Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
BPJ
Caricato da
l10n_assTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
BPJ
Caricato da
l10n_assCopyright:
Formati disponibili
Acute post-streptococcal
glomerulonephritis
In her UPFRONT article
Post-streptococcal glomerulonephritis persists as a problem in the
on infectious disease
upper North Island
patterns (BPJ Issue 5
p4), Professor Diana
Lennon noted the fact
that Post-streptococcal
Although rare, acute post-streptococcal glomerulonephritis (APSGN) is the
most common glomerulonephritis affecting children1,2 particularly those
aged 212 years.
glomerulonephritis
APSGN is typically a complication of group A streptococcal infection, usually
remains an issue in
originating from the skin (impetigo, infected scabies) or occasionally,
the upper north island.
This article explores
its recognition and
management.
the throat. It was first recognised in the 18th century associated with
the convalescence period of scarlet fever.3 There are links today with
overcrowded living conditions, low socio-economic status and areas of
close contact e.g. schools and daycare centres. Countries with tropical
climates, where skin infections are common, have higher incidence.3 In New
Zealand, the upper North Island has the highest rates.
Clinical features vary with severity
of the illness
There is a latent period between the streptococcal infection and the onset
of APSGN generally 34 weeks after skin infection and 12 weeks after
throat infection, so history taking needs to reflect this.
Presenting symptoms vary, depending on the severity. The classic
clinical features are gross haematuria (3050%)1, oedema (6070%)3 and
hypertension (6080%)1,3 but cases may range from those with asymptomatic
microscopic haematuria, who never reach medical attention, up to the 5%
who have hypertensive encephalopathy with seizures, confusion and coma.1
The dark urine, typical of the condition, may not be noticed by children.
Patients may report general malaise, anorexia, nausea, vomiting, headache
or pain in the abdomen or back.2
On examination, signs are related primarily to volume overload facial
oedema, especially periorbital, generalised oedema or even signs of
congestive heart failure (raised JVP, enlarged liver, crepitations in lung bases).
Patients may be pale and could have residual signs of the contributing skin
infection. BP should be checked.
Urinalysis can show frank blood, red cell casts, leucocytes and proteinuria.
Throat swabs are unhelpful as they are rarely positive.1 Further lab tests
may show raised antistreptolysin-O (ASO), decreased complement levels,
increased urea and mild normochromic, normocytic anaemia due to
haemodilution.1,2,3
www.bpac.org.nz
40
BPJ
Issue 7
keyword: Post Strep
APSGN is usually self limiting but supportive
care and careful follow up are required
There is no specific treatment. APSGN is self-limiting supportive care is needed with the major
aims being to control oedema and hypertension, if present. Salt and water restriction may be
beneficial but referral to hospital may be required for accurate fluid and electrolyte management,
and treatment of hypertension with medication (iv frusemide, isradapine, labetalol or others).1,3
Antibiotics can be given to reduce infectivity but they do not help in the actual treatment of APSGN.1
Family members or other contacts are sometimes given prophylactic antibiotics.
The majority of children will recover spontaneously over 23 weeks with resolution of all abnormal
symptoms and signs (see Figure 1). Microscopic haematuria can, however, take up to 2 years to
resolve.1 Chronic renal failure is a rare complication in children but it is suggested that urinalysis and
BP be rechecked at 36 monthly intervals.
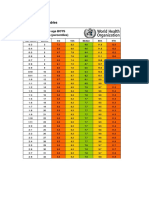
Figure 1: Time course to resolution of APSGN1
Clinical and Laboratory features
Gross H
Hypertension
Low C3
Persistent proteinuria
Intermittent proteinuria
Microhaematuria
2 weeks
4 weeks
2 months
6 months
1 year
2 years
C3 = Complement Protein, Gross H = Gross Haematuria
References
1.
Wong W. Starship Childrens Health Clinical Guideline. Sept 2005. Available on line at www.starship.org.nz
Accessed July 2007.
2.
Bane-Terakubo TM. Nephritic Syndrome, Chapter XIII.1. Case Bases Pediatrics for Medical Students and
Residents. Hawaii. Dept of Pediatrics, Univeristy of Hawaii John A. Burns School of Medicine. 2002.
3.
Geetha D. Glomerulonephritis, Poststreptococcal. 2006. Available on line at http://snipurl.com/1o7v6
Accessed July 2007
BPJ
Issue 7
41
Potrebbero piacerti anche
- Callen2009 Clinically Relevant InformationDocumento4 pagineCallen2009 Clinically Relevant Informationl10n_assNessuna valutazione finora
- Classification of Cutaneous LupusDocumento5 pagineClassification of Cutaneous Lupusl10n_assNessuna valutazione finora
- Callen2004 Update On The Management of Cutaneous Lupus ErythematosusDocumento6 pagineCallen2004 Update On The Management of Cutaneous Lupus Erythematosusl10n_assNessuna valutazione finora
- Beverly J. McCabe, Eric H. Frankel, Jonathan J. Wolfe Handbook of Food-Drug InteractionsDocumento1 paginaBeverly J. McCabe, Eric H. Frankel, Jonathan J. Wolfe Handbook of Food-Drug Interactionsl10n_assNessuna valutazione finora
- Wozniacka2005 Optimal Use of Antimalarials in TreatingDocumento11 pagineWozniacka2005 Optimal Use of Antimalarials in Treatingl10n_assNessuna valutazione finora
- TABLE Boys 3mo To 5yr TRICEPSage PercentileDocumento2 pagineTABLE Boys 3mo To 5yr TRICEPSage Percentilel10n_assNessuna valutazione finora
- NPPA040112 DecisiontreeDocumento1 paginaNPPA040112 Decisiontreel10n_assNessuna valutazione finora
- Jurnal Kriteria Baru SleDocumento10 pagineJurnal Kriteria Baru SleDr Edi HidayatNessuna valutazione finora
- Z Score BMI 5-19yearsold Label GirlDocumento1 paginaZ Score BMI 5-19yearsold Label GirlVienny Widhyanti RosaryaNessuna valutazione finora
- Boeck Ler 2009Documento5 pagineBoeck Ler 2009l10n_assNessuna valutazione finora
- Weight gain by birth weight and age groups for boysDocumento1 paginaWeight gain by birth weight and age groups for boysl10n_assNessuna valutazione finora
- F E T C: Luid AND Lectrolyte Herapy IN HildrenDocumento12 pagineF E T C: Luid AND Lectrolyte Herapy IN HildrenHartantoRezaGazaliNessuna valutazione finora
- Bmi For Age Z-ScoreDocumento1 paginaBmi For Age Z-ScoreTisha Patricia OedoyNessuna valutazione finora
- Vital Signs Reference Chart - 1Documento1 paginaVital Signs Reference Chart - 1l10n_assNessuna valutazione finora
- BMI Chart for Boys Ages 5-19Documento1 paginaBMI Chart for Boys Ages 5-19Justitia LantuNessuna valutazione finora
- CHT Acfa Boys Z 3 5Documento1 paginaCHT Acfa Boys Z 3 5Rivadin NurwanNessuna valutazione finora
- Cunnane2002 Potential Role of Polyunsaturates in Seizure Protection Achieved With The Ketogenic DietDocumento5 pagineCunnane2002 Potential Role of Polyunsaturates in Seizure Protection Achieved With The Ketogenic Dietl10n_assNessuna valutazione finora
- Bmifa Boys Z 5 19 LabelsDocumento1 paginaBmifa Boys Z 5 19 LabelssufigueiraNessuna valutazione finora
- Lubchenco Curve PDFDocumento1 paginaLubchenco Curve PDFWarren Lie25% (4)
- CSFDocumento1 paginaCSFl10n_assNessuna valutazione finora
- Temperature MeasurementDocumento5 pagineTemperature Measurementl10n_ass100% (1)
- Dahlin2005 The Ketogenic Diet Influences The Levels of Excitatory and Inhibitory Amino Acids in The CSF in Children With Refractory EpilepsyDocumento11 pagineDahlin2005 The Ketogenic Diet Influences The Levels of Excitatory and Inhibitory Amino Acids in The CSF in Children With Refractory Epilepsyl10n_assNessuna valutazione finora
- Cross2013 New Research With Diets and EpilepsyDocumento6 pagineCross2013 New Research With Diets and Epilepsyl10n_assNessuna valutazione finora
- PDFDocumento1 paginaPDFl10n_assNessuna valutazione finora
- GCS PDFDocumento1 paginaGCS PDFFrincia100% (1)
- CSFDocumento1 paginaCSFl10n_assNessuna valutazione finora
- PDFDocumento1 paginaPDFl10n_assNessuna valutazione finora
- Brodie2005 Diagnosing and Predicting Refractory EpilepsyDocumento4 pagineBrodie2005 Diagnosing and Predicting Refractory Epilepsyl10n_assNessuna valutazione finora
- Best2000 Cardiac Complications in Pediatric Patients On The Ketogenic DietDocumento3 pagineBest2000 Cardiac Complications in Pediatric Patients On The Ketogenic Dietl10n_assNessuna valutazione finora
- Bough2007 Anticonvulsant Mechanisms of The Ketogenic DietDocumento16 pagineBough2007 Anticonvulsant Mechanisms of The Ketogenic Dietl10n_assNessuna valutazione finora
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (890)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (587)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (265)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (119)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- STA 100: Midterm II Practice QuestionsDocumento9 pagineSTA 100: Midterm II Practice QuestionsxinnianhaoNessuna valutazione finora
- Claire Winzar 2020001513 Final Masters Thesis Amended July2022Documento278 pagineClaire Winzar 2020001513 Final Masters Thesis Amended July2022api-269699003Nessuna valutazione finora
- Clinical Pharmacy: 4 ProfessionalDocumento300 pagineClinical Pharmacy: 4 ProfessionalMobeen AhmedNessuna valutazione finora
- FNCP, Rnking and Scaling, Home Visit PlanDocumento6 pagineFNCP, Rnking and Scaling, Home Visit Planmarie100% (10)
- Chapter One 1.1 History of SiwesDocumento19 pagineChapter One 1.1 History of SiwesOpeyemi JamalNessuna valutazione finora
- Test Bank For Pathophysiology 6th Edition by BanasikDocumento36 pagineTest Bank For Pathophysiology 6th Edition by Banasikknobbyettinjn4u4f100% (37)
- Case Study MNT 1Documento7 pagineCase Study MNT 1api-270486515Nessuna valutazione finora
- Oxford American Cardiology Library HypertensionDocumento190 pagineOxford American Cardiology Library HypertensionWesker Albert100% (1)
- Antihypertensive Effect of Piper Sarmentosum in L - Induced Hypertensive RatsDocumento8 pagineAntihypertensive Effect of Piper Sarmentosum in L - Induced Hypertensive RatsM Hilmi Yanuardi YanuardiNessuna valutazione finora
- Blood Pressure Log Excel TemplateDocumento8 pagineBlood Pressure Log Excel TemplateZeeshan Hyder Bhatti100% (1)
- Balbas Pusa Scientific NameDocumento6 pagineBalbas Pusa Scientific NameJay-Anne BarbadoNessuna valutazione finora
- Low Sodium Diet-A Solution To Health Related ProblemsDocumento2 pagineLow Sodium Diet-A Solution To Health Related ProblemsTanzila SiddiquiNessuna valutazione finora
- Self-Reported Measure Validity for Medication Adherence PredictionDocumento9 pagineSelf-Reported Measure Validity for Medication Adherence PredictionEsti AsadinaNessuna valutazione finora
- Assessment Subjective "Madalas Ako Mahilo" As VerbalizedDocumento2 pagineAssessment Subjective "Madalas Ako Mahilo" As VerbalizedMhek_Calaguio_2659Nessuna valutazione finora
- FNCP (Hypertension)Documento3 pagineFNCP (Hypertension)Jose Emmanuel Ribaya RuivivarNessuna valutazione finora
- Facts and Definition of EclampsiaDocumento5 pagineFacts and Definition of EclampsiaChoi Gong JuNessuna valutazione finora
- ARB and CCB CombinationDocumento11 pagineARB and CCB CombinationLucky PratamaNessuna valutazione finora
- Stats 2B03 Test #1 (Version 1) October 27th, 2010Documento7 pagineStats 2B03 Test #1 (Version 1) October 27th, 2010examkillerNessuna valutazione finora
- Toeflexercise9 ReadingDocumento10 pagineToeflexercise9 Readingklosejn100% (1)
- Cardiovascular Disease BrochureDocumento2 pagineCardiovascular Disease BrochureKawooya Ismael100% (1)
- OCR GCSE Biology B Specification (2012) (J263)Documento152 pagineOCR GCSE Biology B Specification (2012) (J263)astargroupNessuna valutazione finora
- Patient Safety in HemodialysisDocumento14 paginePatient Safety in HemodialysisioakasNessuna valutazione finora
- Angiotensin Receptor Blockers (O)Documento26 pagineAngiotensin Receptor Blockers (O)farmasi_hmNessuna valutazione finora
- Nursing Writing PDFDocumento42 pagineNursing Writing PDFRyu Tse50% (2)
- The 5 Hidden: Libido KillersDocumento6 pagineThe 5 Hidden: Libido KillersscribduserNessuna valutazione finora
- Primary and Secondary CV Prevention - Iman EvanDocumento104 paginePrimary and Secondary CV Prevention - Iman EvanFikriYTNessuna valutazione finora
- MEDICAL - APPLICATIONS - OF - YOGA of DR NAGARATNA PDFDocumento86 pagineMEDICAL - APPLICATIONS - OF - YOGA of DR NAGARATNA PDFKIRAN GARGYANessuna valutazione finora
- Parmed Xpreg PDFDocumento4 pagineParmed Xpreg PDFriddhiNessuna valutazione finora
- Clinical Case 4 PresentationDocumento42 pagineClinical Case 4 PresentationRUSSELL CILOTNessuna valutazione finora
- Women's Heart HealthDocumento3 pagineWomen's Heart HealthMatt ThielkeNessuna valutazione finora