Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Prevalence of Factors Involved in Intracranial Hemorrhage of Premature Neonates Less Than 34 Weeks
Caricato da
TriponiaTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Prevalence of Factors Involved in Intracranial Hemorrhage of Premature Neonates Less Than 34 Weeks
Caricato da
TriponiaCopyright:
Formati disponibili
ORIGINAL REPORT
PREVALENCE OF FACTORS INVOLVED IN INTRACRANIAL
HEMORRHAGE OF PREMATURE NEONATES LESS THAN 34
WEEKS
M. Rahmani*, M. Shabani , F. Nayeri and A. Alikhasi
Department of Radiology, School of Medicine, Tehran University of Medical Sciences, Tehran,
Iran
Abstract- Intracranial hemorrhage is one of the major causes of neonatal mortality and morbidity. It is
the most severe cranial problem in that period. Those who survive would be affected by hydrocephalus,
encephalomalacia, and finally brain atrophy. With accurate knowledge of risk factors, hemorrhage may
be diagnosed earlier and the complications managed earlier. This study was performed in Neonatal
Intensive Care Unit of Imam Khomeini Hospital. All the neonates less than 34 weeks of gestation were
undergone intracranial sonography from Feb 2005 to Feb 2006. Sonography was performed via anterior
fontanel with proper probe according to neonatal age. 113 neonates less than 34 weeks of gestation have
been studied. Mean gestational age was 32 weeks. Mean neonatal weight were 1566 734 grams.
Intracranial hemorrhage was evident in 21% of them; 16.8% was grade 1, 0.9% grade 2, 2.7% grade 3,
0.9% grade 4. The mean weight of neonates with hemorrhage was 1504.11 grams. Intracranial
hemorrhage had correlation with respiratory acidosis and pneumothorax. The latter was also correlated
with hemorrhage grade. Supposing the safety and non-invasiveness of intacranial sonography, we
suggest performing sonography in all premature neonates with low birth weight, and also in those
neonates with pneumothorax and respiratory acidosis.
2008 Tehran University of Medical Sciences. All rights reserved.
Acta Medica Iranica, 46(3): 249-252; 2008
Key words: Sonography, intracranial hemorrhage, premature neonate
INTRODCUTION
Intracranial hemorrhage is one of the main causes of
premature neonatal death. It is the most important,
and the most serious intracranial events in neonatal
period (1). Those neonates with severe hemorrhage
who survive suffer from sequels like hydrocephalus,
encephalomalacia, and finally cortical atrophy (2).
Since intracranial hemorrhage in neonates is not
Received:
, Revised:
, Accepted:
Corresponding Author:
Maryam Rahmani, Department of Radiology, School of Medicine,
Tehran University of Medical Sciences, Tehran, Iran
Tel: +98 21 66910200
Fax: +98 21 66910404
Email:mrahmani@yahoo.com
expressed with obvious clinical symptoms, screening
of high risk groups is of great importance (3). Risk
of intracranial hemorrhage is inversely related to
birth weight and gestational age (2).
Maternal smoking, breech presentation, sex, type
of delivery, fetal infection, and prolonged delivery,
resuscitation after birth, respiratory distress,
metabolic acidosis, and pregnancy induced
hypertension are all proposed risk factors for
neonatal intracranial hemorrhage (4, 5).
Supposing that knowing the risk factors may lead
to better prevention or early detection, we designed
this study to evaluate neonatal intracranial
hemorrhage probable risk factors in a referral center
with NICU. We used sonography as a safe, cheap,
and available diagnostic modality.
Factors involved in ICH in premature infants
MATERIALS AND METHODS
Prematurity was regarded as proven risk factor for
intracranial hemorrhage, so we evaluated all
neonates less than 34 weeks admitted in NICU of
Imam Khomeini General hospital from Feb 2005 till
Feb 2006.
Sonography was performed through anterior
fontanel using appropriate probe. Neonates with
demise before sonography and parents unwillingness
to perform sonography were excluded from the
study. According to previous studies and higher rate
of hemorrhage in the first week, we performed
sonography as soon as admission to NICU,
preferably at 4 hours after birth or the first day. If
signs of hemorrhage were seen the case was
regarded positive. If no sign of hemorrhage was
seen, the second sonography was performed at third
day. If this sonography was negative, the last
sonography was performed on the seventh
day.
Grading was performed according the following
criteria. Grade 1: germinal matrix hemorrhage, grade
2: germinal matrix and intraventricular hemorrhage
without ventricular dilatation, grade 3: germinal
matrix and intraventricular hemorrhage with
ventricular dilatation, grade 4: germinal matrix and
intraventricular and intraparenchymal hemorrhage
(6). Maternal age, type of delivery, presence of
pregnancy induced hypertension, history of
infertility treatment, fetal presentation, neonatal sex,
steroid use in pregnancy, neonatal Apgar score at 1
and 5 minuets, first neonatal hematocrite, history of
sepsis, presence of acidosis, multiparity, history of
tocolysis, history of O2 treatment more than 90%,
history of premature rupture of membrane were all
gathered in a questionnaire.
RESULTS
One hundred thirteen neonates with gestational age
less than 34 weeks were studied. Mean gestational
age, mean age of neonate on performing sonography,
mean birth weight, mean Apgar score at 1 and 5
minutes and mean first hematocrite in addition to SD
and their minimum and maximum are given in table
1.Fifty eight percent of neonates were girl and the
remaining 42% were boy. Maternal and fetal
250
Acta Medica Iranica, Vol. 46, No. 3 (2008)
Table 1. Main Characteristics of neonates
Mean
SD
Min
Max
Gestational age
32 weeks
25
34
Age on sonography
3.6 days
Birth weight
1566 gr
734
540
3800
Apgar at 1 min
6.7
2.2
Apgar at 5 min
8.3
10
First Hct
46.7
11.9
13
68
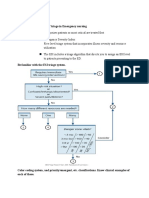
conditions in neonates included in our study are
given in Figure 1.
Respiratory acidosis was evident in 29.5% of
neonates. In 81.1% antibiotics were administered.
4.9% had pneumothorax, while in 29.2% mechanical
ventilation was used, and 5.8% of whom CPAP
mode were also used, 39.6% had history of maternal
hypertension, 80.6% of neonates were singleton, and
16.5% were twins, 1.9% triples, and 1% quadriples.
In 30% history of PROM, and in 4.3% history of
tocolysis were obtained. 3.1% of the mothers
experienced prolonged delivery, and 8.3% of them
used steroid during pregnancy, 9.4% of neonates
were born through infertility treatment. 21.2% of
neonates had intracranial hemorrhage that 16.8% had
grade 1, 0.9% had grade 2, 2.7% had grade 3, and
0.9% of them had grade 4 intracranial hemorrhage
according to sonographic criteria . Mean Apgar score
in 1 minute was 5.81 2.4 and 6.85 2.19 in those
with and without hemorrhage respectively. This
difference was not statistically significant (P = 0.12).
At 5 minutes, the Apgar score was 8 2.09 and
8.39 2.01 in neonates with and without
hemorrhage, respectively, that again were not
different significantly (P = 0.5). Mean first
hematocrite of neonates with and without
hemorrhage 50.01 7.82 and 45.77 12.61 percent
respectively. These figures failed to show significant
difference (P = 0.8). Mean maternal age of neonates
with hemorrhage was 26.135.4 years, while in
neonates without hemorrhage mean maternal age
was 28.29 6.06 years, which was not statistically
different from those with hemorrhage (P = 0.6). 50%
of neonates with hemorrhage were boys and another
50% were girls. No statistical correlation was found
between gender and hemorrhage (X2, P = 0.6).
54.16% of neonates with hemorrhage had metabolic
acidosis, no significant correlation was obtained (X2,
P = 0.07), while a statistically significant correlation
M. Rahmani et al.
90
80
70
60
50
40
30
20
10
0
Respiratory
Acidosis
Antibiotic Use
Pneumothorax
Mechanical
Ventilation
Maternal
Hypertension
Multiple
Pregnancy
PROM
Tocolysis
Prolonged
Delivery
Steroid Use
Infertility
treatment
Fig. 1. Maternal and fetal condition in hemorrhage
was found between respiratory acidosis and
hemorrhage (X2, P = 0.02). 70.83% of neonates with
hemorrhage received antibiotics, which failed to
show significant correlation with hemorrhage (X2, P
= 0.6). 37.5% of neonates with hemorrhage had
history of maternal hypertension during pregnancy.
Maternal hypertension did not have correlation with
hemorrhage (X2, P = 0.78). Mechanical ventilation
used in 16.66% of hemorrhages. Statistically
mechanical ventilation failed to show significant
correlation with hemorrhage (X2, P = 0.78).
Pneumothorax was present in 8.3% of neonates with
hemorrhage, which had statistically significant
correlation with hemorrhage (X2, P < 0.000). In
addition pneumothorax had positive correlation with
the grade of hemorrhage, which means neonates with
pneumothorax had higher grades of hemorrhage.
16.66% of neonates were results of multiple
pregnancies. Multiple pregnancy had not significant
correlation with hemorrhage (X2, P = 0.8). In 12.5%
of the neonates with hemorrhage, tocolysis treatment
had been used during pregnancy. Tocolysis does not
seem to have significant correlation with hemorrhage
(X2, P = 0.6). None of the neonates with hemorrhage
were the result of prolonged delivery or had history
of steroid usage in mother. Infertility treatment was
performed in 3.1% of neonates with hemorrhage. It
failed to show statistical significance (X2, P = 0.4).
Premature rupture of membrane (PROM) was
present in 29.16% of neonates with hemorrhage.
PROM does not have significant correlation with
hemorrhage (X2, P = 0.3).
DISCUSSION
In our study 21% of neonates had intracranial
hemorrhage.In Previous studies prevalence of
intracranial hemorrhage was 10 to 70% depending
on the gestational age and weight of the neonates
included in the study. Intracranial hemorrhage in
neonates has different types. The most common
types are intraventricular, and germinal matrix
hemorrhage. Birth weight and gestational age
were main risk factors in several studies including a
study in Sangerardo hospital (5), so our
study included only neonates with low gestational
age. Among the studied risk factors, only
pneumothorax and respiratory acidosis had
significant
correlation
with
hemorrhage.
Pneumothorax had also positive correlation with
hemorrhage grade. In Nehma Lider and colleagues
study in 2003 depicted that every one mmHg
decrease in PCO2 in the first 24 hours of neonatal
age will decrease risk of intracranial hemorrhage (4).
Meanwhile Jaeger and co-workers declared that
there was no correlation with arterial blood gas and
intracranial hemorrhage (7).
Continuous improvement in premature neonatal
care leads to survive more and more neonates with
very low birth weight and gestational age who are
severely prone to different complications including
intracranial hemorrhage. Along this better
instruments and techniques will lead to diagnose
lower grade intracranial hemorrhages, which need
great care in order to diminish the complications.
Acta Medica Iranica, Vol. 46, No. 3 (2008)
251
Factors involved in ICH in premature infants
In conclusion, supposing the safety and noninvasiveness of intacranial sonography, we suggest
performing sonography in all premature neonates
with low birth weight, and also in those neonates
with pneumothorax and respiratory acidosis.
Conflict of interests
The authors declare that they have no competing
interests.
REFERENCES
1. Richard E. Behrman, Robert M. Kliegman , Hal B.
Jenson. Nelson Textbook of pediatrics. 17th edition:
Saunders, 2007.
2. Fanaroff Avory A, Martin Richard J. Perinatal
Medicine. 17th edition: st . louis: Mosby; 2002: P 879887.
252
Acta Medica Iranica, Vol. 46, No. 3 (2008)
3. Fredric N. Sllverman, Jerald P.Kuhn. Caffeys pediatric
X-ray Diagnosis. 10th edition: Mosby; 2004: 285295.
4. Nehma lider, Orli Haskin, Orlilevit. Risk factors for
intracranial hemorrhage in very low birth weight
premature infunts. Pediatrics 2003; 111: 590-595.
5. Vergani P, Locatelli A, Doria V, Assi F, Paterlini G,
Pezzullo JC, Ghidini A. Intraventricular hemorrhage
and periventricular leukomalacia in preterm infants.
Obstet Gynecol. 2004 Aug; 104(2):225-231.
6. Daivid Sutton, Philip J.A. Robson. Textbook of
radiology and imaging. 7th edition: Cherchil
Livingstone; 2003
7. Jaeger M, Grssner SE, Omwandho CO, Klein K,
Tinneberg HR, Klingmller V. [Cranial sonography for
newborn screening: a 10-year retrospective study in
11,887 newborns]. Rofo. 2004 Jun;176(6):852-858.
German.
Potrebbero piacerti anche
- The Mindbody Workbook - Mar 2013Documento7 pagineThe Mindbody Workbook - Mar 2013paul lukawski100% (6)
- (Mahesh Chandra) Objective Cardiology PDFDocumento609 pagine(Mahesh Chandra) Objective Cardiology PDFfajarNessuna valutazione finora
- Anatomy and Physiology of PlacentaDocumento5 pagineAnatomy and Physiology of PlacentaAdrianne Basa100% (1)
- First-Trimester Ultrasound Nuchal Translucency Screening For Fetal AneuploidyDocumento37 pagineFirst-Trimester Ultrasound Nuchal Translucency Screening For Fetal AneuploidyCTAFDocumentsNessuna valutazione finora
- 2004, Vol.31, Issues 1, Ultrasound in ObstetricsDocumento213 pagine2004, Vol.31, Issues 1, Ultrasound in ObstetricsFebrinata MahadikaNessuna valutazione finora
- What Is Sonography? What Does A Diagnostic Medical Sonographer Do? What Are The Career Opportunities?Documento2 pagineWhat Is Sonography? What Does A Diagnostic Medical Sonographer Do? What Are The Career Opportunities?yogimgurtNessuna valutazione finora
- Hamstring StrainDocumento13 pagineHamstring Strainaraaff100% (2)
- SAMPLE FDAR CHARTING PainDocumento1 paginaSAMPLE FDAR CHARTING Painjpm100% (1)
- SJT Med SchoolDocumento101 pagineSJT Med SchoolErine Novita BasukiNessuna valutazione finora
- Fluids - and - Electrolytes - Cheat - Sheet - PDF Filename - UTF-8''Fluids and Electrolytes Cheat Sheet-1Documento6 pagineFluids - and - Electrolytes - Cheat - Sheet - PDF Filename - UTF-8''Fluids and Electrolytes Cheat Sheet-1RevNessuna valutazione finora
- The Placenta and Neurodisability 2nd EditionDa EverandThe Placenta and Neurodisability 2nd EditionIan CrockerNessuna valutazione finora
- Nsg241 Study Guide Exam 5Documento76 pagineNsg241 Study Guide Exam 5NatalieAndersonNessuna valutazione finora
- Oral Cancer 26.3.19Documento23 pagineOral Cancer 26.3.19Pradeep100% (2)
- CAD/CAM Dentistry and Chairside Digital Impression Making: 4 CE CreditsDocumento11 pagineCAD/CAM Dentistry and Chairside Digital Impression Making: 4 CE CreditsShraddha AgarwalNessuna valutazione finora
- Monitoring & Care of Ventilated ChildrenDocumento12 pagineMonitoring & Care of Ventilated ChildrenRajakumar Padur Sivaraman100% (2)
- Personality DisorderDocumento15 paginePersonality DisorderDherick RosasNessuna valutazione finora
- NaloxoneDocumento3 pagineNaloxoneTracyNessuna valutazione finora
- Maternal and Fetal Outcome of Placenta PDocumento5 pagineMaternal and Fetal Outcome of Placenta Pfamelalusu eaNessuna valutazione finora
- 33873-Article Text-121761-1-10-20170831Documento6 pagine33873-Article Text-121761-1-10-20170831AnggaNessuna valutazione finora
- Ijph 41 92Documento7 pagineIjph 41 92Trung Kien VoNessuna valutazione finora
- Patient's Profile With Hypertension in Pregnancy PatientsDocumento6 paginePatient's Profile With Hypertension in Pregnancy PatientsHendrik SuTopo LidaprajaNessuna valutazione finora
- Neonatal Complications of Premature Rupture of Membranes: AbstractDocumento5 pagineNeonatal Complications of Premature Rupture of Membranes: AbstractPaula CyntiaNessuna valutazione finora
- Neonatal Complications of Premature Rupture of Membranes: AbstractDocumento5 pagineNeonatal Complications of Premature Rupture of Membranes: AbstractAris BayuNessuna valutazione finora
- Journal Atonia Uteri YuyunDocumento6 pagineJournal Atonia Uteri YuyunMoh RamliNessuna valutazione finora
- 37004-Article Text-130842-2-10-20180629Documento5 pagine37004-Article Text-130842-2-10-20180629nishita biswasNessuna valutazione finora
- Aggressive Intervention of Previable Preterm Premature Rupture of MembranesDocumento8 pagineAggressive Intervention of Previable Preterm Premature Rupture of MembranesVanessa Riaño GodoyNessuna valutazione finora
- PT Resp OutcomesDocumento6 paginePT Resp OutcomesHarish SudarsananNessuna valutazione finora
- (Sici) 1097 0215 (19970529) 71 5 800 Aid Ijc18 3.0Documento7 pagine(Sici) 1097 0215 (19970529) 71 5 800 Aid Ijc18 3.0Moh RamliNessuna valutazione finora
- Ijrm 11 385Documento6 pagineIjrm 11 385Obgyn Maret 2019Nessuna valutazione finora
- RM 12021Documento4 pagineRM 12021liana devi oktaviaNessuna valutazione finora
- Risk Factors Associated With Fetal Pleural Effusion in Prenatal Diagnosis: A Retrospective Study in A Single Institute in Southern ChinaDocumento6 pagineRisk Factors Associated With Fetal Pleural Effusion in Prenatal Diagnosis: A Retrospective Study in A Single Institute in Southern Chinachristian roblesNessuna valutazione finora
- Maternal Hypothyroidism During Pregnancy and The Risk of Pediatric Endocrine Morbidity in The OffspringDocumento6 pagineMaternal Hypothyroidism During Pregnancy and The Risk of Pediatric Endocrine Morbidity in The OffspringlananhslssNessuna valutazione finora
- 39 Iajps39052018 PDFDocumento5 pagine39 Iajps39052018 PDFiajpsNessuna valutazione finora
- BMC Pediatrics PregnancyDocumento8 pagineBMC Pediatrics PregnancyMobin Ur Rehman KhanNessuna valutazione finora
- A 5-Year Review of Pattern of Placenta Previa in Ilorin, NigeriaDocumento6 pagineA 5-Year Review of Pattern of Placenta Previa in Ilorin, Nigeriaamalia chairunnisaNessuna valutazione finora
- An Overview of Referral Patients With Severe Preeclampsia in Obstetric and Gynecology Department, Dr. Soetomo Hospital Surabaya in 2011 An OverviewDocumento10 pagineAn Overview of Referral Patients With Severe Preeclampsia in Obstetric and Gynecology Department, Dr. Soetomo Hospital Surabaya in 2011 An OverviewAnonymous y6NmP9NHkYNessuna valutazione finora
- 216 FTPDocumento8 pagine216 FTPapi-289577018Nessuna valutazione finora
- Clinical Risk Factor For Preeclamsia in Twin PregnanciesDocumento8 pagineClinical Risk Factor For Preeclamsia in Twin PregnanciesLouis HadiyantoNessuna valutazione finora
- Alexander 1999Documento5 pagineAlexander 1999Hòa HồNessuna valutazione finora
- Short-Term Outcomes and Mortality of Late Preterm Infants: Cahide Bulut, Tuğba Gürsoy, Fahri OvalıDocumento6 pagineShort-Term Outcomes and Mortality of Late Preterm Infants: Cahide Bulut, Tuğba Gürsoy, Fahri OvalızulfikarNessuna valutazione finora
- Scenario of Neonatal Respiratory Distress in Tertiary HospitalDocumento5 pagineScenario of Neonatal Respiratory Distress in Tertiary HospitalSulabh ShresthaNessuna valutazione finora
- Chorioamnionitis and Prognosis For Term Infants-13Documento5 pagineChorioamnionitis and Prognosis For Term Infants-13ronny29Nessuna valutazione finora
- Scopus (29) Many2017Documento7 pagineScopus (29) Many2017ika puspitaNessuna valutazione finora
- Amniocentesis Results and Retrospective Analysis Performed in The University ClinicDocumento6 pagineAmniocentesis Results and Retrospective Analysis Performed in The University ClinicCindy Denti PratikasariNessuna valutazione finora
- Medical Record Validation of Maternally Reported History of PreeclampsiDocumento7 pagineMedical Record Validation of Maternally Reported History of PreeclampsiezaNessuna valutazione finora
- Placenta Praevia: Correlation With Caesarean Sections, Multiparity and SmokingDocumento6 paginePlacenta Praevia: Correlation With Caesarean Sections, Multiparity and SmokingSaeffurqonNessuna valutazione finora
- Omj D 09 00101Documento6 pagineOmj D 09 00101DewinsNessuna valutazione finora
- Mon 2018Documento7 pagineMon 2018Nadieda Ayu MarthalitasariNessuna valutazione finora
- Gim 20047Documento4 pagineGim 20047Sabhina AnseliaNessuna valutazione finora
- Indications and Risks of Vacuum Assisted Deliveries.: OriginalDocumento2 pagineIndications and Risks of Vacuum Assisted Deliveries.: OriginalgagagigoNessuna valutazione finora
- 61 Goepfert2004Documento7 pagine61 Goepfert2004angela_karenina_1Nessuna valutazione finora
- Management of Monochorionic Twin Pregnancy: Green-Top Guideline No. 51Documento13 pagineManagement of Monochorionic Twin Pregnancy: Green-Top Guideline No. 51indra_strongNessuna valutazione finora
- Screening Utility of Umbilical Artery Doppler Indices in Patients With PreeclampsiaDocumento6 pagineScreening Utility of Umbilical Artery Doppler Indices in Patients With PreeclampsiaAlhajiNessuna valutazione finora
- Premature Rupture of Membrane ReadingDocumento4 paginePremature Rupture of Membrane ReadingAdrienne Nicole AlforteNessuna valutazione finora
- Fetal Intracranial Hemorrhage: Is Minor Maternal Trauma A Possible Pathogenetic Factor?Documento8 pagineFetal Intracranial Hemorrhage: Is Minor Maternal Trauma A Possible Pathogenetic Factor?Kareem AhmedNessuna valutazione finora
- First Trimester Bleeding and Pregnancy Outcomes: Case-Control StudyDocumento4 pagineFirst Trimester Bleeding and Pregnancy Outcomes: Case-Control StudyClara Nur RamadhaniNessuna valutazione finora
- Karakteristik Perdarahan Antepartum Dan Perdarahan PostpartumDocumento7 pagineKarakteristik Perdarahan Antepartum Dan Perdarahan PostpartumHumam UddinNessuna valutazione finora
- Preterm Premature Rupture of Membranes: Diagnosis, Evaluation and Management StrategiesDocumento6 paginePreterm Premature Rupture of Membranes: Diagnosis, Evaluation and Management StrategiesResi Lystianto PutraNessuna valutazione finora
- Placental Abruption.Documento6 paginePlacental Abruption.indahNessuna valutazione finora
- Prediction of Recurrent Preeclampsia Using First-Trimester Uterine Artery DopplerDocumento6 paginePrediction of Recurrent Preeclampsia Using First-Trimester Uterine Artery Dopplerganesh reddyNessuna valutazione finora
- 1 s2.0 S0020729209615502 Main PDFDocumento1 pagina1 s2.0 S0020729209615502 Main PDFPaula UrsuNessuna valutazione finora
- Incidence of Morbidity and Mortality in Neonate Born To Mothers With Premature Rupture of MembranesDocumento7 pagineIncidence of Morbidity and Mortality in Neonate Born To Mothers With Premature Rupture of MembranesTatik HandayaniNessuna valutazione finora
- Prognostic Factors and Clinical Features in Liveborn Neonates With Hydrops FetalisDocumento6 paginePrognostic Factors and Clinical Features in Liveborn Neonates With Hydrops FetalisWulan CerankNessuna valutazione finora
- Al Riyami-2020-Respiratory Distress Syndrome IDocumento6 pagineAl Riyami-2020-Respiratory Distress Syndrome IHidayatt NurulNessuna valutazione finora
- An-Evaluation-Of-Risk-Factors-In-Cases-Of-Perinatal-Asphyxia-9563 2021Documento4 pagineAn-Evaluation-Of-Risk-Factors-In-Cases-Of-Perinatal-Asphyxia-9563 2021Chiki CacaNessuna valutazione finora
- Maternal and Perinatal Complications of Severe Preeclampsia in Three Referral Hospitals in Yaoundé, CameroonDocumento8 pagineMaternal and Perinatal Complications of Severe Preeclampsia in Three Referral Hospitals in Yaoundé, CameroonIke Istofani KNessuna valutazione finora
- Complications Associated With Amniocentesis in The Third TrimesterDocumento14 pagineComplications Associated With Amniocentesis in The Third Trimesteruzlifatil jannahNessuna valutazione finora
- Mousavi 2018Documento6 pagineMousavi 2018Alexandra MateiNessuna valutazione finora
- Maternal and Fetal Outcomes in Term Premature Rupture of MembraneDocumento6 pagineMaternal and Fetal Outcomes in Term Premature Rupture of MembraneMuhammad Fikri RidhaNessuna valutazione finora
- Journal Ectopic Pregnancy-A Rising TrendDocumento5 pagineJournal Ectopic Pregnancy-A Rising TrendEricNessuna valutazione finora
- Previous Abortions and Risk of Pre-Eclampsia: Reproductive HealthDocumento8 paginePrevious Abortions and Risk of Pre-Eclampsia: Reproductive HealthelvanNessuna valutazione finora
- Placenta PreviaDocumento5 paginePlacenta PreviaKuro HanabusaNessuna valutazione finora
- Risk Factors of Persistent Pulmonary Hypertension of Newborn (PPHN) in Different GestationDocumento6 pagineRisk Factors of Persistent Pulmonary Hypertension of Newborn (PPHN) in Different Gestationzionluis007Nessuna valutazione finora
- DyslipidemiaDocumento87 pagineDyslipidemiaCarlos Arturo Paternina Cuello100% (1)
- BLT 11 518Documento10 pagineBLT 11 518TriponiaNessuna valutazione finora
- Neonatal Vomiting: R. Shaoul N.L. JonesDocumento2 pagineNeonatal Vomiting: R. Shaoul N.L. JonesTriponiaNessuna valutazione finora
- Intraventricular HaemorrhageDocumento9 pagineIntraventricular HaemorrhageTriponiaNessuna valutazione finora
- DiphtheriaDocumento12 pagineDiphtheriajenconlu_11Nessuna valutazione finora
- Intracranial Hemorrhage in Full-Term Newborns: A Hospital-Based Cohort StudyDocumento10 pagineIntracranial Hemorrhage in Full-Term Newborns: A Hospital-Based Cohort StudyTriponiaNessuna valutazione finora
- Diphtheria 388970 7Documento5 pagineDiphtheria 388970 7TriponiaNessuna valutazione finora
- Risk Factors of Acquired Prothrombin Complex Deficiency Syndrome A Case-Control StudyDocumento8 pagineRisk Factors of Acquired Prothrombin Complex Deficiency Syndrome A Case-Control StudyTriponiaNessuna valutazione finora
- Australian Public Assessment Report For Human Prothrombin ComplexDocumento51 pagineAustralian Public Assessment Report For Human Prothrombin ComplexTriponiaNessuna valutazione finora
- Intracranial Hemorrhageinthe Preterm I Nfa NT: Under ST A Nding It, Preventing ItDocumento26 pagineIntracranial Hemorrhageinthe Preterm I Nfa NT: Under ST A Nding It, Preventing ItTriponiaNessuna valutazione finora
- Intracranial Hemorrhage in Full-Term Newborns: A Hospital-Based Cohort StudyDocumento10 pagineIntracranial Hemorrhage in Full-Term Newborns: A Hospital-Based Cohort StudyTriponiaNessuna valutazione finora
- The Shapes of Head and Face in Normal Male Newborns in South-East of Caspian Sea (Iran-Gorgan)Documento4 pagineThe Shapes of Head and Face in Normal Male Newborns in South-East of Caspian Sea (Iran-Gorgan)TriponiaNessuna valutazione finora
- 00 B 4952850536271 A 0000000Documento6 pagine00 B 4952850536271 A 0000000TriponiaNessuna valutazione finora
- Intracranial Hemorrhage in Full-Term Newborns: A Hospital-Based Cohort StudyDocumento10 pagineIntracranial Hemorrhage in Full-Term Newborns: A Hospital-Based Cohort StudyTriponiaNessuna valutazione finora
- 43 5 6 3 PDFDocumento3 pagine43 5 6 3 PDFTriponiaNessuna valutazione finora
- Hydrocortisone Treatment For Bronchopulmonary Dysplasia and Brain Volumes in Preterm InfantsDocumento7 pagineHydrocortisone Treatment For Bronchopulmonary Dysplasia and Brain Volumes in Preterm InfantsTriponiaNessuna valutazione finora
- Journal Pone 0000192Documento5 pagineJournal Pone 0000192TriponiaNessuna valutazione finora
- A JR CCM 183121715Documento8 pagineA JR CCM 183121715TriponiaNessuna valutazione finora
- 11chronic Lung Disease in Preterm InfantsDocumento7 pagine11chronic Lung Disease in Preterm InfantsTriponiaNessuna valutazione finora
- 00 B 4952850536271 A 0000000Documento6 pagine00 B 4952850536271 A 0000000TriponiaNessuna valutazione finora
- BPD Pathogen Es IsDocumento10 pagineBPD Pathogen Es IsTriponiaNessuna valutazione finora
- Ventilation and Chronic Lung DiseaseDocumento17 pagineVentilation and Chronic Lung DiseaseTriponiaNessuna valutazione finora
- LDD 08 RDS BPDDocumento6 pagineLDD 08 RDS BPDFaizan AbbasiNessuna valutazione finora
- 11chronic Lung Disease in Preterm InfantsDocumento7 pagine11chronic Lung Disease in Preterm InfantsTriponiaNessuna valutazione finora
- Triage Depkes APDocumento23 pagineTriage Depkes APTriponiaNessuna valutazione finora
- Review Article: Postnatal Corticosteroids For Prevention and Treatment of Chronic Lung Disease in The Preterm NewbornDocumento13 pagineReview Article: Postnatal Corticosteroids For Prevention and Treatment of Chronic Lung Disease in The Preterm NewbornTriponiaNessuna valutazione finora
- Terobosan Baru Penanganan Krisis HipertensiDocumento37 pagineTerobosan Baru Penanganan Krisis HipertensiTriponiaNessuna valutazione finora
- Nonsteroidal Anti-Inflammatory DrugsDocumento21 pagineNonsteroidal Anti-Inflammatory DrugsTriponiaNessuna valutazione finora
- Management Pain and Inflammation - Stand Alone Symp CLXDocumento41 pagineManagement Pain and Inflammation - Stand Alone Symp CLXTriponiaNessuna valutazione finora
- Evaluation of The Vertical Holding Appliance in Treatment of High-Angle PatientsDocumento6 pagineEvaluation of The Vertical Holding Appliance in Treatment of High-Angle PatientsDrGurinder KanwarNessuna valutazione finora
- Introduction To Patient Centred Communication 20-21Documento16 pagineIntroduction To Patient Centred Communication 20-21Ngetwa TzDe TheWirymanNessuna valutazione finora
- Failure Mode and Effect Analysis (FMEA) Sanglah General Hospital 2012Documento28 pagineFailure Mode and Effect Analysis (FMEA) Sanglah General Hospital 2012ferekonstantinusNessuna valutazione finora
- How To Perform A Head To Toe AssessmentDocumento2 pagineHow To Perform A Head To Toe AssessmentLalaine RomeroNessuna valutazione finora
- CIT Training MAL Manual PDFDocumento18 pagineCIT Training MAL Manual PDFFilozófus ÖnjelöltNessuna valutazione finora
- Cerebrovascular Accident CVADocumento8 pagineCerebrovascular Accident CVAFlora Angeli PastoresNessuna valutazione finora
- Acute and Chronic Gastritis Due To Helicobacter PyloriDocumento8 pagineAcute and Chronic Gastritis Due To Helicobacter PyloriCarla HolandNessuna valutazione finora
- Clinical Approach To Rapidly Progressive Renal FailureDocumento6 pagineClinical Approach To Rapidly Progressive Renal FailureBryan RamseyNessuna valutazione finora
- Aae Endodonticglossary2016Documento50 pagineAae Endodonticglossary2016h20pologtNessuna valutazione finora
- Concept of Client TeachingDocumento6 pagineConcept of Client TeachingJoy Anne Lumbres0% (1)
- Stage 1 Visit 1Documento15 pagineStage 1 Visit 1amritakhatra7Nessuna valutazione finora
- 1993 92 723 Larry J. Baraff: Capillary Refill: Is It A Useful Clinical Sign?Documento4 pagine1993 92 723 Larry J. Baraff: Capillary Refill: Is It A Useful Clinical Sign?Citty'Q' HuwalidNessuna valutazione finora
- Maintaining Body AlignmentDocumento6 pagineMaintaining Body AlignmentJan Jamison ZuluetaNessuna valutazione finora
- Nursing Trends Paper: Nursing InformaticsDocumento6 pagineNursing Trends Paper: Nursing Informaticscwarrington09Nessuna valutazione finora
- Enteral Nutrition: Sana Inam Lecturer College of Pharmacy, GCUFDocumento18 pagineEnteral Nutrition: Sana Inam Lecturer College of Pharmacy, GCUFAnum AzamNessuna valutazione finora
- Partial List of Mental Health Services in Metro ManilaDocumento3 paginePartial List of Mental Health Services in Metro ManilaTinoRepaso100% (2)