Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Evaluation of Alkaline Phosphatase (ALP) and Heat Stable-ALP (HS-ALP) in Chronic Obstructive Pulmonary Disease (COPD) PDF
Caricato da
M Fiqih HilmanDescrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Evaluation of Alkaline Phosphatase (ALP) and Heat Stable-ALP (HS-ALP) in Chronic Obstructive Pulmonary Disease (COPD) PDF
Caricato da
M Fiqih HilmanCopyright:
Formati disponibili
1803
International Journal of Collaborative Research on Internal Medicine & Public Health
Evaluation of Alkaline phosphatase (ALP) and Heat StableALP (HS-ALP) in Chronic Obstructive Pulmonary Disease
(COPD)
Anup N. Nillawar 1*, Jayashree S. Bardapurkar 2, Suhas J. Bardapurkar 3
1
Dr.; Assistant Professor (Biochemistry), Government Medical College, Aurangabad, India-431001
2
Dr.; Professor (Biochemistry); Sarasvati Institute Of Medical Sciences, Haapur, UP, India
3
Dr.; Shree Nursing Home, Aurnagabad, MS, India
* Corresponding Author: Dr. Anup N. Nillawar
B-5, Tridal Apartment, Naralibag, Aurangabad, India, 431001
Email: nilawaranup@rediffmail.com
Abstract
Background: COPD (Chronic Obstructive Pulmonary Disease) is defined as a disease state
characterized by airflow limitation that is not fully reversible. The airflow limitation is usually
both progressive and associated with an abnormal inflammatory response of the lungs to noxious
particles and gases. Tobacco smoke remains the main etiological agent. COPD inflammation
initiated by tobacco smoke remains exuberant long after smoking cessation. Functional
impairment of lung organ is reflected by impairment in FEV1% predicted. This is the result of
underlying remodeling and fibrosis in small airways. Type 2 alveolar cells are involved in this
process of remodeling and repair. Many of the studies have showed that heat stable alkaline
phosphatase (HS-ALP) is released from these type 2 alveolar cells.
Objectives: To correlate serum activity of ALP, HS-ALP, FEV1% predicted and BMI in various
stages of COPD patients.
Method: This study tried to evaluate correlation between serum activity of ALP, HS-ALP and
FEV1% predicted and BMI in various stages of COPD. Total 45 patients of stage 2, 3, 4 of
COPD were studied.
Result: We found there is unanimous increase in total ALP activity in all the stages of COPD.
HS- ALP is increased in all the stages of COPD with no difference in between the stages. There
is no relation between ALP and HS-ALP and between FEV1% predicted and BMI. We find that
HS-ALP once considered as carcino-embryonic antigen is increased in lung inflammation of
COPD.
Conclusion: Serum ALP and HS-ALP which can be very easily measured could be the one of
the laboratory marker for diagnostic and prognostication of COPD patients.
Keywords: COPD, ALP, Heat stable-ALP
Running Title: ALP and HS-ALP in COPD
Vol. 4 No. 10 (2012)
1804
International Journal of Collaborative Research on Internal Medicine & Public Health
Introduction
COPD (Chronic Obstructive Pulmonary Disease) is an increasing health problem worldwide.
Global prevalence is estimated to be 8.34/1000. Similarly, COPD is an increasing health problem
even in India where prevalence is found to be 4.1%.1,2 COPD is defined as a disease state
characterized by airflow limitation that is not fully reversible. The airflow limitation is usually
both progressive and associated with an abnormal inflammatory response of the lungs to noxious
particles and gases".3 Tobacco smoke remains the most typical etiological factor for COPD.
Inflammation initiated by the external noxious stimuli remains even after cessation of the
stimulus, this persistence of inflammation leads to progression and fibrosis which is reflected as
functional respiratory impairment. This is measured in terms of reduced FEV1 % predicted.4 The
present system of staging does not include any of the laboratory inflammatory indicators. There
is now renowned interest in finding some cellular and biochemical markers to monitor the
inflammation in various respiratory disorders including COPD.5,6,7 Alkaline phosphatase (ALP)
is one such enzyme which is evaluated in differentiation of various kinds of pleural effusion and
is a component of Lights criterion,.8,9 ALP is nonspecific and ubiquitous enzyme found in the
serum. It is membrane bound extracellular enzyme and has 5 isoforms, which are; Bone; Liver;
kidney; intestinal and placental. Bone, kidney and liver isoforms are encoded by one distinct
genetic locus which differs in their carbohydrate content; all of these isoforms are heat labile.
Other two, intestinal and placental isoforms are encoded by another distinct genetic locus and
these isoforms are heat stable in nature. Normally, Placental and placental like isoforms are not
present in the serum of adult males and adult non-pregnant females.10 Elevation in the heat stable
ALP is seen in the sera of patients with certain malignant diseases. These carcinoplacental
isoenzymes (e.g. Regan isoenzyme) appear to result from the derepression of the placental ALP
gene. The presence of these isoenzymes can be readily detected in serum by their heat stability.10
Alkaline phosphatase fractions derived from lung tissue essentially belongs to placental and
placental like isoforms. In the lungs, ALP is extracellular enzyme bound to type 2 alveolar cells11
the cells which are involved in remodeling process of the lung tissue. Secretory activity of type2
alveolar cells is shown by ALP which is heat stable placental or placental like isoform. Thus,
ALP-HS specifically being the product of type 2 alveolar cells may indicate the activity of
remodeling and fibrosis in the lung tissue.6 Also, COPD is a chronic systemic inflammatory
disease,7,12,13 which results in decreased Body mass index (BMI). So the aim of this study was to
evaluate serum levels of ALP and HS-ALP in various stages of COPD and to correlate the values
with FEV 1 % predicted and BMI (as an indicator of systemic involvement) and to know the
potential of this parameter to encompass the inflammatory face of COPD.
Material and Methods
Total 45 patients of stable COPD were studied attending the internal or chest medicine outpatient
department of (Govt. medical College), Aurangabad. PFTs, oxygen saturation were measured
and patients were classified according to the GOLD criterion into stage 2, 3, 4.2 Patients were
stable without any active exacerbation at the time of study, and patients with any other major
disease were excluded based on history and clinical examination. Guidelines laid by the
Vol. 4 No. 10 (2012)
1805
International Journal of Collaborative Research on Internal Medicine & Public Health
institutes ethical committee were followed. Total 40 age and sex matched controls were
selected; attending Medicine OPD without having COPD or any other respiratory systems
diagnosis were included in the study. ALP and HS-ALP were estimated on semi auto chemistry
analyzer. ALP was estimated by the kinetic assay kit manufactured by Reckon diagnostics which
utilizes stabilized p-NPP. This method is based on the recommendations by German society of
clinical chemistry.14 For estimation of the heat stable component of ALP, serum was incubated at
560 C for half an hour followed by measurement of ALP activity in the serum.
Observation and results
Almost all the patients showed ALP more than the upper normal value (which was 56-140 IU/L
based on manufacturers recommendation). Normal range of Hs ALP is up to 7-21 IU/L.(10) In
our study, 17 patients out of 45 (33 %) showed increase in the HS-ALP, maximum up to
114IU/L. When compared with the control group, activity of total ALP and HS-ALP is
significantly higher in COPD group. (Table 2) Table 1 depicts results obtained after categorizing
patients according to GOLD stages. Total ALP increased in the later stages of COPD (stage 3
and stage 4) when compared with stage 2 (p<0.05). But HS-ALP doesnt differ in between the
COPD GOLD stages.
ALP has negative but insignificant relation with FEV1% predicted. (r=-0.08). There is no
consistent relation with BMI. When the results are viewed in the context of smoking status,
Values of ALP and HS-ALP are more in the smoker group but this is not a statistically
significant finding. HS-ALP values maximum up to 114 IU/L are found in some of the smoker
COPD patients.
Discussion
Type II alveolar cells are important in the repair of alveolar epithelium after any kind of cellular
insult and injury and response to it.15,16 Broncho alveolar lavage fluid (BALF) is the fluid that is
near to the lung tissue and recovered after bronchial washing. Various biomarkers are assayed in
the BALF to assess the pathologic process of lung parenchyma. Normally, type II cells are not
present in BALF. The ALP activity, a marker of type II cell damage and/or proliferation was
reported to be increased in BALF after exposure to pneumotoxicants and associated with
progression of fibrosis.
In smokers, ALP activity is found to be increased in BALF.17 In our study, we found raised value
of serum total ALP and HS-ALP activity. In the light of exclusion of other sources of ALP, it can
be said that raised serum total ALP and HS-ALP activity could be the result of proliferation of
type 2 alveolar cells involved in remodeling process of small airways in COPD. Capelli et al
hypothesized that ALP could be a marker of evolving fibrosis process of diffuse interstitial lung
disease (DILD).16 In our study, activity is seen more in Ex-smokers group than never smoker
COPD group may suggest that disease process is more pronounced in smokers. Interestingly,
individuals in the Ex-smoker group had quit the smoking at least 5 years back which suggests
Vol. 4 No. 10 (2012)
1806
International Journal of Collaborative Research on Internal Medicine & Public Health
that the exaggerated remodeling process which may be initiated by smoke far back is still
continuing. The ALP activity does not show any correlation with BMI (Indicator of systemic
involvement). Going further, these findings need to be ascertained in the COPD patients having
rapid lung volume loss. This may help to establish ALP and HS-ALP as a marker of fibrosing
disease process of COPD which may be helpful for early detection of rapid lung volume losers in
diagnosed COPD patients and also in smokers.
Conflict of Interest: None declared.
References:
1.
Jindal SK, Aggarwal a N, Chaudhry K, Chhabra SK, DSouza G a, Gupta D, et al. A
multicentric study on epidemiology of chronic obstructive pulmonary disease and its
relationship with tobacco smoking and environmental tobacco smoke exposure. The
Indian journal of chest diseases & allied sciences [Internet]. 2005;48(1):239. Available
from: http://www.ncbi.nlm.nih.gov/pubmed/16482948
2.
Global strategy for the Diagnosis, Management, and Prevention of COPD [Internet]. 2010;
Available from: http://www.goldcopd.org/
3.
Rogerio Rufino JR, Lapa Silva. cellualr and biochemical bases of Chronic obstructive
pulmonary Disease. J Bras Pneumol. 2006;32(3):2418.
4.
Reilly JJ, Silverman EK, Shapiro SD. Chronic obstructive pulmonay disease. In: Kasper
Dl, Braunwald E, Fauci AS, Hauser SL, Longo Dl, Jameson JL, editors. Harrisons
Principles of internal medicine. 16th Ed.New York City, McGraw-Hill; 2005. 1548-52.
5.
MacNee W, Rennard SI, Hunt JF, Edwards LD, Miller BE, Locantore NW, et al.
Evaluation of exhaled breath condensate pH as a biomarker for COPD. Respiratory
medicine [Internet]. 2011 Jul 1 [cited 2012 Apr 29];105(7):103745. Available from:
http://www.resmedjournal.com/article/S0954-6111(11)00058-8/abstract
6.
Cobben NA, Drent M, Schols AM, Lamers RJ, Wouters EF, Van Dieijen-Visser MP.
Serum lactate dehydrogenase pattern in ex-coalminers and its isoenzyme. Respir Med.
1997: 61623.
7.
Nillawar A, Bardapurkar S, Bardapurkar J. High sensitive C-reactive protein as a systemic
inflammatory marker and LDH-3 isoenzyme in chronic obstructive pulmonary disease.
Lung India [Internet]. 2012 [cited 2012 Jan 30];29(1):24. Available from:
http://www.lungindia.com/text.asp?2012/29/1/24/92358.
Vol. 4 No. 10 (2012)
1807
International Journal of Collaborative Research on Internal Medicine & Public Health
8.
Light RW. Clinical practice Pleural effusion. N
2002;346(25):1971-7.
Available
http://www.nejm.org/doi/full/10.1056/NEJMcp010731
Engl
Med
[Internet].
from:
9.
Jadhav AA, Bardapurkar JS, Jain A. Alkaline phosphatase: Distinguishing between
tuberculous and nontuberculous pleural effusion. Lung India: official organ of Indian
Chest Society [Internet]. 2009 Jul [cited 2012 Apr 29];26(3):7780. Available from:
http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2862511&tool=pmcentrez&re
ndertype=abstract
10.
Mauro P, Bais R, Wouter W. van Solinge In:Burtis CA, Ashwood ER, Bruns De. Editors.
Tietz textbook of clinical chemistry and molecular diagnostics.4thed. St.Louis, MO:
Elsevier Saunders. 2004.
11.
Edelson JD, Shannon JM, Mason RJ. Alkaline phosphatase: a marker of alveolar type II
cell differentiation. The American review of respiratory disease [Internet]. 1988 Nov
[cited
2012
May
1];138(5):126875.
Available
from:
http://www.ncbi.nlm.nih.gov/pubmed/2462386
12.
Man SFP, Connett JE, Anthonisen NR, Wise RA, Tashkin DP, Sin DD. C-reactive protein
and mortality in mild to moderate chronic obstructive pulmonary disease. Thorax
[Internet]. 2006 Oct [cited 2012 May 1];61(10):84953. Available from:
http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2104755&tool=pmcentrez&re
ndertype=abstract
13.
van Eeden SF, Yeung A, Quinlam K, Hogg JC. Systemic response to ambient particulate
matter: relevance to chronic obstructive pulmonary disease. Proceedings of the American
Thoracic Society [Internet]. 2005 Jan [cited 2012 Apr 29];2(1):617. Available from:
http://www.ncbi.nlm.nih.gov/pubmed/16113470
14.
Recommendations of the German Society for Clinical Chemistry: Standardization of
Methods for the estimation of Enzyme Activity in Biological Fluids. J. Clinical
Chemistry, Clinical Biochemistry. 1972;8:18292.
15.
Henderson RF, Scott GG, Waide JJ. Source of alkaline phosphatase activity in epithelial
lining fluid of normal and injured F344 rat lungs. Toxicology and applied pharmacology
[Internet]. 1995 Sep [cited 2012 May 1];134(1):1704. Available from:
http://www.ncbi.nlm.nih.gov/pubmed/7676452
16.
Capelli A, Lusuardi M, Cerutti CG, Donner CF. Lung alkaline phosphatase as a marker of
fibrosis in chronic interstitial disorders. American journal of respiratory and critical care
medicine [Internet]. 1997 Jan [cited 2012 Apr 29];155(1):24953. Available from:
http://www.ncbi.nlm.nih.gov/pubmed/9001320
17.
McLaughlin PJ, Twist AM, Evans CC, Johnson PM. Serum placental type alkaline
phosphatase in cigarette smokers. Journal of clinical pathology [Internet]. 1984 Jul [cited
Vol. 4 No. 10 (2012)
1808
International Journal of Collaborative Research on Internal Medicine & Public Health
2012
May
1];37(7):8268.
Available
from:
http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=498819&tool=pmcentrez&ren
dertype=abstract
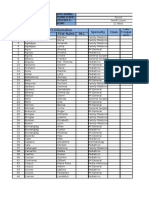
Table 1: Serum total ALP, heat stable ALP in control and COPD patients; GOLD stage wise
40
Complete
Cohort of
COPD
45
54-130
88.752.51
215.79.033*
186.6 17.09
0-20
0.480.78
21.874.3*
22.50 8.051
Reference
value
No
Total ALP
(IU/L)
ALP HS
Control
Stage 2
COPD
Stage 3
COPD
12
17
224.2
15.12
21.12
6.578
Stage 4 COPD
15
225.1 14.43
23.60 9.034
*p=0.00
Table 2: Patients grouped and analyzed according to their BMI
Total ALP
ALP hs
BMI< 19
205.0 13.40 N=22
18.23 4.925 N=22
P=NS
BMI>19
226.0 12.06 N=23
25.35 7.193 N=23
Table 3: ALP and HS-ALP according to smoking status
Parameter
ALP total
ALP-HS
FEV1% predicted
BMI
Smokers
220.6363
44.6226.25
44.6215.51
19.014.15
Non smokers
202.2553.56
22.2538.01
39.5415.73
20.524.82
P value
0.37
0.95
0.33
0.30
Vol. 4 No. 10 (2012)
Potrebbero piacerti anche
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- CAMERON Current Surgical Therapy, Thirteenth EditionDocumento1.667 pagineCAMERON Current Surgical Therapy, Thirteenth Editionniberev100% (2)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Upper Back ExercisesDocumento2 pagineUpper Back ExercisesMarco NgNessuna valutazione finora
- Chapter 1 Nov. 24 RevisionDocumento12 pagineChapter 1 Nov. 24 RevisionOdessa Fortu LandichoNessuna valutazione finora
- NCLEX Questions OB QuestionsDocumento4 pagineNCLEX Questions OB QuestionsAlvin L. Rozier100% (1)
- Cpms College of Nursing Assignment ON Bilimeter: Subject: Child Health Nursing DATED:23 JUNE 2021Documento5 pagineCpms College of Nursing Assignment ON Bilimeter: Subject: Child Health Nursing DATED:23 JUNE 2021Amy Lalringhluani Chhakchhuak100% (3)
- Fanem 1186 Infant Incubator - User ManualDocumento78 pagineFanem 1186 Infant Incubator - User ManualrobinsongiraldoNessuna valutazione finora
- Master ListDocumento100 pagineMaster ListAris GonzalesNessuna valutazione finora
- Basic Pathology of The SkinDocumento59 pagineBasic Pathology of The SkinrowenanuquiNessuna valutazione finora
- Cardiovascular MedicineDocumento50 pagineCardiovascular MedicineCarlos HernándezNessuna valutazione finora
- Fma Ue EnglishDocumento3 pagineFma Ue EnglishAnaa ElleyNessuna valutazione finora
- Chapter 14 Intravenous Solutions, Equipment, and CalculationsDocumento48 pagineChapter 14 Intravenous Solutions, Equipment, and CalculationsEn RasNessuna valutazione finora
- Matrices / Orthodontic Courses by Indian Dental AcademyDocumento26 pagineMatrices / Orthodontic Courses by Indian Dental Academyindian dental academyNessuna valutazione finora
- Chapter 5: Electrolyte and Acid - Base Disorders in MalignancyDocumento7 pagineChapter 5: Electrolyte and Acid - Base Disorders in MalignancyPratita Jati PermatasariNessuna valutazione finora
- Journal Reading Survey OphtalmologyDocumento17 pagineJournal Reading Survey OphtalmologynadyajondriNessuna valutazione finora
- Leah Trellas ResumeDocumento1 paginaLeah Trellas Resumeapi-334646003Nessuna valutazione finora
- Lumbar Punction PDFDocumento4 pagineLumbar Punction PDFmrocrodNessuna valutazione finora
- Defense of Learning Capstone Blood DriveDocumento20 pagineDefense of Learning Capstone Blood Driveapi-194147189Nessuna valutazione finora
- Case 1 Hemiplegia With AphasiaDocumento8 pagineCase 1 Hemiplegia With Aphasialycan007Nessuna valutazione finora
- Important Pediatrics SyndromesDocumento11 pagineImportant Pediatrics SyndromesYogeshRavalNessuna valutazione finora
- Nci Presentation Full VersionDocumento95 pagineNci Presentation Full Versionapi-321890204Nessuna valutazione finora
- Congenital Diaphragmatic Hernia - Wikipedia, The Free Encyclopedia PDFDocumento4 pagineCongenital Diaphragmatic Hernia - Wikipedia, The Free Encyclopedia PDFMilda Inayah100% (1)
- CQC John Radcliffe ReportDocumento99 pagineCQC John Radcliffe ReportOxfordMailEditorialNessuna valutazione finora
- 2008 Annual Report-From ILAEDocumento113 pagine2008 Annual Report-From ILAEarmythunder100% (2)
- Innocent Blood: A History of Hemorrhagic Disease of The NewbornDocumento7 pagineInnocent Blood: A History of Hemorrhagic Disease of The NewbornNasriNessuna valutazione finora
- WHO RHR 14.18 EngDocumento2 pagineWHO RHR 14.18 EngSasi KumarNessuna valutazione finora
- Cell PathologyDocumento10 pagineCell Pathologyapi-300736398Nessuna valutazione finora
- Antiphospholipid Syndrome Challenges in The Laboratory Diagnosis and TreatmentDocumento61 pagineAntiphospholipid Syndrome Challenges in The Laboratory Diagnosis and Treatmentbadshah007777Nessuna valutazione finora
- Orthopaedic NeurologyDocumento10 pagineOrthopaedic NeurologyaiakobyNessuna valutazione finora
- 8977 HiDocumento6 pagine8977 Hiwanwan_adongNessuna valutazione finora
- Cross-Sectional Tomography: Oral and Maxillofacial RadiologyDocumento7 pagineCross-Sectional Tomography: Oral and Maxillofacial RadiologyPhanQuangHuyNessuna valutazione finora