Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
COPD 27480 Lung Functional Decline in Copd 020812
Caricato da
Sondang Farwaty SitanggangCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
COPD 27480 Lung Functional Decline in Copd 020812
Caricato da
Sondang Farwaty SitanggangCopyright:
Formati disponibili
International Journal of COPD
Dovepress
open access to scientific and medical research
R e v ie w
Open Access Full Text Article
Lung function decline in COPD
This article was published in the following Dove Press journal:
International Journal of COPD
8 February 2012
Number of times this article has been viewed
Claudio Tantucci
Denise Modina
Unit of Respiratory Medicine,
Department of Medical and Surgical
Sciences, University of Brescia,
Brescia, Italy
Abstract: The landmark study of Fletcher and Peto on the natural history of tobacco
smoke-related chronic airflow obstruction suggested that decline in the forced expiratory
volume in the first second (FEV1) in chronic obstructive pulmonary disease (COPD) is slow
at the beginning, becoming faster with more advanced disease. The present authors reviewed
spirometric data of COPD patients included in the placebo arms of recent clinical trials to assess
the lung function decline of each stage, defined according to the severity of airflow obstruction
as proposed by the Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines.
In large COPD populations the mean rate of FEV1 decline in GOLD stages II and III is between
47 and 79mL/year and 56 and 59mL/year, respectively, and lower than 35mL/year in GOLD
stage IV. Few data on FEV1 decline are available for GOLD stage I. Hence, the loss of lung
function, assessed as expiratory airflow reduction, seems more accelerated and therefore more
relevant in the initial phases of COPD. To have an impact on the natural history of COPD, it is
logical to look at the effects of treatment in the earlier stages.
Keywords: chronic obstructive pulmonary disease, decline, forced expiratory volume in
1second, FEV1
Introduction
Correspondence: Claudio Tantucci
Clinica di Medicina Interna I, Spedali
Civili di Brescia, Piazzale Spedali
Civili 1, 25100 Brescia, Italy
Tel +39 030 39 80 69
Fax +39 030 39 80 69
Email tantucci@med.unibs.it
submit your manuscript | www.dovepress.com
Dovepress
http://dx.doi.org/10.2147/COPD.S27480
Assumptions about lung function decline occurring in chronic obstructive pulmonary
disease (COPD) have been greatly influenced by the landmark study of Fletcher and
Peto1 on the natural history of tobacco smokerelated chronic airflow obstruction.2
More than 30 years ago, Fletcher and Peto1 measured the forced expiratory volume
in 1second (FEV1) every 6months for an 8-year follow-up period in a cohort of 792
working men, drawing the well-known graph of FEV1 decline over time in COPD
(Figure1). FEV1 was originally expressed as a percentage of the value calculated by
extrapolation back to the age of 25 years, made equal to 100, and time in years from
age 25 to age 75.
A lot of information arose from Fletcher and Petos1 pioneering work: the individual
susceptibility to smoking-related lung functional damage, the unavoidable progression
of the airflow obstruction once COPD is established, the large variability of the abnormal
lung function decline among different subjects, the possible reduction of the excessive
FEV1 decline after smoking cessation at all times, and the paucity of self-reported
symptoms when the airflow reduction is mild to moderate. However, among the various
messages offered by their analysis, the most retained was that the rate of FEV1 decline
increased progressively with time in susceptible smokers. In other words, in the COPD
International Journal of COPD 2012:7 9599
95
2012 Tantucci and Modina, publisher and licensee Dove Medical Press Ltd. This is an Open Access
article which permits unrestricted noncommercial use, provided the original work is properly cited.
Dovepress
FEV1 (% of value of age 25)
Tantucci and Modina
100
Smoked and susceptible
to smoke
75
Never smoked or not
susceptible to smoke
Stopped at 45
years
Symptoms
50
Disability
Stopped at 65
years
25
Death
25
50
Age (years)
75
Figure 1 Modified version of Fletcher and Petos1 graph showing the decline in the forced expiratory volume in the firstsecond (FEV1).
patients who smoked, the lower the FEV1, the greater its
subsequent decline for similar intervals of time.
Some limitations must be acknowledged in the work of
Fletcher and Peto.1 All subjects were male, their recruitment
age was between 30 and 59 years only, and the follow-up
period was relatively short compared with the large time
range shown on the x-axis of Fletcher and Petos1 graph
(Figure1). Therefore, the curves shown in the graph were
largely extrapolated backward and forward with inherent
inaccuracies, possibly leading to an erroneous picture of the
phenomenon. Because of this, the present authors believe
that a false idea of lung function decline in COPD has been
inculcated in pulmonologists, suggesting that the disease progresses slowly at the beginning and that the loss of function
markedly increases only when a given degree of severity has
been reached. As a consequence, major therapeutic efforts
have been focused on severe to very severe airflow obstruction
in COPD patients. Recently, large amounts of data have been
collected to challenge Fletcher and Petos1 hypothesis.
In the framework of the classification of airflow obstruction severity proposed by Global Initiative for Chronic
Obstructive Lung Disease (GOLD) guidelines,3 the authors
analyzed the spirometric data of COPD patients enrolled
in recent prospective clinical trials and randomized in the
placebo arms to assess the natural rate of FEV1 decline of
each stage.
Methods
The authors searched the PubMed database and collected
the data available after 1990 on the average rate of FEV1
decline found in large observational studies and in recently
published prospective randomized control trials on COPD
patients and measured in the respective placebo arms with a
follow-up of at least 3 years.
96
submit your manuscript | www.dovepress.com
Dovepress
Results
The most important data concerning the average rate of FEV1
decline prospectively measured in large COPD cohorts are
shown in Table1.
Only one large study was found about COPD patients
with FEV1 higher than 80% of the predicted value (GOLD
stage I). A total of 430 COPD patients recruited in the first
stage of the Swiss Study on Air Pollution and Lung Diseases
in Adults exhibited an average annual decline in FEV1 of
about 40mL/year over 11 years.4 Within this cohort, the subgroup of asymptomatic patients had a slightly slower decline
than those with chronic cough and phlegm.4 A much smaller
cohort of GOLD stage I and II COPD patients was followed
for 3 years in the Copenhagen City Heart Study,5 and this
cohort showed a similar annual reduction in FEV1. Further
studies are urgently needed to establish firmly how FEV1
declines in GOLD stage I COPD patients. Data collected
on COPD patients recruited in GOLD stage II (with FEV1
between 79% and 50% of the predicted value) by Anthonisen
etal (for the Lung Health Study [LHS]),6 Pauwels etal,7
Anthonisen etal (for the LHS-3),8 the LHS Research Group,9
and Jenkins etal10 are consistent, reporting a mean annual
FEV1 decline of 56, 69, 53, 47, and 60mL/year, respectively.
However, it should be noted that in the post hoc analysis from
the TORCH (TOwards a Revolution in COPD Health) study
the placebo group did not faithfully represent the whole of
GOLD stage II, because the inclusion criteria required a
pre-bronchodilator FEV1 value of less than 60% of the predicted value.10 Accordingly, the COPD patients included in
this placebo group had a baseline pre-bronchodilator FEV1
between 60% and 50% of the predicted value. Recently
published data in the Groningen Leiden Universities Corticosteroids in Obstructive Lung Disease (GLUCOLD)
study showed a decline in the placebo group greater than
International Journal of COPD 2012:7
Dovepress
Lung function decline in COPD
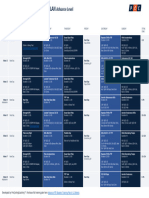
Table 1 Rate of annual decline in the forced expiratory volume in the first second (FEV1) recorded in Global Initiative for Chronic
Obstructive Lung Disease (GOLD) stage IIV chronic obstructive pulmonary disease patients randomized in the control arm during
longitudinal studies with a follow-up period of at least 3 years
Reference
Study
GOLD stage
Patients (n)
Age range (yr)
Follow-up period (yr)
Mean FEV1 decline
(mL/yr)*
Bridevaux et al4
SAPALDIA 1
430
1860
11
Vestbo et al
CCHS
III
145
Anthonisen et al6
Pauwels et al7
Anthonisen et al8
LHS Research Group9
Jenkins et al10
Lapperre et al11
Decramer et al12
LHS
EUROSCOP
LHS-3
LHS-2
TORCH
GLUCOLD
UPLIFT
II
II
II
II
II
II
II
1964
643
1357
557
535
24
1355
59 10
3560
3065
3060
4069
4080
4575
Burge et al
Jenkins et al10
Decramer et al12
ISOLDE
TORCH
UPLIFT
III
III
III
375
775
1331
Jenkins et al10
Decramer et al12
TORCH
UPLIFT
IV
IV
214
271
13
64 9
4075
4080
65 8
4080
63 8
40 37
42
5
3
11
3
3
3
4
56
69
53
47
60
79
49
3
3
4
59
56
38
3
4
34
23
Notes: Mean age plus or minus the standard deviation; *standard deviation is shown when available; pre-bronchodilator FEV1; post-bronchodilator FEV1.
Abbreviations: CCHS, Copenhagen City Heart Study; EUROSCOP, European Respiratory Society Study on Chronic Obstructive Pulmonary Disease; GLUCOLD,
Groningen Leiden Universities Corticosteroids in Obstructive Lung Disease study; ISOLDE, Inhaled Steroids in Obstructive Lung DiseasE study; LHS, Lung Health Study;
LHS-2, Lung Health Study 2; LHS-3, Lung Health Study 3; SAPALDIA 1, first stage of the Swiss Study on Air Pollution and Lung Diseases in Adults; TORCH, TOwards a
Revolution in COPD Health study; UPLIFT, Understanding Potential Long-term Impacts on Function with Tiotropium study; yr, year.
that found in previous studies, in average amounting to
79mL/year.11 A secondary analysis of the Understanding
Potential Long-term Impacts on Function with Tiotropium
(UPLIFT) study evaluated the effects of long-term treatment with tiotropium in GOLD stage II COPD patients.12
Pre-bronchodilator FEV1 declined by a mean of 49mL/year
in the control group. However, this group was not a true
placebo group, because all respiratory medications, except
other inhaled anticholinergic drugs, were allowed during
the trial and about 65% of these patients in the control arm
were taking two active drugs. Because of this, the lower
mean FEV1 decline in the UPLIFT control group cannot
be considered as truly representative of GOLD stage II
COPD. Therefore, it is reasonable to estimate that the mean
post-bronchodilator FEV1 decline of GOLD stage II COPD
patients amounts to 6112mL/year, with a little bias toward
the lowest initial FEV1 values in this stage. Lung function
decline of COPD patients recruited in GOLD stage III is
much better defined. In fact, Jenkins etal10 and Burge etal13
had very homogeneous data with a mean FEV1 decline from
56 to 59mL/year. Interestingly, the FEV1 decline reported by
Anzueto etal14 in a 1-year follow-up study performed in the
same stage of COPD severity amounted in the placebo arm
to 58mL/year. The average FEV1 decline found by Decramer
etal12 in GOLD stage III in the control arm of the UPLIFT
study, amounting to 38mL/year, is likely underestimated for
the same reason mentioned above. A few data available
International Journal of COPD 2012:7
about COPD patients recruited with FEV1 less than 30% of
the predicted value have shown a much slower mean FEV1
decline at GOLD stage IV than at other stages.10,12
Dawkins et al15 published interesting data about lung
function decline in patients with alpha-1-antitrypsin
deficiency-related emphysema stratified according to the
GOLD guidelines (Table 2). In emphysematous COPD
patients with the PiZ phenotype, the mean annual FEV1
decline was higher in moderate disease, corresponding to
GOLD stage II, and was greater than in the general COPD
population. These data suggest that COPD patients suffering
from panlobular emphysema have the highest rate of FEV1
decline occurring in the early phase of the disease. This has
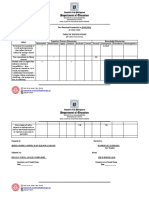
Table 2 Rate of annual decline of the forced expiratory volume in
the first second (FEV1) in Global Initiative for Chronic Obstructive
Lung Disease (GOLD) stage IIV chronic obstructive pulmonary
disease patients with alpha-1-antitrypsin deficiency-related
emphysema measured during a longitudinal study with a 3-year
follow-up period15
GOLD
stage
Patients
(n)
Age range
(yr)
Mean FEV1*
decline (mL/yr)
I
II
III
IV
18
26
38
19
49 9
51 9
53 11
49 9
32 19
90 19
52 8
89
Notes: Data are presented as mean plus or minus the standard error of the mean;
*pre-bronchodilator FEV1.
Abbreviation: yr, year.
submit your manuscript | www.dovepress.com
Dovepress
97
Dovepress
Tantucci and Modina
also been reported by Vestbo etal16 in a recently published
paper on the change in FEV1 over time in the large COPD
population enrolled in the Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints (ECLIPSE)
observational study. In this study patients with computerized
tomography scan evidence of emphysema exhibited the largest rate of FEV1 decline over a 3-year follow-up period.
this approach should be tested and proved by adequate
randomized clinical trials.17
It must be acknowledged that most of the recent large
COPD trials studied had a 3- to 4-year follow-up period,
which is much shorter than the follow-up period in Fletcher
and Petos1 analysis; this could be a limitation in the accuracy
of the FEV1 decline.
Furthermore, in many of these studies the percentage of
dropouts was higher in the placebo arm, meaning that the
average rate of FEV1 decline of healthier COPD patients
is known rather than that of the true COPD population.
As a consequence, the natural rate of FEV1 decline could
be underestimated by the existing data. It is reasonable
that this could be accentuated in the sicker COPD patients
recruited in GOLD stage IV. However, the withdrawal from
these studies is essentially because of symptoms and/or
exacerbations. Since FEV1 is poorly related to symptoms18
and even to exacerbations,19 it is plausible that this reasoning
may similarly be applied to each COPD stage, leaving the
message of a greater loss of function in the early phase of
the disorder still valid.
Finally, it should be recognized that the natural history of
lung function, not only in healthy never smokers and smokers
but also in COPD patients, has been essentially assessed in
terms of expiratory airflow reduction, looking at the FEV1
annual change as the primary measure to track the progressive
decline of lung function. This could be a limitation, especially
in very sick patients.
Discussion
According to the evidence produced, it is clear that the loss
of lung function, assessed as expiratory airflow reduction,
is more accelerated and therefore more relevant in the
early stages of COPD than in the late stages, with some
reservation regarding GOLD stage I where consistent
information is still lacking. Therefore, a different trend of
the FEV1 decline in COPD can be envisaged (Figure 2),
showing an opposite view to that of Fletcher and Petos
diagram (Figure1). This is likely because COPD patients
in the early stages have more to lose than those in the most
advanced stage. In addition, some of the FEV1 loss can be
partly buffered by the increase in total lung capacity in
GOLD stage IV COPD patients.
Based on these findings, it seems that any attempt to
positively interfere with the natural history of COPD by using
different therapeutic options should logically be focused on
COPD patients in at least GOLD stage II. This is suggested
by the subgroup analysis of the treatment group in the GOLD
stage II COPD patients of the UPLIFT study.12 Of course,
FEV1(% predicted)
100
80
Stage I
40 mL/yr
47-79 mL/yr
Stage II
50
56-59 mL/yr
Stage III
30
Stage IV
< 35 mL/yr
Years
Figure 2 Range of average rate of decline in the forced expiratory volume in the first second (FEV1) of chronic obstructive pulmonary disease patients according to initial
severity of airflow reduction.
Notes: The dashed segment of the line highlights any stage or part of it where consistent information is still lacking; control data from the UPLIFT (understanding Potential
Long-term Impacts on Function with Tiotropium) study were not considered in the analysis.
Abbreviation: yr, year.
98
submit your manuscript | www.dovepress.com
Dovepress
International Journal of COPD 2012:7
Dovepress
Conclusion
In summary, the authors have shown that information
provided in recent years about the rate of FEV1 decline in
COPD patients strongly supports the concept that the faster
progression of functional impairment in COPD occurs
early and it particularly occurs in GOLD stage II. This is
in contrast with Fletcher and Petos1 analysis. In the present
authors view it seems more logical to make efforts for an
early (spirometric) detection of COPD, based on risk factors
rather than symptoms, and to plan randomized clinical trials
to show the efficacy of an early strategy of intervention on
the natural history of such a disorder.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Fletcher C, Peto R. The natural history of chronic airflow obstruction.
Br Med J. 1977;1(6077):16451648.
2. Fletcher C, Peto R, Tinker CM, Speizer FE. The Natural History of
Chronic Bronchitis and Emphysema. London: Oxford University Press;
1976.
3. Global Initiative for Chronic Obstructive Lung Disease. Global strategy
for the diagnosis, management and prevention of chronic obstructive
pulmonary disease. Bethesda, MD: National Heart, Lung and Blood
Institute. April 2001 (revised 2007).
4. Bridevaux PO, Gerbase MW, Probst-Hensch NM, Schindler C,
Gaspoz JM, Rochat T. Long-term decline in lung function, utilisation
of care and quality of life in modified GOLD stage 1 COPD. Thorax.
2008;63(9):768774.
5. Vestbo J, Srensen T, Lange P, Brix A, Torre P, Viskum K. Long-term
effect of inhaled budesonide in mild and moderate chronic obstructive pulmonary disease: a randomised controlled trial. Lancet. 1999;353(9167):
18191823.
6. Anthonisen NR, Connett JE, Kiley JP, et al. Effects of smoking
intervention and the use of an inhaled anticholinergic broncodilator on the rate of decline of FEV1: the Lung Health Study. JAMA.
1994;272(19):14971505.
7. Pauwels RA, Lfdhal CG, Laitinen LA, et al. Long-term treatment
with inhaled budesonide in persons with mild chronic obstructive
pulmonary disease who continue smoking: European Respiratory
Society study on chronic obstructive pulmonary disease. N Engl J Med.
1999;340(25):19481953.
Lung function decline in COPD
8. Anthonisen NR, Connett JE, Murray RP. Smoking and lung function of
Lung Health Study participants after 11 years. Am J Respir Crit Care
Med. 2002;166(5):675679.
9. Lung Health Study Research Group. Effect of inhaled triamcinolone
on the decline in pulmonary function in chronic obstructive pulmonary
disease. N Engl J Med. 2000;343(26):19021909.
10. Jenkins CR, Jones PW, Calverly PM, etal. Efficacy of salmeterol/fluticasone propionate by GOLD stage of chronic obstructive pulmonary
disease: analysis from the randomised, placebo-controlled TORCH
study. Respir Res. 2009;10:59.
11. Lapperre TS, Snoeck-Stroband JB, Gosman MM, et al. Effect of
fluticasone with and without salmeterol on pulmonary outcomes in
chronic obstructive pulmonary disease. Ann Intern Med. 2009;151(8):
517527.
12. Decramer M, Celli B, Kesten S, Lystig T, Mehra S, Tashkin DP. Effect
of tiotropium on outcomes in patients with moderate chronic obstructive pulmonary disease (UPLIFT): a prespecified subgroup analysis of
a randomised controlled trial. Lancet. 2009;374(9696):11711178.
13. Burge PS, Calverley PMA, Jones PW, Spencer S, Anderson JA,
Maslen TK. Randomised, double blind, placebo controlled study
of fluticasone propionate in patients with moderate to severe
chronic obstructive pulmonary disease: the ISOLDE trial. BMJ.
2000;320(7245):12971303.
14. Anzueto A, Tashkin D, Menjoge S, Kesten S. One-year analysis of
longitudinal changes in spirometry in patients with COPD receiving
tiotropium. Pulm Pharmacol Ther. 2005;18(2):7581.
15. Dawkins PA, Dawkins CL, Wood AM, Nightingale PG, Stockley JA,
Stockley RA. Rate of progression of lung function impairment in
alpha1-antitrypsin deficiency. Eur Respir J. 2009;33(6):13381344.
16. Vestbo J, Edwards LD, Scanlon PD, et al. Changes in forced expiratory volume in 1 second over time in COPD. N Engl J Med.
2011;365(13):11841192.
17. Decramer M, Cooper CB. Treatment of COPD: the sooner the better?
Thorax. 2010;65(9):837841.
18. Curtis RJ, Deyo RA, Hudson LD. Pulmonary rehabilitation in
chronic respiratory insufficiency: 7. Health-related quality of life
among patients with chronic obstructive pulmonary disease. Thorax.
1994;49(2):162170.
19. Hurst JR, Vestbo J, Anzueto A, et al. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med.
2010;363(12):11281138.
Dovepress
International Journal of COPD
Publish your work in this journal
The International Journal of COPD is an international, peer-reviewed
journal of therapeutics and pharmacology focusing on concise rapid
reporting of clinical studies and reviews in COPD. Special focus is given
to the pathophysiological processes underlying the disease, intervention
programs, patient focused education, and self management protocols.
This journal is indexed on PubMed Central, MedLine and CAS. The
manuscript management system is completely online and includes a
very quick and fair peer-review system, which is all easy to use. Visit
http://www.dovepress.com/testimonials.php to read real quotes from
published authors.
Submit your manuscript here: http://www.dovepress.com/international-journal-of-copd-journal
International Journal of COPD 2012:7
submit your manuscript | www.dovepress.com
Dovepress
99
Potrebbero piacerti anche
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5795)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- TA35 & TA40 Articulated Dumptruck Maintenance Manual: Click Here For Table ofDocumento488 pagineTA35 & TA40 Articulated Dumptruck Maintenance Manual: Click Here For Table ofKot878100% (2)
- Lesson 5 Flight of Projectile, Air Resistance Neglected: OverviewDocumento7 pagineLesson 5 Flight of Projectile, Air Resistance Neglected: OverviewNadjer C. AdamNessuna valutazione finora
- LoRa TechnologyDocumento10 pagineLoRa TechnologyAnonymous CGk2roNessuna valutazione finora
- Mitsubishi IC Pneumatic Forklift PDFDocumento5 pagineMitsubishi IC Pneumatic Forklift PDFfdpc1987Nessuna valutazione finora
- Reconductoring Using HTLS Conductors. Case Study For A 220 KV Double Circuit Transmission LINE in RomaniaDocumento7 pagineReconductoring Using HTLS Conductors. Case Study For A 220 KV Double Circuit Transmission LINE in RomaniaJose ValdiviesoNessuna valutazione finora
- WCDMA19 Prfile Descriptions W19P8 08A APPRDocumento254 pagineWCDMA19 Prfile Descriptions W19P8 08A APPRoaguilar83Nessuna valutazione finora
- Serie10 ElecDocumento75 pagineSerie10 Elecmealier severineNessuna valutazione finora
- SR Cheat Sheets PDFDocumento4 pagineSR Cheat Sheets PDFDevin ZhangNessuna valutazione finora
- SD WanDocumento3 pagineSD Wanraditio ghifiardiNessuna valutazione finora
- Lesson 3 - Practical ResearchDocumento17 pagineLesson 3 - Practical ResearchBenNessuna valutazione finora
- EIC 3 Practice Exercises Unit 4Documento3 pagineEIC 3 Practice Exercises Unit 4Trần ChâuNessuna valutazione finora
- A Randomised Clinical Trial Comparing Myoinositol and Metformin in PCOSDocumento7 pagineA Randomised Clinical Trial Comparing Myoinositol and Metformin in PCOSAtika NajlaNessuna valutazione finora
- Essay Writing TipsDocumento4 pagineEssay Writing TipsSubhasish MitraNessuna valutazione finora
- Creating A Pathway For Every Student: Holyoke High School Redesign Strategic PlanDocumento29 pagineCreating A Pathway For Every Student: Holyoke High School Redesign Strategic PlanMike PlaisanceNessuna valutazione finora
- Unit-I Basic Concepts: Course Code: BTCS9504 Course Name: Network Operating SystemsDocumento17 pagineUnit-I Basic Concepts: Course Code: BTCS9504 Course Name: Network Operating SystemsPradeep BediNessuna valutazione finora
- Namma Kalvi 10th English Pta Model Question Papers 217163Documento36 pagineNamma Kalvi 10th English Pta Model Question Papers 217163609001Nessuna valutazione finora
- FTP Booster Training Plan OverviewDocumento1 paginaFTP Booster Training Plan Overviewwiligton oswaldo uribe rodriguezNessuna valutazione finora
- Exercise On Coordination and ResponseDocumento8 pagineExercise On Coordination and ResponseNorliyana AliNessuna valutazione finora
- Social and Professional Issues Pf2Documento4 pagineSocial and Professional Issues Pf2DominicOrtegaNessuna valutazione finora
- Australia Visa RequirementsDocumento1 paginaAustralia Visa RequirementsJoana DetomasNessuna valutazione finora
- Essentials of Repertorization Tiwari Link PageDocumento11 pagineEssentials of Repertorization Tiwari Link PageBibin TSNessuna valutazione finora
- DrosteDocumento4 pagineDrosteapi-478100074Nessuna valutazione finora
- Issues in Corporate GovernanceDocumento15 pagineIssues in Corporate GovernanceVandana ŘwţNessuna valutazione finora
- Iraqi Portal of Knowledge and Heritage With Format Edits - 11-21-2023Documento6 pagineIraqi Portal of Knowledge and Heritage With Format Edits - 11-21-2023محمد الكربلائيNessuna valutazione finora
- ATMPP Diabetes Change and Review Proposal Npa 2012-18Documento8 pagineATMPP Diabetes Change and Review Proposal Npa 2012-18Juha TamminenNessuna valutazione finora
- Steel Sections PDFDocumento36 pagineSteel Sections PDFTonderai RusereNessuna valutazione finora
- TOS 1st QuarterDocumento6 pagineTOS 1st QuarterQuerisa Ingrid MortelNessuna valutazione finora
- Linear Analysis of Concrete Frames Considering Joint FlexibilityDocumento16 pagineLinear Analysis of Concrete Frames Considering Joint FlexibilityluffiM13Nessuna valutazione finora
- Energy Management Assignment #01: Submitted BY Shaheer Ahmed Khan (MS2019198019)Documento15 pagineEnergy Management Assignment #01: Submitted BY Shaheer Ahmed Khan (MS2019198019)shaheer khanNessuna valutazione finora
- A. in What Way Is Khatri A Surplus Unit?Documento5 pagineA. in What Way Is Khatri A Surplus Unit?Aakriti SanjelNessuna valutazione finora