Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Deep Neck Spaces Infections in Radiology
Caricato da
Anonymous 5m6DRjwCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Deep Neck Spaces Infections in Radiology
Caricato da
Anonymous 5m6DRjwCopyright:
Formati disponibili
ORIGINAL ARTICLE
Deep Neck Spaces radiology and review of deep neck infections at King
Abdulaziz University Hospital
Khaled Al-Nourya, Alsaid Lotfyb
Otolaryngology Departmenta, King Abdulaziz University, Jeddah, Saudi Arabia
Radiology Departmentb, International Medical Centre, Jeddah, Saudi Arabia
Abstract
The anatomy of the deep neck spaces is a complex one, and deep neck infections are a common clinical problem in all
age groups. Otolaryngologists should be familiar with the detailed anatomy and divisions of the neck in order to properly
diagnose and treat patients. Thus, knowledge of the radiological anatomy is paramount for accurately localizing and
evaluating the extent of the deep neck inflammatory processes. In this study, we present the anatomy of normal deep neck
spaces in computerized tomography and magnetic resonance images. The computerized tomography images of 56 patients
that presented with symptoms indicative of deep neck infections were also reviewed to illustrate the different patterns of
neck infections and their relationship with thoracic abnormalities. Because of the frequent thoracic abnormalities associated
with neck infections, we recommend performing a CT scan of chest in the same sitting with the CT of neck and absence
of ring enhancement does not exclude the presence of abscess
Key words: infection, tomography and magnetic resonance
Introduction
nfection of the neck is a common clinical
problem in all age groups, especially among children and
young adults13. Imaging studies that use computerized
tomography (CT) and magnetic resonance imaging (MRI)
are frequently required to confirm a diagnosis and, more
importantly, to localize the infectious process and to
delineate an abscessed cavity. Hence, knowledge of the
anatomy is paramount for localizing and evaluating the
extent of the inflammatory process47.
Neck infections can be categorized as either deep(i.e.,
intrinsic) or extrinsic810. Intrinsic infections include
Ludwigs angina, peritonsillar, parapharyngeal, and
retropharyngeal inflammation, while extrinsic infections
comprise cervical adenitis and submandibular, submental,
and masticator space infections . The causative organisms
of neck infections such as lymphadenitis are varied but
can be subdivided into bacterial, fungal, parasitic, or viral.
Unfortunately, if the treatment of a neck infection is
delayed or inadequate, mediastinal extension may ensue
and result in pain, dyspnea, asphyxia secondary to
aspiration, swelling with mediastinal widening, and
dysphagia from esophageal compression11.
The source of neck infections is unknown in up to
50% of cases. Known source are mainly extrinsic such
EJENTAS Egyptian Journal of ear, nose, throat and Allied Sciences
69
as infections. Some neck infections result from suppurative
adenitis, with the primary infection often originating from
the mucosa of the oral cavity, paranasal sinuses, and
pharynx. Dental caries and periodontal disease of the teeth
are other sources frequently implicated in deep neck
infection12,13 .
Neck Anatomy
A. Fascial Layers in the Neck
The fascial layers in the neck are either superficial or
deep. The superficial fascia lies just below the subcutaneous
tissue and envelopes the platysma muscle. The deep fascial
layers comprise the investing, visceral, and prevertebral
fasciae 1 4 .The investing fascia envelopes the
sternocleidomastoid and trapezius muscles and divides to
form the capsules of the submandibular and parotid glands
(Figure 1). Both the superficial fascia and the investing
layer surround the entire neck14. The visceral (pretracheal)
fascia forms a circle in the center of the anterior neck
(Figure 2). Within its bounds are the pharynx, trachea,
esophagus, and thyroid and parathyroid glands. Posteriorly,
the visceral fascia lies between the esophagus and the
vertebral bodies. Anteriorly, the visceral fascia divides to
form the capsule of the thyroid gland14.The prevertebral
fascia encircles the spine and the paraspinal muscles
(Figure 3). Anterior to the vertebral bodies, the prevertebral
fascia divides into 2 layers: (a) the alar fascia (anterior)
and (b) the true prevertebral fascia (posterior). Between
the alar and true prevertebral fasciae is the important
danger space that is involved in the spread of infection14.
Volume 11, December 2010
Deep Neck Spaces radiology and review of deep neck infections, Al-Noury & Lotfy
The carotid sheath is formed with contributions from
all 3 layers of the deep cervical fascia. The sheath surrounds
the common carotid artery, internal jugular vein, and
vagus nerve. When the common carotid artery divides
into the internal and external branches, the external carotid
artery leaves the carotid sheath, and the internal carotid
artery continues within the sheath to the base of the skull.
The infrahyoid fascia, formed with contributions from the
investing and visceral layers of the deep cervical fascia,
surrounds the strap muscles14.
Figure 4: Axial CT image of the submandibular space, as
outlined in red.
Figure 1: Axial MRI T1WI (A) and CT (B) images of the
investing fascia, as outlined in red.
Figure 2: Axial MRI T1 WI (A) and CT (B) images of the
visceral fascia, as outlined in red.
Figure 3: Axial MRT1 WI (A) and CT images (B) of the
prevertebral fascia, as outlined in red.
B. Neck Spaces
The cervical fascia divides the neck into several distinct
compartments (spaces). One should be aware of these
spaces and their defining landmarks, not only because
they affect the spread of infection, but also because they
influence the differential diagnosis of pathologic
findings15,16.
EJENTAS Egyptian Journal of ear, nose, throat and Allied Sciences
70
The submandibular space corresponds to the submental
and submandibular triangles. The roof of the submandibular
space is the mylohyoid muscle (Figure 4). The structures
within the visceral fascia are said to be in the visceral
space (Figure 5). The larynx, trachea, esophagus, thyroid
gland, and parathyroid glands are included in the visceral
space. Structures within the prevertebral fascia, including
the spine, the paraspinal muscles, the vertebral artery, and
the phrenic nerve, are in the prevertebal space (Figure 6).
The tissues between the pharynx and the vertebral column
are often grouped together as the retropharyngeal space.
There are, in actuality, 4 distinct spaces between the
pharynx (or esophagus) and the vertebral bodies. From
anterior to posterior, they are (1) the visceral space, (2)
the true retropharyngeal space, (3) the danger space, and
the (4) prevertebral space. The true retropharyngeal space
lies between the visceral fascia and the alar fascia. The
retropharyngeal lymph nodes are located within the true
retropharyngeal space (Figure 7) . The danger space lies
between the alar fascia and the true prevertebral fascia,
extending from the skull base to the diaphragm. The
danger space is so termed because infections can spread
vertically along the entire length of the neck and torso17.
Figure 5: Axial CT image of the visceral space, as outlined in red.
The parapharyngeal space lies between the layers of
the deep cervical fascia, with the pharynx medial, the
carotid sheath posterior, and the parotid gland lateral. The
styloid process of the temporal bone, along with its
associated muscles and ligaments, divides the
parapharyngeal space into the prestyloid and neurovascular
compartments.
Volume 11, December 2010
Deep Neck Spaces radiology and review of deep neck infections, Al-Noury & Lotfy
The prestyloid parapharyngeal space contains fat and
extends only to the level of the hyoid bone. The
neurovascular space corresponds to the carotid sheath and
extends the length of the neck (Figure 8).
Figure 9: Spinal accessory lymph nodes in the posterior cervical
space (indicated by the arrow)
Figure 6: Axial CT image of the prevertebral space, as outlined in red.
Figure 7: Axial CT scan of a patient with nasopharyngeal cancer
(indicated by the short, blue arrow) and a retropharyngeal lymph
node within the true retropharyngeal space (long, red arrow)
Patients and Methods
We reviewed the CT images of patients that presented
to our department from January 2001 through March 2008
because of suspected neck infections. For all of these
patients, a study of the neck and chest had been performed
using both multislice CT 4 slices (General Electric
Lightspeed) and 16 slices (Siemens Sensation). For each
patient, 100 cm3 of 300 mg/ml non-ionic contrast material
was intravenously administrated at a rate of 3.5 cm3/s.
The medical records of the patients were reviewed
following the approval of the hospital ethics committee.
The CT images were reviewed for:
1.The neck spaces involved
2.Abnormalities in the neck lymph nodes
3.Presence of ring enhancing lesions
4.Presence of air pockets
5.Mediastinal extensions
6.Parenchymal lesions in the lungs
7.Pleural effusions
8.Mediastinal lymph nodes
9.Chest wall abnormalities
Results
Fifty-six patients (38 males and 18 females) were
included in our study. The mean age was 43.3 years. The
youngest individual was 2 years of age and had HIV, and
the oldest individual was 73 years old. Twenty patients
(35.7 %) had diabetes mellitus, 4 had HIV (7.1 %), 2 (3.6
%) were infected with a branchial cleft cyst, and 6 (10.7
%) had underlying dental problems.
Figure 8: Axial CT image of the parapharyngeal space, as outined in red.
Below the level of the hyoid bone, there are fatfilled spaces anterior and posterior to the carotid sheath.
These are the anterior and posterior cervical spaces. The
posterior cervical space corresponds to the posterior
triangle and contains the spinal accessory and dorsal
scapular nerves, along with the spinal accessory lymph
node chain (Figure 9).
EJENTAS Egyptian Journal of ear, nose, throat and Allied Sciences
71
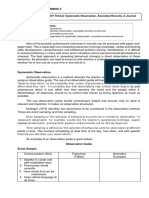
The anatomical space
Peritonsillar
Submandibular
Parapharyngeal
Retropharyngeal
Sublingual
Anterior cervical
Posterior cervical
Parotid space
Number of patients
24
14
14
8
4
8
2
2
Table 1: The neck spaces involved in infection as determined by CT.
Volume 11, December 2010
Deep Neck Spaces radiology and review of deep neck infections, Al-Noury & Lotfy
Figure 10: Axial CT images of a patient with an infected second
branchial cyst extending to the mediastinum (indicated by the
red arrows)
2 patients (3.7 %) had mediastinal (right hilar) lymph
nodal enlargement.
4 patients (7.6 %) had multiple chest wall abscesses.
8 patients (14.3 %) had a pleural effusion.
The most common organisms isolated in the pyogenic
infections were Staphylococcus aureus (14 patients, 25
%) and Klebsiella pneumoniae (8 patients, 14.3 %).
Mycobacterium TB was the source of the infection in
24 patients (42.9 %).
None of our patients (0 %) had jugular vein thrombosis.
2 patients had a large, infected branchial cleft cyst that
extended inferiorly to the mediastinum (Figure 10).
4 patients (7.1 %) had Ludwigs angina (Figure 11).
6 patients (10.7 %) had necrotizing fasciitis (Figure 12).
Discussion
Figure 11: Axial CT of patient with Ludwigs angina.
Figure 12: Axial CT of patient with necrotizing fasciitis and
thickening of skin subcutaneous tissues and muscles. Small
submental lymph nodes (arrows) and air pockets in several neck
spaces are also observed (circle).
The spaces of neck involved, as determined by CT, were
as follows (Table 1): Lymph nodal abnormalities were identified in 36 patients
(32 %). These abnormalities were in the form of:
1.Enlargement (using a 1.5 short axis diameter as the
limit in all levels)
2.Abnormal enhancement (significant or ring
enhancement)
3.Central hypodensity
Ring enhanced fluid collections were found in 30 patients
(53.6 %).
Air pockets were detected in 20 patients (35.7 %).
4 patients with air pockets (7.1 %) and without ring
enhancement were shown to have pus during needle
aspiration.
12 patients (21.4 %) had mediastinal extensions in the
form of mediastinal ring enhancing lesions or air pockets.
4 patients (7.1 %) had lung parenchymal changes in the
form of lung abscess and infiltrations.
EJENTAS Egyptian Journal of ear, nose, throat and Allied Sciences
72
The chief modality for the evaluation of a neck infection
is contrast helical CT carried out in the axial plane. 32
out of the 56 patients (57%) in our study were diabetic (n
= 20), had HIV (n = 4), suffered from dental problems (n
= 6), or had a preexisting pathology (n = 2) that consisted
of a large branchial cyst extending into the mediastinum.
We believe that these factors played a predisposing role
in the neck infections for this group of patients. In support
of dental problems playing a role in causing infection,
Chowdhury et al and Kim et al have found that dental
caries and periodontal disease of the teeth are frequently
implicated in deep neck infections12, 13.
In our study, the most frequently infected neck space
was the peritonsillar space (n = 24) (42.9%), followed by
the parapharyngeal (n = 14) (25%) and the submandibular
(n = 14) (25%) spaces. Consistent with these findings, in
a large study that included 184 patients with deep neck
infections, Wang et al, found that the neck spaces most
frequently involved in infection were the parapharyngeal
(n = 77) (41.9%), peritonsillar (n = 59) (32.1%) and
submandibular (n = 55) (29.9%) spaces18. In another
retrospective study that included 117 children, Ungkanont
et al.found the most frequent neck space involved was
the peritonsillar space (49%), followed by the
retropharyngeal space (22%), the submandibular space
(14%), the buccal space (11%), and the parapharyngeal
space, indicating that children may differ from adults in
their susceptibility to different types of infections1. In our
study, the only child (below 16 years of age) was a 2 year
old, HIV-positive male with a diffuse infective process
and early abscess formation in the submandibular region.
Based on its presence, Mycobacterium tuberculosis was
presumed to be the causative agent.
Retropharyngeal space infections were historically
believed to occur almost exclusively in children less than
6 years of age19. However, with the increase in the
immunocompromised patient population, these infections
have become more frequent in adults, occurring more
commonly in males than in females (2:1) . In our study,
all the patients that had retropharyngeal space infection
were adults (n = 8). In conformity with the general
population ratio, 6 male patients and 2 female patient had
this type of infection. The neck space infections were
either peritonsillar (n = 6) or parapharyngeal (n = 2).
Patients with retropharyngeal space infections often present
with fever, chills, odynophagia, sore throat, dysphagia,
Volume 11, December 2010
Deep Neck Spaces radiology and review of deep neck infections, Al-Noury & Lotfy
nausea, vomiting, respiratory distress, neck pain, and
stiffness. Interestingly, however, in perhaps the first known
case in our department, one of these patients presented
because of odynophagia, dysphagia, nausea and vomiting.
In the first study, we had him swallow barium and then
performed a CT of his neck and chest hence, in the absence
of signs of infections, barium swallow can help to delineate
the infectious process in the retropharyngeal neck space.
The danger point for the spreading of infection is the
space situated dorsal to the retropharyngeal space between
the alar and prevertebral fascia . This space extends from
the skull base to the level of the posterior diaphragm.
Infections that involve the retropharyngeal space may enter
the danger space and thus extend into the mediastinum.
In our study, 12 patients (21.4%) had mediastinal
extensions of the infectious process: 6 from retropharyngeal
space infection and 6 from anterior cervical space infection.
In addition, suppurative uncontrolled infection of the
tonsils may result in a peritonsillar abscess (quinsy) or
rarely in a tonsillar abscess. A peritonsillar abscess is an
accumulation of pus around the palatine tonsils. If this
abscess extends outside the tonsillar fossa, it may involve
the lateral retropharyngeal or parapharyngeal spaces . In
our study, out of 24 patients with a peritonsillar infection,
6 had retropharyngeal extension and 10 had parapharyngeal
extension.
Tuberculosis of the head and neck can involve the
cervical lymph nodes, larynx, temporal bone, sinonasal
cavity, eye, pharynx, thyroid gland, and skull base20. TB
is a rare cause of cervical lymphadenopathy in children
in the United States and is largely seen in children with
AIDS21.The only child included in our study was an AIDS
patient and had a diffuse neck infection and an enhanced
lymph node with central hypodensity. He was shown to
have TB. The other patient with AIDS in our study also
had a TB neck abscess. Other patients with TB in our
study (n = 20) had chest wall abscesses (n = 4), mediastinal
lymph nodes (n = 2), lung abscesses (n = 2) and pleural
effusion (n = 4).
The presence of thoracic manifestations with a neck
infection in our study was a clear finding. Out of the 56
patients, 20 (35.7%) had one or more of the following:
Mediastinal lesions as ring enhancing lesions or air pockets
(n = 4)
Lung abscess or infiltrations (n = 4)
Mediastinal lymphadenopathy (n = 2)
Chest wall abscesses (n = 4)
Bilateral or unilateral pleural effusion (n = 8)
We assumed that mediastinal lesions were basically
due to extension of the infection through the danger space
or anterior cervical space. The lung infiltrations were seen
mainly in patients with TB while lung abscesses were
found in a patients with necrotizing fasciitis and multiple
neck abscesses. The enlarged mediastinal lymph node
right hilar was found in a patient with a TB neck and a
chest wall abscess. The presence of a pleural effusion was
seen in 4 patients with TB and 4 patients with a pyogenic
infection.
In conclusion, CT scan is usually a sufficient technique
in the detection of the extension of various neck infections
and in guiding percutaneous procedures. Because of the
frequent thoracic abnormalities associated with neck
infections, we recommend performing a CT scan of chest
in the same sitting with the CT of neck. This may provide
information about the extent of the disease or give clues
about the diagnosis. Absence of ring enhancement does
not exclude the presence of a abscess. A clinical diagnosis
besides a CT-based one must play a complementary role
before any interventional procedures.
The most common organism found in pyogenic
infections in our study was Staphylococcus aureus (n =
14) (25%), followed by Klebsiella pneumonia (n = 8)
(14.3%). In the study of Wang et al, Klebsiella pneumonia
was the organism most commonly isolated from
infections18.
If an abscess is clearly present, a CT scan usually
shows a central, low attenuation region surrounded by an
enhanced rim . However, the low attenuation center does
not necessarily imply the presence of actual pus, as a
similar appearance can result from lymph nodes undergoing
early liquefaction (pre suppurative phase) and in those
that have undergone complete liquefaction necrosis
(suppurative phase). Again, the absence of a rim
enhancement does not preclude the presence of pus.
Vural et al. studied the accuracy of CT scans of deep
infections in the pediatric population22. They concluded
that CT scans have important limitations in differentiating
abscesses and cellulites and that and clinical findings
besides a CT-based diagnosis should guide the decision
for surgery22.
EJENTAS Egyptian Journal of ear, nose, throat and Allied Sciences
73
Volume 11, December 2010
Deep Neck Spaces radiology and review of deep neck infections, Al-Noury & Lotfy
References
1. Ungkanont K, Yellon RF, Weissman JL, et al. Head and neck
space infections in infants and children. Otolaryngol Head
Neck Surg 1995;112(3):37582.
2.Chow AW. Life threatening infections of the head and neck.
Clin Infec Dis 1992;14:9911004.
3.Nagy M, Pizzuto M, Backstrom J, et al. Deep neck infections
in children: a new approach to diagnosis and treatment.
Laryngoscope 1997;107 (12):162734.
4.Harnsberger HR, Osborn AG. Differential diagnosis of head
and neck lesions based on their space of origin. 1. The
suprahyoid part of the neck. Am J Roentgenol
1991;157:14754.
5.Levitt GW. Cervical fascia and deep neck infections.
Otolaryngol Clin North Am 1976;9:70316.
6.Mukherji SK, Castillo M. A simplified approach to the spaces
of the extracranial head & neck. Radiol Clin North Am
1998;36(5):76180.
7.Paonessa DF, Goldstein JC. Anatomy and physiology of head
and neck infections (with emphasis on the fascia of the face
and neck). Otolaryngol Clin North Am 1976;9(3):56180.
8.Johnson JT. Abscesses and deep space infections of the head
and neck. Infect Dis Clin North Am 1992;6(3):70517.
9. Johnson JT. Changing concepts in the management of deep
neck infection. AAO-HNS Bulletin 1992;11:1721.
10. Marra S, Hotaling AJ. Deep neck infections. Am J Otolaryngol
1996;17:28798.
11.Blomquist IK, Bayer AS. Life-threatening deep fascial space
infections of the head and neck. Infect Dis Clin North Am
1988;2(1):23764.
12. Chowdhury K, Bloom J, Black M, et al. Spontaneous and
non-spontaneous internal jugular vein thrombosis. Head
Neck 1990;12:16873.
13. Kim HJ, Park ED, Kim JH, et al. Odontogenic versus
nondontogenic deep neck space infections. J Comput Assist
Tomogr 1997;21(2):2028.
14. Weber AL, Siciliano A. CT and MR imaging evaluation of
neck infections with clinical correlations. Rad Clin of North
Am 2000;38(5):94168.
15. Bielamowicz SA, Stroper IS, Jabour BA, et al. Spaces and
triangles of the head and neck. Head Neck 1994:16:383-7.
16. Shah RR, Lwein JS. Imaging of the infrahyoid neck.
Neuroimaging Clin North A
17. Weissman JL, Carrau RL. Anterior facial vein and
submandibular gland together: Predicting the histology of
submandibular masses with CT or MR imaging. Radiology
1998;208:4416.
18. Wang LF, Kuo WR, Lin CS, et al. Space infection of the
head and neck. Kaohsiung J Med Sci. 2002;18(8):38692.
[19] Gianoli GJ, Espinola TE, Guarisco JL, et al. Retropharyngeal
space infection: changing trends. Otol Head Neck Surg.
1991;105:92100.
20. Moon WK, Han MH, Chang KH, et al. CT and MR imaging
of head and neck tuberculosis. Radiographics
1997;17(2):391402.
21. Lee KC, Tami TA, Lalwani AK, et al. Contemporary
management of cervical tuberculosis. Laryngoscope
1992;102(1):604.
22. Vural C, Gungor A, Comerci S. Accuracy of computerized
tomography in deep neck infection of pediatric population.
Am J Otolaryngol 2003;24(3):1438.
EJENTAS Egyptian Journal of ear, nose, throat and Allied Sciences
74
Volume 11, December 2010
Potrebbero piacerti anche
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5795)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1091)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- NarcissusDocumento84 pagineNarcissusAlexandra Maria NeaguNessuna valutazione finora
- Acute TonsillitisDocumento22 pagineAcute Tonsillitisg0ldz21100% (10)
- Speculative DesignDocumento16 pagineSpeculative DesignWill Kurlinkus100% (1)
- Process Audit Manual 030404Documento48 pagineProcess Audit Manual 030404azadsingh1Nessuna valutazione finora
- Theatre History TimelineDocumento7 pagineTheatre History TimelineCzar Paulo Dabon100% (2)
- 5 - Data Room Procedure TemplatesDocumento8 pagine5 - Data Room Procedure TemplatesnajahNessuna valutazione finora
- AS and A Level GraphsDocumento16 pagineAS and A Level GraphsManibalanNessuna valutazione finora
- 50 Interview Questions For Adryenn AshleyDocumento5 pagine50 Interview Questions For Adryenn AshleyAdryenn AshleyNessuna valutazione finora
- Section 22 Knapsack CipherDocumento9 pagineSection 22 Knapsack CipherchitrgNessuna valutazione finora
- KISS Notes The World CommunicatesDocumento30 pagineKISS Notes The World CommunicatesJenniferBackhus100% (4)
- Dharnish ReportDocumento13 pagineDharnish Reportdarshan75% (4)
- Trading Floors WSDocumento86 pagineTrading Floors WSAlok Singh100% (3)
- Competition Commission of India: Mahendra SoniDocumento16 pagineCompetition Commission of India: Mahendra SoniSuman sharmaNessuna valutazione finora
- Aol2 M6.1Documento5 pagineAol2 M6.1John Roland CruzNessuna valutazione finora
- Mergers and Acquisitions of Hindalco and NovelisDocumento35 pagineMergers and Acquisitions of Hindalco and Novelisashukejriwal007Nessuna valutazione finora
- Defining Pediatric SepsisDocumento2 pagineDefining Pediatric SepsisArisa DeguchiNessuna valutazione finora
- VocabularyDocumento7 pagineVocabularyReynald Satria Dwiky IrawanNessuna valutazione finora
- Marketing Ethics Amal 12-09-10Documento11 pagineMarketing Ethics Amal 12-09-10amalroy1986Nessuna valutazione finora
- Periods of Nursing HistoryDocumento38 paginePeriods of Nursing HistoryJeny Pearl Hijosa0% (1)
- The Body Shop Marketing Plan AnalysisDocumento18 pagineThe Body Shop Marketing Plan AnalysisHepita0% (1)
- New Values of The Required Hydrophilic-LipophilicBalance For Oil in Water Emulsions of Solid Fatty Acids and AlcoholsDocumento4 pagineNew Values of The Required Hydrophilic-LipophilicBalance For Oil in Water Emulsions of Solid Fatty Acids and AlcoholsRicardo100% (3)
- Intersection of Psychology With Architecture Final ReportDocumento22 pagineIntersection of Psychology With Architecture Final Reportmrunmayee pandeNessuna valutazione finora
- QuestionnaireDocumento4 pagineQuestionnairevishal chauhanNessuna valutazione finora
- Tongue Diagnosis Good AcurateDocumento12 pagineTongue Diagnosis Good AcuratejasoneinsteinNessuna valutazione finora
- 125) League of Cities of The Philippines vs. COMELEC (G.R. No. 176951, April 12, 2011) 2Documento35 pagine125) League of Cities of The Philippines vs. COMELEC (G.R. No. 176951, April 12, 2011) 2Carmel Grace KiwasNessuna valutazione finora
- Podcasts in IndiaDocumento4 paginePodcasts in IndiaShruti MahajanNessuna valutazione finora
- Battleship PotemkinDocumento7 pagineBattleship PotemkinMariusOdobașa100% (1)
- Dina Iordanova - Women in Balkan Cinema, Surviving On The MarginsDocumento17 pagineDina Iordanova - Women in Balkan Cinema, Surviving On The MarginsimparatulverdeNessuna valutazione finora
- Shear Force and Bending MomentssDocumento32 pagineShear Force and Bending Momentssمحمد شمسNessuna valutazione finora
- Paroles by PrevertDocumento29 pagineParoles by PrevertCity Lights90% (10)