Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Bacterial Isolates From Cerebrospinal Fluid
Caricato da
paswordnyalupaTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Bacterial Isolates From Cerebrospinal Fluid
Caricato da
paswordnyalupaCopyright:
Formati disponibili
Original article
Bacterial isolates from cerebrospinal fluids and their
antibiotic susceptibility patterns in Gondar University
Teaching Hospital, Northwest Ethiopia
Andargachew Mulu1, Afework Kassu1, Belay Tessema2
Abstract
Background: Bacterial meningitis remains a common disease worldwide. Its most frequent causes are Nessieria
meningitidis, Streptococcus pneumoniae, and Haemophilus influenzae. Information on the relative frequency of the
isolation and antibiotic susceptibility patterns of these pathogens is scarce in Ethiopia.
Objectives: To identify bacterial pathogens that cause meningitis and to assess the antibiotic susceptibility patterns of
the isolates from the cerebrospinal fluids (CSF) of acute bacterial meningitis cases/specimens.
Methods: A retrospective analysis of 390 cerebrospinal fluid specimens submitted for culture and antibiotic
susceptibility patterns to the bacteriology laboratory of Gondar University Teaching Hospital was conducted between
September 2002 and August 2003.
Results: Bacterial pathogens were isolated from 22 patients showing an isolation rate of 5.6%. The most commonly
isolated bacteria were Neisseria meningitidis 10(45.5%) and Streptococcus pneumoniae 7(31.8%). Among gram
positive organisms S. pneumoniae showed a high level of drug resistance against chloramphenicol 4(57%), tetracycline
3 (43%), co-trimoxazole 3(43%), ampicillin 3(43%), and gentamicin 1(14%). Among gram negative bacteria, N.
meningitidis was found to be resistant to co-trimoxazole 5(50%), chloramphenicol 3(30%), gentamicin 3(30%) and
ampicillin 2(20%). The single isolate from Proteus species was found to be resistant to co-trimoxazole and
tetracycline. E. coli was found to be resistant to all antibiotics except for gentamicin and ciprofloxacin. Multiple drug
resistance was observed in 50% of the isolates. No organism was found to be resistant to ciprofloxacin.
Conclusions: The isolation rate of bacterial pathogens from cerebrospinal fluids was found to be low. However, the
frequency of single as well as multiple drug resistance was very high among the bacterial isolates. Ciprofloxacin may
be used for the empirical treatment of bacterial meningitis when culture and sensitivity report is not available for adult
patients. [Ethiop.J.Health Dev. 2005; 19(2):160-164]
Introduction
Meningitis is a very serious infection of the meninges
that surround the brain and the spinal cord (1). It is
usually caused by viral, bacterial or fungal pathogens.
Bacterial meningitis can be quite severe and may result in
brain damage, hearing loss, or learning disability and
death if not treated early (2). Despite advances in vaccine
development and chemoprophylaxis, bacterial meningitis
remains a common disease worldwide. The disease is
more common in developing countries (3).
The relative frequency of isolation of various bacterial
species as a cause of meningitis varies with age, and
among geographical regions. About 80% of all cases of
bacterial meningitis are caused by N. meningitidis, S.
pneumoniae, and H. influenzae (3-5). Over two-thirds of
all cases of bacterial meningitis occur in children less
than five years old. Meningococcus affects all ages, most
cases occurring in children and adolescents. More than
80% of meningitis caused by H. influenzae occurs in
children less than 5 years old. Group B hemolytic
streptococcus (S. agalactiae) is the commonest cause of
meningitis in neonates. E. coli is a frequent cause of
meningitis in neonates and is rarely a cause after infancy
(5).
The highest burden of meningococcal meningitis occurs
in sub-Saharan Africa, in an area that is referred to as the
meningitis belt, which has an estimated total population
of approximately 300 million (3). Studies on the
epidemiology of meningococcal meningitis in adult
Ethiopians shows fatality rates for meningitis and
meningococcemia to be 16% and 85% respectively (6).
Antimicrobial resistance of bacteria is a worldwide
problem. However, the situation in developing countries
like Ethiopia is particularly serious (7-8). Because of the
absence of well-equipped bacteriological laboratories in
Ethiopia no organized surveillance exists on drug
resistance patterns among common bacterial isolates and
thus published data on drug resistance are few. However,
the presence multiple antimicrobial resistances in
different clinical specimens including CSF have been
indicated (9-15).
Since the presence of drug resistant bacteria in the natural
environment is a great-threat for public health, and
because of the ever increasing number of drug resistant
strains with time, up-to-date information on local
pathogens and their drug susceptibility patterns is very
_____________________________________________________________________________________________
1
Department of Microbiology and Parasitology, Gondar University, P.O. Box 196, Tel. 251-08-11-01-74, EXT 307
Fax 251-08-111479, E-mail andargachewmulu@yahoo.com, Gondar, Ethiopia; 2 Departments of Medical Laboratory
Technology, Gondar University, P. O. Box 196, Gondar, Ethiopia
Bacterial isolates from cerebrospinal fluid and their antibiotic susceptibility pattern in Gondar 161
______________________________________________________________________________
crucial for the treatment of patients, to decide health
priorities, to allocate resources, to monitor the onset of
resistance and for planning the effective use of
antimicrobials in the region. The purpose of this study
was, therefore, to identify the prevalent bacterial
pathogens that cause meningitis and to assess their
antibiotic susceptibility patterns in Gondar University
Teaching Hospital, northwest Ethiopia.
Methods
This Laboratory-based retrospective analysis of 390 CSF
cultures and sensitivity tests was conducted in the
Bacteriology Laboratory of the Department of
Microbiology and Parasitology at Gondar University
Teaching Hospital within a one-year period between
September 2002 and August 2003.
CSF samples were collected as part of the routine clinical
management of patients admitted in different wards of
the hospital. The samples were collected in sterile
containers by attending physicians and delivered to the
Bacteriology laboratory within half an hour after
collection.
The samples were processed following the standard
microbiological procedures by inoculating on blood agar,
chocolate agar, and MacConkey agar plates [(Oxoid Ltd,
Basingstoke, Hampshire, UK) prepared as per the
manufacturer instruction] and incubated at 35- 37oC
aerobically. The chocolate agar plates were incubated by
putting them in a candle jar, which provided 5-10% CO2
concentration to create a microareophilic condition for
fastidious bacteria. After 18-20 hours of incubation, the
plates were examined for the presence of bacterial
colonies. Plates, which did not show any growth, were
further incubated for an additional 24 hours. Organisms
were identified by standard microbiological methods,
which included colony morphology, as well as staining,
biochemical and serological tests (1, 16-17).
Antibiotic sensitivity test was conducted on pure culture
isolates employing the disc diffusion method (18) for the
commonly used antibiotics: ampicillin (10g), gentamicn
(10g), penicillin G (10IU), tetracycline (30g),
chloramphenicol (30g), ciprofloxacin (5g) and cotrimoxazole (25g) (Oxoid Ltd). The diameters of
growth inhibition around the discs were measured and
interpreted as sensitive, intermediate or resistant as per
the guideline set by Bauer, et al (18). Reference strains:
E. coli ATCC 25922 and S. aureus ATCC 25923 were
tested as controls according to the National Committee
for Clinical Laboratory Standards (NCCLS) (19).
Results
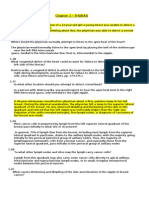
The sex and age distribution patterns of the study
subjects are summarized in Figure 1. Out of the 390
suspected meningitis cases, 249 (63.8%) were males and
the remaining 141 (36.2%) were females. The age range
was from 3 days to 60 years. Over half of the 390
patients, 218 (55.9%) were children and the rest
129(35.1%) and 35(9%) were adults and neonates,
respectively.
Bacterial pathogens were isolated from 22 patients
showing an isolation rate of 5.6%. The number of
pathogens isolated was equal in males and females.
Pathogen isolation rate was higher in adults 8(5.8%) than
in children 12(5.5%).
Number of Patients
250
200
Total
150
Male
100
Female
50
0
Neonate
Children
Adult
Age group
Figure 1: Age and sex distribution of patients investigated for meningitis in Gondar University Teaching
Hospital, Sept. 2002-Aug. 2003
Ethiop.J.Health Dev. 2005; 19(2)
162 Ethiop.J.Health Dev.
_____________________________________________________________________________________
The type and frequency of pathogens isolated from CSF
is shown in Table 1. About 13 (59.1%) of all the isolates
were Gram negative organisms while 9(40.9%) were
Gram positives. N. meningitidis was found to be the most
frequent isolate 10(45.5%) followed by S. pneumoniae
7(31.8), S. aureus 2(9.1); H. influenzae, Proteus species
and E. coli 1 (4.5%) each. The majority of N.
meningitidis (70%) were isolated from children. The
commonest isolate in adults was S. pneumoniae 3(43%).
Multiple infections were not observed. All S. aureus,
Proteus species and E. coli were isolated from adults
(Table 1).
Table 1: Common bacterial isolates from CSF by sex and age distribution, Gondar University Teaching
Hospital, September 2002-august 2003.
Patient category and isolates frequency
Organism
Number (%)
Male
Female
Neonates
Children
Adults
N. meningitidis
10 (45.5)
S. pneumoniae
7 (31.8)
S. aureus
2 (9.1)
H. influenzae
1 (4.5)
Proteus species
1 (4.5)
E. coli
1 (4.5)
Total
22 (100)
11
11
12
The results of the antibiotic susceptibility patterns are
presented in Table 2 below. Among Gram positive
organisms, S. pneumoniae showed a high level of drug
resistance against chloramphenicol 4(57%), tetracycline
3(43%), co-trimoxazole 3(43%), ampicillin 3(43%), and
gentamicin 1(14%). One S. aureus strain was found to be
resistant only to ampicillin and the other showed an
intermediate resistance to ampicillin, penicillin and
tetracycline. Of the Gram-negative bacteria, N.
meningitidis was found to be resistant to co-trimoxazole
5(50%), chloramphenicol 3(30%), gentamicin 3(30%)
and ampicillin 2(20%). The single isolate of Proteus
species was found to be resistant to co-trimoxazole and
tetracycline. E. coli was found to be resistant to all
antibiotics except for gentamicin and ciprofloxacin.
No organism was found to be resistant to ciprofloxacin.
Seven (31.8%) of the isolated pathogens were found to
be sensitive to all antibiotics tested. Four (18%),
5(22.7%), and 2(9%) of the isolated pathogens were
found to be resistant to one, two and three antibiotics
respectively. Resistance to four and five different
antibiotics was found in 3(13.6%) and 1(11%) of the
isolates, respectively.
Table 2: Antibiotic susceptibility pattern of bacterial isolates from CSF, Gondar University
September 2002 - August 2003.
Organisms
Antimicrobial agent
Amp
Gen
Pen
Sxt
TTC
No (%)
No (%)
No (%)
No (%)
No (%)
S
N. meningitidis 10 (45.5)
8 (80)
6 (60)
2 (20)
5 (50)
I
1 (10)
3 (30)
2 (20)
R
2 (20)
3 (30)
5 (50)
3 (30)
S
S. pneumoniae 7 (31.8)
4 (47)
3 (43)
7 (100)
3 (43)
3 (43)
I
3 (43)
1 (14)
1 (14)
R
3 (43)
1 (14)
3 (43)
3 (43)
S
S. aureus 2 (9.1)
2 (100)
1 (50)
2 (100)
2 (100)
I
1 (50
1 (50)
R
1 (50
S
H. Influenzae 1 (4.5)
1 (100)
1 (100)
1 (100)
1 (100)
I
1 (100)
R
S
Proteus species 1 (4.5)
1 (100)
1 (100)
1 (100)
R
1 (100)
S
E. coli 1 (4.5)
1 (100)
R
1 (100)
1 (100)
1 (100)
Key;
Amp=Ampicillin,
Pen=Penicillin,
Gen=Gentamycin,
Sxt=Co-trimoxazole,
CAF=Chloramphenicol, Cip=Ciprofloxacin
S=sensitive, I=Intermediate, R=Resistant
Teaching Hospital,
CAF
Cip
No (%)
No (%)
6 (60)
9 (90)
1 (10)
1 (10)
3 (30)
3 (43)
7 (57)
4 (57)
2 (100)
2 (100)
1 (100)
1 (100)
1 (100)
1 (100)
1 (100)
1 (100)
TTC=Tetracycline,
Ethiop.J.Health Dev. 2005;19(2)
Bacterial isolates from cerebrospinal fluid and their antibiotic susceptibility pattern in Gondar 163
______________________________________________________________________________
Discussion
The successful management of patients suffering from
bacterial illnesses depends upon the identification of the
types of organisms that cause the diseases and the
selection of an effective antibiotic against the organism in
question (16). Thus, the data presented in this study could
provide information of immediate public health
importance to clinicians in northwest Ethiopia on the
selection of antimicrobial agents for the treatment of
patients suffering from acute bacterial meningitis.
The finding of this retrospective study indicated that the
spectrum of bacterial isolates from CSF in general is
basically similar to reports from elsewhere (2-3). N.
meningitidis and S. pneumoniae were the commonest
pathogens of meningitis patients. The isolation rate of
5.6% found in the present study is in agreement with a
previous study conducted in Gondar where an isolation
rate of 5.2% was reported (9). Eventhough all febrile
children and adults without localizing signs have
underwent lumbar puncture to rule out bacterial
meningitis, the bacterial isolation rate was found to be
low. This may be due to the fastidious nature of the
organisms or prior exposure to antibiotics (1, 5, 8) or over
clinical diagnosis of meningitis.
Eighty one percent of cases of acute bacterial meningitis
were caused by N. meningitidis, S. pneumoniae and H.
influenzae. Seventy percent of meningococci were
isolated from children, which is in agreement with CDC
and WHO reports (2-3). However, this is in contrast with
a previous study conducted in Gondar where no
meningococci were isolated (9). The isolation rate of the
menigococci in the present report might be a result of an
epidemic of meningococcal meningitis which occurred in
North Gondar in 2001/ 2002 (21).
H. influenzae have been reported as the most common
pathogen of pyogenic meningitis in children in central and
northwestern Ethiopia (15, 20, 24). The reason for the
existence of only a single isolation of H. influenzae over
the year in the present study is not clear. However, it
might be due to the new vaccine being given as part of
routine child immunization activities, which might have
reduced the occurrence of invasive diseases due to H.
influenzae (3) and/or the more fastidious nature of the
organism (1,5,16). Unlike previous studies conducted in
the same area (21), the common causative organism for
neonatal meningitis in the present study was found to be
N. meningitidis. However, it is in agreement
with a
previous study conducted in Addis Ababa (23-24).
Resistance of S. pneumoniae, N. meningitidis and H.
influenzae to commonly prescribed antibiotics has been
reported in different areas of the country (15). But much
is not known about the drug resistance behaviour of S.
pneumoniae and N. meningitidis from northwest Ethiopia.
Nevertheless, Achamyeleh et al. (14) in 1995 reported
that S. pneumoniae isolated from pediatric patients were
found to be resistant to the commonly prescribed
antibiotics. In agreement to this report S. pneumoniae in
the present study were found to have high levels of drug
resistance against chloroamphenicol, tetracycline, cotrimoxazole, ampicillin, and gentamicin. However, no S.
pneumoniae were found to be resistant to penicillin unlike
a previous report from the same area (15) where 50
percent penicillin resistant pneumococcal meningitis type
was reported. Likewise a high rate of resistance was also
observed in N. meningitidis in the present study.
Previous S. aureus isolates from Gondar (12-13) showed
similar frequencies of resistance to the common
antibiotics tested. On the contrary, better susceptibility
was observed among S. aureus strains to penicillin G in
the present study. The single isolate of E. coli was found
to be sensitive only to gentamicin and ciprofloxacin. And
Proteus species was found to be susceptible to ampicillin,
gentamicin, chloramphenicol and ciprofloxacin. These are
in agreement with previous reports in studies from Jimma
and Gondar (9-10, 12-13). In general, multiple drug
resistance was seen in 50% of the bacterial isolates from
CSF. No organism was found to be resistant to
ciprofloxacin as reported earlier (12-13).
In conclusion the isolation rate of bacteria causing
meningitis is low. This may be probably due to the
fastidious nature of the organisms, prior exposure to
antibiotics or over clinical diagnosis of meningitis,
especially in children. The frequency of single as well as
multiple drug resistance is alarmingly high. This might be
a reflection of the inappropriate use of antimicrobials, or
unavailability of a guideline regarding the selection of
drugs. Producing updated information on local pathogens
and their sensitivity patterns is a prime tool in combating
such a global problem. Since no resistance was seen
against ciprofloxacin, this antibiotic may be used for the
immediate empirical therapy of meningitis before culture
and sensitivity report is available, particularly for adult
patients.
Acknowledgements
The authors are grateful to the Medical Laboratory
Technicians working in the Bacteriology section of the
laboratory and to the Department of Clinical Laboratory
for giving access to their documentation and to the staff
of the Microbiology Department of the College for their
valuable comments.
References
1. Cheesborough M. Medical Laboratory Manual for
Tropical countries II. 1987: 255 275.
2. Richard E.B., et al. Nelson textbook of pediatrics,
16th ed. W.B. Saunders Company. New York USA,
2000. P.707.
Ethiop.J.Health Dev. 2005; 19(2)
164 Ethiop.J.Health Dev.
_____________________________________________________________________________________
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
World Health Organization. Control of epidemic
meningococcal diseases. WHO Practical Guidelines.
2 ed. 1998. Geneva Switzerland.
Solberg C.O. Meningococcal infections, In Fauci
A.S., Braunwald E, Isselbacher K.J, et al (eds.),
Harrisons principles of internal medicine, 14th ed.
McGraw- Hill, New York USA 1998; 9:910-15.
D.C. Shanson. Microbiology in Clinical Practice 3rd
ed. Butterworth Heinemann: 305-306.
Fekade D., Zewde D., Epidemic meningococcal
meningitis in adult Ethiopians in Addis Ababa,
Ethiopia. Ethiop Med J 1992;30(3):135-42.
World Health Organization. WHO Bulletin.
Resistance to antimicrobial agents 1996;74(3):335336.
Robert F. Basic Medical Microbiology. 5th ed.
Lippincott Williams and Wilkins Country of
Publication. 252-267.
Aseffa A, Yohannes G. Antibiotic sensitivity
patterns of prevalent bacterial pathogens in Gondar,
Ethiopia. East Afr Med J. 1996;73(1):67-71.
Beyene G, Abdissu T. Common bacterial pathogens
and their antibiotic sensitivity at Jimma Hospital: A
four-year Retrospective study. Ethiop J Health Sci
2000;10(2):129-35.
Roma B, Worku S, T/Mariam S, Langeland N.
Antimicrobial susceptibility pattern of Shigella
isolates in Awassa. Ethiop J. Health Dev 2000;14(2):
149-154.
Moges F, Genetu A, Mengistu G. Antibiotic
sensitivity of common bacterial pathogens in urinary
tract infections at Gondar Hospital, Ethiopia. East
Afr Med J 2002;79(3):140-142.
Moges F, Mengistu G, Genetu A. Multiple drug
resistance in urinary pathogens at Gondar College of
Medical Science Hospital, Ethiopia. East Afr Med J
2002;79(8):415-419.
Achamyeleh A, Aseffa A, Gedlu E. Bacterial isolates
from CSF over a five year period in Gondar with a
special reference to pediatric admissions and out
come.
Proceeding of an Annual Research
conference, Gondar College of Medical Sciences.
1995:5158.
15. Muhe L, Klugman KP. Pneumococcal and
Haemophilus infleunzae meningitis in a childrens
Hospital in Ethiopia: Serotypes and susceptibility
pattern. Trop Med Int Health 1999;4(6):421-7.
16. Jawetz, Melnick, Adelbergis. Medical Microbiology.
19 Ed. Prentice-Hall International Inc: Antibacterial
and Antifungal chemotherapy.149-179.
17. World Health Organization. Basic laboratory
procedures in clinical bacteriology, WHO, Geneva,
Switzerland, 1991:78 95.
18. Bauer, A.W., Kirby, W.M.M., Sherirs, J.C, Turck,
M. Antibiotic susceptibility testing by standard
single disk method. Am J Clin Pathol 1966;45:433496.
19. National Committee for Clinical Laboratory
Standards. Performance standards for antimicrobial
disc susceptibility tests. Approved Standard, ASM-2
( 2nd ed.) NCCLS, Villanovan, pa. 1979.
20. Gedlu E, Rahlenbeck SI. Pyogenic meningitis in
children in northwest Ethiopia. Ann Trop Paediatr
1995;15(3):243-247.
21. Mengistu G, Mitiku K, Teferi W. Analysis and
reporting of meningococcal meningitis epidemic in
north Gondar. Ethiop Med J 2003;41(4):319-31.
22. Gebremariam A. Neonatal meningitis in Addis
Ababa: A 10-year review. Ann Trop Paediatr.
1995;15(3):243-247.
23. Kristos TG, Muhe L. Epidemic meningococcal
meningitis in children. A retrospective analysis of
cases admitted to ESCH. Ethiop Med J 1993;31(1):
9-14.
24. Hailu M, Muhe L. Childhood meningitis in a tertiary
hospital
in
Addis
Ababa:
Clinical
and
epidemiological features. Ethiop Med J 2001;39(1):
29-38.
Ethiop.J.Health Dev. 2005;19(2)
Potrebbero piacerti anche
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- PNAS 2001 BannisterDocumento2 paginePNAS 2001 BannisterpaswordnyalupaNessuna valutazione finora
- Index-TB Guidelines - Green Colour 2594164Documento134 pagineIndex-TB Guidelines - Green Colour 2594164cdeepak71Nessuna valutazione finora
- CandidiasisDocumento6 pagineCandidiasisyorlandaNessuna valutazione finora
- Damage Control Orthopaedics (DC O: Presented by Specialist of Orthopedic& Traumatology Al-Mahmoudia General HospitalDocumento52 pagineDamage Control Orthopaedics (DC O: Presented by Specialist of Orthopedic& Traumatology Al-Mahmoudia General HospitalpaswordnyalupaNessuna valutazione finora
- Elicits Bronchial With of Leukotrienes C4Documento5 pagineElicits Bronchial With of Leukotrienes C4paswordnyalupaNessuna valutazione finora
- ACEI and Beta Blocker Effect in Heart FailureDocumento3 pagineACEI and Beta Blocker Effect in Heart FailurepaswordnyalupaNessuna valutazione finora
- Bladder Care PostpartumDocumento11 pagineBladder Care PostpartumAji NugrozzNessuna valutazione finora
- Management Bladder IncontinanceDocumento14 pagineManagement Bladder IncontinancepaswordnyalupaNessuna valutazione finora
- Congenital Cardiac DefectsDocumento40 pagineCongenital Cardiac Defectsstrawberry pieNessuna valutazione finora
- Torch Diseases Web CeDocumento48 pagineTorch Diseases Web CepaswordnyalupaNessuna valutazione finora
- TORCH InfectionsDocumento37 pagineTORCH InfectionsEylin Halim Rahardjo100% (1)
- HerniaDocumento3 pagineHerniapaswordnyalupaNessuna valutazione finora
- Tetanus PDFDocumento11 pagineTetanus PDFDwi Andriyani NimanNessuna valutazione finora
- Needlescopy ReviewDocumento5 pagineNeedlescopy ReviewpaswordnyalupaNessuna valutazione finora
- Q Fever ReviewsDocumento13 pagineQ Fever ReviewspaswordnyalupaNessuna valutazione finora
- Meningitis Pathophysiology PDFDocumento59 pagineMeningitis Pathophysiology PDFpaswordnyalupa100% (1)
- Bladder CareDocumento5 pagineBladder CarepaswordnyalupaNessuna valutazione finora
- Bladder CareDocumento5 pagineBladder CarepaswordnyalupaNessuna valutazione finora
- Urinary Retention PostpartumDocumento5 pagineUrinary Retention PostpartumpaswordnyalupaNessuna valutazione finora
- Endometriosis and Infertility PDFDocumento8 pagineEndometriosis and Infertility PDFLaura Isabel JaramilloNessuna valutazione finora
- Postpartum Bladder CareDocumento9 paginePostpartum Bladder CarepaswordnyalupaNessuna valutazione finora
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (120)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- 1-2 Concepts of NormalityDocumento8 pagine1-2 Concepts of NormalitynesumaNessuna valutazione finora
- INTRA ABl Abscess-Case StudyDocumento15 pagineINTRA ABl Abscess-Case StudypinezNessuna valutazione finora
- Pediatric DentistryDocumento15 paginePediatric Dentistrymirfanulhaq100% (2)
- PNFDocumento13 paginePNFMohd Murtadha Ramly100% (1)
- Assessmen 1Documento2 pagineAssessmen 1Marice VenNessuna valutazione finora
- Risk of Perforation Using Rigid Oesophagoscopy in The Distal Part of OesophagusDocumento4 pagineRisk of Perforation Using Rigid Oesophagoscopy in The Distal Part of OesophagusAgus KarsetiyonoNessuna valutazione finora
- Trasturel 440mg Anti CancerDocumento3 pagineTrasturel 440mg Anti CancerRadhika ChandranNessuna valutazione finora
- Delayed Awakening From AnaesthesiaDocumento3 pagineDelayed Awakening From AnaesthesiaSenthooran ArudshivsmNessuna valutazione finora
- Medsurg QuestionsDocumento12 pagineMedsurg QuestionsPatziedawn GonzalvoNessuna valutazione finora
- Check List For AmbulanceDocumento2 pagineCheck List For AmbulanceEka B100% (1)
- Practise Questions Keith & Moore 5th Edition - Should ReadDocumento113 paginePractise Questions Keith & Moore 5th Edition - Should ReadAmirsalar Eslami83% (6)
- Kidney Transplantation: Group 9 Syazwaniyati Nurulasmira Nur Hamiza Siti NursuhadaDocumento12 pagineKidney Transplantation: Group 9 Syazwaniyati Nurulasmira Nur Hamiza Siti NursuhadaSiti Nursuhada binti Mohd AminNessuna valutazione finora
- Access RecirculationDocumento2 pagineAccess RecirculationHemanth PrakashNessuna valutazione finora
- Poor and Rich CountriesDocumento5 paginePoor and Rich Countriestwentyeight28Nessuna valutazione finora
- Workbook Amedd Sanantonio 2012july20 Revaugust2013Documento56 pagineWorkbook Amedd Sanantonio 2012july20 Revaugust2013api-337285911100% (1)
- Thread Lift ReviewDocumento8 pagineThread Lift ReviewFrench Sarah NeraNessuna valutazione finora
- Government of Nunavut EHB Policy GuidelinesDocumento5 pagineGovernment of Nunavut EHB Policy GuidelinesNunatsiaqNewsNessuna valutazione finora
- Basic Life Support & Medical EmergencyDocumento39 pagineBasic Life Support & Medical EmergencyRoyle LolingNessuna valutazione finora
- Blood DonationDocumento76 pagineBlood Donationlanie_bluegirl100% (1)
- ADR News Dec2008 Vol10 No3Documento8 pagineADR News Dec2008 Vol10 No3William ChandraNessuna valutazione finora
- Approaches To Abdominal MassDocumento49 pagineApproaches To Abdominal MassPatrick JohnNessuna valutazione finora
- Cardiology Clinic 2006Documento620 pagineCardiology Clinic 2006JoNykolasNessuna valutazione finora
- Interpretation: S03 - FPSC DILSHAD COLONY (C004263143) J-50 Dilshad Colony, DelhiDocumento6 pagineInterpretation: S03 - FPSC DILSHAD COLONY (C004263143) J-50 Dilshad Colony, DelhiAll VIDEOS TechNessuna valutazione finora
- APAP 37018 Appendices-Learning-CBT-2 Wright PDFDocumento15 pagineAPAP 37018 Appendices-Learning-CBT-2 Wright PDFAnonymous gj6H8mc8uNessuna valutazione finora
- Drug Study 2Documento2 pagineDrug Study 2tristanpaulNessuna valutazione finora
- Roles and Responsibilities of The First AiderDocumento8 pagineRoles and Responsibilities of The First AiderPascual Ronald PatrickNessuna valutazione finora
- Olivia Mills-ResumeDocumento1 paginaOlivia Mills-Resumeapi-457509028Nessuna valutazione finora
- Community Patient Education Preparation ProjectDocumento2 pagineCommunity Patient Education Preparation Projectapi-272791065Nessuna valutazione finora
- Velopharyngeal InsufficiencyDocumento9 pagineVelopharyngeal InsufficiencyJASPREETKAUR0410Nessuna valutazione finora
- Ortho Case Write-UpDocumento4 pagineOrtho Case Write-UpYang Pascua100% (1)