Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Splenectomy: Disclaimer
Caricato da
Mimi FatinTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Splenectomy: Disclaimer
Caricato da
Mimi FatinCopyright:
Formati disponibili
Starship Childrens Health Clinical Guideline
Note: The electronic version of this guideline is the version currently in use. Any printed version can
not be assumed to be current. Please remember to read our disclaimer.
SPLENECTOMY
Disclaimer
Indications
Preoperative Preparation
Post Operative Care and Discharge
Planning
References
Disclaimer
Paediatric clinical guidelines are guides to treatment for medical and surgical staff. They are not
protocols. Management of each patient is at the discretion of the primary consultant.
Indications
Haematological disorders
o Hereditary spherocytosis
o Thalassaemia major
o ITP unresponsive to medical management
o Myeloproliferative disorders
o Sickle cell disease
Traumatic injury to spleen
Intra-operative splenic injury
Splenic abscesses, cysts, malignancy/mass of spleen or adjacent organ
Non-cirrhotic portal hypertension with GI bleeding (usually as part of a portosystemic shunt
operation)
Preoperative Preparation
Consent
FBC, U&E, G&H (consider Xmatch)
Platelets may be required
Peri-operative antibiotics usually IV cefazolin at induction, to continue for 24hours
Immunisations and antibiotic plan (see below)
Consent
Laparoscopic splenectomy, where possible, is now the standard of care. Alternatively open
(left subcostal incision)
Wound infection, incisional hernia, haemorrhage, subphrenic abscess, pancreatic
pseudocyst, gastric fistula/perforation
Those with myeloproliferative disorders have higher risk of bleeding and thrombosis
Overwhelming post splenectomy infection
Infection Risk in Splenectomised patients
The risk of post-splenectomy sepsis is greatest in the following groups:
o younger children
Authors:
Editor:
Splenectomy
Elizabeth Wilson, Rachel Webb, Nyree Cole, Jane
Skeen, James Hamill, Lochie Teague, Helen Evans,
Tim Prestidge
Greg Williams
Services:
Date Reviewed:
Page:
Paediatric Surgery, Infectious
Diseases, Haematology-Oncology,
Hepatology
4 July 2014
1 of 5
Starship Childrens Health Clinical Guideline
Note: The electronic version of this guideline is the version currently in use. Any printed version can
not be assumed to be current. Please remember to read our disclaimer.
SPLENECTOMY
o early in the post-operative course (up to 2 years)
o individuals with an underlying haematologic disorder
o immune suppressed children - eg following liver transplantation
Streptococcus pneumoniae (pneumococcus) is the commonest pathogen
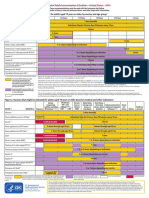
Immunisations
No vaccines are contraindicated for splenectomised /hyposplenic patients.
Ensure patient is up to date with routine immunisations according to National Immunisation
Schedule, especially pneumococcal, Haemophilus influenzae type b (Hib) and MMR.
Additional immunisations are recommended for asplenia/hyposplenia; commence
immunisation programme as soon as condition is recognised.
For elective splenectomy extra immunisations should be commenced as soon as possible
and at least 2 weeks pre-operatively
For emergency splenectomy commence immunisations 2 weeks post-operatively.
The recommended schedule varies according to age and is complicated by which vaccines
are funded which can vary over time. As at May 2014 the recommended schedule is as
follows. Please discuss with the Paediatric Infectious Diseases or Haematology team to
clarify immunisation plan. Funded vaccines shown below are accurate as at 1 July 2014
but are subject to change. Check latest pharmaceutical schedule for currently funded
vaccines.
Age at
diagnosis
Vaccine
(trade name)
Vaccine schedule
Infants aged
under
12 months with
functional
asplenia or prea
or postspctomy
PCV13
(Prevenar 13)
and
23PPV
(Pneumovax 23)
PCV13b at age 6 weeks, 3, 5 and 15 months (usual childhood Schedule),
or age-appropriate catch-up schedule:
if commencing immunisation at ages
711 months, give 2 doses of PCV13 at least 4 weeks apart, followed
by a booster dose at age 15 months
for children aged 711 months who have completed the primary
course with PCV10, give 1 dose of PCV13 followed by the scheduled
PCV13 booster at age 15 months.
Following the completion of the PCV course, give 1 dose of 23PPV at age
2 years. There must be at least 8 weeks between the last PCV dose and
the 23PPV dose.
Revaccinate once with 23PPV, 5 years after the 1st 23PPV.
MenCCV
NeisVacC)
and
MCV4-D
(Menactra)
Age-appropriate MenCCV schedule:
if aged under 6 months at diagnosis, give 2 doses 8 weeks apart, with
a booster at age 12 months
if aged 611 months at diagnosis, give 1 dose, with a further dose at
age 12 months.
At age 2 years, give 2 doses of MCV4-Dc
8 weeks apart, then a booster dose after
3 years, then 5-yearly.
Influenza
Annual immunisation from age 6 months.
Authors:
Editor:
Splenectomy
Elizabeth Wilson, Rachel Webb, Nyree Cole, Jane
Skeen, James Hamill, Lochie Teague, Helen Evans,
Tim Prestidge
Greg Williams
Services:
Date Reviewed:
Page:
Paediatric Surgery, Infectious
Diseases, Haematology-Oncology,
Hepatology
4 July 2014
2 of 5
Starship Childrens Health Clinical Guideline
Note: The electronic version of this guideline is the version currently in use. Any printed version can
not be assumed to be current. Please remember to read our disclaimer.
SPLENECTOMY
(Influvac or
Fluarix)
In the first year, give 2 doses 4 weeks apart, then 1 dose in each subsequent
year.
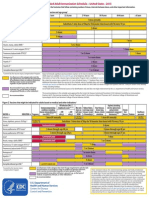
PCV13
(Prevenar 13) and
23PPV
(Pneumovax 23)
PCV13,b,d age-appropriate catch-up schedule:
e
children aged >12 months who have completed the primary course of
PCV10 require 1 dose of PCV13b
previously unimmunised children aged 12 months to under 5 years
require 2 doses of PCV13,d 8 weeks apart
f
d
children aged 5 years to under 18 years require 1 dose of PCV13.
Following the completion of the PCV13 course, give 1 dose of 23PPV at
age 2 years. There must be at least 8 weeks between the last PCV13
dose and the 23PPV dose.
Revaccinate once with 23PPV, 5 years after the 1st 23PPV.
MenCCV
(NeisVacC) and
MCV4-D
(Menactra)
If aged 1223 months at diagnosis, give 1 dose of MenCCV, followed by
MCV4-Dc at age 2 years, 2 doses 8 week3s apart; then a booster of
MCV4-D after three years, then 5-yearly.
If aged 2 years at diagnosis, give 2 doses of MCV4-Dc 8 weeks apart,
and:
if the 1st MCV4-D dose was given at age <7 years, give a booster
after 3 years, then 5-yearly, or
if the 1st MCV4-D dose was given at age 7 years, give a booster
dose every 5 years.
Hib
(Act-HIB)
If aged 1215 months, give 1 dose at age 15 months as per the National
Immunisation Schedule.
If aged 16 months to under 5 years and has not received a single Hib
dose after age 12 months, give 1 dose.
If aged 5 years and older, give 1 dose, even if fully vaccinated.
Children aged
12 months to
under 18 years
(continued)
Influenza
(Influvac or
Fluarix)
Annual immunisation. In previously unvaccinated children aged under 9
years, give 2 doses 4 weeks apart, then 1 dose in each subsequent year.
Varicella
(Varilrix)
If no history of varicella disease or immunisation, give 2 doses at least 6
weeks apart.
Adults
18 years, pre-a
or postsplenectomy
PCV13
(Prevenar 13)
1 dose of PCV13.d,f
23PPV
(Pneumovax 23)
Give a maximum of 3 doses of 23PPV in a lifetime, a minimum of 5 years
apart. The 1st 23PPV dose is given at least 8 weeks after PCV13; the
2nd a minimum of 5 years later; the 3rd dose at age 65 years.
MCV4-D
(Menactra)
Give 2 doses of MCV4-D, 8 weeks apart, then 1 dose every 5 years.c,g
Hib
(Act-HIB)
Give 1 dose regardless of previous vaccination history.
Influenza (Influvac
or Fluarix)
Annual immunisation.
Varicella
(Varilrix)
If no history of varicella disease or immunisation, give 2 doses, at least 6
weeks apart.
Children aged
12 months to
under 18 years
with functional
asplenia or prea
or postsplenectomy
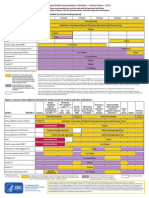
Where possible, the vaccines should be administered at least 2 weeks before elective splenectomy. For emergency splenectomy,
the vaccines should be administered 2 weeks post-operatively.
PCV13 replaces PCV10 (Synflorix) on the Schedule.
Give MCV4-D at least 4 weeks after PCV13.
If 23PPV has already been given (prior to any doses of PCV13), wait at least 1 year before administering PCV13.
There are no safety concerns, regardless of the interval between the last dose of PCV10 and the 1st dose of PCV13.
Authors:
Editor:
Splenectomy
Elizabeth Wilson, Rachel Webb, Nyree Cole, Jane
Skeen, James Hamill, Lochie Teague, Helen Evans,
Tim Prestidge
Greg Williams
Services:
Date Reviewed:
Page:
Paediatric Surgery, Infectious
Diseases, Haematology-Oncology,
Hepatology
4 July 2014
3 of 5
Starship Childrens Health Clinical Guideline
Note: The electronic version of this guideline is the version currently in use. Any printed version can
not be assumed to be current. Please remember to read our disclaimer.
SPLENECTOMY
f
PCV13 is registered for children aged under 5 years and adults aged 50 years and older. There is emerging but limited efficacy data
for PCV13 use outside of these age ranges. However, PCV13 can be used for high-risk older children and adults.
MCV4-D is registered for individuals aged 9 months to 55 years, but there are not expected to be any safety concerns when
administered to adults older than 55 years.
Antibiotic prophylaxis
Some children may require long term antibiotic prophylaxis against pneumococcal infection
(with amoxicillin, penicillin or erythromycin if beta lactam allergy) please discuss with
childs haematologist or the Paediatric Infectious Diseases team.
Post Operative Care and Discharge Planning
Bloods FBC, U&E evening or next morning as per operation note
Watch platelet count may need anticoagulants if increases ++
Antibiotics as per operation note (Usually IV cephazolin 24hours)
Chest physiotherapy to prevent chest infection may be required
Discuss medical alert bracelet (www.medicalert.co.nz for more info)
Ensure vaccination plan is clearly documented on discharge letter and clarify who will
follow this through (GP or local paediatrician)
Antibiotics: if recommended after discussion with Haematology or Paediatric Infectious
Diseases:
1) Daily oral antibiotic prophylaxis (if recommended by childs haematologist / ID team)
Amoxicillin
all ages
20mg/kg once daily (max 500mg)
OR
Penicillin VK
< 5yrs
125mg bd
> 5yrs
250mg bd
OR
If beta lactam allergy please discuss with Paediatric Infectious Diseases. Options
include roxithromycin (if able to swallow tablets) and erythromycin.
2) Standby antibiotics to take if unwell and unable to access immediate medical care
Usually amoxicillin PO high dose (90mg/kg/day in three divided doses)
Discuss importance of seeking medical attention early for febrile illnesses, malaria
precautions if travelling overseas, antibiotics for dog / animal bites
Provide patient education leaflet
References
Davies J, Lewis MN, Wimperis J, Rafi I, Ladhani S, Bolton-Maggs, PHB. Review of Guideline for
the Prevention of Infection in patients with an absent of dysfunctional spleen. British Journal of
Haematology 2011; 155: 308 317.
Spelman D, Buttery J, Daley A, et Al. Guidelines for the prevention of sepsis in asplenic and
hyposplenic patients. Internal Medicine Journal 2008; 38: 349 356.
American Academy of Pediatrics. Immunisation in special clinical circumstances: children with
asplenia or functional asplenia. In Pickering LK, Baker CJ, Kimberlin DW, Long SS, eds. Report of
Authors:
Editor:
Splenectomy
Elizabeth Wilson, Rachel Webb, Nyree Cole, Jane
Skeen, James Hamill, Lochie Teague, Helen Evans,
Tim Prestidge
Greg Williams
Services:
Date Reviewed:
Page:
Paediatric Surgery, Infectious
Diseases, Haematology-Oncology,
Hepatology
4 July 2014
4 of 5
Starship Childrens Health Clinical Guideline
Note: The electronic version of this guideline is the version currently in use. Any printed version can
not be assumed to be current. Please remember to read our disclaimer.
SPLENECTOMY
the Committee on Infectious diseases. Red Book: 2012 Report of the Committee on Infectious
diseases.
Society for Surgery of the Alimentary Tract. Indications for splenectomy. Manchester (MA): Society
for Surgery of the Alimentary Tract; 2000. 4 p. [5 references]
Authors:
Editor:
Splenectomy
Elizabeth Wilson, Rachel Webb, Nyree Cole, Jane
Skeen, James Hamill, Lochie Teague, Helen Evans,
Tim Prestidge
Greg Williams
Services:
Date Reviewed:
Page:
Paediatric Surgery, Infectious
Diseases, Haematology-Oncology,
Hepatology
4 July 2014
5 of 5
Potrebbero piacerti anche
- WHO Immunization RecommendationsDocumento9 pagineWHO Immunization RecommendationsMeeKo VideñaNessuna valutazione finora
- States, 2011 United Recommended Childhood and Adolescent Immunization SchedulesDocumento7 pagineStates, 2011 United Recommended Childhood and Adolescent Immunization SchedulesDolores KilpatrickNessuna valutazione finora
- IZSchedule0 6yrsDocumento1 paginaIZSchedule0 6yrsKaty ForemanNessuna valutazione finora
- 1 CombineDocumento726 pagine1 CombineSong Hành Vạn KiếpNessuna valutazione finora
- Urinary Tract Infection PDFDocumento9 pagineUrinary Tract Infection PDFTigerEyzNessuna valutazione finora
- WHO Position Papers - Recommended Routine Immunizations for ChildrenDocumento8 pagineWHO Position Papers - Recommended Routine Immunizations for Childrenfadityo1Nessuna valutazione finora
- WHO Immunization Schedule ChildrenDocumento9 pagineWHO Immunization Schedule Childrenashchua21Nessuna valutazione finora
- Pneumococcal Conjugate: VaccineDocumento2 paginePneumococcal Conjugate: VaccineJenny TaylorNessuna valutazione finora
- Summary of Recommendations For Child Teen Immunization: (Age Birth Through 18 Years)Documento5 pagineSummary of Recommendations For Child Teen Immunization: (Age Birth Through 18 Years)Annie AnnaNessuna valutazione finora
- Catch-up immunization schedule for persons aged 4 months through 18 yearsDocumento1 paginaCatch-up immunization schedule for persons aged 4 months through 18 yearsJesus A. Pineda GarciaNessuna valutazione finora
- Immunization Part 2Documento13 pagineImmunization Part 2Marleen ShehadaNessuna valutazione finora
- EPIDocumento10 pagineEPIBo ChoiNessuna valutazione finora
- Adult Immunization Schedule and RecommendationsDocumento3 pagineAdult Immunization Schedule and RecommendationsdrmanojvimalNessuna valutazione finora
- Philippine College of Chest Physicians: Media Kit For PneumoniaDocumento4 paginePhilippine College of Chest Physicians: Media Kit For PneumoniaWilsonne ChuaNessuna valutazione finora
- Adult ScheduleDocumento3 pagineAdult SchedulelcmurilloNessuna valutazione finora
- Human Papillomavirus Bivalent Vaccin1Documento8 pagineHuman Papillomavirus Bivalent Vaccin1alejandro fernandezNessuna valutazione finora
- Adult Pocafeket SizeDocumento2 pagineAdult Pocafeket SizedadfNessuna valutazione finora
- Practice Changing UpDates - UpToDateDocumento13 paginePractice Changing UpDates - UpToDatemayteveronica1000Nessuna valutazione finora
- CDC Healthcare Personnel Vaccination RecommendationsDocumento1 paginaCDC Healthcare Personnel Vaccination RecommendationsdocktpNessuna valutazione finora
- USMLE Step 3 Lecture Notes 2021-2022: Internal Medicine, Psychiatry, EthicsDa EverandUSMLE Step 3 Lecture Notes 2021-2022: Internal Medicine, Psychiatry, EthicsValutazione: 5 su 5 stelle5/5 (9)
- Adult Immunization Recommendations SummaryDocumento5 pagineAdult Immunization Recommendations SummaryHannah Caburian RemoNessuna valutazione finora
- Nephrotic Syndrome in ChildhoodDocumento5 pagineNephrotic Syndrome in ChildhoodJessica SilaenNessuna valutazione finora
- Splenectomy - Factsheet - For - Health - Professionals 2022 FinalDocumento4 pagineSplenectomy - Factsheet - For - Health - Professionals 2022 Finalalpha.blocker11Nessuna valutazione finora
- Table 2: Summary of WHO Position Papers - Recommended Routine Immunizations For ChildrenDocumento7 pagineTable 2: Summary of WHO Position Papers - Recommended Routine Immunizations For ChildrenKrishnendu PramanikNessuna valutazione finora
- Highlghts in Pediatric Infectious DiseasesDocumento37 pagineHighlghts in Pediatric Infectious DiseasesLibay Villamor IsmaelNessuna valutazione finora
- Expanded Program On ImmunuzationDocumento37 pagineExpanded Program On ImmunuzationRose AnnNessuna valutazione finora
- Office of The Secretary: Pneumococcal Conjugate Vaccines (PCV) Reassessment in The PhilippinesDocumento17 pagineOffice of The Secretary: Pneumococcal Conjugate Vaccines (PCV) Reassessment in The Philippinesbandicot21Nessuna valutazione finora
- Epi PowerpointDocumento29 pagineEpi PowerpointFelisa Lacsamana Gregorio100% (3)
- Drug Study On CeftriaxoneDocumento7 pagineDrug Study On CeftriaxoneleoNessuna valutazione finora
- Influvac: New Zealand Data SheetDocumento7 pagineInfluvac: New Zealand Data SheetAtthapu ThirupathaiahNessuna valutazione finora
- Expanded Program Immunization & Reproductive HealthDocumento24 pagineExpanded Program Immunization & Reproductive HealthPrince Jhessie L. AbellaNessuna valutazione finora
- Types of ImmunizationsDocumento21 pagineTypes of Immunizationsmacmactongos100% (6)
- Adult Combined ScheduleDocumento5 pagineAdult Combined SchedulelcmurilloNessuna valutazione finora
- Immunization Review GPDocumento46 pagineImmunization Review GPKishore ChandkiNessuna valutazione finora
- Cervarix 2018Documento26 pagineCervarix 2018Jacob PaglinawanNessuna valutazione finora
- Assignment On Drugs Used For NewbornDocumento11 pagineAssignment On Drugs Used For Newbornvarshasharma05Nessuna valutazione finora
- Immunization ScheduleDocumento2 pagineImmunization ScheduleTracy100% (1)
- Summary of Recommendations For Adult Immunization: (Age 19 Years & Older)Documento4 pagineSummary of Recommendations For Adult Immunization: (Age 19 Years & Older)gyna_2002Nessuna valutazione finora
- ScheduleDocumento2 pagineScheduleapi-286634335Nessuna valutazione finora
- 0 6yrs Schedule BWDocumento1 pagina0 6yrs Schedule BWRyan ArdyantoNessuna valutazione finora
- Adult Immunization ScheduleDocumento3 pagineAdult Immunization ScheduleBryan Mae H. DegorioNessuna valutazione finora
- Polio: The Disease and ImmunizationDocumento36 paginePolio: The Disease and ImmunizationJeetendra SahNessuna valutazione finora
- Kepi Vaccines (2) - Gi - 1Documento30 pagineKepi Vaccines (2) - Gi - 1okwadha simionNessuna valutazione finora
- Figure 1. Recommended Immunization Schedule For Adults Aged 19 Years or Older, by Vaccine and Age GroupDocumento2 pagineFigure 1. Recommended Immunization Schedule For Adults Aged 19 Years or Older, by Vaccine and Age GroupmsarasNessuna valutazione finora
- VaccinesDocumento4 pagineVaccinesSam smithNessuna valutazione finora
- Typhoid Fever Follow-Up PDFDocumento16 pagineTyphoid Fever Follow-Up PDFPlot BUnniesNessuna valutazione finora
- Ethinylestradiol 30mcg + Gestodene 75mcg (Gynera)Documento20 pagineEthinylestradiol 30mcg + Gestodene 75mcg (Gynera)asdwasdNessuna valutazione finora
- Recommended Immunization - Canadian Immunization Guide - Seventh Edition - 2006Documento2 pagineRecommended Immunization - Canadian Immunization Guide - Seventh Edition - 2006Maja MudriNessuna valutazione finora
- Journjkljal 2 PDFDocumento9 pagineJournjkljal 2 PDFAan AchmadNessuna valutazione finora
- IZSchedule0 6yrsDocumento1 paginaIZSchedule0 6yrsgeany2911Nessuna valutazione finora
- SOMis AdminDocumento14 pagineSOMis AdminLINGGA DEWINessuna valutazione finora
- Recommended Immunization Schedule For Persons Aged 0-6 YearsDocumento3 pagineRecommended Immunization Schedule For Persons Aged 0-6 YearsAlvaro FloresNessuna valutazione finora
- Guideline For The Management of Toxoplasmosis EncephalitisDocumento8 pagineGuideline For The Management of Toxoplasmosis EncephalitisFersha Syafir RamadhanNessuna valutazione finora
- Annex I Summary of Product CharacteristicsDocumento33 pagineAnnex I Summary of Product CharacteristicsVimala BohoNessuna valutazione finora
- Ethinylestradiol 0.02mg + Gestodene 0.075mg (Meliane)Documento18 pagineEthinylestradiol 0.02mg + Gestodene 0.075mg (Meliane)asdwasdNessuna valutazione finora
- Adult ScheduleDocumento3 pagineAdult ScheduleerilarchiNessuna valutazione finora
- Adult ImmunizationDocumento6 pagineAdult ImmunizationAmit GoelNessuna valutazione finora
- Iap Guide Book On Immunization Immunization in Special Situations PDFDocumento8 pagineIap Guide Book On Immunization Immunization in Special Situations PDFGirdhari Lal Saini100% (1)
- Expanded Program On Immunization ReportDocumento38 pagineExpanded Program On Immunization ReportKimm Delos ReyesNessuna valutazione finora
- Clinical Management Review 2023-2024: Volume 1: USMLE Step 3 and COMLEX-USA Level 3Da EverandClinical Management Review 2023-2024: Volume 1: USMLE Step 3 and COMLEX-USA Level 3Valutazione: 5 su 5 stelle5/5 (1)
- Presentation 1Documento8 paginePresentation 1Mimi FatinNessuna valutazione finora
- Respi 2011Documento19 pagineRespi 2011Mimi FatinNessuna valutazione finora
- Addiction: by Wan Mohd Fikri Bin Wan Mohd NasirDocumento26 pagineAddiction: by Wan Mohd Fikri Bin Wan Mohd NasirMimi FatinNessuna valutazione finora
- Fixed Drug EruptionDocumento31 pagineFixed Drug EruptionMimi FatinNessuna valutazione finora
- Anatomy N Physiology MataDocumento6 pagineAnatomy N Physiology MataMimi FatinNessuna valutazione finora
- RefernsiDocumento1 paginaRefernsiMimi FatinNessuna valutazione finora
- Lapsus RadioDocumento5 pagineLapsus RadioMimi FatinNessuna valutazione finora
- Classification of CLPDocumento6 pagineClassification of CLPMimi FatinNessuna valutazione finora
- Bloodstain Patterns 2Documento10 pagineBloodstain Patterns 2Mimi FatinNessuna valutazione finora
- DP 1Documento15 pagineDP 1Mimi FatinNessuna valutazione finora
- Tinea CapitisDocumento35 pagineTinea CapitisMimi FatinNessuna valutazione finora
- Collodion Baby: eISSN 1307 - 394XDocumento5 pagineCollodion Baby: eISSN 1307 - 394XMimi FatinNessuna valutazione finora
- Group 2Documento23 pagineGroup 2Mimi FatinNessuna valutazione finora
- Salter-Harris Fractures - Radiology Reference Article - RadiopaediaDocumento6 pagineSalter-Harris Fractures - Radiology Reference Article - RadiopaediaMimi FatinNessuna valutazione finora
- Sputum CrudumDocumento1 paginaSputum CrudumMimi FatinNessuna valutazione finora
- Physio FeverDocumento2 paginePhysio FeverMimi FatinNessuna valutazione finora
- Bronkitis Pada AnakDocumento5 pagineBronkitis Pada AnakMimi FatinNessuna valutazione finora
- Cannabis Use and Cognitive Dysfunction PDFDocumento9 pagineCannabis Use and Cognitive Dysfunction PDFMimi FatinNessuna valutazione finora
- Referat JiwaDocumento3 pagineReferat JiwaMimi FatinNessuna valutazione finora
- Report Pleno GeriatryDocumento18 pagineReport Pleno GeriatryMimi FatinNessuna valutazione finora
- SGPT PDFDocumento2 pagineSGPT PDFMimi FatinNessuna valutazione finora
- Pleno 2 (Cataract)Documento3 paginePleno 2 (Cataract)Mimi FatinNessuna valutazione finora
- Colour of MucousDocumento3 pagineColour of MucousMimi FatinNessuna valutazione finora
- JUSTIN TIMBERLAKE - Mirrors (Boyce Avenue FeatDocumento2 pagineJUSTIN TIMBERLAKE - Mirrors (Boyce Avenue FeatMimi FatinNessuna valutazione finora
- COMMUNICABLE DISEASE NURSING (Part II: Diseases)Documento21 pagineCOMMUNICABLE DISEASE NURSING (Part II: Diseases)ROBERT C. REÑA, BSN, RN, MAN (ue)88% (34)
- Evaluation Liver Function TestsDocumento74 pagineEvaluation Liver Function TestsMeylinda LinNessuna valutazione finora
- Asepsis and Infection Control Nursing SchoolDocumento20 pagineAsepsis and Infection Control Nursing Schoolleonardo orozco100% (1)
- Taenia InfectionDocumento2 pagineTaenia InfectionJayesh MahajanNessuna valutazione finora
- Chronic Rhinosinusitis and Nasal PolypsDocumento9 pagineChronic Rhinosinusitis and Nasal PolypssuriskuNessuna valutazione finora
- MICP211 Midterm ReviewerDocumento39 pagineMICP211 Midterm ReviewerKrista CruzNessuna valutazione finora
- Escherichia Coli (EDocumento16 pagineEscherichia Coli (EDiyantoro NyoNessuna valutazione finora
- Arellano University College of Nursing Legarda - Pasay - PasigDocumento3 pagineArellano University College of Nursing Legarda - Pasay - PasigCharles Loriaga Cruz IINessuna valutazione finora
- Poultry ParasitesDocumento164 paginePoultry ParasitesGiselle Castro Sabino100% (1)
- Disease Unit ExamDocumento3 pagineDisease Unit ExamdavidNessuna valutazione finora
- Global HIV Neurology A Comprehensive Review.1-1Documento22 pagineGlobal HIV Neurology A Comprehensive Review.1-1Sadam Yondaime AriesNessuna valutazione finora
- Tips Handbook World Heart Federation RheachDocumento120 pagineTips Handbook World Heart Federation RheachJulidiaNessuna valutazione finora
- Lab 7 Genus NeisseriaDocumento20 pagineLab 7 Genus NeisseriaAAANessuna valutazione finora
- Acute BronchitisDocumento4 pagineAcute BronchitisLenjunNessuna valutazione finora
- DurianDocumento1 paginaDuriankakangmasNessuna valutazione finora
- Important For ExamDocumento11 pagineImportant For ExamJagveer ChauhanNessuna valutazione finora
- Anavar (Oxandrolone)Documento26 pagineAnavar (Oxandrolone)illicitdrugsNessuna valutazione finora
- PARASITOLOGYDocumento33 paginePARASITOLOGYAli AhmedNessuna valutazione finora
- HIV/AIDS CrimilizationDocumento13 pagineHIV/AIDS CrimilizationC2EA YouthNessuna valutazione finora
- Ear Infections: These Include Otitis Externa, Otitis Media, MastoiditisDocumento32 pagineEar Infections: These Include Otitis Externa, Otitis Media, Mastoiditiseugene ugayNessuna valutazione finora
- Dengue Fever Signs, Symptoms, and PreventionDocumento9 pagineDengue Fever Signs, Symptoms, and PreventionKyla BalboaNessuna valutazione finora
- Cestosis y Cestodos PDFDocumento14 pagineCestosis y Cestodos PDFErnesto VersailleNessuna valutazione finora
- 04 Soybean Growth and DevelopmentDocumento21 pagine04 Soybean Growth and DevelopmentLiyana ShahiminNessuna valutazione finora
- Vancomycin Pharmacokinetics GuideDocumento5 pagineVancomycin Pharmacokinetics GuidedrblondyNessuna valutazione finora
- PBSDocumento72 paginePBSKavi KaviNessuna valutazione finora
- Hemagglutination AssayDocumento4 pagineHemagglutination Assayऋषभ गर्गNessuna valutazione finora
- Progress Exam - MicrobiologyDocumento75 pagineProgress Exam - MicrobiologyAngelicaNessuna valutazione finora
- CDC 118387 DS1Documento132 pagineCDC 118387 DS1Sina AyodejiNessuna valutazione finora
- Deases of Middle EarDocumento43 pagineDeases of Middle EarPrathamesh ParekhNessuna valutazione finora
- Syok HipovolemikDocumento22 pagineSyok HipovolemikNurmasdalina IthninNessuna valutazione finora