Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Clinical Case Studies Ocd Copilarie
Caricato da
Agentia RonetCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Clinical Case Studies Ocd Copilarie
Caricato da
Agentia RonetCopyright:
Formati disponibili
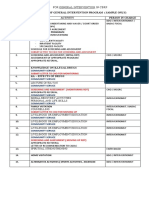
Clinical
Case Studies
http://ccs.sagepub.com/
Introduction to the Special Issue: Treatment of Childhood Obsessive-Compulsive
Disorder
Dean McKay and Eric A. Storch
Clinical Case Studies 2014 13: 3
DOI: 10.1177/1534650113504486
The online version of this article can be found at:
http://ccs.sagepub.com/content/13/1/3
Published by:
http://www.sagepublications.com
Additional services and information for Clinical Case Studies can be found at:
Email Alerts: http://ccs.sagepub.com/cgi/alerts
Subscriptions: http://ccs.sagepub.com/subscriptions
Reprints: http://www.sagepub.com/journalsReprints.nav
Permissions: http://www.sagepub.com/journalsPermissions.nav
Citations: http://ccs.sagepub.com/content/13/1/3.refs.html
>> Version of Record - Dec 31, 2013
What is This?
Downloaded from ccs.sagepub.com at University of Bucharest on December 7, 2014
504486
research-article2013
CCS13110.1177/1534650113504486Clinical Case StudiesMcKay and Storch
Article
Introduction to the Special Issue:
Treatment of Childhood
Obsessive-Compulsive Disorder
Clinical Case Studies
2014, Vol 13(1) 38
The Author(s) 2013
Reprints and permissions:
sagepub.com/journalsPermissions.nav
DOI: 10.1177/1534650113504486
ccs.sagepub.com
Dean McKay1 and Eric A. Storch2
Obsessive-compulsive disorder (OCD) has long been considered a complex and disabling psychiatric condition, marked by intrusive and unwanted imagery (obsessions) that is usually accompanied by ritualized behavior designed to neutralize the obsessions. Treatment research has
shown that, for those who complete treatment, significant improvement can be achieved (Simpson
et al., 2011; Storch, Geffken, et al., 2007). There is a growing consensus that the first-line psychosocial treatment for OCD is exposure with response prevention (ERP; McKay et al., 2013;
Olatunji et al., 2013). In the case of children, meta-analyses have shown that ERP is highly efficacious, with large effect sizes (mean d = 1.98; Abramowitz, Whiteside, & Deacon, 2005).
Indeed, practice parameters recommend ERP monotherapy as the treatment of choice for mild
and moderate cases, and together with antidepressant medication for only the most severe presentation. Although this augurs well for the treatment of children with OCD, not all children respond
to treatment and ERP dissemination remains a challenge.
Accordingly, this special issue is devoted to cases involving variations in treatment delivery
and symptom presentation in childhood OCD. The articles that form this special issue address a
variety of special circumstances that take the reader beyond the findings from randomized controlled trials that evaluate the efficacy of ERP in general. Instead, these cases help the reader
understand the issue of comorbidity and how to successfully contend with it during treatment,
and provide a peek at several promising avenues that are emerging in the treatment of childhood
OCD. These include addressing family-related complications in treatment delivery, specific
developmental phases (i.e., in very young children), Also examined in this special are cases with
under severe stigmatizing conditions, when symptoms present with complex comorbidities, and
evaluation of interventios that by capitalizes on technological advances in service delivery.
Beyond ERP: Presenting Symptoms That Necessitate Additional
Interventions
As treatment delivery becomes more sophisticated, we have come to understand that symptom
presentations do not always immediately lend themselves to exposure. One prominent example is
hoarding, which is now a separate disorder in a broader category of obsessive-compulsive-related
disorders in the Diagnostic and Statistical Manual of Mental Disorders (5th ed.; DSM-V; American
Psychiatric Association, 2013). This was the result of extensive research showing that hoarding
1Fordham
University, Bronx, NY, USA
of South Florida, Tampa, FL, USA
2University
Corresponding Author:
Dean McKay, Department of Psychology, Fordham University, 441 East Fordham Road, Bronx, NY 10458, USA.
Email: mckay@fordham.edu
Downloaded from ccs.sagepub.com at University of Bucharest on December 7, 2014
Clinical Case Studies 13(1)
was highly dissimilar from other symptoms of OCD (Pertusa et al., 2010) and that ERP typically
resulted in poor outcome with hoarding (Abramowitz, Franklin, Schwartz, & Furr, 2003). While
initial hoarding symptoms are thought to onset during childhood for many (Storch, Rahman, Park,
Murphy, & Lewin, 2011), there are very few data on its treatment in pediatric patients. In the present case series, Ale, Arnold, Whiteside, and Storch (2014) present a case of pediatric hoarding
whereby family treatment was implemented to successfully use ERP, illustrating that ERP may be
viewed as an essential component, but not necessarily a sufficient condition, for improvement.
In clinical practice, most cases present with comorbidities (Ollendick, Jarrett, Grills-Taquechel,
Hovey, & Wolff, 2008). Nonetheless, treatment outcome is typically unaffected in cases of
comorbidities that do not substantially and additionally interfere with cognitive processing
(Storch et al., 2008). This is not always the case, and in children, OCD may be present with other
developmental disorders. One condition that is particularly challengingand receiving more
clinical and research attentionis when OCD is accompanied by autism spectrum disorders.
Nadeau, Arnold, Storch, and Lewin (2014) illustrate the utility of a modular-based family therapy
approach to alleviate symptoms in a child with OCD with autism. This case demonstrates yet
again that while exposure may be viewed as a necessary component, it is not necessarily sufficient for success, and indeed, using ERP without other methods for ensuring successful implementation may impede progress rather than facilitate it.
Speaking of Family Treatment . . .
Child-based treatment rarely takes place without being set in the context of the family environment. Interestingly, ERP has at times been viewed in the absence of the family environment,
particularly in the research with adults, but even in the meta-analysis of child treatment outcome
for OCD, there was virtually no mention of family interventions because the literature to that
point had ignored it, and it was cited as a potential avenue to evaluating potential mediators of
outcome (Abramowitz et al., 2005). These cases showcase the role of family-based interventions
in varying degrees in a young child (Labouliere, Arnold, Storch, & Lewin, 2014), as a result of
failed ERP when oppositional-defiant disorder was also present (Hughes-Scalise & Przeworski,
2014) and in a case of remote treatment delivery using web-camera (Ojserkis, Morris, & McKay,
2014). In all cases, functional assessment was crucial in determining family environment factors
that required intervention beyond simply ERP.
Technology and Treatment Delivery
Availability of expert treatment for OCD is a significant challenge for the profession, and there
have been efforts to address this problem, such as the behavior therapy training institute offered
by the International Obsessive Compulsive Disorder Foundation (Szymanski, 2012) that trains
new providers in the provision of ERP. One promising new frontier in this regard is the use of
web-camera delivered therapy (Storch, Caporino, et al., 2011and utilized in one of the cases in
this series (Ojserkis et al., 2014). This approach has the promise of reducing the impact of geographic and financial/academic barriers (e.g., parent and/or child missing a large amount of
work/school when traveling to sessions that are far away) that hinder treatment access. Additional
technological advances have momentary value for implementation such as through smartphone
applications. Whiteside, Ale, Douglas, Tiede, and Dammann (2014) illustrate the use of a smartphone app for treatment of mild obsessive-compulsive symptoms in children. This novel approach
provides a means for demonstrating cost-effective alternatives to treatment and serves as a potential preventive measure for early-onset OCD.
Downloaded from ccs.sagepub.com at University of Bucharest on December 7, 2014
McKay and Storch
The Implications of a Biological Model of OCD
For several years now, policy makers and the American Psychiatric Association have emphasized
the importance of biological models to the exclusion of perspectives that emphasize multiple
causes of behavior disorders. To wit, the recent Research Domains Criteria (RDoCs) explicitly
stress biological mechanisms. Indeed, in an editorial on the RDoCs, the following was offered:
. . . the RDoC framework conceptualizes mental illnesses as brain disorders. In contrast to
neurological disorders with identifiable lesions, mental disorders can be addressed as disorders of
brain circuits. (Insel et al., 2010, p. 749)
Paradoxically, the emphasis on biological models has increased the stigmatizing effects of
mental illness (Pescosolido et al., 2010).1 Mental health providers will likely observe a rise in
stigma complicating their efforts to offer relief to their clients in light of the increasing emphasis
on biological causes of mental illness. In this case series, a case of a child with OCD who faced
stigma associated with a physical handicap and that, based on functional analysis, revealed to be
a complicating feature in his or her presenting symptoms and was successfully treated with additional coping strategies to alleviate the stigma the child experienced (Babinski, Pelham, &
Waxmonsky, 2013). This case is instructive for future problems associated with stigma, whether
physical handicapping conditions or stigma imposed from the community or other agencies due
to observable symptoms of mental illness.
Where Do We Go Next?
As we hope is clear, ERP presents as a powerful treatment associated with robust effects in the
treatment of youth with OCD, as well as many other psychological disorders. However, not all
youth respond to this intervention and response is not always complete. Given this, the next generation of studies must consider how to tailor interventions to address comorbidity and how to
maximize treatment response. To this end, we highlight several specific directions for future
research and clinical attention.
First, there is a great need to improve on the degree of treatment response experienced by the
average child with OCD. Approximately, 40% to 50% of children with OCD who are treated with
ERP achieve remission, indicating that many others are partial responders or did not glean clinically significant benefit. Given this, efforts to enhance treatment response are greatly needed.
One promising avenue involves d-cycloserine (DCS) augmentation of ERP. Preliminary results
have been promising, demonstrating an advantage for DCS augmentation or ERP relative to
placebo (Storch et al., 2010). Beyond the overall treatment effects, this approach may accelerate
the rate of response (Chasson et al., 2010) and, importantly, do so in a very safe manner that is
acceptable to parents. We are currently in the middle of a large-scale randomized controlled trial
examining the efficacy of this approach in youth with OCD (McGuire et al., 2012). A second
approach to this issue involves how to incorporate family into treatment. For many providers,
individual child treatment means just thatthat the child is the exclusive focus of treatment, and
family members are included marginally if at all. We believe that having a robust family componentas shown in the Labouliere et al. (2014) articleis one method of enhancing treatment
outcome. In this model, parents are taught to be their childs therapist so that they are able to
implement exposure tasks and other therapeutic assignments independently in the natural environment (Storch, Geffken, et al., 2007). Because it is clear that homework is integrally related to
treatment outcome (Abramowitz, Franklin, Zoellner, & DiBernardo, 2002) and that parents are
able to effectively monitor compliance when involved in treatment, we believe this is one method
Downloaded from ccs.sagepub.com at University of Bucharest on December 7, 2014
Clinical Case Studies 13(1)
of enhancing overall response. Similarly, it is clear that OCD affects the entire family and that
family members are often involved in a childs symptoms (Storch, Merlo, et al., 2007). Inclusion
of family members allows the clinician to address family factors that are involved in treatment
that, without being addressed, would negatively influence treatment outcome (Merlo, Lehmkuhl,
Geffken, & Storch, 2009).
Second, as the above articles demonstrate, comorbidity in pediatric OCD is the rule rather
than the exception. It is relatively infrequent that a child presents with no comorbid conditions.
Many times it is easy to address the comorbidity in the context of treating the OCD. For example,
some data suggest that improving obsessive-compulsive symptoms is actually associated with
reduced depressive symptoms in children with OCD (Meyer et al., 2013). At other times, however, one must consider how to address the OCD and comorbid conditions in a theoretically
informed fashion that considers the available evidence base. In this vein, personalizing the treatment approach to address the OCD and the comorbid problem is likely to result in improved
outcomes. We believe that there are several particular comorbidities for which this may be most
relevant (Storch et al., 2008). In the case of disruptive behavior, addressing the disruptiveness
and defiance sequentially to the obsessive-compulsive symptoms may facilitate the treatment
process by reducing interference in exposure tasks due to oppositionality. Depressive symptoms
may impact the treatment course by the childs unwillingness or inability to participate in treatment due to his or her depression; there are some data that suggest that habituation may be
affected in those with OCD who are also depressed (Abramowitz, 2004).Thus, addressing depression sequentially and/or concurrently to OCD may be appropriate at times. Finally, many children with OCD also present with attention deficit hyperactivity disorder. Problematically, these
symptoms often interfere with the childs ability to engage during treatment as well as his or her
ability to independently utilize therapeutic skills. Consideration of evidence-based attention deficit hyperactivity disorder interventions may be one method of addressing these symptoms to
foster improved OCD treatment outcome.
Finally, as each of the articles point out, ERP is a very effective intervention for children with
OCD. However, dissemination is greatly lacking. Many providers are not engaging in evidencebased OCD interventions at all, and many of those who do provide some elements of evidencebased treatment are leaving out exposure therapy (Marques et al., 2010), which is the most robust
element of this approach. Because of this, antidepressants, either alone or with psychotherapy
(often not ERP), are used with frequency in youth with OCD despite more modest efficacy (but
greater dissemination) relative to ERP and the potential for side effects. In the absence of available ERP, families are left with precious few choices of how best to treat their childs OCD,
which is a scenario that we view as unacceptable.
In sum, we hope that the present series stimulates thoughtful discussion and consideration
about the nature of pediatric OCD and methods of effective treatment. Ultimately, it is our goal
to improve the well-being of children affected by this disabling condition so that they may continue their development with happiness and without the burden of a mental health problem.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or
publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Note
1. Deacon (2013) provides a detailed analysis explaining why, despite the claims that ascribing biological causes to mental illness will decrease stigma, there is no compelling reason to expect this, and that
Downloaded from ccs.sagepub.com at University of Bucharest on December 7, 2014
McKay and Storch
the available research from medicine and social psychology clearly point to biological causes leading
to increased stigma. Furthermore, even within psychiatry, there are prominent voices who decry to
biological monoculture and instead emphasize the need for understanding mental illness in the context
of multiple causes (for a notable illustration, see Kendler, 2012).
References
Abramowitz, J. S. (2004). Treatment of obsessive-compulsive disorder in patients who have comorbid
major depression. Journal of Clinical Psychology, 60, 1133-1141.
Abramowitz, J. S., Franklin, M. E., Schwartz, S. A., & Furr, J. M. (2003). Symptom presentation and outcome of cognitive-behavioral therapy for obsessive-compulsive disorder. Journal of Consulting and
Clinical Psychology, 71, 1049-1057.
Abramowitz, J. S., Franklin, M. E., Zoellner, L. A., & DiBernardo, C. L. (2002). Treatment compliance and
outcome in obsessive-compulsive disorder. Behavior Modification, 26, 447-463.
Abramowitz, J. S., Whiteside, S. P., & Deacon, B. J. (2005). The effectiveness of treatment for pediatric
obsessive-compulsive disorder: A meta-analysis. Behavior Therapy, 36, 55-63.
Ale, C. M., Arnold, E., Whiteside, S. P. H., & Storch, E. A. (2014). Family-based behavioral treatment of
pediatric compulsive hoarding: A case example. Clinical Case Studies, 13, 9-21.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.).
Washington, DC: Author.
Babinski, D. E., Pelham, W. E., & Waxmonsky, J. G. (2014). Cognitive-behavioral therapy for pediatric
obsessive-compulsive disorder complicated by stigma: A case study. Clinical Case Studies, 13, 95-110.
Chasson, G. S., Buhlmann, U., Tolin, D. F., Rao, S. R., Reese, H. E., Rowley, T., . . . Wilhelm, S. (2010).
Need for speed: Evaluating slopes of OCD recovery in behavior therapy enhanced with d-cycloserine.
Behaviour Research and Therapy, 48, 675-679.
Deacon, B. J. (2013). The biomedical model of mental disorders: A critical analysis of its validity, utility
and effects on psychotherapy research. Clinical Psychology Review, 33, 846-861.
Hughes-Scalise, A., & Przeworski, A. (2014). All in the family: Family-based behavioral treatment of child
obsessive-compulsive disorder & oppositional defiant disorder within the context of marital and family
discord. Clinical Case Studies, 13, 52-67.
Insel, T., Cuthbert, B., Garvey, M., Heinssen, R., Pine, D. S., Quinn, K., . . . Wang, P. (2010). Research
Domain Criteria (RDoC): Toward a new classification framework for research on mental disorders.
American Journal of Psychiatry, 167, 748-751.
Kendler, K. S. (2012). The dappled nature of causes of psychiatric illness: Replacing the organic-functional/
hardware-software dichotomy with empirically-based pluralism. Molecular Psychiatry, 17, 377-388.
Labouliere, C. D., Arnold, E. B., Storch, E. A., & Lewin, A. B. (2014). Family based cognitive-behavioral
treatment for a preschooler with obsessive compulsive disorder. Clinical Case Studies, 13, 37-51.
Marques, L., LeBlanc, N. J., Weingarden, H. M., Timpano, K. R., Jenike, M., & Wilhelm, S. (2010).
Barriers to treatment and service utilization in an internet sample of individuals with obsessive-compulsive symptoms. Depression and Anxiety, 27, 470-475.
McGuire, J. F., Lewin, A. B., Geller, D. A., Brown, A., Ramsey, K., Mutch, P. J., . . . Storch, E. A. (2012).
Advances in the treatment of pediatric OCD: Rationale and design for the evaluation of D-cycloserine
with exposure and response prevention. Neuropsychiatry, 2, 291-300.
McKay, D., Sookman, D., Neziroglu, F., Wilhelm, S., Simpson, H. B., Stein, D., . . . Veale, D. (2013).
Efficacy of cognitive-behavior therapy for obsessive-compulsive disorder. Manuscript submitted for
publication.
Merlo, L. J., Lehmkuhl, H., Geffken, G. R., & Storch, E. A. (2009). Decrease in family accommodation
is associated with improved cognitive-behavioral therapy outcome in pediatric obsessive-compulsive
disorder. Journal of Consulting and Clinical Psychology, 77, 355-360.
Meyer, J., McNamara, J. P. H., Reid, A. M., Storch, E. A., Geffken, G. R., Mason, D. M., . . . Bussing, R.
(2013). Prospective relationship between obsessive-compulsive and depressive symptoms during multimodal treatment in pediatric obsessive-compulsive disorder. Child Psychiatry & Human Development.
doi: 10.1007/s10578-013-0388-4
Nadeau, J., Arnold, E. B., Storch, E. A., & Lewin, A. B. (2014). Family cognitive-behavioral treatment for
a child with autism and comorbid obsessive compulsive disorder. Clinical Case Studies, 13, 22-36.
Downloaded from ccs.sagepub.com at University of Bucharest on December 7, 2014
Clinical Case Studies 13(1)
Ojserkis, R., Morris, B., & McKay, D. (2014). Pediatric obsessive-compulsive disorder: An illustration of
intensive family-based treatment delivered via web camera. Clinical Case Studies, 13, 68-71.
Olatunji, B. O., Rosenfield, D., Tart, C. D., Cottraux, J., Powers, M. B., & Smits, J. A. J. (2013). Behavioral
versus cognitive treatment outcome of obsessive-compulsive disorder: An examination of outcome and
mediators of change. Journal of Consulting and Clinical Psychology, 81, 415-428.
Ollendick, T. H., Jarrett, M. A., Grills-Taquechel, A. E., Hovey, L. D., & Wolff, J. C. (2008). Comorbidity
as a predictor and moderator of treatment outcome in youth with anxiety, affective, attention deficit/hyperactivity disorder, and oppositional/conduct disorders. Clinical Psychology Review, 28,
1447-1471.
Pertusa, A., Frost, R. O., Fullana, M. A., Samuels, J., Steketee, G., Tolin, D. F., . . . Mataix-Cols, D. (2010).
Refining the diagnostic boundaries of compulsive hoarding: A critical review. Clinical Psychology
Review, 30, 371-386.
Pescosolido, B. A., Martin, J. K., Long, J. S., Medina, T. R., Phelan, J. C., & Link, B. G. (2010). A disease
like any other? A decade of change in public reactions to schizophrenia, depression, and alcohol dependence. American Journal of Psychiatry, 167, 1321-1330.
Simpson, H. B., Maher, M. J., Wang, Y., Bao, Y., Foa, E. B., & Franklin, M. (2011). Patient adherence
predicts outcome from cognitive-behavioral therapy in obsessive-compulsive disorder. Journal of
Consulting and Clinical Psychology, 79, 247-252.
Storch, E. A., Caporino, N. E., Morgan, J. R., Lewin, A. B., Rojas, A., Brauer, L., . . . Murphy, T. K.
(2011). Preliminary investigation of a web-camera delivered cognitive-behavioral therapy for youth
with obsessive-compulsive disorder. Psychiatry Research, 189, 407-412.
Storch, E. A., Geffken, G. R., Merlo, L. J., Mann, G., Duke, D., Munson, M., . . . Goodman, W. K. (2007).
Cognitive-behavioral therapy for pediatric obsessive-compulsive disorder: Comparison of intensive
and weekly approaches. Journal of the American Academy of Child & Adolescent Psychiatry, 46,
469-478.
Storch, E. A., Merlo, L. J., Larson, M. J., Fernandez, M., Jacob, M. L., Geffken, G. R., . . . Goodman, W. K.
(2007). Family accommodation in pediatric obsessive-compulsive disorder. Journal of Clinical Child
& Adolescent Psychology, 36, 207-216.
Storch, E. A., Merlo, L. J., Larson, M., Geffken, G. R., Lehmkuhl, H. D., Jacob, M. L., . . . Goodman,
W. K. (2008). The impact of comorbidity on cognitive-behavioral therapy response in pediatric obsessive
compulsive disorder. Journal of the American Academy of Child & Adolescent Psychiatry, 47, 583-592.
Storch, E. A., Murphy, T. K., Goodman, W. K., Geffken, G. R., Lewin, A. B., Henin, A., . . . Geller, D. A.
(2010). A preliminary study of D-cycloserine augmentation of cognitive-behavioral therapy in pediatric obsessive-compulsive disorder. Biological Psychiatry, 68, 1073-1076.
Storch, E. A., Rahman, O., Park, J. M., Murphy, T. K., & Lewin, A. B. (2011). Compulsive hoarding in
children. Journal of Clinical Psychology, 67, 507-516.
Szymanski, J. (2012). Using direct-to-consumer marketing strategies with obsessive-compulsive disorder in
the nonprofit sector. Behavior Therapy, 43, 251-256.
Whiteside, S. P. H., Ale, C. M., Douglas, K. V., Tiede, M. S., & Dammann, J. E. (2014). Case examples of
enhancing pediatric OCD treatment with a smartphone application. Clinical Case Studies, 13, 80-94.
Author Biographies
Dean McKay, PhD, is a professor of psychology at Fordham University. His primary areas of interest are
anxiety disorders and their treatment.
Eric Storch, PhD is the All Childrens Hospital Guild Endowed Chair and Professor in the Department of
Pediatrics at the University of South Florida. His primary research and clinical interests are in the phenomenology and treatment of children and adults with obsessive-compulsive and related disorders and anxiety
disorders.
Downloaded from ccs.sagepub.com at University of Bucharest on December 7, 2014
Potrebbero piacerti anche
- Therapist's Guide to Pediatric Affect and Behavior RegulationDa EverandTherapist's Guide to Pediatric Affect and Behavior RegulationNessuna valutazione finora
- Educational Strategies for Children With Autism Spectrum DisordersDa EverandEducational Strategies for Children With Autism Spectrum DisordersNessuna valutazione finora
- Sample Adhd Research PaperDocumento7 pagineSample Adhd Research Paperfvhqqm3b100% (1)
- Parent basedtreatmentforchildhoodandadolescentOCD PDFDocumento7 pagineParent basedtreatmentforchildhoodandadolescentOCD PDFwilmaNessuna valutazione finora
- Research Paper On Autism and Early InterventionDocumento8 pagineResearch Paper On Autism and Early Interventiondyf0g0h0fap3100% (1)
- 345-356 Behavioral Intervention For Young Children With AutismDocumento22 pagine345-356 Behavioral Intervention For Young Children With AutismUlilta MuktadiraNessuna valutazione finora
- Menninger OCD SPACEDocumento22 pagineMenninger OCD SPACEilda.jackmakianNessuna valutazione finora
- Example of A Research Paper On AdhdDocumento6 pagineExample of A Research Paper On Adhdnadevufatuz2100% (1)
- Article Psicometria PDFDocumento14 pagineArticle Psicometria PDFEstela RecueroNessuna valutazione finora
- Supporting Teens' Academic NeeDocumento41 pagineSupporting Teens' Academic NeeAsima MishraNessuna valutazione finora
- Adhd Research Paper ConclusionDocumento7 pagineAdhd Research Paper Conclusionafedthktn100% (1)
- Autism Literature ReviewDocumento7 pagineAutism Literature Reviewnaneguf0nuz3100% (1)
- Icare Basado en InternetDocumento12 pagineIcare Basado en InternetDaysy Katherine Pabon PochesNessuna valutazione finora
- Parents Suggest Which Indicators of Progress and Outcomes Should Be Measured in Young Children With Autism Spectrum DisorderDocumento11 pagineParents Suggest Which Indicators of Progress and Outcomes Should Be Measured in Young Children With Autism Spectrum DisorderAna GambaNessuna valutazione finora
- Early Start DENVER Model: A Meta-AnalysisDocumento14 pagineEarly Start DENVER Model: A Meta-AnalysisIris CostillasNessuna valutazione finora
- Clinical Case Studies-Anx - CopilDocumento15 pagineClinical Case Studies-Anx - CopilmudeteNessuna valutazione finora
- A Case Study Analysis of Children With AutismDocumento6 pagineA Case Study Analysis of Children With AutismKenny Rey GuillenNessuna valutazione finora
- Summarize The Article (2 Paragraphs)Documento4 pagineSummarize The Article (2 Paragraphs)Chris NorrisNessuna valutazione finora
- Smith Wendy WebsiterationalepartoneDocumento7 pagineSmith Wendy Websiterationalepartoneapi-667405381Nessuna valutazione finora
- Zheng Et Al. 2021Documento16 pagineZheng Et Al. 2021JonathanNessuna valutazione finora
- Schema Therapy in Adolescents With Externalizing Behavior Problems Bridging Theory and Practice Marjolein Van WijkDocumento258 pagineSchema Therapy in Adolescents With Externalizing Behavior Problems Bridging Theory and Practice Marjolein Van Wijkmina mirNessuna valutazione finora
- Major Evidence Based Interventions - EditedDocumento6 pagineMajor Evidence Based Interventions - EditedPaul WahomeNessuna valutazione finora
- The Role of Neuropsychological AssessmentDocumento28 pagineThe Role of Neuropsychological AssessmentJovani Gonzales VillarealNessuna valutazione finora
- Autism Literature Review ExampleDocumento6 pagineAutism Literature Review Exampleafmzadevfeeeat100% (1)
- Adhd Research Paper IntroductionDocumento6 pagineAdhd Research Paper Introductionehljrzund100% (1)
- Adhd Term Paper TopicsDocumento8 pagineAdhd Term Paper TopicsWriteMyPaperApaFormatUK100% (1)
- Adhd Research ThesisDocumento6 pagineAdhd Research Thesismegansimmonskansascity100% (2)
- Um ThesisDocumento5 pagineUm Thesisazyxppzcf100% (2)
- Literature Review Adhd in AdultsDocumento7 pagineLiterature Review Adhd in Adultsc5s8r1zc100% (1)
- 10 1016@j Spen 2020 100831Documento17 pagine10 1016@j Spen 2020 100831tania luarteNessuna valutazione finora
- Behavior TherapyDocumento35 pagineBehavior Therapynikos kasiktsisNessuna valutazione finora
- 1 s2.0 S0005789423000370 MainDocumento10 pagine1 s2.0 S0005789423000370 MainAli JNessuna valutazione finora
- School Behavioral Health: Mark D. Weist Kathleen B. Franke Robert N. Stevens EditorsDocumento142 pagineSchool Behavioral Health: Mark D. Weist Kathleen B. Franke Robert N. Stevens EditorsRoger AndreyNessuna valutazione finora
- العلاج التفاعلىDocumento90 pagineالعلاج التفاعلىHamada ElzaiatNessuna valutazione finora
- Running Head: Early Interventions For FASD 1Documento20 pagineRunning Head: Early Interventions For FASD 1api-289842236Nessuna valutazione finora
- Literature Review Example AdhdDocumento4 pagineLiterature Review Example Adhddrnpguwgf100% (1)
- Research Paper On Emotional and Behavioral DisordersDocumento5 pagineResearch Paper On Emotional and Behavioral Disordersgw219k4yNessuna valutazione finora
- Arch Dis Child 2004 Cuestas 290Documento6 pagineArch Dis Child 2004 Cuestas 290Hafizah FzNessuna valutazione finora
- Introduction For A Research Paper On AutismDocumento7 pagineIntroduction For A Research Paper On Autismh015trrr100% (1)
- Evidence Has To Do With TrustDocumento6 pagineEvidence Has To Do With TrustladyjennieNessuna valutazione finora
- From The Center's Clearinghouse ..Documento13 pagineFrom The Center's Clearinghouse ..Anonymous 4BpXDcQWNessuna valutazione finora
- Hallett-2021 - Predictive Parent TrainingDocumento11 pagineHallett-2021 - Predictive Parent TrainingLia C CriscoulloNessuna valutazione finora
- 2-Ped. Clinics of North America-April 2009, Vol.56, Issues 2, Child Abuse and Neglect - Advancements and Challenges in The 21st CenturyDocumento122 pagine2-Ped. Clinics of North America-April 2009, Vol.56, Issues 2, Child Abuse and Neglect - Advancements and Challenges in The 21st CenturyDina HottestwopiemNessuna valutazione finora
- Evaluation of The Child With Global Developmental DelayDocumento14 pagineEvaluation of The Child With Global Developmental DelayplaincircleNessuna valutazione finora
- A Baseline Controlled Examination of A 5-Day Intensive Treatment For Pediatric Obsessive-Compulsive Disorder - Whiteside 2014 PDFDocumento6 pagineA Baseline Controlled Examination of A 5-Day Intensive Treatment For Pediatric Obsessive-Compulsive Disorder - Whiteside 2014 PDFLaura HdaNessuna valutazione finora
- Medical Students Perceptions Awareness Societal Attitudes and Knowledge of Autism Spectrum Disorder An Exploratory Study in MalaysiaDocumento11 pagineMedical Students Perceptions Awareness Societal Attitudes and Knowledge of Autism Spectrum Disorder An Exploratory Study in MalaysiaHobieNessuna valutazione finora
- Adhd Research Paper PDFDocumento7 pagineAdhd Research Paper PDFgw1w9reg100% (1)
- Pzaa 232Documento11 paginePzaa 232Aroa BermudezNessuna valutazione finora
- Free Research Paper On Cerebral PalsyDocumento6 pagineFree Research Paper On Cerebral Palsyp0lolilowyb3100% (1)
- CatnumounoDocumento10 pagineCatnumounoapi-285628051Nessuna valutazione finora
- Psychiatry Clinical Child Psychology andDocumento20 paginePsychiatry Clinical Child Psychology andirimes carmelaNessuna valutazione finora
- Cognitive-Behavioral Therapy For ADHD in Adolescents Clinical ConsiderationsDocumento11 pagineCognitive-Behavioral Therapy For ADHD in Adolescents Clinical Considerationsdmsds100% (1)
- Birchalllindsay651final-Dec 4 - 2013Documento26 pagineBirchalllindsay651final-Dec 4 - 2013api-289842236Nessuna valutazione finora
- ASHA Scholarship Essay 2Documento3 pagineASHA Scholarship Essay 2sip805Nessuna valutazione finora
- Young2010 Tratamientos No Farmacológicos en El TdahDocumento18 pagineYoung2010 Tratamientos No Farmacológicos en El TdahJuan Carlos A S ⃝⃒⃤Nessuna valutazione finora
- Thesis Papers AdhdDocumento7 pagineThesis Papers Adhdfjcsyx0f100% (1)
- Annis - Phase 3 PaperDocumento9 pagineAnnis - Phase 3 Paperapi-246877565Nessuna valutazione finora
- Research Paper AdhdDocumento4 pagineResearch Paper Adhdiqfjzqulg100% (1)
- TranscriptDocumento3 pagineTranscriptDanna Sofia Gomez DuqueNessuna valutazione finora
- Manejo Farmacologico de La EspasticidadDocumento15 pagineManejo Farmacologico de La EspasticidadssanabriaaNessuna valutazione finora
- CCCRS Coding Manual v5 WebDocumento23 pagineCCCRS Coding Manual v5 WebAgentia RonetNessuna valutazione finora
- By Carlton E. Munson: Handbook of Clinical Social Work SupervisionDocumento2 pagineBy Carlton E. Munson: Handbook of Clinical Social Work SupervisionAgentia RonetNessuna valutazione finora
- BIS/BAS ScalesDocumento2 pagineBIS/BAS ScalesAgentia RonetNessuna valutazione finora
- Acasa 1longitudinalDocumento10 pagineAcasa 1longitudinalmudeteNessuna valutazione finora
- Acasa 1longitudinalDocumento10 pagineAcasa 1longitudinalmudeteNessuna valutazione finora
- Situri Carti GratisDocumento3 pagineSituri Carti GratisAgentia Ronet75% (4)
- Ost 2010 Applied RelaxationDocumento16 pagineOst 2010 Applied RelaxationAgentia RonetNessuna valutazione finora
- Pachet de Servicii Integrate Psiholog La Inceput de DrumDocumento17 paginePachet de Servicii Integrate Psiholog La Inceput de DrumAgentia RonetNessuna valutazione finora
- BIS/BAS ScalesDocumento2 pagineBIS/BAS ScalesAgentia RonetNessuna valutazione finora
- CCCRS Coding Manual v5 WebDocumento23 pagineCCCRS Coding Manual v5 WebAgentia RonetNessuna valutazione finora
- CCCRS Score Feedback Sheet v5 WebDocumento4 pagineCCCRS Score Feedback Sheet v5 WebAgentia RonetNessuna valutazione finora
- Clinical Case Studies-Fobie - SangeDocumento15 pagineClinical Case Studies-Fobie - SangemudeteNessuna valutazione finora
- PH ApaDocumento1 paginaPH ApaAgentia RonetNessuna valutazione finora
- Pachet de Servicii Integrate Psiholog La Inceput de DrumDocumento17 paginePachet de Servicii Integrate Psiholog La Inceput de DrumAgentia RonetNessuna valutazione finora
- Fani 2012 PTSD Attention Bias BrainDocumento9 pagineFani 2012 PTSD Attention Bias BrainAgentia RonetNessuna valutazione finora
- Ost 2010 Applied RelaxationDocumento16 pagineOst 2010 Applied RelaxationAgentia RonetNessuna valutazione finora
- Pachet de Servicii Integrate Psiholog La Inceput de DrumDocumento17 paginePachet de Servicii Integrate Psiholog La Inceput de DrumAgentia RonetNessuna valutazione finora
- FeedingDocumento69 pagineFeedingAgentia RonetNessuna valutazione finora
- Healthy EatingDocumento8 pagineHealthy EatingAgentia RonetNessuna valutazione finora
- Healthy Eating DepressionDocumento16 pagineHealthy Eating DepressionTanya ParnellNessuna valutazione finora
- 2.D.. CALMS Rating FormDocumento7 pagine2.D.. CALMS Rating FormmudeteNessuna valutazione finora
- Clinical Case Studies MBT - Depresie StudentDocumento14 pagineClinical Case Studies MBT - Depresie StudentAgentia RonetNessuna valutazione finora
- Fani 2012 PTSD Attention Bias BrainDocumento9 pagineFani 2012 PTSD Attention Bias BrainAgentia RonetNessuna valutazione finora
- Ost 2010 Applied RelaxationDocumento16 pagineOst 2010 Applied RelaxationAgentia RonetNessuna valutazione finora
- Clinical Case Studies Narativa Tulb AlimentDocumento16 pagineClinical Case Studies Narativa Tulb AlimentAgentia RonetNessuna valutazione finora
- Aftermath of A Fight or Regrettable IncidentDocumento10 pagineAftermath of A Fight or Regrettable IncidentAgentia Ronet100% (2)
- Criminology Australian & New Zealand Journal Of: Police Torture in China and Its Causes: A Review of LiteratureDocumento24 pagineCriminology Australian & New Zealand Journal Of: Police Torture in China and Its Causes: A Review of LiteratureAgentia RonetNessuna valutazione finora
- Criminology Australian & New Zealand Journal ofDocumento32 pagineCriminology Australian & New Zealand Journal ofAgentia RonetNessuna valutazione finora
- Criminology Australian & New Zealand Journal Of: Police Torture in China and Its Causes: A Review of LiteratureDocumento24 pagineCriminology Australian & New Zealand Journal Of: Police Torture in China and Its Causes: A Review of LiteratureAgentia RonetNessuna valutazione finora
- Kristin Layous, Et Al. Delivering Happiness. Translating Positive Psychology Intervention Research For Treating Major and Minor Depressive DisordersDocumento11 pagineKristin Layous, Et Al. Delivering Happiness. Translating Positive Psychology Intervention Research For Treating Major and Minor Depressive DisordersCésar Daniel GonzálezNessuna valutazione finora
- Accommodations MenuDocumento7 pagineAccommodations Menuapi-508300120Nessuna valutazione finora
- Example Personal Statement PDFDocumento2 pagineExample Personal Statement PDFRajeev SrinivasNessuna valutazione finora
- NCP Sleep PatternDocumento3 pagineNCP Sleep PatternRA Balaoing100% (1)
- Foundations Mental Health Care 6th Morrison Valfre Test BankDocumento10 pagineFoundations Mental Health Care 6th Morrison Valfre Test BankRaadqqqNessuna valutazione finora
- Abnormal Psychology: Shiba Saeed Assistant Professor Govt. College, Township, LahoreDocumento36 pagineAbnormal Psychology: Shiba Saeed Assistant Professor Govt. College, Township, LahoreM.Fizan JavedNessuna valutazione finora
- Klein PublicationDocumento66 pagineKlein PublicationPsiholog Monica StănescuNessuna valutazione finora
- Detailed Lesson Plan in HealthDocumento5 pagineDetailed Lesson Plan in HealthRashel Villanueva100% (1)
- Reflection On Creative Writing - EditedDocumento3 pagineReflection On Creative Writing - EditedMWANGI ANASTASIA MWIHAKINessuna valutazione finora
- A Comparison of Somatic Symptoms Between Depressive Disorder and Somatoform DisorderDocumento8 pagineA Comparison of Somatic Symptoms Between Depressive Disorder and Somatoform DisorderInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- Kurt CobainDocumento12 pagineKurt CobainKC Respicio100% (1)
- TheraDocumento4 pagineTheramaircusNessuna valutazione finora
- AI150286 - ARIF HIDAYAT SASTRA INGGRIS - Arif HidayatDocumento72 pagineAI150286 - ARIF HIDAYAT SASTRA INGGRIS - Arif HidayatBang UcupNessuna valutazione finora
- Psychotherapy With Children and AdolescentsDocumento599 paginePsychotherapy With Children and AdolescentsirinaNessuna valutazione finora
- Behavior TherapyDocumento27 pagineBehavior TherapyMacBelenzoNessuna valutazione finora
- For General Intervention in CBRP: Submit Letter To Cho For Screening and AssessmentDocumento1 paginaFor General Intervention in CBRP: Submit Letter To Cho For Screening and AssessmentUy Henry0% (1)
- Communicating Phonics Selective Mutism PDFDocumento5 pagineCommunicating Phonics Selective Mutism PDFancadianaNessuna valutazione finora
- The Differential Diagnosis of FatigueDocumento4 pagineThe Differential Diagnosis of Fatiguemsmith6477Nessuna valutazione finora
- Overcoming Disordered Eating - 06 - Improving Low Self-EsteemDocumento11 pagineOvercoming Disordered Eating - 06 - Improving Low Self-EsteemYesha ShahNessuna valutazione finora
- Mood Disorders Important Considerations in Distinguishing Clinical Depressions From Normal SadnessDocumento4 pagineMood Disorders Important Considerations in Distinguishing Clinical Depressions From Normal SadnessJena CalalangNessuna valutazione finora
- Stress Management: 1. Self - Awareness and MindfulnessDocumento3 pagineStress Management: 1. Self - Awareness and MindfulnessyekiboomNessuna valutazione finora
- The Plight of The Parentified ChildDocumento2 pagineThe Plight of The Parentified Childeric parlNessuna valutazione finora
- PsychologyDocumento4 paginePsychologySushmita SahuNessuna valutazione finora
- Childhood Traumas: An Outline and OverviewDocumento13 pagineChildhood Traumas: An Outline and Overviewd17o100% (1)
- 2015 Article AbstractsOfThe16thInternationa PDFDocumento303 pagine2015 Article AbstractsOfThe16thInternationa PDFNatalia Michelle García MartínezNessuna valutazione finora
- Herbert Et Al. EmdrDocumento27 pagineHerbert Et Al. Emdrcatalina_serbanNessuna valutazione finora
- Parent Training in Autism Spectrum Disorder - What's in A Name - PDFDocumento20 pagineParent Training in Autism Spectrum Disorder - What's in A Name - PDFFarbodNessuna valutazione finora
- Eating Disorder Assessment (EDA-5) : January 2015Documento13 pagineEating Disorder Assessment (EDA-5) : January 2015Eminencia Garcia PerezNessuna valutazione finora
- Journal of Religion, Disability & HealthDocumento11 pagineJournal of Religion, Disability & HealthBlondaRobyNessuna valutazione finora
- What Are The Symptoms of Conduct Disorder?Documento5 pagineWhat Are The Symptoms of Conduct Disorder?Jasper TrinidadNessuna valutazione finora