Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Essential Respiratory Calculation: Lung Volumes, Dead Space, and Alveolar Ventilation
Caricato da
Héctor GarcíaTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Essential Respiratory Calculation: Lung Volumes, Dead Space, and Alveolar Ventilation
Caricato da
Héctor GarcíaCopyright:
Formati disponibili
108
PHYSIOLOGY CASES AND PROBLEMS
Case 20
Essential Respiratory Calculations: Lung Volumes,
Dead Space, and Alveolar Ventilation
This case will guide you through some of the important, basic calculations involving the respiratory system. Use the information provided to answer the questions.
Figure 31 shows a record from a person breathing into and out of a spirometer. The volume
displaced by the spirometer's bell is recorded on calibrated paper. The person took one normal
breath followed by a maximal inhalation, a maximal exhalation, and another normal breath.
(The volume remaining in the lungs after maximal expiration is not measurable by spirometry
and was determined by other techniques.)
1000
Time
Figure 3-1 Spirometry diagram showing a tidal breath, followed by maximal inspiration and maximal
expiration.
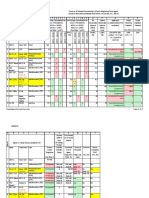
TABLE 3-1
Respiratory Values for Case 20
Breathing rate
Pac02 (arterial Pc02)
Pao2 (arterial P02)
Pko, (Pc02 in expired air)
Pio, (P02 in humidified inspired air)
P1c 02 (Pco2 in inspired air)
c),. (rate of CO 2 production)
(rate of 02 consumption)
12 breaths/min
40 mm Hg
100 mm Hg
30 mm Fig
150 mm Hg
0
200 mL/min
250 mL/min
Pc02, partial pressure of carbon dioxide; P0,, partial pressure of oxygen.
RESPIRATORY PHYSIOLOGY
pi
109
QUESTIONS
1. Using the information provided in Table 3-1 and Figure 3-1, what are the values for tidal volume,
inspiratory capacity, expiratory reserve volume, functional residual capacity, vital capacity, and
total lung capacity? (Hint: It may be helpful to label the spirometry diagram with the names of
the lung volumes and capacities.)
2. What is the name of the volume remaining in the lungs after maximal expiration that is not
measurable by spirometry? What other lung volumes or capacities are not measurable by
spirometry?
3. What is the meaning of the term "physiologic dead space"? What assumptions are made in calculating the physiologic dead space? What is the volume of the physiologic dead space in this
case?
4. What is the value for minute ventilation?
5. What is the value for alveolar ventilation?
6. What is the alveolar ventilation equation? Use this equation to calculate alveolar partial pressure
of carbon dioxide (PAcc,,, ) in this case.
7. What is the value for alveolar partial pressure of oxygen (PA02)?
110 PHYSIOLOGY CASES AND PROBLEMS
FA1 ANSWERS AND EXPLANATIONS
1. Static lung volumes (except for residual volume) are measured by spirometry. They include the
tidal volume, inspiratory reserve volume, expiratory reserve volume, and residual volume. Lung
capacities include two or more lung volumes. If you began by labeling the lung volumes and
capacities, as shown in Figure 3-2 and Table 3-2, then determining the numerical values should
be a straightforward exercise.
(6000
5000
Inspiratory
reserve
volume
Inspiratory
capacity
4000
Vital
capacity
Tidal
volume
Total
lung
capacity
3000
Expiratory
reserve j 2000
volume
Residual
volume
Functional
residual
capacity
1000
Time
Figure 3-2 Spirometry diagram labeled with lung volumes and capacities.
TABLE 3-2
Lung Volumes and Capacities in Case 20
Tidal volume
Inspiratory capacity
Expiratory reserve volume
Functional residual capacity
Vital capacity
Total lung capacity
500 ml,
3500 mL
1000 mL
2500 mL
4500 mL
6000 mL
2. The volume remaining in the lungs after maximal expiration is called the residual volume. This
volume is not measurable by spirometry. Therefore, any lung volume or capacity that includes
the residual volume is also not measurable by spirometry (i.e., functional residual capacity, total
lung capacity).
RESPIRATORY PHYSIOLOGY 111
3. Physiologic dead space is the volume of air in the lungs that does not participate in gas
exchange (i.e., it is "dead"). Physiologic dead space has two components: (1) anatomic dead
space, which is the volume of conducting airways; and (2) functional dead space, which is alveoli that do not participate in gas exchange (i.e., alveoli that are ventilated, hut are not perfused
by pulmonary capillary blood). By comparing the physiologic dead space with the tidal volume,
it is possible to estimate how much ventilation is "wasted."
The volume of the physiologic dead space is estimated with a method based on the Pco 2 of
expired air (PEco2 ) that applies the following three assumptions. (1) There is no CO 2 in inspired
air (i.e., Picot = 0). (2) The physiologic dead space does not participate in gas exchange; therefore, it does not contribute any CO 2 to expired air. (3) All of the CO2 in expired air comes from
the exchange of CO2 in functioning alveoli.
When discussing physiologic dead space, it is helpful to consider two examples, one in which
there is no physiologic dead space and the other in which some degree of physiologic dead space
is present. If there is no physiologic dead space, PEr 02 should equal the Pc02 in alveolar air (PAco2).
If there is a physiologic dead space present, then PEco 2 will be "diluted" by air expired from the
dead space (air that contains no CO,), and PEco2 will be less than PAco2.
One problem in comparing the Pc 02 of alveolar and expired air is that alveolar air cannot be
sampled directly; in other words, we cannot measure PAco 2. This problem can be solved, however, because alveolar gas normally equilibrates with pulmonary capillary blood (which
becomes systemic arterial blood). Thus, by measuring arterial Pco (Paco2), we can determine
PAc02. Using the foregoing assumptions, physiologic dead space is calculated as follows:
VD = VT X
Pa co, PE c0,
Paco2
where
Vo = physiologic dead space (mL)
VT = tidal volume (mL)
Paco2 = Pcoz of arterial blood (mm Hg)
PEco2 = Pc.02 of expired air (mm Hg)
In words, physiologic dead space is the tidal volume multiplied by a fraction that expresses the
dilution of alveolar Pco , by dead-space air.
We have all of the values we need to calculate the physiologic dead space in this case. Tidal
volume was determined from spirometry, and the values for Paco 2 and PEco2 are given in the
case data.
VD = VT x Pac' PEccrz
Paco2
= 500 mL x 40 mm Hg 30 mm Hg
40 mm Hg
= 500 mL x 0.25
= 125 mL
Thus, in the tidal volume of 500 mL, 125 mL occupied the physiologic dead space (i.e., the conducting airways and nonfunctional alveoli). In other words, 125 mL was "wasted" in lung
spaces that cannot participate in gas exchange.
4. Minute ventilation is the tidal volume multiplied by the number of breaths per minute. In this
case:
Minute ventilation VT x breaths/min
= 500 mL x 12/min
= 6000 mL/min
112 PHYSIOLOGY CASES AND PROBLEMS
5. Alveolar ventilation (VA) is minute ventilation corrected for physiologic dead space, or:
VA = (VT VD) x breaths/min
where
VA = alveolar ventilation (mL/min)
VT = tidal volume (mL)
Vo = physiologic dead space (mL)
In this case, tidal volume was determined by spirometry (500 mL), and physiologic dead space
was calculated in the previous question (125 mL). Thus, alveolar ventilation is:
VA = (500 mL 125 mL) x 12 breaths/min
= 375 mL x 12 breaths/min
= 4500 mL/min
6. In considering these questions about alveolar ventilation and alveolar Pco 2, perhaps you wondered what alveolar ventilation has to do with alveolar Pco 2 . The answer is everything! The
fundamental relationship in respiratory physiology is an inverse correlation between alveolar
ventilation (the volume of air reaching functional alveoli per minute) and alveolar Pco 2 . If CO2
production is constant, the higher the alveolar ventilation, the more CO 2 expired and the
lower the alveolar Pco2 . Conversely, the lower the alveolar ventilation, the less CO 2 expired
and the higher the alveolar Pco 2 . This relationship is expressed by the alveolar ventilation
equation:
Vco, x K
PAco,
Rearranging to solve for PAc02:
PACO2=
\ICC/ 2 X
where
PAc02 = alveolar P002
VA = alveolar ventilation
VCO2 = rate of CO2 production (mL/min)
K = constant (863 mm Hg)
The constant (K) requires a brief explanation. The value for K is 863 mm Hg under conditions
of BTPS, when VA and Vc02 are expressed in the same units (e.g., mL/min). BTPS refers to body
temperature (310 K), ambient pressure (760 mm Hg), and gas saturated with water vapor.
Now, let's calculate the value for Paco,. The rate of CO 2 production was given (200 mL/min),
and alveolar ventilation was calculated in the previous question (4500 mL/min).
200 mL/min
PAco, =
x 863 mm Hg
4500 mL/min
= 38.4 mm Hg
7. Because we cannot sample alveolar gas, we cannot directly measure PAD ,. However, we can use
the following approach to estimate its value. PA 02 is determined by the balance between removal
of 02 from alveolar gas (to meet the body's demands for 0 2 ) and replenishment of 0 2 by alveolar ventilation. Therefore, if 0 2 consumption is constant, alveolar Po, is determined by alveolar
ventilation (just as alveolar Pco 2 is determined by alveolar ventilation).
This relationship is expressed by the alveolar gas equation, which incorporates the factors
that determine PA0 , [including partial pressure of 0 2 in inspired air (P102)1, PAco 2 (which reflects
alveolar ventilation, as explained earlier), and respiratory quotient (R, the ratio of CO 2 production to 0 2 consumption):
RESPIRATORY PHYSIOLOGY 113
PA 02 = P102 PAcoz
R
where
PA02 = alveolar P 02 (mm Hg)
P1 0, = P 02 in inspired air (mm Hg)
PAc0, = alveolar Pc 02 (mm Hg)
R = respiratory quotient (ratio of CO 2 production to 0 2 consumption)
In this case, the value for P102 (150 mm Hg) was given, the value for PAco z (38.4 mm Hg) was
calculated in the previous question, and the value for respiratory quotient can be calculated as
the rate of CO 2 production (200 mL/min) divided by the rate of 02 consumption (250 mL/min),
or 0.8.
PA , = 150
mm Hg 38.4 mm Hg
0.8
= 150 mm Hg 48 mm Hg
= 102 mm Hg
Key topics
Alveolar gas equation
Alveolar ventilation
Alveolar ventilation equation
Anatomic dead space
Expiratory reserve volume
Functional residual capacity
Inspiratory capacity
Inspiratory reserve volume
Minute ventilation
Physiologic dead space
Residual volume
Respiratory quotient
Spirometry
Tidal volume
Total lung capacity
Vital capacity
Potrebbero piacerti anche
- Stephen C. Wood, Ph.D. Medical Physiology Metabolic Rate and Alveolar VentilationDocumento9 pagineStephen C. Wood, Ph.D. Medical Physiology Metabolic Rate and Alveolar VentilationSimran SukhijaNessuna valutazione finora
- Respi PhysioDocumento7 pagineRespi PhysioAmal JohnsonNessuna valutazione finora
- Pulmonary VentilationDocumento35 paginePulmonary Ventilationnirilib100% (1)
- AbgDocumento66 pagineAbgindyaphdNessuna valutazione finora
- Arterial Blood Gas InterpretationDocumento65 pagineArterial Blood Gas InterpretationDaniel AryanNessuna valutazione finora
- PaCO2 and End-Tidal PCO2Documento3 paginePaCO2 and End-Tidal PCO2phobicmdNessuna valutazione finora
- Anesth AnalgDocumento9 pagineAnesth Analgfher14bcNessuna valutazione finora
- Breathtaking Physics - Human Respiration As A HeatDocumento3 pagineBreathtaking Physics - Human Respiration As A HeatErik MaldonadoNessuna valutazione finora
- 15, 16, and 17 - Respiratorio 2011Documento86 pagine15, 16, and 17 - Respiratorio 2011Redes HostNessuna valutazione finora
- Arterial Blood Gas InterpretationDocumento66 pagineArterial Blood Gas InterpretationlenafitriyaniNessuna valutazione finora
- Respiration HandoutDocumento9 pagineRespiration HandoutSharif M Mizanur RahmanNessuna valutazione finora
- AbgDocumento66 pagineAbgIan OrwaNessuna valutazione finora
- Calculations Commonly Used in Respiratory Care (Saunders)Documento15 pagineCalculations Commonly Used in Respiratory Care (Saunders)Gleo MatthewNessuna valutazione finora
- Oxygen Toxicity CalculationsDocumento12 pagineOxygen Toxicity CalculationsAdmNessuna valutazione finora
- Review of Respiratory PhysiologyDocumento46 pagineReview of Respiratory Physiologylovelyc95Nessuna valutazione finora
- Chapter 1 Respiratory System Nomenclature and Ambient ConditionsDocumento9 pagineChapter 1 Respiratory System Nomenclature and Ambient Conditionsaisyahasrii_Nessuna valutazione finora
- Respiratory System During A Progressive Work TestDocumento11 pagineRespiratory System During A Progressive Work TestDilanNessuna valutazione finora
- Helpful Formulas for Gas Exchange, Mechanics, Weaning, Acid-Base, and CirculationDocumento2 pagineHelpful Formulas for Gas Exchange, Mechanics, Weaning, Acid-Base, and CirculationJen NeeNessuna valutazione finora
- CO2 NarcoseDocumento5 pagineCO2 NarcoseHasan NyambeNessuna valutazione finora
- Capnography in DogsDocumento14 pagineCapnography in DogswalczakcNessuna valutazione finora
- Ventilation: Describe Alveolar and Pulmonary VentilationDocumento6 pagineVentilation: Describe Alveolar and Pulmonary VentilationNorrifhan Akmal IsmailNessuna valutazione finora
- Measurement of Lung Volumes by Plethysmography: Ers/Ats Workshop Report SeriesDocumento13 pagineMeasurement of Lung Volumes by Plethysmography: Ers/Ats Workshop Report SeriesCarlos Cortez MansillaNessuna valutazione finora
- Abnormal Ventilation, Abnormal Gas ExchangeDocumento52 pagineAbnormal Ventilation, Abnormal Gas ExchangekateNessuna valutazione finora
- Wexler and Lok Formula paCO2Documento3 pagineWexler and Lok Formula paCO2riyty54y54Nessuna valutazione finora
- Respiratory PhysiologyDocumento113 pagineRespiratory PhysiologyNurul AfiqahNessuna valutazione finora
- Translateturn Off Instant TranslationDocumento38 pagineTranslateturn Off Instant TranslationListaNessuna valutazione finora
- Arterial Blood Gas InterpretationDocumento66 pagineArterial Blood Gas InterpretationkabatchinoooNessuna valutazione finora
- Respiratory ICU PDFDocumento130 pagineRespiratory ICU PDFAhmed Shihab AhmedNessuna valutazione finora
- Resp PhysiologyDocumento45 pagineResp PhysiologyGirija BhamidiNessuna valutazione finora
- Acute Respiratory Failure Learning Guide: Phone: Email: Campus AddressDocumento8 pagineAcute Respiratory Failure Learning Guide: Phone: Email: Campus Addressiancooke09Nessuna valutazione finora
- Test Bank For Mechanical Ventilation 7th Edition J M CairoDocumento13 pagineTest Bank For Mechanical Ventilation 7th Edition J M CairoMary Lawson100% (33)
- Respiratory PhysiologyDocumento137 pagineRespiratory PhysiologysramvigneshNessuna valutazione finora
- 3 Gaseous Exchange Through The Respiratory Membrane.Documento23 pagine3 Gaseous Exchange Through The Respiratory Membrane.Ahmed AliNessuna valutazione finora
- Blood GasDocumento31 pagineBlood GasHusna Nur FitrianaNessuna valutazione finora
- Lung Volumes & CapacitiesDocumento35 pagineLung Volumes & CapacitiesEfrain AnayaNessuna valutazione finora
- CapnographyReferenceHandbook OEM1220ADocumento40 pagineCapnographyReferenceHandbook OEM1220Abayu_teNessuna valutazione finora
- Transfer FaktorDocumento19 pagineTransfer FaktorJelenaJankovNessuna valutazione finora
- Rules and Equations for Oxygen Therapy and Gas ExchangeDocumento11 pagineRules and Equations for Oxygen Therapy and Gas ExchangeJenn77x1Nessuna valutazione finora
- Respiratory Acidosis 2Documento11 pagineRespiratory Acidosis 2soyabosticaNessuna valutazione finora
- Respiratory Care Standard Abbreviations and SymbolsDocumento6 pagineRespiratory Care Standard Abbreviations and SymbolsHussein FatalNessuna valutazione finora
- 653 Full PDFDocumento5 pagine653 Full PDFalejandroNessuna valutazione finora
- 11 Respiratory SystemDocumento19 pagine11 Respiratory SystemSenthereng MoaisiNessuna valutazione finora
- Arterial Blood Gas InterpretationDocumento69 pagineArterial Blood Gas InterpretationostuffeNessuna valutazione finora
- Test Bank For Pilbeams Mechanical Ventilation 5th Edition CairoDocumento13 pagineTest Bank For Pilbeams Mechanical Ventilation 5th Edition Cairochowryurduq0krhNessuna valutazione finora
- Ajrccm 160 1 9807127Documento11 pagineAjrccm 160 1 9807127DPC LUMAJANGNessuna valutazione finora
- Oxygen Deficit, EPOCDocumento2 pagineOxygen Deficit, EPOCCorteza, Ricardo Danilo E. UnknownNessuna valutazione finora
- Pulmonary Physiology - ACS CC Review Course - FinalDocumento8 paginePulmonary Physiology - ACS CC Review Course - FinalIvulik87Nessuna valutazione finora
- 1 2 2 PDFDocumento1 pagina1 2 2 PDFmariaNessuna valutazione finora
- Pulmonary Function Tests and Alveolar Ventilation: Introductory Human PhysiologyDocumento3 paginePulmonary Function Tests and Alveolar Ventilation: Introductory Human PhysiologySherida GibbsNessuna valutazione finora
- Draeger-Medical Ventilation GuideDocumento38 pagineDraeger-Medical Ventilation GuideAviya EkutamiNessuna valutazione finora
- Class11 Biology Chapter 17. BREATHING AND EXCHANGE OF GASESDocumento5 pagineClass11 Biology Chapter 17. BREATHING AND EXCHANGE OF GASESrn0828027Nessuna valutazione finora
- Respiratory Monitoring in Mechanical Ventilation: Techniques and ApplicationsDa EverandRespiratory Monitoring in Mechanical Ventilation: Techniques and ApplicationsJian-Xin ZhouNessuna valutazione finora
- Lung Function in Health and Disease Basic Concepts of Respiratory Physiology and PathophysiologyDa EverandLung Function in Health and Disease Basic Concepts of Respiratory Physiology and PathophysiologyNessuna valutazione finora
- Aerosols and the Lung: Clinical and Experimental AspectsDa EverandAerosols and the Lung: Clinical and Experimental AspectsStewart W. ClarkeNessuna valutazione finora
- Monitoring Mechanical Ventilation Using Ventilator WaveformsDa EverandMonitoring Mechanical Ventilation Using Ventilator WaveformsNessuna valutazione finora
- Recommended Reference Materials for Realization of Physicochemical Properties: Pressure–Volume–Temperature RelationshipsDa EverandRecommended Reference Materials for Realization of Physicochemical Properties: Pressure–Volume–Temperature RelationshipsE. F. G. HeringtonNessuna valutazione finora
- Understanding Oscilloscope BasicsDocumento29 pagineUnderstanding Oscilloscope BasicsRidima AhmedNessuna valutazione finora
- ROPE TENSIONER Product-Catalog-2019Documento178 pagineROPE TENSIONER Product-Catalog-2019jeedanNessuna valutazione finora
- Guide to Fair Value Measurement under IFRS 13Documento3 pagineGuide to Fair Value Measurement under IFRS 13Annie JuliaNessuna valutazione finora
- BoQ East Park Apartment Buaran For ContractorDocumento36 pagineBoQ East Park Apartment Buaran For ContractorDhiangga JauharyNessuna valutazione finora
- Ch07 Spread Footings - Geotech Ultimate Limit StatesDocumento49 pagineCh07 Spread Footings - Geotech Ultimate Limit StatesVaibhav SharmaNessuna valutazione finora
- Abinisio GDE HelpDocumento221 pagineAbinisio GDE HelpvenkatesanmuraliNessuna valutazione finora
- Planview Innovation Management Maturity Model PDFDocumento1 paginaPlanview Innovation Management Maturity Model PDFMiguel Alfonso Mercado GarcíaNessuna valutazione finora
- Reinvestment Allowance (RA) : SCH 7ADocumento39 pagineReinvestment Allowance (RA) : SCH 7AchukanchukanchukanNessuna valutazione finora
- Desert Power India 2050Documento231 pagineDesert Power India 2050suraj jhaNessuna valutazione finora
- Domingo V People (Estafa)Documento16 pagineDomingo V People (Estafa)Kim EscosiaNessuna valutazione finora
- Political Reporting:: Political Reporting in Journalism Is A Branch of Journalism, Which SpecificallyDocumento6 paginePolitical Reporting:: Political Reporting in Journalism Is A Branch of Journalism, Which SpecificallyParth MehtaNessuna valutazione finora
- PWC Global Project Management Report SmallDocumento40 paginePWC Global Project Management Report SmallDaniel MoraNessuna valutazione finora
- May, 2013Documento10 pagineMay, 2013Jakob Maier100% (1)
- Tygon S3 E-3603: The Only Choice For Phthalate-Free Flexible TubingDocumento4 pagineTygon S3 E-3603: The Only Choice For Phthalate-Free Flexible TubingAluizioNessuna valutazione finora
- Finance at Iim Kashipur: Group 9Documento8 pagineFinance at Iim Kashipur: Group 9Rajat SinghNessuna valutazione finora
- Measuring Renilla Luciferase Luminescence in Living CellsDocumento5 pagineMeasuring Renilla Luciferase Luminescence in Living CellsMoritz ListNessuna valutazione finora
- Sekolah Menengah Kebangsaan Ss17 JALAN SS17/1, Subang Jaya English Scheme of Work Form 3Documento11 pagineSekolah Menengah Kebangsaan Ss17 JALAN SS17/1, Subang Jaya English Scheme of Work Form 3Rohana YahyaNessuna valutazione finora
- Username: Password:: 4193 Votes 9 Days OldDocumento6 pagineUsername: Password:: 4193 Votes 9 Days OldΘώμηΜπουμπαρηNessuna valutazione finora
- Roadmap For Digitalization in The MMO Industry - For SHARINGDocumento77 pagineRoadmap For Digitalization in The MMO Industry - For SHARINGBjarte Haugland100% (1)
- Clean Agent ComparisonDocumento9 pagineClean Agent ComparisonJohn ANessuna valutazione finora
- Device Interface Device Type (Router, Switch, Host) IP Address Subnet Mask Default GatewayDocumento2 pagineDevice Interface Device Type (Router, Switch, Host) IP Address Subnet Mask Default GatewayRohit Chouhan0% (1)
- Basic Five Creative ArtsDocumento4 pagineBasic Five Creative Artsprincedonkor177Nessuna valutazione finora
- Yanmar America publication listing for engine parts, service, and operation manualsDocumento602 pagineYanmar America publication listing for engine parts, service, and operation manualsEnrique Murgia50% (2)
- New Brunswick CDS - 2020-2021Documento31 pagineNew Brunswick CDS - 2020-2021sonukakandhe007Nessuna valutazione finora
- Covey - Moral CompassingDocumento5 pagineCovey - Moral CompassingAsimNessuna valutazione finora
- Lady Allen On Froebel Training School, Emdrup, CopenhagenDocumento5 pagineLady Allen On Froebel Training School, Emdrup, CopenhagenLifeinthemix_FroebelNessuna valutazione finora
- Florence Walking Tour MapDocumento14 pagineFlorence Walking Tour MapNguyễn Tấn QuangNessuna valutazione finora
- 00 CCSA TestDocumento276 pagine00 CCSA TestPedro CubillaNessuna valutazione finora
- Weekly Choice - Section B - February 16, 2012Documento10 pagineWeekly Choice - Section B - February 16, 2012Baragrey DaveNessuna valutazione finora
- 13 Fashion Studies Textbook XIDocumento158 pagine13 Fashion Studies Textbook XIMeeta GawriNessuna valutazione finora