Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Diagnosis and New Treatments in Muscular Dystrophies: Doi: 10.1136/jnnp.2008.158329
Caricato da
anisarahma718Descrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Diagnosis and New Treatments in Muscular Dystrophies: Doi: 10.1136/jnnp.2008.158329
Caricato da
anisarahma718Copyright:
Formati disponibili
Downloaded from jnnp.bmj.com on January 20, 2010 - Published by group.bmj.
com
Diagnosis and new treatments in muscular
dystrophies
A Y Manzur and F Muntoni
J Neurol Neurosurg Psychiatry 2009 80: 706-714
doi: 10.1136/jnnp.2008.158329
Updated information and services can be found at:
http://jnnp.bmj.com/content/80/7/706.full.html
These include:
References
Email alerting
service
Topic collections
This article cites 74 articles, 27 of which can be accessed free at:
http://jnnp.bmj.com/content/80/7/706.full.html#ref-list-1
Receive free email alerts when new articles cite this article. Sign up in the
box at the top right corner of the online article.
Articles on similar topics can be found in the following collections
Genetics (1215 articles)
Muscle disease (1306 articles)
Neuromuscular disease (8310 articles)
Musculoskeletal syndromes (16668 articles)
Notes
To order reprints of this article go to:
http://jnnp.bmj.com/cgi/reprintform
To subscribe to Journal of Neurology, Neurosurgery & Psychiatry go to:
http://jnnp.bmj.com/subscriptions
Downloaded from jnnp.bmj.com on January 20, 2010 - Published by group.bmj.com
Review
Diagnosis and new treatments in muscular
dystrophies
A Y Manzur, F Muntoni
Dubowitz Neuromuscular
Centre, Department of Paediatric
Neurology, Great Ormond Street
Hospital for Children & Institute
of Child Health, London, UK
Correspondence to:
Dr A Y Manzur, Dubowitz
Neuromuscular Centre,
Department of Paediatric
Neurology, Great Ormond Street
Hospital for Children & Institute
of Child Health, London WC1N
3JH, UK; manzua@gosh.nhs.uk
Received 3 February 2009
Revised 10 March 2009
Accepted 14 March 2009
ABSTRACT
Duchenne muscular dystrophy (DMD), Becker muscular
dystrophy (BMD) and limb girdle muscular dystrophies
(LGMD) represent a significant proportion of paediatric
and adult neuromuscular neurology practice. The proactive symptom-based multidisciplinary team (MDT) management and access to non-invasive ventilation have
enabled improved survival into adulthood. Nevertheless
the severe disability imposed by conditions such as DMD
poses a challenge for successful transition of care and
management for paediatric and adult neurology teams.
DMD is discussed in detail as a paradigm illustrating
diagnosis, management and role for different pharmacological interventions to improve survival, but also
challenges in adulthood care, and cutting-edge therapies.
LGMDs are much rarer than DMD and BMD, and in
addition there is a significant genetic and clinical
heterogeneity, which leads to diagnostic difficulties. The
clinical and laboratory diagnostic features of seven LGMD
subtypes are summarised, and their allelic non-limb
girdle phenotypes are tabulated to illustrate the theme
of one gene causing multiple clinical phenotypes, with
the aim of refining the clinicians diagnostic approach.
The lessons learnt from DMD MDT management to
improve survival are broadly applicable to LGMDs with
severe motor disability/multisystem complications.
The muscular dystrophies are an inherited group of
disorders characterised by muscle wasting and
weakness, and sharing common histological features of dystrophic muscle biopsy changes,
including variation in muscle fibre size, muscle
fibre degeneration and regeneration, and replacement of muscle by connective tissue and fat. The
clinical and genetic heterogeneity of these conditions is well recognised: some have prenatal onset,
while others affect only adults, some are rapidly
progressive, while others are associated with prolong periods of stability; some are associated with
multisystem involvement including cardiac and
central nervous system. The major advances over
the last two decades have improved diagnostic
precision and focused symptomatic management
and are increasingly leading to development of
cutting-edge therapies.
This review article focuses on Duchenne muscular dystrophy (DMD), Becker muscular dystrophy (BMD) and limb girdle muscular dystrophies
(LGMD), emphasising diagnosis and new treatments from the clinicians viewpoint, and in
particular, the presentations and complications in
the adolescent, and early adulthood.
DMD is discussed in detail as a paradigm
illustrating diagnosis, the impact of presently
available symptomatic managements on survival,
706
challenges in adolescent and young adulthood care,
and genetic-based therapeutic interventions.
DUCHENNE MUSCULAR DYSTROPHY
DMD is the most frequent muscular dystrophy
variant, affecting one in every 3500 live male
births. Common presentation is with abnormal
gait, calf hypertrophy and difficulty in rising from
the floor between 2 and 5 years of age; speech/
global developmental delay may dominate the
presentation in a minority of cases.1 2 Untreated,
progression of muscle weakness leads to complete
wheelchair dependence by the 13th birthday,
followed by scoliosis, respiratory insufficiency,
cardiomyopathy and death in the late teens or
early twenties. Feeding difficulties and weight loss
are common in the late stages of the disease.
Though a curative treatment is not yet available,
the multidisciplinary team (MDT) proactive
approach3 for optimal surveillance and management of multisystem complications together with
pharmacological intervention with corticosteroids
has altered the natural history of DMD, so that
most of these individuals can now be anticipated
to survive into adulthood, with transfer of care to
the adult neurologists.
GENETICS AND PATHOPHYSIOLOGY
A brief review of the molecular genetic basis of
DMD is essential to understand the approach to
diagnosis and limitations of the various diagnostic
techniques. DMD is caused by mutations in the
dystrophin gene at Xp21. The dystrophin locus
contains 85 exons and encodes for a large but low
abundance
protein,
named
dystrophin.4
Dystrophin is a rod-shaped protein, which localises
at the cytoplasmic side of the sarcolemma: the
carboxyl-terminal end binds to the dystrophin
associated glycoprotein complex at the sarcolemma, while the aminoterminal end binds to the
cytoskeletal actin. Dystrophin is postulated to be
essential for protection of the sarcolemma from the
stress of repeated contractions by providing an
indirect link between the subsarcolemmal cytoskeletal actin and the intermediate filaments in the
muscle fibre with the extracellular matrix. Other
functions in the control of signalling molecules
such as neuronal nitric oxide synthase and
intracytoplasmic calcium homeostasis are also
postulated. The mutations in the dystrophin gene,
which result in DMD, cause disruption of the
reading frame, resulting in a severe reduction or
absence of dystrophin in the skeletal and cardiac
muscle. This in turn leads to increased intracytoplasmatic calcium content, followed by muscle
fibre damage and degeneration. Several dystrophin
J Neurol Neurosurg Psychiatry 2009;80:706714. doi:10.1136/jnnp.2008.158329
Only two pages have been converted.
Please go to https://pdfburger.com and sign up to convert all pages.
Potrebbero piacerti anche
- Neuroimmunology: Multiple Sclerosis, Autoimmune Neurology and Related DiseasesDa EverandNeuroimmunology: Multiple Sclerosis, Autoimmune Neurology and Related DiseasesAmanda L. PiquetNessuna valutazione finora
- Multiple Sclerosis: Practical Comprehensive EssentialsDa EverandMultiple Sclerosis: Practical Comprehensive EssentialsNessuna valutazione finora
- Willmann Mammalian Animal Models For Duchenne Muscular Dystrophy 2009Documento9 pagineWillmann Mammalian Animal Models For Duchenne Muscular Dystrophy 2009vidyasagarsNessuna valutazione finora
- Gao 2015Documento17 pagineGao 2015saherrodriguezNessuna valutazione finora
- Lamperti 2010Documento10 pagineLamperti 2010Marina GomesNessuna valutazione finora
- Distrofia Muscular de Duchenne: Actualidad y Perspectivas de Tratamiento SENSE OF SMELL, Physiological Ageing An..Documento8 pagineDistrofia Muscular de Duchenne: Actualidad y Perspectivas de Tratamiento SENSE OF SMELL, Physiological Ageing An..Anibal SalazarNessuna valutazione finora
- Assessing The Use of The SGC Stimulator BAY-747, As A Potential Treatment For Duchenne Muscular DystrophyDocumento19 pagineAssessing The Use of The SGC Stimulator BAY-747, As A Potential Treatment For Duchenne Muscular Dystrophybose21Nessuna valutazione finora
- Molecules: Duchenne Muscular Dystrophy: From Diagnosis To TherapyDocumento17 pagineMolecules: Duchenne Muscular Dystrophy: From Diagnosis To TherapyzzooooeeeeeeNessuna valutazione finora
- The DMD Gene and Therapeutic Approaches To Restore - 2021 - Neuromuscular DisorDocumento8 pagineThe DMD Gene and Therapeutic Approaches To Restore - 2021 - Neuromuscular DisorSuzie Simone Mardones SilvaNessuna valutazione finora
- Becker Muscular DystrophyDocumento9 pagineBecker Muscular DystrophyManusama HasanNessuna valutazione finora
- Myopathies: DMD, BMD, FSHDocumento15 pagineMyopathies: DMD, BMD, FSHLeica Mae CalooyNessuna valutazione finora
- Ayurvedic Treatment of Muscular DystrophyDocumento9 pagineAyurvedic Treatment of Muscular DystrophyMukesh JainNessuna valutazione finora
- New Developments in Diagnosis, Treatment, and Management of Duchenne Muscular DystrophyDocumento14 pagineNew Developments in Diagnosis, Treatment, and Management of Duchenne Muscular DystrophyRooh UllahNessuna valutazione finora
- Assignment/ TugasanDocumento16 pagineAssignment/ TugasanfaezNessuna valutazione finora
- Ijms 22 05654Documento22 pagineIjms 22 05654Alber AvendañoNessuna valutazione finora
- 18.actualización en Distrofias MuscularesDocumento12 pagine18.actualización en Distrofias MuscularesLizeth LorancaNessuna valutazione finora
- Complexity of Skeletal Muscle Degeneration Multi Systems Pathophysiology and Organ Crosstalk in DystrophinopathyDocumento27 pagineComplexity of Skeletal Muscle Degeneration Multi Systems Pathophysiology and Organ Crosstalk in Dystrophinopathybose21Nessuna valutazione finora
- Endocrinopathies Are Now Well Recognized. These Include Myopathies Associated With ThyroidDocumento10 pagineEndocrinopathies Are Now Well Recognized. These Include Myopathies Associated With ThyroidTeves AdrianNessuna valutazione finora
- Iannitti Et Al., 2010Documento21 pagineIannitti Et Al., 2010Tommaso IannittiNessuna valutazione finora
- The Multidisciplinary Management of Duchenne Muscular DystrophyDocumento22 pagineThe Multidisciplinary Management of Duchenne Muscular DystrophyranihentynovitaNessuna valutazione finora
- DYSTROPHYDocumento15 pagineDYSTROPHYleeyan2wenty6Nessuna valutazione finora
- NDT 12 1795 PDFDocumento13 pagineNDT 12 1795 PDFAdrian KhomanNessuna valutazione finora
- Muscular Dystrophy and Its Ayurvedic PerspectivesDocumento149 pagineMuscular Dystrophy and Its Ayurvedic PerspectivesMuktha ShenoyNessuna valutazione finora
- Neuromuscular Diseases PDFDocumento205 pagineNeuromuscular Diseases PDFsalmazzNessuna valutazione finora
- Read-Through Approach For Stop Mutations in Duchenne Muscular Dystrophy. An UpdateDocumento8 pagineRead-Through Approach For Stop Mutations in Duchenne Muscular Dystrophy. An UpdateL ANessuna valutazione finora
- ATROFIA MUSCULAR ESPINAL Lancet 2008Documento14 pagineATROFIA MUSCULAR ESPINAL Lancet 2008Sebastián Silva SotoNessuna valutazione finora
- Neuromuscular DisordersDocumento3 pagineNeuromuscular Disordersapi-321778954Nessuna valutazione finora
- Term Paper Duchenne Muscular DystrophyDocumento7 pagineTerm Paper Duchenne Muscular Dystrophyafmzbufoeifoof100% (1)
- Muscular DystrophyDocumento89 pagineMuscular Dystrophyvijay1234568883Nessuna valutazione finora
- CaseDocumento7 pagineCaseEka NurjannahNessuna valutazione finora
- Advanced PhysiotherapyDocumento15 pagineAdvanced PhysiotherapyJhon AlefeNessuna valutazione finora
- Agingwithmuscular Dystrophy: Pathophysiologyand ClinicalmanagementDocumento22 pagineAgingwithmuscular Dystrophy: Pathophysiologyand ClinicalmanagementDeborah SalinasNessuna valutazione finora
- DuchenneDocumento13 pagineDuchennejenika studiesNessuna valutazione finora
- Part 25: Muscle Chapter 216: The Muscular DystrophiesDocumento73 paginePart 25: Muscle Chapter 216: The Muscular DystrophiesVane100% (1)
- Neuromuscular DiseaseDocumento69 pagineNeuromuscular DiseaseDevi SiswaniNessuna valutazione finora
- Distrofia Muscular - DUCHENNEDocumento4 pagineDistrofia Muscular - DUCHENNEMariano RamisNessuna valutazione finora
- Skeletal MuscleDocumento11 pagineSkeletal MuscleStefania CristinaNessuna valutazione finora
- Primary Mitochondrial Myopathies in Childhood 2021 Neuromuscular DisordersDocumento10 paginePrimary Mitochondrial Myopathies in Childhood 2021 Neuromuscular DisordersSuzie Simone Mardones SilvaNessuna valutazione finora
- Narayanaswami 2014Documento13 pagineNarayanaswami 2014tuliocsgNessuna valutazione finora
- Atualização NeuromuscularDocumento5 pagineAtualização NeuromuscularRodrigo VanzelliNessuna valutazione finora
- Zaman Muscle PathologyDocumento14 pagineZaman Muscle PathologyartikslennonNessuna valutazione finora
- Duchenne Muscular Dystrophy: Current Cell Therapies: Therapeutic Advances in Neurological Disorders ReviewDocumento12 pagineDuchenne Muscular Dystrophy: Current Cell Therapies: Therapeutic Advances in Neurological Disorders ReviewFajri MuhammadNessuna valutazione finora
- Duchenne Muscular Dystrophy: June 2014Documento6 pagineDuchenne Muscular Dystrophy: June 2014Beta Yunita PNessuna valutazione finora
- 60 Rathod EtalDocumento3 pagine60 Rathod EtaleditorijmrhsNessuna valutazione finora
- LGMDDocumento10 pagineLGMDidno1008Nessuna valutazione finora
- Demyelination Lesion Spine NeuroradiologyDocumento25 pagineDemyelination Lesion Spine NeuroradiologylauraalvisNessuna valutazione finora
- Myotonic Dystrophy - Etiology, Clinical Features, and Diagnosis - Uptodate FreeDocumento49 pagineMyotonic Dystrophy - Etiology, Clinical Features, and Diagnosis - Uptodate FreekpajouhtNessuna valutazione finora
- Mitochondrial Myopathies - Clinical Features and Diagnosis - UpToDateDocumento37 pagineMitochondrial Myopathies - Clinical Features and Diagnosis - UpToDateNana ShkodinaNessuna valutazione finora
- Muscular Dystrophy (MD) Is A Group ofDocumento4 pagineMuscular Dystrophy (MD) Is A Group ofbettyNessuna valutazione finora
- Afect .NeuromusculareDocumento33 pagineAfect .NeuromusculareAloexandru All IonNessuna valutazione finora
- Duchenne Muscular Dystrophy: Marek Michalak, Michal OpasDocumento5 pagineDuchenne Muscular Dystrophy: Marek Michalak, Michal OpasZurezki Yuana YafieNessuna valutazione finora
- Current and Emerging Treatment Strategies For Duchenne Muscular DystrophyDocumento14 pagineCurrent and Emerging Treatment Strategies For Duchenne Muscular DystrophyANAMIKA ANANDINessuna valutazione finora
- Myotonic Dystrophy - Treatment and Prognosis - Uptodate FreeDocumento32 pagineMyotonic Dystrophy - Treatment and Prognosis - Uptodate FreekpajouhtNessuna valutazione finora
- Mitochondrial Disorders Overview - GeneReviews® - NCBI Bookshelf HTTPSWWW - Ncbi.nlm - nih.govbooksNBK1224Documento24 pagineMitochondrial Disorders Overview - GeneReviews® - NCBI Bookshelf HTTPSWWW - Ncbi.nlm - nih.govbooksNBK1224denisaNessuna valutazione finora
- Type Gene Description: Becker's Muscular Dystrophy Duchenne Muscular Dystrophy DystrophinDocumento4 pagineType Gene Description: Becker's Muscular Dystrophy Duchenne Muscular Dystrophy DystrophinNikhilKapoorNessuna valutazione finora
- Muscular DystrophyDocumento554 pagineMuscular DystrophyJosé RamírezNessuna valutazione finora
- Full Book Intech DMD May 2012 Chapter Page 349Documento554 pagineFull Book Intech DMD May 2012 Chapter Page 349Tommaso IannittiNessuna valutazione finora
- Duchenne Muscular Dystrophy Information SheetDocumento2 pagineDuchenne Muscular Dystrophy Information Sheetapi-319448388Nessuna valutazione finora
- Abdul-Razak Et Al. 2016 - DMD Gene TherapyDocumento7 pagineAbdul-Razak Et Al. 2016 - DMD Gene TherapyVassili CrispiNessuna valutazione finora
- Living with MS: A Comprehensive Guide for Patients and FamiliesDa EverandLiving with MS: A Comprehensive Guide for Patients and FamiliesNessuna valutazione finora
- Rekap Data Kehadiran Okt 23Documento5 pagineRekap Data Kehadiran Okt 23anisarahma718Nessuna valutazione finora
- 25 OS OD: Progression of Diabetic Retinopathy in The Hypertension Intervention Nurse Telemedicine StudyDocumento2 pagine25 OS OD: Progression of Diabetic Retinopathy in The Hypertension Intervention Nurse Telemedicine Studyanisarahma718Nessuna valutazione finora
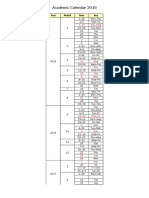
- 2016 Undergraduate Academic ScheduleDocumento4 pagine2016 Undergraduate Academic Scheduleanisarahma718Nessuna valutazione finora
- 050906A Nurse Led Approach To Diabetic Retinal Screening 2Documento3 pagine050906A Nurse Led Approach To Diabetic Retinal Screening 2anisarahma718Nessuna valutazione finora
- Scabies GuidelineJanuary 2013Documento13 pagineScabies GuidelineJanuary 2013anisarahma718Nessuna valutazione finora
- Personal HygieneDocumento2 paginePersonal Hygieneanisarahma718Nessuna valutazione finora
- Reference 5Documento4 pagineReference 5anisarahma718Nessuna valutazione finora
- Top10ReasonsToUseIVUS PDFDocumento71 pagineTop10ReasonsToUseIVUS PDFDiana PânteaNessuna valutazione finora
- Pulpotomy Pediatric Prevention Diagnosis Treatment PlanningDocumento122 paginePulpotomy Pediatric Prevention Diagnosis Treatment PlanningTamara Nitya ArianiNessuna valutazione finora
- What Is An Ear InfectionDocumento4 pagineWhat Is An Ear Infectionapi-236387116Nessuna valutazione finora
- Kertas Kerja Program Sayangkan KitaDocumento5 pagineKertas Kerja Program Sayangkan Kitaaknb2702Nessuna valutazione finora
- Sci-Doku Chips LongDocumento4 pagineSci-Doku Chips LongDave Remerata100% (2)
- Classic Radiology SignsDocumento9 pagineClassic Radiology SignsJui DirDapNessuna valutazione finora
- List of Top Level Categories: CHAPTER 01 Certain Infectious or Parasitic DiseasesDocumento148 pagineList of Top Level Categories: CHAPTER 01 Certain Infectious or Parasitic Diseasesျပည္ စိုးNessuna valutazione finora
- Reference: Maglumi TSH (Clia)Documento5 pagineReference: Maglumi TSH (Clia)Lidia NarbNessuna valutazione finora
- Albumin Drug StudyDocumento1 paginaAlbumin Drug StudyMaine Concepcion100% (1)
- HSV1 HSV2 R-Gene & VZV R-GeneDocumento2 pagineHSV1 HSV2 R-Gene & VZV R-GeneSachinNessuna valutazione finora
- Causes of InflammationDocumento1 paginaCauses of InflammationZainab KhanNessuna valutazione finora
- He Grade 7 Jss Revision.Documento28 pagineHe Grade 7 Jss Revision.nyabinge silvesterNessuna valutazione finora
- PyelonephritisDocumento10 paginePyelonephritisalina abu rumi100% (1)
- Heparin - ClinicalKeyDocumento85 pagineHeparin - ClinicalKeydayannaNessuna valutazione finora
- Eye Docs GlaucomaDocumento147 pagineEye Docs GlaucomaMuneeb ShahzadNessuna valutazione finora
- Module 3 A PresentationDocumento79 pagineModule 3 A PresentationMelinda FiskaNessuna valutazione finora
- B Blab 6 Crossmatch SP 05Documento14 pagineB Blab 6 Crossmatch SP 05Rutchelle Joyce PugoyNessuna valutazione finora
- Parapat: Jalan Kolonel T.P.R.Sinagatelp. (0625-41332)Documento3 pagineParapat: Jalan Kolonel T.P.R.Sinagatelp. (0625-41332)Odelie KerinciNessuna valutazione finora
- Hemorrhage PathophysiologyDocumento3 pagineHemorrhage PathophysiologyJubelle Sipalay0% (1)
- Intracellular AccumulationsDocumento19 pagineIntracellular AccumulationsWajiha106Nessuna valutazione finora
- Small Animal Surgery Internship - Proposed Program Description (2021)Documento4 pagineSmall Animal Surgery Internship - Proposed Program Description (2021)Shubham HarishNessuna valutazione finora
- Perspectives in Clinical Gastroenterology and Hepatology: A Gastroenterologist's Guide To ProbioticsDocumento9 paginePerspectives in Clinical Gastroenterology and Hepatology: A Gastroenterologist's Guide To ProbioticsMihajilo TosicNessuna valutazione finora
- COURSE OBJECTIVES or NursingDocumento5 pagineCOURSE OBJECTIVES or NursingFil AquinoNessuna valutazione finora
- Safety Data Sheet: Section 1. Chemical Product and Company IdentificationDocumento17 pagineSafety Data Sheet: Section 1. Chemical Product and Company IdentificationEngr Qaisar NazeerNessuna valutazione finora
- InTech-Yamamoto New Scalp Acupuncture Ynsa Development Principles Safety Effectiveness and Clinical ApplicationsDocumento17 pagineInTech-Yamamoto New Scalp Acupuncture Ynsa Development Principles Safety Effectiveness and Clinical Applicationsdasamoro100% (3)
- Local AnestheticsDocumento47 pagineLocal AnestheticsKeerthi LakshmiNessuna valutazione finora
- Allergies or Food Intolerances.: Therapeutic DietDocumento3 pagineAllergies or Food Intolerances.: Therapeutic DietBryan Mae H. DegorioNessuna valutazione finora
- Behandlingstudier - Overblik Over Planlagte Og Igangværende Studier Af Lægemidler Til Behandling Af COVID-19Documento217 pagineBehandlingstudier - Overblik Over Planlagte Og Igangværende Studier Af Lægemidler Til Behandling Af COVID-19Ishan ShahNessuna valutazione finora
- Essential NB Care Checklist 2020 3Documento2 pagineEssential NB Care Checklist 2020 3karenbescaserNessuna valutazione finora
- A Case of Paediatric CholelithiasisDocumento4 pagineA Case of Paediatric CholelithiasisHomoeopathic PulseNessuna valutazione finora