Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Controlled Studies of Disorders Treatment And: An Overview of Anxiety in Children Adolescents
Caricato da
Alexandra YoelitaDescrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Controlled Studies of Disorders Treatment And: An Overview of Anxiety in Children Adolescents
Caricato da
Alexandra YoelitaCopyright:
Formati disponibili
An Overview of Controlled Studies of Anxiety
Disorders Treatment in Children and
Adolescents
Roxanne W. Scott, MD; Kess Mughelli, BA; and Deborah Deas, MD, MPH
Charleston, South Carolina
Objective: Although several treatments for children and
adolescents with anxiety disorders are available, there are
few well-controlled studies in the literature that compare
these treatments for efficacy. The objective of this paper is
to provide an overview of controlled treatment studies for
children and adolescents with anxiety disorders.
Method: The research literature on controlled treatment
studies of anxiety disorders in children and adolescents was
systematically reviewed through a search of PsycINFO and
Medline. Studies that did not compare the efficacy of treatment modalities were excluded.
Results: This review focuses specifically on three main treatment modalities: cognitive-behavioral therapy, both individual and group; family-based interventions; and pharmacotherapy. Each of these modalities is reviewed in the
context of the separate disorders as defined by DSM-111-R
and/or DSM-IV. The results are especially promising for cognitive-behavioral therapy and pharmacotherapy for many
of the anxiety disorders; however, there are concerns about
small sample sizes, lack of descrbed comorbidity within the
groups and generalizability.
Conclusion: While great strides have been made in the
treatment of child and adolescent anxiety disorders, empircally based studies are quantitatively limited. More research
is needed involving head-to-head trials of the different
modalities.
Key words: children/adolescents * anxiety U treatment
2005. From the Medical University of South Carolina (Scott, clinical assistant professor of psychiatry; Mughelli, medical student; Deas, associate
professor of psychiatry) and the Charleston Area Mental Health Center
(Scott, child psychiatrist), Charleston, SC. Send correspondence and
reprint requests for J Natl Med Assoc. 2005;97:13-24 to: Deborah Deas,
Department of Psychiatry, Medical University of South Carolina, 67 President St., 460 IOP, Charleston, SC 29425; phone: (843) 792-5214; fax: (843)
792-7353; e-mail: deasd@musc.edu
JOURNAL OF THE NATIONAL MEDICAL ASSOCIATION
Anxiety disorders are the most common group of
psychiatric illnesses in children.'-' Kashani and
Orvaschel4 reported prevalence rates of 17.3% for
anxiety disorders in a sample of adolescents. There
are psychosocial and psychopharmacological treatment modalities based on research with sound experimental design; however, there is a paucity of proven
efficacious treatments for children and adolescents.
There are limited data on the psychopharmacological
treatment of anxiety disorders in children, with the
exception of obsessive-compulsive disorder (OCD).s
Over the last several years, more controlled studies
have been conducted to examine the effectiveness of
different treatments for childhood anxiety disorders,
however, few of these include head-to-head trials
comparing interventions between and within different
categories. This review focuses specifically on studies
that compare outcomes ofthese interventions for children and adolescents.
The purpose of this paper is to present an
overview of controlled studies conducted in the past
10 years that compares the standard treatments most
often used in clinical practice to treat children and
adolescents with anxiety disorders. An extensive literature search was conducted using Medline and
Psyclnfo. Articles included were limited to randomized, controlled studies performed in the last decade
focusing on treatment of various anxiety disorders.
The articles included focus on a broad spectrum of
treatment modalities for specific anxiety disorders,
such as OCD, as well as for anxiety disorders in general (mainly generalized anxiety disorder, separation
anxiety disorder and social anxiety disorder). The
three main categories of treatment modalities
include: 1) cognitive-behavioral therapy (CBT) with
subdivision into individual and group, 2) family
interventions paired with CBT, and 3) pharmacological interventions. This review will provide a general
overview of specific anxiety disorders in children/
adolescents and the controlled studies conducted to
define efficacious treatment. In the literature, generalized anxiety disorder, social anxiety disorder
VOL. 97, NO. 1, JANUARY 2005 13
ANXIETY DISORDERS TREATMENT
(social phobia) and separation anxiety disorder were
often combined in the studies, and thus, this review
will maintain that designation. The other anxiety
disorders that have been studied in controlled trials
are OCD, posttraumatic stress disorder (PTSD),
school phobia and specific phobias.
Separation Anxiety Disorder,
Generalized Anxiety Disorder and
Social Anxiety Disorder
The essential feature of separation anxiety disorder is excessive worry concerning separation from
the home or from those to whom the person is
attached.6 This worry is beyond what is expected for
the individual's developmental level. In clinical samples, the disorder is equally common in males and
females; however, in epidemiological samples the
disorder is more frequent in females.
Generalized anxiety disorder (GAD) is character-
ized by excessive worry about a variety of situations.
In children and adolescents, the worries often concern the quality of performance at school or in sporting events, punctuality or catastrophic events.7 The
diagnosis of overanxious disorder from DSM-IJI-R
was eliminated in DSM-IV and the criteria for GAD
modified for children. Therefore, there is some controversy about the link between overanxious disorder and generalized anxiety disorder in children. In a
study by Kendall and Warman,8 a large group of
children with overanxious disorder met criteria for
generalized anxiety disorder. Therefore, the prevalence rates for the two closely approximate each other. As a result, many of the studies reviewed here
tended to collapse the two groups into one category.
In community epidemiological studies, the prevalence rates for overanxious disorder have ranged
from 2.9% to 4.6%.9
Social anxiety disorder (social phobia) has as its
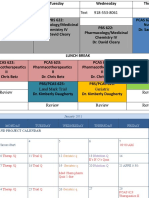
Table 1. Summary of Controlled
Study
Kendall,
1994
Barrett PM
et al., 1996
Treatment Modality
Outcome Measure(s)
Cognitive-behavioral therapy
(n=27) vs. wait-list control (n=20)
(total=47)
The Revised Children's Manifest Anxiety Scales (RCMAS),
State-Trait Anxiety Inventory for Children (STAIC-C), Fear
Survey Schedule for Children-Revised (FSSC-R), Children's
Depression Inventory (CDI), Coping Questionnaire-Child
(CQ-C), Children's Negative Affectivity Self-Statement
Questionnaire (NASSQ), Child Behavior Checklist (CBCL),
Child-Behavior Checklist-Teacher Report Form (TRF)
Cognitive-behavioral therapy
(CBT) (n=28) vs. CBT plus family
anxiety management (CBT+
FAM) (n=25) vs. waiting list (n=26)
RCMAS, FSSC-R, CDI, CBCL, Depression Anxiety Stress
Scales (DASS), Family Enhancement of Avoidant
Responses (FEAR)
(total =79)
Kendall et
al., 1997
CBT (n=60) vs. waiting list (n=34)
(total=94)
RCMAS, STAIC, FSSC-R, CDI, CQ-C, NASSQ, CBCL, STAICModification of trait version for parents (STAIC-A-Trait-P),
Coping Questionnaire-Parent (CQ-P), State Trait Anxiety
Inventory, Beck Depression Inventory (BDI), CBCL-TRF
Silverman
et al., 1999
Group cognitive-behavioral
therapy (GCBT) (n=37) wait-list
control (WLC) (n=19)
(total=56)
Anxiety Disorders Interview Schedule for Children (ADISC) and (ADIS-P), RCMAS, FSSC-R, Child Behavior Checklist
(CBCL), Parent Global Rating of Severity (PGRS)
Mendlowitz
et al., 1999
CBT parent-child condition
(n=18), vs. CBT child-only
condition (n=23) vs. CBT parentonly condition (n=21)
RCMAS, CDI, Children's Coping Strategies Checklist
(CCSC), Global Improvement Scale (CGI)
(total=62)
Shortt et
al., 2001
Family-based cognitive-
RCMAS, CBCL
behavioral treatment (FGCBT)
(n=54) vs. wait-list condition
(n= 17)
(total=71)
14 JOURNAL OF THE NATIONAL MEDICAL ASSOCIATION
VOL. 97, NO. 1, JANUARY 2005
ANXIETY DISORDERS TREATMENT
core feature excessive anxiety about social or performance situations in which the individual fears
scrutiny or exposure to unfamiliar persons.8 Onset of
social anxiety most commonly occurs in mid-adolescence. Adolescents with social anxiety disorder
may have few friends, have difficulties with intimate
relationships and/or develop substance abuse. Figures based on DSM-IJI-R criteria placed the prevalence rate at 1%. Kendall and Warman's study found
that 18% of their sample met DSM-III-R criteria for
social phobia, yet 40% of the same sample met
DSM-IV criteria.8 This may indicate an underestimation of the prevalence of social anxiety disorder.
The literature has relatively recently begun to
evolve to include clinical trials of childhood anxiety
disorders. Kendall performed the first randomized
clinical trial investigating the efficacy of a cognitive-behavioral therapy intervention for children
diagnosed with an anxiety disorder (these disorders
did not include specific phobias or OCD).'0 Fortyseven children aged 9-13 years old were randomly
assigned to either cognitive-behavioral therapy
(N=27) or a wait-list condition (N=20). Children in
the CBT condition received 16 weekly sessions that
included helping the child to: 1) recognize anxious
feelings and somatic reactions to anxiety, 2) clarify
cognition in anxiety-provoking situations, 3) develop a plan to help cope with the situation, and 4) evaluate performance and administer self-reinforcement
as appropriate. The wait-list condition was for eight
weeks, at the end of which time those children could
receive the CBT intervention. The results revealed
that the subjects treated with the CBT intervention
made clinically significant gains as measured at the
end of treatment and that these gains were maintained at a one-year follow-up. Kendall's study has
since been followed by a controlled trial by Barrett,
Dadds, and Rapee in Queensland, Australia," and
Studies of Anxiety Disorder Treatment
Findings
The CBT group showed significantly greater improvement compared to the wait-list group. In the CBT
group, 64% of patients no longer met anxiety disorder diagnostic criteria after treatment compared to
5% participants in the wait-list group.
Treatment children (CBT and CBT + FAM) showed significantly greater improvement compared to the wait-list
group. During posttreatment, 69.8% of all the CBT treatment children no longer met anxiety diagnostic criteria
compared to 26% of the wait-list children. The CBT + FAM condition exhibited significant improvements
compared to CBT-only condition. At 12-month follow-up, 95.6% of children in CBT + FAM group no longer met
diagnostic criteria compared to 70.3% CBT-only children.
The CBT treatment group showed significant improvement over time compared to the wait-list group.
Seventy-one percent of the CBT group no longer met their primary diagnosis at the end of treatment. At
posttreatment, 53% of CBT children no longer met their anxiety disorder diagnosis compared to 6% of
wait-list children.
Participants in the GCBT group showed more significant improvement when compared to the wait-list
group. Based on the CBCL scores, 82% of GCBT subjects exhibited significant improvement at
posttreatment, while 9% of the wait-list subjects showed improvement.
Parents of children in the CBT parent-child group evaluated their children as significantly more improved
compared to parent-evaluations of children from the other two groups. Decreases in anxiety and depression
symptoms were reported for all the treatment groups at posttreatment. Children in the parent-child group used
their coping skills more actively than the children in the other two treatment conditions. Overall, in posttreatment,
females reported less anxiety than males.
In posttreatment, significantly more FGCBT children were diagnosis-free compared to wait-list children.
Results from this study show that 69% of participants who finished FGCBT were diagnosis-free, while 6% of
the wait-list children were diagnosis-free.
JOURNAL OF THE NATIONAL MEDICAL ASSOCIATION
VOL. 97, NO. 1, JANUARY 2005 15
ANXIETY DISORDERS TREATMENT
another study by Kendall et al. in 1997, again looking at treatment of anxiety disorders in children
using a cognitive-behavioral approach.'2
There is emerging evidence that group CBT is
efficacious in the treatment of childhood anxiety
disorders. Barrett conducted the first study exploring the efficacy of group CBT (GCBT).13 The three
treatment conditions included GCBT, GCBT plus
family management (GCBT + FAM) and wait-list.
At the 12-month follow-up, there was no statistically
significant difference between the GCBT and
GCBT + FAM groups; however, both groups maintained significantly better outcomes than the waitlist condition. Thus, it appeared that GCBT was
effective but that the parental involvement was
equivocal.
In a study by Silverman and colleagues,'4 the primary goal was to evaluate the efficacy of GCBT for
treating anxiety in children. A secondary goal was to
extend and complement the ratings instruments that
had been used in previous studies to measure outcome. Two global ratings of clinical severity were
Table 1. Summary of Controlled
Study
Beidel et
al., 2000
l
__________
Treatment Modality
Social effectiveness therapy for
children (SET-C) group (n=36) vs.
nonspecific treatment control
group (Testbusters) (n=31)
| (total=67)
Outcome Measure(s)
CDI, Eysenck Personality Inventory, Social Phobia and
Anxiety Inventory for Children (SPAI-C), and STAIC-C,
CBCL, Children's Global Assessment Scale (K-GAS)
l
Pediatric
Psychophar
macology
Anxiety
Study
Group, 2001
Fluvoxamine 50-300 mg/day for
eight weeks (n=63) vs. placebo
(n=65)
(total= 128)
Pediatric Anxiety Rating Scale, Clinical Global ImpressionsImprovement Scale, Multidimensional Anxiety Scale for
Children, Screen for Child Anxiety-Related Emotional
Disorders
Rynn et al.,
2001
Sertraline 25-50mg for nine
weeks (n=1 1) vs. placebo (n=1 1)
(total=22)
Hamilton Anxiety Scale, Clinical Global Impression (CGI),
Multidimensional Anxiety Scale for children, RCMAS, 17-item
Hamilton Depression Rating Scale
DeVaughGeiss et al.,
1992
Clomipramine hydrochloride
(CMI) 25-200mg for 10 weeks
(n=31) vs. placebo (n=29)
(total=60)
Yale-Brown Obsessive-Compulsive Scale (Y-BOCS), NIMH
Global Obsessive-Compulsive Scale (NIMH GOCS),
Physician Global Evaluation of Change, Patient SelfRating Scale
March et
al., 1998
Sertraline (25-200mg/day for 12
weeks) (n=92) vs. placebo (n=95)
(total=187)
Children's Yale-Brown Obsessive-Compulsive Scale (CYBOCS), NIMH GOCS, NIMH Clinical Global Impressions of
Severity of Illness (CGI-S) and Improvement (CGI-1) rating
scales
Riddle et
al., 1992
Fluoxetine 20 mg for eight weeks
(n=7) vs. placebo (n=6)
(total=1 1)
CY-BOCS, Clinical Global Impression-Obsessive Compulsive
Disorder scale (CGI-OCD), Leyton Obsessional InventoryChild Version (LOI-CV), RCMAS, CDI, K-GAS
Geller et
al., 2001
Fluoxetine 20-60mg for 13 weeks
(n=71) vs. placebo (n=32)
(total= 103)
CY-BOCS, CGI-Severity Scale, CGI-lmprovement Scale,
Patients Global Impressions Scale (PGI), NIMH-GOCS,
Children's Depression Rating Scale-Revised (CDRS-R)
16 JOURNAL OF THE NATIONAL MEDICAL ASSOCIATION
VOL. 97, NO. 1, JANUARY 2005
ANXIETY DISORDERS TREATMENT
used as well as three child self-report measures and
three parent-report measures. In addition, frequency
of follow-up intervals was increased to three-, sixand 12 months. Fifty-six children ages 6-16 years
old were randomly assigned to GCBT or wait-list
condition. The results showed that 64% of the children in the GCBT were recovered at posttreatment,
compared to 13% ofthe children in the wait-list condition. Significant treatment gains were also maintained in the GCBT subjects at 12 months.
Cognitive-behavioral therapy, both individual and
group, has been shown to be efficacious when treating childhood anxiety disorders when compared to a
wait-list condition. Several investigators have identified that and are seeking to understand how the
parental component contributes to the improvement
of these children. There is growing evidence that
anxiety in children is significantly related to frequent negative feedback and parental restriction.15
Prior to a 1996 study by Barrett and associates, no
study had yet examined the value of incorporating
parent training in treatment outcome studies in
Studies of Anxiety Disorder Treatment continued
Findings
The SET-C group showed significantly more improvement than the Testbusters group. In posttreatment,
67% of participants in the SET-C group no longer met criteria for social phobia, while only 5% of
participants in Testbusters no longer met criteria. These improvement remained the same for the sixmonth follow-up.
The fluvoxamine group showed significantly greater improvement than the placebo group. On the
Pediatric Anxiety Rating Scale, subjects in the fluvoxamine group had a decrease of 9.7 points, while
subjects in the placebo group had a decrease of 3.1 points. Based on the CGI scale, 76% fluvoxamine
subjects responded to treatment vs. 29% placebo subjects.
The results favor a 50-mg dosage of sertraline as being more effective than placebo in treating
generalized anxiety disorder in children. The Hamilton Anxiety Scale showed that sertraline patients had
a decrease of 13.8 points in their anxiety scores from baseline to week nine compared to a 2.3 point
decrease in placebo patients. The CGI severity and improvement scale scores also showed significant
treatment differences in favor of sertraline.
Based on Y-BOCS scores, the CMI group exhibited greater improvement than the placebo group. The CMI
group had a mean reduction of 37% in their Y-BOCS score vs. 8% reduction in the placebo group. The
Physicians Global Scores indicate that 60% of CMI patients received a very-much or much-improved rating
compared to 10-17% placebo subjects. NIMH GOCS scores and Patient Self-Rating Scales were all
consistent with the Y-BOCS results in favor of CMI treatment.
Subjects receiving sertraline exhibited significantly greater improvement overall than did placebo
subjects. In the sertraline group, 53% received a 25% decrease in CY-BOCS score from baseline to end
point, compared to 37% in the placebo group. Additionally, 42% of sertraline subjects received a NIMH
CGI-I rating of very-much-improved or much-improved, compared to 26% in the placebo group.
The subjects in the fluoxetine group showed significant decreases in the severity of obsessive-compulsive
symptoms (CY-BOCS mean decrease=44% and CGI-OCD mean decrease= 33%). The placebo subjects
showed smaller nonsignificant decreases in obsessive compulsive symptom severity (CY-BOCS mean
decrease=27% and CGI-OCD mean decrease=1 2%). On the CGI-OCD, the fluoxetine group showed
significantly greater improvement in scores from baseline to end of treatment when compared to placebo.
This study's results demonstrated that fluoxetine is safe and effective for the short-term treatment of children
and adolescents with OCD.
The fluoxetine group showed significantly greater improvement compared to placebo. Based on CYBOCS, 49% fluoxetine subjects were responders to treatment, whereas only 25% placebo subjects
responded to treatment. Fifty-five percent of patients in the fluoxetine group were rated much-improved
or very-much-improved on the CGI scales compared to 18.8% of placebo subjects.
JOURNAL OF THE NATIONAL MEDICAL ASSOCIATION
VOL. 97, NO. 1, JANUARY 2005 17
ANXIETY DISORDERS TREATMENT
childhood anxiety. One significance of this study is
its design, which compared two methods of treatment with a control condition. Barrett and colleagues investigated the effectiveness of cognitivebehavioral and family management training
procedures with childhood anxiety disorders. Seventy-nine children aged 7-14 years were randomly
assigned to receive child-only CBT, child CBT plus
family anxiety management training (CBT + FAM)
or a wait-list condition. The family intervention
involved three phases: 1) parenting skills for managing child distress and avoidance, 2) parenting skills
to manage their own anxiety and 3) parental communication and problem-solving skills. The results
of the study were very promising indeed. Both the
CBT and CBT + FAM groups had significantly better outcomes than the wait-list group, and the CBT +
FAM was found to be significantly more efficacious
than the CBT group. Sixty-one percent of the children in the CBT group no longer met DSM-ILI-R
criteria for any anxiety disorder as compared to 88%
of the CBT + FAM group, which no longer met
diagnostic criteria. At the 12-month follow-up, the
difference between the CBT and the CBT + FAM
Table 1. Summary of Controlled
Treatment Modality
Outcome Measure(s)
Riddle et
al., 2001
Fluvoxamine 25-200 mg for 10
weeks (n=57) vs. placebo (n=63)
(total=1 20)
Children's Yale-Brown Obsessive Compulsive Scale
(CY-BOCS), NIMH GOCS and CGI scales for the clinician,
parent and subject
De Haan E
et al., 1998
Behavioral therapy (BT) (n=12),
vs. clomipramine (n=10) (total
CY-BOCS, LOI-CV, Children's Depression Scale (CDS),
CBCL
Study
=22)
(total=34)
School Attendance, Fear Thermometer (FT), FSSC-R II,
RCMAS, CDI, Self-Efficacy Questionnaire for School
Situations (SEQSS), CBCL, CBCL-TRF, Global Assessment of
Functioning (GAF)
Last et al.,
1998
CBT (n=23) vs. ES (n=21)
(total=44)
School Attendance Record, Global Improvement Scale,
FSSC-R, modified STAIC-C (STAIC-M), CDI, Posttreatment
Diagnosis
Bernstein
et al., 2000
Impramine (25 mg for eight
weeks) plus CBT (n=31) vs.
placebo plus CBT (n=32)
Anxiety Rating for Children-Revised (ARC-C), Children's
Depression Rating Scale-Revised (CDRS-R), RCMAS, BDI,
school attendance
King et
al., 1998
CBT (n= 1 7) vs. wait-list condition
(WLC) (n=1 7)
(total=63)
Cohen et
al., 1996
CBT for sexually abused
preschool children (CBT-SAP)
(n=39) vs. nondirect supportive
therapy (NST) (n=28)
Preschool Symptom Self Report (PRESS), CBCL-Parent
Version, Child Sexual Behavior Inventory (CSBI), Weekly
Behavior Record (WBR)
(total=67)
King et al.,
2000
Child-alone CBT (n=12) vs. Family
cognitive therapy CBT (n=12)
vs. wait-List condition (n= 1 2)
(total=36)
Silverman
et al., 1999
Contingency management
treatment condition (CM) (n=40)
vs. cognitive self-control
condition (SC) (n=41) vs. ES
FT for sexually abused children, Coping Questionnaire for
Sexually Abused Children, RCMAS, CDI, CBCL, GAF
RCMAS, FSSC-R, FT, CDI, Children's Negative Cognitive
Error Questionnaire (CNCEQ), CBCL, Parent Global
Rating of Severity (PGRS)
(n=23)
(total= 104)
18 JOURNAL OF THE NATIONAL MEDICAL ASSOCIATION
VOL. 97, NO. 1, JANUARY 2005
ANXIETY DISORDERS TREATMENT
groups remained significant. Fifty-two of the participants from the original study participated in a sixyear follow-up to examine not only if the treatment
gains were still present within the two groups but
also whether the CBT + FAM group still had relative
superiority to the CBT-only group. The results
showed that 87% of the children no longer met diagnostic criteria for an anxiety disorder and that both
treatments were equally effective.
Mendlowitz and colleagues also examined the
role of parental involvement coupled with group
cognitive-behavioral therapy in the treatment of
childhood anxiety disorders.'6 Sixty-two children
were randomly assigned to one of three 12-week
treatment conditions: 1) parent and child intervention, 2) child-only intervention and 3) parent-only
intervention. All treatment groups experienced a
reduction in both anxiety and depressive symptoms,
suggesting that group CBT is efficacious in treating
children with anxiety disorders. It was also noted
that parental involvement uniquely contributed to
improved coping strategies in the parent-child condition. In this study, there was no 12-month followup posttreatment.
Studies of Anxiety Disorder Treatment continued
Findings
Fluvoxamine subjects showed significantly greater improvement compared to placebo subjects. Based
on CY-BOCS scores, 42% of the fluvoxamine group showed improvement compared to 26% of those
taking placebo.
Both treatment studies showed significant improvement. CY-BOCS obsessive compulsive scores
decreased from 21.5 to 9.1 for the BT group, compared to a 23.8-to-I 7.6 decrease in the clomipramine
group. Based on the CY-BOCS data, behavioral therapy resulted in stronger therapeutic changes
compared to clomipramine. However, the LOI-CV data showed that there were no significant
differences between the two treatments.
CBT children showed significant school attendance improvement when compared to the wait-list
children. CBT children went from being present 61.47% of school days at pretreatment to 93.53% of the
days at posttreatment. The WLC children increased attendance from 40% days present at pretreatment
to 56% days present at posttreatment. CBT children also showed more improvement than WLC children
in the self-report measures and in the clinician's GAF.
Overall, the measures showed no significant differences between the two treatment groups. The two
treatments were found to be equally effective at decreasing children's anxiety and depressive symptoms.
In posttreatment, 65% from the CBT group and 50% of the ES group no longer met diagnostic criteria.
The impramine plus CBT group significantly improved their school attendance over the course of
treatment, whereas the placebo plus CBT group showed no significant improvement in school
attendance. The impramine group went from a mean attendance rate of 28% at baseline to 70% at
week eight. The placebo group increased attendance rate from 17% at baseline to 36% on week eight.
The CBT-SAP group displayed more symptomatic improvement on most of the outcome measures when
compared to the NST group. On the CBCL-Total Behavior Problems Scale, 56% of the CBT-SAP subjects
showed clinical improvement compared to 22% of the NST subjects. For the CBCL-Internalizing scale, 60%
of CBT-SAP improved vs. 1 % of the NST subjects. On the CBCL-Externalizing Scale, 64% of CBT-SAP
improved vs. 12% from the NST group.
Children from the treatment groups (child CBT and family CBT) exhibited more improvement than wait-list
children. However, the analysis of covariance data did not reveal any significant difference between
child-CBT and family-CBT treatment results.
Children from all three treatment groups showed equally significant improvement on all outcome
measures. There was no consistent pattern of differences. Clinically significant improvement was defined
as having a less-than-70 total score on the CBCL Anxious/Depressed Subscale. Based on CBCL scores,
67% from the SC group, 56% from the CM group and 75% from the ES group showed clinically significant
improvement at posttreatment.
JOURNAL OF THE NATIONAL MEDICAL ASSOCIATION
VOL. 97, NO. 1, JANUARY 2005 19
ANXIETY DISORDERS TREATMENT
Shortt and colleagues conducted the first randomized clinical trial evaluating the efficacy of the
FRIENDS program, a family-based group cognitivebehavioral treatment (FGCBT) for anxious children.'7
FRIENDS is an acronym for the strategies taught in
the sessions (F-Feeling worried?; R-Relax and
feel good; I-Inner thoughts; E-Explore plans; NNice work so reward yourself; D-Don't forget to
practice; and S-Stay calm, you know how to cope
now). FRIENDS has a number of unique features,
including two forms for children ages 6-1 1 years and
ages 12-16 years. Also, it incorporates a family skills
component involving cognitive restructuring for parents and assisting families in building social support.
Seventy-one children ranging in age from 6-10 years
who met diagnostic criteria for separation anxiety disorder, generalized anxiety disorder or social anxiety
disorder were randomly assigned to the FRIENDS
group or a wait-list control. Children in the treatment
group participated in 10 weekly sessions in addition
to two booster sessions that occurred one- and three
months following completion of treatment. The
results indicated that children who completed the
FRIENDS program showed greater improvement
than the wait-list condition. Sixty-nine percent of
children who completed the FGCBT were diagnosisfree, as compared to 6% ofthe children in the wait-list
condition. At 12-month follow-up, 68% of the children in the treatment group were diagnosis-free.
Beidel and colleagues conducted a study evaluating the efficacy of Social Effectiveness Therapy for
Children (SET-C) a structured behavioral therapy.'8
The therapy consisted of 24 sessions with 12 group
sessions and 12 individual exposure sessions. Sixtyseven children aged 8-12 years were randomly
assigned to either the SET-C group or an active, nonspecific intervention (Testbusters). Testbusters is a
program that includes study skills and test-taking
strategies but does not specifically address social
anxiety. Fifty children completed the study. Those in
the SET-C group showed significant improvement in
functioning and decrease in symptoms. Sixty-seven
percent ofthe SET-C group no longer met diagnostic
criteria for social phobia compared to 5% ofthe control group. Treatment gains were maintained at sixmonth follow-up.
Few controlled studies exist that examine the
pharmacological treatment of childhood anxiety disorders. The Research Unit on Pediatric Psychopharmacology Anxiety Study Group'9 conducted a randomized, double-blind trial of fluvoxamine and
placebo in children with social phobia, separation
anxiety disorder or generalized anxiety disorder. The
study included 128 children aged 6-17 years. All
children received supportive psychotherapy during
the eight-week study period. Significant differences
20 JOURNAL OF THE NATIONAL MEDICAL ASSOCIATION
between the treatment groups were detected as early
as week three and increased through week six, at
which time they plateaued. In a second study, Rynn
and colleagues conducted the first randomized, double-blind, placebo-controlled trial of a selective
serotonin reuptake inhibitor (SSRI)-sertraline-in
children and adolescents with a primary diagnosis of
generalized anxiety disorder.20 Twenty-two children
and adolescents aged 5-17 years were assigned to
either the sertraline or placebo group for a nineweek study. Psychotherapy except for cognitivebehavioral therapy was allowed, provided the
patients had been receiving the same therapy for the
three months prior to the study and that the level of
intensity remained unchanged throughout the study.
The results of this study suggest that sertraline at a
low dose of 50 mg daily is safe and efficacious in
treating generalized anxiety disorder in children.
There were no significant differences between the
groups with respect to adverse events.
Obsessive Compulsive Disorder
OCD is a disorder of early onset characterized by
recurrent obsessions or compulsions severe enough to
be time-consuming or result in marked distress or significant impairment.6 Obsessions are defined as
recurrent and persistent thoughts, images or impulses
that are egodystonic and intrusive. Compulsions serve
to alleviate dysphoric affects associated with obsessions. Costello et al.2' reported a prevalence of less
than 1% in prepubertal children. Lifetime prevalence
rates for adolescents range from 1.9% to 3.6%.2224
OCD has received much attention from investigators seeking efficacious pharmacological therapy for
children and adolescents. There is much more in the
literature examining the use of SSRI's in the treatment
of OCD than of any other anxiety disorder in children; however, there are few double-blind, controlled
studies. In one study, DeVeaugh-Geiss and
colleagues25 found that 60% of patients that received
clomipramine treatment showed significant improvement. In a study completed by March et al,5 sertraline
was found to be effective for treatment of pediatric
OCD. Riddle et al. found that fluoxetine was significantly better than placebo on major outcome variables
and was generally well-tolerated.26 Geller and colleagues also conducted a study to determine the efficacy of fluoxetine in the treatment of pediatric OCD.27
Fluoxetine was found to be significantly more effective than placebo as evidenced by greater reductions
in Children's Yale-Brown Obsessive Compulsive
Scale (CY-BOCS) scores. Riddle and colleagues also
conducted a 10-week, multicenter, randomized, double-blind, placebo-controlled trial examining the efficacy of fluvoxamine.28 The results indicate that the
decrease in symptom severity was significant when
VOL. 97, NO. 1, JANUARY 2005
ANXIETY DISORDERS TREATMENT
compared with placebo and was comparable to the
rates of response in other studies. Children were
found to have a higher rate of response than adolescents in this particular study. Both sertraline and fluvoxamine have been approved for the treatment of
OCD in children and adolescents. The tricyclic drug
clomipramine has also been approved for treatment of
OCD but is considered a second-line agent due to its
side-effect profile.29
De Haan and colleagues conducted the first study
comparing a psychosocial treatment to drug treatment
for OCD in children.30 Twenty-two children aged
8-18 years were assigned to one of two groups:
behavior therapy or clomipramine therapy. The
behavior therapy consisted of 12 weekly sessions
incorporating exposure and response prevention. The
drug therapy group also met weekly. Initial dose of
clomipramine was 25 mg for the first week and was
titrated to a maximum of 200 mg/day. In the behavior
therapy condition, the mean improvement was 59.9%
as compared to 33.4% in the clomipramine condition.
The results for the behavior therapy condition are
comparable to those from March's study.31 In his
study, the mean improvement was 50%; however,
most of those children received concomitant medication. Improvement in the clomipramine condition was
rather low compared to other studies.
Behavioral treatment for OCD has emerged as
the treatment of choice; however, there is a lack of
rigorous randomized controlled trials examining the
efficacy of CBT versus control or other comparison
treatments. March and colleagues have conducted a
number of open trials and case studies investigating
the use of CBT for children with OCD. Those studies will not be discussed here since the focus of this
paper is to review controlled studies.
School Refusal
School refusal is another disorder with emerging
treatment data in the literature. King and Bernstein32
define school refusal as difficulty attending school
that is associated with emotional distress, especially
anxiety and depression. Separation anxiety and
school phobia have been used interchangeably; however, several studies focus on treatment of school
refusal as its own entity apart from separation anxiety. School refusal affects approximately 5% of all
school-age children.33-35 There is a bimodal peak for
age of onset-5-6 years and 10-1 1 years of age.
There have been two studies that support the efficacy of CBT for school refusal since 1992. In a trial by
King et al,36 34 children ages 5-15 years were randomly assigned to a four-week cognitive-behavioral
intervention which included six individual therapy
sessions evenly distributed across the four-week
treatment period with the child, five with the parents
JOURNAL OF THE NATIONAL MEDICAL ASSOCIATION
involving training in behavior management skills
with the goal being school attendance, and one session with the teacher or a wait-list control condition.
The results indicated that CBT is efficacious in the
treatment of school-refusing children. Eighty-eight
percent of the CBT children in contrast to 29% of
the wait-list children showed clinical improvement
in school attendance. Last and colleagues conducted
a study randomizing 56 children to either a 12-week
CBT group or an attention-placebo control group.37
The CBT condition consisted of graduated in vivo
exposure, cognitive restructuring and coping selfstatement training. The attention-placebo control
group received educational-support therapy. The
findings revealed no statistically significant differences between the CBT children and the educational-support-therapy children. Both groups showed
improvements on a variety of measures, including
school attendance.
Generally, medications are considered as part of a
multimodal treatment plan for children and adolescents diagnosed with anxiety disorders. To our
knowledge, there is only one study that has investigated a multimodal treatment for school refusal.
Bernstein and colleagues7 investigated the efficacy
of eight weeks of imipramine versus placebo, with
each group receiving cognitive-behavioral therapy
for the treatment of school-refusing adolescents. A
noteworthy fact regarding this study is that major
depressive disorder was not an exclusion criterion as
it is in many of the other studies reviewed. Anxiety
and depressive symptoms improved for both groups;
however, school attendance lagged in the placebo
group. The low response rate with the placebo-plusCBT group can be explained by the fact that school
refusers with comorbid depression and anxiety have
more severe symptoms. These findings support a
multimodal treatment approach using pharmacotherapy plus CBT.
Posttraumatic Stress Disorder
Recently, there has been a dramatic increase in
the knowledge of the phenomenology of PTSD in
children. This may be due in part to the increasing
number of children who are exposed to violence.
Giaconia and colleagues found that by age 18 years,
greater than two-fifths of youths in a community
sample met criteria for at least one trauma, and more
than 6% met criteria for a lifetime diagnosis of
PTSD.38 The hallmark features of PTSD involve
symptoms from three clusters: 1) persistent re-experiencing of the event, 2) avoidance of reminders of
the event and numbing of responsiveness, and 3)
persistent symptoms of arousal. It is important to
note that often children may not meet full diagnostic
criteria but still have symptoms that are significant
VOL. 97, NO. 1, JANUARY 2005 21
ANXIETY DISORDERS TREATMENT
enough to warrant treatment. Another factor to bear
in mind when considering treatment is the comorbidity associated with PTSD. Youths with a diagnosis of PTSD have an increased risk of depression,
other anxiety disorders and substance use disorders.38 There is a paucity of controlled studies in the
literature evaluating effective treatment for PTSD in
children. Much ofthe literature has focused on treatment of sexually abused children. In a study by
Cohen and Mannarino,39 cognitive-behavioral therapy was found to have superior clinical efficacy compared with nondirective supportive therapy in the
treatment of sexually abused preschool-age children
with emotional and behavioral symptomatology.
Deblinger et al. evaluated the effects of participation
by mothers in cognitive-behavioral interventions for
sexually abused children with PTSD symptoms.40
Families were randomly assigned to one of three
conditions: child only, mother only, or child and
mother. A community condition served as the control group. The cognitive-behavioral interventions
were significantly more effective than the community control group. The groups that included the child
in treatment were also more efficacious than the
mother only group. As in the study by Barrett,"1
parental involvement in CBT resulted in a reduction
of reported externalizing behavior by the participating parent. Deblinger and colleagues completed a
two-year follow-up of the 100 children in the initial
study.41 The results of this study indicate that the
improvements in externalizing behavior, depression
and PTSD were maintained over the two-year period. There was a slight but significant deterioration
in the effectiveness of parenting practices for the
mothers that had participated in treatment at the
one-year follow-up. King et al.42 had the first published randomized clinical trial to use a wait-list
condition to examine the efficacy of CBT for sexually abused children with PTSD symptoms. The
children were randomly assigned to one of three
groups: child CBT, family CBT or wait-list condition. Children in the treatment condition received 20
weekly individual sessions aimed at helping the
child overcome his or her postabuse distress and
PTSD symptoms. Treatment resulted in a significant
reduction of PTSD symptoms in all three clusters.
However, there was no significant improvement
related to caregiver involvement.
Specific Phobia
DSM-IV defines a specific phobia as an excessive and unreasonable fear of circumscribed objects
or situations where the avoidance, anxiety or distress
related to the fear is associated with functional
impairment or significant distress.6 Children may
not realize that their fears are marked or unreason22 JOURNAL OF THE NATIONAL MEDICAL ASSOCIATION
able. Ollendick and Francis reported the prevalence
rate of specific phobias to be 3-4% of the population.43 There is a paucity of randomized controlled
trials on treating childhood phobias. Silverman et al.
conducted a study evaluating the relative efficacy of
an exposure-based contingency management (CM)
treatment condition and an exposure-based cognitive
self-control (SC) treatment condition to an education support (ES) control condition for the treatment
of childhood phobic disorders."4 The majority of the
subjects (N=87) met criteria for specific phobia, and
the remainder met criteria for social phobia (N=10)
and agoraphobia (N=7). The findings indicate that
both the CM and SC conditions were efficacious in
treating phobic children. What was unexpected was
the level of improvement in the ES condition. More
research is needed to determine what components of
the attention placebo mediate improvement.
Limitations
The controlled studies that have been conducted
tend to have several limitations in common. One is
the small size of the groups. Many of the studies
reviewed here had low participation and/or relatively
high attrition rates. A second concern regarding
these studies is generalizability. Many of the major
comorbid diagnoses met exclusion criteria. Given
that anxiety disorders commonly occur with depression, substance abuse and other anxiety disorders,
researchers need to take this into account when
designing studies and applying the results to clinical
populations. Along those same lines, the demographic make-up of studies needs to reflect the
demographics of the treatment population; otherwise, we can only extrapolate the results to certain
groups of children. A third concern is the small
number of studies comparing two treatment modalities. It is difficult to know which modalities are efficacious in combination or alone and how the results
compare to each other versus placebo.
DISCUSSION
Anxiety disorders are very common during the
childhood/adolescence period and because of the
chronicity, severity and comorbidity, children need
to be identified early, and treatment needs to be initiated to limit the deleterious effects on function.
Although there are many modalities of treatment
being used for the various disorders, few have been
validated by rigorous controlled studies. This underscores the importance of conducting controlled trials. Further, these trials will add to the options of
available evidenced-based treatments for anxiety
disorders in this population. Table 1 provides an
overview of the controlled trials of anxiety disorder
treatment for children and adolescents and offers the
VOL. 97, NO. 1, JANUARY 2005
ANXIETY DISORDERS TREATMENT
reader a quick review of the trials. Even though
there seem to be a number of hurdles to leap in
empirically validating interventions for the treatment of childhood anxiety disorders, researchers
have accomplished a tremendous amount within the
last decade and are continuing to make strides to
ensure that our children receive optimal treatment
that will improve their quality of life. Clinicians and
researchers should make the most use of what has
been done in the past decade and use the knowledge
and data as a springboard for future studies.
ACKNOWLEDGEMENT
The authors wish to gratefully acknowledge Alva
Blair, Robyn Mixon and Rachel Friendly for their
assistance with the preparation ofthis manuscript.
REFERENCES
1. Klein RG, Pine DS. Anxiety disorders. In: Rutter M, Taylor E, Hersor L, eds.
Child and adolescent psychiatry: Modern Approaches, 4th ed. London:
Blackwell Scientific; in press.
2. Pine DS. Childhood anxiety disorders. Curr Opinion Pediatrics. 1997;9:329338.
3. Shaffer D, Fisher P, Dulcan MK, et al. The NIMH diagnostic interview
schedule for children version 2.3: description, acceptability, prevalence
rates, and performance in the MECA study: methods for the epidemiology
of child and adolescent mental disorders study. J Am Acad Child Adolesc
Psychiatry. 1996;35:865-877.
4. Kashani JH, Orvaschel H. Anxiety disorders in mid-adolescence: a community sample. Am J Psychiatry. 1988;145:960-964.
5. March JS, Biederman J, Wolkow R, et al. Sertraline in children and adolescents with obsessive-compulsive disorder: a multicenter randomized
controlled trial. JAMA. 1998;280:1752-1756.
6. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. text revision (DSM-IV-TR). Washington, DC: American Psychiatric Association; 2000.
7. Bernstein GA, Borchardt CM, Perwein AR, et al. Imipramine plus cognitive-behavioral therapy in the treatment of school refusal. J Am Acad
Child Adolesc Psychiatry. 2000;39:276-283.
8. Kendall PC, Warman MJ. Anxiety disorders in youth: diagnostic consistency across DSM-111-R and DSM-IV. J Anxiety Disord. 1996;10:452-463.
9. Bowen RC, Offord DR, Boyle MH. The prevalence of overanxious disorder
and separation anxiety disorder: results from the Ontario child health study.
J Am Acad Child Adolesc Psychiatry. 1990;29:753-758.
10. Kendall PC. Treating anxiety disorders in children: results of a randomized clinical trial. J Consult Clin Psychol. 1994;62:100-1 10.
11. Barrett PM, Dadds MR, Rapee RM. Family treatment of childhood anxiety: a controlled trial. J Consult Clin Psychol. 1996;64:333-342.
12. Kendall PC, Flannery-Schroeder E, Panichelli-Mindel SM, et al. Therapy
for youths with anxiety disorders: a second randomized clinical trial. J Consult Clin Psychol. 1997;65:366-380.
13. Barrett PM. Evaluation of cognitive-behavioral group treatments for
childhood anxiety disorders. J Clin Child Psychol. 1998;27:459-468.
14. Silverman WK, Kurtines WM, Ginsburg GS, et al. Treating anxiety disorders in children with group cognitive-behavioral therapy: a randomized
clinical trial. J Consult Clin Psychol. 1999;67:995-1003.
15. Krohne HW, Hock M. Relationships between restrictive mother-child
interactions and anxiety of the child. AnxietyResearch. 1991:4:109-124.
16. Mendlowitz SL, Manassis K, Bradley S, et al. Cognitive-behavioral group
treatments in childhood anxiety disorders: the role of parental involvement. J Am Acad Child Adolesc Psychiatry. 1999;38:1223-1229.
17. Shortt AL, Barrett PM, Fox TL. Evaluating the FRIENDS program: a cognitive-behavioral group treatment for anxious children and their parents. J
Clin Child Psychol. 2001:30:525-535.
18. Beidel DC, Turner SM, Morris TL. Behavioral treatment of childhood
JOURNAL OF THE NATIONAL MEDICAL ASSOCIATION
social phobia. J Consult Clin Psychol. 2000;68:1072-1080.
19. Pediatric Psychopharmacology Anxiety Study Group. Fluvoxamine for
the treatment of anxiety disorders in children and adolescents. N Eng J
Med. 2001 ;344:1279-1285.
20. Rynn MA, Siqueland L, Rickels K. Placebo-controlled trial of sertraline in
the treatment of children with generalized anxiety disorder. Am J Psychiatry. 2001;158:2008-2014.
21. Costello EJ, Burns BJ, Angold A, et al. How can epidemiology improve
mental health services for children and adolescents? J Am Acad Child
Adolesc Psychiatry. 1993;32:1 106-1113.
22. Flament MF, Whitaker A, Rapoport JL. Obsessive-compulsive disorder in
adolescence: an epidemiological study. J Am Acad Child Adolesc Psychiatry. 1988;27:766-771.
23. Valleri-Basile LA, Garrison CZ, Jackson KL. Frequency of obsessive-compulsive disorder in a community sample of young adolescents. J Am Acad
Child Adolesc Psychiatry. 1994;33:782-791.
24. Zohar AH. The epidemiology of obsessive-compulsive disorder in children and adolescents. Child Adolesc Psychiatr Clin N Am. 1999;8:445-460.
25. DeVeaugh-Geiss J, Moroz G, Biederman J, et al. Clomipramine
hydrochloride in childhood and adolescent obsessive-compulsive disorder: a multicenter trial. J Am Acad Child Adolesc Psychiatry. 1992;31:45-49.
26. Riddle MA, Scahill L, King RA, et al. Double-blind, crossover trial of fluoxetine and placebo in children and adolescents with obsessive-compulsive
disorder. J Am Acad Child Adolesc Psychiatry. 1992;31 :1062-1069.
27. Geller DA, Hoog SL, Heiligenstein JH, et al. Fluoxetine treatment for obsessive-compulsive disorder in children and adolescents: a placebo-controlled
clinical trial. J Am Acad Child Adolesc Psychiatry. 2001;40:773-779.
28. Riddle MA, Reeve EA, Yaryura-Tobias JA, et al. Fluvoxamine for children
and adolescents with obsessive-compulsive disorder: a randomized controlled multicenter trial. J Am Acad Child Adolesc Psychiatry. 2001;40:222-229.
29. American Academy of Child and Adolescent Psychiatry. Practice
parameters for the assessment and treatment of children and adolescents
with obsessive-compulsive disorder. J Am Acad Child Adolesc Psychiatry.
1 998;37(suppl):27S-45S.
30. De Haan E, Hoogduin KAL, Builelaar JK, et al. Behavior therapy versus
clomipramine for the treatment of obsessive-compulsive disorder in children
and adolescents. J Am Acad Child Adolesc Psychiatry. 1998;37:1022-1029.
31. March JS, Mulle K, Herbel B. Behavioral psychotherapy for children and
adolescents with obsessive-compulsive disorder: an open trial of a new
protocol-driven treatment package. J Am Acad Child Adolesc Psychiatry.
1994;33:333-341.
32. King NJ, Bernstein GA. School refusal in children and adolescents: a
review of the past 10 years. J Am Acad Child Adolesc Psychiatry. 2001;40:
197-205.
33. Burke AE, Silverman WK. The prescriptive treatment of school refusal.
Clin Psychol Rev. 1987;7:353-362.
34. Kearney CA, Roblek TL. Parent training in the treatment of school refusal
behavior. In: Briesmeister JM, Schaefer CD, eds. Handbook of Parent Training: Parents as Co-Therapists for Children's Behavior Problems, 2nd ed.
New York: Wiley; 1997.
35. King NJ, Ollendick TH, Tonge BJ. School refusal: assessment and treatment. Boston: Allyn and Bacon; 1995.
36. King NJ, Tonge BJ, Heyne D, et al. Cognitive-behavioral treatment of
school refusing children: a controlled evaluation. J Am Acad Child Adolesc Psychiatry. 1998;37:395-403.
37. Last CG, Hansen C, Franco N. Cognitive-behavioral treatment of
school phobia. J Am Acad Child Adolesc Psychiatry. 1998;37:404-41 1.
38. Giaconia RM, Reinherz HZ, Silverman AB, et al. Traumas and posttraumatic stress disorder in a community population of older adolescents. J Am
Acad Child Adolesc Psychiatry. 1995;34:1369-1380.
39. Cohen JA, Mannarino AP. A treatment study for sexually abused preschool children: initial findings. J Am Acad Child Adolesc Psychiatry. 1996;
35:42-50.
40. Deblinger E, Lippman J, Steer R. Sexually abused children suffering posttraumatic stress symptoms: initial treatment outcome findings. Child Maltreat. 1996;1:310-321
41. Deblinger E, Steer RA, Lippman J. Two-year follow-up study of cognitive-behavioral therapy for sexually abused children suffering posttraumatVOL. 97, NO. 1, JANUARY 2005 23
ANXIETY DISORDERS TREATMENT
ic stress symptoms. Child Abuse Neglect. 1999;23:1371-1378.
42. King NJ, Tonge BJ, Mullen P, et al. Treating sexually abused children with
posttraumatic stress symptoms: a randomized clinical tral. J Am Acad Child
Adolesc Psychiatry. 2000;39:1347-1355.
43. Ollendick T, Francis G. Behavioral assessment and treatment of child-
v EDUCATION
hood phobias. Behavior Modification. 1988;12:165-204.
44. Silverman WK, Kurtines WM, et al. Contingency management, self-control and education support in the treatment of childhood phobic disorders:
a randomized clinical trial. J Consult Clin Psychol. 1999;67:675-687. a
V WOMEN
v OBESITY
JNMA would like to publish three "theme issues" in calendar year 2005 covering
the following topics: (1 ) Education {to include the undergraduate medical school
curriculum, updates on medical schools with special emphasis on the historically
black institutions and residency/fellowship issues}, (2) women/children issues and
(3) obesity/metabolic syndrome. This is a "call for manuscripts" in all three areas.
The timeliness and scholarship of submissions will determine whether any or all of
these initiatives come to fruition. This is JNMA's first foray in this area and
submissions can be "open-ended". In subsequent years we would hope to have
more focused submissions.
Please indicate the particular "theme issue" in your cover letter. Submission
guidelines are located in at least every other issue of JNMA, on NMA's website at
www.nmanet.org under publications, JNMA. Please e-mail your submissions to
isheyn@nma net.org.
FNMMA.
Eddie Hoover, MD i
JNMA Editor-in-Chiefm
24 JOURNAL OF THE NATIONAL MEDICAL ASSOCIATION
VOL. 97, NO. 1, JANUARY 2005
Potrebbero piacerti anche
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Complete Ca1 Prelim ReviewersDocumento37 pagineComplete Ca1 Prelim ReviewersANDREW DEL ROSARIONessuna valutazione finora
- Grieco Et Al-2023-Intensive Care MedicineDocumento4 pagineGrieco Et Al-2023-Intensive Care MedicineDr Vikas GuptaNessuna valutazione finora
- Daftar Pustaka: LUTFIANA DESY S, Drs. Gede Bayu Suparta, MS., PH.DDocumento3 pagineDaftar Pustaka: LUTFIANA DESY S, Drs. Gede Bayu Suparta, MS., PH.DanaNessuna valutazione finora
- Mental Health DirectoryDocumento24 pagineMental Health DirectoryCMO Bestla GroupNessuna valutazione finora
- The Bradley Method® Course ContentDocumento1 paginaThe Bradley Method® Course ContentbirthmommaNessuna valutazione finora
- DMSCO Log Book Vol.3 7/1925-6/1926Documento109 pagineDMSCO Log Book Vol.3 7/1925-6/1926Des Moines University Archives and Rare Book RoomNessuna valutazione finora
- Checklist For Initiating Gender Affirming Hormone Treatment 1Documento1 paginaChecklist For Initiating Gender Affirming Hormone Treatment 1Cara ThanomkulNessuna valutazione finora
- Rguhs Thesis Topics in AnesthesiaDocumento5 pagineRguhs Thesis Topics in AnesthesiaDltkCustomWritingPaperMurfreesboro100% (2)
- Text 918-553-8061Documento4 pagineText 918-553-8061MD6Nessuna valutazione finora
- FDA Bans Times Natural Capsules, X Plus Men, OthersDocumento2 pagineFDA Bans Times Natural Capsules, X Plus Men, OthersGhanaWeb EditorialNessuna valutazione finora
- 2021 SAISD Mask Mandate-LetterheadDocumento2 pagine2021 SAISD Mask Mandate-LetterheadDavid IbanezNessuna valutazione finora
- Deepu Pps Front PgesDocumento6 pagineDeepu Pps Front PgesM. Shoeb SultanNessuna valutazione finora
- Alma Ata DeclarationDocumento3 pagineAlma Ata DeclarationGeorgios MantzavinisNessuna valutazione finora
- W.G. NHMDocumento48 pagineW.G. NHMRajesh pvkNessuna valutazione finora
- Procedur Injection (Group 9)Documento16 pagineProcedur Injection (Group 9)Shinta HerawatiNessuna valutazione finora
- Minnie Germano New Resume 2023Documento1 paginaMinnie Germano New Resume 2023api-655682809Nessuna valutazione finora
- Injection TechniqueDocumento47 pagineInjection TechniqueGeminiQueenNessuna valutazione finora
- OET Discharge Letter - Sample Letter For Doctors and NursesDocumento5 pagineOET Discharge Letter - Sample Letter For Doctors and NursesClassNessuna valutazione finora
- Personal StatementDocumento2 paginePersonal StatementShahryar Ahmad KhanNessuna valutazione finora
- Jkt-g11-Ielts-Assignment 1 (10 Aug 21)Documento4 pagineJkt-g11-Ielts-Assignment 1 (10 Aug 21)Novantho NugrohoNessuna valutazione finora
- Research Paper On Knowledge Management Practices in Pharma CompanyDocumento7 pagineResearch Paper On Knowledge Management Practices in Pharma Companyafnhekkghifrbm100% (1)
- Children's Miracle Network Presents Capital GrantsDocumento3 pagineChildren's Miracle Network Presents Capital GrantsNewzjunkyNessuna valutazione finora
- Cancer Registry Standard Operating ProceduresDocumento3 pagineCancer Registry Standard Operating ProceduresAnan AghbarNessuna valutazione finora
- 9 Key Radiology Medical Coding Tips For CodersDocumento4 pagine9 Key Radiology Medical Coding Tips For Codersayesha100% (1)
- 23andme and The FDADocumento4 pagine23andme and The FDAChristodoulos DolapsakisNessuna valutazione finora
- OET Test 14Documento10 pagineOET Test 14shiela8329gmailcomNessuna valutazione finora
- TM1 PresentationDocumento33 pagineTM1 PresentationJas Sofia90% (10)
- Article1381852119 NwokoDocumento8 pagineArticle1381852119 NwokoChukwukadibia E. NwaforNessuna valutazione finora
- 6 Pharmacists in Public HealthDocumento22 pagine6 Pharmacists in Public HealthJoanna Carla Marmonejo Estorninos-Walker100% (1)
- P4 - Primary and Secondary Survey in EmergencyDocumento22 pagineP4 - Primary and Secondary Survey in Emergencylia agustinaNessuna valutazione finora