anesthesiologist who did intra operative and
post operative monitoring were blinded to study. Patients were randomized into 2 groups50 each into Group A
& B.
Baseline parameters like HR,PR,NIBP,SPO2 were recorded in all the 2 groups. After shifting the
patient to operating room routine monitors like NIBP, SPO2 and ECG were applied to the patient. Anemergency
resuscitation equipment were kept ready. 18G I V cannula was secured and all patients were preloaded with
10ml per Kg oflactated Ringers solution. The patients were placed either in the left lateral or right lateral
position, under strict aseptic precautions the lumbar puncture was carried out in midline through L3-L4
interspace with 25G quink babcocks needle. Group A(n=50) patients received 0.5% hyperbaric
bupivacaine(3ml) with 0.9% normal saline(0.5ml). Group B(n=50) patients received 0.5% hyperbaric
bupivacaine(3ml) with midazolam 2.5mg (0.5ml)
In all the groups the total volume administered was made upto 3.5ml to achieve subarachnoid block.
Intra operatively bradycardia was treated with 1mg of I V atropine. Hypotension was treated with rapid boluses
of I V fluids and incremental doses of 6mg of ephedrine. The following parameters were observed.
1. Sensory block was assessed by using Pinprick method. Onset time and duration of sensory blockade
was recorded.
2. Motor block was assessed by using bromage scale (Table-I). Onset time and duration of motor
blockade was noted between 2 groups.
3. Haemodynamic parameters like HR, BP were noted between the 2 groups.
4. Time to first request of analgesia (the duration of post operative analgesia) was compared between the
2 groups.
5. Adverse effects were also noted between the groups. The possible adverse effects like hypotension,
bradycardia, nausea, vomiting, sedation, pruritis, urinary retention, respiratory depression etc., were
noted.
Table 1Bromage Scale
BROMAGE SCALE
0
1
2
3
Free movement of legs and feet, with ability to raise extended leg
Inability to raise extended leg and knee flexion is decreased but full flexion of feet and ankle is present
Unable to flex knees but some flexion of feet and ankle is possible
Unable to move feet, legs or toes
III.
Statistical Analysis:
Demographic data was analysed by using fischers exart test. Sensory and motor characteristics
analysed by using one way analysis of variants of student-t test. Time to first request of analgesia was assessed
by using student-t test. It was expressed in Mean, Standard deviation, Absolute numbers and percentage.
P>0.005 was considered significant.
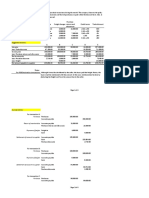
Table 2Age And Sex Distribution In Both The Groups
GROUP I
Age in years
16-25
26-35
36-45
46-55
>55
Total
Male
5
5
8
7
7
32
GROUP - II
Female
4
4
3
5
2
18
Male
6
5
7
6
8
32
Female
4
4
3
4
3
18
The mean age of the patient in Group I was 40.814 and in Group II was 41.1 14.3. Age incidence
between two groups and age distribution between two groups were comparable. In the both the groups male
patients were 64% and female patients were 36%. The sex ratio in both the groups is equal.
DOI: 10.9790/0853-141033136
www.iosrjournals.org
32 | Page
Comparative Study of Midazolam on the Characteristics of Intrathecal Bupivacaine
Table -3Distribution Of Height Of The Patients In Both The Groups
GROUP I
Height in
Centimeters
145-150
150-160
160-170
>170
Male
1
6
2
3
GROUP - II
Female
1
12
5
0
Male
2
7
21
2
TOTAL
Female
1
13
4
0
5
38
32
5
Table -4Distribution Of Weight Of The Patients In Both The Groups
GROUP I
Weight in Kgs
Male
1
3
10
8
8
2
46-50
51-55
56-60
61-65
66-70
71-75
GROUP - II
Female
2
7
3
3
3
0
Male
1
3
6
10
9
3
TOTAL
Female
3
5
5
3
2
0
7
18
24
24
22
5
The height and weight of the patients in Group-I and Group-II are comparable.
Table -5Perioperative SBP (Systolic Blood Pressure)Of The Patients At Different Time Intervals.
Time
minutes
0
5
10
20
30
45
60
120
in
Group I
MeanSD
124.0411.75
119.2810.66
114.749.14
113.068.78
116.727.94
118.448.03
118.848.40
120.329.30
Group II
MeanSD
125.489.94
120.168.9
115.048.80
112.649.08
114.888.74
117.888.76
119.968.75
120.928.57
Significance
p>0.05
p>0.05
p>0.05
p>0.05
p>0.05
p>0.05
p>0.05
p>0.05
There was a fall in SBP in both the groups during first 20 minutes after intrathecal injection and there
was gradual recovery after 20 minutes. This difference of recovery in SBP between the groups at different time
intervals studied was statistically insignificant(P>0.05).
Table 6Perioperative DBP (Diastolic Blood Pressure) At Different Time Intervals
Time
minutes
0
5
10
20
30
45
60
120
in
Group I
MeanSD
79.905.21
76.885.30
74.765.11
74.245.19
74.365.12
74.885.25
75.125.28
80.205.38
Group II
MeanSD
78.286.29
76.325.90
74.085.50
73.165.37
73.765.51
73.445.38
74.765.49
79.965.67
Significance
p>0.05
p>0.05
p>0.05
p>0.05
p>0.05
p>0.05
p>0.05
p>0.05
There was a fall in DBP in both the groups during first 20 minutes after intrathecal injection and was
gradual recovery after 20 minutes. This difference of recovery in DBP between the groups at different time
intervals studied was statistically insignificant.(P>0.05).
TABLE -7 Perioperative Heart Rate At Different Time Intervals
Time
minutes
0
5
10
20
30
45
60
120
in
DOI: 10.9790/0853-141033136
Group I
MeanSD
81.327.35
82.486.78
83.367.00
83.706.32
81.647.13
81.447.12
82.327.13
82.847.13
Group II
MeanSD
81.167.18
82.126.78
82.206.57
82.405.60
81.345.66
81.045.63
81.245.64
80.606.39
www.iosrjournals.org
Significance
p>0.05
p>0.05
p>0.05
p>0.05
p>0.05
p>0.05
p>0.05
p>0.05
33 | Page
Comparative Study of Midazolam on the Characteristics of Intrathecal Bupivacaine
There was an increase in heart rate in both the groups during first 20 minutes and then gradual decrease
towards normal. The heartrate was slightly lower in group II at all time intervals. The difference between the
groups at different time intervals studied was statistically insignificant.(p>0.05)
Table 8Onset Of Sensory Blockade (Seconds) In Eithergroups
Group I
MeanSD
149.1611.30
Group II
MeanSD
170.8413.83
Significance
P<0.001
The onset of Sensory blockade was 149.1611.30 sec in Group-I and 170.8413.83 sec in Group-II
was delayed in Group-II. The difference between the groups was statistically highly significant.(P<0.001)
Table 9Onset Of Motor Blockade (Seconds) In Eithergroups
Group I
MeanSD
217.4038.80
Group II
MeanSD
239.9611.83
Significance
P<0.001
The onset of Motor blockade was 217.4038.80 sec in Group-I and 239.9611.83 sec in Group-II was
delayed in Group-II. The difference between the groups was statistically highly significant.(P<0.001)
Table 10Regression Of Sensory Levels To L2 Dermatome In Minutes
Group I
MeanSD
140.487.28
Group II
MeanSD
165.485.03
Significance
P<0.001
The time to regression of sensory level to L2 dermatome in Group-I was 140.487.28 min and in
Group-II was 165.485.03 min. The regression time was more in group-II than in group-I. The difference
between the groups was statistically highly significant (P<0.001).
Table 11Time For Complete Motor Recovery In Minutes
Group I
MeanSD
180.045.15
Group II
MeanSD
181.125.20
Significance
P>0.05
The time for complete motor recovery was 180.045.15 min in Group-I, 181.125.20 min in Group-II.
The recovery time for motor blockade was similar in both the groups. The difference between the groups was
statistically insignificant(P>0.05).
Table 12Time Of First Request Analgesics By The Patients In Either Group In Minutes
Group I
MeanSD
206.968.31
Group II
MeanSD
361.308.25
Significance
P<0.001
The time of first request analgesics by the patients in Group-I was 206.968.31 min and 361.308.25
min in Group II, which was longer in Group II than in Group I. The difference between the groups was
statistically highly significant (P<0.001).
Table 13 Adverse Effects
Group I
2
4
3
0
0
0
Adverse Effects
Nausea Vomiting
Hypotension
Shivering
Pruritus
Seizures
Respiratory depression
IV.
Group II
1
4
2
0
0
0
Discussion
Regional Anaesthesia, particularly spinal anaesthesia is most commonly used technique worldwide for
lower abdominal and orthopaedic surgeries. Using local anaesthetics alone will provide less duration of
analgesia. In order to improve the quality of analgesia as well as to provide extended postoperative analgesia,
various adjuvants are being added to intrathecal local anaesthetics. Of which midazolam have gained
prominence due to their multiple beneficial effects like prolonged postoperative analgesia, stable
DOI: 10.9790/0853-141033136
www.iosrjournals.org
34 | Page
Comparative Study of Midazolam on the Characteristics of Intrathecal Bupivacaine
haemodynamics, reducing postoperative analgesic requirements, facilitate early ambulation and reduced hospital
stay. The procedure should not cause complications, simple, easy and not time consuming. Should be prevent
discomfort due to multiple pricks of IM/IV injections and relieve more work load on nursing staff.
The principle mechanism by which intrathecalmidazolam provides analgesia is through the GABABenzodiazepine system in the spinal cord and there is ample evidence to show the GABA receptors in the spinal
cord are involved in nociceptive mechanisms.
This prospective study was conducted to compare intrathecal bupivacaine and bupivacaine with
midazolam in lower abdominal and lower limb surgeries. The patients were selected at random to avoid any
kind of bias and to allow comparability of results obtained.
Intrathecal administration of midazolam relieved post operative pain of somatic origin. This study was well
correlated with Goodchild CS; Noble j (1987 Mar)4.
Edwards M, Serro JM, Gent JP, Good child CS (1990)5 studied the mechanism by which midazolam causes
spinally mediated analgesia. Our study was well correlated with this study.
Valentine, J.MJ; Lyons, GL Bellamy, M.C.(1996)6 studied the effect of intrathecal midazolam on
postoperative pain. 52 patients scheduled for elective caesarean section under spinal anaesthesia were randomly
allocated to receive either bupivacaine(B), bupivacaine with diamorphine(BD), bupivacaine with midazolam or
all three(BMD) by intrathecal injection. Post operatively no differences in Visual analogue score (VAS),
sedation, post operative nausea and vomiting could be demonstrated between groups. No side effects
attributable to midazolam were identified. Intrathecal midazolam appears safe and has clinically detectable
analgesic properties. Our study was well correlated with the study.
Batra.YK; Jain.K; Chari.P; Dhillon MS; Shaheen.B; Reddy-GM (1999)7 to evaluate the post operative
analgesic effect of intrathecal midazolam and bupivacaine mixture in patients undergoing knee
arthroscopyprovided better post operative analgesia without any adverse effects well correlated with our study.
Sen A, Rudra A, Sarkar SK, Biswas B (2001 Dec.)8 conducted a study about intrathecal midazolam for
postoperative pain relief in caesarean section deliveries. It produces highly significant post operative pain relief.
Our study well correlated with the study.
Kim M.H; Lee Y.M. (January 2001)9 showed the intrathecal midazolam increases the analgesic effects of
spinal blockade with bupivacaine in patients undergoing haemorrhoidectomy well correlated with our study.
Amr M.Abdelfatah, MD; Ahmed A.Fawaz, MD; Hesham M.AL-Azazi, MD(2003)10 studied the post
operative analgesic effect of intrathecal fentanyl versus midazolam in knee arthroscopy. Midazolam bupivacaine
mixture appears to be superior to fentanyl-bupivacaine mixture by its reduced magnitude of undesirable effects,
correlates with our study.
Bharti N, Madan R, Mohanty PR, Kaul HL (2003)11 studied the effect of addition of midazolam to intrathecal
bupivacaine on the duration and quality of spinal blockade, significantly improves the duration of quality of
spinal anaesthesia and provides prolonged perioperative analgesia without significant side-effects well
correlated with our study.
Yegin Sanli S, Dosemeci L, Kayacan N, Akbas M, Karsli B (2004) 12 conducted as study to evaluate the
analgesic and sedative effects of intrathecal midazolam with bupivacaine in spinal anaesthesia in patients
undergoing perianal surgery produces more effective and longer analgesia with mild sedative effect well
correlates with our study.
Prakash Smitha; Joshi N; Gogia AR; Prakash Sunil; Singh R(2006)13 conducted a study on analgesic effect
of intrathecal midazolam with bupivacaine. It provides moderate prolongation of post operative analgesia when
used as an adjuvant to bupivacaine. Our study was well correlated with this study.
Mi Ja Yun; Yoon Hee Kim; Jin Hee Kim; Kyoung Ok Kim; Aa Young Oh; Hee P Park (2007) 14 examined
the effect of 1 or 2 mg of intrathecal midazolam added to bupivacaine on the duration of spinal anaesthesia to
T10 in orthopaedic patients. Addition of 2mg midazolam to bupivacaine prolonged the duration of spinal block
to T10 well correlated with our study.
Mohammed Saeed Abd EI Aziz (2009)15 conducted a study on intrathecal midazolam as adjuvant to
bupivacaine 0.5% in orthopaedic surgeries increases the analgesic effects and lowers side effects well correlates
with our study.
Shadangi BK; Garg R; Pandey R; Das T (2011)16 conducted a prospective randomized case control study on
effects of intrathecal midazolam resulted in prolonged post operative analgesia without increasing motor block
in lower limb and gynaecological procedures.
V.
Conclusion
Addition of 2.5mg of midazolam with 0.5% hyperbaric bupivacaine produces better quality of
analgesia, longer duration of analgesia reduced post operative analgesia requirements without gross
hemodynamic disturbances compared to bupivacaine alone in lower abdominal and lower limb surgeries.
DOI: 10.9790/0853-141033136
www.iosrjournals.org
35 | Page
Comparative Study of Midazolam on the Characteristics of Intrathecal Bupivacaine
Bibliography
[1].
[2].
[3].
[4].
[5].
[6].
[7].
[8].
[9].
[10].
[11].
[12].
[13].
[14].
[15].
[16].
Brown DL. Spinal block in Atlas of Regional Anesthesia, 2 nd Edition, Philadelphia, WB Saunders Company, 1999.
Cousins MJ, Bridenbaugh PO. Spinal neural blockade in Neural Blockade. In: Clinical Anesthesia and Management of Pain. 3 rd
Edition, Philadelphia Lippincott-Raven, 1998.
Collins VJ. Spinal anesthesia, In: Principles of Anesthesiology General& Regional Anesthesia, 3 rd Edition, Philadelphia, Lea and
Febiger, 1993.
Goodchild CS, Noble J. The effects of intrathecal midazolam on sympathetic nervous system reflexes in man A Pilot Study.
Br.J.Clin.Pharmacol, 1987 March;23(3):279-85.
Edward! M, Serrao JM, Gent JP, Goodchild CS. On the mechanism by which midazolam causes spinally mediated analgesia.
Anesthesiology 1990 Aug;73(2):273-7.
Valentine JMJ, Lyons G, Bellamy MC. The effect of intrathecal midazolam on postoperative pain. European Journal of
Anaesthesiology, Nov.1996;13(6):589-593.
Batra YK, Jain K, Chari P, Dillon MS, Shaheen B, Reddy GM, Addition of intrathecal midazolam to bupivacaine produces better
postoperative analgesia without prolonging recovery, Int.J.Clin.Pharmacol. Ther., 1999Oct;37(10):519-23.
Sen A, Rudra A, Sarkar SK, Biswas B. Intrathecal midazolam for postoperative pain relief in caesarean section delivery. J Indian
Med Assoc 2001 Dec;99(12):683-4:686.
Kim MH, Lee YM. Intrathecal midazolam increases the analgesic effects of spinal blockade with bupivacaine in patients
undergoing haemorrhoidectomy. British Journal of Anaesthesia, January 2001; 86(1):77-79.
Amr M Abdelfatah, Ahmed A Fawaz, Hesham M AI-Azazi. The post operative analgesic effect of intrathecal fentanyl versus
midazolam in knee arthroscopy. Eng.J.Anaesth.2003: 19:173-177.
Bharti N, Madan R, Mohanty PR, Kaul HL. Intrathecal midazolam added to bupivacaine improve the duration and quality of spinal
anaesthesia. Acta Anaesthesiol Scand. 2003 Oct; 47(9); 1101-5.
Yegin A, Sanli S, Dosemeci L, Kayacan N, Akbas M, Karsli B. The analgesic and sedative effects of intrathecal midazolam in
perianal surgery. Eur J Anesthesiol.2004 Aug;21(8):658-62.
Prakash S, Joshi N, Gogia AR, Praksh S, Singh R. Analgesic efficacy of two doses of intrathecal midazolam with bupivacaine in
patients undergoing cesarean delivery. Reg Anesth Pain Med.2006 may-Jun; 31(3):221-6.
Mi Ja Yun; Yoon Hee Kim; Jin Hee Kim; Kyoung Ok Kim; Aa Young Oh; Hee P Park. Intrathecal Midazolam added to
bupivacaine prolongs the duration of spinal blockade to T10 dermatome in orthopedic patients. Korean J Anesthesiol 2007;53:S228.
Mohammed Saeed Abd El Aziz, Evaluation of intrathecal midazolam as adjuvant to bupivacaine 0.5% in orthopedic surgery; Ain
Shams journal of anesthesia; Vol-2 jan2009 pp31-34.
Shadangi BK; Garg R; Pandey R; Das: Effects of intrathecal midazolam in spinal anaesthesia: a prospective randomized case
control study. Original article-Singapore Med J 2011; 52(6): 432-5.
DOI: 10.9790/0853-141033136
www.iosrjournals.org
36 | Page
Potrebbero piacerti anche
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Attitude and Perceptions of University Students in Zimbabwe Towards HomosexualityDocumento5 pagineAttitude and Perceptions of University Students in Zimbabwe Towards HomosexualityInternational Organization of Scientific Research (IOSR)Nessuna valutazione finora
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- A Review of Rural Local Government System in Zimbabwe From 1980 To 2014Documento15 pagineA Review of Rural Local Government System in Zimbabwe From 1980 To 2014International Organization of Scientific Research (IOSR)Nessuna valutazione finora
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- "I Am Not Gay Says A Gay Christian." A Qualitative Study On Beliefs and Prejudices of Christians Towards Homosexuality in ZimbabweDocumento5 pagine"I Am Not Gay Says A Gay Christian." A Qualitative Study On Beliefs and Prejudices of Christians Towards Homosexuality in ZimbabweInternational Organization of Scientific Research (IOSR)Nessuna valutazione finora
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Socio-Ethical Impact of Turkish Dramas On Educated Females of Gujranwala-PakistanDocumento7 pagineSocio-Ethical Impact of Turkish Dramas On Educated Females of Gujranwala-PakistanInternational Organization of Scientific Research (IOSR)Nessuna valutazione finora
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Role of Extrovert and Introvert Personality in Second Language AcquisitionDocumento6 pagineThe Role of Extrovert and Introvert Personality in Second Language AcquisitionInternational Organization of Scientific Research (IOSR)Nessuna valutazione finora
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- A Proposed Framework On Working With Parents of Children With Special Needs in SingaporeDocumento7 pagineA Proposed Framework On Working With Parents of Children With Special Needs in SingaporeInternational Organization of Scientific Research (IOSR)Nessuna valutazione finora
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Assessment of The Implementation of Federal Character in Nigeria.Documento5 pagineAssessment of The Implementation of Federal Character in Nigeria.International Organization of Scientific Research (IOSR)Nessuna valutazione finora
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- The Impact of Technologies On Society: A ReviewDocumento5 pagineThe Impact of Technologies On Society: A ReviewInternational Organization of Scientific Research (IOSR)100% (1)
- Comparative Visual Analysis of Symbolic and Illegible Indus Valley Script With Other LanguagesDocumento7 pagineComparative Visual Analysis of Symbolic and Illegible Indus Valley Script With Other LanguagesInternational Organization of Scientific Research (IOSR)Nessuna valutazione finora
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Investigation of Unbelief and Faith in The Islam According To The Statement, Mr. Ahmed MoftizadehDocumento4 pagineInvestigation of Unbelief and Faith in The Islam According To The Statement, Mr. Ahmed MoftizadehInternational Organization of Scientific Research (IOSR)Nessuna valutazione finora
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Edward Albee and His Mother Characters: An Analysis of Selected PlaysDocumento5 pagineEdward Albee and His Mother Characters: An Analysis of Selected PlaysInternational Organization of Scientific Research (IOSR)Nessuna valutazione finora
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Topic: Using Wiki To Improve Students' Academic Writing in English Collaboratively: A Case Study On Undergraduate Students in BangladeshDocumento7 pagineTopic: Using Wiki To Improve Students' Academic Writing in English Collaboratively: A Case Study On Undergraduate Students in BangladeshInternational Organization of Scientific Research (IOSR)Nessuna valutazione finora
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- An Evaluation of Lowell's Poem "The Quaker Graveyard in Nantucket" As A Pastoral ElegyDocumento14 pagineAn Evaluation of Lowell's Poem "The Quaker Graveyard in Nantucket" As A Pastoral ElegyInternational Organization of Scientific Research (IOSR)Nessuna valutazione finora
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- Importance of Mass Media in Communicating Health Messages: An AnalysisDocumento6 pagineImportance of Mass Media in Communicating Health Messages: An AnalysisInternational Organization of Scientific Research (IOSR)Nessuna valutazione finora
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Role of Madarsa Education in Empowerment of Muslims in IndiaDocumento6 pagineRole of Madarsa Education in Empowerment of Muslims in IndiaInternational Organization of Scientific Research (IOSR)Nessuna valutazione finora
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Relationship Between Social Support and Self-Esteem of Adolescent GirlsDocumento5 pagineRelationship Between Social Support and Self-Esteem of Adolescent GirlsInternational Organization of Scientific Research (IOSR)Nessuna valutazione finora
- Designing of Indo-Western Garments Influenced From Different Indian Classical Dance CostumesDocumento5 pagineDesigning of Indo-Western Garments Influenced From Different Indian Classical Dance CostumesIOSRjournalNessuna valutazione finora
- Application List: Required Items: A: Cpu-95 Ignition ModuleDocumento12 pagineApplication List: Required Items: A: Cpu-95 Ignition ModuleShubra DebNessuna valutazione finora
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- CH 3 TestDocumento50 pagineCH 3 TestVK ACCANessuna valutazione finora
- Curriculum Vitae ofDocumento4 pagineCurriculum Vitae ofAndrew OlsonNessuna valutazione finora
- Olp Lesson PlanDocumento2 pagineOlp Lesson Planapi-654865620Nessuna valutazione finora
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- Pengaruh Promosi Dan Brand Image (Citra Produk) Terhadap Loyalitas Pembelian Produk Pepsodent Di Ramayana Plaza, Jalan Aksara, Medan Dita AmanahDocumento13 paginePengaruh Promosi Dan Brand Image (Citra Produk) Terhadap Loyalitas Pembelian Produk Pepsodent Di Ramayana Plaza, Jalan Aksara, Medan Dita AmanahAhmad HerdandiNessuna valutazione finora
- Upsa Y5 2023Documento8 pagineUpsa Y5 2023Faizal AzrinNessuna valutazione finora
- A Single-Stage Asymmetrical Half-Bridge Flyback CoDocumento16 pagineA Single-Stage Asymmetrical Half-Bridge Flyback CoSantosh KumarNessuna valutazione finora
- Handout No. 03 - Purchase TransactionsDocumento4 pagineHandout No. 03 - Purchase TransactionsApril SasamNessuna valutazione finora
- 8 - Packed Tower Design-1Documento65 pagine8 - Packed Tower Design-1M.H vafaeiNessuna valutazione finora
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Report Text The Duck Billed Platypus: (Ornithorhynchus Anatinus)Documento2 pagineReport Text The Duck Billed Platypus: (Ornithorhynchus Anatinus)Lilis IndriyaniNessuna valutazione finora
- Sheiko 13week Beginner ProgramDocumento16 pagineSheiko 13week Beginner ProgramAnders DahlNessuna valutazione finora
- Future Scope and ConclusionDocumento13 pagineFuture Scope and ConclusionGourab PalNessuna valutazione finora
- Itf EssayDocumento18 pagineItf EssayTharshiNessuna valutazione finora
- CongressWatch #197: RA 1337-Innovative Startup ActDocumento1 paginaCongressWatch #197: RA 1337-Innovative Startup ActMakati Business ClubNessuna valutazione finora
- List of ErpDocumento2 pagineList of Erpnavyug vidyapeeth trust mahadNessuna valutazione finora
- E650E650M-17 Guía Estándar para El Montaje de Sensores Piezoeléctricos de Emisión Acústica1Documento4 pagineE650E650M-17 Guía Estándar para El Montaje de Sensores Piezoeléctricos de Emisión Acústica1fredy lopezNessuna valutazione finora
- Educational Strategic Plans in Nigeria: Challenges of Implementation and Ways ForwardsDocumento7 pagineEducational Strategic Plans in Nigeria: Challenges of Implementation and Ways ForwardsresearchparksNessuna valutazione finora
- Pset 2Documento13 paginePset 2rishiko aquinoNessuna valutazione finora
- Historic Trial of Ali Brothers and Shankaracharya-1921Documento276 pagineHistoric Trial of Ali Brothers and Shankaracharya-1921Sampath Bulusu100% (3)
- Platos Apology SummaryDocumento3 paginePlatos Apology SummaryFMSANessuna valutazione finora
- CH 6 Answers (All) PDFDocumento29 pagineCH 6 Answers (All) PDFAhmed SideegNessuna valutazione finora
- M 3 Nceog 2Documento110 pagineM 3 Nceog 2Bharti SinghalNessuna valutazione finora
- Sap Business Objects Edge Series 3.1 Install Windows enDocumento104 pagineSap Business Objects Edge Series 3.1 Install Windows enGerardoNessuna valutazione finora
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- GundamDocumento25 pagineGundamBattlecruiser ScharnhorstNessuna valutazione finora
- Business English IDocumento8 pagineBusiness English ILarbi Ben TamaNessuna valutazione finora
- Optimizing Patient Flow: Innovation Series 2003Documento16 pagineOptimizing Patient Flow: Innovation Series 2003Jeff SavageNessuna valutazione finora
- UKAYUNIK Chapter 1 To 12Documento31 pagineUKAYUNIK Chapter 1 To 12Chiesa ArellanoNessuna valutazione finora
- Altium Designer Training For Schematic Capture and PCB EditingDocumento248 pagineAltium Designer Training For Schematic Capture and PCB EditingAntonio Dx80% (5)
- Pyrethroids April 11Documento15 paginePyrethroids April 11MadhumithaNessuna valutazione finora
- Course: Consumer Behaviour: Relaunching of Mecca Cola in PakistanDocumento10 pagineCourse: Consumer Behaviour: Relaunching of Mecca Cola in PakistanAnasAhmedNessuna valutazione finora
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedDa EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedValutazione: 5 su 5 stelle5/5 (81)
- The Obesity Code: Unlocking the Secrets of Weight LossDa EverandThe Obesity Code: Unlocking the Secrets of Weight LossValutazione: 4 su 5 stelle4/5 (6)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionDa EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionValutazione: 4 su 5 stelle4/5 (404)