Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Comparison of Intramuscular Olanzapine, Orally
Caricato da
Anonymous 4LIXFKUCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Comparison of Intramuscular Olanzapine, Orally
Caricato da
Anonymous 4LIXFKUCopyright:
Formati disponibili
ORIGINAL CONTRIBUTION
Comparison of Intramuscular Olanzapine, Orally
Disintegrating Olanzapine Tablets, Oral Risperidone
Solution, and Intramuscular Haloperidol in the
Management of Acute Agitation in an Acute
Care Psychiatric Ward in Taiwan
Wen-Yu Hsu, MD,* Si-Sheng Huang, MD,* Bo-Shyan Lee, MD,* and Nan-Ying Chiu, MD*
Introduction: The purpose of this study was to compare efcacy
and safety among intramuscular olanzapine, intramuscular haloperidol,
orally disintegrating olanzapine tablets, and oral risperidone solution for
agitated patients with psychosis during the rst 24 hours of treatment
in an acute care psychiatric ward.
Methods: Forty-two inpatients from an acute care psychiatric ward of
a medical center in central Taiwan were enrolled. They were randomly
assigned to 1 of the 4 treatment groups (10-mg intramuscular olanzapine, 10-mg olanzapine oral disintegrating tablet, 3-mg oral risperidone
solution, or 7.5-mg intramuscular haloperidol). Agitation was measured
by using the excited component of the Positive and Negative Syndrome Scale (PANSS-EC), the Agitation-Calmness Evaluation Scale,
and the Clinical Global ImpressionVSeverity Scale during the rst
24 hours.
Results: There were signicant differences in the PANSS-EC total
scores for the 4 intervention groups at 15, 30, 45, 60, 75, and 90 minutes after the initiation of treatment. More signicant differences were
found early in the treatment. In the post hoc analysis, the patients who
received intramuscular olanzapine or orally disintegrating olanzapine
tablets showed signicantly greater improvement in PANSS-EC scores
than did patients who received intramuscular haloperidol at points 15,
30, 45, 60, 75, and 90 minutes after injection.
Conclusions: These ndings suggest that intramuscular olanzapine,
orally disintegrating olanzapine tablets, and oral risperidone solution are
as effective treatments as intramuscular haloperidol for patients with
acute agitation. Intramuscular olanzapine and disintegrating olanzapine
tablets are more effective than intramuscular haloperidol in the early
phase of the intervention. There is no signicant difference in effectiveness among intramuscular olanzapine, orally disintegrating olanzapine tablets, and oral risperidone solution.
Key Words: olanzapine, haloperidol, risperidone, agitation,
injection, orally
(J Clin Psychopharmacol 2010;30: 230Y234)
iolence and aggressive behavior are common among
patients with psychiatric disorders. Grassi et al1 reported a
7.5% prevalence rate for violence in acute psychiatric inpatients
in Italy. Violence is a complex behavioral phenomenon with
many causes.2
There are many ways to manage violent situations. Environmental intervention, behavior therapy, talking down, and medication intervention may all be effective. Rapid tranquilization is
the assertive use of medication to calm severely agitated patients
quickly, decrease dangerous behavior, and allow treatment of
the underlying condition.3 In the past, conventional antipsychotic
agents augmented with benzodiazepines have been the standard treatment;4,5 however, there are now many other choices.
Haloperidol, a high-potency butyrophenone, is one of the most
frequently used rst-generation antipsychotic agents for the
treatment of acute agitation6; however, extrapyramidal symptoms are a concern after haloperidol treatment. Several kinds of
second-generation antipsychotic agents have been used to manage agitation and violence.7Y9
Olanzapine and risperidone are second-generation antipsychotic agents, and they both have more than 1 route of delivery. Lambert et al10 reported that intramuscular olanzapine
(olanzapine IM) was effective in managing the agitation of
psychosis. A naturalistic, open-label study showed that an
olanzapine-treated group made statistically signicant improvement over a group that received conventional treatment.11 Villari
et al8 reported that risperidone, olanzapine, and quetiapine were
found to be as effective as haloperidol and better tolerated.
Hatta et al12 stated that orally disintegrating olanzapine tablets
(olanzapine ODT) and oral risperidone solution (risperidone
OS) produced similar improvements in acutely agitated patients.
The main purpose of this study was to compare efcacy
and safety between rst- and second-generation antipsychotic
agents and between different methods of medication delivery.
METHODS
From the *Department of Psychiatry, Lu-Tung Branch of Changhua Christian
Hospital, Lukang; Department of Psychiatry, Changhua Christian Hospital,
Changhua; Center of General Education, Central Taiwan University of
Science and Technology, Taichung; and Department of Respiratory Care,
Chang Jung Christian University, Tainan, Taiwan.
Received September 16, 2009; accepted after revision March 1, 2010.
Reprints: Nan-Ying Chiu, MD, Department of Psychiatry, Lu Tung Branch
of Changhua Christian Hospital, No. 888, Sec. 2, Lu Tung Rd, Lukang,
Changhua 505, Taiwan (e-mail: 117006@cch.org.tw).
Copyright * 2010 by Lippincott Williams & Wilkins
ISSN: 0271-0749
DOI: 10.1097/JCP.0b013e3181db8715
230
www.psychopharmacology.com
This was a prospective, randomized, rater-blinded study
comparing olanzapine IM, olanzapine ODT, risperidone OS, and
intramuscular haloperidol (haloperidol IM) in an acute care
psychiatric unit for the rst 24 hours after admission.
The study was conducted from January 2007 to January
2008 in the acute care psychiatric ward of Changhua Christian
Hospital. The study protocol was approved by the institutional
review board, and all the subjects in this study provided informed consents. There was no commercial funding for this
study.
The study subjects were male and female patients in the
acute care psychiatric ward who were 18 to 65 years old; had a
Journal of Clinical Psychopharmacology
&
Volume 30, Number 3, June 2010
Copyright @ 2010 Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
&
Journal of Clinical Psychopharmacology
Volume 30, Number 3, June 2010
Comparison of Medications for Acute Agitation
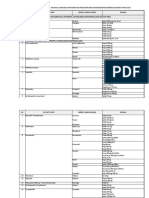
TABLE 1. Subjects Demographic Data
Age, mean T SD (range), y
Sex, male/female
Psychiatric diagnosis
Schizophrenia
Bipolar I disorder
Schizoaffective disorder
Others
Baseline PANSS-EC score,
mean T SD
Baseline ACES score,
mean T SD
Baseline CGI-S Scale score,
mean T SD
10-mg
Olanzapine IM
(n = 11)
10-mg
Olanzapine ODT
(n = 10)
3-mg
Risperidone Solution
(n = 10)
7.5-mg
Haloperidol IM
(n = 11)
37.55 T 11.69 (22Y56)
6/5
40.9 T 11.34 (26Y56)
6/4
34.6 T 11.85 (22Y62)
3/7
36.36 T 12.35 (22Y60)
5/6
0.68
0.55
3
6
1
1
25.55 T 3.8
3
5
0
2
24.7 T 5.01
9
1
0
0
25.00 T 2.58
5
6
0
0
28.18 T 2.82
0.13
1.36 T 0.50
1.60 T 0.70
2.00 T 0.47
1.55 T 0.52
0.08
4.91 T 0.54
5.20 T 1.32
5.10 T 0.74
5.18 T 1.25
0.91
Diagnostic and Statistical Manual, Fourth Edition, Text Revision,
diagnosis of schizophrenia, bipolar I disorder, schizoaffective
disorder, delusional disorder, or other psychotic disorders; and
had an excited component score of 14 or higher on the Positive
and Negative Syndrome Scale (PANSS-EC), with a score of 4 or
higher on at least 1 item (1- to 7-point scale). Pregnant or lactating women; patients with serious medical illnesses; patients with
closed-angle glaucoma; patients with an allergic reaction to olanzapine, risperidone, or haloperidol; or patients who had received
a long-acting antipsychotic agent injection within 30 days were
excluded. Patients were randomly assigned to receive 1 of 4
interventions over a 24-hour period. The assigned process was
performed by random ballot of the 4 interventions. The 4 groups
were 10-mg olanzapine IM, 10-mg olanzapine ODT, 3-mg risperidone OS, and 7.5-mg haloperidol IM.
To evaluate agitation, the excited component of the
PANSS-EC (tension, uncooperativeness, hostility, poor impulse
control, and excitement) and the Agitation-Calmness Evaluation
Scale (ACES) were completed at 15, 30, 45, 60, 75, 90, 105, and
120 minutes and 12 and 24 hours after the rst intervention.
The patients were also assessed with the Clinical Global
ImpressionVSeverity (CGI-S) Scale at baseline and 2, 12, and
24 hours after receiving medications. Possible adverse effects
were recorded by subjective report and objective observation
during the 24 hours. The raters were blind to the treatment
group, and all had received rater training twice before the
study. Rating was performed by senior nurses who have joined a
rater training before the study. A total of 42 patients completed
the study.
Statistical analyses were performed using the software system SPSS PC 10.0 (SPSS Inc, Chicago, Ill). Categorical data
were analyzed using the W2 test. Continuous data were analyzed
using the independent t test and repeated measures analysis of
variance (ANOVA).
the patients had a total PANSS-EC score (mean T SD) of
25.90 T 3.80, an ACES score of 1.62 T 0.58, and a CGI-S Scale
score of 5.10 T 0.98. The patients had a Diagnostic and
Statistical Manual, Fourth Edition, Text Revision, diagnosis of
schizophrenia (n = 20), bipolar I disorder (n = 18), schizoaffective disorder (n = 1), or other psychotic disorders (n = 3).Table 1
lists the demographic data for all the patients in these 4 groups.
Positive and Negative Syndrome Scale
Figure 1 presents the course of change in the PANSS-EC
score from baseline to end point in the 4 groups. We found that
RESULTS
Demographic Data
The 42 patients were randomly assigned to receive 10-mg
olanzapine IM (n = 11), 10-mg olanzapine ODT (n = 10), 3-mg
risperidone oral solution (n = 10), or 7.5-mg haloperidol IM
(n = 11). For the total patient group, the mean T SD age was
37.33 T 11.61 years. At the time of entry into the study,
* 2010 Lippincott Williams & Wilkins
FIGURE 1. Change in PANSS-EC score within 24 hours. To test
for the effects of treatment on PANSS-EC score, 10 time points
repeated-measures ANOVA was used in the 4 groups.
www.psychopharmacology.com
Copyright @ 2010 Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
231
Journal of Clinical Psychopharmacology
Hsu et al
&
Volume 30, Number 3, June 2010
TABLE 2. Change in PANSS-EC Score From Baseline
Comparison (Mean Difference T SE)
15 min
30 min
45 min
60 min
75 min
90 min
105 min
120 min
12 h
24 h
Overall
P
Olz IM vs
Olz ODT
Olz IM vs
Ris OS
Olz IM vs
Hal IM
Olz ODT vs
Ris OS
Olz ODT vs
Hal IM
Ris OS vs
Hal IM
0.004
0.004
0.008
0.010
0.016
0.026
0.046
0.089
0.161
0.157
1.49 T 1.62
1.18 T 1.66
0.94 T 1.68
0.81 T 1.62
0.52 T 1.56
0.17 T 1.54
j0.22 T 1.50
j0.50 T 1.51
j0.63 T 1.38
j0.84 T 1.34
j0.76 T 1.62
j1.09 T 1.66
j0.96 T 1.68
j1.05 T 1.62
j1.06 T 1.56
j1.10 T 1.54
j1.20 T 1.50
j1.15 T 1.51
j0.82 T 1.38
j1.06 T 1.34
j4.55 T 1.58
j5.00 T 1.62
j4.77 T 1.64
j4.55 T 1.58
j4.26 T 1.52
j4.12 T 1.50
j3.88 T 1.46
j3.60 T 1.47
j2.96 T 1.35
j2.97 T 1.31
j2.25 T 1.66
j2.27 T 1.70
j1.90 T 1.71
j1.86 T 1.65
j1.58 T 1.59
j1.27 T 1.57
j0.99 T 1.53
j0.66 T 1.54
j0.19 T 1.41
j0.22 T 1.37
j6.04 T 1.62
j6.18 T 1.66
j5.71 T 1.68
j5.36 T 1.62
j4.78 T 1.56
j4.28 T 1.54
j3.66 T 1.50
j3.10 T 1.51
j2.33 T 1.38
j2.12 T 1.34
j3.79 T 1.62
j3.91 T 1.66
j3.81 T 1.68
j3.50 T 1.62
j3.20 T 1.56
j3.01 T 1.54
j2.67 T 1.50
j2.44 T 1.51
j2.14 T 1.38
j1.91 T 1.34
P G 0.05 was regarded as statistically signicant. Overall P was analyzed by repeated measures ANOVA. Overall P values in italics are statistically
signicant. The comparison between the 4 groups tested was done using post hoc analysis. The P values in italics are less than 0.05.
Hal IM indicates haloperidol intramuscular; Olz IM, olanzapine intramuscular; Olz ODT, olanzapine orally disintegrating tablet; Ris OS, risperidone
oral solution.
there were signicant differences in the PANSS-EC scores
between the 4 interventions at points 15, 30, 45, 60, 75, and
90 minutes after injection. We found that a more signicant
difference occurred in the earlier period after intervention. The
patients who received olanzapine IM or olanzapine ODT had
signicantly greater improvement in PANSS-EC scores than
the patients who received haloperidol IM at points 15, 30, 45,
60, 75, and 90 minutes after initiation of the treatment. However,
there were no signicant differences between olanzapine IM
and risperidone OS, olanzapine ODT and risperidone OS, risperidone OS and haloperidol IM, or olanzapine IM and olanzapine ODT at these points. After 90 minutes, we found no
signicant differences among the 4 groups. Table 2 shows these
differences at each point in time.
Agitation-Calmness Evaluation Scale
The changes in ACES score in the 4 groups are shown
in Figure 2. There were no differences in the mean ACES
score changes among the groups at 15, 30, 45, 60, 75, 90, 105,
120 minutes and 12 and 24 hours after the rst treatment.
Clinical Global ImpressionVSeverity Scale
The changes in the CGI-S Scale score in the 4 groups are
shown in Figure 3. No differences in the mean CGI-S Scale
scores were found from baseline to 24 hours.
Adverse Effects
The most commonly reported and observed adverse effects
related to medications were found in all the 4 groups. Drowsiness was most common. Olanzapine IM and olanzapine ODT
FIGURE 2. Change in ACES Scale score within 24 hours. hal IM
indicates haloperidol intramuscular; olz IM, olanzapine
intramuscular; olz ODT, olanzapine orally disintegrating tablet;
ris OS, risperidone oral solution.
232
www.psychopharmacology.com
FIGURE 3. Change in CGI-S Scale score within 24 hours.
* 2010 Lippincott Williams & Wilkins
Copyright @ 2010 Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
Journal of Clinical Psychopharmacology
&
Volume 30, Number 3, June 2010
produced more drowsiness than oral risperidone and haloperidol IM, but the difference was not signicant.
DISCUSSION
The choices for the management of agitation in a psychiatric ward are multiple and include behavioral intervention,
pharmacological intervention, environmental intervention, and
emotional management. Pharmacological interventions include
benzodiazepines and antipsychotic agents.3
Olanzapine and risperidone are both second-generation
antipsychotic agents. In our study, olanzapine IM and olanzapine ODT produced greater improvement in the PANSS-EC
scores than did haloperidol IM within 90 minutes after the
treatment. There was no signicant difference after 90 minutes
among the 4 groups. Wright et al reported that signicant differences between olanzapine IM and haloperidol IM were observed at 15, 30, and 45 minutes after the rst injection.13 This
nding is supported by our results. Olanzapine is more effective
than haloperidol in the early phase after the intervention.
Olanzapine, a dopamine/serotonin antagonist in the thienobenzodiazepine class, is available in tablet, oral disintegrating
tablet, and intramuscular injection forms.
Castle et al7 reported that olanzapine IM provided somewhat more effective control of acute agitation than did other
assessed IM antipsychotic agents. Wright et al13 reported that
olanzapine IM represented a rapid, effective, and safe treatment
of acute agitation in schizophrenia. Villari et al8 reported that
oral olanzapine was as effective as oral haloperidol and better
tolerated. A naturalistic, open-label study demonstrated that
20-mg oral olanzapine was effective, rapid, and safe in patients
with severe agitation.11 The evidence from the previous studies
supported the observation that olanzapine is effective in the
management of agitation with different ways of delivery. To the
best of our knowledge, no previous study has compared olanzapine IM and olanzapine ODT.
Options in the pharmacotherapy for acute agitation include
parenteral administration of antipsychotic agents to facilitate the
onset of drug action and quickly alleviate symptoms. We found
that olanzapine ODT produced a better response in PANSS-EC
scores than did olanzapine IM within 60 minutes after the treatment; however, the difference was not statistically signicant.
Intramuscular injectable antipsychotic agents offer advantages
over the traditional oral tablets in the emergency treatment of
schizophrenia in its acute phase. However, situations occur
wherein patients have difculty swallowing traditional oral tablets, patients may spit out liquid medications, or an injectable
formulation is contraindicated or unacceptable.14 Intramuscular injection is also a more aggressive treatment than oral
medication. Intramuscular injection might result in difculty in
maintaining a therapeutic relationship. The orally disintegrating
formulation has been developed as an alternative to improve
medication compliance. Olanzapine ODT dissolves rapidly on
contact with saliva in the mouth and has a more rapid onset of
action.15,16 Olanzapine ODT could solve the problem of poor
cooperation by agitated patients because it is easy to handle
and convenient to use. From an economic perspective, olanzapine ODT is cheaper than olanzapine IM and haloperidol in
Taiwan. Olanzapine ODT might therefore be another choice in
the management of acute agitation.
No difference in extrapyramidal symptoms was found
among the 4 groups in our study. Extrapyramidal symptoms do
occur after emergency intervention and might result in poor adherence to the same medication or cause problems in the relationship between patient and physician. Avoiding medications
* 2010 Lippincott Williams & Wilkins
Comparison of Medications for Acute Agitation
that easily lead to extrapyramidal symptoms is important for
later treatment. Second-generation antipsychotic agents may be a
better choice in this regard.
Our study had some limitations. First, our sample size
was small. Second, we had no placebo group. Third, we did
not assess interrater reliability. In the future, well-designed, randomized, controlled studies with adequate subjects are needed
to provide more evidence to support a preference for these
medications.
CONCLUSIONS
These ndings suggest that olanzapine IM, olanzapine
ODT, and risperidone OS are as effective as haloperidol IM in
the treatment of acute agitation. There were no signicant differences between olanzapine IM, olanzapine ODT, and risperidone OS. Olanzapine IM and ODT were more effective in the
early phase after intervention than haloperidol IM. Olanzapine
ODT was effective, convenient, and well tolerated in rapidly
reducing acute agitation. It offers clinicians a therapeutic
alternative.
ACKNOWLEDGMENTS
The authors thank Mr Yi-Shin Lin and Mrs Yu-Jiun Chang
for assisting in the statistical analyses.
AUTHOR DISCLOSURE INFORMATION
The authors have nothing to disclose.
REFERENCES
1. Grassi L, Peron L, Marangoni C, et al. Characteristics of violent
behaviour in acute psychiatric in-patients: a 5-year Italian study.
Acta Psychiatr Scand. 2001;104:273Y279.
2. Lindenmayer JP. The pathophysiology of agitation. J Clin Psychiatry.
2000;61(suppl 14):5Y10.
3. Battaglia J. Pharmacological management of acute agitation. Drugs.
2005;65:1207Y1222.
4. Battaglia J, Moss S, Rush J, et al. Haloperidol, lorazepam, or both
for psychotic agitation? A multicenter, prospective, double-blind,
emergency department study. Am J Emerg Med. 1997;15:335Y340.
5. Salzman C, Green AI, Rodriguez-Villa F, et al. Benzodiazepines
combined with neuroleptics for management of severe disruptive
behavior. Psychosomatics. 1986;27:17Y22.
6. Buckley PF. The role of typical and atypical antipsychotic medications
in the management of agitation and aggression. J Clin Psychiatry.
1999;60(suppl 10):52Y60.
7. Castle DJ, Udristoiu T, Kim CY, et al. Intramuscular olanzapine
versus short-acting typical intramuscular antipsychotics: comparison
of real-life effectiveness in the treatment of agitation. World J Biol
Psychiatry. 2009;10:43Y53.
8. Villari V, Rocca P, Fonzo V, et al. Oral risperidone, olanzapine and
quetiapine versus haloperidol in psychotic agitation. Prog
Neuropsychopharmacol Biol Psychiatry. 2008;32:405Y413.
9. Kinon BJ, Stauffer VL, Kollack-Walker S, et al. Olanzapine
versus aripiprazole for the treatment of agitation in acutely ill
patients with schizophrenia. J Clin Psychopharmacol. 2008;28:
601Y607.
10. Lambert M, Huber CG, Naber D, et al. Treatment of severe agitation
with olanzapine in 166 patients with schizophrenia, schizoaffective,
or bipolar I disorder. Pharmacopsychiatry. 2008;41:182Y189.
www.psychopharmacology.com
Copyright @ 2010 Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
233
Journal of Clinical Psychopharmacology
Hsu et al
&
Volume 30, Number 3, June 2010
11. Pascual JC, Perez V, Martin JL, et al. Olanzapine orally-disintegrating
tablet in severe psychotic agitation: a naturalistic study. Actas Esp
Psiquiatr. 2007;35:47Y51.
14. Chue P, Jones B, Taylor CC, et al. Dissolution profile, tolerability,
and acceptability of the orally disintegrating olanzapine tablet in
patients with schizophrenia. Can J Psychiatry. 2002;47:771Y774.
12. Hatta K, Kawabata T, Yoshida K, et al. Olanzapine orally
disintegrating tablet vs. risperidone oral solution in the treatment
of acutely agitated psychotic patients. Gen Hosp Psychiatry.
2008;30:367Y371.
15. Reeves RR, Torres RA. Onset of action of orally disintegrating
olanzapine versus conventional olanzapine. South Med J.
2004;97:212.
13. Wright P, Birkett M, David SR, et al. Double-blind,
placebo-controlled comparison of intramuscular olanzapine and
intramuscular haloperidol in the treatment of acute agitation in
schizophrenia. Am J Psychiatry. 2001;158:1149Y1151.
234
www.psychopharmacology.com
16. Markowitz JS, DeVane CL, Malcolm RJ, et al. Pharmacokinetics
of olanzapine after single-dose oral administration of standard
tablet versus normal and sublingual administration of an orally
disintegrating tablet in normal volunteers. J Clin Pharmacol.
2006;46:164Y171.
* 2010 Lippincott Williams & Wilkins
Copyright @ 2010 Lippincott Williams & Wilkins. Unauthorized reproduction of this article is prohibited.
Potrebbero piacerti anche
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (890)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Textbook of Personality Disorders PDFDocumento729 pagineTextbook of Personality Disorders PDFAnonymous 4LIXFKU96% (25)
- Textbook of Personality Disorders PDFDocumento729 pagineTextbook of Personality Disorders PDFAnonymous 4LIXFKU96% (25)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Nursing Care Plan For "Herniated Nucleus Pulposus Ruptured Inter Vertebral Disc"Documento9 pagineNursing Care Plan For "Herniated Nucleus Pulposus Ruptured Inter Vertebral Disc"jhonroks100% (7)
- MRCS Part A 10 Jan 2017 Recalls (DR Salah Group) .Documento7 pagineMRCS Part A 10 Jan 2017 Recalls (DR Salah Group) .Umair Ashfaq0% (1)
- Maual de Terapia SistemicaDocumento60 pagineMaual de Terapia Sistemicaapi-2631069682% (17)
- 2011 BSQValidacioDocumento11 pagine2011 BSQValidacioAnonymous 4LIXFKUNessuna valutazione finora
- Maual de Terapia SistemicaDocumento60 pagineMaual de Terapia Sistemicaapi-2631069682% (17)
- Some Thoughts About Schizoid Dynamics Nancy McwilliamsDocumento31 pagineSome Thoughts About Schizoid Dynamics Nancy Mcwilliams0x2362100% (1)
- 2007 Article 381Documento15 pagine2007 Article 381Cintia Ferris LanteroNessuna valutazione finora
- Diabetes y DepresionDocumento9 pagineDiabetes y DepresionAnonymous 4LIXFKUNessuna valutazione finora
- StressDisorder-PTSD - Guideline 2011Documento12 pagineStressDisorder-PTSD - Guideline 2011Jose Perez Huircacho CacaowebNessuna valutazione finora
- BullyingDocumento7 pagineBullyingAnonymous 4LIXFKUNessuna valutazione finora
- StressDisorder-PTSD - Guideline 2011Documento12 pagineStressDisorder-PTSD - Guideline 2011Jose Perez Huircacho CacaowebNessuna valutazione finora
- AdhdDocumento3 pagineAdhdfahruludinNessuna valutazione finora
- Trico Tilo Man I An I Hms 317347Documento16 pagineTrico Tilo Man I An I Hms 317347Anonymous 4LIXFKUNessuna valutazione finora
- Neuroimaging in Anxiety Disorders PDFDocumento9 pagineNeuroimaging in Anxiety Disorders PDFAnonymous 4LIXFKUNessuna valutazione finora
- Neurobiological Basis ofDocumento30 pagineNeurobiological Basis ofAnonymous 4LIXFKUNessuna valutazione finora
- The Analysis of Childrens DrawingsDocumento6 pagineThe Analysis of Childrens DrawingsAnonymous 4LIXFKUNessuna valutazione finora
- Neuroanatomia Funcional Del PlaceboDocumento10 pagineNeuroanatomia Funcional Del PlaceboAnonymous 4LIXFKUNessuna valutazione finora
- Medical Surgical Nursing Module 12Documento45 pagineMedical Surgical Nursing Module 12weissNessuna valutazione finora
- Wellness Course Notes 2Documento1 paginaWellness Course Notes 2Eywon AbundoNessuna valutazione finora
- Caring Adoption Associates: Medical Examination Report of Prospective Adoptive ParentDocumento1 paginaCaring Adoption Associates: Medical Examination Report of Prospective Adoptive ParentaniketsethiNessuna valutazione finora
- Meningitis MedscapeDocumento73 pagineMeningitis MedscapeBujangNessuna valutazione finora
- Low Cost Portable Ventilator DesignDocumento8 pagineLow Cost Portable Ventilator DesignRashmi SinghNessuna valutazione finora
- VEC Question Bank on Biomedical InstrumentationDocumento13 pagineVEC Question Bank on Biomedical InstrumentationNisha ManiNessuna valutazione finora
- Internal Medicine Mar 2022Documento8 pagineInternal Medicine Mar 2022Sanielle Karla Garcia LorenzoNessuna valutazione finora
- SEMINAR ON MULTIPLE PREGNANCY ContentDocumento21 pagineSEMINAR ON MULTIPLE PREGNANCY ContentMonika shankar0% (1)
- Ad70 PDFDocumento7 pagineAd70 PDFDnyaneshwar Dattatraya PhadatareNessuna valutazione finora
- Otc DrugsDocumento71 pagineOtc DrugsEthan Morgan100% (2)
- Literature Review 1Documento5 pagineLiterature Review 1api-582800401Nessuna valutazione finora
- AIJ Clasif PRINTO 2019Documento9 pagineAIJ Clasif PRINTO 2019Michael ParksNessuna valutazione finora
- Pedia OphthaDocumento29 paginePedia OphthajeffaguilarNessuna valutazione finora
- FreeStyle Libre - Sensor Adhesion GuideDocumento1 paginaFreeStyle Libre - Sensor Adhesion GuidemgkyawthuhlaingNessuna valutazione finora
- Vas 1Documento10 pagineVas 1Abdul Latiful KhabirNessuna valutazione finora
- Gout Presentation Group 2 Defines Metabolic Disorder and ManagementDocumento10 pagineGout Presentation Group 2 Defines Metabolic Disorder and ManagementVon Valentine MhuteNessuna valutazione finora
- Chronic HK NewInsightDocumento107 pagineChronic HK NewInsightKHALID NAAMNessuna valutazione finora
- Understanding the Key Elements of a HemogramDocumento53 pagineUnderstanding the Key Elements of a Hemogramromanas25Nessuna valutazione finora
- Ultimately, The Greatest Lesson That COVID-19 Can Teach Humanity Is That We Are All in This Together.Documento3 pagineUltimately, The Greatest Lesson That COVID-19 Can Teach Humanity Is That We Are All in This Together.SanjeevNessuna valutazione finora
- Polydioxanone Thread LiftingDocumento4 paginePolydioxanone Thread LiftingGLORIANessuna valutazione finora
- Patient HIV and Urine Test ResultsDocumento5 paginePatient HIV and Urine Test ResultsPsyche's CupidoNessuna valutazione finora
- Virtual ColonosDocumento200 pagineVirtual ColonosDiana VershyninaNessuna valutazione finora
- Genetic Etiologies of Leukocyte Adhesion DefectsDocumento6 pagineGenetic Etiologies of Leukocyte Adhesion DefectsCosmin BarbosNessuna valutazione finora
- Journal ClubDocumento12 pagineJournal ClubAnonymous ibmeej9Nessuna valutazione finora
- Medical Terms by MJADocumento2 pagineMedical Terms by MJAMacy DysancoNessuna valutazione finora
- Psychosis 2020Documento10 paginePsychosis 2020moebius70Nessuna valutazione finora
- Standar Obat Nayaka Siloam Okt 2019 Receive 30092019Documento33 pagineStandar Obat Nayaka Siloam Okt 2019 Receive 30092019Retno Agusti WulandariNessuna valutazione finora
- 02-09 2022 Pharm Pediatrics 2022 R4Documento44 pagine02-09 2022 Pharm Pediatrics 2022 R4Amira HelayelNessuna valutazione finora