Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Chapter 12 Drugs, Microbes, The Elements of Chemotherapy: Building Your Knowledge
Caricato da
malenya1Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Chapter 12 Drugs, Microbes, The Elements of Chemotherapy: Building Your Knowledge
Caricato da
malenya1Copyright:
Formati disponibili
,
Chapter 12 Drugs, Microbes, Hos.~
The Elements of Chemotherapy
Building Your Knowledge
,
1) In 1900, what percentage of all children in the United States died of infectious disease before
age 51
.
.
2) Explain the concept of selective toxicity .
3) Design the perfect antibiotic. Please consider ease of administration, target microbe, distribution
throughout the body (if necessary for the targeted microbe) length of activity, host toxicity and
potential for the development of antibiotic resistance to the drug .
..
Does the perfect antibiotic actually exist? Why or why not?
4) Compare and contrast narrow and broad spectrum antibiotics .
If you know what the causative agent of a disease is, which would you want to use?
If a patient is septic (seriously ill) with an unknown organism, which would you recommend?
5) Where do most antibiotics originate, in the lab or from nature?
Why is this the case?
..
6) Which drugs are most selectively toxic to bacterial cells (in general)?
Which are the least selectively toxic?
Why?
~92-
7) Are drugs that target the cell wall 'more or less selectively toxic than those that target the plasma
membrane? Why?
8) Are most penicillin and penicillin-like antibiotics more effective against actively growing cells, or
old, dormant cells? Why?
Are they more effective against Gram-positive or Gram-negative cells? Why?
-.
9) What is competitive inhibition and what does it have to do with sulfonamide activity against
bacterial cells?
IO).Why don't sulfonamides damage host cells as much as they do bacterial cells?
11) Are the membrane-disrupting drugs generally used topically (on body surfaces) or administered
internally?
t)
,
,
12) Fill in the diagram with several example antibiotics that target each of the following structures or
processes in a bacterial cell.
Block synthesis and repair
>.
Inhibit replication and transcription
Inhibit gyrase (unwinding enzymes)
Inhibit RNA polymerase
..
Inhlbit folic acid metabolism
- 93 I
13) How is most penicillin produced?
,
14) List 3 members of the penicillin family.
a.
b.
...
c.
,
15) What is the advantage of using semi-synthetic penicillins, like ampicillin or nafcillin?
16) Why add clavulanic acid to penicillins (e.g., Augmentin)?
-,
17) What are the two
major' problems that limit the usefulness of the penicillin antimicrobials?
.
,
18) What are cephalosporins?
~,
"
.'
How arethey generally administered?
Why?
What are the "generations" of cephalosporins based on?
,
'.
19) What group of antibiotics does aztreonam belong to?
..
How does this antibiotic affect bacterial cells?
20) What are the tetracyclines?
",
What is their mechanism' of action?
21) Why is chloramphenicol not a widely used antimicrobial?
....
,,"
22) What do erythromycin, clindamycin, vancomycin and rifamycin have in common?
,
How do these drugs act against bacteria?
Why are they not more widely used?
..
- 94-
23) What are the bacillus antibiotics?
What is their mechanism of action?
Why are they generally not given systemically?
24) Describe the new classes of antibiotics recently discovered and approved by. the FDA?
"
25) Where do sulfamides come from?
How does this origin differ from that of penicillins and cephalosporins?
26) What are fosofmycin and synercid?
.
t 1,
Why are they not widely used?
r
27) Why are scientists hopeful that resistance to theoxazolidinones will be slow to develop?
28) Why did the CDC change the recommendation from ciprofloxacin to doxycycline for the treatment
of anthrax in 2001 ?
29) Why are anti-fungals generally more toxic to human tissues than antibacterial agents?
30) List 4 separate antifungals and the conditions they treat.
I
Antifun gal a gent
Condition(s) treated
,
"
- 95 -
31) Why are polyenes effective against fungal cells, but not bacterial cells?
-,
32) Why are there few effective anti-parasite drugs?
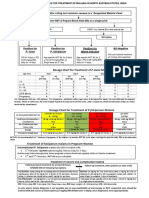
What drugs are used to treat malaria?
What drugs are used to treat roundworm?
33) Why is selective toxicity so difficult to achieve in anti-viral therapies?
34) Why are. viral diseases like measles and mumps fairly rare in the U.S.?
35) What are 3 basic mechanisms of action of anti-viral agents?
,
a.
b.
c.
36) Why is the fact HIV is a retrovirus significant when designing anti-viral therapies?
37) How does chromosomal drug resistance originate? Does this typeof resistance spread in a
population?
38) What 'is the difference between intrinsic and extrinsic drug resistance? Which is of more concern?
39) What are R factors? Do these spread through a bacterial population?
,
- 96-
40) Describe 4 distinct ways bacteria .may become resistant to antibiotics they were once sensitive to .
a.
b.
c.
d.
41) What are beta-lactamases and what antimicrobial drugs do they confer resistance to?
\
42) Do pumps generally confer resistance to 1 type of antimicrobial or many? Why?
How do bacteria become resistant to rifampin or streptomycin?
43) How do bacteria become resistant to sulfonamide?
44) Does exposure to an antibiotic increase or decrease the percentage of resistant cells in a
population? Explain .
45) Why does combining drug therapies limit the spread of drug resistance?
46) What are prebiotics, probiotics and lantibiotics?
"
How does each prevent disease?
- 97 -
,
47) There are 3 major categories of antibiotic side-effects. Name them .
a.
b.
c.
48) Why are the liver and kidneys often damaged by antibiotics?
49) Why are tetracyclines not given to pregnant women or young children?
50) How may antibiotics cause diarrhea? (list 2 ways)
51) If a person takes penicillin once and does not have an allergic reaction to it, does that mean they
are not allergic?' Explain,
.
52) What 3 factors do doctors generally consider when choosing
antimicrobial therapies?
.
a.
b.
c.
53) If the causative agent of a disease is unknown, do doctors generally give narrow-spectrum or
broad-spectrum antibiotics? Why?
54) What 2 methods are commonly used to tell which antibiotics are most and least effective against a
given pathogen? .,
,
a.
b.
- 98-
,
.
Organizing Your Knowledge
Antimicrobial Agent
penicillin
Commonly Used to Treat
Mechanism of Action
sulfonamide
chloroquine
gentamicin
polymyxins .
nystatin
rifampicin
mebendazole
metronidazole
rib av irin
AZT
"
amphotericin B
chloramphenicol
,
tetracycline
vancomyci n
-,
'
- 100-
Antimicrobial Drug
Group
Mechanism of Action
.Mechanism of
Resistance
vancomyci n
tetracycline
,
,
sulfonamide
..
,
rifampicin
ribavirin
polymyxins .
.
,
penicillin
nystatin
metroriidazole
"
"
mebendazole
. gentamicin
I
,
i
"
chloroquine
chloramphenicol
AZT
"
amphotericin B
Practicing .Your Knowledge
1. Which of the following is NOT a common
target for antibacterial drugs?
a. cell wall synthesis
b. nucleic acid structure
c. protein synthesis
d. bacterial cell nucleus
3. Prophylatic antibiotics are given_
a. after a person is infected with a
VIruS
b. to people at increased risk of viral
infection
c. after a person is infected with
bacteria
d. to people at increased risk of
bacterial infection
,
2. All of the following antibiotics target
procaryotic ribosomes EXCEPT
.
a. streptomycin.
b. cephalexiii "
c. gentamicin
d. erythromycin
\
4. An antibiotic with a high therapeutic index
(TI)
.
a. is a less risky choice than one with
, a low TI
b. is generally very toxic
c. has a high MIC and low toxic dose
- 101 -
5. Which of the following is NOT a
characteristic of an ideal antimicrobial drug?
a. not excessive in cost
b. microbistatic, not microbicidal
c. selectively toxic to microbe
d. easy to deliver to site of infection
11. An organism becomes resistant to
penicillin when it
.
. a. produces thymidine kinase
b. acquires its folic acid from the
enviroment
c. produces beta lactamase .
d. loses its DNA
'
,
6. Anti-viral drugs are _.
a. commonly used to treat head colds .
b. hard to design because the viruses are
intracellular parasites
c. generally safer to use than anti
bacterial drugs .
d. not subject to anti-viral resistance
12. Clavulanic acid is added to the penicillin
group of drugs because
.
a. it inhibits beta-lactamase enzymes
b. it works against Gram-positive
bacteria, penicillins don't
c. it lengthens the shelf-life of
penicillins
d. it distupts bacterial cell
.,
membranes
7. A MDR pump will confer resistance to _.
a. a single class of antibiotics (e.g., the
penicillins)
b. many different.antibiotics from
different groups
c. only gralV-~negativebacteria
d. onlygram-positive bacteria
~
13. The major drawbacks to penicillin use are
a. development of resistance and host
cell toxicity
b. synergistic effects with anti-viral
therapies '
c. development of resistance and host
allergic responses
. d. purine degradation and host
allergic responses
9. When the cause of a disease is unknown, but
suspected to be bacterial, a useful course of
action would be
.
a. to start anti-viral therapy
b. to disinfect the patient
c. to start a broad-spectrum antibiotic
. d. to start a narrow-spectrum antibiotic
I
14. Antibiotics that disrupt microbial plasma
membranes
.
a. are more toxic than those that
disrupt microbial cell walls
b. are. commonly given systemically
c. are not toxic to host cells
d. generally have a high therapeutic
index
,
10. Two ways to determine an organism's
resistance to antimicrobial drugs are _
methods.
15.
is commonly used to treat fungal
infections.
a. Tetracycline
b. Vancomycin
c. Amphotericin B
d. Quinine
a. MIC and therapeutic index
b. Kirby-Bauer and therapeutic index
c. MIC and Kirby-Bauer .
d. Kirby-Bauer and beta-lactamase
- 102 (
-.
Potrebbero piacerti anche
- Practical Guidelines in Antiviral TherapyDa EverandPractical Guidelines in Antiviral TherapyG.J. GalassoNessuna valutazione finora
- DysenteryDocumento9 pagineDysenteryRifki HerdaniNessuna valutazione finora
- Antiprotozoal AgentsDocumento4 pagineAntiprotozoal AgentsReem NurNessuna valutazione finora
- Vaginitis: - Trichomoniasis - Vulvovaginal Candidiasis (VVC) - Bacterial Vaginosis (BV)Documento94 pagineVaginitis: - Trichomoniasis - Vulvovaginal Candidiasis (VVC) - Bacterial Vaginosis (BV)AileenNessuna valutazione finora
- Fever with Chills and Rigors: A Case of MalariaDocumento19 pagineFever with Chills and Rigors: A Case of MalariaREETHUNessuna valutazione finora
- Findings of Fact & Conclusions of Law in Faber DecisionDocumento184 pagineFindings of Fact & Conclusions of Law in Faber DecisionLeslie RubinNessuna valutazione finora
- Clinical Guidelines Diagnosis and Treatment Manual PDFDocumento324 pagineClinical Guidelines Diagnosis and Treatment Manual PDFBaba IsubNessuna valutazione finora
- Anne Gershon (Editor), Peter Hotez (Editor), Samuel Katz (Editor) - Krugman's Infectious Diseases of Children-Mosby, in PDFDocumento2.854 pagineAnne Gershon (Editor), Peter Hotez (Editor), Samuel Katz (Editor) - Krugman's Infectious Diseases of Children-Mosby, in PDFyudhoNessuna valutazione finora
- The Who Treatment Protocol For MalariaDocumento18 pagineThe Who Treatment Protocol For MalariatabletvodaNessuna valutazione finora
- Anti Microbial Chemotherapy: Dr. Ashish Jawarkar M.D. Consultant Pathologist Parul Sevashram HospitalDocumento41 pagineAnti Microbial Chemotherapy: Dr. Ashish Jawarkar M.D. Consultant Pathologist Parul Sevashram HospitalDr. Ashish JawarkarNessuna valutazione finora
- Environmental Hazards and Human Health: © 2011 Pearson Education, IncDocumento100 pagineEnvironmental Hazards and Human Health: © 2011 Pearson Education, IncHarshit SinghNessuna valutazione finora
- Infectious Dermatology 1Documento206 pagineInfectious Dermatology 1markylopez23Nessuna valutazione finora
- Drug Calculation ReviewDocumento124 pagineDrug Calculation Reviewhgfree41392100% (1)
- DR Romila Chimoriya Lecturer Department of Pediatrics: Acute Rheumatic FeverDocumento27 pagineDR Romila Chimoriya Lecturer Department of Pediatrics: Acute Rheumatic FeverDhiraj PantNessuna valutazione finora
- Malaria Case Management Training Manual For Health Professionals in Ethiopia Participants ManualDocumento200 pagineMalaria Case Management Training Manual For Health Professionals in Ethiopia Participants ManualEleni HagosNessuna valutazione finora
- Antiprotozoal Drugs Classification and Mechanism of ActionDocumento21 pagineAntiprotozoal Drugs Classification and Mechanism of ActionCurex QANessuna valutazione finora
- Malaria FalciparumDocumento35 pagineMalaria FalciparumAboubakar Moalim Mahad moh'dNessuna valutazione finora
- 7 Case Definitions of Infectious Disease in MalaysiaDocumento110 pagine7 Case Definitions of Infectious Disease in MalaysiaICNessuna valutazione finora
- Sub Acute Haemophilus Parainfluenzae Endocarditis: A Case Report and Review of LiteratureDocumento6 pagineSub Acute Haemophilus Parainfluenzae Endocarditis: A Case Report and Review of LiteratureIJAR JOURNALNessuna valutazione finora
- Antimicrobial ReviewDocumento57 pagineAntimicrobial Reviewemiliow_1Nessuna valutazione finora
- Microbiology Chapter 2Documento109 pagineMicrobiology Chapter 2Täð Œvê MîðNessuna valutazione finora
- Diagnosis and Treatment of Kaposi SarcomaDocumento11 pagineDiagnosis and Treatment of Kaposi SarcomaSantiago Pedro Medina LópezNessuna valutazione finora
- K46 Pharmacology of Anthelminthics, Antiprotozoal, & Antimalaria (Farmakologi)Documento78 pagineK46 Pharmacology of Anthelminthics, Antiprotozoal, & Antimalaria (Farmakologi)ayapillaiNessuna valutazione finora
- Antimicrobial Therapy for Infectious DiseasesDocumento212 pagineAntimicrobial Therapy for Infectious Diseasesaleen qawareetNessuna valutazione finora
- Illustrated Manual of Infectious Diseases of Livestock in AfghanistanDocumento245 pagineIllustrated Manual of Infectious Diseases of Livestock in Afghanistanqadir-qadis100% (2)
- Infectious Diseases of The Female Genital TractDocumento1.111 pagineInfectious Diseases of The Female Genital TractJohn Ntokos100% (2)
- Infectious DiseaseDocumento151 pagineInfectious Diseasebolt boltNessuna valutazione finora
- Tropical Infectious Diseases PDFDocumento1.788 pagineTropical Infectious Diseases PDFMax Izarra Almonacid0% (1)
- Hiv Treatment: IC2 Haemato-Lymphoid and Tropical Medicine HLTM Dr. Eoghan de Barra 2014Documento55 pagineHiv Treatment: IC2 Haemato-Lymphoid and Tropical Medicine HLTM Dr. Eoghan de Barra 2014Faiq Syukri Bin SaparudinNessuna valutazione finora
- Intestinal Parasitosis: For The Ethiopian Health Center TeamDocumento137 pagineIntestinal Parasitosis: For The Ethiopian Health Center TeamStefan LucianNessuna valutazione finora
- Coomunicable DiseaseDocumento182 pagineCoomunicable DiseaseAbdi DanielNessuna valutazione finora
- Malaria 2Documento1 paginaMalaria 2jvNessuna valutazione finora
- Hiv TreatmentDocumento54 pagineHiv TreatmentCharlie BravoNessuna valutazione finora
- Sepsis Management, National Clinical GuidelineNo. 6 (2020update) PDFDocumento200 pagineSepsis Management, National Clinical GuidelineNo. 6 (2020update) PDFNg Khian LungNessuna valutazione finora
- Australasian ED COVID-19 GuidelinesDocumento126 pagineAustralasian ED COVID-19 GuidelinesridaNessuna valutazione finora
- New 2-Acylamino-5-nitrothiazole Derivatives Show Potent Activity Against Neglected Protozoan ParasitesDocumento8 pagineNew 2-Acylamino-5-nitrothiazole Derivatives Show Potent Activity Against Neglected Protozoan ParasitesJulianaRinconLopezNessuna valutazione finora
- Understanding the Physical and Sexual SelfDocumento8 pagineUnderstanding the Physical and Sexual SelfApril ZarsosaNessuna valutazione finora
- Development, Characterization and in Vitro Antifungal Evaluation of Topical Formulation of Tridax Procumbens L. Leaf ExtractDocumento7 pagineDevelopment, Characterization and in Vitro Antifungal Evaluation of Topical Formulation of Tridax Procumbens L. Leaf Extractburhan madriNessuna valutazione finora
- Anti Microbial NotesDocumento10 pagineAnti Microbial NotesMohammed Faisal UddinNessuna valutazione finora
- Infectious DermatologyDocumento206 pagineInfectious DermatologyAaron Christian Earl VillosoNessuna valutazione finora
- MALARIA TREATMENT REGIMENSDocumento2 pagineMALARIA TREATMENT REGIMENSMuhammad NuansaNessuna valutazione finora
- Aids ComprehensiveDocumento2 pagineAids ComprehensiveErororoNessuna valutazione finora
- East Timor Antibiotic Guidelines Jan17 PRINT v3Documento114 pagineEast Timor Antibiotic Guidelines Jan17 PRINT v3Yoan Manuel Ruiz ArencibiaNessuna valutazione finora
- Infectology The Clinician's Guide To DXDocumento645 pagineInfectology The Clinician's Guide To DXAndres Gonzalez CruzNessuna valutazione finora
- Therapeutic Hypothermia - Principles, Indications, Practical ApplicationDa EverandTherapeutic Hypothermia - Principles, Indications, Practical ApplicationNessuna valutazione finora
- Case Definition Infectious Disease 2016Documento143 pagineCase Definition Infectious Disease 2016unit cdc pkd raubNessuna valutazione finora
- PROTOZOADocumento3 paginePROTOZOAMaria Jevica Barandon SolimanNessuna valutazione finora
- ESC 2015 Guidelines For PV EndocarditisDocumento54 pagineESC 2015 Guidelines For PV Endocarditisbminor7Nessuna valutazione finora
- Basic Virology InfectionDocumento118 pagineBasic Virology Infectionlatha100% (1)
- MalariaDocumento12 pagineMalariaManish DasNessuna valutazione finora
- Antiprotozoal Drugs ResistanceDocumento4 pagineAntiprotozoal Drugs Resistance111techie999Nessuna valutazione finora
- Antiparasitic DrugsDocumento17 pagineAntiparasitic DrugsJuan Luis RuizNessuna valutazione finora
- Antiprotozoal and Antihelminthic Drugs - HandoutDocumento21 pagineAntiprotozoal and Antihelminthic Drugs - HandoutdonzNessuna valutazione finora
- Drug Benefit ListDocumento221 pagineDrug Benefit ListPharmaruthiNessuna valutazione finora
- AntiMalarial PharmDocumento3 pagineAntiMalarial PharmKartik ReddyNessuna valutazione finora
- NVBDCP guidelines malaria treatment North Eastern statesDocumento1 paginaNVBDCP guidelines malaria treatment North Eastern statesHtet Lynn HtunNessuna valutazione finora
- Ethiopia FormularyDocumento543 pagineEthiopia Formularyabrham100% (1)
- Pathogenesis, Treatment and Prevention of LeishmaniasisDa EverandPathogenesis, Treatment and Prevention of LeishmaniasisMukesh SamantNessuna valutazione finora
- Cellular CommunicationDocumento5 pagineCellular Communicationmalenya1Nessuna valutazione finora
- Lecture 5-The Vanadium GroupDocumento38 pagineLecture 5-The Vanadium Groupmalenya1Nessuna valutazione finora
- Parasitology Introduction Quiz 1Documento2 pagineParasitology Introduction Quiz 1malenya1Nessuna valutazione finora
- QUIZ 2 Anatomy and Physiology CellsDocumento1 paginaQUIZ 2 Anatomy and Physiology Cellsmalenya1Nessuna valutazione finora
- 3-SCH 401 - Fuel Cells - Applictions of Elctrolysi (Compatibility Mode)Documento34 pagine3-SCH 401 - Fuel Cells - Applictions of Elctrolysi (Compatibility Mode)malenya1Nessuna valutazione finora
- Anatomy and Physiology Chapter 11 Self TestDocumento4 pagineAnatomy and Physiology Chapter 11 Self Testmalenya1Nessuna valutazione finora
- CHD 121 Anatomy and Physiology Course OutlineDocumento2 pagineCHD 121 Anatomy and Physiology Course Outlinemalenya1Nessuna valutazione finora
- Lecture 4 - Titanium GroupDocumento31 pagineLecture 4 - Titanium Groupmalenya1Nessuna valutazione finora
- Lecture 1-Transition Metals ChemistryDocumento58 pagineLecture 1-Transition Metals Chemistrymalenya1100% (1)
- LipidsDocumento4 pagineLipidsmalenya1Nessuna valutazione finora
- Microbiology Quiz 1Documento2 pagineMicrobiology Quiz 1malenya1Nessuna valutazione finora
- Microbiology Introduction To Prokaryotes Quiz 2Documento1 paginaMicrobiology Introduction To Prokaryotes Quiz 2malenya1Nessuna valutazione finora
- Anatomy and Physiology Chapter 11 Practice TestDocumento12 pagineAnatomy and Physiology Chapter 11 Practice Testmalenya150% (2)
- QUIZ 1 Anatomy and Physiology Introduction To The Human BodyDocumento1 paginaQUIZ 1 Anatomy and Physiology Introduction To The Human Bodymalenya1Nessuna valutazione finora
- Anatomy and Physiology Test 1 FlashcardsDocumento14 pagineAnatomy and Physiology Test 1 Flashcardsmalenya1100% (1)
- Anatomy and Physiology CH 4 To 7 Flash CardsDocumento19 pagineAnatomy and Physiology CH 4 To 7 Flash Cardsmalenya1Nessuna valutazione finora
- Muscular System FlashcardsDocumento5 pagineMuscular System Flashcardsmalenya1Nessuna valutazione finora
- Anatomy and Physiology Chapter 2 Test Flash CardsDocumento8 pagineAnatomy and Physiology Chapter 2 Test Flash Cardsmalenya1Nessuna valutazione finora
- Anatomy & Physiology Muscles Flashcards - QuizletDocumento10 pagineAnatomy & Physiology Muscles Flashcards - Quizletmalenya1Nessuna valutazione finora
- Anatomy & Physiology 1 Chapter 9 The Nervous System Flashcards - QuizletDocumento7 pagineAnatomy & Physiology 1 Chapter 9 The Nervous System Flashcards - Quizletmalenya1100% (1)
- Kemu A & P 1Documento4 pagineKemu A & P 1malenya1Nessuna valutazione finora
- Kemu A & P 4Documento7 pagineKemu A & P 4malenya1Nessuna valutazione finora
- R05412302 - Bio Ethics, Bio Safety and Intellectual Property Rights PDFDocumento4 pagineR05412302 - Bio Ethics, Bio Safety and Intellectual Property Rights PDFmalenya1Nessuna valutazione finora
- Kemu A & P 3Documento9 pagineKemu A & P 3malenya1Nessuna valutazione finora
- Jkuat A & PDocumento4 pagineJkuat A & Pmalenya1Nessuna valutazione finora
- Micro 260 DNA Synthesis OverlaysDocumento18 pagineMicro 260 DNA Synthesis Overlaysmalenya1Nessuna valutazione finora
- Kemu A & P 2Documento6 pagineKemu A & P 2malenya1Nessuna valutazione finora
- Bio SafetyDocumento2 pagineBio Safetymalenya1100% (1)
- R05412302 - Bio Ethics, Bio Safety and Intellectual Property Rights PDFDocumento4 pagineR05412302 - Bio Ethics, Bio Safety and Intellectual Property Rights PDFmalenya1Nessuna valutazione finora
- CHAPTER TEN Respiratory and Chapter Eleven DigestiveDocumento21 pagineCHAPTER TEN Respiratory and Chapter Eleven Digestivemalenya1Nessuna valutazione finora
- DDAL05-02 The Black RoadDocumento45 pagineDDAL05-02 The Black Roadlpokm100% (1)
- Credit Card Statement: Payment Information Account SummaryDocumento4 pagineCredit Card Statement: Payment Information Account SummaryShawn McKennanNessuna valutazione finora
- Limiting and Excess Reactants Lesson PlanDocumento3 pagineLimiting and Excess Reactants Lesson Planapi-316338270100% (3)
- Relation of Sociology with other social sciencesDocumento4 pagineRelation of Sociology with other social sciencesBheeya BhatiNessuna valutazione finora
- Introduction To Mass Communication Solved MCQs (Set-3)Documento5 pagineIntroduction To Mass Communication Solved MCQs (Set-3)Abdul karim MagsiNessuna valutazione finora
- FeistGorman - 1998-Psychology of Science-Integration of A Nascent Discipline - 2Documento45 pagineFeistGorman - 1998-Psychology of Science-Integration of A Nascent Discipline - 2Josué SalvadorNessuna valutazione finora
- The Beatles - Allan Kozinn Cap 8Documento24 pagineThe Beatles - Allan Kozinn Cap 8Keka LopesNessuna valutazione finora
- Masters of Death: The Assassin ClassDocumento5 pagineMasters of Death: The Assassin Classjbt_1234Nessuna valutazione finora
- The Revival Strategies of Vespa Scooter in IndiaDocumento4 pagineThe Revival Strategies of Vespa Scooter in IndiaJagatheeswari SelviNessuna valutazione finora
- The Power of Compounding: Why It's the 8th Wonder of the WorldDocumento5 pagineThe Power of Compounding: Why It's the 8th Wonder of the WorldWaleed TariqNessuna valutazione finora
- Risk Assessment: Act/Hse/Ra 001: Use of Suspended Access Cradles and Platforms (Temporary Works)Documento2 pagineRisk Assessment: Act/Hse/Ra 001: Use of Suspended Access Cradles and Platforms (Temporary Works)Saravana0% (1)
- Talking About Your Home, Furniture and Your Personal Belongings - Third TemDocumento4 pagineTalking About Your Home, Furniture and Your Personal Belongings - Third TemTony Cañate100% (1)
- 20 Reasons Composers Fail 2019 Reprint PDFDocumento30 pagine20 Reasons Composers Fail 2019 Reprint PDFAlejandroNessuna valutazione finora
- Modern Dental Assisting 11Th Edition Bird Test Bank Full Chapter PDFDocumento37 pagineModern Dental Assisting 11Th Edition Bird Test Bank Full Chapter PDFRichardThompsonpcbd100% (9)
- Ward A. Thompson v. City of Lawrence, Kansas Ron Olin, Chief of Police Jerry Wells, District Attorney Frank Diehl, David Davis, Kevin Harmon, Mike Hall, Ray Urbanek, Jim Miller, Bob Williams, Craig Shanks, John Lewis, Jack Cross, Catherine Kelley, Dan Ward, James Haller, Dave Hubbell and Matilda Woody, Frances S. Wisdom v. City of Lawrence, Kansas Ron Olin, Chief of Police David Davis, Mike Hall, Jim Miller, Bob Williams, Craig Shanks, John L. Lewis, Jack Cross, Kevin Harmon, Catherine Kelley, Dan Ward and James Haller, Jr., 58 F.3d 1511, 10th Cir. (1995)Documento8 pagineWard A. Thompson v. City of Lawrence, Kansas Ron Olin, Chief of Police Jerry Wells, District Attorney Frank Diehl, David Davis, Kevin Harmon, Mike Hall, Ray Urbanek, Jim Miller, Bob Williams, Craig Shanks, John Lewis, Jack Cross, Catherine Kelley, Dan Ward, James Haller, Dave Hubbell and Matilda Woody, Frances S. Wisdom v. City of Lawrence, Kansas Ron Olin, Chief of Police David Davis, Mike Hall, Jim Miller, Bob Williams, Craig Shanks, John L. Lewis, Jack Cross, Kevin Harmon, Catherine Kelley, Dan Ward and James Haller, Jr., 58 F.3d 1511, 10th Cir. (1995)Scribd Government DocsNessuna valutazione finora
- History of LotteryDocumento29 pagineHistory of LotteryBala G100% (2)
- Theory of Karma ExplainedDocumento42 pagineTheory of Karma ExplainedAKASH100% (1)
- Respiration NotesDocumento2 pagineRespiration NotesBriana TaylorNessuna valutazione finora
- SWSP6033 00 2022T3 V1.0-1Documento14 pagineSWSP6033 00 2022T3 V1.0-1ayman.abaidallah1990Nessuna valutazione finora
- HSG Anh 9 Thanh Thuy 2 (2018-2019) .Documento8 pagineHSG Anh 9 Thanh Thuy 2 (2018-2019) .Huệ MẫnNessuna valutazione finora
- Cultural Briefing: Doing Business in Oman and the UAEDocumento2 pagineCultural Briefing: Doing Business in Oman and the UAEAYA707Nessuna valutazione finora
- Periodic - Properties - Part 2 - by - AKansha - Karnwal - 1702453072953Documento68 paginePeriodic - Properties - Part 2 - by - AKansha - Karnwal - 1702453072953Saktipratik MishraNessuna valutazione finora
- A Business Development PlanDocumento90 pagineA Business Development PlanRishabh Sarawagi100% (1)
- AMA Manual 10th Edition PDFDocumento1.014 pagineAMA Manual 10th Edition PDFKannan Fangs S100% (2)
- 15-8377 - 3521 Calandria Communications L. Rivera PDFDocumento20 pagine15-8377 - 3521 Calandria Communications L. Rivera PDFRecordTrac - City of OaklandNessuna valutazione finora
- Music Literature (Western Music)Documento80 pagineMusic Literature (Western Music)argus-eyed100% (6)
- Certificate of Compliance ATF F 5330 20Documento2 pagineCertificate of Compliance ATF F 5330 20Jojo Aboyme CorcillesNessuna valutazione finora
- Topic 8 - Managing Early Growth of The New VentureDocumento11 pagineTopic 8 - Managing Early Growth of The New VentureMohamad Amirul Azry Chow100% (3)
- Bhagavad Gita: Chapter 18, Verse 47Documento3 pagineBhagavad Gita: Chapter 18, Verse 47pankaj kararNessuna valutazione finora
- Importance of Time Management To Senior High School Honor StudentsDocumento7 pagineImportance of Time Management To Senior High School Honor StudentsBien LausaNessuna valutazione finora