Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Poli Arthritis ......
Caricato da
sylviaaa08Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Poli Arthritis ......
Caricato da
sylviaaa08Copyright:
Formati disponibili
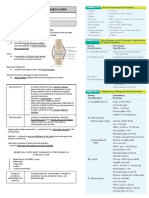
Acute polyarthritis has a very wide differential diagnosis, presenting significant
diagnostic difficulties. Where oligoarthritis (<5 joints affected) is the presenting feature,
some of the causes of acute monoarthritis must be considered, of which the most
important not to miss is septic arthritis (particularly that due to gonococcal
infection which may affect several joints).
History
Demographic details such as age, sex, ethnic origin and occupation can give
useful diagnostic clues. For example, juvenile chronic arthritis is the most common
arthritis in children.
Family history may be present in cases of rheumatoid arthritis (RA), seronegative
arthropathies andosteoarthritis.
Pain is not often discriminatory in diagnostic terms. Speed of onset may help
- gout tends to come on abruptly, whereas RA is usually more gradual. Similarly,
gout tends to cause very severe, excruciating pain.
Diurnal variation of symptoms may give useful clues. An inflammatory arthritis
tends to be worse on waking and eases as the day goes on. Mechanical pain tends
to have the opposite effect.
Ask about morning stiffness and joint swelling.
Migratory arthritis (flitting from joint to joint over a period of days) might suggest
gonococcal infection, rheumatic fever (RF), sarcoidosis, systemic lupus
erythematosus (SLE), Lyme disease or bacterial endocarditis.
Pattern of joint involvement is very useful in suggesting a diagnosis. For example:
Osteoarthritis of the hand affects the distal interphalangeal (DIP) and
proximal interphalangeal (PIP) joints but spares the metacarpophalangeal
(MCP) joints.
RA affects the MCP and PIP joints but spares the DIP joints.
Psoriatic arthritis, crystal arthropathies and sarcoidosis can affect all these
joints.
Large weight-bearing joints and facet joints of the spine are often affected
by osteoarthritis.
Axial involvement in younger patients suggests a seronegative arthropathy such
as ankylosing spondylitis or inflammatory bowel disease-associated arthropathy.
Symmetrical joint involvement tends to occur in systemic syndromes such as RA,
SLE, viral arthritis and drug/serum sickness reactions.
In asymmetrical joint involvement consider gout, psoriatic arthritis, and reactive
arthritis.
Extra-articular symptoms should be asked about and can aid diagnosis. The
eyes, parotid glands, skin, mouth, genitals and muscles can all be affected by
rheumatological diagnoses.
Take a full drug history - some drugs (eg, hydralazine, procainamide, quinidine
and minocycline) can cause a lupus-like syndrome [3] and there have been reports
of a variety of drugs associated with polyarthralgia (eg, moxifloxacin). [4]
Systemic symptoms should also be sought - eg, fever and weight loss. [5]
Are there any other associated presenting symptoms - eg, abdominal or
respiratory disease?
Examination
Check temperature.
Nail changes (eg, pitting) may suggest psoriatic arthropathy.
Look at eyes for signs of inflammation.
Check major lymph nodes for evidence of lymphadenopathy.
Check skin for rashes (eg, psoriasis, SLE) and evidence of vasculitis. Feel
extensor aspects of forearms for nodules. Check shins for evidence of erythema
nodosum.
Cardiac examination - listen for murmurs if there is reason to suspect RF.
Abdominal examination - may reveal evidence of hepatomegaly and/or
splenomegaly.
Examine other systems as indicated by the history and clinical hypotheses.
Joint examination:
Look for signs of inflammation in the joint, such as heat, tenderness and
synovial thickening.
Establish whether there are symmetrical or asymmetrical joints involved.
Active and passive movements of affected joints and the degree of pain
and/or crepitus may also be helpful. However, crepitus and pain will not
differentiate between inflammatory and non-inflammatory causes of joint pain.
They may, however, give some indication as to the degree of damage.
Also examine the structures around the joint and determine if the
symptoms are intra-articular or periarticular.
Investigations
Where there is any suspicion of septic arthritis, immediate aspiration of synovial fluid
should be carried out. Synovial fluid analysis may play a role in diagnosis of crystal
arthropathies and inflammatory conditions but results need to be carefully interpreted in
context. See the separate article on Acute Monoarthritis for a table of synovial fluid
findings in the more common causes of joint inflammation.
Urinalysis - indicates any renal involvement.
Blood tests - FBC, ESR, CRP and U&E are useful screening investigations which
give diagnostic clues.
Autoantibodies - can help to confirm a diagnosis but are often relatively
nonspecific or insensitive.[2] They should be interpreted in the context of the clinical
presentation, preferably with specialist rheumatological input for the less common
markers.
Radiology - X-rays play a variable role in their contribution to diagnosis but are a
useful first-line investigation. Other imaging modalities may need to be conducted
with rheumatological/radiological advice.
Joint aspiration is helpful in the differential diagnosis of arthritis and is the
definitive method for diagnosis of septic arthritis and crystal arthritis. [7]
Management
Directed at the underlying diagnosis. See the links to the individual diagnoses for detail.
Symptomatic treatment of inflammatory conditions with non-steroidal anti-inflammatory
drugs should be considered whilst awaiting the evolution of an arthritis, where there are
no contra-indications or significant drug interactions.
Where there is a significant inflammatory illness as revealed by clinical severity and
CRP/ESR, etc, early advice for disease-modifying interventions can significantly reduce
joint pathology in some conditions.
If in doubt, seek advice on the appropriate course.
Potrebbero piacerti anche
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Mental Health Effects of ObesityDocumento7 pagineMental Health Effects of ObesityMohd FaizNessuna valutazione finora
- SyndesmologyDocumento3 pagineSyndesmologyPetru BuruianaNessuna valutazione finora
- Complications of Ankylosing SpondylitisDocumento10 pagineComplications of Ankylosing SpondylitisNafeesa AliNessuna valutazione finora
- Word Search Muscles Bones and Joints-3Documento4 pagineWord Search Muscles Bones and Joints-3api-308609686Nessuna valutazione finora
- Dissertation ArthritisDocumento5 pagineDissertation ArthritisWriteMyPaperForMeIn3HoursSpringfield100% (1)
- Chapter 5 Skeletal SystemDocumento9 pagineChapter 5 Skeletal SystemClarisse Anne QuinonesNessuna valutazione finora
- Knee Osteoarthritis A Review of LiteratureDocumento8 pagineKnee Osteoarthritis A Review of LiteratureKurnia Elka VidyarniNessuna valutazione finora
- Chapter 5 The Skeletal SystemDocumento139 pagineChapter 5 The Skeletal SystemCharlz ZipaganNessuna valutazione finora
- Skeletal System - Study MaterialDocumento4 pagineSkeletal System - Study MaterialNabeel UndreNessuna valutazione finora
- Chapter 7. Musculoskeletal Injuries and DisordersDocumento22 pagineChapter 7. Musculoskeletal Injuries and DisordersMonica CiorneiNessuna valutazione finora
- Home Remedies For Joint Pain - Find Relief The Natural Way - Top 10 Home RemediesDocumento33 pagineHome Remedies For Joint Pain - Find Relief The Natural Way - Top 10 Home RemediesshaukijameelNessuna valutazione finora
- Muskuloskelatal (English) : Senin Selasa Rabu Kamis JumatDocumento3 pagineMuskuloskelatal (English) : Senin Selasa Rabu Kamis JumatArsul RNessuna valutazione finora
- Thesis-MECHANICAL EVALUATION OF POLYCARBONATEDocumento185 pagineThesis-MECHANICAL EVALUATION OF POLYCARBONATEWahyu DwilestariNessuna valutazione finora
- Introduction To Community Health: What Is Community Health and Why Is It Important?Documento35 pagineIntroduction To Community Health: What Is Community Health and Why Is It Important?Mark Johnson Dela PeñaNessuna valutazione finora
- Science 6 Skeletal SystemDocumento10 pagineScience 6 Skeletal SystemJECONIAH ADONANessuna valutazione finora
- Chapter 015Documento14 pagineChapter 015api-281340024100% (1)
- Causes of Restriction of ROMDocumento33 pagineCauses of Restriction of ROMRonak Patel100% (3)
- Patient Education Gout The Basics - UptodateDocumento3 paginePatient Education Gout The Basics - Uptodateapi-347602513Nessuna valutazione finora
- GONIOMETRYDocumento20 pagineGONIOMETRYkushi98mandyaNessuna valutazione finora
- Interna Medicine RheumatologyDocumento15 pagineInterna Medicine RheumatologyHidayah13Nessuna valutazione finora
- Human Anatomy JointsDocumento17 pagineHuman Anatomy JointsEntirety 4uNessuna valutazione finora
- Barral InstituteDocumento32 pagineBarral InstituteIoan-ovidiu Cordis100% (3)
- Compound RX Form PDFDocumento1 paginaCompound RX Form PDFGordon FagrasNessuna valutazione finora
- Acute Arthritis: BY Dr. Mehrunnisa UmarDocumento64 pagineAcute Arthritis: BY Dr. Mehrunnisa UmardrusmanjamilhcmdNessuna valutazione finora
- AUBF Synovial FluidDocumento6 pagineAUBF Synovial FluidRichelyn Grace B. VenusNessuna valutazione finora
- Arthritis: Osteoarthritis (OA or Degenerative Arthritis) Osteoarthritis FactsDocumento6 pagineArthritis: Osteoarthritis (OA or Degenerative Arthritis) Osteoarthritis FactsFelisitas FellNessuna valutazione finora
- Physiology in Sports - PE, Class 12Documento21 paginePhysiology in Sports - PE, Class 12Jasnoor Singh RainooNessuna valutazione finora
- Complete: BiologyDocumento8 pagineComplete: BiologyConcordia Mannargudi20% (5)
- Advanced Muscle Integration TechniqueDocumento4 pagineAdvanced Muscle Integration Techniquepatsim0% (1)
- MC1 REVIEWER (Skeletal System) - PRELIMSDocumento5 pagineMC1 REVIEWER (Skeletal System) - PRELIMSFrancine Dominique CollantesNessuna valutazione finora