Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Early Gastric Cancer
Caricato da
Sarah SilaenCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Early Gastric Cancer
Caricato da
Sarah SilaenCopyright:
Formati disponibili
Early Gastric Cancer
KATHARINE J. CARTER, M.D., HUGH A. SCHAFFER, M.D., WALLACE P. RITCHIE, JR., M.D., PH.D.
Although common in Japan, early gastric cancer (EGC = gastric
adenocarcinoma confined to the mucosa and submucosa of the
stomach, with or without regional lymph node metastases) is
thought to be an infrequent occurrence in the United States.
However, a review of all "curative" resections for carcinoma of
the gastric body and antrum at the University of Virginia between
1974 and 1982 revealed EGC in five of 31 patients (16%). The
purpose of the present study was to compare EGC to more
advanced gastric cancer (ADV; n = 26) to determine whether
any presenting historical, laboratory, x-ray, or endoscopic features distinguished the two groups before surgery and to ascertain
whether postoperative survival in the United States mimicked
the Japanese experience. All surviving patients were contacted,
all charts were abstracted, all pathologic specimens were reexamined, and all radiographs were reviewed blindly by an experienced radiologist. Statistical evaluation was accomplished
using Kaplan-Meier plots, chi square analysis, and unpaired "t"
tests, as appropriate. At presentation, patients with EGC were
younger (44 6 vs. 67 2 years, p < 0.01) with higher admission
albumin levels (4.1 0.2 vs. 3.7 0.1 mgm/dl, p < 0.01).
Although not significantly different, admission hemoglobin
tended to be higher (41 2 vs. 35 2%), the incidence of
weight loss tended to be less (40 vs. 65%), duration of symptoms
tended to be longer (21 11 vs. 8 3 months), and tumor
diameter tended to be smaller (1.7 0.6 vs. 5.8 0.7 cm) in
EGC. No differences were apparent with respect to endoscopic
or radiographic appearance, tumor location (>70% antrum),
presence of regional lymph node metastases (EGC = 2/5;
ADV = 20/26), or type of resection (subtotal gastrectomy in
4/5 EGC, in 19/26 ADV). On median 5-year follow-up, however,
survival with EGC has been 100%. In contrast, the KaplanMeier estimate of 5-year survival in ADV is 15% (42% with
muscularis invasion, 0% with serosal invasion, 12% with extragastric spread; p < 0.01 vs. EGC). One suture line recurrence
in EGC was successfully treated by re-resection. No ADV patient
with recurrence survives (p < 0.01). Thus, EGC behaves similarly
in the United States and Japan; for example, prognosis is excellent even in the presence of lymph node metastases. Inability
to distinguish EGC from ADV before surgery justifies an aggressive surgical approach to all patients with resectable gastric
neoplasms.
Presented at the Ninety-Fifth Annual Meeting of the Southern Surgical
Association, December 5-7, 1983, Hot Springs, Virginia.
Reprint requests: Wallace P. Ritchie, Jr., M.D., Ph.D., Professor and
Chairman, Temple University Hospital, Health Sciences Center, Philadelphia, PA 19140.
Submitted for publication: January 9, 1984.
604
From the Departments of Surgery and Radiology, University
of Virginia School of Medicine, Charlottesville, Virginia
EARLY GASTRIC CANCER (EGC) is defined as adenocarcinoma confined to the mucosa or submucosa of
the stomach with or without regional lymph nodes metastases. 2 Although common in Japan, EGC is thought
to be rare in the United States where the prognosis for
gastric cancer is considered to be poor. However, a review
of all cases of "curative" resections for gastric adenocarcinoma performed at the University of Virginia between
1974 and 1982 demonstrated a 16% incidence of EGC.
The purpose of the present study was to review these
cases in order to determine if any presenting historical,
laboratory, x-ray, or endoscopic features distinguished
patients with EGC from those with more advanced disease
and to ascertain whether or not postoperative survival in
the United States mimicked the Japanese experience.
Methods
All cases of gastric adenocarcinoma resected for "cure"
(all gross tumor removed, no distant metastases noted)
between 1974 and 1982 at the University of Virginia were
reviewed. Adenocarcinoma of gastroesophageal junction
with extension into the esophagus was excluded as no
instance of EGC in this tumor location was found. Thirtyone patients met the inclusion criteria. Of these, five demonstrated EGC histologically; the remainder were designated as advanced gastric cancer (ADV). All charts were
abstracted to ascertain the type and duration of symptoms,
history of weight loss, admission hemogram, liver function
tests, electrolyte levels, endoscopic appearance, type of
gastric resection, and recurrence and survival rates. Endoscopic reports were available in four of five patients
with EGC and in 23 of 26 patients with ADV. In addition,
all pathologic specimens wre reviewed by a senior experienced pathologist to determine depth of gastric wall
invasion, tumor location, tumor diameter, and presence
or absence of regional lymph node metastases.
Further, all available radiographs were reviewed by a
senior experienced gastrointestinal radiologist unaware of
VOL. 199.- NO. 5
EARLY GASTRIC CANCER
the purpose of the study or of the clinical histories of the
individual patients. He was asked to categorize the appearance of any lesions detected on the upper gastrointestinal series as either benign, malignant, or indeterminate. Lesions were also classified as ulcerative, polypoid,
or infiltrating. Upper gastrointestinal series were available
for review in four of five EGC patients and in 25 of 26
ADV patients.
Results are reported as mean standard error. Statistical evaluation was accomplished using unpaired "t" tests,
chi square analysis, and Kaplan-Meier plots, as appropriate.
Results
Length of Follow-up
Median length of follow-up in EGC is 62 months,
ranging from 24 to 100 months after surgery. Median
length of follow-up on all surviving patients with ADV
has been 68 months, ranging from 39 to 96 months.
Age and Sex Ratios
At presentation, patients with EGC were, on average,
23 years younger than those with ADV: 44 6 years
(range 26-61 years) vs. 67 2 years (range 37-83 years),
a difference which was statistically significant (p < 0.01).
Male:female ratios were 1:1.5 in patients with EGC vs.
2.5:1 for those with ADV.
Symptoms
Mean duration of symptoms tended to be longer in
the EGC patients (21 11 months) vs. patients with
ADV (8 3 months) (Table 1). The incidence and amount
of weight lost and the incidence of hematemesis were
greater in the ADV group than in the EGC group, whereas
a principal complaint of epigastric pain was more common in EGC than in ADV. None of these differences
were significant, however.
Admission Laboratory Assessment
There were no significant differences between EGC
and ADV for virtually all of the admission laboratory
data, although admission hematocrits tended to be higher
in the EGC group (41 2% vs. 35 2%). The only
significantly different parameter was the admission albumin level that was substantially higher in patients with
EGC (4.1 0.2 vs. 3.7 0.1 mg/dl; p < 0.01).
Preoperative Evaluation
The preoperative diagnosis of carcinoma was established either endoscopically or radiographically in 80%
605
TABLE 1. Symptoms at Presentation
Epigastric pain
Nausea
Anorexia
Fatigue
Hematemesis
Weight loss
Duration
EGC
ADV
"p" Value
4/5
1/5
0
0
0
2/5
21 11 Months
8/26
10/26
5/26
5/26
3/26
16/26
8 3 Months
NS
NS
NS
NS
NS
NS
NS
of the EGC group and in 77% of the advanced group.
Routine upper gastrointestinal series were uniformly insensitive, however, even when interpreted by a senior
experienced gastrointestinal radiologist. None of the radiographs in the EGC group were regarded as malignant:
two of the four available for review were read as benign,
the remainder as indeterminate. Even in the advanced
group, only 60% of patients were felt to have an upper
gastrointestinal series indicative of gastric adenocarcinoma; 12% were read as benign and 28% as indeterminate.
Lesions were said to be infiltrating in the majority of
instances in the ADV group (Table 2).
Endoscopy proved more sensitive in the diagnosis of
gastric adenocarcinoma, but only when combined with
biopsy. The endoscopist's impression in the EGC group
was that two had benign disease, one was clearly malignant, and one was indeterminate. In patients with ADV,
five of 23 were felt to be benign, 13 of 23 malignant, and
six of 23 were considered indeterminate. Tissue obtained
at endoscopy was positive for carcinoma in all four of
the EGC group in whom biopsies were performed. However, biopsies were positive for carcinoma in only 15 of
23 ADV patients. Thus, no radiographic or endoscopic
criteria reliably distinguished EGC from ADV.
Operative Approach
Subtotal gastrectomy was performed in four of five
patients in the EGC group and in 19 of 26 in the ADV
group. Total gastrectomy was performed in the remainder.
There was no operative mortality in the EGC group. Three
patients died in the ADV group within 30 days of operation, one from an arrythmia and two from sepsis.
These differences were not statistically significant.
TABLE 2. Radiologic Evaluation
Benign
Indeterminate
Malignant
Ulcerative
Polypoid
Infiltrating
EGC
ADV
"p" Value
2/4
2/4
0/4
3/4
1/4
0/4
3/25
7/25
15/25
NS
NS
NS
NS
NS
NS
5/25
1/25
9/25
606
CARTER, SCHAFFER, AND RITCHIE
Ann.
Surg. * May 1984
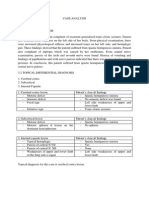
FIG. 1. Photomicrograph of early
gastric cancer confined to the mucosa (X250).
Tumor Location and Size
More than 70% of both EGC and ADV tumors were
antral in location. The EGC group had a predominance
of lesser curvature lesions, whereas ADV cancers were
evenly distributed between the lesser and greater curvature. EGC tumors tended to be smaller (1.7 0.6 vs. 5.8
0.7 cm in greatest diameter) although the difference
was not significant. Three patients among the ADV group
had microscopic evidence of tumor at the margin of resection; all developed recurrence by 4 months.
Histology
All tumors were adenocarcinomas. An example of EGC
is shown in Figure 1, demonstrating foci of adenocarcinoma in areas of atrophic gastritis. Three patients with
EGC had tumor confined to the mucosa while, in two,
tumor extended into the submucosa. In the ADV group,
TABLE 3. Correlation of Positive Regional Lymph Nodes
with Depth of Gastric Wall Invasion
EGC
Invasion
Mucosa
Submucosa
Muscularis propria
Serosa
Perigastric tissues
ADV
Number
of
%(+)
Nodes
3
2
33%
50%
%(+)
Number
of
Nodes
8
6
12
38%
83%
100%
tumor extension to the muscularis propria was noted in
eight, to the serosa in six, and into the perigastric tissue
in 12.
Lymph Node Metastases
Metastases to regional lymph nodes were found in two
of five patients with EGC and in 20 of 26 ADV, a difference which was not significant statistically. Positive
nodes were found at all levels of tumor invasion, although
the percentage of patients harboring lymph node metastases increased with increasing depth of invasion (Table 3).
Adjuvant Therapy
Thirty-eight per cent of the ADV group received postoperative chemotherapy and 15% received radiation therapy. In general, these treatments were begun after tumor
recurrence and did not appear to improve survival. One
patient in the EGC group received a partial course of
chemotherapy; none received radiation therapy.
Recurrence
Twenty of 26 ADV patients (73%) developed either
local or systemic recurrence of disease at a mean interval
of 17 6 months after surgery. In contrast, only one
patient in the EGC group developed recurrence
(p < 0.01). This proved to be a suture line recurrence,
found 2 years following the initial operation. The patient
Vol. 199 * No. 5
was
successfully treated by subsequent near-total
1.0
gas-
trectomy and is alive without detectable disease 3 years
following this procedure. In contrast, no patient who de-
in ADV is alive (p < 0.01 vs. EGC),
mean survival in this group being 5 9 months following
detection of recurrent tumor.
veloped
607
EARLY GASTRIC CANCER
0.9 _
A
E
recurrence
Advanced gastric cancer (n=26)
Early gastric cancer (n=5)
-J
-j
0.8 _
cc
Survival
Median 5-year survival in the patient with EGC is
100% (Fig. 2). In contrast, the Kaplan-Meier estimate of
5-year survival in the ADV group is only 15% (p < 0.01).
Estimated survival is clearly influenced by the depth of
gastric wall invasion by tumor: 42% 5-year survival for
tumor confined to the muscularis propria, 0% for tumor
extending into the serosa, and 12% with tumor invasion
of the perigastric tissue (Fig. 3).
n
C/)
0
w
0.6 _
0.5 _
cc
0.4 _
U.
Discussion
In 1962, the Japanese Gastroenterologic Endoscopy
Society adopted the term "early gastric cancer" to signify
the Society's belief that, when detected early, gastric adenocarcinoma could be cured.3 This belief was based on
the survival statistics of the Japanese surgeon, Saeki, who
demonstrated in 1938 that a subset of patients with gastric
adenocarcinoma, those with tumor confined to the mucosa or submucosa, had a 91% 5-year survival, irrespective
of the presence or absence of regional lymph node metastases. It is now clear that EGC is a distinctive malignancy, at least in terms of prognosis, and that it is identifiable in areas outside of Japan: the superficial spreading
carcinomas of Stout4 and Friesen5 in the United States
and the superficial carcinomas and surface gastric cancers
reported from Britain',' are pathologically identical
to EGC.
The relative proportion of EGC to all diagnosed gastric
adenocarcinomas is a function of the diligence with which
the diagnosis is sought. In Japan, the advent of mass
screening examinations has resulted in an increase in
incidence of EGC among resected gastric carcinomas from
16% in 1960 to 63% in 1974.8 The 16% incidence of EGC
in the present series is comparable to the incidence reported by Machado from England,6 Miller from Western
Europe,9 and Paulino from South America.'0 It is also
comparable to the 13% incidence of EGC found by Green
in 213 gastric resections for adenocarcinoma at Columbia
University. "
In the United States, the prognosis for gastric adenocarcinoma is regarded as being uniformly grim. This belief
has lead some to adopt a posture of "therapeutic nihilism"
with respect to the disease, while others feel bound to
employ exhaustive (and costly) preoperative testing in
order to identify "suitable" candidates for surgery. The
present study suggests that both approaches are inappropriate. In the first instance, no distinctive historical, lab-
0.7
LL
6i
Q-
0.3 _
0.2 _
A
0.1
II
4
1-
TIME IN YEARS
FIG. 2. Survival of early gastric cancer versus advanced gastric
patients.
Mucosa'(n=3)
09
2
3
\3
5
-j0.
>
08
4
5
cc
(n=2)
Submrcosa
Muscularis proprie (n=8)
Penr-gastric tissues (n=12)
=Serosa (n=6)
0.7
c/)
Z 0.6
4
0.5
)
w3
ax:
0.4
0.3
<~~~~
a.
<
cancer
1,2
1.0
C:
0.2
TIME IN YEARS
FIG. 3. Survival by depth of gastric invasion.
608
Ann. Surg. May 1984
CARTER, SCHAFFER, AND RITCHIE
oratory, radiographic, or endoscopic features reliably distinguished the patients with early gastric cancer from those
with more advanced disease. At presentation, only two
significant differences were identified between these
groups: age and admission albumin levels. Neither is specific. Furthermore, larger series report very similar age
distribution between EGC and ADV; Johansen'2 noted
a mean of 66 years in a series of 70 patients with EGC
while Miller,' in a review of 658 patients with EGC, found
the disease most common in the sixth and seventh decades
of life. In addition, symptoms of patients with EGC are
vague, often consisting only of epigastric fullness or indigestion. The present study is in agreement with other
reports that indicate that epigastric pain is, indeed, the
most common presenting symptom in EGC, whereas significant weight loss, hematemesis, or melena suggest (but
do not prove) the presence of more advanced carcinoma. 11,13
The diagnosis ofgastric adenocarcinoma is most readily
made by endoscopy when seven to ten biopsies are routinely obtained.'4 However, endoscopic biopsies cannot
distinguish early from more advanced gastric cancer.
Routine upper gastrointestinal series, at least as performed
in the United States, is also relatively insensitive, although
the air-contrast techniques used in the mass screening
examinations in Japan are reportedly more accurate.'5
In the present series, neither the location, the appearance, nor the size of the lesions reliably distinguish EGC
from ADV.
Adequate surgical resection is the mainstay of therapy,
with subtotal gastrectomy the treatment of choice for
EGC of the antrum and total gastrectomy reserved for
lesions high in the fundus or for patients with recurrent
disease.'3 Adjuvant chemotherapy or radiation therapy
do not appear to improve survival of patients with EGC,
even in those with nodal metastases.'6 Therefore, neither
modality can be recommended. Recurrence rates of 3%
have been noted by others in EGC with a mean diseasefree interval of 3 years.'6"7 Higher local recurrence rates
(9%) have been reported for patients in whom the diagnosis of adenocarcinoma was not suspected before surgery.'8 As a rule, recurrence tends to be local and can be
treated successfully by repeat resection.
That "therapeutic nihilism" is also inappropriate is
suggested by the superb survival statistics noted in the
present (admittedly small) series, as well as those reported
from Japan by Kishimoto (97% 5-year survival for intramucosal cancers, 96% for submucosal cancers).'9 In
Western European Countries and in the United States,
survival rates in EGC are somewhat lower: 87% in Germany,20 71% in Britain,'8 and 68% in New York." Unlike
other solid tumors of the gastrointestinal tract, depth of
gastric wall invasion and not metastases to regional nodes
appears to be the primary determinate of prognosis in
both EGC and ADV.
In summary, early gastric cancer behaves similarly in
the United States and Japan; for example, prognosis is
excellent even in the presence of regional lymph node
metastases. Inability to distinguish early from advanced
gastnc cancer before surgery justifies an aggressive surgical
approach to patients with resectable gastric neoplasms.
Acknowledgment
The authors gratefully acknowledge the technical assistance of Ms.
Catherine Norman.
References
1. Qizilbash AH, Stevenson GW. Early gastric cancer. Pathol Annu
1979; 1:317-351.
2. Johansen AA. Early gastric cancer. In Morson BC, ed. Pathology
of the Gastrointestinal Tract. Current Topics in Pathology. New
York: Springer-Verlag, 1976; 1-47.
3. Murakami T. Pathomorphological diagnosis. Definition and gross
classification. In Murakami T, ed. Early Gastric Cancer. Gann
Monograph 11. Tokyo: University of Tokyo Press, 1971; 53-55.
4. Stout AP. Superficial spreading type of carcinoma of the stomach.
Arch Surg 1942; 44:651-657.
5. Friesen G, Dogherty MB, Remine WH. Superficial carcinoma of
the stomach. Surgery 1961; 51:300-312.
6. Machado G, Davis JD, Tudway A, et al. Superficial carcinoma of
the stomach. Br Med J 1976; 2:77-79.
7. Mason M. Surface carcinoma of the stomach. Gut 1965; 6:185-
193.
8. Yamagata S, Hisamichi S. Epidemiology of cancer of the stomach.
World J Surg 1979; 3:663-669.
9. Miller G, Kaufman M. Das magenfruhkarzinon in Europa. Dtsch
Med Wochenschr 1975; 100:1946-1949.
10. Paulino F, Roselli A. Early gastric cancer: report of twenty-five
cases. Surgery 1979; 85:172-176.
11. Green PH, O'Toole KM, Weinberg LM, Goldfarb JP. Early gastric
cancer. Gastroenterology 1981; 81:247-256.
12. Johansen AA. Early gastric cancer: a contribution to the pathology
and to gastric cancer histogenesis. Copenhagen: Poul Petri 1981;
123.
13. Murakami T. Early cancer of the stomach. World J Surg 1979;
3:685-692.
14. Graham D, Schwartz J, Cain G, Gyorky F. Prospective evaluation
of biopsy number in the diagnosis of esophageal and gastric
carcinoma. Gastroenterology 1982; 82:228-231.
15. Maruyama M. Diagnostic limits for early gastric cancer by radiography. In Murakami T, ed. Early Gastric Cancer. Gann Monograph 11. Tokyo: University of Tokyo Press, 1971.
16. Lwanga T, Furukawa H, Kosaki G. Relapse of early gastric cancer
and its prevention. J Clin Surg (Rinsho Geka) 1979; 31:29.
17. Yamada E. Surgical results for early gastric carcinoma. Int Surg
1975; 60:139-142.
18. Fielding J, Ellis D, Jones B. Natural history of "early" gastric cancer:
results of a 10 year regional survey. Br Med J 1980; 281:965967.
19. Kishimoto H, Fukii T, Adachi H, Koga N. Resection line and longterm results in early cancer of the stomach. J Clin Surg (Rinsho
Geka) 1976; 31:541-545.
20. Gentsch HH, Groitl H, Giedl J. Results of surgical treatment of
early gastric cancer in 113 patients. World J Surg 1981; 5:103107.
Potrebbero piacerti anche
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Cover Pedoman Penilaian Kinerja Puskesmas PDFDocumento5 pagineCover Pedoman Penilaian Kinerja Puskesmas PDFmarley4321Nessuna valutazione finora
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Chapter IIDocumento9 pagineChapter IISarah SilaenNessuna valutazione finora
- Layout Dermatitis AtopiDocumento2 pagineLayout Dermatitis AtopiSarah SilaenNessuna valutazione finora
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Layout Psoriasis VulgarisDocumento2 pagineLayout Psoriasis VulgarisSarah SilaenNessuna valutazione finora
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Acute Diarrhea EryfhhefnfdsDocumento49 pagineAcute Diarrhea EryfhhefnfdskikilutNessuna valutazione finora
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Follow UpDocumento6 pagineFollow UpSarah SilaenNessuna valutazione finora
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- Cover CA TiroidDocumento1 paginaCover CA TiroidSarah SilaenNessuna valutazione finora
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Case ReportDocumento11 pagineCase ReportSarah SilaenNessuna valutazione finora
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Case AnalysisDocumento2 pagineCase AnalysisSarah SilaenNessuna valutazione finora
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Selamat Datang: 1St Palembang Neurology Update 2014Documento4 pagineSelamat Datang: 1St Palembang Neurology Update 2014Sarah SilaenNessuna valutazione finora
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Laporan: Tutorial 3 Blok 4Documento36 pagineLaporan: Tutorial 3 Blok 4Sarah SilaenNessuna valutazione finora
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Skenario 1 Blok 4Documento23 pagineSkenario 1 Blok 4Sarah SilaenNessuna valutazione finora
- Placenta PreviaDocumento5 paginePlacenta PreviaSarah SilaenNessuna valutazione finora
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- Mechanisms of Trauma During Breech Delivery.20Documento7 pagineMechanisms of Trauma During Breech Delivery.20Sarah SilaenNessuna valutazione finora
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Singleton Term Breech Deliveries in Nulliparous and Multiparous Women: A 5-Year Experience at The University of Miami/Jackson Memorial HospitalDocumento6 pagineSingleton Term Breech Deliveries in Nulliparous and Multiparous Women: A 5-Year Experience at The University of Miami/Jackson Memorial HospitalSarah SilaenNessuna valutazione finora
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Effects of Citicoline On Phospholipid and Glutathione Levels in Transient Cerebral IschemiaDocumento6 pagineEffects of Citicoline On Phospholipid and Glutathione Levels in Transient Cerebral IschemiaMuhammad Ilham FarizNessuna valutazione finora
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- Patient DatasheetDocumento28 paginePatient DatasheetMohit RajNessuna valutazione finora
- Pediatric DisordersDocumento182 paginePediatric DisordersErnesto Trinidad Jr RN83% (6)
- Cardiac Catheterization and MonitoringDocumento40 pagineCardiac Catheterization and MonitoringMarissa Asim100% (1)
- Photochemical & Photobiological SciencesDocumento13 paginePhotochemical & Photobiological SciencesNazliah SyarbinNessuna valutazione finora
- 207Documento5 pagine207Satria 'arceus' DewantaraNessuna valutazione finora
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- IRBD Scales Abnormal Involuntary Movement ScaleDocumento2 pagineIRBD Scales Abnormal Involuntary Movement ScaleRoberto LlanesNessuna valutazione finora
- The Case of Dora and Her DreamsDocumento5 pagineThe Case of Dora and Her DreamsHardik Motsara100% (1)
- Nursing As A ProfessionDocumento35 pagineNursing As A ProfessionAparna Aby75% (8)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Buset Na ResearchDocumento5 pagineBuset Na Researchmk soberanoNessuna valutazione finora
- Diagnosis & Management of NstemiDocumento26 pagineDiagnosis & Management of NstemiwlshakespeareNessuna valutazione finora
- New Microsoft Office Word DocumentDocumento14 pagineNew Microsoft Office Word DocumentMohamed RashadNessuna valutazione finora
- Transfusion Reactions and Their ManagementDocumento59 pagineTransfusion Reactions and Their ManagementAida AlaudinNessuna valutazione finora
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (120)
- Autologous Rib Microtia Construction: Nagata TechniqueDocumento15 pagineAutologous Rib Microtia Construction: Nagata Techniqueandi ilmansyahNessuna valutazione finora
- 1.1 Plumbing History and Terminologies - Building Utilities 1 (Course Materials)Documento13 pagine1.1 Plumbing History and Terminologies - Building Utilities 1 (Course Materials)Princessdy CocadizNessuna valutazione finora
- PneumoniaDocumento20 paginePneumoniaKartika RezkyNessuna valutazione finora
- Practice Test Questions Downloaded From FILIPINO NURSES CENTRALDocumento37 paginePractice Test Questions Downloaded From FILIPINO NURSES CENTRALFilipino Nurses Central50% (8)
- Scapula Setting AnaIsabel AlmeidaDocumento1 paginaScapula Setting AnaIsabel AlmeidaPeter ZachNessuna valutazione finora
- ResumeDocumento4 pagineResumeapi-283952616Nessuna valutazione finora
- Handbook: For Clinical Management of DengueDocumento124 pagineHandbook: For Clinical Management of DengueraattaiNessuna valutazione finora
- Sleep Gauge - Sleep Quality ScoreDocumento1 paginaSleep Gauge - Sleep Quality ScoreMike UyNessuna valutazione finora
- The FRCPath Exam - Paul BennettDocumento130 pagineThe FRCPath Exam - Paul BennettVictor ChanNessuna valutazione finora
- NURSING CARE PLAN Impaired Transfer AbilityDocumento1 paginaNURSING CARE PLAN Impaired Transfer AbilityAce Dioso Tubasco100% (1)
- CystoceleDocumento7 pagineCystocelesandeepv08Nessuna valutazione finora
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- (Trabajo) LRAMP - Linehan PDFDocumento7 pagine(Trabajo) LRAMP - Linehan PDFBreno PMNessuna valutazione finora
- Endometriosis: Epidemiology, Diagnosis and Clinical ManagementDocumento9 pagineEndometriosis: Epidemiology, Diagnosis and Clinical ManagementRubiahSheBiachNessuna valutazione finora
- Case Presentation:: DR - Amra Farrukh PG.T Su.IDocumento75 pagineCase Presentation:: DR - Amra Farrukh PG.T Su.IpeeconNessuna valutazione finora
- Periodontal Infection Control: Current Clinical ConceptsDocumento10 paginePeriodontal Infection Control: Current Clinical ConceptsNunoGonçalvesNessuna valutazione finora
- Don Mottin - Stage Hypnosis - Class HandoutsDocumento46 pagineDon Mottin - Stage Hypnosis - Class HandoutsRaphael Maurin100% (2)
- Vitapex. A Case Report PDFDocumento4 pagineVitapex. A Case Report PDFPamela GuzmánNessuna valutazione finora
- The Obesity Code: Unlocking the Secrets of Weight LossDa EverandThe Obesity Code: Unlocking the Secrets of Weight LossValutazione: 4 su 5 stelle4/5 (5)