Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Diabetes Self Management
Caricato da
Rizky BangkitTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Diabetes Self Management
Caricato da
Rizky BangkitCopyright:
Formati disponibili
University of Warwick institutional repository: http://go.warwick.ac.
uk/wrap
This paper is made available online in accordance with
publisher policies. Please scroll down to view the document
itself. Please refer to the repository record for this item and our
policy information available from the repository home page for
further information.
To see the final version of this paper please visit the publishers website.
Access to the published version may require a subscription.
Author(s): Jackie Sturt , Hilary Hearnshaw and Melanie Wakelin
Article Title: Validity and reliability of the DMSES UK: a measure of
self-efficacy for type 2 diabetes self-management
Year of publication: 2009
Link to published article: http://dx.doi.org/
10.1017/S1463423610000101
Publisher statement: Cambridge University Press 2009. Sturt, J. et
al. 2009. Validity and reliability of the DMSES UK: a measure of selfefficacy for type 2 diabetes self-management. Primary Health Care
Research & Development, June 2010
Primary Health Care Research & Development page 1 of 8
doi:10.1017/S1463423610000101
RESEARCH
Validity and reliability of the DMSES UK: a
measure of self-efficacy for type 2 diabetes
self-management
Jackie Sturt1, Hilary Hearnshaw1 and Melanie Wakelin2
1
Health Sciences Research Institute, Warwick Medical School, University of Warwick, Coventry CV4 7AL, UK
Statistical Consultant, Wakelin Statistical Services, 42 Tailors, Bishops Stortford, Hertfordshire, UK
Objectives: Self-efficacy is an important outcome measure of self-management
interventions. We aimed to establish UK validity and reliability of the diabetes management self-efficacy scale (DMSES). Methods: The 20 item DMSES was available for
Dutch and US populations. Consultation with people with type 2 diabetes and health
professionals established UK content and face validity resulting in item reduction to
15. Participants were adults with type 2 diabetes enrolled in a randomised controlled
trial (RCT) of the diabetes manual, a self-management education intervention, with an
HbA1c over 7% and who understood English. Baseline trial data and follow-up control
group data were used. Results: A total of 175 participants completed all 15 items.
Pearsons correlation coefficient of 20.46 (P , 0.0001) between the DMSES UK and the
problem areas in diabetes scale demonstrated criterion validity. Intra-class correlation
between data from 67 of these participants was 0.77, demonstrating test-retest reliability. The correlation coefficients between item scores and total scores were .0.30.
Cronbachs alpha was 0.89 over all items. Conclusion: This evaluation demonstrates
that the scale has good internal reliability, internal consistency, construct validity,
criterion validity, and test-retest reliability. Practice Implications: The 15 item
DMSES UK is suitable for use in research and clinical settings to measure the selfefficacy of people living with type 2 diabetes in managing their diabetes.
Key words: diabetes; outcome measure; self-efficacy; self-management
Received 11 November 2009; accepted 10 March 2010
Introduction
International and UK health policy have developed standards stating that people with diabetes
should be empowered and supported to participate in decision-making and self-management to
optimise the control of blood glucose, blood
pressure, and other risk factors for developing the
complications of diabetes (Department of Health,
2002; 2005; International Diabetes Federation,
2003). This marks a shift in the treatment of those
Correspondence to: Jackie Sturt, Health Sciences Research
Institute, Warwick Medical School, University of Warwick,
Coventry CV4 7AL, UK. Email: jackie.sturt@warwick.ac.uk
r Cambridge University Press 2010
with chronic diseases away from health-care
professional management towards ensuring that
patients are enabled to self-manage their health
effectively and engage in active partnership with
health professionals. One of the dominant concepts in the literature on supporting self-management is that of self-efficacy (Day et al., 1997;
Norris et al., 2001; Guevara et al., 2003).
Perceived self-efficacy is a reliable predictor of
behaviour initiation (Bandura, 1977; Gillis, 1993).
It demonstrates its value as the cornerstone of
effective chronic disease self-management through
its increasing use as a self-management research
outcome measure (Lorig et al., 1999; Farmer et al.,
2005; Sturt et al., 2006a; 2006b; Davies et al., 2008).
2 Jackie Sturt, Hilary Hearnshaw and Melanie Wakelin
Perceived self-efficacy is defined as an individuals
perceptions or beliefs about their capabilities to
undertake certain activities (Bandura, 1994). It
influences how they think, feel, become motivated
and behave. People with strong perceptions of
their personal efficacy approach difficult tasks as
challenges to be mastered; they set themselves
challenging goals and maintain strong commitment
to them. In the face of failure they increase their
efforts and rapidly recover their self-efficacy after
setbacks. This efficacious outlook produces personal accomplishments, reduces stress, and lowers
vulnerability to depression. In contrast, people who
doubt their capabilities avoid difficult tasks, they
have low aspirations and weak commitment to
their chosen goals. When faced with difficult tasks,
they dwell on their personal deficiencies and on the
obstacles and their efforts weaken in the face of
these challenges. Individuals with low perceptions
of efficacy are vulnerable to stress and depression
(Bandura, 1994). Self-efficacy is often communicated to lay audiences, for example, in research
measures, as degree of confidence although this is
not technically accurate and Bandura does describe
important differences between confidence and selfefficacy in his web site (http://www.des.emory.edu/
mfp/self-efficacy.html).
Self-efficacy is supported in four ways (in order
of influence): personal mastery experiences,
vicarious (or peer) experiences, emotional state,
and verbal encouragement and it offers a framework for enabling health-care professionals to
guide people towards experiences that will
strengthen their self-efficacy (Bandura, 1977).
Measurement of perceived self-efficacy is behaviour-specific and measurement predicts the
likelihood that an individual will engage in a
behaviour, the degree to which they will persist
and overcome obstacles, and their ultimate success in maintaining behaviour in the longer term
(Bandura, 1977; Sentcal et al., 2000; Sniehotta
et al., 2005). However, measurement is complicated by the lack of generalisability of self-efficacy
between types of behaviour, for example, stopping
smoking and increasing physical activity. Attempts
to develop measures across different behaviour
types have limited usefulness (Bandura, 1997;
2006). Scales to measure perceived self-efficacy
must, therefore, be highly specific to the behaviour or activity of interest, such as aspects of selfmanagement in diabetes.
Diabetes is a complex metabolic condition
requiring high levels of self-efficacy to perform
the many facets of self-management required
for blood glucose control, and hence prevention
of complications. Diabetes self-efficacy measurement scales currently available provide good
psychometric validity for the measurement of
psychosocial aspects of living with diabetes, of
self-management for people with type 1 diabetes,
and for type 2 diabetes self-management for
Dutch/US and Australian populations (Bijl et al.,
1999; Anderson et al., 2000; Van Der Ven et al.,
2003; McDowell et al., 2005). The Dutch/US scale
assesses behavioural aspects of type 2 diabetes
self-management and had the potential to offer a
strongly aligned outcome measure for the type 2
diabetes patient education and self-management
intervention studies that we were designing and
which were strongly influenced by self-efficacy
theory. Scale items assess self-efficacy for performing a range of self-management activities
that will influence blood glucose control including
managing healthy eating and monitoring skin
integrity of the feet (Bijl et al., 1999). A scale for
measuring perceived self-efficacy, validated for
use with a UK population, focusing on diabetesspecific self-management activities would offer a
tool for researchers and clinicians to evaluate
progress towards meeting the UK Diabetes
National Service Framework standards.
The aim of this paper is to present the evaluation of aspects of the validity and reliability of
an adapted version of the Dutch/US diabetes
management self-efficacy scale (DMSES) as a
measure of perceived self-efficacy in relation to
the management of diabetes in patients with type
2 diabetes, in the UK population.
Methods
Adaptation of the Dutch/US DMSES
The 20-item Dutch/US DMSES measures the
individuals efficacy expectations for engaging in
20 type 2 diabetes self-management activities, for
example, taking daily exercise, keeping to a healthy
eating plan when away from home (Bijl et al., 1999).
The scale is scored according to a 15 point numerical scale indicating the level of efficacy expectation
the respondent has for each item with higher
scores indicating greater levels of self-efficacy.
Validity and reliability of the DMSES UK scale 3
The Dutch/US evaluation of the DMSES covered
content and construct validity, internal consistency,
and temporal stability. That process, involving a
panel of experts within diabetes and self-efficacy,
resulted in the reduction of an original 42-item
scale to 20 items. The DMSES was translated from
Dutch to US English as part of the scale development work. The construct validity of the scale was
demonstrated through the findings of a positive
relationship in a second, US-based study, testing
the relationship between the self-efficacy scores of
individuals living with diabetes and the self-efficacy
scores of their significant other for supporting and
assisting them in the 20 self-management activities,
for example, How confident are you that you could
support and assist your significant other in choosing
the correct foods (Shortridge-Bagget and van der
Bijl, 2002).
Assessing face validity
Face validation of a DMSES for the UK started
by consulting with the Warwick Diabetes Research
& Education User Group (WDREUG), a lay
advisory group of 1012 people living with diabetes,
during two meetings over six months (Lindenmeyer
et al., 2007). The WDREUG provided advice to
ensure appropriate use of vocabulary (eg, blood
glucose monitoring) and concepts (eg, confidence),
which resulted in changes made to items, for
example, diabetic diet was replaced by healthy
eating pattern. Following WDREUG consultation
and with regard to the literature (Donaldson, 2003)
the stem phrase I am confident that y was used
to precede each item in the 20-item DMSES UK.
The 20 UK items are described in Table 1.
The five-point response scale used in the
Dutch/US DMSES has a poorer predictive capacity than a 0 to 10-point scale (Pajares et al.,
2001). The DMSES UK incorporated an 11-point
010 scale reflecting Banduras thesis (Bandura,
2006). The WDREUG advised on the anchor
point terms used in the scale, which were as follows; 01 Cannot do at all, 4/5 Maybe yes maybe
no, 9/10 Certain can do. The centre anchor point
recommended by Bandura is moderately certain
can do. The WDREUG felt this was ambiguous
and using Maybe yes, maybe no enabled a
responder to judge their certainty based on a
collective experience of their perceived confidence for a particular behaviour, indicating that
Table 1 Initial version of the DMSES UK with 20 items
I am confident that
1 I am able to check my blood/urine sugar if necessary
2 I am able to correct my blood sugar when the sugar
level is too high
3 I am able to correct my blood sugar when the blood
sugar level is too low
4 I am able to choose the correct food
5 I am able to choose different foods and stick to a
healthy eating pattern
6 I am able to keep my weight under control
7 I am able to examine my feet for cuts
8 I am able to take enough exercise, for example,
walking the dog or riding a bicycle
9 I am able to adjust my eating plan when ill
10 I am able to follow a healthy eating pattern most of
the time
11 I am able to take more exercise if the doctor advises
me to
12 When taking more exercise I am able to adjust my
eating plan
13 I am able to follow a healthy eating pattern when I
am away from home
14 I am able to adjust my eating plan when I am away
from home
15 I am able to follow a healthy eating pattern when I
am on holiday
16 I am able to follow a healthy eating pattern when I
am eating out or at a party
17 I am able to adjust my eating plan when I am feeling
stressed or anxious
18 I am able to visit my doctor once a year to monitor
my diabetes
19 I am able to take my medication as prescribed
20 I am able to adjust my medication when I am ill
DMSES 5 diabetes management self-efficacy scale.
some days they might be more confident than
others. The scale instructions were determined with
reference to Banduras guidance on the construction of self-efficacy scales and with regard to the
opinions of the users (Bandura, 1997). The scale
was intended for self-completion, in private, so clear
instructions were an important aspect of the scale.
The Flesch reading ease score (tool available in
Microsoft Office Word) for the DMSES UK was
assessed as 82.9% or grade 2.6 equivalent to a
reading age of seven to eight years, and therefore
appropriate. This process of consultation in adapting the scale established high-face validity.
Assessing content validity
Once face validity was established we amended
the DMSES and content validity was assessed
4 Jackie Sturt, Hilary Hearnshaw and Melanie Wakelin
Table 2 Redundant items from initial 20-item DMSES UK
Item Reason for redundancy
5
14
15
18
Item 5 (concerning choice and adherence) is an
amalgamation of item 4 (concerning choice) and
item 10 (concerning adherence), indicating limited
value
Item 8 wording enough exercise is a subjective
and interpretive question whereas adherence to
doctor advice (item 11) is an appropriate selfmanagement activity for type 2 diabetes. Item 11
therefore retained
Item meaning was closely related to item 13 and
offered no additional challenge in relation to type 2
diabetes. Respondents were unable to distinguish
between healthy eating pattern and eating plan
supporting the removal of item 14
Being on holiday is a subset of being away from
home and respondents were unable to distinguish
between items 13 and 15. Respondents were
unable to distinguish between healthy eating
pattern and eating plan. The removal of item 15
removed the duplication
Access to annual GP care in the UK is a relatively
certain activity and suggests that item 18 does not
lend itself to Likert scale measurement. This item
was removed
DMSES 5 diabetes management self-efficacy scale.
with both people living with type 2 diabetes
and with diabetes health-care professionals. Thirty
individuals attending two lay diabetes events in
2003, volunteered to complete the 20-item DMSES
UK with the available support of a researcher (JS/
HH). During completion the volunteers with type 2
diabetes identified duplications and ambiguities in
the scale, which were recorded in field notes. This
process confirmed the views of the WDREUG.
Health professionals undergoing continuing
professional development in diabetes care at the
Warwick Medical School were also consulted on
the validity of the constructs. Group discussions
were held with three cohorts of professionals,
approximately 20 people per cohort. This revealed
ambiguity around a number of items and some
duplication. The professional and lay consultation
led to the removal of five items from the DMSES
UK. Two items were ambiguous (items 8,18) and
three involved duplicate items or elements of
items (items 5,14,15) (Table 2). The health professionals confirmed that the scale content was
sufficiently broad to cover the salient and challenging aspects of self-managing type 2 diabetes
giving high content validity. The face and content
validity of the DMSES UK was determined to be
of sufficient strength for the revised 15 item scale
to undergo further psychometric evaluation.
Diabetes manual randomised controlled trial
(RCT) and participants
Evaluation of the criterion and construct validity
and the reliability of the DMSES UK was undertaken using data from the cluster randomised trial of
the Diabetes Manual, a structured education programme for type 2 diabetes undertaken from 2005
to 2007 (Sturt et al., 2006a; 2006b; 2008). RCT participants were 245 people with type 2 diabetes resident across the West Midlands, UK. All participants
were recruited from primary care and randomised
to receive the diabetes manual intervention or a sixmonth deferred intervention. The diabetes manual is
a self-management and structured education programme to be used by practice nurses and patients
on a one to one basis. It consists of two-day facilitator training for the nurse, a patient workbook
for recommended completion over three months, a
frequently asked questions CD, a relaxation CD, and
three nurse-delivered telephone support calls. The
aim of the intervention is to strengthen the patients
self-efficacy by developing skills and confidence in
managing their diabetes, quickly, and progressively.
The intervention is theoretically underpinned by
self-efficacy theory (Bandura, 1977).
RCT outcome measures
Baseline data were collected from 245 participants before randomisation and consisted of
HbA1c as the primary outcome and completion
of a six-page questionnaire including the 15 item
DMSES UK, the 20 item problem areas in diabetes (PAID) scale (Polonsky et al., 1995), and
10 demographic questions. The PAID scale is a
20-item measure of diabetes-specific emotional
distress; with a maximum score of 100 and higher
scores indicting greater emotional distress. The
maximum score on the DMSES UK is 150 with
higher scores indicating higher self-efficacy. Since
higher self-efficacy is related to lower emotional
distress (Fisher et al., 2007) a strong correlation
between low PAID scores (a gold standard),
indicating low distress, and high scores on the
DMSES UK, indicating high self-efficacy, would
indicate criterion validity. Two hundred and
Validity and reliability of the DMSES UK scale 5
thirty-two (95%) randomised participants completed some elements of the questionnaire, of
whom 175 (71%) participants responded to all of
the DMSES UK questions. These 175 participants
form the sample used for this psychometric evaluation of the DMSES UK.
At the six-month follow-up for the trial, the sixpage questionnaire was completed again by participants. Within four weeks of that, all control
group patients were sent a repeat questionnaire.
This group was chosen for the test-retest because
they were awaiting the deferred intervention and
could be expected to complete the repeat questionnaire. The repeat questionnaire was returned
by 67 participants.
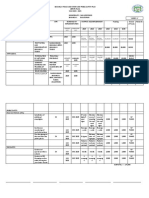
Table 3 Characteristics of participants
Demographic and clinical characteristics of participants
No. of participants
Age median (quartiles)
Gender no (%)
Men
Women
No. of years since diagnosed with
diabetes, no. (%)
,1 year
115 years
.15 years
Median HbA1c % (quartiles)
Mean DMSES score (SD)
Mean PAID score (SD)
175
61 (52, 70)
110 (63%)
65 (37%)
12
155
8
8.5
103
21
(7%)
(89%)
(4%)
(7.6, 9.7)
(27.8)
(15.4)
DMSES 5 diabetes management self-efficacy scale;
PAID 5 problem areas in diabetes.
Results
Patient characteristics
The demographic and clinical characteristics of
the participants who completed the DMSES UK
questions at baseline are summarised in Table 3.
Principal component analysis
Principal components analysis was used to
investigate whether DMSES should be considered as several subscales or as one general
factor. The item coefficients for the first principal
component varied from 0.38 to 0.80 demonstrating that it was indeed a weighted average of all
questions, rather than being dominated by a small
subset of questions. The first principal component
accounted for 41% of the total variance. The
second component accounted for only 11% of the
variance and the third component accounted for
10%. The scree plot (Figure 1) indicates that one
factor was important, confirmed as a weighted
average, supporting the reporting of DMSES as
one overall score.
Internal reliability and internal consistency
The correlation coefficients between item scores
and total scores were all .0.30 (minimum 5
0.34, maximum 5 0.71). Internal consistency was
demonstrated by a Cronbachs alpha of 0.89 over
all 15 items. Internal reliability of DMSES UK was
therefore deemed to be acceptable.
Scree plot for baseline DMSES UK (n=175)
7
6
Eigenvalue
5
4
3
2
1
0
0
Figure 1
6
5
7
8
9 10
Principal Component No.
11
12
13
14
15
Scree plot for baseline diabetes management self-efficacy scale (DMSES UK; n 5 175)
6 Jackie Sturt, Hilary Hearnshaw and Melanie Wakelin
Criterion validity
A Pearsons correlation coefficient of 20.46,
P , 0.0001 was found indicating a negative correlation between DMSES scores and PAID scores.
This demonstrates the criterion validity of the
DMSES, since the PAID is a well established and
validated gold standard scale (Fisher et al., 2007).
Construct validity
A negative correlation between DMSES scores
and HbA1c (Pearsons correlation coefficient
20.21, P 5 0.002) was found. Since higher selfefficacy should lead to greater self-care behaviours resulting in lower blood glucose levels and
ultimately lower HbA1c levels (Fisher et al.,
2007), this demonstrates the construct validity of
the DMSES.
Test-retest reliability
Analysis of test-retest data from 67 participants, who completed the DMSES UK questionnaire twice within a four-week time period,
produced an intra-class correlation of 0.77. This
demonstrates the reliability over time of the
DMSES UK.
Discussion
The results from this evaluation of aspects of the
validity and reliability of DMSES UK, demonstrate that the scale has good internal reliability
and high internal consistency. DMSES UK score
was found to be negatively correlated with both
PAID score and HbA1c. These findings demonstrate the criterion validity and the construct
validity of DMSES UK. Acceptable test-retest
reliability was demonstrated by an intra-class
correlation coefficient of 0.77.
The data were drawn from an intervention
study in which participants consented to a programme of self-management education with some
burden attached. This may represent a different
population from one who were just asked to
complete a single questionnaire on two occasions.
The trial participants were not found to differ
from the eligible participants on any variable
although the low 18.5% RCT response rate indicates that acceptance of burden may have been a
distinguishing feature of our participants (Sturt
et al., 2008). Our participants also had a mean
diabetes distress level of 21 as measured by the
PAID scale at baseline. This compares slightly
lower to typical diabetes out-patient populations
in the USA and Germany where scores in the
range of 2030 were detected (Polonsky et al.,
1995; Welch et al., 2003). These study sample
factors may distort the validity of the findings
were it used on a population not involved in an
intervention trial. One further limitation may be
the anchor points of maybe yes, maybe no which
may confound moderate efficacy with uncertainty.
Given the observed inter-items and inter-scale
correlations, we expect any such confounding to
have been small.
A validation and psychometric evaluation of the
20 item DMSES in an Australian population also
reported some probable redundancy (McDowell et
al., 2005). The authors identified inter-item correlations between items 2/3, 8/11, 13/14, 13/15, and
14/15, which map well onto the items found to be
redundant in the DMSES UK. The DMSES UK
is the first national validation and psychometric
evaluation of the DMSES to have been used as
an outcome measure in RCTs of self-management
interventions (Sturt et al., 2008; Dale et al., 2009).
The DMSES UK has undergone face validation for
use in audio-delivery and symbol self-completion
for Bangladeshi and Pakistani populations resident
within the UK whose main language has no written
form (Lloyd et al., 2008). The psychometric evaluation of the DMSES UK now enables confident
use of the Sylheti and Mirpuri DMSES UK scales
in diabetes self-management intervention studies
for these South Asian populations vulnerable to
diabetes and its consequences.
Conclusions
The DMSES UK is available as a measure of
diabetes management self-efficacy for both clinical and research use. The predictive reliability
of self-efficacy means that the DMSES UK can
be used to enable more effective targeting of selfmanagement interventions and clinical resources
to the individual patient. It has strong face validity
and is a reliable scale for use as an outcome
measure in research studies. Future research could
evaluate the predictive capacity of the DMSES
UK, in particular sub-groups of people with type 2
diabetes.
Validity and reliability of the DMSES UK scale 7
Clinicians have a tool available, which has
strong face validity, with both clinicians and
patients, to help identify in which areas of diabetes self-management a patients self-efficacy is
more or less secure. This will enable clinicians to
coach the patients into goal choice areas, where
new behavioural challenges are more likely to
be successful. Early success in new behavioural
challenges will lead to strengthening of self-efficacy
in more challenging goals over time.
Acknowledgements
The authors would like to thank the WDREUG,
the people with type 2 diabetes and the health care
professionals who have participated in this study.
Thanks are due to Professor Shortridge-Baggett
and Dr van der Bijl for their collaborative engagement with this UK validation study. The study was
funded by Diabetes UK and the UK Department of
Health NCCRCD programme.
References
Anderson, R.M., Funnell, M.M., Fitzgerald, A.T. and Marrero,
D.G. 2000: The diabetes empowerment scale: a measure of
psychosocial self-efficacy. Diabetes Care 23, 73943.
Bandura, A. 1977: Self-efficacy theory: towards a unifying
theory of behaviour change. Psychological Review 84,
191215.
Bandura, A. 1994: Self-efficacy. In Ramachaudran, V.S., editor,
Encyclopedia of human behavior. New York: Academic
Press, 7181.
Bandura, A. 1997: Self-efficacy: the exercise of control. New
York: Freeman.
Bandura, A. 2006: Guide for constructing self-efficacy scales.
In Pajares, F. and Urdan, T. editors, Self-efficacy beliefs of
adolescents. Charlotte NC: Information Age Publishing,
30737.
Bijl, V.J., Poelgeest-Eeltink, A.V. and Shortridge-Baggett, L.
1999: The psychometric properties of the diabetes
management self-efficacy scale for patients with type 2
diabetes mellitus. Journal of Advanced Nursing 30, 35259.
Dale, J., Caramlau, I., Sturt, J., Friede, T. and Walker, R. 2009:
Telephone peer-delivered intervention for diabetes
motivation and support: the telecare exploratory RCT.
Patient Education and Counselling 75, 9198.
Davies, M.J., Heller, S., Skinner, T.C., Campbell, M.J., Carey,
M.E., Cradock, S., Dallosso, H.M., Daly, H., Doherty, Y.,
Eaton, S., Fox, C., Oliver, L., Rantell, K., Rayman, G. and
Khunti, K. 2008: Effectiveness of the diabetes education
and self management for ongoing and newly diagnosed
(DESMOND) programme for people with newly
diagnosed type 2 diabetes: cluster randomised controlled
trial. BMJ 336, 49195.
Day, J.L., Bodmer, C.W. and Dunn, O.M. 1997: Development
of a questionnaire identifying factors responsible for
successful self-management of insulin-treated diabetes.
Diabetic Medicine 13, 56473.
Department of Health. 2002: The national service framework
for diabetes standards document. London: Department of
Health.
Department of Health. 2005: Structured patient education in
diabetes: report from the patient education working group,
2005. London: Department of Health.
Donaldson, L. 2003: Expert patients usher in a new era of
opportunity for the NHS. BMJ 326, 127980.
Farmer, A., Wade, A., French, D.P., Goyder, E., Kinmonth,
A.L. and Neil, A. 2005: The DiGEM rial protocol a
randomised controlled trial to determine the effect on
glycaemic control of different strategies of blood glucose
self-monitoring in people with type 2 diabetes
[ISRCTN47464659]. BMC Family Practice 6, 18.
Fisher, E.B., Thorpe, C.T., Devellis, B.M. and Devellis, R.F.
2007: Healthy coping, negative emotions, and diabetes
management: a systematic review and appraisal. Diabetes
Educator 33, 1080103.
Gillis, A.J. 1993: Determinants of health promoting lifestyle;
an integrative review. Journal of Advanced Nursing 18,
54553.
Guevara, J.P., Wolf, F.M., Grum, C.M. and Clark, N.M.
2003: Effects of educational interventions for self management of asthma in children and adolescents: systematic
review and meta-analysis. British Medical Journal 326,
1308309.
International Diabetes Federation. 2003: International standards
for diabetes education. Retrieved 30 April 2009 from
www.idf.org/webdata/docs/International%20standards.pdf
Lindenmeyer, A., Hearnshaw, H. and Sturt, J. 2007:
Assessment of the benefits of user involvement in health
research from the warwick diabetes care research user
group: a qualitative case study. Health Expectations 10,
26877.
Lloyd, C.E., Sturt, J., Johnson, M., Mughal, S., Collins, G. and
Barnett, A.H. 2008: Development of alternative methods
of data collection in South Asians with Type 2 diabetes.
Diabetic Medicine 25, 45562.
Lorig, K.R., Sobel, D.S., Stewart, A.L., Brown, B.W. Jr.,
Bandura, A., Ritter, P., Gonzalez, V.M., Laurent, D.D. and
Holman, H.R. 1999: Evidence suggesting that a chronic
disease self-management programme can improve health
status whilst reducing hospitalisation. A randomised trial.
Medical Care 37, 514.
McDowell, J., Courtney, M., Edwards, H. and ShortridgeBagget, H. 2005: Validation of the Australian/English
version of the diabetes management self-efficacy scale.
International Journal of Nursing Practice 11, 17784.
8 Jackie Sturt, Hilary Hearnshaw and Melanie Wakelin
Norris, S.L., Engelgau, M.M. and Venkat Narayan, K.M. 2001:
Effectiveness of self-management training in type 2
diabetes. A systematic review of randomised controlled
trials. Diabetes Care 24, 56187.
Pajares, F., Hartley, J. and Valiante, G. 2001: Response format
in writing self-efficacy assessment: greater discrimination
increases prediction. Measurement and Evaluation in
Counseling and Development 33, 21421.
Polonsky, W.H., Anderson, B.J., Lohrer, P.A., Welch, G.,
Jacobson, A.M., Aponte, J.E. and Schwartz, C.E. 1995:
Assessment of diabetes-related distress. Diabetes Care 18,
75460.
Sentcal, C., Nouwen, A. and White, D. 2000: Motivation
and dietary self-care in adults with diabetes: are selfefficacy and autonomous self-regulation complementary or competing constructs? Health Psychology 19,
45257.
Shortridge-Bagget, L.M. and van der Bijl, J.J. 2002:
Measurement of significant others self-efficacy in diabetes
management. In Sigma Theta Tau International
Conference, Brisbane.
Sniehotta, F.F., Scholzu, U. and Schwarzer, R. 2005: Bridging
the intention behaviour gap: planning, self-efficacy, and
action control in the adoption and maintenance of physical
exercise. Psychology and Health 20, 14360.
Sturt, J., Hearnshaw, H., Farmer, A., Dale, J. and Eldridge, S.
2006a: The diabetes manual trial protocol a cluster
randomized controlled trial of a self-management
intervention for type 2 diabetes [ISRCTN06315411].
BMC Family Practice 7.45.
Sturt, J., Taylor, H., Docherty, A., Dale, J. and Louise, T.
2006b: A psychological approach for providing selfmanagement education for people with type 2 diabetes:
the diabetes manual. BMC Family Practice 7.70.
Sturt, J.A., Whitlock, S., Fox, C., Hearnshaw, H., Farmer, A.J.,
Wakelin, M., Eldridge, S., Griffiths, F. and Dale, J. 2008:
Effects of the diabetes manual 1:1 structured education in
primary care. Diabetic Medicine 25, 72231.
Van Der Ven, N.C., Weinger, K., Yi, J., Pouwer, F., Ader, H.,
Van Der Ploeg, H.M. and Snoek, F.J. 2003: The confidence
in diabetes self-care scale: psychometric properties of a
new measure of diabetes-specific self-efficacy in Dutch and
US patients with type 1 diabetes. Diabetes Care 26, 71318.
Welch, G., Weinger, K., Anderson, B. and Polonsky, W.H.
2003: Responsiveness of the problem areas in diabetes
(PAID) questionnaire. Diabetic Medicine 20, 6972.
Potrebbero piacerti anche
- Early Signs of AutismDocumento27 pagineEarly Signs of AutismErica Alejandra Schumacher100% (1)
- The Summary of Diabetes Self Care Activities Measure Results From 7 Studies and A Revised Scale PDFDocumento8 pagineThe Summary of Diabetes Self Care Activities Measure Results From 7 Studies and A Revised Scale PDFDiabetesBhNessuna valutazione finora
- Healthier Lifestyle, Behaviour ChangeDocumento4 pagineHealthier Lifestyle, Behaviour ChangeupelworopezaNessuna valutazione finora
- COCOMODocumento21 pagineCOCOMOanirban_surNessuna valutazione finora
- Form16 (2021-2022)Documento2 pagineForm16 (2021-2022)Anushka PoddarNessuna valutazione finora
- Nestlé Management Trainee ProgramDocumento10 pagineNestlé Management Trainee ProgramRiki Risandi100% (1)
- Responsibility MatrixDocumento6 pagineResponsibility MatrixRizky Bangkit100% (1)
- Project Report On Biodegradable Plates, Glasses, Food Container, Spoon Etc.Documento6 pagineProject Report On Biodegradable Plates, Glasses, Food Container, Spoon Etc.EIRI Board of Consultants and Publishers0% (1)
- Fundamentals of Plant BreedingDocumento190 pagineFundamentals of Plant BreedingDave SubiyantoNessuna valutazione finora
- Penicillin G Benzathine-Drug StudyDocumento2 paginePenicillin G Benzathine-Drug StudyDaisy Palisoc67% (3)
- Care of The Client Utilizing The Goal Attainment TheoryDocumento8 pagineCare of The Client Utilizing The Goal Attainment TheoryInternational Journal of Innovative Science and Research Technology100% (1)
- Diabetes Artigo EdDocumento15 pagineDiabetes Artigo EdEduarda CarvalhoNessuna valutazione finora
- Self EfficacyDocumento8 pagineSelf Efficacy130011035 RATNA YUNITA SARINessuna valutazione finora
- Poster Carozaramos 4Documento1 paginaPoster Carozaramos 4api-290348341Nessuna valutazione finora
- Assessing The ProblemDocumento10 pagineAssessing The ProblemKeyvoh KeymanNessuna valutazione finora
- Dia Care 2002 Pastors 608 13Documento6 pagineDia Care 2002 Pastors 608 13Isnar Nurul AlfiyahNessuna valutazione finora
- Perceived Barriers and Effective Strategies To Diabetic Self-ManagementDocumento18 paginePerceived Barriers and Effective Strategies To Diabetic Self-ManagementArceeJacobaHermosaNessuna valutazione finora
- A Study To Assess The Level of Coping Strategies Among The Patients With Chronic Diabetes Mellitus Admitted in Selected HospitalsDocumento9 pagineA Study To Assess The Level of Coping Strategies Among The Patients With Chronic Diabetes Mellitus Admitted in Selected HospitalsIJAR JOURNALNessuna valutazione finora
- Mediating The Effect of Self-Care Management InterventionDocumento13 pagineMediating The Effect of Self-Care Management InterventionDa TaoNessuna valutazione finora
- Association of Self-Efficacy and Self-Care With Glycemic Control in DiabetesDocumento7 pagineAssociation of Self-Efficacy and Self-Care With Glycemic Control in DiabetesSeptian M SNessuna valutazione finora
- Diabetes ManagementDocumento6 pagineDiabetes Managementapi-259018499Nessuna valutazione finora
- Upaya Pemberdayaan Kader Kesehatan Dalam Peningkatan Berbasis Konservasi LevineDocumento6 pagineUpaya Pemberdayaan Kader Kesehatan Dalam Peningkatan Berbasis Konservasi LevineDyan NittaRahayuNessuna valutazione finora
- The Validity and Reliability of The Summary of Diabetes Self-Care Activities Questionnaire: An Indonesian VersionDocumento12 pagineThe Validity and Reliability of The Summary of Diabetes Self-Care Activities Questionnaire: An Indonesian VersionPopi SopiahNessuna valutazione finora
- Optimal EngDocumento11 pagineOptimal EngIRENE ORTIZ LOPEZNessuna valutazione finora
- PHD Proposalmaterial 2Documento7 paginePHD Proposalmaterial 2ghaji jonathanNessuna valutazione finora
- Bibliography Journal On Diabetic FootDocumento3 pagineBibliography Journal On Diabetic FootCamille GraceNessuna valutazione finora
- Richardson Synthesis Summative 280613Documento13 pagineRichardson Synthesis Summative 280613api-217086261Nessuna valutazione finora
- Patient Education and CounselingDocumento9 paginePatient Education and CounselingJavi PatónNessuna valutazione finora
- JPHR 2021 2240Documento5 pagineJPHR 2021 2240Muhammad MulyadiNessuna valutazione finora
- The Influence of Complication Events On The Empowerment Selfcare of Diabetes Mellitus PatientsDocumento5 pagineThe Influence of Complication Events On The Empowerment Selfcare of Diabetes Mellitus PatientsInternational Journal of Innovative Science and Research TechnologyNessuna valutazione finora
- Content ServerDocumento8 pagineContent ServerPaul CenabreNessuna valutazione finora
- Pamungkas2017 PDFDocumento17 paginePamungkas2017 PDFPaskalya eroNessuna valutazione finora
- Patient Education and CounselingDocumento8 paginePatient Education and CounselingSri WahyuniNessuna valutazione finora
- A Systematic Review On The Kap-O Framework For Diabetes Education and ResearchDocumento21 pagineA Systematic Review On The Kap-O Framework For Diabetes Education and ResearchToyour EternityNessuna valutazione finora
- Increasing Diabetes Self-Management Education in Community SettingsDocumento2 pagineIncreasing Diabetes Self-Management Education in Community Settingsmuhammad ade rivandy ridwanNessuna valutazione finora
- Group-Based Dietary Program Improves HypertensionDocumento14 pagineGroup-Based Dietary Program Improves HypertensionNur Fadillah B21741419601Nessuna valutazione finora
- Jurnal Self Management DM Literacy 4Documento8 pagineJurnal Self Management DM Literacy 4Rifa AinunNessuna valutazione finora
- Systematic Review Revised EditionDocumento43 pagineSystematic Review Revised EditionjunaidNessuna valutazione finora
- Conclusion and RecommendationDocumento3 pagineConclusion and RecommendationMarcelo MalabananNessuna valutazione finora
- Chronic Illnesses Are Becoming An Increasingly Serious Public Health Issue Across The WorldDocumento7 pagineChronic Illnesses Are Becoming An Increasingly Serious Public Health Issue Across The WorldHaneenNessuna valutazione finora
- Quality Improvement Project.Documento7 pagineQuality Improvement Project.rhinoNessuna valutazione finora
- Effectiveness of diabetes education and self-management programme at 3 yearsDocumento22 pagineEffectiveness of diabetes education and self-management programme at 3 yearsUlva HirataNessuna valutazione finora
- De Guzman Christelle Marie P. Dela Cruz Claire D. Assessment Shared Journal Reflection CP4Documento2 pagineDe Guzman Christelle Marie P. Dela Cruz Claire D. Assessment Shared Journal Reflection CP4Christelle Marie De GuzmanNessuna valutazione finora
- Low Carb For DiabetesDocumento6 pagineLow Carb For DiabetesChrisNessuna valutazione finora
- Arun ArticleDocumento8 pagineArun Articleslacker77725Nessuna valutazione finora
- 2965-Article Text-12063-3-10-20211018Documento7 pagine2965-Article Text-12063-3-10-20211018Nur Laili FitrianiNessuna valutazione finora
- Chronic Illnesses Are Becoming An Increasingly Serious Public Health Issue Across The WorldDocumento7 pagineChronic Illnesses Are Becoming An Increasingly Serious Public Health Issue Across The WorldHaneenNessuna valutazione finora
- The Impact of Orem's Self-CareDocumento9 pagineThe Impact of Orem's Self-CareRiski Official GamersNessuna valutazione finora
- Emagrecimento Determinantes ShowwwwDocumento41 pagineEmagrecimento Determinantes ShowwwwÉomer LanNessuna valutazione finora
- Lin 2012Documento7 pagineLin 2012Ferdy LainsamputtyNessuna valutazione finora
- Diabetes Distress Paper EfmjDocumento16 pagineDiabetes Distress Paper EfmjAhmed NabilNessuna valutazione finora
- King JournalClubDocumento7 pagineKing JournalClubTimothy Samuel KingNessuna valutazione finora
- Motivation Implementation of Hba1C Decrease in Patients Diabetes Mellitus (Riview Literature) Christianto NugrohoDocumento6 pagineMotivation Implementation of Hba1C Decrease in Patients Diabetes Mellitus (Riview Literature) Christianto Nugrohomarisa isahNessuna valutazione finora
- Nutrition Knowledge, Attitudes, and Self-Regulation As PDFDocumento9 pagineNutrition Knowledge, Attitudes, and Self-Regulation As PDFJoem cNessuna valutazione finora
- Running Head: Integrative Literature Review 1Documento20 pagineRunning Head: Integrative Literature Review 1api-456537311Nessuna valutazione finora
- Migraine and Body Mass Index Categories: A Systematic Review and Meta-Analysis of Observational StudiesDocumento14 pagineMigraine and Body Mass Index Categories: A Systematic Review and Meta-Analysis of Observational StudiesRetno ManggalihNessuna valutazione finora
- Caudill IntegrativereviewDocumento28 pagineCaudill Integrativereviewapi-453322312Nessuna valutazione finora
- Edinburgh Research Explorer: Pilot Study of Acceptance and Commitment Therapy For Irritable Bowel SyndromeDocumento25 pagineEdinburgh Research Explorer: Pilot Study of Acceptance and Commitment Therapy For Irritable Bowel SyndromeJuan Alberto GonzálezNessuna valutazione finora
- Nursing Agency Improves Diabetes Self-CareDocumento23 pagineNursing Agency Improves Diabetes Self-CareWisnu KhawirianNessuna valutazione finora
- International Journal of Diabetes and Clinical Research Ijdcr 8 134Documento7 pagineInternational Journal of Diabetes and Clinical Research Ijdcr 8 134Rio Raden Partotaruno TamaelaNessuna valutazione finora
- Effectiveness of Motivational Interviewing for Health BehaviorsDocumento11 pagineEffectiveness of Motivational Interviewing for Health BehaviorsPasca Liana MariaNessuna valutazione finora
- Instrumen Quality of Life WHOQOL-BREEFDocumento9 pagineInstrumen Quality of Life WHOQOL-BREEFSri Wulandari 15026760201Nessuna valutazione finora
- HMB Weight ManagementDocumento5 pagineHMB Weight ManagementJesse M. MassieNessuna valutazione finora
- BMC 2008Documento10 pagineBMC 2008Fadel TrianzahNessuna valutazione finora
- Perceptions, Attitudes, and Behaviors of Primary Care Providers Toward Obesity Management: A Qualitative StudyDocumento18 paginePerceptions, Attitudes, and Behaviors of Primary Care Providers Toward Obesity Management: A Qualitative StudyFitriani WidyastantiNessuna valutazione finora
- Impact of A Designed Self-Care Program On Selected Outcomes Among Patients Undergoing HemodialysisDocumento18 pagineImpact of A Designed Self-Care Program On Selected Outcomes Among Patients Undergoing HemodialysisImpact JournalsNessuna valutazione finora
- VA Diabetes Education Program Improves HbA1c & WeightDocumento8 pagineVA Diabetes Education Program Improves HbA1c & WeightNsafifahNessuna valutazione finora
- Dinamika Kelompok Tani SaiyoDocumento10 pagineDinamika Kelompok Tani SaiyoYoudz VoLvoc100% (1)
- Work Breakdown StructureDocumento9 pagineWork Breakdown StructureArif ForhadNessuna valutazione finora
- Kepuasan Kerja Petugas Kesehatan Di Instalasi Rawat Inap Rs Islam FaisalDocumento14 pagineKepuasan Kerja Petugas Kesehatan Di Instalasi Rawat Inap Rs Islam FaisalRizky BangkitNessuna valutazione finora
- Dinamika Kelompok Tani SaiyoDocumento10 pagineDinamika Kelompok Tani SaiyoYoudz VoLvoc100% (1)
- AdapRandomSearch4 05 2009Documento16 pagineAdapRandomSearch4 05 2009Meo Meo ConNessuna valutazione finora
- 1TA11813Documento8 pagine1TA11813Septy AmorrindaNessuna valutazione finora
- Effect of Parenting, School Environment, and Peers on Teen EQDocumento11 pagineEffect of Parenting, School Environment, and Peers on Teen EQRizky BangkitNessuna valutazione finora
- Simple Additive Weighting (SAW) MethodDocumento1 paginaSimple Additive Weighting (SAW) MethodRizky BangkitNessuna valutazione finora
- The Relationship Between Self Efficacy and Well Being in Stroke Survivors 2329 9096.1000159Documento10 pagineThe Relationship Between Self Efficacy and Well Being in Stroke Survivors 2329 9096.1000159anangdwiresdiantoNessuna valutazione finora
- LETOR: Benchmark Dataset For Research On Learning To Rank For Information RetrievalDocumento8 pagineLETOR: Benchmark Dataset For Research On Learning To Rank For Information RetrievalRizky BangkitNessuna valutazione finora
- User ManualDocumento193 pagineUser Manualcrazymax90Nessuna valutazione finora
- Perhitungan Manual Metode AHP RevisedDocumento16 paginePerhitungan Manual Metode AHP RevisedNana Rusmar100% (1)
- Edge Detection: Xy, and Y2, We Will Approximate - L (M+X, N+y) - L (M, N) - (L (M+X, N+y) - L (M, N) ) by The LinearDocumento25 pagineEdge Detection: Xy, and Y2, We Will Approximate - L (M+X, N+y) - L (M, N) - (L (M+X, N+y) - L (M, N) ) by The LinearRizky BangkitNessuna valutazione finora
- Worksheet - Solubility - Water As A SolventDocumento2 pagineWorksheet - Solubility - Water As A Solventben4657Nessuna valutazione finora
- Soni Clinic & Pathology Center Chanda: Address:-Front of TVS AgencyDocumento1 paginaSoni Clinic & Pathology Center Chanda: Address:-Front of TVS AgencyVishalNessuna valutazione finora
- Seizure Acute ManagementDocumento29 pagineSeizure Acute ManagementFridayana SekaiNessuna valutazione finora
- CH 23 PDFDocumento42 pagineCH 23 PDFkrishnaNessuna valutazione finora
- Food Sample Test For Procedure Observation InferenceDocumento2 pagineFood Sample Test For Procedure Observation InferenceMismah Binti Tassa YanaNessuna valutazione finora
- 2018 Nutrition Month ReportDocumento1 pagina2018 Nutrition Month ReportAnn RuizNessuna valutazione finora
- DaloDocumento2 pagineDalojosua tuisawauNessuna valutazione finora
- Frontier DL650 Maintenance Guide Ver 1.0Documento25 pagineFrontier DL650 Maintenance Guide Ver 1.0philippe raynalNessuna valutazione finora
- MSDS - ENTEL BatteryDocumento3 pagineMSDS - ENTEL BatteryChengNessuna valutazione finora
- Excipients As StabilizersDocumento7 pagineExcipients As StabilizersxdgvsdgNessuna valutazione finora
- As en 540-2002 Clinical Investigation of Medical Devices For Human SubjectsDocumento8 pagineAs en 540-2002 Clinical Investigation of Medical Devices For Human SubjectsSAI Global - APACNessuna valutazione finora
- CD - 15. Republic of The Philippines Vs Sunlife Assurance of CanadaDocumento2 pagineCD - 15. Republic of The Philippines Vs Sunlife Assurance of CanadaAlyssa Alee Angeles JacintoNessuna valutazione finora
- EMAAR HOUSING HVAC SYSTEM SPECIFICATIONSDocumento91 pagineEMAAR HOUSING HVAC SYSTEM SPECIFICATIONSBhuvan BajajNessuna valutazione finora
- BrochureDocumento2 pagineBrochureRajib DasNessuna valutazione finora
- Atlas Copco Generators: 15-360 kVA 15-300 KWDocumento10 pagineAtlas Copco Generators: 15-360 kVA 15-300 KWAyoub SolhiNessuna valutazione finora
- Deltair BrochureDocumento4 pagineDeltair BrochureForum PompieriiNessuna valutazione finora
- Rorschach y SuicidioDocumento17 pagineRorschach y SuicidioLaura SierraNessuna valutazione finora
- Dladla Effect 2013Documento231 pagineDladla Effect 2013TheDreamMNessuna valutazione finora
- Single Inlet Centrifugal FanDocumento43 pagineSingle Inlet Centrifugal Fan4uengineerNessuna valutazione finora
- Computed Tomography (CT) - BodyDocumento7 pagineComputed Tomography (CT) - Bodyfery oktoraNessuna valutazione finora
- Barangay Peace and Order and Public Safety Plan Bpops Annex ADocumento3 pagineBarangay Peace and Order and Public Safety Plan Bpops Annex AImee CorreaNessuna valutazione finora
- Calculate Size of Transformer / Fuse / Circuit Breaker: Connected Equipment To TransformerDocumento16 pagineCalculate Size of Transformer / Fuse / Circuit Breaker: Connected Equipment To TransformerHari OM MishraNessuna valutazione finora
- Bioreactor For Air Pollution ControlDocumento6 pagineBioreactor For Air Pollution Controlscarmathor90Nessuna valutazione finora
- 16 Point Msds Format As Per ISO-DIS11014 PDFDocumento8 pagine16 Point Msds Format As Per ISO-DIS11014 PDFAntony JebarajNessuna valutazione finora
- Nabertherm RHTH Tube Furnace SOPDocumento4 pagineNabertherm RHTH Tube Furnace SOPIyere PatrickNessuna valutazione finora