Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Psychosocial Profile, Mode of Attempt and Psychiatric Co-Morbidity in Attempted Suicide Patients - A Study From South India
Caricato da
IOSRjournalTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Psychosocial Profile, Mode of Attempt and Psychiatric Co-Morbidity in Attempted Suicide Patients - A Study From South India
Caricato da
IOSRjournalCopyright:
Formati disponibili
IOSR Journal Of Humanities And Social Science (IOSR-JHSS)
Volume 20, Issue 5, Ver. V (May. 2015), PP 28-31
e-ISSN: 2279-0837, p-ISSN: 2279-0845.
www.iosrjournals.org
Psychosocial Profile, Mode of Attempt and Psychiatric
Co-Morbidity in Attempted Suicide Patients A
Study From South India
Sujeetha, B., Ph.Da., and Ilangovan, S., M.B.B.S., M.D.(Psy) b
a
Assistant Professor cum Clinical Psychologist, Department of Psychiatry, Thanjavur Medical College, Thanjavur
and b Professor & Head, Department of Psychiatry, Thanjavur Medical College, Thanjavur
I.
Introduction
Suicide is the tragic loss of human life, which is untimely and devastating. Suicidal behaviour is all the
more mystifying because it is a mindful volitional act. It is a lethal act due to a complex interaction of social,
environmental, biological and cultural factors working on an individuals life. The curse of suicidal behaviour
touches many lives and knows few limitations. More than one lakh persons (1,34,599) in India lost their lives by
committing suicide during the year 2010, this indicates an increase of 5.9% over the previous year's figure
(1,27,151). Rate of suicides, i.e., the number of suicides per one lakh population, has been widely accepted as a
standard yardstick. The All India rate of suicides was 11.4 during the year which is marginally higher than 10.9
reported in the year 2009. Sikkim reported the highest rate of suicide (45.9) followed by Puducherry (45.5), A & N
Islands (36.1), Chhattisgarh (26.6) and Kerala (24.6) in 2010 (1). Suicide attempt rates are found to be 1040 times
higher than rates for completed suicides (2). The rates of death show only a northward increase all over the world,
with estimates of one death every 20s by 2020 (3). In Asia, around 5 lakh people die by suicide every year,
representing more than 3/5th of all suicides worldwide (4). Despite such high numbers, suicide has engrossed less
attention in Asia than it has in Western countries. The situation is worse in India, where the last recorded deaths due
to suicide were 134,599 (5) with an annual suicide rate of 11.4. In recent years, suicidal attempts have been
increasingly studied since they pose a high risk of going on to a completed suicide (6). A suicide attempt refers to
engagement in a potentially self-injurious behavior in which there is at least some intent to die (7).
Steady cross-national risk factors include being female, younger, less educated, unmarried and having a
mental disorder (8). The strongest diagnostic risk factors were mood disorders in high-income countries but impulse
control disorders in low and middle income countries (8). One or more diagnosis on Axis 1 was made for 93% of
victims and the most prevalent disorders were depressive disorders and alcohol dependence (9). Human beings are
unique, as are their reasons for suicide. National Crime Records Bureau statistics state that social and economic
causes have led most of the males to commit suicide whereas emotional and personal causes have mainly driven
females to end their lives (1). Methods used for suicidal attempts are mostly non-violent and in the WHO
multicentre Study 64% of males and 80% of females used self poisoning (10). There is difference in the methods
used between countries and this may be related to the differences in the accessibility of certain methods. More than
50% of the suicide attempters made more than one attempt, and nearly 20% of the second attempts were made
within 12 months after the first attempt (2). Socio-demographic risk factors linked with repetition are belonging to
the age group of 25 to 49 years, being divorced, unemployed, and coming from low social class (10). In this above
back ground the present study has been undertaken with the aim to assess the psychosocial profile, mode of attempt
and psychiatric disorders in attempted suicide in a Government Hospital in Tamil Nadu.
II.
Method
One hundred and fifty six patients, referred from a General Hospital, South India served as sample. They
came for the treatment during the month of October to December, 2014 with a history of attempted suicide. The
written informed consent obtained from them. All patients were above 18 years of age and were in clear sensorium
at the time of consent and administration of the study. These patients had been initially admitted to the emergency
ward of the hospital and after undergoing acute medical care for at least 3 days, had been sent to the Department of
Psychiatry. In addition, a detailed case record form also recorded the mode of attempt and causes for the attempt.
They were also diagnosed according to ICD 10.
DOI: 10.9790/0837-20552831
www.iosrjournals.org
28 | Page
Psychosocial Profile, Mode Of Attempt And Psychiatric Co-Morbidity In Attempted Suicide
III.
Results
Most patients were married (52%) and female gender constituted (53%). Majority of them were Hindus
(96%) and hailed from low socioeconomic status (84%). Mostly (89%) had presented with their first attempt. The
frequent method of suicide adopted was the consumption of OPC poison (45%), followed by rat killer (13%) and ant
killer poison (8%). Conflict with family members (42%) were cited as the most frequent reason for the suicidal
attempt. Especially the conflict with spouse (22%), health problems (8%), financial issues (5%), death of dear ones
(3%) and under the influence of alcohol (3%) were the next most frequently cited reasons. There were no dropouts
or patients who refused consent for the study.
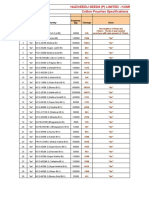
Table 1 Socio-demographic variables of the attempted suicide patients
Gender
Marital Status
Habitat
Religion
Family type
Socio-economic status
Male
Female
Married
Unmarried
Rural
Urban
Hindu
Christian
Muslim
Joint
Nuclear
Low
Middle
No. of cases
73
83
81
74
131
25
149
5
2
107
49
131
25
Percentage
47
53
52
47
84
16
96
03
01
31
69
84
16
Table 2 Clinical variables of the attempted suicide patients
Sl. No
1.
2.
3.
1.
2.
3.
4.
5.
6.
7.
1.
2.
3.
4.
5.
6.
No. of attempts
1
2
More than 3
Mode of attempt
OPC
Rat killer
Ant killer
Hanging
Sedative
Oleander seeds
Cutting throat
Precipitating factors for attempt
Conflict with family members
Conflict with husband/wife
Health problems
Financial issues
Death of loved ones
Under the influence of alcohol
No. of cases
139
14
03
Percentage
89
9
2
70
20
13
12
6
6
4
45
13
8
8
4
4
3
65
35
13
8
4
4
42
22
8
5
3
3
Table 3 Psychiatric co-morbidity of attempted suicide patients
Sl. No
1.
2.
3.
4.
5.
6.
Psychiatric disorder
Adjustment disorder
Impulsive reaction
Alcohol dependence syndrome
Depression
Alcohol abuse
Borderline Personality Disorder
DOI: 10.9790/0837-20552831
No. of cases
58
31
18
16
6
5
www.iosrjournals.org
Percentage
37
20
12
11
4
2
29 | Page
Psychosocial Profile, Mode Of Attempt And Psychiatric Co-Morbidity In Attempted Suicide
IV.
Discussion
Attempted suicides are an entirely preventable cause of death, especially when 1 in 10 attempts goes on to a
completed suicide (3). With increased urbanization leading to increasing isolation, suicides and attempted suicides
are becoming increasingly common. This study observed OPC poisoning to be the most common cause of attempt,
similar to that observed earlier from a different part of the country (11) as well as to the national report on suicides
(1) and to other international studies from neighboring regions (1215). The most common agents used for suicidal
attempt are organophosphates and other household poisons. Studies conducted revealed that the method of suicide is
poisoning (36.6%), hanging (32.1%) and self-immolation (7.9%) were the common methods used to commit suicide
(Accidental Deaths and suicides in India, 2005). Domestic quarrels (48%) and relationship issues (23%) were found
to be the major reasons to attempt suicide in our study which confirms the trend of other studies from India (16).
Financial problems (18%) seemed to notable cause leading to suicide which is similar to the observations made in
few earlier studies (17).
Psychiatric disorder: In our study more than 80% of the suicide attempters had psychiatric disorder and
adjustment disorder (37%) and alcohol dependence (12%) were found to be most common diagnosed disorders. On
the contrary, in other studies it was observed that about 90% were diagnosed with at least one psychiatric disorder.
Co-morbidity of two or more psychiatric disorders was also reported. Family problems and medical illnesses were
the commonly mentioned causes for attempting suicide, which is again similar to earlier reports (3). With such
similarities noted, there remains a high risk of repeat attempts being made (5). Although only 11% of our sample
had presented with repeat attempts, the 1-year incidence of repetition has been estimated at 16% and that of fatal
repetition at 2% (18). Other authors also (19) confirm how previous suicide attempts increase the risk of suicide 30
40 times and are the strongest predictor of further suicidal behavior. The presence of a psychiatric disorder is among
the most consistently reported risk factors for suicidal behavior (20). This study also observed a prevalence of more
than 80% psychiatric co-morbidity in our sample population. In addition, about 12% also had alcohol use disorders.
With regard to personality disorders, borderline and dependent personality was detected in small numbers in contrast
to higher numbers from Western countries. This is supported by several studies (21) which have observed the
greatest risk factors to be mood disorders, other depressive disorders, anxiety disorders, alcohol misuse, drug misuse
and personality disorders.
Other reported risk factors include previous inpatient treatment, unemployment, frequent change of
address, hostility, hopelessness and living alone (22). Yet, one must still keep in mind that these would not explain
the high rates of suicide among farmers or the contribution of domestic violence/child abuse on suicide rates.
However, the differences in both reasons and mode of attempt are similar to what has been observed by the national
report on suicides (4). Therefore, risk factors for suicidal behaviors that have been found in this research include
being of either gender, being married, and having any psychiatric co-morbidity including mood disorders, alcohol
use, personality disorders and chronic medical illness which are often are preceded by stressful events, including
family and romantic conflicts (23). This study has a range of limitations. Firstly, patients were selected from
Government hospital emergency units. Secondly, samples were volunteers. Yet, knowing that patients with
attempted suicides often try to hide the fact due to stigma or fear of the legal consequences (24), it is therefore
believed that any information gathered from this populace could indeed serve as a valuable instrument to plan and
chart public policy.
V.
Conclusion
Thus, it can be concluded that substantial number of attempters had psychiatric disorder. Early diagnosis of
the psychiatric disorders and supportive measures for various stressors would help in prevention of suicidal
attempts. Lack of restriction for procurement of oral agents, easy accessibility and impulsive nature of the attempters
may be the reason for the preference to use these agents for attempting suicide. Taken together these findings, our
results lead us to the conclusion that the variables enhancing the risk of suicide among the vulnerable groups if
identified and the predictive items linked with suicidal risks are enlisted, it would efficiently help in early detection
and prevention of suicide attempts. Thus, many lives could be saved in time. Our findings also revealed that suicide
attempts are treated as a Coping mechanism by attempters under stress to express their needs and distress. Hence,
creating awareness about healthy coping mechanism and stress management is required to reduce such attempts.
Care of patients who present with an attempted suicide should include routine psychiatric and
psychological assessment. This is crucial since such patients generally leave accident and emergency departments
without being comprehensively assessed by a well-qualified health care professional or do not receive a specialist
psychological assessment. In addition, for people with psychiatric disorders such as depression, alcohol dependence
DOI: 10.9790/0837-20552831
www.iosrjournals.org
30 | Page
Psychosocial Profile, Mode Of Attempt And Psychiatric Co-Morbidity In Attempted Suicide
and personality disorders, psycho-education of the family plays a vital role. Repeated visit to a health care
professional either in person or on telephone might help prevent repeat attempts.
References
[1].
[2].
[3].
[4].
[5].
[6].
[7].
[8].
[9].
[10].
[11].
[12].
[13].
[14].
[15].
[16].
[17].
[18].
[19].
[20].
[21].
[22].
[23].
[24].
National crime records Bureau, Accidental deaths and Suicides in India, Ministry of Home Affairs, Govt. of India, 2010.
Schmidtke, A., Bille-Brahe, U. and DeLeo, D. (1996). Attempted suicide in Europe: rates, trends and sociodemographic characteristics of
suicide attempters during the period 19891992. Results of the WHO/EURO Multicentre Study on Parasuicide. Acta Psychiatrica
Scandinavica, 93(5), 327 338.
WHO. The World Health report. shaping the future. Geneva: World Health Organization; 2003.
Vijayakumar, L. (2005). Suicide and mental disorders in Asia. Int Rev Psychiatry, 17, 10914.
Suicidal deaths in India. National Crime Records Bureau 2010. Available at http://www.ncrb.nic.in/ADSI2010/suicides-10.pdf.
Mocicki, E.K. (1997). Identification of suicide risk factors using epidemiologic studies. Psychiatr Clin North Am, 20, 499517.
Silverman, M.M., Berman, A.L, Sanddal, N.D., O'Carroll, P.W. and Joiner, T.E. (2007). Rebuilding the Tower of Babel: a revised
nomenclature for the study of suicide and suicidal behaviors: part 2. Suicide-related ideations, communications, and behaviors. Suicide
Life Threat Behav, 37, 26477.
Matthew, J. (2008). Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. The British Journal of
Psychiatry, 192, 98-105.
Henriksson, M. (1993). Mental disorders & Comorbidity in Suicide. Am J Psychiatry, 150(6), 935-940.
Kerkhof and Arensman. (2000). Attempted suicide and deliberate self-harm: epidemiology and risk factors, 4.15.2, 1039-1044, vol.1,
New Oxford Textbook of Psychiatry. Oxford University Press, New York.
Emma, R. B., Sarah, M., Iris, W., Brandon, Z., Stephen, A., Stansfeld, D. E., Stewart, E. D., Caine and Yeates, C. (2008). Psychosocial
and clinical correlates of suicidal acts: results from a national population survey. The British Journal of Psychiatry, 192, 279-284.
Nilamadhab, K. (2010). Profile of risk factors associated with suicide attempts: A Study from Orissa, India. Indian Journal of Psychiatry,
52(1), 48-56.
Partha, P.D., Sandeep, G., Ajit, A., Subho, C., Savita, M. and Suresh, K. (2008). Intentional self-harm seen in psychiatric referrals in
tertiary care hospital. Indian Journal of Psychiatry, 50(3), 187-191
Annette, L. B. (2000). Methods of youth suicide in New Zealand: trends and implications for prevention. Australian and New Z ealand.
Journal of Psychiatry, 34(3), 413419.
Ping, Q., Esben, A., Preben, B. and Mortensen. (2003). Suicide Risk in Relation to Socioeconomic, Demographic, Psychiatric, and
Familial Factors: A National RegisterBased Study of All Suicides in Denmark, 19811997. Am J Psychiatry, 160, 765-772.
Ponnudurai, R., Jey, A. and Saraswathy. M. (1986). Attempted suicide in Madras. Indian Journal of Psychiatry, 28(1), 59-62.
Srivastava, M.K., Sahoo, R.N., Ghotekar, L.H., Srihari, D., Danabalan, M., Dutta, T.K. and Das, A.K. (2004). Risk factors associated
with Attempted Suicide: A case control study. Indian Journal of Psychiatry, 46(1), 33-38.
Takeshi, S., Masashi, T. and Tomihide, H. (1993). Suicide attempts by agriculture chemicals. Indian Journal of Psychiatry, 35 (4), 209210.
Anuradha, B., Sejbaek, C.S., Suganthy, P., Venkata, R., Alex, R., Jayaprakash, M. and Konradsen, F. (2009). Self-harm and selfpoisoning in southern India: choice of poisoning agents and treatment. Tropical Medicine and International Health, 14(7), 761 765.
Krysinska, K. and Lester, D. (2010). Post-traumatic stress disorder and suicide risk: a systematic review. Arch Suicide Res, 4, 123.
Scoliers, G., Portzky, G., Heeringen, K. and Audenaert, K. (2009). Sociodemographic and psychopathological risk factors for repetition
of attempted suicide: a 5-year follow-up study. Arch Suicide Res, 13, 20113.
Nordentoft, M. (2007). Prevention of suicide and attempted suicide in Denmark. Epidemiological studies of suicide and intervention
studies in selected risk groups. Dan Med Bull, 54, 30669.
Nock, M.K., Borges, G., Bromet, E.J., Cha, C.B., Kessler, R.C. and Lee, S. (2008). Suicide and suicidal behavior. Epidemiol R ev, 30(1),
13354.
Saddichha, S., Prasad, M.N.V. and Saxena, M.K. (2010). Attempted suicides in India: a comprehensive look. Arch Suicide Res, 14(1),
5665.
DOI: 10.9790/0837-20552831
www.iosrjournals.org
31 | Page
Potrebbero piacerti anche
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Surat Textile MillsDocumento3 pagineSurat Textile MillsShyam J VyasNessuna valutazione finora
- Safe Britannia PDFDocumento2 pagineSafe Britannia PDFeden4872Nessuna valutazione finora
- Masmud Vs NLRC and Atty Go DigestDocumento2 pagineMasmud Vs NLRC and Atty Go DigestMichael Parreño Villagracia100% (1)
- "I Am Not Gay Says A Gay Christian." A Qualitative Study On Beliefs and Prejudices of Christians Towards Homosexuality in ZimbabweDocumento5 pagine"I Am Not Gay Says A Gay Christian." A Qualitative Study On Beliefs and Prejudices of Christians Towards Homosexuality in ZimbabweInternational Organization of Scientific Research (IOSR)Nessuna valutazione finora
- Socio-Ethical Impact of Turkish Dramas On Educated Females of Gujranwala-PakistanDocumento7 pagineSocio-Ethical Impact of Turkish Dramas On Educated Females of Gujranwala-PakistanInternational Organization of Scientific Research (IOSR)Nessuna valutazione finora
- Attitude and Perceptions of University Students in Zimbabwe Towards HomosexualityDocumento5 pagineAttitude and Perceptions of University Students in Zimbabwe Towards HomosexualityInternational Organization of Scientific Research (IOSR)Nessuna valutazione finora
- A Proposed Framework On Working With Parents of Children With Special Needs in SingaporeDocumento7 pagineA Proposed Framework On Working With Parents of Children With Special Needs in SingaporeInternational Organization of Scientific Research (IOSR)Nessuna valutazione finora
- A Review of Rural Local Government System in Zimbabwe From 1980 To 2014Documento15 pagineA Review of Rural Local Government System in Zimbabwe From 1980 To 2014International Organization of Scientific Research (IOSR)Nessuna valutazione finora
- The Role of Extrovert and Introvert Personality in Second Language AcquisitionDocumento6 pagineThe Role of Extrovert and Introvert Personality in Second Language AcquisitionInternational Organization of Scientific Research (IOSR)Nessuna valutazione finora
- The Impact of Technologies On Society: A ReviewDocumento5 pagineThe Impact of Technologies On Society: A ReviewInternational Organization of Scientific Research (IOSR)100% (1)
- An Evaluation of Lowell's Poem "The Quaker Graveyard in Nantucket" As A Pastoral ElegyDocumento14 pagineAn Evaluation of Lowell's Poem "The Quaker Graveyard in Nantucket" As A Pastoral ElegyInternational Organization of Scientific Research (IOSR)Nessuna valutazione finora
- Assessment of The Implementation of Federal Character in Nigeria.Documento5 pagineAssessment of The Implementation of Federal Character in Nigeria.International Organization of Scientific Research (IOSR)Nessuna valutazione finora
- Comparative Visual Analysis of Symbolic and Illegible Indus Valley Script With Other LanguagesDocumento7 pagineComparative Visual Analysis of Symbolic and Illegible Indus Valley Script With Other LanguagesInternational Organization of Scientific Research (IOSR)Nessuna valutazione finora
- Edward Albee and His Mother Characters: An Analysis of Selected PlaysDocumento5 pagineEdward Albee and His Mother Characters: An Analysis of Selected PlaysInternational Organization of Scientific Research (IOSR)Nessuna valutazione finora
- Investigation of Unbelief and Faith in The Islam According To The Statement, Mr. Ahmed MoftizadehDocumento4 pagineInvestigation of Unbelief and Faith in The Islam According To The Statement, Mr. Ahmed MoftizadehInternational Organization of Scientific Research (IOSR)Nessuna valutazione finora
- Relationship Between Social Support and Self-Esteem of Adolescent GirlsDocumento5 pagineRelationship Between Social Support and Self-Esteem of Adolescent GirlsInternational Organization of Scientific Research (IOSR)Nessuna valutazione finora
- Importance of Mass Media in Communicating Health Messages: An AnalysisDocumento6 pagineImportance of Mass Media in Communicating Health Messages: An AnalysisInternational Organization of Scientific Research (IOSR)Nessuna valutazione finora
- Role of Madarsa Education in Empowerment of Muslims in IndiaDocumento6 pagineRole of Madarsa Education in Empowerment of Muslims in IndiaInternational Organization of Scientific Research (IOSR)Nessuna valutazione finora
- Topic: Using Wiki To Improve Students' Academic Writing in English Collaboratively: A Case Study On Undergraduate Students in BangladeshDocumento7 pagineTopic: Using Wiki To Improve Students' Academic Writing in English Collaboratively: A Case Study On Undergraduate Students in BangladeshInternational Organization of Scientific Research (IOSR)Nessuna valutazione finora
- Designing of Indo-Western Garments Influenced From Different Indian Classical Dance CostumesDocumento5 pagineDesigning of Indo-Western Garments Influenced From Different Indian Classical Dance CostumesIOSRjournalNessuna valutazione finora
- Cotton Pouches SpecificationsDocumento2 pagineCotton Pouches SpecificationspunnareddytNessuna valutazione finora
- Seven Seas of CommunicationDocumento2 pagineSeven Seas of Communicationraaaj500501Nessuna valutazione finora
- 03-Volume II-A The MIPS64 Instruction Set (MD00087)Documento793 pagine03-Volume II-A The MIPS64 Instruction Set (MD00087)miguel gonzalezNessuna valutazione finora
- HUAWEI P8 Lite - Software Upgrade GuidelineDocumento8 pagineHUAWEI P8 Lite - Software Upgrade GuidelineSedin HasanbasicNessuna valutazione finora
- FACT SHEET KidZaniaDocumento4 pagineFACT SHEET KidZaniaKiara MpNessuna valutazione finora
- Sugar Industries of PakistanDocumento19 pagineSugar Industries of Pakistanhelperforeu50% (2)
- Grade 10 Science - 2Documento5 pagineGrade 10 Science - 2Nenia Claire Mondarte CruzNessuna valutazione finora
- IKEA AyeshaDocumento41 pagineIKEA AyeshaAYESHAREHMAN100Nessuna valutazione finora
- Vocabulary Words - 20.11Documento2 pagineVocabulary Words - 20.11ravindra kumar AhirwarNessuna valutazione finora
- Referensi PUR - Urethane Surface coating-BlockedISO (Baxenden) - 20160802 PDFDocumento6 pagineReferensi PUR - Urethane Surface coating-BlockedISO (Baxenden) - 20160802 PDFFahmi Januar AnugrahNessuna valutazione finora
- DODGER: Book Club GuideDocumento2 pagineDODGER: Book Club GuideEpicReadsNessuna valutazione finora
- ViTrox 20230728 HLIBDocumento4 pagineViTrox 20230728 HLIBkim heeNessuna valutazione finora
- Maratua Island Survey ReportDocumento8 pagineMaratua Island Survey ReportJoko TrisyantoNessuna valutazione finora
- IN THE BEGINNING WAS AFFECT RolnikDocumento22 pagineIN THE BEGINNING WAS AFFECT RolnikFabiana PaulinoNessuna valutazione finora
- Sycip v. CA (Sufficient Funds With The Drawee Bank)Documento15 pagineSycip v. CA (Sufficient Funds With The Drawee Bank)Arnold BagalanteNessuna valutazione finora
- WIKADocumento10 pagineWIKAPatnubay B TiamsonNessuna valutazione finora
- Peer-to-Peer Lending Using BlockchainDocumento22 paginePeer-to-Peer Lending Using BlockchainLuis QuevedoNessuna valutazione finora
- Knowledge, Attitude and Practice of Non-Allied Health Sciences Students of Southwestern University Phinma During The Covid-19 PandemicDocumento81 pagineKnowledge, Attitude and Practice of Non-Allied Health Sciences Students of Southwestern University Phinma During The Covid-19 Pandemicgeorgemayhew1030Nessuna valutazione finora
- Modul9 VPNDocumento34 pagineModul9 VPNDadang AbdurochmanNessuna valutazione finora
- 2-Emotional Abuse, Bullying and Forgiveness Among AdolescentsDocumento17 pagine2-Emotional Abuse, Bullying and Forgiveness Among AdolescentsClinical and Counselling Psychology ReviewNessuna valutazione finora
- EEN 203 Slide Notes Year 2018: PART I - Numbers and CodesDocumento78 pagineEEN 203 Slide Notes Year 2018: PART I - Numbers and CodesSHIVAM CHOPRANessuna valutazione finora
- Determination of Physicochemical Pollutants in Wastewater and Some Food Crops Grown Along Kakuri Brewery Wastewater Channels, Kaduna State, NigeriaDocumento5 pagineDetermination of Physicochemical Pollutants in Wastewater and Some Food Crops Grown Along Kakuri Brewery Wastewater Channels, Kaduna State, NigeriamiguelNessuna valutazione finora
- TG - Health 3 - Q3Documento29 pagineTG - Health 3 - Q3LouieNessuna valutazione finora
- GMAT Sentence Correction Practice Test 03Documento5 pagineGMAT Sentence Correction Practice Test 03krishnachivukulaNessuna valutazione finora
- Dry Wall, Ceiling, and Painting WorksDocumento29 pagineDry Wall, Ceiling, and Painting WorksFrance Ivan Ais100% (1)
- Did Angels Have WingsDocumento14 pagineDid Angels Have WingsArnaldo Esteves HofileñaNessuna valutazione finora
- Thick Teak PVT LTD Aoa and MoaDocumento17 pagineThick Teak PVT LTD Aoa and MoaVj EnthiranNessuna valutazione finora