Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Efficacy of Platelet Transfusions in Immune Thrombocytopenia
Caricato da
Fadel BilondatuDescrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Efficacy of Platelet Transfusions in Immune Thrombocytopenia
Caricato da
Fadel BilondatuCopyright:
Formati disponibili
Efficacy of Platelet Transfusions in Immune Thrombocytopenia
JUSTINE M. CARR, M.D.
MARGOT S. KRUSKALL, M.D.
JAMES A. KAYE, M.D.*
STEPHEN H. ROBINSON, M.D.
Boston, Massachusetts
Records of 11 patients with immune thrombocytopenia (idiopathic and
quinidine-induced) were evaluated retrospectively for response to
platelet transfusion. Good post-transfusion platelet count increments
occurred on one or more occasions in seven of the 11 patients, with 13
of 31 platelet transfusions (42 percent) resulting in immediate posttransfusion increments of 20,000/mm3 or more. Next-day platelet
counts remalned elevated in association with five of these 13 transfusions. This study demonstrates that, contrary to common opinion,
platelet transfusia
can raise the platelet count in many patients with
immune thrombocytopenia, and therefore may be beneficial in actively
bleeding or high-risk patients with this disorder.
Conflicting recommendations have been made regarding the role of
platelet transfusion in the management of immune thrombocytopenia.
Because of accelerated platelet destruction in patients with idiopathic
thrombocytopenic purpura, many authors have concluded that platelet
transfusions are either useless [ 1,2] or should be reserved for lifethreatening hemorrhage [3-91. Some authors have warned that platelet
transfusions could further lower the platelet count [3, IO] or cause severe
febrile reactions [l I]. In contrast, a few have encouraged the use of
platelet transfusions in patients with so-called wet purpura (gingival
bleeding, epistaxis, guaiac-positive stools, hematuria, or menorrhagia)
[ 12,131. However, clinical studies to resolve the usefulness of platelet
transfusions in immune thrombocytopenia have not been reported, and
documentation of patient response has been limited to individual case
descriptions [ 14,151.
We noted that house officers in our hospital were administering
platelet transfusions to many patients admitted to the hospital with
immune thrombocytopenia. This report is a retrospective analysis of the
response to platelet transfusion by these patients.
From the Departments
of Medicine
and Pathology, Beth Israel
Hospital
and Harvard
Medical
School, and the Charles
A. Dana Research
Institute, Beth Israel Hospital,
Boston,
Massachusetts. Dr. Carr is the recipient
of American
Cancer Society
Physicians
Research
Training
Fellowship PRTF 7. Requests
for reprints
should be
addressed
to Dr. Justine
M. Carr, Beth Israel
Hospital,
330 Brookline
Avenue,
Boston,
Massachusetts
02215.
Manuscript
accepted
April 12,
1985.
* Current address:
Dana Farber Cancer
Institute,
Boston,
Massachusetts
02 115.
PAllENTS AND METHODS
Patient Population. Records of all patients with immune thrombocytopenia, either idiopathic or quinidine-induced, with platelet counts of less than
20,000/mm3, who were admitted to Beth Israel Hospital and received
platelet transfusions between January 1981 and July 1984 were reviewed.
The diagnosis of idiopathic thrombocytopenic purpura was made in six
patients with a history of recent-onset thrombocytopenia, absence of
splenomegaly, adequate megakaryocytes without other abnormalities on
bone marrow examination, and no evidence of disseminated intravascular
coagulation, sepsis, microangiopathic hemolytic anemia, post-transfusion
purpura, or recent use of marrow-suppressive drugs. Five of the six patients (Patients 1, and 3 to 6) had antiplatelet antibody studies performed;
June 1986 The American Journal of
Medicine
Volume
80
1051
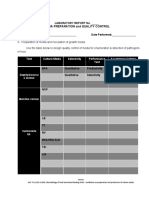
PLATELET
TABLE
TRANSFUSION
Clinical
Patient
1
2
3
4
5
8
Average
7
8
9
10
11
IN IMMUNE
Summary
Diagnosisof
Thrombocytopenia
Idiopathic
Idiopathic
Idiopathic
Idiopathic
Idiopathic
Idiopathic
Quinidine-induced
Quinidine-induced
Quinidine-induced
Quinidine-induced
Quinidine-induced
THROMBOCYTOPENIA-CARR
ET AL
of Patients
with immune
Age and Sex
Nadir Platelet
Count(per mm3)
82F
71F
27F
79M
43M
25M
55
88F
77F
74F
67F
70M
Thrombocytopenia
1,000
3,000
1,000
500
15,000
1,000
5,000
2,000
3,000
1,000
6,000
1,000
Bleeding*
Steroid
Therapy
Central nervous system hemorrhage?
Eljistaxis
Epistaxis
Eplstaxis
Central nervous system hemorrhagex
Epistaxis
i+
+
+
+
+
Upper gastrointestinal hemorrhage
Upper gastrointestinal hemorrhage
Epistaxis
None
Epistaxis
+
-
Average
75
2,600
* All patients also had petechiae and/or ecchymoses.
7 Subdural hematoma occurred after head trauma.
x Hemorrhage occurred in a previously undiagnosed brain stem subependymoma.
of Medicine
Volume
2.4
the immediate post-transfusion
recovery of platelets is approximately 70 percent, since 30 percent are sequestered
by the spleen [ 191.
RESULTS
Patient Population. Table I summarizes the clinical
data of the six patients with idiopathic thrombocytopenic
purpura and the five patients with quinidine purpura evaluated. Two patients in each group had serious hemorrhages during their period of thrombocytopenia, including
acute gastrointestinal bleeding requiring red cell transfusion (Patients 7 and 8) and hemorrhage into the central
nervous system (Patients 1 and 5). Six other patients had
epistaxis and petechiae; one (Patient 10) had petechiae
only.
Platelet Transfusions. All patients received a platelet
transfusion within seven hours of the admission platelet
count, and seven patients received transfusions on subsequent occasions during their hospitalization (Table I).
Platelet transfusions were given to these patients for a
variety of reasons, including frank bleeding, wet purpu;
ra, or, in some instances, as a diagnostic test, where it
was assumed that a good post-transfusion increment in
platelet count would be evidence against the diagnosis of
immune thrombocytopenia. Nineteen of the 31 platelet
transfusions were given to patients with idiopathic thrombocytopenic purpura, and 12 to patients with quinidineinduced thrombocytopenia. One or more post-transfusion
platelet counts were pet-formed after each transfusion.
Platelet transfusions were evaluated by calculating the
proportion of platelets found in the circulation after transfusion (the recovery), and the effect these platelets had on
103mm3/kg (females), and the number of platelets transJournal
afebrile, nonbleeding patient with a normal-sized spleen,
platelets transfused X 100 percent, where blood volume =
weight in kg X 72 X 103mm3/kg (males) or X 68 X
The American
or an estimate of 7.1 X lOi plateletd/unit
times the number
of units transfused for random-donor concentrates. In an
transfusion count per mm31 X blood volume)/number of
June 1986
4
3
5
1
5
1
3.2
6
2
1
fused was the precise bag count for singledonor products,
results of all tests were positive, as measured by the presence of immunoglobulin
and/or complement
on platelets
[ 16,171. The diagnosis of quinidine-induced
thrombocytopenia was made in five patients with a history of recent
quinidlne ingestion preceding
a sudden drop in platelet
count, no clinical or laboratory evidence for other causes of
acute thrombocytopenia,
and recovery of the platelet count
within 10 days of discontinuation
of the drug. Antiplatelet
antibodies were found in four of these five patients (Patients
8 to 11).
Platelet Transfusions.
Excluding transfusions given within 24 hours of a patients recovery from thrombocytopenia,
or during a septic episode in one patient, a total of 31
transfusions was evaluated. Patients received either random-donor, pooled platelet concentrates
(28 transfusions)
or singledonor
non-HLA-matched
platelets (three transfusions). Twenty-five of the 31 products were more than 24
hours old at the time of transfusion.
No febrile or other
transfusion reaction was reported.
Platelet Count increments
and Post-Transfusion
Platelet
Recoveries.
Absolute increments in platelet counts were
measured using the platelet count drawn one to five hours
after transfusion (the immediate count) and the platelet
count drawn 10 to 24 houis after transfusion (the next-day
count). Platelet counts were measured with a Coulter model
S-Plus for counts greater than 50,000/mm3, and with phase
microscopy for lower counts. In an afebrile, nonbleeding,
average-sized
adult patient with a normal-sized spleen, the
expected immediate count increment per unit of platelets
transfused is approximately
7,000/mm3 [ 181.
Post-transfusion
platelet recoveries were estimated using a formula that compares the number of platelets measurable after transfusion, using the immediate or next-day
count, with the number transfused, expressed as a percentage: Recovery = ([ post-transfirsion
count per mm3 - pre-
1052
Numberol
PlateletTransfusions
60
PLATELET
the patients platelet count (the increment). immediate
post-transfusion platelet increments and recoveries were
evaluable for 29 transfusions, the next-day values for 24
transfusions (Figure 1). For purposes of this analysis, a
platelet transfusion was considered successful (albeit
suboptimal) if it resulted in an increment of at least
20,000/mm3 in the platelet count or a recovery of at least
20 percent of the transfused platelets.
As shown in Figure 1, seven of the 11 patients in this
study (64 percent) received one or more successful platelet transfusions according to these criteria (four patients
with idiopathic thrombocytopenic purpura, three with
quinidine-induced thrombocytopenia). Thirteen of the 3 1
transfusions (42 percent) were associated with satisfactory immediate increments. Although platelet counts decreased rapidly thereafter, five of these 13 transfusions
(38 percent, or 16 percent of all transfusions) resulted in
persistently successful next-day increments, including
one to a patient with idiopathic thrombocytopenic purpura, and two to each of two patients with quinidine-induced
thrombocytopenia. With six transfusions, good post-transfusion increments were attained despite poor platelet
recoveries, due either to a large dose of platelets in some
transfusions (three 20-unit transfusions to Patient 7) or to
some patients small blood volumes (Patients 1 and 8). No
patient had a decrease in platelet count after platelet
transfusion. In two patients (Patients 7 and 8), successful platelet transfusions were temporally related to a
decrease or cessation of hemorrhage. In one other patient
(Patient 2), clinical improvement occurred despite a poor
post-transfusion platelet increment and recovery. In all
other patients, a clinical response either was not appreciated (Patients 1 and 5) or was not evaluable because
bleeding was minimal or absent.
TRANSFUSION
IN IMMUNE
THROMBOCYTOPENIA-CARR
ET AL
PATIENTS
Figure 1.
Post-transfusion
platelet increments (panel A)
and recoveries (panel s) using the immediate post-transfe
sion (one to five hours) platelet count (0) and the next day
( 10 to 24 hours) count (A). A single line connects counts
that refer to the same transfusion ( l -A).
Some transfu
sions were followed by only a single post-transfusion
count,
indicated by a symbol without a line. For purposes of anaiysis, an unavailable immediate post-transfusion
increment
and recovery after one transfusion to Patient 5 was as
sumed to be no lower than the next-day values, indicated by
-A.
Most transfusions consisted of 10 units of platelets.
Transfusions of other than 10 units are indicated by the
numbers in parentheses.
Points designating
successful
transfusions, as defined in the text, fall above the dashed
lines in each panel. ITP = idiopathic thrombocytopenic
purpura.
COMMENTS
The efficacy of platelet transfusion in immune thrombocytopenia is poorly documented in the literature. By chromium survival studies, both autologous and transfused platelets in idiopathic thrombocytopenic purpura have shottened survivals [20,21]. Several authors have stated,
without presenting clinical data, that little or no increase in
platelet count can be obtained in these settings [ 1,6,7,9],
although some note that hemostasis may be improved
after platelet transfusion [3,7-9,121. A few authors advocate prophylactic platelet transfusion in patients with wet
purpura due to idiopathic thrombocytopenic purpura or
quinidine-induced thrombocytopenia [ 12,131. However,
we could find only two case reports documenting satisfactory platelet count increments after transfusion in the
setting of immune thrombocytopenia, one in a patient with
idiopathic thrombocytopenic purpura [ 141 and the other in
a patient with quinidine-induced thrombocytopenia [ 151.
This study demonstrates that, contrary to what is often
taught, platelet transfusions increase the platelet count
immediately after transfusion in many patients with im-
mune thrombocytopenia, whether quinidine-induced or
idiopathic. In addition, in over one third of these successful transfusions, satisfactory platelet count elevations
are still observed the day after transfusion. The relative
success of transfusions in this retrospective study may
even have been underestimated. For example, platelet
counts may have been adversely affected by factors in
addition to immune destruction, including the age of the
June
1986
The American
Journal
of Medicine
Volume
60
1053
PLATELET
TRANSFUSION
IN IMMUNE
THROMBOCYTOPENIA-CARR
ET AL
platelet product at the time of transfusion (25 of 31
platelet products were more than 24 hours old) [22],
active bleeding during the transfusion (four transfusions),
and fever at the start of the transfusion (two transfusions).
Alloimmunization to transfused platelets may also have
played a role, since some patients had been pregnant or
had received blood products in the past. In one instance
(Patient 7), the relative success of platelet transfusion
was in part due to the large dose of platelets given in
several transfusions (20 units), which allowed for higher
post-transfusion platelet count increments despite the
often poor platelet recoveries. In addition, steroid therapy
may have played a role in the good transfusion increments
(four of seven transfusions) seen in this patient with
quinidine-induced thrombocytopenia, and in all the patients with idiopathic thrombocytopenic purpura, but this
patient population is too small to allow a firm conclusion
to be drawn about this point.
Our findings point to the fallacy of using a response to
platelet transfusion as evidence against the diagnosis of
immune thrombocytopenia, since two thirds of our patients with this otherwise well-documented diagnosis had
successful post-transfusion increments at some point
in their courses. Further, an unsuccessful platelet transfusion on one occasion was not necessarily predictive of
subsequent responses to transfusion. The variable re
sponse to platelets may have been due to the effect of
steroids, a fall in drug levels in patients with quinidineinduced thrombocytopenia, or a problem specific to individual transfusion products.
Although transfusions of platelets can raise the platelet
count in many patients with immune thrombocytopenia,
this finding should not be interpreted as meaning that
platelets should be given routinely to these patients. Pro
phylactic platelet transfusions have decreased morbidity
in patients with thrombocytopenia due to conditions of
marrow failure such as leukemia [23]; however, platelet
counts of 20,000/mm3 or less in patients with immune
thrombocytopenia are associated with much shorter
bleeding times than in patients with marrow failure, contributing to a reduced risk of bleeding [24]. Most patients
with immune thrombocytopenia do not experience major
hemorrhage even though they do not receive platelet
support. In addition, platelet concentrates carry the same
risks as other blood components, including alloimmunization to both red cells and platelets and transmission of
infection. On the other hand, this study demonstrates a
rational basis for the use of platelet transfusions in patients with immune thrombocytopenia and life-threatening
hemorrhage. Whether platelet transfusion may be a useful
prophylactic therapy in patients with immune thrombocytopenia who are judged to be at high risk for bleeding
is a question that should be addressed by a prospective
study.
REFERENCES
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
1054
Ahn YS, Harrington
WJ: Treatment
of idiopathic
thrombocytopenic
purpura.
Annu Rev Med 1977; 28: 299-309.
Huestis DW, Bove JR, Busch S: Practical
blood transfusion,
3rd ed. Boston:
Little Brown,
1981: 285-313.
Kelton JG, Gibbons
S: Autoimmune
platelet
destruction.
Semin Thromb
Hemost
1982; 8: 83-104.
Gardner
FH: Preservation
and clinical
use of platelets.
In:
Williams
WJ, Beutler
E. Erslev
AJ. Lichtman
MA. eds.
Hematology,.
3rd ed. New
York: McGraw-Hill,
i983;
1556-1563.
Slichter
SJ: Controversies
in platelet
transfusion
therapy.
Annu Rev Med 1980: 31: 509-540.
Menitove
JE, Aster RH:Transfusion
of platelets
and plasma.
Clin Haematol
1983; 12: 239-266.
Aisner
J: Platelet transfusion
therapy.
Med Clin North Am
1977; 61: 1133-I
145.
Baldini M: Idiopathic
thrombocytopenic
purpura.
N Engl J
Med 1966; 274: 1360-1367.
Lacey JV, Penner JA: Management
of idiopathic
thrombocytopenic
purpura in the adult. Semin Thromb Hemost
1977:
3:.IBO-i74.
Kelton JG, McDonald
JWD, Barr RM, et al: The reversible
binding of vinblastine
to platelets:
implications
for therapy. Blood 1981; 57: 431-436.
Becker GA, Aster RH: Platelet transfusion
therapy.
Med Clin
North Am 1982; 56: 81-94.
Crosby
WH: Wet purpura,
dry purpura.
JAMA
1975; 232:
744-745.
Kelton JG, Blajcham
MA: Platelet
transfusions.
Can Med
Assoc J 1979; 121: 1353-1358.
Abrahm J, Ellman L: Platelet transfusion
in immune thrombocytopenic
purpura
(letter). JAMA 1976; 236: 1847.
June
1988
The American
Journal
of Medicine
Volume
15.
16.
17.
18.
19.
20.
21.
22.
23.
24.
80
Moss RA, Castro
P: Platelet
transfusion
for quinidine-induced
thrombocytopenia.
N Engl J Med 1973;
288:
522-523.
Verheugt
FWA, Von Dem Borne AEGK, Van Noord-Bokhorst
JC, Engelfriet
CP: Autoimmune
granulocytopenia:
the detectionof
granulocyte
autoantibodies
with the immunofluorescence
test. Br J Haematol
1978: 39: 339-350.
Handin R, Stossel T: Phagocytosis
of antibody-coated
platelets by human granulocytes.
N Engl J Med 1974; 290:
989-993.
Schiffer
CA, Aisner J: Platelet and granulocyte
transfusion
therapy
for patients with cancer.
In: Petz LD, Swisher
SN,
eds. Clinical
practice
of blood transfusion.
New York:
Churchill-Livingstone,
1981: 551-572.
Kahn RA: Clinical
evaluation
of platelet
transfusions
in
thrombocytopenic
patients:
methods
and interpretation.
VOX Sang 1981; 4O(suppl
1): 87-97.
Najean Y, Ardaillou
N, Caen J, Larrieu MJ, Bernard J: Survival of radiochromium-labeled
platelets
in thrombocytopenia. Blood 1963; 22: 718-732.
Baldini M: Idiopathic
thrombocytopenic
purpura.
N Engl J
Med 1966; 272: 1245-1251.
Hester J, Stoldt R, Ayyar R, Freireich
E: Effects
of 24 hour
storage
of single donor platelet
concentrates
(SDPC) on
transfusion
response
(abstr).
Blood 1984; 64(suppl
1):
227a.
Murphy S, Litwin S, Herring LM, et al: Indications
for platelet
transfusion
in children
with acute leukemia.
Am J Hemato1 1982; 12: 347-356.
Harker LA, Slichter SJ: The bleeding time as a screening
test
for evaluating
platelet function.
N Engl J Med 1972; 287:
155-159.
Potrebbero piacerti anche
- Best Practices of Apheresis in Hematopoietic Cell TransplantationDa EverandBest Practices of Apheresis in Hematopoietic Cell TransplantationSyed A. AbutalibNessuna valutazione finora
- Transfusion of ABO-mismatched Platelets Leads To Early Platelet RefractorinessDocumento6 pagineTransfusion of ABO-mismatched Platelets Leads To Early Platelet Refractorinessmy accountNessuna valutazione finora
- Indications For Platelet Transfusion in Children With Acute LeukemiaDocumento10 pagineIndications For Platelet Transfusion in Children With Acute LeukemiaAbidi HichemNessuna valutazione finora
- How I Use Platelet TransfusionsDocumento12 pagineHow I Use Platelet TransfusionstheriversongsNessuna valutazione finora
- Immature Platelet Fraction Measured On The Sysmex XNeDocumento7 pagineImmature Platelet Fraction Measured On The Sysmex XNetuanbu164Nessuna valutazione finora
- How I Use Platelet TransfusionsDocumento12 pagineHow I Use Platelet TransfusionsJovanna OrtuñoNessuna valutazione finora
- Blood - BLD 2022 016558 C MainDocumento12 pagineBlood - BLD 2022 016558 C MaincnshematologiaNessuna valutazione finora
- How I Use Platelet Transfusions - Blood 2022Documento12 pagineHow I Use Platelet Transfusions - Blood 2022Jessica FloresNessuna valutazione finora
- Advances 017699Documento9 pagineAdvances 017699Danang Bagus UntoroNessuna valutazione finora
- Algoritmo de Transfusion en Pacientes CardiologicosDocumento8 pagineAlgoritmo de Transfusion en Pacientes CardiologicosLyonTrioréNessuna valutazione finora
- Briggs2006 PDFDocumento10 pagineBriggs2006 PDFRonal WinterNessuna valutazione finora
- Blood in TraumaDocumento17 pagineBlood in TraumaEmtha SeeniNessuna valutazione finora
- 862 FullDocumento3 pagine862 FullFadel BilondatuNessuna valutazione finora
- Massive Transfusion ProtocolDocumento11 pagineMassive Transfusion ProtocolAlaa Abdelmoaty OmranNessuna valutazione finora
- The Misunderstood Coagulopathy of Liver Disease - WJM 2018Documento9 pagineThe Misunderstood Coagulopathy of Liver Disease - WJM 2018J doeNessuna valutazione finora
- Bloodproducttransfusions Andreactions: Jessica L. Osterman,, Sanjay AroraDocumento12 pagineBloodproducttransfusions Andreactions: Jessica L. Osterman,, Sanjay AroraAdi ParamarthaNessuna valutazione finora
- NIH Public Access: Author ManuscriptDocumento20 pagineNIH Public Access: Author ManuscriptSantiago PilataxiNessuna valutazione finora
- Platelet Transfusion: A Clinical Practice Guideline From The AABB FreeDocumento6 paginePlatelet Transfusion: A Clinical Practice Guideline From The AABB FreeUJI MUTUNessuna valutazione finora
- Activity No 2 ImmunohematologyDocumento3 pagineActivity No 2 ImmunohematologyAegina FestinNessuna valutazione finora
- Seminario 13 2014 PDFDocumento8 pagineSeminario 13 2014 PDFJuan Jose PereiraNessuna valutazione finora
- Yagmur Et Al 2013 Platelet Hyperaggregability Is Highly Prevalent in Patients With Chronic Kidney Disease AnDocumento7 pagineYagmur Et Al 2013 Platelet Hyperaggregability Is Highly Prevalent in Patients With Chronic Kidney Disease AnMister FannaniNessuna valutazione finora
- Chest Masive TransfDocumento16 pagineChest Masive TransfMacario Ismael Chavez CutzNessuna valutazione finora
- Risk Factors For Intraoperative Massive Transfusion in Pediatric Liver Transplantation: A Multivariate AnalysisDocumento8 pagineRisk Factors For Intraoperative Massive Transfusion in Pediatric Liver Transplantation: A Multivariate AnalysisSanti ParambangNessuna valutazione finora
- 5.6 TransfusionDocumento2 pagine5.6 TransfusionamandajaeNessuna valutazione finora
- Thrombocytopenia in Chronic Liver Disease: Lessons From Transplanted PatientsDocumento5 pagineThrombocytopenia in Chronic Liver Disease: Lessons From Transplanted PatientsElena CuibanNessuna valutazione finora
- Blood Transfusion in Critical Care: Giora Netzer, Richard P Dutton and John R HessDocumento3 pagineBlood Transfusion in Critical Care: Giora Netzer, Richard P Dutton and John R Hessnevermore11Nessuna valutazione finora
- Arteriovenous Thrombosis in Chronic Renal Failure Patients Receiving Renal Replacement TherapyDocumento6 pagineArteriovenous Thrombosis in Chronic Renal Failure Patients Receiving Renal Replacement TherapyMaya RustamNessuna valutazione finora
- Addison K May, MD John P Reilly, MD, Msce Scott Manaker, MD, PHD Arthur J Silvergleid, MD Geraldine Finlay, MD Contributor DisclosuresDocumento12 pagineAddison K May, MD John P Reilly, MD, Msce Scott Manaker, MD, PHD Arthur J Silvergleid, MD Geraldine Finlay, MD Contributor DisclosuresAlvaro HaroNessuna valutazione finora
- A Prospective Study To CorrelateDocumento6 pagineA Prospective Study To Correlateelaaannabi1Nessuna valutazione finora
- Platelet Transfusion TherapyDocumento3 paginePlatelet Transfusion TherapydrrdchauhanNessuna valutazione finora
- TransfusiDocumento10 pagineTransfusiDevia PebriyentiNessuna valutazione finora
- HP94 04 PredictingDocumento8 pagineHP94 04 PredictingSa 'ng WijayaNessuna valutazione finora
- Embolizare Splenica PartialaDocumento5 pagineEmbolizare Splenica PartialaElena CuibanNessuna valutazione finora
- Stationary Versus Agitated Storage of Whole Blood.6 PDFDocumento5 pagineStationary Versus Agitated Storage of Whole Blood.6 PDFAngel CallesNessuna valutazione finora
- Emboli ParuDocumento10 pagineEmboli Paruindry_purnamasariNessuna valutazione finora
- Blood Product Replacement For Postpartum HemorrhageDocumento13 pagineBlood Product Replacement For Postpartum HemorrhageEvelyn Yanet Facho BautistaNessuna valutazione finora
- CMQCC - Transfusion in Obstetric HemorrhageDocumento10 pagineCMQCC - Transfusion in Obstetric HemorrhageBerri RahmadhoniNessuna valutazione finora
- Jama Neal 2023 Ed 230070 1696973944.14124Documento2 pagineJama Neal 2023 Ed 230070 1696973944.14124Luz Elena ValderramaNessuna valutazione finora
- Management of Adult Patients With Persistent Idiopathic Thrombocytopenic Purpura Following Splenectomy - A Systematic Review - PDocumento2 pagineManagement of Adult Patients With Persistent Idiopathic Thrombocytopenic Purpura Following Splenectomy - A Systematic Review - PSimona Persida Fulgeanu SoficaruNessuna valutazione finora
- Eppley 2004 GF in PRP Using GPS SystemDocumento7 pagineEppley 2004 GF in PRP Using GPS SystemViviane KaramNessuna valutazione finora
- Massive Tranfusion Protocol: Oleh ErtigaDocumento13 pagineMassive Tranfusion Protocol: Oleh ErtigaAnonymous BQM9271ZXNessuna valutazione finora
- Frank 2019Documento15 pagineFrank 2019Oliver ArteagaNessuna valutazione finora
- Postpartum Hemorrhage With A Standardized Massive Transfusion ProtocolDocumento9 paginePostpartum Hemorrhage With A Standardized Massive Transfusion Protocolmedicinaun74100% (2)
- Survival After Transarterial Embolization For Spontaneous Ruptured Hepatocellular CarcinomaDocumento5 pagineSurvival After Transarterial Embolization For Spontaneous Ruptured Hepatocellular CarcinomaRollin SidaurukNessuna valutazione finora
- Heparin-Induced Thrombocytopenia,: Thrombosis, and HemorrhageDocumento5 pagineHeparin-Induced Thrombocytopenia,: Thrombosis, and HemorrhageAchmad HafirulNessuna valutazione finora
- Review of Current Transfusion Therapy and Blood Banking PracticesDocumento52 pagineReview of Current Transfusion Therapy and Blood Banking PracticesAmaranto SantosoNessuna valutazione finora
- Misra 2012Documento7 pagineMisra 2012Carlos RiquelmeNessuna valutazione finora
- Kjg066 02 06Documento8 pagineKjg066 02 06Nguyễn PhúcNessuna valutazione finora
- General: Anaemia & Blood Cell Transfusion in Critical IllnessDocumento1 paginaGeneral: Anaemia & Blood Cell Transfusion in Critical IllnessOlfiany Laurenzia PongohNessuna valutazione finora
- Article in Press: Age of Blood and Survival After Massive TransfusionDocumento5 pagineArticle in Press: Age of Blood and Survival After Massive TransfusionJosé BlasNessuna valutazione finora
- Cost-Effectiveness of Blood Transfusion and White Cell Reduction in Elective Colorectal SurgeryDocumento4 pagineCost-Effectiveness of Blood Transfusion and White Cell Reduction in Elective Colorectal Surgerymy accountNessuna valutazione finora
- Plasma Exchange For Heparin-Induced Thrombocytopenia: Is There Enough Evidence?Documento4 paginePlasma Exchange For Heparin-Induced Thrombocytopenia: Is There Enough Evidence?sayednourNessuna valutazione finora
- Curley 2018 Platelet Transfusion Threshols in NeonatesDocumento11 pagineCurley 2018 Platelet Transfusion Threshols in NeonatesEllya Latifah IlyasNessuna valutazione finora
- J Jamcollsurg 2013 01 004Documento8 pagineJ Jamcollsurg 2013 01 004Wanjak ChawaponchaiNessuna valutazione finora
- Jeffrey L Carson Restrictive or Liberal TransfusionDocumento11 pagineJeffrey L Carson Restrictive or Liberal Transfusionmiguel aghelNessuna valutazione finora
- 3144.full MoyamoyaDocumento8 pagine3144.full MoyamoyaDarren ZytkiewiczNessuna valutazione finora
- Platelet Count in Predicting Bleeding Complication After Elective Endoscopy in Children With Portal Hypertension and ThrombocytopeniaDocumento4 paginePlatelet Count in Predicting Bleeding Complication After Elective Endoscopy in Children With Portal Hypertension and ThrombocytopeniaMasri YaniNessuna valutazione finora
- Bloody Easy PDFDocumento164 pagineBloody Easy PDFJenny JeongNessuna valutazione finora
- Bloodbook 2017 660 PDFDocumento7 pagineBloodbook 2017 660 PDFSambit DashNessuna valutazione finora
- Annsurg00185 0122Documento6 pagineAnnsurg00185 0122Fajr MuzammilNessuna valutazione finora
- Acid-Base Tutorial - Strong Ion DifferenceDocumento3 pagineAcid-Base Tutorial - Strong Ion DifferenceFadel BilondatuNessuna valutazione finora
- 4-2-3-1 Wide ,, Gatling Project ,, The Invicible ,, 142 Goals in League - (Update)Documento8 pagine4-2-3-1 Wide ,, Gatling Project ,, The Invicible ,, 142 Goals in League - (Update)Fadel BilondatuNessuna valutazione finora
- 14 Artikel MetaDocumento6 pagine14 Artikel MetaFadel BilondatuNessuna valutazione finora
- 862 FullDocumento3 pagine862 FullFadel BilondatuNessuna valutazione finora
- Comprehensive Pediatric NephrologyDocumento3 pagineComprehensive Pediatric NephrologyFadel BilondatuNessuna valutazione finora
- Symptoms and Diagnosis - ADHD - NCBDDD - CDCDocumento4 pagineSymptoms and Diagnosis - ADHD - NCBDDD - CDCFadel BilondatuNessuna valutazione finora
- WHO Immunologic Classification For HIVDocumento1 paginaWHO Immunologic Classification For HIVFadel BilondatuNessuna valutazione finora
- Ucm 439476Documento1 paginaUcm 439476Fadel BilondatuNessuna valutazione finora
- Disinfectants: Exercise 4Documento11 pagineDisinfectants: Exercise 4Jake GerolagaNessuna valutazione finora
- StreptococciDocumento91 pagineStreptococciDr. Ashish JawarkarNessuna valutazione finora
- STR 2.4 - Specific Technical Requirements For Accreditation of Haematology LaboratoriesDocumento16 pagineSTR 2.4 - Specific Technical Requirements For Accreditation of Haematology LaboratoriesTauke SengNessuna valutazione finora
- Unit 5 Module 12 CombinedDocumento9 pagineUnit 5 Module 12 Combinedapi-293001217Nessuna valutazione finora
- Isolation of Pure CultureDocumento7 pagineIsolation of Pure CultureVignesh ReddyNessuna valutazione finora
- Study of Illness Condition: Assessment Organ Involved Normal Function Pathophysiology AnalysisDocumento2 pagineStudy of Illness Condition: Assessment Organ Involved Normal Function Pathophysiology Analysisahmad ryanNessuna valutazione finora
- Steps in Viral Pathogenesis-Lecture ThreeDocumento3 pagineSteps in Viral Pathogenesis-Lecture ThreeIM CTNessuna valutazione finora
- Rocky Mountain Spotted Fever: Breeana Bardill Microbiology 429 LabDocumento22 pagineRocky Mountain Spotted Fever: Breeana Bardill Microbiology 429 LabbNessuna valutazione finora
- MLT ValidationDocumento3 pagineMLT Validationdeepanmb007100% (1)
- Streptococci and Enterococci and OthersDocumento11 pagineStreptococci and Enterococci and OthersthedarkwingNessuna valutazione finora
- Culture Characteristics of Common OrganismsDocumento5 pagineCulture Characteristics of Common OrganismssaketNessuna valutazione finora
- Probiotics in AquacultureDocumento7 pagineProbiotics in AquaculturemoiNessuna valutazione finora
- Nosocomial Infections in Pediatric Intensive Care UnitDocumento6 pagineNosocomial Infections in Pediatric Intensive Care UnitEditor IJTSRDNessuna valutazione finora
- Media Preparation and Quality ControlDocumento3 pagineMedia Preparation and Quality ControlclairealbertiniNessuna valutazione finora
- Controlling Microbial Growth in Vivo Using Antimicrobial AgentsDocumento30 pagineControlling Microbial Growth in Vivo Using Antimicrobial AgentsJen PanganibanNessuna valutazione finora
- Introduction To MicrobiologyDocumento55 pagineIntroduction To Microbiologymeldestacamentojr100% (3)
- Bacterial Contamination of Multiple-DoseDocumento5 pagineBacterial Contamination of Multiple-DoseMuhammad HabibieNessuna valutazione finora
- DarahDocumento14 pagineDarahChristantya VitaNessuna valutazione finora
- Foundations in Microbiology: TalaroDocumento71 pagineFoundations in Microbiology: Talaromertx013Nessuna valutazione finora
- Industrial Importance of MicrobesDocumento23 pagineIndustrial Importance of MicrobesDiah AyuningrumNessuna valutazione finora
- Prompt Inoculation System-D-3251-3000 PDFDocumento40 paginePrompt Inoculation System-D-3251-3000 PDFbogdan.tomosNessuna valutazione finora
- Multiple AllelesDocumento14 pagineMultiple AllelesSabs100% (2)
- Group 6 Blood Analysis 2Documento6 pagineGroup 6 Blood Analysis 2Kim TangoNessuna valutazione finora
- Lab 5 Coombs TestsDocumento26 pagineLab 5 Coombs TestsJennifer DixonNessuna valutazione finora
- DR Zalina - Trafusion Reaction and Management PDFDocumento77 pagineDR Zalina - Trafusion Reaction and Management PDFvasu_5iveNessuna valutazione finora
- SPREad PlateDocumento7 pagineSPREad PlateJermeLou BaoNessuna valutazione finora
- Immunohematology & Transfusion Medicine FinalDocumento33 pagineImmunohematology & Transfusion Medicine FinalCollen Mae Silos Diapues100% (1)
- Test Report: Complete Blood Count (CBC)Documento3 pagineTest Report: Complete Blood Count (CBC)WSC ALMANessuna valutazione finora
- Use This Form BLANK Blood Monitoring Report From RVBSPDocumento21 pagineUse This Form BLANK Blood Monitoring Report From RVBSPBadjoy Arcilla Dollente-ParialNessuna valutazione finora
- Study of Drug Resistance in Bacteria Using AntibiotiDocumento10 pagineStudy of Drug Resistance in Bacteria Using AntibiotiAshwin Rockzz75% (4)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedDa EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedValutazione: 4.5 su 5 stelle4.5/5 (82)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDDa EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDValutazione: 5 su 5 stelle5/5 (4)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionDa EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionValutazione: 4 su 5 stelle4/5 (404)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Da EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Valutazione: 3 su 5 stelle3/5 (1)
- The Age of Magical Overthinking: Notes on Modern IrrationalityDa EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityValutazione: 4 su 5 stelle4/5 (35)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsDa EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNessuna valutazione finora
- The Twentysomething Treatment: A Revolutionary Remedy for an Uncertain AgeDa EverandThe Twentysomething Treatment: A Revolutionary Remedy for an Uncertain AgeValutazione: 4.5 su 5 stelle4.5/5 (2)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsDa EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsValutazione: 4 su 5 stelle4/5 (5)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeDa EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeValutazione: 2 su 5 stelle2/5 (1)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Da EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Valutazione: 4.5 su 5 stelle4.5/5 (110)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryDa EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryValutazione: 4 su 5 stelle4/5 (46)
- The Obesity Code: Unlocking the Secrets of Weight LossDa EverandThe Obesity Code: Unlocking the Secrets of Weight LossValutazione: 4 su 5 stelle4/5 (6)
- To Explain the World: The Discovery of Modern ScienceDa EverandTo Explain the World: The Discovery of Modern ScienceValutazione: 3.5 su 5 stelle3.5/5 (51)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsDa EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsValutazione: 4.5 su 5 stelle4.5/5 (170)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaDa EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsDa EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsNessuna valutazione finora
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeDa EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeValutazione: 4.5 su 5 stelle4.5/5 (254)
- Critical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsDa EverandCritical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsValutazione: 4.5 su 5 stelle4.5/5 (39)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisDa EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisValutazione: 5 su 5 stelle5/5 (8)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsDa EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsValutazione: 5 su 5 stelle5/5 (1)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesDa EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesValutazione: 4.5 su 5 stelle4.5/5 (1412)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisDa EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisValutazione: 4.5 su 5 stelle4.5/5 (44)