Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Syllabus Outline Beginning Family 2 Revised 2011-12 #2
Caricato da
Jerilee SoCute WattsCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Syllabus Outline Beginning Family 2 Revised 2011-12 #2
Caricato da
Jerilee SoCute WattsCopyright:
Formati disponibili
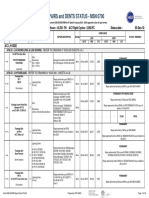
CCC/2012/05/22A
UNIVERSITY OF TECHNOLOGY, JAMAICA
SYLLABUS OUTLINE
COLLEGE:
College of Health Sciences
SCHOOL:
Caribbean School of Nursing
COURSE OF STUDY:
General Nursing BSN Level 1
MODULE TITLE:
The Beginning Family: Part I1
MODULE CODE:
NUR 4001
DURATION:
45 hours theory; 45 hours practical
CREDIT VALUE:
PRE REQUISITE:
The Beginning Family Part 1 [NUR3006]
1.0
MODULE DESCRIPTION
This module consists of two parts. Part 1 deals with the pregnant woman, the foetus and
her family during pregnancy, labour and the puerperium and the neonate from birth to 28
days.
Part 11 deals with the child from birth to 18 years. This module aims to prepare nurses to
promote the health and wellbeing of children and adolescents in a variety of health care
settings. Growth and development of the child from 0-18 years, the normal child as well as
the sick and hospitalized child with a variety of health problems and their families are
emphasized.
The nursing process using a needs framework and a team approach is the basis for
promoting and maintaining health. Strategies for assisting the parents/family, the neonate
and the child at any stage in the health-illness continuum to maintain needs satisfaction are
included. Family and community resources are identified as supportive services.
This section is divided into the following four units:
Unit 1:
Unit 2:
Unit 3:
Unit 4:
2.0
Review of Principles of Growth and Development in the Child 0-18 years
Health Promotion and Maintenance of Health in the Child 0-18 years
Concepts of Illness Relating to the Child 0-18 years
Nursing Care of the Child 0-18 Years with Interference to Basic Needs
MODULE OBJECTIVES/ LEARNING OUTCOMES
General Objectives:
Upon completion of the module, the student will be able to:
1.
Review growth and developmental principles in the assessment of the normal child;
2.
Utilize the nursing process in the promotion and maintenance of health of the child;
3.
Utilize health promotion strategies in assisting the child and family to develop and maintain
healthy lifestyle;
4.
Understand the concept of illness as it relates to assisting and supporting the child and
family through hospitalization and recovery;
5.
Utilize knowledge of physiological and psychosocial forces affecting health to assist the
child to achieve and maintain basic needs satisfaction;
6.
Provide nursing care to the child with interferences of basic needs;
7.
Provide preventive and supportive nursing interventions for children and their families at
risk for and experiencing illness;
1
CCC/2012/05/22A
8.
Understand the role of play in the development of the child;
9.
Utilize effectively community resources in the delivery of child care;
10.
Appreciate the importance of the team approach in childcare.
3.0
MODULE CONTENT AND CONTEXT
UNIT 1: PRINCIPLES OF GROWTH AND DEVELOPMENT IN THE CHILD 0-18
YEARS
Hours: 5 Theory
Specific Objectives
At the end of the unit, the student will be able to:
1.
Discuss the principles of growth and development;
2.
Discuss factors that influence growth and development;
3.
Explain patterns of growth and development;
4.
Explain physical and physiological changes in the major body systems that take place
during the process of growth and development;
5.
Describe the basic divisions of childhood;
6.
Review developmental stages according to major developmental theorists;
7.
Describe developmental tasks for the child at various stages of development;
8.
Explain the influence of mass media on moral and cognitive development;
9.
Describe the role of play in the growth and development of the child.
UNIT 1: Content
1. Definition of terms
Growth
Development
Maturation
Personality
2. Factors influencing growth and development:
Genetics
Gender
Health
Environment
Nutrition
Socio-cultural factors
Interpersonal relationships
3. Patterns of growth and development
Directional: cephalocaudal, proximodistal
Sequential
Differentiation
Developmental pace
4. Physical development
5. Physiological changes in development
6. Basic development of childhood
Neonate
birth-28 days
Infant
29 days-1 year
Toddler
1-3 years
Preschool child
3-5 years
School child
5-12 years
Adolescent
12-18 years
CCC/2012/05/22A
7. Theories of Development
7.1 Freud Psychosexual Stages of Development
Oral
birth to 1 year
Anal
1-3 years
Phallic
3-6 years
Latent
6-12 years
Genital
12 years and over
7.2 Developmental tasks
Erikson: Personality Development
Trust versus mistrust
birth to 1 year
Autonomy versus shame
1-3 years
Initiative versus guilt
3-6 years
Industry versus inferiority
6-12 years
Identity versus role confusion
2-19 years
7.3 Piaget Stages of Cognitive Development
Sensorimotor: (birth - 2 years)
Intellectual development; from reflex to imitative behaviour to object permanence.
Preoperational: (2-7 years)
Egocentrism; Intuitive Reasoning Transductive Reasoning:
Concrete operational: 7-11 years
Inductive reasoning
Formal operational: 12-18 years
deductive and abstract reasoning
7.4 Kohlberg moral development
Pre-conventional (pre-moral level) punishment and obedience orientation
Pre-conventional (pre-moral level) nave instrumental orientation
Conventional good boy-nice girl orientation law and order orientation
Post-conventional, post-conventional or principled level. Social contract orientation
8. Influence of mass media on moral/cognitive development
Movies
Television
Computers
Reading materials
9. Play
Classification
Content
Social character
Functions
Toys
Safety
Age appropriate
Environmental hazards
Stress in childhood
Coping strategies
CCC/2012/05/22A
UNIT 2: PROMOTION AND MAINTENANCE OF HEALTH IN THE CHILD 0-18
YEARS
Hours: 5 Theory
15 Practical
Specific Objectives
At the end of the unit, the student will be able to:
1.
2.
3.
4.
5.
6.
Discuss the role of play in health promotion for the child;
Assess and promote child-parent attachment behaviours (bonding);
Demonstrate an understanding of the role of peer group in the socialization of the child;
Utilize health promotion strategies to achieve and maintain healthy lifestyle of the child;
Identify causes of injury in the child;
Discuss injury preventive strategies for the child.
UNIT 2: Content
1. Health promotion strategies for the child
The Neonate: Birth 28 days
Play
Tactile stimulation
Visual stimulation
Use of sound
Education (caregiver)
Bonding
Wanted child
Relationship between parents/family
Family support
Psychosocial/economic status
Rooming-in
Breast feeding
Temperament of child/parent
Nutrition
Breast feeding on demand
Alternative to breast milk
Weight gain
Nutrition education
Exercise
Freedom to kick
Positioning
Safety
Pre-natal care
Delivery by trained attendant
Identification bracelet at birth
Establishment of respiration at birth
Complete physical assessment
Maintenance of warmth
Cord care
Hand hygiene
Food preparation
Immunization
4
CCC/2012/05/22A
Prevention of accidents
Prevention of infection
Use of cots
Use of car seat
Screening for genetic conditions e.g., sickle cell disease
Infant: 29 days 1 year
Play
Solitary play
Interpersonal contact
Vocalizes
Tactile
Visual - mobiles
Aural - music
Kinetic
Selection of toys safety, durability
Self-amusement
Stage of physical development
Bonding
Social development
Intimate child/caregiver contact
Separation anxiety
Stranger fear
Limit setting
Discipline
Family/sibling relationship
Nutrition
Breast feeding
Weaning/introduction of solids
Selection and preparation of food
Mealtimes
Snacks
Weight gain
Food preparation
Parental education
Oral health
Exercise
Sleep and activity
Motor development
Physical and mental stimulation
Safety
Food tolerance/allergy
Avoidance of small objects/nuts
Childcare arrangements
Discipline
Use of pacifier
Sterilization of equipment
Cot rails
Car seat
Proper positioning
Prompt attention for infections
Immunization encourage completion
5
CCC/2012/05/22A
Injury prevention
Storage of poisons
Prevention of falls
Prevention of suffocation
Water safety/bath time
Safe /durable toys
Safe physical environment
Toddler: 1-3 years
Play
Parallel play
Choice of toys sturdy/durable encourage gross motor skills & creativity
Imitation/fantasy
Gender specific toys
Social interaction
Peer companionship/new experiences
Bonding
Sibling rivalry
Negativitism/regression/rivalry
Loss of parental attention
Grandparents
Carer/nursery
Normality of negativitism
Nutrition
Food preference /finger foods
Physiological anorexia
Picky fussy eaters
Meal planning/selection/preparation
Group eating
Nutrients
Weight gain/static weight/weight loss
Exercise
Constant play/physical activity
Types of play
Pace of play activity
Outdoor/indoor
Choice of toys for cognitive development
Safety
Immunization status
Prompt attention to infections
Prevention of accidents/injuries
Car seat
Bed rails
Safety in the home falls, poisons, electrical sockets, stair gates
Supervision out doors/crowded places/ near water
Prevention of falls
Guided play/supervised play
Explore safely/curiosity
Discipline
Body damage
Helmet/elbow/knee pads
Hygiene habits
Dental health
6
CCC/2012/05/22A
Avoid small hard food e.g., peanut, popcorn
Avoid burns/scalds
Shaking/tossing in air
Pre-Schooler: 3-5 years
Play
Associative play
Alternates quiet play with boisterous play
Electronic/educational toys
Imaginary play- drama
Imaginary playmates
Energetic
Bonding
Bonds with playmates/carers teachers
Accepts parental values
Questions parents prefers peers/teachers
Avoid criticisms and over-protectiveness
Praise for accomplishments
Nutrition
Fads
Food preferences
Dine with family
Willing to try new foods
Attractive presentations
Eats approximately 50% of adult portions
Weight gain /growth parameters according to age
Exercise
Skillful at play
Energetic physical activity
Activity level high
Supervised play parks/climbing/swimming
Safety
Immunization booster
Prone to infections at school colds, chicken pox
Accidents/falls
Physical
Sexual abuse teach awareness/erotic touch
Characteristics of child/adult relationship
Mal treatment
Sex education
Road safety education
Motor car seat belts/helmets
Elbow/knee pads for cycling; skateboarding
Awareness of strangers
Swimming lessons/water safety
School-Age Child: 5-12 years
Play
Team play rituals
Competitive games
Quiet play board games and other activities
Ego mastery
Sense of industry
Pride in accomplishments
7
CCC/2012/05/22A
Bonding
Temperament of child
Temperament of parents
Discipline and limit-setting
Regression
Peer group attachment strong
Separation from family unit
Provide positive statements that demonstrate being valued, important and loved
Nutrition
Likes and dislikes influenced by mass media
Caloric needs
Interest in fast foods/Affinity for junk foods
Irregular family meals/schedule of working parents
Need for foods to promote growth
Obesity
Nutrition education
Parental education
Exercise
Less vigorous play
Display of agility
Increase in physical skills
Competitive sports
Swimming
Dance
Ballet
Climbing/ run/jump/cycle
New skills
Emphasize physical activity for 20-25 minutes at least three times weekly
Adult type activities but not ready for strenuous competitive sports
Safety
Latch key/time alone
Lack of supervision
Delinquent behaviour
Experiment with substance
Emphasize traffic safety/road code
Motor vehicle accident/seat belts/helmets/suitable shoes/eye and elbow shields, bicycle,
scooter and skateboard safety
Water safety
Dental health
Injury prevention
School health
Personal hygiene
Sex play
Sex education
Adolescent: 12-18 years
Play
Competitive sports and games
Organized play physical education in school
Interaction with peers
Risk of overexertion
Bonding
8
CCC/2012/05/22A
Protection and dependence on mutual affection and equality
Turmoil and ambiguity
Facilitate independence while providing love and consistent rules
Peer relationship/peer group/best friend
Heterosexual relationships
Homosexual relationships
Nutrition
Rapid increase in height and size
Discuss healthy eating habits
Food fads
Overeating/obesity
Under-eating/underweight
Fast foods
Increased need for iron and calcium
Attitude towards fast foods
Food habits
Vegetarians
Missed meals
Snacking
Nutrition education
Exercise
Sports
Physical education/organized
Dance
Games competitive
Fitness fads
Safety
Immunization/boosters
Personal care
Vision
Posture
Hearing/noise
Body piercing
Stress/Stress reduction
Substance abuse physical and psychosocial consequences
Tobacco use
Alcohol consumption
Risky behaviour
Diving
Swimming
Sex
Motor vehicles/ driving habits
Sexually transmitted infections
Accidents
Violence
Sports injuries
Firearms
Falls
Suicide
Safety Education including sex education.
UNIT 3: CONCEPTS OF ILLNESS RELATING TO THE CHILD 0-18 YEARS
Hours: 7 Theory
9
CCC/2012/05/22A
10 Practical
Specific Objectives
At the end of this unit; the student will be able to:
1. Describe the influence of childhood morbidity and mortality on child health;
2. Describe the role and responsibility of the nurse in paediatric nursing;
3. Discuss legal and ethical issues relating to child health nursing;
4. Discuss the impact of hospitalization on the child and family;
5. Identify stressors of illness and hospitalization for children during each developmental stage;
6. Outline nursing interventions that prevent anxiety and promote family support during a
childs illness and hospitalization;
7. Describe the methods of assessing and managing pain in children;
8. Formulate guidelines for preparing children for surgery;
9. Describe age appropriate pre and postoperative care of the child undergoing surgery;
10. *Describe the symptoms of normal grief;
11. *Outline nursing interventions that support the child and family facing death;
12. *List common manifestations of childhood cancers;
13. *Demonstrate an understanding of the nursing care associated with caring for the child with cancer;
14. *Discuss interventions that promote the familys optimum adjustment to the child with cancer.
UNIT 3: Content
1. Overview of paediatric nursing
Influence of morbidity and mortality on child health
Role and responsibility of the nurse in paediatric nursing
Legal and ethical issues of child health nursing
2. Hospitalized child
Care of the ill child and family in hospital
Preparing the ill child and family for hospitalization
Preparing family care givers
Preparing the infant
Preparing the toddler and pre-schooler
Preparing the school-age child and adolescent
Admitting the ill child and family to hospital
Promoting positive hospital stay
Minimizing negative effects of procedures
Discharge planning
3. Child having surgery
Preparing a child for surgery
Emotional support
Psychological preparation
Age appropriate pre-operative teaching
Informed consent
Physical preparation
Transportation to surgery
Parental/family support
Post-operative care
10
CCC/2012/05/22A
Immediate
Post-recovery from anaesthesia
Subsequent post-operative care
Discharge information
4. Child with cancer
General considerations
Types of childhood cancers
Warning signals of cancers in children
Treatment modalities
5. Pain management in children
Physiology of pain
Factors affecting pain
Assessing type and degree of pain
Developmental considerations
Pain assessment in children
Pain rating scales
Pain control methods
Pain management
Chronic pain
Acute pain/post op pain
Ongoing pain relief
6. Grieving family
Grief and bereavement
Reaction to grief
The childs understanding of death
Care of the dying child
Care of the family after death of a child
UNIT 4: NURSING CARE OF THE CHILD 0-18 YEARS OLD WITH INTERFERENCE
TO BASIC NEEDS
Hours: 28 Theory
20 Practical
Specific Objectives
At the end of the unit, the student will be able to:
1.
2.
3.
4.
5.
6.
7.
8.
9.
List common health conditions in the child;
Perform health assessment on the child according to age;
Describe the pathophysiology, incidence, clinical manifestation and prognosis of each
disease process;
Explain diagnostic tests for each condition identified;
Describe treatment modalities for the different conditions;
Use the nursing process to provide age appropriate nursing care for the child with
interference to basic needs;
Describe health promotion strategies used to restore health;
Identify community agencies/institutions for involvement in the delivery of health care to
the child and family;
Make necessary referrals in a timely manner to appropriate agencies/institutions in the
delivery of care to the child and family.
UNIT 4: Content
Common health conditions and related nursing care
1. The Respiratory System
Respiratory distress syndrome
11
CCC/2012/05/22A
Asphyxia neonatorum
Mecomium aspiration syndrome
Pneumonia (Broncho-pneumonia, Aspiration pneumonia)
Laryngeal stridor
Laryngo-tracheo bronchitis (Croup)
Coryza
Acute bronchiolitis
Pulmonary tuberculosis
Diphtheria
Foreign body in airway
Smoke inhalation
Influenza
Sinusitis
Allergic rhinitis (Hay fever)
Asthma
Asphyxiation
Drowning/Near drowning
Drug overdose
2. The Cardiovascular System
2.1 Congenital heart disease: Four classifications
Increased pulmonary blood flow
o Ventricular septal defect
o Atrial septal defect)
o Atrioventricular canal
o Patent ductus arteriosus
Obstruction to blood flow leaving the heart
o Pulmonary stenosis
o Aortic stenosis
o Coarctation of the aorta
Mixed blood flow
o Transposition of the great arteries
o Total anomalous pulmonary venous return
o Truncus arteriosus a rare defect
o Hypoplastic left heart syndrome
Decreased pulmonary blood flow
o Tricuspid atresia
o Tetralogy of Fallot
2.2 Acyanotic heart disease versus Cyanotic heart disease
2.3 Congestive heart failure
2.4 Rheumatic Fever
3.
*Nervous System
Intra-cranial haemorrhage
Peripheral nerve injury
Anencephaly
Microcephaly
Hydrocephalus
Spina bifida
Meningocoele
Myelomeningocoele
Tetanus
Poliomyelitis
12
CCC/2012/05/22A
Meningitis
Encephalitis
Head injuries
Epilepsy
Cerebral palsy
Intra-cranial tumours
Neuroblastoma
4. Gastro-Intestinal System
Cleft lip
Cleft palate
Dental caries
Oesophageal atresia
Oesophageal stricture
Gastro-oesophageal reflux
Gastroenteritis
Necrotizing enterocolitis
Tracheo-oesophageal fistula
Gastroschesis/omphalocoele
Hypertrophic pyloric stenosis
Hirschsprungs disease
Hernias
o Hiatal hernia
o Umbilical hernia
o Inguinal hernia
Diarrhoeal diseases
Helminthiasis
Imperforate anus
Protein-energy malnutrition
Intussusseption
Obesity
Hepatitis
Appendicitis
*Reproductive System
Undetermined sex
Malformation of reproductive organs
Congenital adrenogenital syndrome
Undescended testes/Crypto-orchiditis
Vulvo-vaginitis
Vaginitis
Pelvic inflammatory disease
Dysmenorrhoea
Amenorrhoea
Gynaecomastia
Sexually transmitted diseases
HIV/AIDS
Teenage pregnancy
6. *Renal System
Congenital cystic kidneys
Extrophy of the bladder
Polycystic kidney disease
Vesico-urethral reflux
Hypospadias/epispadias/chordee
Urinary tract infection
Ruptured kidney
Ruptured bladder
Nephroblastoma (Wilms Tumour)
5.
13
CCC/2012/05/22A
7.
Phimosis
Paraphimosis
Hydrocoele
Urethritis
Cystitis
Pyelitis
Nephritis
Pyelonephritis
Nephrotic syndrome
Nephritic syndrome
Renal failure (Acute and Chronic)
*Integumentary System
Impetigo
Pemphigus
Eczema
Burns
Dermatitis (contact, diaper, seborrheic)
Tinea (capitis, corporis, pedis, cruris)
Pediculosis (capitis, corporis)
Scabies
Acne
Wounds
*Musculo-skeletal System
Clubfoot
Scoliosis
Juvenile osteochondrosis
Osteogenesis imperfecta
Rheumatoid arthritis
Neonatal tetanus
Fractures
Syndactily/polydactily
Genuvarum /Genuvalgum
Osteomyelitis
Osteosarcoma
9. *Sensory System
Ophthalmia neonatorum
Strabismus
Congenital cataract
Conjunctivitis
Ear infections
o Otitis media
o Otitis externa
Mastoiditis
Tonsillitis /Adenoiditis
Corneal lacerations
Hyphaema
Myopia
Astigmatism
Epistaxis
8.
10.
*The at-risk infant
The child with birth injuries
Rubella syndrome
The child with low APGAR score (below 6)
The pre-term infant
Infant of the diabetic mother
14
CCC/2012/05/22A
Haemolytic disease of the newborn
o Rhesus incompatibility
o ABO incompatibility
Physiological jaundice
Neonatal sepsis
Glucose-6-phosphate dehydrogenase (G6PD) deficiency
Mental retardation
Failure-to-thrive
Anemia
o Folic acid anemia
o Iron deficiency anemia
Poisoning
Learning disability
Attention deficit syndrome/ADHD
Suicide
Trauma
Automobile accidents
Violence
Depression
Abuse
o Physical/Battered child syndrome
o Psychological
o Sexual
11. Genetic/Chromosomal/Endocrine
Sickle cell disease
Thalassaemia
Haemophilia
Down syndrome
Dwarfism
Diabetes
4.0 TEACHING/LEARNING METHODS
Lecture/Discussion
Ward rounds
Demonstration
Role play
Tutorials
Pre- and post-clinical conferences
Projects
Areas used for Learning
Classroom
Library
Hospitals: Paediatric/Adolescent wards and clinics
Community agencies including Non-Government Organizations (NGOs)
Nurseries
Basic Schools
Childrens Homes
Institutions for the mentally and physically challenged children
Post-natal wards and neonatal units
Learning Experiences
Visits to Day Care Centres, Basic Schools, Child Welfare Clinics, Health Centres/Clinics,
Residential/Childrens Homes, Paediatric Wards:
To observe developmental status of children.
To observe the health status of children.
To participate in health education and care.
15
CCC/2012/05/22A
Visits to schools to observe school health services.
Visits to Family Court to observe organization and function.
Visits to institutions of mentally and physically challenged children to observe behaviours
and functions and developmental stages.
5.0 RELATED SKILLS
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
Measuring vital signs of infants and children
Measurement of growth parameters
Holding infant and young children for procedures:
Mommy restraint
Elbow restraint
Clover-hitch restraint
Examination of the ear infant lying
Examination of the ear infant sitting on nurses lap
Lumbar puncture infant/young child
Venepuncture
Administration of medication
Infant feeding (breast, bottle, cup and spoon and NGT)
Bathing infants and children
Collecting specimens from infants and children
Urine specimens
Stool specimens
Blood from heel and finger pricks
Sputum specimens
Throat swabs
Care of infant in incubator
Transporting the ill child
Child barrier nursing/Isolation
Fever reducing measures
Oxygen therapy (cannula, mask, tent and head box)
Nebulization
6.0 ASSESSMENT PROCEDURES
6.1 Module work
Written objective-type tests
Skill laboratory
Attendance
Participation
Projects:
Group assignment/Play
Child/Family case study
Final examination
100%
20%
10%
[5%]
[5%]
20%
[10%]
[10%]
50%
6.2 Skill laboratory assessment criteria
Attendance all practical sessions are mandatory (minimum attendance is 90 %). All
students must be present at the beginning of class (grace period of 15 minutes). In the event
of illness a medical certificate must be presented.
All students must wear a laboratory coat or apron for all practical sessions.
Participation all students are expected to perform a return demonstration.
6.0
BREAKDOWN OF HOURS
Classroom lecture/discussion (3 hours per week)
Practical/Observation Visits and Class Presentations
Mid-Semester Test
Final Examination
16
39 hours
48 hours
1 hour
2 hours
CCC/2012/05/22A
Total Hours
90 hours
7.0 TEXTBOOK AND REFERENCES
7.1 Required Reading
Pillitteri, A. (2010). Maternal and Child Health Nursing: Care of the Childbearing and
Childrearing Family. Baltimore: Lippincott.
7.2 Recommended Reading
Wong, D. L. (1999). Whaley & Wong Nursing Care of Infants and Children. St Louis: C.V.
Mosby.
Wong, D.L & Hockenberry-Eaton, M. (2001). Wongs Essentials of Pediatric Nursing. St.
Louis: C. V. Mosby.
Campbell, S. & Glasper, E. A. (1995).Whaley and Wongs Childrens Nursing. London: C. V.
Mosby.
Ball, J. & Bindler, R. (1999). Paediatric Nursing: Caring for Children. Connecticut: Appleton &
Lange.
Carpenito, L. J. (2002). Handbook of Nursing Diagnoses. Philadelphia: J. B. Lippincott.
8.0
NAME OF SYLLABUS WRITER/DEVELOPER
8.1
NAME OF SYLLABUS REVIEWER/S
Marjorie E. Ming and Marsha Cole Lecturers
9.0
DATE OF PRESENTATION OR REVISION
November, 2011
10.0 DATE OF ACCEPTANCE ________________
___________________________________
Programme Director
____________________________________
OCDE
SUMMARY of CHANGES MADE to: The Beginning Family: Part I1
In Unit 3 conditions were listed according to age group, same revised and now listed according to body
systems.
2. Changes made to evaluation pattern of the course.
3. Added skills laboratory criteria.
1.
17
Potrebbero piacerti anche
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- SkinDocumento43 pagineSkinFhen Farrel100% (1)
- Digestive SystemDocumento48 pagineDigestive SystemJerilee SoCute WattsNessuna valutazione finora
- Urinary SystemDocumento105 pagineUrinary SystemJerilee SoCute WattsNessuna valutazione finora
- The Circulatory System-: TransportDocumento13 pagineThe Circulatory System-: TransportJerilee SoCute WattsNessuna valutazione finora
- The HeartDocumento42 pagineThe HeartJerilee SoCute WattsNessuna valutazione finora
- Skin Diseases Disorders ConditionsDocumento104 pagineSkin Diseases Disorders ConditionsJerilee SoCute WattsNessuna valutazione finora
- PDFDocumento64 paginePDFJerilee SoCute WattsNessuna valutazione finora
- The Digestive System: Cont'd (From Swallowing)Documento56 pagineThe Digestive System: Cont'd (From Swallowing)Jerilee SoCute WattsNessuna valutazione finora
- Reproductive SystemDocumento80 pagineReproductive SystemJerilee SoCute WattsNessuna valutazione finora
- Respiration System PP TDocumento57 pagineRespiration System PP Troyanirudh99Nessuna valutazione finora
- The Digestive System Part 1Documento28 pagineThe Digestive System Part 1Jerilee SoCute WattsNessuna valutazione finora
- The Conducting System of The HeartDocumento37 pagineThe Conducting System of The HeartJerilee SoCute WattsNessuna valutazione finora
- The Lymphatic SystemDocumento50 pagineThe Lymphatic SystemJerilee SoCute Watts100% (1)
- Reproduction and DevelopmentDocumento53 pagineReproduction and DevelopmentJerilee SoCute WattsNessuna valutazione finora
- Pulmonary and Systemic CircuitsDocumento38 paginePulmonary and Systemic CircuitsJerilee SoCute WattsNessuna valutazione finora
- The Digestive System EssayDocumento3 pagineThe Digestive System EssayJerilee SoCute Watts0% (1)
- Lecture 21 - Respiratory SystemDocumento59 pagineLecture 21 - Respiratory SystemSkyBirdNessuna valutazione finora
- Review Questions - HeartDocumento1 paginaReview Questions - HeartJerilee SoCute WattsNessuna valutazione finora
- Human ReproductionDocumento42 pagineHuman ReproductionAliDarimiKRNessuna valutazione finora
- Respiratory System 2Documento39 pagineRespiratory System 2Jerilee SoCute WattsNessuna valutazione finora
- Respiratory System 1Documento29 pagineRespiratory System 1Jerilee SoCute WattsNessuna valutazione finora
- Respiratory Centers of The BrainDocumento36 pagineRespiratory Centers of The BrainJerilee SoCute WattsNessuna valutazione finora
- Reproductive System DisordersDocumento62 pagineReproductive System DisordersJerilee SoCute Watts100% (2)
- Lymphatic System: Marieb Chapter 20Documento22 pagineLymphatic System: Marieb Chapter 20Jerilee SoCute WattsNessuna valutazione finora
- Lecture 1 Cardiovascular SystemDocumento70 pagineLecture 1 Cardiovascular SystemJerilee SoCute WattsNessuna valutazione finora
- Platelets and HemostasisDocumento19 paginePlatelets and HemostasisJerilee SoCute WattsNessuna valutazione finora
- Reproduction NotesDocumento20 pagineReproduction NotesMario BaemamentengNessuna valutazione finora
- Reproduction Summary NotesDocumento16 pagineReproduction Summary NotesJerilee SoCute WattsNessuna valutazione finora
- Unit 6 OsmolarityDocumento59 pagineUnit 6 Osmolaritykrystal1994Nessuna valutazione finora
- Lecture 2 Cardiovascular SystemDocumento70 pagineLecture 2 Cardiovascular SystemJerilee SoCute WattsNessuna valutazione finora
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Binder 3 of 4 Dec-2018Documento1.169 pagineBinder 3 of 4 Dec-2018Anonymous OEmUQuNessuna valutazione finora
- Igcse Revision BookDocumento23 pagineIgcse Revision BookJo Patrick100% (2)
- Pref - 2 - Grammar 1.2 - Revisión Del IntentoDocumento2 paginePref - 2 - Grammar 1.2 - Revisión Del IntentoJuan M. Suarez ArevaloNessuna valutazione finora
- Iron Ore ProcessDocumento52 pagineIron Ore Processjafary448067% (3)
- All Pop SongsDocumento53 pagineAll Pop SongsMadeleneQuiogueNessuna valutazione finora
- Lc420euf Sda1 LGDocumento41 pagineLc420euf Sda1 LGjavierNessuna valutazione finora
- Tuesday, 16 November 2021 - Afternoon Discovering ElectronicsDocumento20 pagineTuesday, 16 November 2021 - Afternoon Discovering Electronicsnvmalt070Nessuna valutazione finora
- Present Simple TaskDocumento3 paginePresent Simple TaskMaria AlejandraNessuna valutazione finora
- E-OLSS: Electronic ControlDocumento12 pagineE-OLSS: Electronic ControlSamidiNessuna valutazione finora
- Crashing Is A Schedule Compression Technique Used To Reduce or Shorten The Project ScheduleDocumento1 paginaCrashing Is A Schedule Compression Technique Used To Reduce or Shorten The Project ScheduleRaymart BulagsacNessuna valutazione finora
- Ni Elvis ManualDocumento98 pagineNi Elvis ManualZhi YiNessuna valutazione finora
- PEDocumento12 paginePEMae Ann Base RicafortNessuna valutazione finora
- Ask A Monk EnlightenmentDocumento16 pagineAsk A Monk EnlightenmentPetruoka EdmundasNessuna valutazione finora
- Southwest Airlines Final ReportDocumento16 pagineSouthwest Airlines Final Reportapi-427311067Nessuna valutazione finora
- Electrical Power System Device Function NumberDocumento2 pagineElectrical Power System Device Function Numberdan_teegardenNessuna valutazione finora
- Aesculap Saw GD307 - Service ManualDocumento16 pagineAesculap Saw GD307 - Service ManualFredi PançiNessuna valutazione finora
- 9701 w09 QP 21Documento12 pagine9701 w09 QP 21Hubbak KhanNessuna valutazione finora
- Time Value of Money LectureDocumento54 pagineTime Value of Money LectureRanin, Manilac Melissa SNessuna valutazione finora
- ASCE Snow Loads On Solar-Paneled RoofsDocumento61 pagineASCE Snow Loads On Solar-Paneled RoofsBen100% (1)
- Manual 35S EnglishDocumento41 pagineManual 35S EnglishgugiNessuna valutazione finora
- The Dry Bulk Management StandardDocumento18 pagineThe Dry Bulk Management Standardamu_more44100% (1)
- (Eng) Zx890lch 5a Ks En316Documento13 pagine(Eng) Zx890lch 5a Ks En316MC TAK LEENessuna valutazione finora
- 09 Passport 7K 15K Performance Guidelines PCR 3 0Documento44 pagine09 Passport 7K 15K Performance Guidelines PCR 3 0thed719Nessuna valutazione finora
- Meet The Profesor 2021Documento398 pagineMeet The Profesor 2021Raúl AssadNessuna valutazione finora
- MATLAB Fundamentals Quick ReferenceDocumento43 pagineMATLAB Fundamentals Quick ReferenceCarlos Manuel Cardoza EspitiaNessuna valutazione finora
- Kodak Easyshare Z712 Is Zoom Digital Camera: User'S GuideDocumento75 pagineKodak Easyshare Z712 Is Zoom Digital Camera: User'S GuideIronko PepeNessuna valutazione finora
- Raspberry Pi 3 and BeagleBone Black For Engineers - UpSkill Learning 124Documento124 pagineRaspberry Pi 3 and BeagleBone Black For Engineers - UpSkill Learning 124Dragan IvanovNessuna valutazione finora
- QuantAssay Software Manual 11-Mar-2019Documento51 pagineQuantAssay Software Manual 11-Mar-2019LykasNessuna valutazione finora
- Poems Prescribed For 2012-2014 English B CSEC ExamsDocumento24 paginePoems Prescribed For 2012-2014 English B CSEC ExamsJorge Martinez Sr.100% (2)
- Basses: Pricelist March 2019Documento3 pagineBasses: Pricelist March 2019zhaihaijunNessuna valutazione finora