Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Makalah
Caricato da
I Nyoman WidiyanaTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Makalah
Caricato da
I Nyoman WidiyanaCopyright:
Formati disponibili
Acta Orthop. Belg.
, 2005, 71, 590-596
ORIGINAL STUDY
Ultrasound and colour Doppler sonography in acute osteomyelitis in children
Quamar AZAM, Ibne AHMAD, Mazhar ABBAS, Anjum SYED, Faisal HAQUE
From the Jawaharlal Nehru Medical College, Aligarh Muslim University, Aligarh, India
Early diagnosis of osteomyelitis is of paramount
importance to avoid irreversible sequelae. This often
requires a multimodal approach. The purpose of the
present study was primarily to evaluate how ultrasound might be useful in early diagnosis of
osteomyelitis in the paediatric age group. The evolution of ultrasound findings with progression and resolution of disease was also analysed.
In this prospective study, 55 children with osteomyelitis of limbs were subjected to sonographic
examination including colour Doppler study. The
sonographic machine used was a LOGIC-500, using
a linear multifrequency transducer (7-9 MHz).
Ultrasound guided aspiration was performed in all
cases showing sub-periosteal accumulation of fluid,
and the aspirate was sent for culture and sensitivity
report. Surgical drainage was undertaken in all
patients in which a sub-periosteal abscess was
demonstrated.
Anechoic fluid accumulation contiguous with bone
was highly suggestive of osteomyelitis, whereas presence of soft tissue between the bone and the fluid suggested a non-osseous origin of the fluid. Subperiosteal accumulation of fluid was seen in 42 cases
(76.3%). A subperiosteal abscess with periosteal
reaction was demonstrated in 35 children (63.63%).
Colour Doppler study revealed increased vascular
flow within or around the affected periosteum in all
cases. Concurrent involvement of a joint was noted in
13 cases.
Ultrasound is a rapid, cheap, easily available, nonionising and reasonably accurate diagnostic modality. It also helps in localising the lesion for diagnostic
aspiration. Serial ultrasound and technical innovations such as colour Doppler sonography further
Acta Orthopdica Belgica, Vol. 71 - 5 - 2005
help in monitoring the progression and resolution of
the disease.
Key words : osteomyelitis ; children ; ultrasound ;
colour Doppler.
INTRODUCTION
Osteomyelitis is a significant cause of morbidity
in childhood with a reported incidence of 1 in
5000 children less than 13 years of age. Early diagnosis of osteomyelitis is of paramount importance (14), so that definitive and adequate treatment
is not delayed, an important step to avoid irreversible damage and morbidity.
The clinical diagnosis of osteomyelitis especially in the early stage still remains a challenge. A
Quamar Azam, MD, MS (orthopaedics) Registrar.
Mazhar Abbas, MD, MS (orthopaedics) Consultant.
Department of Orthopaedic Surgery, J.N.M.C., A.M.U.,
Aligarh, India.
Ibne Ahmad, MD (Radiodiagnosis) Reader.
Anjum Syed, MD (Radiodiagnosis) Registrar.
Faisal Haque, MD, (Radiodiagnosis) Consultant.
Department of Radiodiagnoasis, J.N.M.C., A.M.U., Aligarh,
India.
Correspondence : Dr Quamar Azam, Department of
Orthopaedic Surgery, J.N.M.C., A.M.U., Aligarh, India.
E-mail : qazam47@rediffmail.com.
2005, Acta Orthopdica Belgica.
ACUTE OSTEOMYELITIS IN CHILDREN
multimodal approach is often needed to establish
the diagnosis (1). This involves routine laboratory
tests such as white blood cell count (WBC), erythrocyte sedimentation rate (ESR) and C-reactive
protein (CRP), bacteriological tests such as blood
and bone culture and radiological examination.
Markers of the acute phase reactants are nonspecific, and plain radiographs are unable to pick
up early changes in osteomyelitis. In such circumstances, bone scan (10) and magnetic resonance
imaging (MRI) (13, 15) remain sensitive tests.
Unfortunately, these modalities of investigations
are not available in all centers, especially so in
developing countries like ours. Furthermore,
expenses incurred and radiation associated with CT
and bone scan make repeated use of these tests
undesirable and also beyond reach of most people.
Well-controlled trials have already established
the value of ultrasound imaging in areas like developmental dysplasia of the hip in infants, pathology
of the rotator cuff, tendon and ligament abnormalities, monitoring of limb lengthening etc. Careful
review of literature (3, 4, 7-9, 17) further revealed
that ultrasound is emerging as a new imaging
modality for the early diagnosis of osteomyelitis.
This allows early detection of an occult collection
and provides guidance for diagnostic aspiration
(for bacteriological culture and sensitivity).
Ultrasound also detects concurrent adjacent joint
involvement.
The purpose of the present study was primarily
to evaluate how ultrasound might be useful in early
diagnosis of osteomyelitis and also to analyse the
evolution of sonographic findings with the progression or resolution of the disease.
MATERIALS AND METHODS
Over a period of one and a half year from June 2002
to December 2003, 55 patients in the age group of
7 months to 12 years were diagnosed to have osteomyelitis. The clinical diagnosis of osteomyelitis was
based on the diagnostic criteria established by Petola
and Vahvanen (11). They considered that in the presence
of two of the following four criteria, the diagnosis of
osteomyelitis was firm :
1. Pus aspirated from bone,
591
2. Positive bone or blood culture,
3. Classic symptoms of localised pain, swelling, warmth
and limited range of motion (ROM) of the adjacent
joint,
4. Radiographic changes typical of osteomyelitis.
Operative findings in 42 cases and MR imaging in
nine cases further confirmed the diagnosis of
osteomyelitis.
Haematological examination including pus culture,
radiographs of the part (anteroposterior and lateral
views) and sonographic examination including colour
Doppler study were performed in all patients at the time
of admission. Haematological and sonographic examinations were repeated as and when required to reaffirm
the diagnosis and also to obtain a correlation between
these and clinical progression.
The sonographic machine used was LOGIC-500 by
GE (General Electrical) using a linear multifrequency
transducer (7-9 MHz). Scans (longitudinal and transverse) covering the full thickness of the relevant areas
were obtained. Both proximal and distal joints were
always scanned as part of the ultrasonographic examination. Vascular images were evaluated by colour Doppler
ultrasonography using low velocity and filter setting.
Dynamic colour adjustment was done during the examination to maximise the visualisation of the blood flow.
The unaffected contralateral side was also examined for
comparison when required. This allowed detection of
subtle changes.
Sonography demonstrated normal muscle layers to be
hypoechoic with linear echogenic striations separating
the layers. The cortex of normal bone appeared as a
dense echogenic line with a smooth surface. Vascular
structures were clearly visualised with colour Doppler
flow analysis.
Ultrasonography-guided aspiration of pus was performed under local anaesthesia or sedation (depending
on age and co-operation of the patient) in cases where
subperiosteal fluid was demonstrated, and the pus thus
obtained was sent for Gram staining, culture and sensitivity. A large bore, shallow, tapered needle was used for
the aspiration. Care was taken to insert the needle till it
came in contact with the bone. If aspiration at this point
failed to withdraw pus, the needle was twisted till it was
felt to penetrate the bone.
All cases which demonstrated an abnormal collection
of fluid adjacent to the bone without intervening soft tissue, underwent surgery. Intravenous (IV) antibiotic was
started in the remaining 13 cases that showed only deep
soft tissue swelling adjacent to the affected bone. Repeat
Acta Orthopdica Belgica, Vol. 71 - 5 - 2005
592
Q. AZAM, I. AHMAD, M. ABBAS, A. SYED, F. HAQUE
Table I. Anatomical Distribution
Site
No. of patients
Proximal Femur
Distal Femur
Proximal Tibia
Distal Tibia
Proximal Humerus
Distal Humerus
12
25
8
3
4
3
sonographic examination was performed on the third
day after initiation of therapy.
RESULTS
Fifty-five children, 38 boys and 17 girls ranging
in age from 7 months to 15 years were included in
the study. They had systemic features of acute
infection and the duration of symptoms varied from
2 to 15 days, with a mean duration of symptoms of
4.6 days at the time of admission. High fever,
inability to use the extremity, along with local
swelling and redness were the most common symptoms, while local tenderness and painful restriction
of movement were the signs most commonly elicited. In our series the femur was the bone most commonly involved, followed by the tibia ; the hip was
the joint most commonly involved, followed by the
knee. The anatomical sites involved are shown in
table I. Concurrent involvement of a joint was
noted in 13 cases.
No radiographic findings were appreciated in
patients symptomatic for up to seven days at the
time of admission. Soft tissue swelling with blurring of muscle planes could be seen in eight cases
which presented after seven days. Periosteal reaction, rarification and cortical erosion were visible
only in four patients with symptoms of at least
10 days duration.
Sonographic examination in patients with symptoms of less than three days duration demonstrated
increased soft tissue swelling adjacent to bone in
ten children, while in the remaining three patients
no abnormality was detected. In nine of the
13 cases, the diagnosis was confirmed by MR
imaging, however the diagnosis in the other four
cases was based on the clinical criteria of Pettola
Acta Orthopdica Belgica, Vol. 71 - 5 - 2005
c
Fig. 1. a) Longitudinal sonogram of right femur (anterolateral aspect) showing elevated periosteum with hypoechoic
collection adjacent to bone ; b) Colour and spectral Doppler of
the same patient showing increased vascularity around the
involved periosteum ; c) Colour Doppler and grey scale image
of the same patient, showing hypoechoic subperiosteal collection with increased vascularity. Scan of normal right femur is
shown for comparison.
593
ACUTE OSTEOMYELITIS IN CHILDREN
and Vahvanen (11). All but two of these children
showed clinical improvement following conservative treatment (IV antibiotic). Repeat sonographic
examination performed in these two cases revealed
a subperiosteal collection. Surgical drainage was
immediately performed in both of them.
Subperiosteal fluid collection was demonstrated
in 42 patients (figs 1, 2) who presented after three
days. Pus was aspirated in all of them under real
time sonographic guidance. These children underwent surgical drainage and had remarkable
improvement.
A positive culture was reported in 81.8%
(36 cases) of the aspirates. Positive blood culture
Fig. 2. Sonogram of left femur (posterior aspect) demonstrating periosteal elevation and subperiosteal collection.
Fig. 3. a) Grey scale and colour Doppler scan showing large
hypoechoic collection adjacent to left radius. The bone cortex
is irregular and vascularity around it is increased ; b) Sagittal
sonogram of both hips of the same patient showing effusion in
both hips with hypoechoic collection at the neck of left femur
with elevated periosteum.
Table II. Relevant details of radiographic and sonographic features according to duration of symptoms
Duration of symptoms
Number of cases
Radiographic findings
Sonographic features (number)
1-3 days
13
No abnormality
4-7 days
30
No abnormality
8-15 days
12
Blurring of muscle planes
adjacent to bone
Rarification
Periosteal reaction
No abnormality (3)
Soft tissue swelling adjacent to bone (10)
Soft tissue swelling adjacent to bone
Subperiosteal abscess
Increased vascularity in/around periosteum
Periosteal reaction
Subperiosteal abscess
Periosteal reaction
Cortical erosion, irregularity and cloacae
Acta Orthopdica Belgica, Vol. 71 - 5 - 2005
594
Q. AZAM, I. AHMAD, M. ABBAS, A. SYED, F. HAQUE
Fig. 4. Ultrasonographic scan of right upper tibia showing
periosteal reaction and subperiosteal collection.
Fig. 5. Longitudinal scan of the anterior aspect of the right
upper third of the femur demonstrating small cortical defects
(cloacae) with a hypoechoic collection.
was obtained in 24 patients (43.63%). Common
organisms isolated in our series were Staphylococcus aureus (58.18%), Gr-A Streptococcus
(9.09%), S. pneumoniae (7.27%), H. influenzae
(18.18%) and others (7.27%).
Figure 3 shows scans of a child diagnosed to
have multifocal osteomyelitis. Other important
sonographic features such as periosteal reaction
(fig 4), cortical erosions, cortical thickening and
cloacae (fig 5), appeared only after the seventh day
with symptoms (table II). Concurrent septic arthritis was noted in 13 cases (fig 6).
The location of fluid in relation to bone was a
very valuable finding in discriminating between
osteomyelitis and soft tissue collections. Fluid collection contiguous with bone was highly suggestive
of osteomyelitis, whereas presence of any soft tissue between the bone and the fluid tilted the diagnosis in favour of a non- osseous origin of the fluid.
Interestingly, three of the 42 children who did
quite well after surgical debridement and had no
clinical signs of infection, demonstrated a substantial collection of pus when routine sonographic
examination was performed at the time of discharge as a part of our study. Surgical drainage was
performed in all these cases and they were advised
antibiotics for a longer duration.
Patients who responded satisfactorily showed no
abscess on ultrasound examination at the time of
discharge, and vascularity in and around the affect-
ed periosteum was decreased. Serum CRP and ESR
were elevated in all the cases at the time of admission. The CRP value decreased significantly or
became normal at the fifth day of treatment in all
such cases. However, the ESR either decreased
minimally or remained elevated at that moment.
Acta Orthopdica Belgica, Vol. 71 - 5 - 2005
DISCUSSION
Early diagnosis of acute osteomyelitis and timely institution of appropriate therapy is of paramount importance in osteomyelitis of children to
achieve good outcome. Better imaging technology
and improved antibiotic therapy have improved
diagnostic accuracy and decreased morbidity.
Nevertheless, overlapping clinical symptoms and
signs, non-specificity of haematological parameters, positive blood culture in only 25-50% cases,
inability of plain radiographs to pick up early
changes, may make the diagnosis of osteomyelitis
in children (especially in the early stage) a formidable challenge. A multimodal approach involving
plain radiographs, bone scintigraphy (10), CT and
MRI (13, 15) has been used for diagnosis of infection of the musculo-skeletal system.
Diagnostic modalities like bone scan, CT and
MRI are sensitive but are not commonly available,
especially in developing countries like ours. In
addition, the expenses incurred are beyond reach of
common people. Ionisation hazards further make
595
ACUTE OSTEOMYELITIS IN CHILDREN
Fig. 6. Sonogram of left humerus with shoulder joint showing periosteal reaction with linear hypoechoic subperiosteal
fluid accumulation with effusion in the joint.
repetition of these tests to monitor the clinical
course of the disease undesirable and unacceptable.
In such circumstances, ultrasound facilitates an
early diagnosis of osteomyelitis, permits real time
guided aspiration for bacteriological examination
and helps in monitoring success of therapy.
Capitanio and Kirpatrick (2) described that soft
tissue swelling and loss of muscle planes are discernible in plain radiograph as early as 48 hours.
However, in our study, these features could not be
seen before 7 days. Destructive changes in the bone
strongly suggestive of osteomyelitis were seen on
plain radiographs no earlier than 10 days after the
onset of osteomyelitis.
We experienced that an anechoic fluid collection, when seen in direct contact with bone, was
highly suggestive of osteomyelitis. Serial ultrasound examination revealed that the spectrum of
findings changes with the duration of the disease.
Deep soft tissue swelling adjacent to bone was the
earliest finding, noted as early as the second day of
symptoms, followed by a thin layer of subperiosteal fluid, subperiosteal abscess and periosteal
reaction in patients with symptoms duration of
more than three days. In patients who presented
late after 7-10 days, cortical erosion and cloacae
were noted. Demonstration of intervening soft tissue between the fluid and bone suggests a nonosseous origin of the fluid. These findings corrob-
orated with similar findings noted by authors like
Sarti (12), Abiri et al (1) and Mah et al (8).
Subperiosteal fluid accumulation was seen in
42 cases (76.36%). Subperiosteal abscess and
periosteal reaction together was seen in 35 children
(63.63%). Howard and Einhorn (5) reported
periosteal reaction in 100% of cases. Kaiser and
Rosenberg (6) showed subperiosteal fluid in 41% of
cases and Mah et al (8) demonstrated periosteal
reaction and subperiosteal accumulation in 50% of
cases.
We compared serial sonographic findings following treatment with clinical status and haematological parameters (CRP and ESR) in an attempt to
draw a correlation among them. ESR proved to be
neither a reliable indicator of disease nor a valuable
tool for following the resolution of infection as it
lags behind the improvement seen clinically. Serum
CRP and ultrasound findings correlated well with
clinical improvement. Our study indicated that sonographic findings and increased vascularity (on colour
Doppler sonography) are sufficiently accurate in
monitoring the disease. Previous literature (11, 16)
has also emphasised the importance of serum CRP
as a valuable indicator to monitor the disease.
Authors of the present study are of the view that
pus should be drained as quickly as possible and
early demonstration of subperiosteal abscess by
ultrasound helped in diagnostic aspiration, early
surgical intervention and in deciding the approach
of surgery. Howard and Einhorn (5) and Harris (4)
also feel that all cases of subperiosteal abscess
must be drained. This is in contrast with Mah et
al (8), who observed that subperiosteal abscesses of
3 mm or even more resolved completely with
antibiotic treatment alone.
CONCLUSION
Ultrasound is a rapid, easily available, portable,
non-invasive, non-ionising, cheap and reasonably
accurate diagnostic modality, for screening and
early diagnosis of osteomyelitis and concurrent
septic arthritis in all patients who are clinically
suspected of having osteomyelitis.
Ultrasound helps in differentiating conditions
with overlapping clinical symptoms and signs such
Acta Orthopdica Belgica, Vol. 71 - 5 - 2005
596
Q. AZAM, I. AHMAD, M. ABBAS, A. SYED, F. HAQUE
as soft tissue abscess, pyomyositis and cellulitis.
Furthermore, by localising the lesion it guides
for diagnostic aspiration. Ultrasonography is
quantifiable and reproducible, and we recommend
its use as a first line of investigation in such situations. Serial ultrasound and technical innovations
such as colour Doppler examination reasonably
help in monitoring the progression or resolution of
disease process.
However in the absence of localising features
(i.e. when survey of a large area is required) and in
suspected multifocal osteomyelitis, scintigraphy
and MR imaging are better suited diagnostic
modalities.
7.
8.
9.
10.
11.
12.
REFERENCES
1. Abiri MM, Kirpekar M, Ablow RC. Osteomyelitis :
detection with ultrasonography. Radiology 1989 ; 172 :
509-511.
2. Capitanio M, Kirpatrick J. Early roentgen observations
in acute osteomyelitis. Am J Roentgenol 1970 ; 108 : 488496.
3. Chao HC, Lin SJ, Huang YC, Lin TY. Color Doppler
ultrasonographic evaluation of osteomyelitis in children.
J Ultrasound Med 1999 ; 18 : 729-734.
4. Harris NH. Some problems in the diagnosis and treatment
of acute osteomyelitis. J Bone Joint Surg 1960 ; 42-B :
535-541.
5. Howard CB, Einhorn MS. Ultrasound in the detection of
subperiosteal abscess. J Bone Joint Surg 1991 ; 73-B :
175-176.
6. Kaiser S, Rosenberg M. Early detection of subperiosteal
abscess by ultrasonography : a means for further success-
Acta Orthopdica Belgica, Vol. 71 - 5 - 2005
13.
14.
15.
16.
17.
ful treatment in pediatric osteomyelitis. Pediatr Radiol
1994 ; 24 : 336-339.
Loyer EM, DuBrow RA, David CL et al. Imaging of
superficial soft tissue infection : sonographic findings in
cases of cellulitis and abscess. Am J Roentgenol 1996 ;
166 : 149-152.
Mah ET, Le Quesne GW, Gent RJ, Patersson DC. Acute
osteomyelitis in children. J Bone Joint Surg 1994 ; 76-B :
969-974.
Nath AK, Sethu AU. Use of ultrasonography in
osteomyelitis. Br J Radiol 1992 ; 65 : 649-652.
Paterson DC, Foster BK & Savage JP. The present status of bone scanning in clinical orthopaedic diagnosis.
Recent Advances in Orthopaedics. 1987 ; 5 : 19-41.
Pettola H, Vahvanen V, Aalto K. Fever, C-reactive protein
and ESR in monitoring recovery from septic arthritis : A
preliminary study. J Pediatr Orthop 1984 ; 4 : 170-174.
Sarti DA. Ultrasonography of the lower extremity. In :
Sarti DA and Sample WF (eds). Diagnostic Ultrasound.
1st ed, G.K. Hall &Co., Boston, pp 486-501.
Schlesinger AE, Hernandez RJ. Diseases of the musculoskeletal system in children : Imaging with CT,
Sonography and MR. Am J Roentgenol 1992 ; 158 : 729741.
Trueta J, Morgan JD. Late results in the treatment of
one hundred cases of acute hematogenous osteomyelitis.
Br J Surg 1954 ; 41 : 449-457.
Unger E, Moldofsky P, Gatenby R. Diagnosis of
osteomyelitis by MR imaging. Am J Roentgenol 1988 ;
150 : 605-610.
Unkila-Kallio L, Kallio MJT, Eskola J, Pettola H.
Serum C-reactive protein, erythrocyte sedimentation rate
and white blood cell count in acute hematogenous
osteomyelitis of children. Pediatrics 1994 ; 4 : 170-174.
Wright NB, Abbott GT, Carty HML. Ultrasonography
in children with osteomyelitis. Clin Radiol 1995 ; 50 : 623627.
Potrebbero piacerti anche
- Ewing Sarcoma, Anatomie NR 1Documento5 pagineEwing Sarcoma, Anatomie NR 1Ioana PelinNessuna valutazione finora
- Nice 1stDocumento6 pagineNice 1staldiNessuna valutazione finora
- So Sang Sieu Am Va MriDocumento12 pagineSo Sang Sieu Am Va Mrithu hangNessuna valutazione finora
- Mandibular Traumatic Peripheral Osteoma: A Case ReportDocumento5 pagineMandibular Traumatic Peripheral Osteoma: A Case ReportrajtanniruNessuna valutazione finora
- Orthopedic Diagnostic Imaging in Exotic PetsDocumento25 pagineOrthopedic Diagnostic Imaging in Exotic PetsHidaNessuna valutazione finora
- Celulitis PeriorbitariaDocumento4 pagineCelulitis PeriorbitariaJose Carlos Guerra RangelNessuna valutazione finora
- Endoscopic Resection of Symptomatic Osteochondroma of The Distal FemurDocumento4 pagineEndoscopic Resection of Symptomatic Osteochondroma of The Distal FemurAlex CirlanNessuna valutazione finora
- 026 Prof-2033Documento4 pagine026 Prof-2033dgina8800Nessuna valutazione finora
- Glomus TumourDocumento5 pagineGlomus TumourDiamond DustNessuna valutazione finora
- The Relevance of Clinical and Radiographic Features of Jaw Lesions: A Prospective StudyDocumento9 pagineThe Relevance of Clinical and Radiographic Features of Jaw Lesions: A Prospective StudydaruNessuna valutazione finora
- Jurnal r4Documento9 pagineJurnal r4Rezkina Azizah PutriNessuna valutazione finora
- Transforaminal Lumbar Interbody Fusion (TLIF) : Assessment of Clinical and Radiological OutcomeDocumento6 pagineTransforaminal Lumbar Interbody Fusion (TLIF) : Assessment of Clinical and Radiological OutcomeJosh JoshiNessuna valutazione finora
- Updatesinpediatric Cholesteatoma: Minimizing Intervention While Maximizing OutcomesDocumento11 pagineUpdatesinpediatric Cholesteatoma: Minimizing Intervention While Maximizing OutcomesenviNessuna valutazione finora
- Articol ORLDocumento6 pagineArticol ORLSabina BădilăNessuna valutazione finora
- Uso de Ultrasonografia para Medial EpycondilitisDocumento5 pagineUso de Ultrasonografia para Medial EpycondilitisSantiago BianchiNessuna valutazione finora
- Bone TumorsDocumento8 pagineBone TumorsHikari AoiNessuna valutazione finora
- Sonoanatomy Scanning Technique and Basic Pathology of The Wrist and HandDocumento6 pagineSonoanatomy Scanning Technique and Basic Pathology of The Wrist and Handpippen333Nessuna valutazione finora
- Medi 94 E369Documento9 pagineMedi 94 E369solikin ikinNessuna valutazione finora
- Diagnostic Imaging of Gout: Comparison of High-Resolution US Versus Conventional X-RayDocumento10 pagineDiagnostic Imaging of Gout: Comparison of High-Resolution US Versus Conventional X-RayHaryo Chandra KusumosariNessuna valutazione finora
- DownloadDocumento3 pagineDownloadnoname19191Nessuna valutazione finora
- 17 Rajpal EtalDocumento4 pagine17 Rajpal EtaleditorijmrhsNessuna valutazione finora
- Hiperplasia Condilar3Documento5 pagineHiperplasia Condilar3Alejandra Oliveros VargasNessuna valutazione finora
- Transforaminal Debridement With A Posterior Only.62Documento6 pagineTransforaminal Debridement With A Posterior Only.62Jean Marcel Castelo VegaNessuna valutazione finora
- MainDocumento9 pagineMainimagen.hgsNessuna valutazione finora
- Palest Ro 2006Documento22 paginePalest Ro 2006Djancok bangetNessuna valutazione finora
- Gajewski DA 2006 PDFDocumento5 pagineGajewski DA 2006 PDFOliver BlandyNessuna valutazione finora
- Ultrasonographic Evaluation of Plantar Fasciitis After Low-Level Laser Therapy: Results of A Double-Blind, Randomized, Placebo-Controlled TrialDocumento7 pagineUltrasonographic Evaluation of Plantar Fasciitis After Low-Level Laser Therapy: Results of A Double-Blind, Randomized, Placebo-Controlled TrialSri HariNessuna valutazione finora
- 1 s2.0 S0720048X16300286Documento6 pagine1 s2.0 S0720048X16300286Yuda ArifkaNessuna valutazione finora
- Medi 97 E11210Documento6 pagineMedi 97 E11210فرجني موغNessuna valutazione finora
- Tatalaksana OsteonekrosisDocumento78 pagineTatalaksana OsteonekrosisRama MahendraNessuna valutazione finora
- Surgical Management of Cervical Ossified Posterior Longitudinal LigamentDocumento13 pagineSurgical Management of Cervical Ossified Posterior Longitudinal Ligamentinfobusiness2010Nessuna valutazione finora
- Osteoradionecrosis of The Jaws: de Finition, Epidemiology, Staging and Clinical and Radiological Findings. A Concise ReviewDocumento9 pagineOsteoradionecrosis of The Jaws: de Finition, Epidemiology, Staging and Clinical and Radiological Findings. A Concise ReviewCecilia AhuetNessuna valutazione finora
- Assessment of Pelvic Floor Dysfunctions Using Dynamic Magnetic Resonance ImagingDocumento11 pagineAssessment of Pelvic Floor Dysfunctions Using Dynamic Magnetic Resonance ImagingsalahzotoNessuna valutazione finora
- Sipola. Detection and Quantification of Rotator Cuff Tears With Ultrasonography and Magnetic Resonance Imaging - A ProsDocumento9 pagineSipola. Detection and Quantification of Rotator Cuff Tears With Ultrasonography and Magnetic Resonance Imaging - A Prossteven saputraNessuna valutazione finora
- Tu of The OrbitDocumento12 pagineTu of The OrbitChavdarNessuna valutazione finora
- Use of Allograft in Skeletally Immature Patients For Calcaneal Neck Lengthening OsteotomyDocumento5 pagineUse of Allograft in Skeletally Immature Patients For Calcaneal Neck Lengthening OsteotomyMonem ShakeerNessuna valutazione finora
- Eosinophilic Granuloma of The Occipital Bone in An Adult: A Case ReportDocumento4 pagineEosinophilic Granuloma of The Occipital Bone in An Adult: A Case ReportHalbar August KandaNessuna valutazione finora
- Srinivasan 2011Documento5 pagineSrinivasan 2011miaubooksNessuna valutazione finora
- 2011-Sonographic Appearances of Morton's Neuroma - UMBDocumento6 pagine2011-Sonographic Appearances of Morton's Neuroma - UMBAsim AliNessuna valutazione finora
- Osteosarcoma of The Jaw An Analysis of A Series of 74 Cases (2013)Documento8 pagineOsteosarcoma of The Jaw An Analysis of A Series of 74 Cases (2013)sTEVENNessuna valutazione finora
- Burud 2020Documento8 pagineBurud 2020Wirda Elya SariNessuna valutazione finora
- Clavicle Fracture Following Neck Dissection: Imaging Features and Natural CourseDocumento6 pagineClavicle Fracture Following Neck Dissection: Imaging Features and Natural CourseAngel IschiaNessuna valutazione finora
- TMJ Imaging in JIA Patients - An OverviewDocumento9 pagineTMJ Imaging in JIA Patients - An OverviewYuda ArifkaNessuna valutazione finora
- Art:10.1186/1824 7288 40 S1 A27Documento1 paginaArt:10.1186/1824 7288 40 S1 A27Itsirch AydinNessuna valutazione finora
- Cefelometria y ATMDocumento7 pagineCefelometria y ATMSharon Tolentino VidalNessuna valutazione finora
- Risk of Perforation Using Rigid Oesophagoscopy in The Distal Part of OesophagusDocumento4 pagineRisk of Perforation Using Rigid Oesophagoscopy in The Distal Part of OesophagusAgus KarsetiyonoNessuna valutazione finora
- Raccourcissement Cubitus - Acta Ortho BelgicaDocumento6 pagineRaccourcissement Cubitus - Acta Ortho BelgicaLedouxNessuna valutazione finora
- Diagnostic Value of Combined Static-Excretory MR Urography in Children With HydronephrosisDocumento9 pagineDiagnostic Value of Combined Static-Excretory MR Urography in Children With HydronephrosisnyimasNessuna valutazione finora
- Acute Concomitant Esotropia of Adulthood: Abraham Spierer, MDDocumento4 pagineAcute Concomitant Esotropia of Adulthood: Abraham Spierer, MDFarah Basotjatjo KaharNessuna valutazione finora
- Current Diagnostic Techniques in Veterinary Surgery PDFDocumento2 pagineCurrent Diagnostic Techniques in Veterinary Surgery PDFKirti JamwalNessuna valutazione finora
- Ringe 2013Documento3 pagineRinge 2013Minh ChíNessuna valutazione finora
- Role of Ultrasonography in Knee Osteoarthritis: EviewDocumento6 pagineRole of Ultrasonography in Knee Osteoarthritis: EviewSandroLao0% (1)
- JCM 11 01202Documento9 pagineJCM 11 01202anca_adam_26Nessuna valutazione finora
- Diagnostic Medical Sonography: Name: Krystyle Course Name: DateDocumento13 pagineDiagnostic Medical Sonography: Name: Krystyle Course Name: DateshahzaibNessuna valutazione finora
- Accepted Manuscript: Injury, Int. J. Care InjuredDocumento16 pagineAccepted Manuscript: Injury, Int. J. Care InjuredDwi AryanataNessuna valutazione finora
- JMID-00662 OsteomeilitissteoDocumento4 pagineJMID-00662 OsteomeilitissteoJackill ArmstrongNessuna valutazione finora
- Complications of Temporomandibular Joint Arthroscopy: A Retrospective Analytic Study of 670 Arthroscopic ProceduresDocumento5 pagineComplications of Temporomandibular Joint Arthroscopy: A Retrospective Analytic Study of 670 Arthroscopic ProceduresAbhishek SinghNessuna valutazione finora
- Cytology of Bone MarrowDocumento62 pagineCytology of Bone MarrowFabrício CamargoNessuna valutazione finora
- Ganesh 2011Documento5 pagineGanesh 2011Giang Nguyễn NgânNessuna valutazione finora
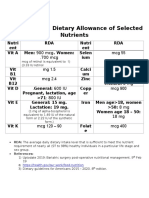
- Recommended Dietary Allowance of Selected NutrientsDocumento3 pagineRecommended Dietary Allowance of Selected Nutrientsأبو عبيدةNessuna valutazione finora
- Copyright 8Documento1 paginaCopyright 8أبو عبيدةNessuna valutazione finora
- Detailed Answers of Q91-100 Jun15Documento6 pagineDetailed Answers of Q91-100 Jun15أبو عبيدةNessuna valutazione finora
- CompleteBloodCounts NORMAL VALUEDocumento4 pagineCompleteBloodCounts NORMAL VALUEWoro Hapsari Wahyuningrum100% (1)
- MeningiomaDocumento5 pagineMeningiomaأبو عبيدةNessuna valutazione finora
- Copyright 8Documento1 paginaCopyright 8أبو عبيدةNessuna valutazione finora
- 1000 Most Common Words (SAT)Documento70 pagine1000 Most Common Words (SAT)grellian95% (20)
- This Certificate Given ToDocumento1 paginaThis Certificate Given Toأبو عبيدةNessuna valutazione finora
- Copyright 8Documento1 paginaCopyright 8أبو عبيدةNessuna valutazione finora
- Copyright 8Documento1 paginaCopyright 8أبو عبيدةNessuna valutazione finora
- Copyright 8Documento1 paginaCopyright 8أبو عبيدةNessuna valutazione finora
- Copyright 8Documento1 paginaCopyright 8أبو عبيدةNessuna valutazione finora
- Copyright 8Documento1 paginaCopyright 8أبو عبيدةNessuna valutazione finora
- Copyright 8Documento1 paginaCopyright 8أبو عبيدةNessuna valutazione finora
- Copyright 8Documento1 paginaCopyright 8أبو عبيدةNessuna valutazione finora
- Copyright 8Documento1 paginaCopyright 8أبو عبيدةNessuna valutazione finora
- Copyright 8Documento1 paginaCopyright 8أبو عبيدةNessuna valutazione finora
- Copyright 8Documento1 paginaCopyright 8أبو عبيدةNessuna valutazione finora
- Copyright 8Documento1 paginaCopyright 8أبو عبيدةNessuna valutazione finora
- Copyright 8Documento1 paginaCopyright 8أبو عبيدةNessuna valutazione finora
- Copyright 8Documento1 paginaCopyright 8أبو عبيدةNessuna valutazione finora
- Copyright 8Documento1 paginaCopyright 8أبو عبيدةNessuna valutazione finora
- Copyright 8Documento1 paginaCopyright 8أبو عبيدةNessuna valutazione finora
- Copyright 8Documento1 paginaCopyright 8أبو عبيدةNessuna valutazione finora
- Copyright 8Documento1 paginaCopyright 8أبو عبيدةNessuna valutazione finora
- Copyright 8Documento1 paginaCopyright 8أبو عبيدةNessuna valutazione finora
- Copyright 8Documento1 paginaCopyright 8أبو عبيدةNessuna valutazione finora
- Copyright 8Documento1 paginaCopyright 8أبو عبيدةNessuna valutazione finora
- Copyright 8Documento1 paginaCopyright 8أبو عبيدةNessuna valutazione finora
- Copyright 8Documento1 paginaCopyright 8أبو عبيدةNessuna valutazione finora
- The Obesity Code: Unlocking the Secrets of Weight LossDa EverandThe Obesity Code: Unlocking the Secrets of Weight LossValutazione: 4 su 5 stelle4/5 (6)
- The Age of Magical Overthinking: Notes on Modern IrrationalityDa EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityValutazione: 4 su 5 stelle4/5 (28)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsDa EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNessuna valutazione finora
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeDa EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeValutazione: 2 su 5 stelle2/5 (1)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDDa EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDValutazione: 5 su 5 stelle5/5 (1)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionDa EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionValutazione: 4 su 5 stelle4/5 (404)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsDa EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsValutazione: 5 su 5 stelle5/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisDa EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisValutazione: 4.5 su 5 stelle4.5/5 (42)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedDa EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedValutazione: 5 su 5 stelle5/5 (81)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsDa EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsValutazione: 3.5 su 5 stelle3.5/5 (3)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisDa EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisValutazione: 4 su 5 stelle4/5 (1)
- Why We Die: The New Science of Aging and the Quest for ImmortalityDa EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityValutazione: 4 su 5 stelle4/5 (3)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaDa EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningDa EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningValutazione: 4 su 5 stelle4/5 (3)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Da EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Nessuna valutazione finora
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisDa EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisValutazione: 3.5 su 5 stelle3.5/5 (2)
- Gut: the new and revised Sunday Times bestsellerDa EverandGut: the new and revised Sunday Times bestsellerValutazione: 4 su 5 stelle4/5 (392)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryDa EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryValutazione: 4 su 5 stelle4/5 (44)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Da EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Valutazione: 4.5 su 5 stelle4.5/5 (110)
- The Marshmallow Test: Mastering Self-ControlDa EverandThe Marshmallow Test: Mastering Self-ControlValutazione: 4.5 su 5 stelle4.5/5 (58)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessDa EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessValutazione: 4.5 su 5 stelle4.5/5 (328)
- Dark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingDa EverandDark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingValutazione: 4 su 5 stelle4/5 (1138)
- Troubled: A Memoir of Foster Care, Family, and Social ClassDa EverandTroubled: A Memoir of Foster Care, Family, and Social ClassValutazione: 4.5 su 5 stelle4.5/5 (26)