Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Ig E
Caricato da
Rishiraj SahooTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Ig E
Caricato da
Rishiraj SahooCopyright:
Formati disponibili
ASIAN PACIFIC JOURNAL OF ALLERGY AND IMMUNOLOGY (2006) 24: 191-199
Relevance of Serum IgE Estimation in
Allergic Bronchial Asthma with
Special Reference to Food Allergy
Raj Kumar1, Bhanu P. Singh2, Prakriti Srivastava1, Susheela Sridhara2, Naveen Arora2 and
Shailendra N. Gaur1
SUMMARY Studies suggest the importance of serum total and specific IgE in clinical evaluation of allergic manifestations. Such studies are lacking in Indian subcontinent, though a large population suffer from bronchial asthma.
Here relevance of serum total and specific IgE was investigated in asthmatics with food sensitization. A total of 216
consecutive patients (mean age 31.9 years, S.D. 11.8) were screened by various diagnostic testing. Out of 216 patients, 172 were with elevated serum total IgE (201 to > 800 IU/ml). Rice elicited marked positive skin prick test reactions (SPT) in 24 (11%) asthma patients followed by black gram 22 (10%), lentil 21 (9.7%) and citrus fruits 20
(9.2%). Serum total IgE and specific IgE showed significant correlation, p = 0.005 and p = 0.001, respectively, with
positive skin tests. Blinded food challenges (DBPCFC) with rice and or black gram confirmed food sensitization in
28-37% of cases. In summary, serum total IgE of 265 IU/ml or more with marked positive SPT (4 mm or more) can
serve as marker for atopy and food sensitization. Specific IgE, three times of normal controls correlates well with
positive DBPCFC and offers evidence for the cases of food allergy.
Inflammation is the hallmark of bronchial
asthma, which results in airway hyperresponsiveness
and resistance to flow in the lower airways of
lungs.1,2 Various stimuli such as environmental allergens, psychic disturbances, infection, etc. are responsible for triggering inflammation and causing
mild, moderate or severe airflow obstruction in
asthmatics.3,4 After discovery of IgE antibody,5 attempts have been made to classify extrinsic asthma
from intrinsic asthma.6 Earlier studies suggest the
importance of serum total IgE in the pathophysiology of asthma and the development of airflow obstruction.3,4,7 Besides, a close association has been
reported between the presence of elevated total IgE
levels and symptomatic asthma.
Incidence of asthma has increased world
over including Asian countries.8,9 In India about 2-
8% population is estimated to suffer from bronchial
asthma with or without rhinitis.8 Like pollen and
other allergens, foods are also known to cause severe
systemic reactions and asthma in atopic individuals.
But in India, very few attempts are made to study
food sensitization and the allergic manifestations.10,11
Currently, the methods used to diagnose food allergy
include skin prick tests, measurement of food specific IgE, oral food challenges and double blinded
placebo controlled food challenge. Determination of
serum total IgE distinguishes atopic and/or nonatopic status of individuals.12,13 Skin prick testing
1
From the Department of Respiratory Medicine, Vallabhbhai
2
Patel Chest Institute, University of Delhi, Delhi-110007, Allergy
and Immunology Laboratory, Institute of Genomics and Integrative Biology (CSIR), Delhi University Campus, Delhi-110007, India.
Correspondence: Raj Kumar
E-mail: rajkumar_27563@yahoo.co.in
KUMAR, ET AL.
192
with allergen extracts is carried out to find out sensitization against offending allergens. Specific IgE estimation against respective allergen offers further
evidence14,15 to skin test results. However, all these
methods of diagnosis, even double blinded placebo
controlled food challenge may sometimes be misleading.16 In view of the shortcomings in individual
methods, the present study was undertaken to validate relevance of specific IgE estimations in diagnosing food allergy in asthmatics. Serum total IgE
levels in these patients were also correlated with skin
prick tests, oral food challenge and pulmonary obstruction.
nasal blockade, post nasal drip, etc. Various steps
involved in patient selection and testing in present
study are described in Fig. 1.
The patients (asthmatics) from both sexes
and non-smokers were included with history suggestive of atopy (inclusion criteria). Patients with other
associated pulmonary diseases including tuberculosis, COPD and systemic diseases, e.g. diabetes, hypertension and heart diseases were excluded (exclusion criteria) from the study. Patients with mechanical causes of airway obstruction, steroid dependent
and psychologically unstable cases were also excluded.
MATERIALS AND METHODS
Subjects
Two hundred sixteen patients of bronchial
asthma with or without rhinitis were included in the
present study from referred cases to Out Patient Department of V.P. Chest Institute, Delhi, in the years
2003-2004. These patients aged 8-65 years comprised 115 (53.2%) males and 101 (46.7%) females.
The patients were with history of food allergy as recorded using a standard questionnaire.17 The diagnosis of asthma was made based on history and
clinical investigation following the criteria of American Thoracic Society 1991.18 More than 15% reversibility of airway obstruction with 200 g of salbutamol was taken as criteria for diagnosing asthma.
The rhinitis19 was assigned to patients having any
two of the symptoms such as sneezing, rhinorrhea,
The written consent of each patient was obtained for participation in the study. The patients
were persuaded to give blood for serum total and
specific IgE estimation. The study protocol is approved by human ethics committee of the Institute.
Pulmonary function test
Spirometric evaluation of patients was done
as per American Thoracic Society guidelines18 with
Morgan Pulmolab equipment, England. The best of
the three readings were taken for assessing their
pulmonary function.
Skin prick tests (SPT)
Skin tests were carried out in 216 patients
with history suggestive of sensitization to food and
216 asthma patients (referred cases)
History & clinical investigation
(blood, X-ray, stool, physical examination, PFT [n = 182] etc.)
Skin prick tests (n = 216),
Normal (n = 41)
Serum total IgE estimation (n = 216)
NHS (n = 41 normal control)
Specific IgE estimation (n = 144)
NHS (n = 41 normal control)
Open food challenge
(n = 40, SPT+ELISA positive cases)
Blinded oral food challenge (DBPCFC)
(n = 30, SPT + ELISA positive cases)
Fig. 1 Flow chart describing the steps involved in patients selection and testing for the present study.
192
RELEVANCE OF SERUM IgE IN ASTHMA
193
common environmental allergens. The skin test reactions were graded after 20 minutes20 in comparison
to the wheal size of positive control, i.e. histamine
diphosphate (5 mg/ml). Skin tests with mean diameter of wheal three mm and above were considered as
marked positive reaction. For SPT, the allergen extracts (1:10 w/v, 50% glycerinated) were obtained
from Antigen Laboratory, Institute of Genomics and
Integrative Biology (CSIR), Delhi.
Total IgE estimation
Serum total IgE estimation21 was carried out
for each patient and normal control by enzymelinked immunosorbent assay (ELISA) using
Pathozyme IgE kit (Omega Diagnostic Ltd, UK).
Monoclonal anti-IgE was coated into wells as per
manufacturers instruction. After washing, patients
serum diluted 1:10 v/v with the zero buffer was incubated for 30 minutes at 25C. Followed by washing, horse radish peroxidase conjugated anti-human
IgE was added and incubated for 30 minutes. The
color was developed by adding tetramethyl benzidene. The enzyme reaction was stopped with 100
l of hydrochloric acid. Absorbance was read at 450
nm using Dynatech ELISA reader.
Specific IgE estimation
Sera of patients showing marked positive
skin reactions were evaluated by ELISA for specific
IgE22 against respective food extract. Briefly, 2 g
protein (extract) was coated (100 l) per well in carbonate-bicrbonate buffer (pH 9.0) overnight at 4C.
After washing five times with phosphate buffered saline (PBS), unbound sites were blocked with 3%
BSA. Following washing, wells were incubated with
1:10 v/v diluted patients sera (100 l) overnight at
4C. The plate was washed again with PBS-Tween20 and incubated with horse radish peroxidase conjugated anti-human IgE for 4 hours at 37C. The
color was developed using O-phenylenediamine. The
reaction was stopped by adding 50 l of sulphuric
acid. Absorbance was read at 490 nm using an
ELISA reader.
Open food challenge (OFC)
In open food challenge test, the patients were
given orally 20-60 g of suspected food(s) as per the
history and kept under observation for 20 to 60 minutes. Spirometry evaluation was done before and af-
ter food challenge and fall in force vital capacity was
recorded. OFCs were performed under medical supervision and patients were asked to stay in the clinic
for at least 2 hours after the test. During the observation time blood pressure, pulse rate, forced expiratory volume in 1 second and peak expiratory flow
were measured. Subjects showing a positive OFC
were subsequently tested with DBPCFC.
Double blinded placebo controlled food challenge
(DBPCFC)
Double blinded placebo controlled food
challenges (DBPCFCs) were performed as per the
guidelines described earlier.23 Briefly, the active
food was masked to make it indistinguishable from
the placebo and was administered in double blinded
fashion, i.e. neither the patient nor the observer recording clinical manifestation knew about the content. The initial dose of food administered in
DBPCFC was chosen based on the results of OFC.
Approximately 20-30 g of the test food was sufficient to provoke allergic reactions in susceptible patients.
Spirometry evaluation, forced expiratory
volume at one second (FEV1) was made prior and after food challenge. The airflow obstruction (PFT)
was noted after food challenge test and obstruction
of more than 15% in FEV1 or 200 ml change was
taken as significant value. The patients who developed symptoms such as breathlessness, cough,
sneezing, rhinorrhea, vomiting and significant
changes in spirometry were scored as DBPCFC positive. The patients were kept under observation for at
least 2 hours after the food challenge test. In case of
anaphylactic reaction as a result of provocation the
patients were given epinephrine and avil and were
nebulized with salbutamol and ipratropium bromide.
Same ingredients of placebo were used in
both the active food and placebo. Placebo was selected from food materials which showed negative
SPT, ELISA (Specific IgE) and oral challenge test in
patients. The test recipe was usually prepared in the
ratio of 3:1 (Placebo:test food).
Statistical analysis
The statistical analysis was performed using
SPSS (Statistical Package for Social Sciences) ver-
193
KUMAR, ET AL.
194
sion 10.5 software. The data was analyzed for all
variables using the Chi-square test. The comparison
was made between serum total IgE levels with pulmonary function, serum total IgE with skin prick test
and specific IgE with skin prick test and oral food
challenge test. The differences were considered to be
statistically significant at p = 0.05.
RESULTS
Out of 216 patients included in the present
study, 54 were suffering with asthma alone, whereas
162 had associated rhinitis. Most of the patients
were in the age group of 21-40 years with mean age
31.9 (SD 11.8). Serum total IgE was estimated in all
cases (n = 216) by ELISA. Age wise distribution of
total IgE values (IU/ml) has been presented in Table
1. Maximum patients (n = 56) with elevated IgE
(201 to > 800 IU/ml) were in 21-30 years age group
followed by 31-40 years (n = 54) and least (n = 12)
were in 51 years and above group. The serum total
IgE data was analyzed in two groups of patients: (a)
bronchial asthma alone and (b) asthma with associated rhinitis (Table 2). Altogether 61 patients showed
total IgE in the range of 201-400 IU/ml, 28 patients,
IgE 401-600 IU/ml and 44 patients showed IgE values, 601-800 IU/ml. Thirty-nine patients demonstrated serum total IgE > 800 IU/ml.
Out of the 216 cases, pulmonary function
test could be performed in 182 asthma patients to record air flow obstruction. The patients were categorized as normal (> 80% of the predicted FEV1), mild
(60-80% of the predicted FEV1), moderate (40-60%
of the predicted FEV1) and severe (< 40% of the predicted FEV1) on the basis of airflow obstruction.
Pulmonary obstruction (FEV1) and serum total IgE
values were analyzed for all asthmatics (with or
without rhinitis) and presented in Fig. 2. The total
IgE values in normal healthy volunteers (NHS, n =
41) ranged from 6-231 IU/ml. Mean 2SD was calculated and values > 265 IU/ml IgE were taken to
classify ELISA cut off for patients with significantly
elevated IgE levels (Fig. 2). Among the patients
with mild (n = 55) to moderate (n = 40) airflow obstruction, 40 and 27 patients, respectively demonstrated remarkably elevated IgE levels (265 IU/ml).
Severe airflow obstruction was recorded in 19 cases
Table 1 Serum total IgE values in different age groups of asthma patients
Age group
(years)
Total IgE (IU/ml)
Total
6-200
201-400
401-600
601-800
> 800
08-20
09
08
02
10
10
39
21-30
17
16
11
16
13
73
31-40
07
20
09
14
11
61
41-50
07
11
03
03
03
27
51 & above
04
06
03
01
02
16
Table 2 Distribution of serum total IgE in two groups of asthma patients
Total IgE (IU/ml)
Bronchial asthma
No.
Asthma with rhinitis
No.
Total
No. (%)
6-200
11
33
44 (20.4)
201-400
14
47
61 (28.2)
401-600
11
17
28 (13.0)
601-800
12
32
44 (20.4)
> 800
06
33
39 (18.1)
194
RELEVANCE OF SERUM IgE IN ASTHMA
195
and 15 of them demonstrated significantly elevated
IgE levels. Comparative analysis of the data showed
no statistically significant correlation (p = 0.815) between serum total IgE levels and pulmonary obstruction (PFT).
SPT reactivity of these patients (n = 216)
was evaluated with different food extracts (Table 3).
Rice extract elicited marked positive SPT in 24
(11%) patients followed by black gram 22 (10%),
lentil 21 (9.7%) and citrus fruits 20 (9.2%). The
food extracts such as pea, maize, French bean, Lima
bean, fish and mustard exhibited marked positive
skin reactivity in 5-6% patients. Many food extracts
demonstrated marked positive skin reactions in 2-4%
of the cases tested. Beside food extracts, these patients were skin tested with 9 dominant pollen allergen extracts. Some of the patients positive to foods
also showed marked positive skin reactivity to pollen
extracts. This may be due to co-sensitization or presence of cross reactive proteins in the extracts.
Specific IgE estimations were carried out in
sera of patients against 9 major food allergens (Table
4). About 60-91% of SPT positive patients showed
raised specific IgE levels. Specific IgE values three
times of normal control (OD = 0.27 or more) were
designated as ELISA positive. Comparative analysis
of marked positive SPT and specific IgE (n = 144)
showed significant correlation (p = 0.001). Serum
total IgE values (n = 216) showed highly significant
correlation (p = 0.005) against marked positive skin
tests.
Open food challenge (OFC) was carried out
in 40 SPT and ELISA (specific IgE) positive asthma
patients. The OFC was positive in 27 (67.5%) cases
tested with rice, black gram, citrus fruits, banana,
French bean and lentil. DBPCFCs conducted with
rice (n = 16) and black gram (n = 14) in SPT positive
cases, demonstrated positive challenges in 6 (37.5%)
and 4 (28.5%) cases, respectively. The patients suffered with breathlessness, cough, sneezing, rhinor-
1400
Total IgE (IU/ml)
1200
1000
800
600
400
Mean +2 SD
200
Mean + SD
NHS
Fig. 2
Mild
Moderate
Severe
Analysis of total IgE levels and airflow obstruction in bronchial asthma patients. Out of
182 asthma patients, 55 showed mild, 40 moderate and 19 severe airflow obstruction.
The remaining 68 asthmatics showed normal airflow obstruction at the time of testing
(data not included) mean + 2 SD of normal human sera (NHS, n = 41) was calculated
as given in parenthesis (ODs > 265 IU/ml).
195
KUMAR, ET AL.
196
rhea, vomiting, stomach upset etc. after the challenge
test. Specific IgE and DBPCFCs with rice and black
gram were correlated for 30 patients. The patients
with specific IgE, three times of normal control or
more (OD > 0.27) demonstrated positive DBPCFC.
DISCUSSION
Open food challenge (OFC) and/or double
blinded placebo controlled food challenge
(DBPCFC) are recommended to achieve definitive
diagnosis of food allergy.23 DBPCFCs are cumbersome, associated with risk and results of OFCs are
not always reliable. In recent years, some studies
have related the total and specific IgE levels in serum and respiratory symptoms in patients sensitized
to food or inhalant allergens.11,24,25 Choi et al.26 observed that sensitivity of skin test was higher than
specific IgE test, whereas the specificity of IgE test
was better than skin test. Therefore, both the tests
should be used in a complimentary manner.
Sampson and Ho27 have established cut off points in
the specific IgE serum levels for different foods that
can predict clinical reactivity after ingestion in 9095% of the group studied. In the present study, relevance of serum total IgE levels was evaluated in
terms of airway responsiveness, i.e. pulmonary obstruction in allergic asthmatics. The data for serum
total IgE and specific IgE against respective food allergen were collected, analyzed and correlated for
clinical use.
Previously serum total IgE levels were
shown to be related with age, genetic predisposition,
race, immune status and some disease processes.28
The upper limit for IgE in normal adults has been recorded in the range of 40.9 IU/ml to 200 IU/ml in
different studies.7,29 Lindeberg and Arroyave30 have
defined 100 IU/ml as the cutoff to differentiate allergic and non-allergic subjects. For children less than
Table 3 Skin prick tests (SPT) with food allergen extracts on patients of asthma (n = 216)
Sample
number
Allergen extracts
2+
No.
3+
No.
4+
No.
Total
No.
Rice
23
24
11.1
Black gram
19
22
10.1
Lentil
21
21
9.7
Citrus fruits*
15
20
9.2
Pea
10
13
6.0
Maize
11
13
6.0
5.5
Lima bean
French bean
12
11
12
Fish
5.5
11
5.0
10
11
Mustard
10
11
5.0
Peanut
09
12
4.1
Banana
09
4.1
13
Soybean
07
3.2
14
Coconut
07
3.2
15
Chicken
07
3.2
16
Radish
06
2.7
17
Almond
05
2.3
18
Carrot
05
2.3
19
Cashew nut
05
2.3
20
Wheat
04
1.8
Total food extracts tested (n = 38); food extracts (n = 15) not included here showed SPT +ve reactions in < 1% cases; 2+ to 4+ = markedly positive skin reactions.
*Citrus fruits include orange, grapes, mausami and lemon.
196
RELEVANCE OF SERUM IgE IN ASTHMA
197
Table 4 Specific IgE levels against food allergen extracts in skin prick test (SPT)
positive asthma patients
Sample
number
Allergen extracts
SPT +ve
Specific IgE positive*
No.
Rice
24
16
66.6
Black gram
22
16
72.7
Lentil
21
16
76.1
Citrus fruits
20
12
60.0
Pea
13
09
69.2
French bean
12
11
91.6
Lima bean
12
08
66.6
Mustard
11
07
63.6
Banana
09
07
77.7
* ELISA positive = ODs > 0.27 (three times of normal control), Normal control = 0.09.
one year of age, the cut off value of 10 IU/ml provided 100% specificity and sensitivity. In the present study, 265 IU/ml serum total IgE (mean 2SD
of NHS) was taken as cutoff for ELISA positive.
Based on this, 82 (45.1%) asthmatics showed mild,
moderate or severely impaired lung function (Fig. 2).
The patients with significantly elevated IgE levels
(201 to > 800 IU/ml) were in 21- 40 years age group.
But no statistically significant correlation was observed between age and total IgE levels in our study
(p = 0.12). Burrows et al.12 reported similar findings
about serum total IgE and rate of disease in different
age group patients. Shadick and co-workers31 observed association between serum total IgE concentrations at the early life with lower level of pulmonary function. But it is not predictive of accelerated
rate in decline of FEV1 among middle aged and
older man. Taylor and coworkers32 observed in a 7.5
years follow up study, that decline in FEV1 was unrelated to total serum IgE levels. This is in agreement
to our findings since no statistically significant correlation (p = 0.815) was observed between total IgE
levels and pulmonary obstruction in allergic asthmatics.
Earlier studies suggest that quantitation of
food specific IgE is a useful test for diagnosing allergy to milk, egg, peanut and fish.11,33 This could
eliminate the need of double blinded placebo controlled challenges in a significant number of subjects.
Garcia-Ara et al.34 also stated that, milk allergic
cases with positive SPT and 2.5 kU/l specific IgE or
greater should not be subjected to oral food challenges. In the present study, many asthmatics
showed food sensitization as evaluated by history
and skin prick tests (SPT). Specific IgE estimation
with 9 common food allergen extracts showed significantly raised levels in SPT positive cases. The
data for marked positive skin tests and specific IgE
showed statistically significant (p = 0.012) correlation. Among 40 SPT and ELISA positive (specific
IgE 3 times of control) cases, 27 (67.5%) patients
gave OFC positive test. However, no statistically
significant correlation (p = 0.608) was observed between higher specific IgE and open food challenge
positivity. DBPCFC carried out with rice and black
gram showed positive challenges in 37.5% to 28.5%
cases tested. The patients showing DBPCFC positive
were with marked positive skin tests (4 mm or more
wheal) and significantly elevated specific IgE (OD >
0.27, i.e. three times or more of normal control)
against respective food.
In conclusion, elevated serum total IgE levels (> 265 IU/ml) indicate towards atopic status of
patients, but it did not correlate with pulmonary obstruction in allergic asthmatics. Specific IgE three
times of control and skin prick tests 4 mm wheal or
more offer substantial evidence for food hypersensitivity in asthmatics. Based on this, the patients can
be advised to undertake avoidance measures against
the offending food allergen.
197
KUMAR, ET AL.
198
ACKNOWLEDGEMENTS
This work was funded by grant from Indian
Council of Medical Research (ICMR), New Delhi.
The authors are thankful to Mr. Harsh Kumar (statistical analyst) for analysis of data.
16.
17.
18.
REFERENCES
1. Taylor KJ, Luksza AR. Peripheral blood eosinophil counts
and bronchial responsiveness. Thorax 1987; 42: 452-56.
2. Kuntz KM, Kitch BT, Fuhlbrigge AL, Paltiel AD, Weiss ST.
A novel approach to defining the relationship between lung
function and symptom status in asthma. J Clin Epidemiol
2002; 55: 11-8.
3. Peat JK, Salome CM, Woolcock AJ. Longitudinal changes in
atopy during a 4 year period, relation to bronchial hyperresponsiveness and respiratory symptoms in a population sample of Australian school children. J Allergy Clin Immunol
1990; 85: 65-74.
4. Sherrill DL, Lebowitz MD, Halonen M, Barbee RA, Burrows B. Longitudinal evaluation of the association between
pulmonary function and total serum IgE. Am J Respir Crit
Care Med 1995; 152: 98-102.
5. Johansson SGO, Bennich H. Immunological studies of an
atypical (myeloma) immunoglobin. Immunology 1967; 13:
381-94.
6. Humbert M, Menz G, Ying S, Corrigan CJ, Robinson DS,
Durham SR, Kay AB. The immunopathology of extrinsic
(atopy) and intrinsic (non-atopic) asthma: more similarities
than difference. Immunology Today 1999; 20: 528-33.
7. Annesi I, Oryszozyn MP, Frette C, Neukirch F, OrvoenFrija E, Kauffman F. Total circulating IgE and FEV1 in adult
men; an epidemiologic longitudinal study. Chest 1992; 101:
642-48.
8. Anonymous. Worldwide variation in prevalence of symptoms of asthma, allergic rhinoconjunctivitis and atopic eczema: ISAAC. Lancet 1998; 351: 1225-32.
9. Wong GWK, Leung TF, Fok TF. Asthma epidemiology and
hygiene hypothesis in Asia. Allergy Clin Immunol Int 2004;
16: 155-60.
10. Kumar R, Sridhara S, Verma J, Arora N, Singh BP. Clinicoimmunologic studies on allergy to pulses- a case report. Indian J Allergy Asthma Immunol 2000; 14: 7-12.
11. Patil SP, Niphadkar PV, Bapat MM. Chickpea a major food
allergen in the Indian subcontinent and its clinical and immunochemical correlation. Ann Allergy Asthma Immunol
2001; 87: 140-5.
12. Burrows B, Bloom JW, Traver GA, Cline MG. The course
and prognosis of different forms of chronic airway obstruction in a sample from the general population. N Engl J Med
1987; 317: 1309-14.
13. Klinke M, Cline MG, Halonen M, Burrows B. Problems in
defining normal limits for serum IgE. J Allergy Clin Immunol 1990; 80: 440-4.
14. Clark MCA, Kilburn SA, Hourihane JOB, Dean KR, Warner
JO, Dean TP. Serological characteristics of peanut allergy.
Clin Exp Allergy 1998; 28: 1251-7.
15. Martinez TB, Garcia-Ara C, Diaz-Pena JM, Munoz FM,
Sanchez GG, Esteban MM. Validity of specific IgE antibod-
19.
20.
21.
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
198
ies in children with egg allergy. Clin Exp Allergy 2001; 31:
1464-9.
Niggemann B, Beyer K. Diagnostic pitfalls in food allergy in
children. Allergy 2005; 60: 104-7.
Vally H, de Klerk N, Thompson PJ. Asthma induced by alcoholic drinks: a new Food Allergy Questionnaire. Aust NZJ
Public Health 1999; 23: 590-4.
American Thoracic Society. Lung function testing: selection
of reference values and interpretative strategies. Am Rev
Respir Dis 1991; 144: 1202-18.
Adamopoulous G, Monolopolous L, Giotakis I. A comparison of the efficacy and the patients acceptability of budesonide and beclomethasone dipropionate aqueous nasal sprays
in patients with perennial rhinitis. Clin Otolaryngol 1995;
20: 340-4.
Dreborg S. Skin testing- the safety of skin tests and the information obtained from using different methods and concentration of allergen. Allergy 1993; 48: 473-5.
Kumari D, Kumar R, Sridhara S, Arora N, Gaur SN, Singh
BP. Sensitization to black gram in patients with bronchial
asthma and rhinitis: clinical evaluation and characterization
of allergens. Allergy 2006; 61:104-110.
Voller A, Bidwel DE, Barlett A. Enzyme-linked immunosorbant assay. Manual of Clinical Immunology. Washington, DC, American Society of Microbiology, 1980.
Anonymous. American Gastroenterological Association
Medical Position Statement: guidelines for the evaluation of
food allergies. Gasteroenterology 2001; 120: 1023-5.
Pastorello EA, Incorvaia C, Ortolani C, et al. Studies on the
relationship between the level of specific IgE antibodies and
the clinical expression of allergy. I. Definition of levels distinguishing patients with symptomatic from patients with asymptomatic allergy to common aeroallergens. J Allergy Clin
Immunol 1995; 96: 580-7.
Kerkhof M, Dubois AE, Postma DS, Schouten JP, de Monchy JG. Role and interpretation of total serum IgE measurements in the diagnosis of allergic airway disease in adults.
Allergy 2003; 58: 905-11.
Choi IS, Koh YI, Koh JS, Lee MG. Sensitivity of the skin
prick test and the specificity of the serum specific IgE test
for airway responsiveness to house dust mites in asthma. J.
Asthma 2005; 42: 197-202.
Sampson HA, Ho DG. Relationship between food specific
IgE concentrations and the risk of positive food challenges in
children and adolescents. J Allergy Clin Immunol 1997; 100:
444-51.
Martinez FD, Holberg CJ, Halonen M, Morgan WJ, Wright
AL, Taussig LM. Evidence for Mendelian inheritance of serum IgE levels in Hispanic and non-Hispanic white families.
Am J Human Genet 1994; 55: 555-65.
Burrows B, Halonen M, Lebowitz MD, Knudsen RJ, Barbee
RJ. The relationship of serum immunoglobulin E, allergy
skin tests and smoking to respiratory disorders. J Allergy
Clin Immunol 1982; 70: 199-204.
Lindberg RE, Arroyave C. Levels of IgE in serum from
normal children and allergic children as measured by an enzyme immunoassay. J Allergy Clin Immunol 1986; 78: 614-8.
Shadick NA, Sparrow D, OConnor GT, DeMolles D, Weiss
ST. Relationship of serum IgE concentration to level and rate
of decline of pulmonary function: The Normative Aging
Study. Thorax 1996; 51: 787-92.
RELEVANCE OF SERUM IgE IN ASTHMA
199
32. Taylor RG, Joyce H, Gross E, Holland F, Pride NB. Bronchial reactivity to inhaled histamine and annual rate of decline in FEV1 in male smokers and ex-smokers. Thorax
1985; 40: 9-16.
33. Sampson HA. Utility of food specific IgE concentrations in
predicting symptomatic food allergy. J Allergy Clin Immunol 2001; 107: 891-6.
34. Garcia-Ara C, Martinez TB, Diaz-Pena JM, Martin-Munoz
F, Reche-Frutos M, Martin-Esteban M. Specific IgE levels in
the diagnosis of immediate hypersensitivity to cows milk
protein in the infant. J Allergy Clin Immunol 2001; 107:
185-90.
199
Potrebbero piacerti anche
- Coal Mining Safety PDFDocumento204 pagineCoal Mining Safety PDFamiruddinNessuna valutazione finora
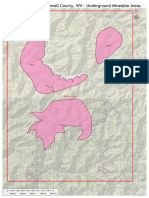
- Beckley Seam Underground Mineable AreaDocumento1 paginaBeckley Seam Underground Mineable AreaRishiraj SahooNessuna valutazione finora
- Table 28. Average Sales Price of Coal by State and Mine Type, 2018 and 2017Documento1 paginaTable 28. Average Sales Price of Coal by State and Mine Type, 2018 and 2017Rishiraj SahooNessuna valutazione finora
- USGS Time Scale FS10-3059 PDFDocumento2 pagineUSGS Time Scale FS10-3059 PDFcuiviewenNessuna valutazione finora
- FTG-10 Corridor H GuidebookDocumento89 pagineFTG-10 Corridor H GuidebookRishiraj SahooNessuna valutazione finora
- ReportDocumento46 pagineReportAlvin GuadizNessuna valutazione finora
- Mine Pool AtlasDocumento172 pagineMine Pool AtlasRishiraj SahooNessuna valutazione finora
- Coal Utilization - PrintDocumento16 pagineCoal Utilization - PrintRishiraj SahooNessuna valutazione finora
- Pub - Coal Camp Chronicles PDFDocumento261 paginePub - Coal Camp Chronicles PDFRishiraj SahooNessuna valutazione finora
- Properties Affecting Coal Utilization Coal RankDocumento37 pagineProperties Affecting Coal Utilization Coal RankRishiraj SahooNessuna valutazione finora
- Coal - A Complex Natural Resource - USGSDocumento6 pagineCoal - A Complex Natural Resource - USGSRishiraj SahooNessuna valutazione finora
- National Coal OverviewDocumento8 pagineNational Coal OverviewRishiraj SahooNessuna valutazione finora
- Coal Mining BritinicaDocumento28 pagineCoal Mining BritinicaRishiraj SahooNessuna valutazione finora
- Mine Pool AtlasDocumento172 pagineMine Pool AtlasRishiraj SahooNessuna valutazione finora
- ChapterF PDFDocumento198 pagineChapterF PDFRishiraj SahooNessuna valutazione finora
- Raoul Jacquand ContactDocumento1 paginaRaoul Jacquand ContactRishiraj SahooNessuna valutazione finora
- Holeid Projectcode Prospect East North RL Depth: Azimuth DIPDocumento2 pagineHoleid Projectcode Prospect East North RL Depth: Azimuth DIPRishiraj SahooNessuna valutazione finora
- Travel LogDocumento3 pagineTravel LogRishiraj SahooNessuna valutazione finora
- Fe Mag CalculationDocumento778 pagineFe Mag CalculationRishiraj SahooNessuna valutazione finora
- Clean Coal 2020-05-28Documento233 pagineClean Coal 2020-05-28Rishiraj SahooNessuna valutazione finora
- ChapterD PDFDocumento21 pagineChapterD PDFRishiraj SahooNessuna valutazione finora
- CoalDocumento20 pagineCoalShashankNessuna valutazione finora
- Executive Summary - CoalDocumento7 pagineExecutive Summary - CoalRishiraj SahooNessuna valutazione finora
- 2020 05 07 Clean - Coal - 1ftDocumento644 pagine2020 05 07 Clean - Coal - 1ftRishiraj SahooNessuna valutazione finora
- ChapterF PDFDocumento198 pagineChapterF PDFRishiraj SahooNessuna valutazione finora
- MIneral Comodity Summery Iron Ore-20198Documento2 pagineMIneral Comodity Summery Iron Ore-20198Rishiraj SahooNessuna valutazione finora
- Mineral Yearbook-Iron ORe-2016Documento13 pagineMineral Yearbook-Iron ORe-2016Rishiraj SahooNessuna valutazione finora
- Monthprod 2018 TotDocumento1 paginaMonthprod 2018 TotRishiraj SahooNessuna valutazione finora
- mcs2019 All PDFDocumento204 paginemcs2019 All PDFRheydel BartolomeNessuna valutazione finora
- Existing Gen Units 2017Documento12 pagineExisting Gen Units 2017Rishiraj SahooNessuna valutazione finora
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (120)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Ria ImmunoassayDocumento10 pagineRia ImmunoassayDinkey SharmaNessuna valutazione finora
- Learning Activity Sheet in Science 10Documento10 pagineLearning Activity Sheet in Science 10Sheee ShhheshNessuna valutazione finora
- CytogeneticsDocumento5 pagineCytogeneticsDennyvie Ann D. CeñidozaNessuna valutazione finora
- Structure of ADC-68, a novel carbapenem-hydrolyzing class C extended-spectrum β-lactamase isolated from Acinetobacter baumanniiDocumento14 pagineStructure of ADC-68, a novel carbapenem-hydrolyzing class C extended-spectrum β-lactamase isolated from Acinetobacter baumanniigeerthi vasanNessuna valutazione finora
- 269 - Embryology Physiology) Development of The Heart  - ÏDocumento11 pagine269 - Embryology Physiology) Development of The Heart  - ÏFood Safety CommunityNessuna valutazione finora
- Genetic Influences in Human BehaviorDocumento24 pagineGenetic Influences in Human BehaviorGuillermo ArriagaNessuna valutazione finora
- ASNC AND EANM Amyloidosis Practice Points WEBDocumento12 pagineASNC AND EANM Amyloidosis Practice Points WEBElena FlorentinaNessuna valutazione finora
- The Nervous System PDFDocumento3 pagineThe Nervous System PDFPerry SinNessuna valutazione finora
- Biological Impact of Feeding Rats With A Genetically Modified-Based DietDocumento11 pagineBiological Impact of Feeding Rats With A Genetically Modified-Based DietJesús Rafael Méndez NateraNessuna valutazione finora
- Flow Cytometry: Surface Markers and Beyond: Methods of Allergy and ImmunologyDocumento10 pagineFlow Cytometry: Surface Markers and Beyond: Methods of Allergy and ImmunologyMunir AliNessuna valutazione finora
- Swyer SyndromeDocumento1 paginaSwyer SyndromeHaNessuna valutazione finora
- AutoimunDocumento23 pagineAutoimunEllya AfianiNessuna valutazione finora
- Biology SL P2Documento8 pagineBiology SL P2KenanNessuna valutazione finora
- Aplastic Hemolitic 2021 OlgaDocumento43 pagineAplastic Hemolitic 2021 OlgalaibaNessuna valutazione finora
- Lab Report 1: Dna Extraction From Peripheral Blood Mononuclear Cells (PBMC)Documento7 pagineLab Report 1: Dna Extraction From Peripheral Blood Mononuclear Cells (PBMC)Nida RidzuanNessuna valutazione finora
- Tay-Sachs DiseaseDocumento2 pagineTay-Sachs Diseaseapi-251963850Nessuna valutazione finora
- Resume CV Dr. Kang Zhang MD PHDDocumento15 pagineResume CV Dr. Kang Zhang MD PHDKang ZhangNessuna valutazione finora
- NCERT Books For Class 11 BiotechnologyDocumento336 pagineNCERT Books For Class 11 BiotechnologyPiyush MohapatraNessuna valutazione finora
- Calcinosis Cutis Report of 4 CasesDocumento2 pagineCalcinosis Cutis Report of 4 CasesEtty FaridaNessuna valutazione finora
- Referensi CK2Documento1 paginaReferensi CK2Rahma UlfaNessuna valutazione finora
- Neural Control of MasticationDocumento34 pagineNeural Control of MasticationAnonymous k8rDEsJsU10% (1)
- Chab MTO 8e Mod 2 Final QuizDocumento24 pagineChab MTO 8e Mod 2 Final Quizshawnas09100% (1)
- Chemical Carcinogenesis I and Ii: Michael Lea 2016Documento31 pagineChemical Carcinogenesis I and Ii: Michael Lea 2016aasiyaNessuna valutazione finora
- Lymphomas: Varun. M M-Pharm (Pharmacology) IyriisemDocumento32 pagineLymphomas: Varun. M M-Pharm (Pharmacology) IyriisemPintoo Pintu100% (2)
- Leprosy: Pathogenesis Updated: ReviewDocumento15 pagineLeprosy: Pathogenesis Updated: ReviewagneselimNessuna valutazione finora
- Peripheral Neuropathy Associated With Mitochondrial Disease in ChildrenDocumento8 paginePeripheral Neuropathy Associated With Mitochondrial Disease in ChildrenRenata CardosoNessuna valutazione finora
- Brain Tumor SymtomsDocumento3 pagineBrain Tumor SymtomsvsalaiselvamNessuna valutazione finora
- Amniotic Fluid and ItDocumento8 pagineAmniotic Fluid and ItSaman SarKoNessuna valutazione finora
- Cancer Cells Induce Metastasis-Supporting Neutrophil Extracellular DNA TrapsDocumento13 pagineCancer Cells Induce Metastasis-Supporting Neutrophil Extracellular DNA TrapsJoe DaccacheNessuna valutazione finora
- Biology 1010 General ObjectivesDocumento2 pagineBiology 1010 General Objectivesapi-241247043Nessuna valutazione finora