Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Toronto Notes Nephrology 2015 24
Caricato da
JUSASBCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Toronto Notes Nephrology 2015 24
Caricato da
JUSASBCopyright:
Formati disponibili
NP24 Nephrology
Parenchymal Kidney Diseases
Essential Med Notes 2015
Systemic Lupus Erythematosus
lupus nephritis can present as any of the glomerular syndromes
nephrotic syndrome with an active sediment is most common presentation
GN caused by immune complex deposition in capillary loops and mesangium with resulting
renal injury
serum complement levels are usually low during periods of active renal disease
children and males with SLE are more likely to develop nephritis
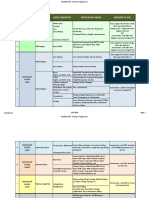
SLE Classification
Class I
Class II
Class III
Class IV
Class V
Class VI
Minimal
mesangial
lupus nephritis
Mesangial
proliferative
lupus nephritis
Focal
lupus nephritis
Diffuse
lupus nephritis
Membranous
lupus nephritis
Advanced sclerotic
lupus nephritis
Treatment
Treatment
Treatment
Treatment
Treatment
Class I and II do not
need treatment directed
at renal lesions
Lowest possible
dose of steroids
and observation
Steroids
Steroids
+
(controversial)
cytotoxic drugs
(consider dialysis or renal
transplant with severe disease)
ESRD
planning
Figure 15. International Society of Nephrology/Renal Pathology Society classification of
lupus nephritis 2003
Henoch-Schnlein Purpura
seen more commonly in children
purpura on buttocks and legs, abdominal pain, arthralgia, and fever
glomeruli show varying degrees of mesangial hypercellularity
IgA and C3 staining of mesangium
usually benign, self-limiting course, 10% progress to CKD
Goodpastures Disease
antibodies against type IV collagen present in lungs and GBM
more common in 3rd and 6th decades of life, males slightly more affected than females
present with RPGN type I and hemoptysis/dyspnea
pulmonary hemorrhage more common in smokers and males
treat with plasma exchange, cyclophosphamide, prednisone
ANCA-Associated Vasculitis (e.g. Granulomatosis with Polyangiitis and Microscopic
Polyangiitis [formerly Wegeners Granulomatosis])
PR3-ANCA (c-ANCA) most commonly associated with the clinical picture of granulomatosis
with polyangiitis (previously called Wegener's granulomatosis)
MPO-ANCA (p-ANCA) most commonly associated with the clinical picture of microscopic
polyangiitis
renal involvement very common
focal segmental necrotizing RPGN with no immune staining
may be indolent or fulminant in progression
vasculitis and granulomas rarely seen on renal biopsy
treating typically involves cyclophosphamide and prednisone
Cryoglobulinemia
cryoglobulins: monoclonal IgM and polyclonal IgG
presents as purpura, fever, Raynauds phenomenon, and arthralgias
at least 50% of patients have hepatitis C
renal disease seen in 40% of patients (isolated proteinuria/hematuria progressing to nephritic
syndrome)
most patients have decreased serum complement (C4 initially)
treat hepatitis C, plasmapheresis
overall prognosis: 75% renal recovery
Shunt Nephritis
immune-complex mediated nephritis associated with chronically infected ventriculoatrial
shunts inserted for treatment of hydrocephalus
presents as acute nephritic syndrome with decreased serum complement
nephrotic range proteinuria in 25% of patients
EULAR Recommendations for the Management
of Systemic Lupus Erythematosus (SLE)
Ann Rheum Dis 2008;67:195-205
Lupus Nephritis Recommendations
Monitoring: Renal biopsy, urine sediment analysis,
proteinuria, and kidney function may have
independent predictive ability for clinical outcome in
therapy of lupus nephritis but need to be interpreted
in conjunction. Changes in immunological tests
(anti-dsDNA, serum C3) have only limited ability to
predict the response to treatment and may be used
only as supplemental information.
Treatment: In patients with proliferative lupus
nephritis, glucocorticoids in combination with
immunosuppressive agents are effective against
progression to end-stage renal disease. Longterm efficacy has been demonstrated only for
cyclophosphamide-based regimens, which are
also associated with considerable adverse effects.
In short- and medium-term trials, mycophenolate
mofetil has demonstrated at least similar efficacy
compared with pulse cyclophosphamide and a
more favorable toxicity profile: failure to respond by
6 mo should evoke discussions for intensification
of therapy. Flares following remission are not
uncommon and require diligent follow-up.
End-Stage Renal Disease: Dialysis and
transplantation in SLE have long-term patient
and graft-survival rates comparable with those
observed in non-diabetic non-SLE patients, with
transplantation being the method of choice.
Potrebbero piacerti anche
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (120)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Worksheet 2 - TLC - Updated Summer 2021Documento4 pagineWorksheet 2 - TLC - Updated Summer 2021Bria PopeNessuna valutazione finora
- 1635 The Papal Stakes - Eric FlintDocumento1.813 pagine1635 The Papal Stakes - Eric Flintwon100% (2)
- Toronto Notes Nephrology 2015 37Documento1 paginaToronto Notes Nephrology 2015 37JUSASBNessuna valutazione finora
- Antipsychotics Factsheet pg2Documento1 paginaAntipsychotics Factsheet pg2JUSASBNessuna valutazione finora
- FA 2016 Step 1 - Reference ValuesDocumento2 pagineFA 2016 Step 1 - Reference ValuesJUSASBNessuna valutazione finora
- COMLEX Normal Adult Laboratory ValuesDocumento5 pagineCOMLEX Normal Adult Laboratory ValuesJUSASBNessuna valutazione finora
- Toronto Notes Nephrology 2015 33Documento1 paginaToronto Notes Nephrology 2015 33JUSASBNessuna valutazione finora
- Antipsychotics - FactsheetDocumento12 pagineAntipsychotics - FactsheetColonNessuna valutazione finora
- Toronto Notes Nephrology 2015 34Documento1 paginaToronto Notes Nephrology 2015 34JUSASBNessuna valutazione finora
- Toronto Notes Nephrology 2015 36Documento1 paginaToronto Notes Nephrology 2015 36JUSASBNessuna valutazione finora
- Toronto Notes Nephrology 2015 38Documento1 paginaToronto Notes Nephrology 2015 38JUSASBNessuna valutazione finora
- Toronto Notes Nephrology 2015 27Documento1 paginaToronto Notes Nephrology 2015 27JUSASBNessuna valutazione finora
- References: NP40 Nephrology Landmark Nephrology Trials/References Essential Med Notes 2015Documento1 paginaReferences: NP40 Nephrology Landmark Nephrology Trials/References Essential Med Notes 2015JUSASBNessuna valutazione finora
- Toronto Notes Nephrology 2015 17Documento1 paginaToronto Notes Nephrology 2015 17JUSASBNessuna valutazione finora
- Toronto Notes Nephrology 2015 39Documento1 paginaToronto Notes Nephrology 2015 39JUSASBNessuna valutazione finora
- Toronto Notes Nephrology 2015 28Documento1 paginaToronto Notes Nephrology 2015 28JUSASBNessuna valutazione finora
- Toronto Notes Nephrology 2015 32Documento1 paginaToronto Notes Nephrology 2015 32JUSASBNessuna valutazione finora
- Toronto Notes Nephrology 2015 35Documento1 paginaToronto Notes Nephrology 2015 35JUSASB50% (2)
- Toronto Notes Nephrology 2015 30Documento1 paginaToronto Notes Nephrology 2015 30JUSASBNessuna valutazione finora
- Toronto Notes Nephrology 2015 29Documento1 paginaToronto Notes Nephrology 2015 29JUSASBNessuna valutazione finora
- Toronto Notes Nephrology 2015 5Documento1 paginaToronto Notes Nephrology 2015 5JUSASBNessuna valutazione finora
- Toronto Notes Nephrology 2015 31Documento1 paginaToronto Notes Nephrology 2015 31JUSASBNessuna valutazione finora
- Toronto Notes Nephrology 2015 23Documento1 paginaToronto Notes Nephrology 2015 23JUSASBNessuna valutazione finora
- Toronto Notes Nephrology 2015 18Documento1 paginaToronto Notes Nephrology 2015 18JUSASBNessuna valutazione finora
- Toronto Notes Nephrology 2015 26Documento1 paginaToronto Notes Nephrology 2015 26JUSASBNessuna valutazione finora
- Toronto Notes Nephrology 2015 22Documento1 paginaToronto Notes Nephrology 2015 22JUSASB0% (1)
- Toronto Notes Nephrology 2015 25Documento1 paginaToronto Notes Nephrology 2015 25JUSASBNessuna valutazione finora
- Toronto Notes Nephrology 2015 14Documento1 paginaToronto Notes Nephrology 2015 14JUSASBNessuna valutazione finora
- Toronto Notes Nephrology 2015 15Documento1 paginaToronto Notes Nephrology 2015 15JUSASBNessuna valutazione finora
- Toronto Notes Nephrology 2015 20Documento1 paginaToronto Notes Nephrology 2015 20JUSASBNessuna valutazione finora
- 06-433rev7 HFC-227ea IVO ManualDocumento109 pagine06-433rev7 HFC-227ea IVO ManualFelix MartinezNessuna valutazione finora
- NANOGUARD - Products and ApplicationsDocumento2 pagineNANOGUARD - Products and ApplicationsSunrise VenturesNessuna valutazione finora
- Chapter 2Documento5 pagineChapter 2ERICKA MAE NATONessuna valutazione finora
- The Modern Fire Attack - Phil Jose and Dennis LegearDocumento7 pagineThe Modern Fire Attack - Phil Jose and Dennis LegearTomNessuna valutazione finora
- MS Fresher HR DocumentDocumento4 pagineMS Fresher HR DocumentJahanvi KambojNessuna valutazione finora
- Handover Paper Final 22 3 16 BJNDocumento13 pagineHandover Paper Final 22 3 16 BJNsisaraaah12Nessuna valutazione finora
- Polymer ProDocumento25 paginePolymer ProJeerisuda KingklangNessuna valutazione finora
- Doka H20 BeamDocumento20 pagineDoka H20 Beamshoaib100% (1)
- Nitrile Butadiene Rubber (NBR), Synthetic Latex: ApplicationDocumento2 pagineNitrile Butadiene Rubber (NBR), Synthetic Latex: ApplicationbobNessuna valutazione finora
- From Crème Fraîche To Sour Cream: What's The Difference?Documento14 pagineFrom Crème Fraîche To Sour Cream: What's The Difference?Maricel BautistaNessuna valutazione finora
- National Step Tablet Vs Step Wedge Comparision FilmDocumento4 pagineNational Step Tablet Vs Step Wedge Comparision FilmManivannanMudhaliarNessuna valutazione finora
- Activity 2: College of EngineeringDocumento3 pagineActivity 2: College of EngineeringMa.Elizabeth HernandezNessuna valutazione finora
- Manual Jib 25 10 02Documento256 pagineManual Jib 25 10 02Luis Jose LlobanNessuna valutazione finora
- q5 Nursery SchoolDocumento4 pagineq5 Nursery SchoolPK CheahNessuna valutazione finora
- Teoria Do Campo Ligante - Part IIDocumento25 pagineTeoria Do Campo Ligante - Part IIArthurGrafdeSousaNessuna valutazione finora
- Pia AlgebraDocumento12 paginePia AlgebraCarvajal EdithNessuna valutazione finora
- Msds M-Toluoyl ChlorideDocumento4 pagineMsds M-Toluoyl ChloridecrisNessuna valutazione finora
- Pipe TobaccoDocumento6 paginePipe TobaccoVictorIoncuNessuna valutazione finora
- YuzurtDocumento2 pagineYuzurtFranco Ascari100% (1)
- Ir33+ Range: ... Continuity, Innovation and DesignDocumento4 pagineIr33+ Range: ... Continuity, Innovation and DesignbenNessuna valutazione finora
- Practice Questions Human Nutrition Part 1Documento4 paginePractice Questions Human Nutrition Part 1PeiYi TanNessuna valutazione finora
- WAUZZZ8K0BA159120Documento10 pagineWAUZZZ8K0BA159120Vedad VedaddNessuna valutazione finora
- Reclaimer Inspection ReportDocumento51 pagineReclaimer Inspection ReportThiru Malpathi100% (1)
- Scots-Supply Chain ManagementDocumento3 pagineScots-Supply Chain Managementgamer godNessuna valutazione finora
- New-DLP Phase2 Assignment-3 Module-B Final-9.8.18Documento6 pagineNew-DLP Phase2 Assignment-3 Module-B Final-9.8.18PNessuna valutazione finora
- Ujian Diagnostik Ting 2 EnglishDocumento9 pagineUjian Diagnostik Ting 2 EnglishJ-Gie JaulahNessuna valutazione finora
- Battle Healing PrayerDocumento9 pagineBattle Healing PrayerSolavei LoanerNessuna valutazione finora
- Impact of Textiles and Clothing Industry On EnvironmentDocumento15 pagineImpact of Textiles and Clothing Industry On Environmentranjann349Nessuna valutazione finora