Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Gupta - Echocardiographic Evaluation of Heart in COPD and Corelation With Severity
Caricato da
xtraqrkyCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Gupta - Echocardiographic Evaluation of Heart in COPD and Corelation With Severity
Caricato da
xtraqrkyCopyright:
Formati disponibili
Original Article
Echocardiographic evaluation of heart in chronic obstructive
pulmonary disease patient and its co-relation with the
severity of disease
N. K. Gupta, Ritesh Kumar Agrawal, A. B. Srivastav, M. L. Ved
Department of Tuberculosis and Chest Diseases, R N T Medical College, Udaipur, Rajasthan, India
ABSTRACT
Background: Chronic obstructive pulmonary disease (COPD) has considerable effects on cardiac functions, including
those of the right ventricle, left ventricle, and pulmonary blood vessels. Most of the increased mortality associated with
COPD is due to cardiac involvement. Echocardiography provides a rapid, noninvasive, portable, and accurate method
to evaluate the cardiac changes. Aims: To assess the cardiac changes secondary to COPD by echocardiography and
to find out the correlation between echocardiographic findings and severity of COPD, if there is any. Materials and
Methods: A total 40 of patients of COPD were selected and staged by pulmonary function test (PFT) and evaluated
by echocardiography. Results: On echocardiographic evaluation of COPD, 50% cases had normal echocardiographic
parameters. Measurable tricuspid regurgitation (TR) was observed in 27/40 cases (67.5%). Pulmonary hypertension (PH),
which is defined as systolic pulmonary arterial pressure (sPAP) > 30 mmHg was observed in 17/27 (63%) cases in which
prevalence of mild, moderate, and severe PH were 10/17 (58.82%), 4/17 (23.53%), and 3/17 (17.65%), respectively.
The frequencies of PH in mild, moderate, severe, and very severe COPD were 16.67%, 54.55%, 60.00%, and 83.33%,
respectively. Right atrial pressure was 10 mmHg in 82.5% cases and 15 mmHg in 17.5% cases. Cor pulmonale was
observed in 7/17 (41.17%) cases; 7.50% cases had left ventricle (LV) systolic dysfunction and 47.5% cases had evidence
of LV diastolic dysfunction defined as A E (peak mitral flow velocity of the early rapid filling wave (E), peak velocity
of the late filling wave caused by atrial contraction (A) on mitral valve tracing). Left ventricle hypertrophy was found in
22.5% cases. Conclusion: Prevalence of PH has a linear relationship with severity of COPD and severe PH is almost
associated with cor pulmonale. Echocardiography helps in early detection of cardiac complications in COPD cases
giving time for early interventions.
KEY WORDS: Chronic obstructive pulmonary disease, cor pulmonale, echocardiography, pulmonary hypertension
Address for correspondence: Dr. Ritesh Kumar Agrawal, Rajkumar Cloth Store, Rauja Bazar Mau, Mau Nath Bhanjan, India. E-mail: dr.ritesh_99@yahoo.com
INTRODUCTION
Chronic obstructive pulmonary disease (COPD), defined
by GOLD as a preventable and treatable disease with some
significant extrapulmonary effects, is a very common
clinical entity in clinical practice. COPD is a leading
cause of death and disability worldwide. According to
World Bank data it is expected to move from its status in
Access this article online
Quick Response Code:
Website:
www.lungindia.com
DOI:
10.4103/0970-2113.80321
2000 as the 4th and 12th most frequent cause of mortality
and morbidity, respectively, to the 3rd and 5th leading
cause of mortality and morbidity, respectively, in 2020.[1,2]
COPD is associated with significant extrapulmonary
(systemic) effects among which cardiac manifestations
are most common. Cardiovascular disease accounts for
approximately 50% of all hospitalization and nearly one
third of all deaths, if forced expiratory volume in one
second (FEV1) > 50% of predicted.[3] In more advanced
disease cardiovascular disease account for 20%25%
of all deaths in COPD.[4] COPD affects pulmonary blood
vessels, right ventricle, as well as left ventricle leading to
development of pulmonary hypertension, cor pulmonale,
right ventricular dysfunction, and left ventricular
dysfunction too. Echocardiography provides a rapid,
noninvasive portable and accurate method to evaluate the
right ventricle function, right ventricular filling pressure,
Lung India Vol 28 Issue 2 Apr - Jun 2011 105
Gupta, et al.: Echocardiographic evaluation of heart in COPD patient
tricuspid regurgitation, left ventricular function and
valvular function.[5] Many studies have confirmed that
echocardiographically derived estimates of pulmonary
arterial pressure co-relate closely with pressures measured
by right heart catheter (r > 0.7).[6,7]
Hence the present study was undertaken with the following
aims and objectives:
1. To assess the cardiac changes secondary to COPD by
echocardiography, and
2. To find out the correlation between echocardiographic
findings and the severity of COPD using GOLD
guidelines.
MATERIALS AND METHODS
Forty patients of COPD confirmed by clinical history,
radiology of chest, and pulmonary function test were
selected from Chest and T.B. Hospital of R.N.T. Medical
College, Udaipur, Rajasthan. During selection, patients
with H/O of chronic lung disease other than COPD,
hypertension, any primary cardiac disease, any systemic
disease that can cause pulmonary hypertension, patients
with poor echo window, and patients who were unable to
perform spirometry were excluded from the study.
All selected patients were subjected to routine
investigations, including complete blood count, lipid
profile, blood sugar, blood urea, serum creatinine,
electrocardiography, and so on, as needed.
All the patients were investigated by spirometry and
diagnosed and classified according to GOLD guidelines
(postbronchodilator FEV 1/forced vital capacity (FVC)
ratio < 70% predicted), mild (FEV1 80% of predicted),
moderate (50% FEV1 < 80% predicted), severe (30%
FEV1 < 50% predicted), and very severe (FEV1 < 30%
predicted), respectively.
All patients were subjected to resting two-dimension
transthoracic Doppler echocardiography in the cardiology
department of R.N.T. Medical College and associated
hospitals by expert cardiologists. The machine used
was VIVID 7 model of GE health care system with a
multifrequency probe with a range of 24.3 MHz. Both 2D
and M-Mode studies were done.
Echocardiography was reviewed to assess the pericardium,
valvular anatomy and function, left and right side chamber
size and cardiac function. Tricuspid regurgitant flow
was identified by color flow Doppler technique and the
maximum jet velocity was measured by continuous wave
Doppler without the use of intravenous contrast. Right
ventricular systolic pressure was estimated based on the
modified Bernoulli equation and was considered to be
equal to the sPAP in the absence of right ventricular outflow
obstruction: sPAP (mmHg) = right ventricular systolic
pressure = trans-tricuspid pressure gradient (TTPG) +
106
right atrial pressure (RAP), where trans-tricuspid gradient
is 4v2 (v = peak velocity of tricuspid regurgitation, m/s).[6,8,9]
RAP was empirically estimated as 15 mmHg before 1997.
Since 1997, RAP was estimated to be 5, 10, or 15 mmHg
based on the variation in the size of inferior vena cava with
inspiration as follows: complete collapse, RAP = 5 mmHg;
partial collapse, RAP = 10 mmHg; and no collapse, RAP
= 15 mmHg.[10]
Pulmonary hypertension (PH) was defined in this study
as sPAP 30 mmHg.[11] This value was chosen according
to the definition of pulmonary hypertension. PH was
classified into mild, moderate, and severe category as sPAP
3050, 5070, >70 mmHg, respectively (using Chemla
formula, mean pulmonary arterial pressure (MPAP) =0.61
PASP + 2 mmHg and putting value of 2535, 3545, and
>45 mmHg of MPAP for mild, moderate, and severe
pulmonary hypertension, respectively).[12]
Right ventricle dimension was measured by M-Mode echo
and right ventricular dilation or cor pulmonale was said to
be present when it exceeded the normal range of 0.92.6
cm. Right ventricle contractility was also noted and right
ventricular systolic dysfunction was said to be present
when it was hypokinetic.
Left ventricular function was also assessed by using the
following parameters: EF (ejection fraction) = measure
of how much end-diastolic value is ejected from LV with
each contraction (56%78%).
FS (fractional shortening) = it is a percentage change in LV
dimension with each LV contraction (28%44%).
LV mass = left ventricular mass (88224 g).
E/A = diastolic filling of left ventricles usually classified
initially on the basis of the peak mitral flow velocity
of the early rapid filling wave (E), peak velocity of the
late filling wave caused by atrial contraction (A). In
normal subjects LV elastic recoil is vigorous because
of normal myocardial relaxation, therefore more filling
is completed during early diastolic, so left ventricular
diastolic dysfunction (LVDD) is said to be present when
E/A is <1.3 (age group 4549 years), <1.2 (age group
5059 years), <1.0 (age group 6069 years), and <0.8
(age group 70 years).[13]
RESULTS
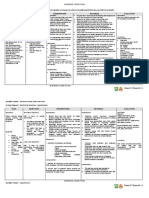
A total of 40 patients were recruited in our study and out of
them, the number of patients with mild, moderate, severe,
and very severe COPD were 18/40 = 45%, 11/40 = 27.5%,
5/40 = 12.5%, and 6/40 = 15%, respectively [Table 1].
On echocardiography 20 patients (20/40 = 50%) had
normal study.
Lung India Vol 28 Issue 2 Apr - Jun 2011
Gupta, et al.: Echocardiographic evaluation of heart in COPD patient
Table 1: Patients classification according to severity of
COPD
Table 4: Frequency of cor pulmonale with severity of
COPD
Severity of COPD
Severity of COPD
Mild (FEV1 > 80% predicted)
Moderate (50% < FEV1 <80% predicted)
Severe (30%< FEV1 < 50% predicted)
Very severe (FEV1 < 30% predicted)
No. of patients
% Patients
18
11
5
6
45
27.50
12.50
15
% and number of patients with PH
Mild (18)
Moderate (11)
Severe (5)
Very severe (6)
11.11% (2)
9% (1)
40% (2)
33.33% (2)
Majority of cases belong to mild COPD. FEV1: Forced expiratory volume
in one second; COPD: Chronic obstructive pulmonary disease
NO co-relation exists between frequency of cor pulmonale and severity of
COPD
Table 2: Echocardiographic findings in our study
Table 5: Frequency of cor pulmonale with severity of PH
Findings
Normal study
Pulmonary hypertension
(sPAP > 30 mmHg)
Mild (30-50 mmHg)
Moderate (50--70 mmHg )
Severe (>70 mmHg)
Cor pulmonale
RVSD
LVH
LVDD
LVSD
No. of patients
% Patients
20
50
17
10
4
3
7
3
9
19
3
42.50
25
10
7.50
17.50
7.50
22.50
47.50
7.50
Besides PH and cor pulmonale, left ventricular dysfunction is also
common. RVSD: Right ventricular systolic dysfunction; LVH: Left
ventricular hypertrophy; LVDD: Left ventricular diastolic dysfunction;
LVSD: Left ventricular systolic dysfunction
Table 3 : Frequency of PH with severity of COPD
Severity of COPD
Mild (18)
Moderate (11)
Severe (5)
Very severe (6)
% and number of patients with PH
16.7% (3)
54.6% (6)
60% (3)
83.3% (5)
Frequency of PH increases as the severity of COPD
Measurable tricuspid regurgitation (TR) was observed in
27 patients (27/40 = 67.5%). Mean TTPG for the entire
group in which TR could be measured was 37.04 mmHg.
PH defined as sPAP > 30 mmHg was observed in 17
patients (17/40 = 42.5% of the total study population)
(17/27 = 63% of measurable TR). Out of those 17 patients
with pulmonary hypertension, 10 patients were in mild
PH (sPAP 3050 mmHg) (10/40 = 25%) (10/17 = 58.82%),
4 were in moderate PH (sPAP 5070 mmHg) (4/40 = 10%)
(4/17 = 23.53%), and 3 were in severe PH (sPAP > 70
mmHg) (3/40 = 7.5%) (3/17 = 17.65%) [Table 2]. The
frequencies of PH in mild, moderate, severe, and very
severe COPD were 3/18 = 16.67%, 6/11 = 54.55%, 3/5
= 60%, 5/6 = 83.33%, respectively; thus we can see that
there is a good co-relation between the frequency of PH
and severity of COPD [Table 3].
The frequencies of cor pulmonale in patients with mild,
moderate, and severe PH were 10%, 75%, and 100%,
respectively; so we can see a good co-relation between
severity of PH and the development of cor pulmonale
[Tables 4 and 5].
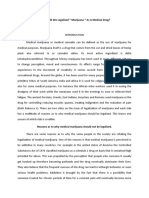
Comparative study of various stages of severity of COPD
Severity of PH
Frequency of cor pulmonale
Mild (10)
Moderate (4)
Severe (3)
10% (1)
75% (3)
100% (3)
Frequency of cor pulmonale increases with severity of PH
Table 6: Echocardiographic findings according to
severity of COPD
Mild (18)
Normal
PH
Cor pulmonale
RHF
LVDD
LVH
LVSD
13
3
2
1
6
3
1
Moderate (11) Severe (5) Very severe (6)
5
6
0
0
4
2
0
2
3
3
1
3
2
1
0
5
2
1
6
2
1
As severity of COPD increases the prevalence of cardiac dysfunction also
increases. COPD: Chronic obstructive pulmonary disease; PH: Pulmonary
hypertension; RHF: Right heart failure; LVDD: Left ventricular diastolic
dysfunction; LVH: Left ventricular hypertrophy; LVSD: Left ventricular
systolic dysfunction
reveals that as severity of COPD increases the prevalence
of cardiac dysfunction increases, so more severe COPD is
associated with more prevalent and more severe cardiac
manifestations [Table 6].
DISCUSSION
The cardiac manifestations of COPD are numerous.
Impairment of right ventricular dysfunction and
pulmonary blood vessels are well known to complicate
the clinical course of COPD and co-relate inversely
with survival. Significant structural changes occur
in the pulmonary circulation in patients with COPD.
The presence of hypoxemia and chronic ventilator
insufficiency is associated with early evidence of intimal
thickening and medial hypertrophy in the smaller branches
of the pulmonary arteries. Coupled with these pathological
changes are pulmonary vasoconstriction arising from
the presence of alveolar hypoxemia, destruction of
pulmonary vascular bed, changes in intrinsic pulmonary
vasodilator substances (such as decrease in PGI 2 s
(prostacyclin synthase), decrease in eNOS (endothelial
nitric oxide synthase), and increase in ET1 (endothelin1)
leads to remodeling, increase in blood viscosity, and
alteration in respiratory mechanics. All these lead to a
significant increase in pulmonary vascular resistance,
the consequence of which is pulmonary hypertension.
Lung India Vol 28 Issue 2 Apr - Jun 2011 107
Gupta, et al.: Echocardiographic evaluation of heart in COPD patient
Severe PH increases right ventricular after load with a
corresponding increase in right ventricular work, which
results in uniform hypertrophy of the right ventricle. In
patients with COPD, hypoxic vasoconstriction is associated
with not only right ventricular hypertrophy but also right
ventricular dilation which eventually leads to clinical
syndrome of right heart failure with systemic congestion
and inability to adapt right ventricular output to the
peripheral demand on exercise.
Although the true prevalence of PH in COPD is unknown,
an elevation of pulmonary arterial pressure is reported
to occur in 20%90% of patients when measured by
right heart catheterization with some evidence that
pulmonary hemodynamic worsens with worsening airflow
obstruction.[14-19] Two studies have shown an abnormal
increase in mean pulmonary arterial pressure (Ppa) in
COPD of 0.40.6 mmHg per year. These studies illustrate
that PH in COPD progresses slowly and occurs in mild as
well as severe forms of disease.[20,21]
The level of PH has a prognostic value in COPD patients
that has been demonstrated by several studies. In one
of these studies, the 5-year survival rates were 50% in
patients with mild PH (2030 mmHg), 30% in those with
moderate-to-severe PH (3050 mmHg), and 0% in the
small group of patients with very severe PH (>50 mmHg).
Thus a high degree of PH bears a poor prognosis, and
this also has been observed in COPD patients receiving
long-term oxygen therapy.[22] The present study finding
reveals 42.5% patients of various severity of COPD have
findings of pulmonary hypertension, that is similar in
prevalence of previous studies. The frequencies of PH
in mild, moderate, severe, and very severe COPD were
16.67%, 54.55%, 60.00%, and 83.33%, respectively. In
one study it was found to be 25%, 43%, and 68% in mild,
moderate, and severe COPD, respectively.[23] In our study
it is also observed that severe PH is present only in severe
or very severe COPD. In conclusion, the incidence of PH
is directly proportional to severity of disease. Previous
studies showed the frequencies of severe PH in COPD from
about 1%3%,[24,25] but in our study it is 4.7%; this may be
due to small study population comprising more percentage
of severe and very severe COPD patients.
Cor pulmonale is present in 17.5% of patients in our
study. Approximately 25% patients with COPD eventually
develop cor pulmonale.[26] Cor pulmonale was found
in 40% patients with COPD in one autopsy study.[27,28]
It is estimated that every year between 10% and 30% of
all hospital admissions for heart failure in the United
States are due to cor pulmonale[29] and approximately 85%
patients with cor pulmonale have COPD.[26]
Some studies indicate that LV function remains normal
in persons with COPD, whereas others suggest that LV
dysfunction may be present.[30,31] Abnormal LV performance
in persons with COPD may be due to a number of factors,
such as hypoxemia and acidosis; concurrent coronary
108
artery disease; ventricular interdependence (because the
right ventricle (RV) and LV share a common septum, RV
dilatation may lead to bulging of the septum into the LV,
which would in turn increase LV end-diastolic pressure,
decrease venous return, and diminish LV stroke volume
and cardiac output (CO) and large swings in intrathoracic
pressure (pronounced negative pleural pressure would
increase Ppa and diminish LV stroke volume due to
ventricular interdependence, negative pleural pressures
may also increase LV after load).[32]
In our study, left ventricular systolic dysfunction (LVSD)
is present in 7.5% patients, in previous studies it was
present in 4%32% patients of COPD.[33-36] LVDD was seen
in COPD patients with normal pulmonary arterial pressure
and it increased with right ventricular after load. [37]
In our study LVDD is present in 47.5% of patients, out of
which 16 patients had PH and 3 did not have PH, various
mechanisms might explain the presence of left diastolic
dysfunction in COPD patients. This may be due to
chronic hypoxemia leading to abnormalities of myocardial
relaxation, lung hyperinflation, and distension leading to
increased stiffness of the parietal pleura and thus of the
wall of cardiac fossa leading to added load on ventricle,
and also due to ventricular interdependence.
Left ventricular hypertrophy (LVH) was present in 22.5%
patients in our study, in one previous study LVH was found
in 25%60% patients dying of COPD mainly in patient who
also had right ventricular hypertrophy.[38]
CONCLUSION
To conclude, the present study shows high prevalence of
pulmonary hypertension, cor pulmonale, left ventricular
dysfunction complicating COPD, more so with more severe
COPD. We suggest screening of all COPD patients for cardiac
complications. This would contribute to the assessment
of prognosis in these patients and assist in identifying
individuals likely to suffer increased mortality and morbidity
warranting close monitoring and intense treatment.
REFERENCES
1.
2.
3.
4.
5.
6.
7.
Murray CJ, Lopez AD. Evidence based health policy-lessons from the
Global Burden of disease Study. Science 1996;274:740-3.
World Health Report. Geneva: World Health Organisation; 2000.
Available from: http://www.who.int/whr/2000/en/statistics.htm. [Last
accessed on 2004 Jan].
Anthonisen N, Connett JE, Kiley JP, Altose MD, Bailey WC, et al.
Effects of Smoking Intervention and the Use of an Inhaled Anticholinergic
Bronchodilator on the Rate of Decline of FEV1. JAMA 1994;272:14971505.
Sin DD, Anthonisen NR, Soriano JB, Agusti AG. Mortality in COPD:
Role of comorbidities. Eur Respir J 2006;28:1245-57.
Daniels LB, Krummen DE, Blanchard DG. Echocardiography in
pulmonary vascular disease. Cardiol Clin 2004;22:383-99.
Yock PG, Popp RL. Noninvasive estimation of right ventricular systolic
pressure by Doppler ultrasound in patients with tricuspid regurgitation.
Circulation 1984;70:657-62.
Tramarin R, Torbicki A, Marchandise B, Laaban JP, Morpurgo M. Doppler
echocardiographic evaluation of pulmonary artery pressure in chronic
Lung India Vol 28 Issue 2 Apr - Jun 2011
Gupta, et al.: Echocardiographic evaluation of heart in COPD patient
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
24.
obstructive pulmonary disease. A European multicentre study. Eur Heart
J 1991;12:103-11.
Currie PJ, Seward JB, Chan KL, Fyfe DA, Hagler DJ, Mair DD, et al.
Continuous wave Doppler estimation of right ventricular pressure: A
simultaneous Doppler-catheterization study in 127 patients. J Am Coll
Cardiol 1985;6:750-6.
Chan KL, Currie PJ, Seward JB, Hagler DJ, Mair DD, Tajik AJ. Comparison
of three Doppler ultrasound methods in the prediction of pulmonary
artery pressure. J Am Coll Cardiol 1987;9:549-54.
Bredikis AJ, Liebson PR. The echocardiogram in COPD: Estimating right
heart pressures. J Respir Dis 1998;19:191-8.
Rappaport E. Cor pulmonale. In, Murray JJ, Nadel JA, Mason RM, Boushey
H (eds). Textbook of respiratory medicine, 4th Edition. Philadelphia, W.B.
Saunders 2000;1631-48.
Chemla D, Castelain V, Humbert M, Simonneau JLHG, Lecarpentier Y,
Herv P. New Formula for Predicting Mean Pulmonary Artery Pressure
Using Systolic Pulmonary Artery Pressure: Chest 2004;126;1313-17.
Braunwalds Heart Disease. 8th Edition. By Libby P, Bonow RO, Zipes
DP, Mann DL. Philadelphia: Saunders 2008. p. 251.
Weitzenblum E, Hirth C, Ducolone A, Mirhom R, Rasaholinjanahary
J, Ehrhart M. Prognostic value of pulmonary artery pressure In chronic
COPD: Thorax 1981;36:752-8.
Weitzenblum E, Sautegeau A, Ehrhart M, Mammosser M, Hirth C, Roegel
E. long term course of pulmonary artery pressure In chronic COPD. Am
Rev Respir Dis 1984;130:993-8.
Burrows B, Kettel LJ, Niden AH, Rabinowitz M, Diener CF. Patterns of
cardiovascular dysfunction in COPD. N Engl J Med 1972;286:912-8.
Fishman AP. State of the art: Chronic cor pulmonale. Am Rev Respir
Dis 1976;114:775-94.
Pietra G. Pathology of the pulmonary vasculature and heart. In; Cherniack
N, editor. COPD. Philadelphia: WB Saunders; 1996. p. 21-6.
Thabut G, Dauriat G, Stern JB, Logeart D, Lvy A, Marrash-Chahla
R, et al: Pulmonary haemodynamics in advanced COPD candidates
for lung volume reduction surgery or lung transplantation. Chest
2005;127:1531-6.
Weitzenblum E, Sautegeau A, Ehrhart M, Mammosser M, Pelletier A.
Long-term oxygen therapy can reverse the progression of pulmonary
hypertension in patients with chronic obstructive pulmonary disease.
Am Rev Respir Dis 1985;131:493-8.
Kessler R, Faller M, Weitzenblum E, Chaouat A, Aykut A, DucoloneA,
et al. Natural history of pulmonary hypertension in a series of 131
patients with chronic obstructive pulmonary disease. Am J Respir Crit
Care Med 2001;164:219-24.
Oswald-Mammosser M, Weitzenblum E, Quoix E, Moser G, Chaouat
A, Charpentier C, et al. Prognostic factors in COPD patients receiving
long-term oxygen therapy. Chest 1995;107:1193-8.
Higham MA, Dawson D, Joshi J, Nihoyannopoulos P, Morrell NW.
Utility of echocardiography in assessment of pulmonary hypertension
secondary to COPD. Eur Respir J 2001;17:350-5.
Chaouat A, Bugnet AS, Kadaoui N, Schott R, Enache I, Ducolon A, et al.
Severe pulmonary hypertension and chronic obstructive pulmonary
disease. Am J Respire Care Med 2005;172:189-94.
25. Thabut G, Dauriat G, Stern JB, Logeart D, Lvy A, Marrash-Chahla
R, et al. Pulmonary Haemodynamics in advanced COPD candidate
for lung volume reduction surgery or lung transplantation. Chest
2005;127:1531-6.
26. Springhouse. Respiratory disorders. In, Springhouse (ed). Professional
Guide to Diseases.9th Edition.Philadelphia, Lippincott William and
Wilkins 2008;120.
27. Rigolin VH, Robiolio PA, Wilson JS, Harrison JK, Bashore TM. The
forgotten chamber: The importance of the right ventricle. Cathet
Cardiovasc Diagn 1995;35:18-28.
28. Fishman AP. State of the art: Chronic Cor Pulmonale. Am Rev Respire
Dis 1976;114:775-94.
29. Macnee W. Pathophysiology of cor pulmonale in chronic obstructive
pulmonary disease. Part One. Am J Respire Crit Care Med
1994;150:833-52.
30. Murphy ML, Adamson J, Hutcheson F. Left ventricular hypertrophy
in patients with chronic bronchitis and emphysema. Ann Intern Med
1974;81:307-13.
31. Fluck DC, Chandrasekar RG, Gardner FV. Left ventricular hypertrophy
in chronic bronchitis. Br Heart J 1966;28:92-7.
32. Robotham JL, Lixfeld W, Holland L, MacGregor D, Bryan AC, Rabson
J. Effects of respiration on cardiac performance. J Appl Physiol
1978;44:703-9.
33. Render, ML, Weinstein, AS, Blaustein, AS Left ventricular dysfunction
in deteriorating patients with chronic obstructive pulmonary disease.
Chest 1995;107:162-8.
34. Vizza CD, Lynch JP, Ochoa LL, Richardson G, Trulock EP. Right and
left ventricular dysfunction in patients with severe pulmonary disease.
Chest 1998;113;576-83.
35. Jardin F, Gueret P, Prost JF, Farcot JC, Ozier Y, Bourdarias JP.
Two-dimensional echocardiographic assessment of left ventricular
function in chronic obstructive pulmonary disease. Am Rev Respir Dis
1984;129:135-42.
36. Louridas G, Patakas D, Stavropoulos C. Left ventricular function in
patients with chronic obstructive pulmonary disease. Cardiology
1981;67:73-80.
37. Funk GC, Lang I, Schenk P, Valipour A, Hartl S, Burghuber OC.
Left Ventricular Diastolic Dysfunction in Patients With COPD in the
Presence and Absence of Elevated Pulmonary Arterial Pressure: Chest
2008;133:1354-9.
38. Poddar AK, Chakraborti BN, Ghosh JL, Nandy S, Hazra S. Assessment
of left ventricular function in patients of COPD :Ind J Tub. 1997; 44-181
How to cite this article: Gupta NK, Agrawal RK, Srivastav AB, Ved
ML. Echocardiographic evaluation of heart in chronic obstructive
pulmonary disease patient and its co-relation with the severity of
disease. Lung India 2011;28:105-9.
Source of Support: Nil, Conflict of Interest: None declared.
Lung India Vol 28 Issue 2 Apr - Jun 2011 109
Reproduced with permission of the copyright owner. Further reproduction prohibited without permission.
Potrebbero piacerti anche
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Kurt Cobain Case StudyDocumento11 pagineKurt Cobain Case StudyKC Respicio67% (3)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- Acute Kidney Injury W/ Hyperkalemia NCPDocumento5 pagineAcute Kidney Injury W/ Hyperkalemia NCPMyrvic Ortiz La OrdenNessuna valutazione finora
- Erectile DysfunctionDocumento145 pagineErectile Dysfunctionluna palitoNessuna valutazione finora
- Sanctification of The Heart 4th Edition by DR Michelle StrydomDocumento771 pagineSanctification of The Heart 4th Edition by DR Michelle StrydomDios Estrella67% (3)
- Prostho MCQ Www-Matterhere-Com NRRDocumento10 pagineProstho MCQ Www-Matterhere-Com NRRYoung FlameNessuna valutazione finora
- Neonatal Emergencies FinalDocumento90 pagineNeonatal Emergencies FinalDr Raseena VattamkandathilNessuna valutazione finora
- Weitzenblum - Chronic Cor PulmonaleDocumento6 pagineWeitzenblum - Chronic Cor PulmonalextraqrkyNessuna valutazione finora
- Weitzenblum - Review Series Heart & Lung Disease Cor PulmonaleDocumento10 pagineWeitzenblum - Review Series Heart & Lung Disease Cor PulmonalextraqrkyNessuna valutazione finora
- Pearson - Age-Associated Changes in Blood Pressure in A Longitudinal Study of Healthy Men & WomenDocumento7 paginePearson - Age-Associated Changes in Blood Pressure in A Longitudinal Study of Healthy Men & WomenxtraqrkyNessuna valutazione finora
- Commentary Occupational Factors, Fatigue & Cardiovascular DiseaseDocumento5 pagineCommentary Occupational Factors, Fatigue & Cardiovascular DiseasextraqrkyNessuna valutazione finora
- Little - What You Need To Know About Chronic BronchitisDocumento4 pagineLittle - What You Need To Know About Chronic BronchitisxtraqrkyNessuna valutazione finora
- Diagnosis and Management of Nail PigmentationsDocumento13 pagineDiagnosis and Management of Nail PigmentationsxtraqrkyNessuna valutazione finora
- Selim (2008) - Melanonychia A Question of DensityDocumento2 pagineSelim (2008) - Melanonychia A Question of DensityxtraqrkyNessuna valutazione finora
- Curkendall - COPD Severity & Cardiovascular OutcomesDocumento12 pagineCurkendall - COPD Severity & Cardiovascular OutcomesxtraqrkyNessuna valutazione finora
- Chiacchio Et Al. (2013) - Longitudinal MelanonychiasDocumento8 pagineChiacchio Et Al. (2013) - Longitudinal MelanonychiasxtraqrkyNessuna valutazione finora
- Kingsbury - Structural Remodelling of Lungs in Chronic Heart FailureDocumento10 pagineKingsbury - Structural Remodelling of Lungs in Chronic Heart FailurextraqrkyNessuna valutazione finora
- Bowser (1998) - Biopsy Good Choice For Diagnosing Melanonychia StriataDocumento2 pagineBowser (1998) - Biopsy Good Choice For Diagnosing Melanonychia StriataxtraqrkyNessuna valutazione finora
- Baran & Kechijian (1996) - Hutchinson's Sign - A ReappraisalDocumento4 pagineBaran & Kechijian (1996) - Hutchinson's Sign - A ReappraisalxtraqrkyNessuna valutazione finora
- Finch Et Al. (2011) - Fungal MelanonychiaDocumento12 pagineFinch Et Al. (2011) - Fungal MelanonychiaxtraqrkyNessuna valutazione finora
- Petrou (2012) - Melanonychia InsightsDocumento3 paginePetrou (2012) - Melanonychia InsightsxtraqrkyNessuna valutazione finora
- Medscape - MelanonychiaDocumento5 pagineMedscape - MelanonychiaxtraqrkyNessuna valutazione finora
- Reinsberger Et Al. (2009) - Dose-Dependent Melanonychia by MitoxantroneDocumento3 pagineReinsberger Et Al. (2009) - Dose-Dependent Melanonychia by MitoxantronextraqrkyNessuna valutazione finora
- Kernbach (2010) - Tarsal Coalitions - Etiology, Diagnosis, Imaging, and StigmataDocumento13 pagineKernbach (2010) - Tarsal Coalitions - Etiology, Diagnosis, Imaging, and StigmataxtraqrkyNessuna valutazione finora
- Leung (2008) - Familial Melanonychia StriataDocumento4 pagineLeung (2008) - Familial Melanonychia StriataxtraqrkyNessuna valutazione finora
- Sakellariou & Claridge (1998) - Tarsal Coalition - Aetiology, Diagnosis and Treatment PDFDocumento8 pagineSakellariou & Claridge (1998) - Tarsal Coalition - Aetiology, Diagnosis and Treatment PDFxtraqrkyNessuna valutazione finora
- Zaw & Calder (2010) - Tarsal CoalitionsDocumento16 pagineZaw & Calder (2010) - Tarsal CoalitionsxtraqrkyNessuna valutazione finora
- Selim (2008) - Melanonychia A Question of DensityDocumento2 pagineSelim (2008) - Melanonychia A Question of DensityxtraqrkyNessuna valutazione finora
- Linklater (2009) - Anatomy of The Subtalar Joint and Imaging of Talo-Calcaneal CoalitionDocumento14 pagineLinklater (2009) - Anatomy of The Subtalar Joint and Imaging of Talo-Calcaneal CoalitionxtraqrkyNessuna valutazione finora
- Kelo & Riddle (1998) - Examination and Management of A Patient With Tarsal CoalitionDocumento8 pagineKelo & Riddle (1998) - Examination and Management of A Patient With Tarsal CoalitionxtraqrkyNessuna valutazione finora
- Stelmach (2003) - The Subtalar Joint in CoalitionDocumento5 pagineStelmach (2003) - The Subtalar Joint in CoalitionxtraqrkyNessuna valutazione finora
- Sartoris & Resnick (1985) - Tarsal CoalitionDocumento8 pagineSartoris & Resnick (1985) - Tarsal CoalitionxtraqrkyNessuna valutazione finora
- Morrison & Ferrari (2009) - Inter-Rater Reliability of The Foot Posture Index (FPI-6) in The Assessment of The Paediatric FootDocumento6 pagineMorrison & Ferrari (2009) - Inter-Rater Reliability of The Foot Posture Index (FPI-6) in The Assessment of The Paediatric FootxtraqrkyNessuna valutazione finora
- Nyska Et Al. (1996) - Posterior Talocalcaneal CoalitionDocumento3 pagineNyska Et Al. (1996) - Posterior Talocalcaneal CoalitionxtraqrkyNessuna valutazione finora
- Hayashi Et Al. (2014) - Endoscopic Resection of A Talocalcaneal Coalition Using A Posteromedial ApproachDocumento5 pagineHayashi Et Al. (2014) - Endoscopic Resection of A Talocalcaneal Coalition Using A Posteromedial ApproachxtraqrkyNessuna valutazione finora
- Fopma & McNicol (2002) - Tarsal CoalitionDocumento9 pagineFopma & McNicol (2002) - Tarsal CoalitionxtraqrkyNessuna valutazione finora
- MSUDDocumento23 pagineMSUDDivya AjithNessuna valutazione finora
- 2012 Karshaniya YavaguDocumento4 pagine2012 Karshaniya YavaguRANJEET SAWANTNessuna valutazione finora
- Abnormal PuerperiumDocumento65 pagineAbnormal PuerperiumNigus AfessaNessuna valutazione finora
- Multiple PregnancyDocumento16 pagineMultiple Pregnancyjane7arian7berzabalNessuna valutazione finora
- Should Medical Marijuana Be Legalized For PatientsDocumento4 pagineShould Medical Marijuana Be Legalized For PatientsBing Cossid Quinones CatzNessuna valutazione finora
- Choose 2 From The Disease Below That Are Emerging in The PhilippinesDocumento4 pagineChoose 2 From The Disease Below That Are Emerging in The PhilippinesMICHELLE BIANCA PATRICE CRUZNessuna valutazione finora
- C-Section Guide: What to Expect with Cesarean DeliveryDocumento3 pagineC-Section Guide: What to Expect with Cesarean DeliveryFEALABREPORTSNessuna valutazione finora
- US Elsevier Health Bookshop - Mosby, Saunders, Netter & MoreDocumento4 pagineUS Elsevier Health Bookshop - Mosby, Saunders, Netter & MoreWilmer Zambrano GuerreroNessuna valutazione finora
- Unipex Onepager CapixylDocumento1 paginaUnipex Onepager CapixylalbertitorubinNessuna valutazione finora
- Milobar Alexus Resume MayoDocumento2 pagineMilobar Alexus Resume Mayoapi-338646789Nessuna valutazione finora
- ACTIVIDAD INGLES Reading ComprehensionDocumento3 pagineACTIVIDAD INGLES Reading Comprehensionyulis mesaNessuna valutazione finora
- It 18 - Neonatal Seizure - HerDocumento35 pagineIt 18 - Neonatal Seizure - HerRurie Awalia SuhardiNessuna valutazione finora
- Bronchopulmonary Dysplasia (BPD)Documento13 pagineBronchopulmonary Dysplasia (BPD)Joan BuiNessuna valutazione finora
- Infectiile Grave Extensive Ale Partilor MoiDocumento49 pagineInfectiile Grave Extensive Ale Partilor MoiLoredana BoghezNessuna valutazione finora
- Lesson 3 ReviewDocumento4 pagineLesson 3 ReviewHo Yong WaiNessuna valutazione finora
- Ann BibDocumento5 pagineAnn Bibapi-317311486Nessuna valutazione finora
- Prevalence of Hypothyroidism in Adults An EpidemioDocumento6 paginePrevalence of Hypothyroidism in Adults An EpidemioCindy Auliah NasutionNessuna valutazione finora
- 6 5 Nerves Hormones and HomeostasisDocumento19 pagine6 5 Nerves Hormones and Homeostasisapi-235355872Nessuna valutazione finora
- Study On The Efficacy of Nosocomial Infection Control (Senic Project) - Summary of Study DesignDocumento14 pagineStudy On The Efficacy of Nosocomial Infection Control (Senic Project) - Summary of Study DesignMunawir GazaliNessuna valutazione finora
- A Case of Beauvieux'S Syndrome and Its EvolutionDocumento7 pagineA Case of Beauvieux'S Syndrome and Its EvolutionAndrea ModestieNessuna valutazione finora
- Fetal risks of macrosomia in diabetic pregnanciesDocumento27 pagineFetal risks of macrosomia in diabetic pregnanciesIful SaifullahNessuna valutazione finora
- Diet PlanDocumento6 pagineDiet Plantrical27 tricalNessuna valutazione finora
- Rheumatic Fever For All For DR Wilfredo Stokes B. Guatemala Nov 2,009Documento9 pagineRheumatic Fever For All For DR Wilfredo Stokes B. Guatemala Nov 2,009drwstokes100% (1)
- Not Eligible As No Experience of Teaching and ResearchDocumento5 pagineNot Eligible As No Experience of Teaching and ResearchVasanth Kumar AllaNessuna valutazione finora