Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Elaziz & Bakr 2008 PDF
Caricato da
Rusida LiyaniDescrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Elaziz & Bakr 2008 PDF
Caricato da
Rusida LiyaniCopyright:
Formati disponibili
Khaled M. Abd Elaziz and Iman M.
Bakr
Assessment of knowledge, Attitude
Assessment of knowledge, attitude and practice of hand washing
among health care workers in Ain Shams University hospitals in
Cairo.
Khaled M. Abd Elaziz, Iman M. Bakr
Community, Environmental and occupational department, Faculty of medicine, Ain
Shams University, Cairo
Abstract
Background: Most nosocomial infections are thought to be transmitted by the hands
of health care workers. The aims of this work were to assess the knowledge, attitude
and practice of hand washing among health care workers (HCW) in Ain-Shams
University hospitals and to assess its different wards for facilities required for hand
washing (HW). Methods: A cross-sectional descriptive and observational study was
conducted for six months from June till November 2006. It included preparatory
phase, observational phase for practice and assessment of knowledge & attitude
through self-administered questionnaire to HCW in 10 different departments. 2189
opportunities among HCW were observed. Results: Doctors showed a significantly
higher compliance (37.5%) than other groups of HCW (P=0.000), however only
11.6% of them had done the HW in an appropriate way. The most common type of
HW practiced among HCW was the routine HW (64.2%) and the least was the
antiseptic HW (3.9%). Having a short contact time and improper drying (23.2%) was
the most common form of inappropriate HW. Most of the wards had available sinks
(80%) but none of them had available paper towels. The mean score knowledge was
higher in nurses than in doctors (42.611.7 versus 39.110.5). 97.3% of the nurses
believe that administrative orders and continuous observation can improve hand
washing practices. Conclusion: Compliance to hand washing was low.
Implementation of multifaceted interventional behavioral hand hygiene program with
continuous monitoring and performance feedback, increase supplies necessary for
HW and institutional support is important for improving the compliance of hand
hygiene guidelines.
Keywords: hand washing, medical health care workers, knowledge, attitude, practice
Introduction
Most nosocomial infections are
thought to be transmitted by the hands
of health care workers. It has long been
known that hand hygiene among health
care workers plays a central role in
preventing the transmission of
infectious agents. Hand-washing is the
most effective way of preventing the
spread of infectious diseases.(1) But
despite
a
Joint
Commission
requirement that Centers for Disease
Control and Prevention hand hygiene
guidelines
be
implemented
in
The Egyptian Journal of Community Medicine
hospitals, compliance among health
care workers remains low. (2)
The reasons of lack of compliance to
hand washing include: lack of
appropriate equipment, low staff to
patient ratios, allergies to hand
washing
products,
insufficient
knowledge among staff about risks and
procedures, the time required and
casual attitudes among staff towards
biosafety. (3)
Improved compliance with hand
washing was associated with a
significant decrease in overall rates of
Vol. 26
No. 2
April 2008
Khaled M. Abd Elaziz and Iman M. Bakr
Assessment of knowledge, Attitude
nosocomial infection and respiratory
infections in particular. (4)
Hand hygiene technique is seldom
incorporated into research studies and
audits
designed
to
increase
compliance. As a result, numerous
unanswered
questions
remain
concerning this aspect of hand
hygiene.(5) In order to be effective,
efforts to improve compliance with
hand washing guidelines must be
multifaceted (6) and should include
increasing
the
availability
and
accessibility of hand washing sinks and
alcohol-based hand rubs. (7)
Aim of the work
1- Assessment of knowledge,
attitude and practice of hand
washing among health care
workers (HCW) in Ain- Shams
University hospitals
2- Assessment of different wards
in Ain- Shams University
hospitals for facilities required
for hand washing
Subjects and methods
A cross sectional descriptive &
observational study was conducted in
Ain Shams University hospitals. The
practical part extended for six months
(from June till November 2006) was
implemented in three phases:
Phase one: Preparatory phase, Two
infection control nurses from 10
departments were selected and trained
on
observing
hand
washing
opportunities and filling out the forms
needed. Training included lectures on
the importance of hand washing and its
impact on nosocomial infection rate
and the correct practice of hand
washing.
Phase two: Observational phase, a) for
HCW, Observational forms to record
the events in each opportunity
The Egyptian Journal of Community Medicine
observed as regard the hand washing
compliance (done or not done) and
hand washing technique and practices
(if done). The observation was done
unobtrusively. The opportunities of
hand
washing
included
those
opportunities where the HCW could do
invasive procedures, come into
personal contact with the patient, do
non-invasive procedures as blood
pressure or temperature measurement,
body fluid contact, waste disposal or
come in contact with contaminated
inanimate
objects.
Multiple
opportunities could be observed for a
single health care worker. b) Ward
inspection forms were filled throw
inspection of the availability of
facilities needed for hand washing in
each department, as hand hygiene
guidelines, posters, sinks, towels, soap,
alcohol-based hand rubs and gloves.
Phase three: assessment of knowledge
and attitude of hand washing through a
self-administered questionnaire. It
targeted different aspects, indications
and types of hand washing for doctors
and nurses (20 questions) and workers
(10 questions). Questions about
knowledge were answered as True,
False or Unsure. They included: Is HW
indicated even if sterile gloves were
used? The most common mode of
transmission of infection is through
hands of HCW? Four questions on
different techniques of hand washing
whether routine, antiseptic or alcohol
hand rub and the difference between
them. Two questions on the minimum
time needed for routine and antiseptic
HW. Also question on hand drying
after antiseptic HW and turning the tap
off,. Whether routine HW is done after
doing invasive procedure or not, and if
the hands are contaminated with blood,
is it a must to use antiseptic HW. Also
questions on the action of soap and
alcohol on the flora of the skin,
bacteria and viruses, the type of the
antimicrobial used in relation to the
Vol. 26
No. 2
April 2008
Khaled M. Abd Elaziz and Iman M. Bakr
Assessment of knowledge, Attitude
onset and duration of action. Types of
alcohol used in alcohol hand rub.
Whether adding glycerine can reduce
skin irritation and whether rinsing
betadine scrub should be done
immediately (before iodine irritates the
skin)
Attitude questionnaire included 4
questions and were filled by nurses in
different departments. They included:
Whether HW is protective to HCW,
whether it could be improved by
administrative orders and continues
observation, whether it lowers the
nosocomial infection rate more than
any other measure and whether it could
be improved in their hospitals by good
role models by doctors.
A total score was given to the
knowledge (out of 20) and attitude
questionnaire (out of 20). Attitude
questions were four questions based on
Likart scale. Totally agree and agree
answers were considered as positive
attitude and a percentage was
calculated.
Forms were revised for completeness
and consistency. Data entry, data
checking and data analysis were done
with the program SPSS (Statistical
package for social science) version
11.0.5.
Ethical consideration: approval of the
design and steps of the study were
conducted with members of the
infection control unit in Ain Shams
University hospitals. A consent was
taken from the participants of the study
before answering the questionnaires.
Also the observation of the hand
washing practices was among the
routine work of the infection control
nurse responsible for all the activities
of infection control in the studied units.
Results
2189 opportunities among health care
workers in Ain Shams University
The Egyptian Journal of Community Medicine
hospital were observed for compliance
to hand Hygiene.
Most of the observed opportunities for
hand washing were done by nurses
(1180) followed by doctors (465).
Collectively doctors (37.5%) showed a
significantly higher compliance to
hand washing than the other groups of
health care workers (P=0.000),
however only 11.6% of them had done
the hand hygiene in an appropriate way
(Table 1).
Departments
included
in
the
observations were the Orthopedic,
neurosurgery, plastic and general
surgery (722 observations), pediatric,
gynecology and chest intensive care
units (1193 observations) and the
hematology departments.(Table 2)
The most practiced type of hand
washing among the health care
workers was the routine hand washing
(64.2%) and the least was the
antiseptic hand wash (3.9%). (Table 2)
Hand washing was observed during
different intervention. Hand washing
was performed at a higher rate after
doing the different intervention than
before doing them, however hand
washing was done in a more
appropriate way before doing the
different intervention than after doing
them except for the non-invasive
procedures were it was nearly similar
before and after.
A self-administered questionnaire
containing twenty different aspects,
indications and types of hand washing
was filled by 152 HCW. Workers were
allowed to answer only 10 of these
items. The mean score knowledge was
higher in nurses than in doctors
(42.611.7 versus 39.110.5).
The assessment of the knowledge of
HCWs in different departments
showed that the highest mean scores
was in the NICU pediatric department.
Doctors had high mean score in
knowledge in General surgery
department 7 (47.58.6), nurses
Vol. 26
No. 2
April 2008
Khaled M. Abd Elaziz and Iman M. Bakr
Assessment of knowledge, Attitude
(482.7) and workers (63.31105) in
the NICU pediatric department. (Table
4)
Although the highest mean knowledge
of hand washing was among nurses in
the NICU pediatric 48.02.7 yet the
lowest attitude scores were found
among nurses in the same department
68.0 7.5 (results not shown in tables).
As regards the attitude of nurses
towards hand hygiene, it was found
that 96% of nurses believe that hand
washing is protective health care
personnel from infection. Also it is
noted that 97.3% of the nurses believe
that
administrative
orders
and
continuous observation can improve
hand washing practices. As regards
lowering of nosocomial infection rates
92% of the nurses believe that this
method (Hand washing) can lower
nosocomial infection rates more than
any other method of infection control
Only 70.7% of the nurses had positive
attitude towards the improvement of
hand washing by watching role models
do hand washing. (Table 5)
The
most
common
form
of
inappropriate hand washing was in the
improper drying and having short
contact time(23.2%).(Figure 1).
As regards the ward assessment, most
of the wards had available sinks (80%)
and none of them had available paper
towels. (Table 6)
Discussion
Hand hygiene prevents cross infection
in hospitals, however adherence to
guidelines is commonly poor. (8) While
the techniques involved in hand
hygiene are simple, the complex
interdependence of factors that
determine hand hygiene behavior
makes the study of hand hygiene
complex. (9)
In our study the overall hand hygiene
compliance among Health care
workers is 34%, this agrees with
Patarakul et al., (2005) who had found
The Egyptian Journal of Community Medicine
from their observational study that
hand hygiene among HCWs before
patient contact was less than 50%.(10)
Also it agrees with Pittet et al., (2000)
who had observed 20000 opportunities
for hand hygiene before implementing
a hand hygiene campaign during
routine patient care in a teaching
hospital in Geneva to be 48%.(11)This
gives an idea for our need to such
programs in order to raise our
compliance to hand hygiene. Our result
was much better than Kim et al.,
(2003) study who had found the
overall compliance of hand washing to
be 22.1%.(12)
As regard compliance to hand hygiene
in ICU. Our results in the chest
ICU=33.4%, NICU ped.= 62.5%
&NICU gyn.39.4%, were much better
than Rosenthal et al., (2003) who had
found a rate of 23.1% before
implementing
a
hand
hygiene
education, training and performance
feedback program in one medical
surgical ICU and one coronary ICU of
one hospital in Argentina.(13) Also our
results lie within the range of Lipsett &
Swoboda (2001) which is 28%74%.(14)Our results were comparable
with Won et al., (2004) who had
conducted their study in NICU in a
level III teaching hospital where they
found compliance to hand hygiene to
be 43%.(4)
As regard the variation in compliance
to hand washing hygiene among
different health care workers. Doctors
showed the highest compliance
(37.5%) in comparison to nurses
(36.4%) and housekeepers (22.6%) and
this disagree with Lipsett and Swoboda
(2001) who had found that nurses
showed higher compliance (50%) than
doctors (15%) and nursing supporting
personnel (37%).(14) Minimizing the
gap found between the knowledge and
attitude in nurses as found in Pediatric
Vol. 26
No. 2
April 2008
Khaled M. Abd Elaziz and Iman M. Bakr
Assessment of knowledge, Attitude
NICU could improve the compliance
rates to HW in nurses.
The mean score knowledge on hand
washing was higher among nurses than
among doctors (42.6 11.7 versus
39.110.5 resp.), however Zakzouk et
al., (2004) had found a slight
difference between them (94.77.0,
95.27.4 resp.) and showed a
collectively higher means compared to
our results in their study conducted in a
burn unit in Ain Shams University
hospital including 9 physicians and 19
nurses.(15) Mohamed, (1999) had found
the level of correct knowledge about
HW among health care workers in
Elgalaa governmental hospital was
73.1% and in Cleopatra private
hospital was72.7%.(16)
Good hand washing technique,
ensuring that all surfaces of the hands
receive
contact
with
the
decontaminating agent, has been
accepted for many years and is
acknowledged in current guidelines .(5)
23.2% of the observed opportunities
showed inappropriate hand washing.
This appeared most in both having a
short contact time less than 30 sec. and
improper drying. Basurrah and Madam
(2006) who had studied hand washing
in medical and surgical wards in a
tertiary center in Riyadh found that the
duration of hand washing was
suboptimal for all HCWs.(7) 14.5% of
our opportunities showed improper
drying of hands, Kuzu et al., (2005) in
a university hospital in Turkey found
that 79.8% of HCWs didn't dry their
hands.(17) Mohamed, (1999) had found
that HW was done correctly in 14.4%
of HCW (doctors and nurses) in
Elgalaa hospital and 44.7% in
Cleopatra hospital.(16) Talaat, (1998)
had reported that 90 % of the nurses in
his study were performing hand
washing inadequately.(18) Appropriate
health education programs should be
The Egyptian Journal of Community Medicine
implemented to raise the compliance in
this issue.
A complex interplay of cognitive,
socioeconomic and technical factors
may determine hand washing practice
among hospital based health workers
especially doctors, regardless of the
location of the country or hospital they
work in. (19) Administrative support (13)
and improved availability of resources
(20)
provides a positive influence in
efforts to improve HW adherence to
improve infection control in hospitals.
In our study ward assessment had
marked deficiency in supplies and
resources necessary for performing
hand washing as only 10% of the
wards had available automatic sinks
and hand drying material. Only 40% of
the wards had sinks where soap was
available. Ji et al., (2005) had found
that being short of water accounted for
22% of reasons of non compliance to
hand washing.(21) In our study 20% of
the observed wards had no available
sinks. Improving the availability of
materials and supplies essential for
hand hygiene is a basic step in
improving the compliance with hand
washing.
Alcohol- based rubbing reduces the
mean bacterial counts on hands more
effectively than hand washing with
antimicrobial soaps (22,23). In our study
64.2% of the observed opportunities in
this study used routine hand washing
with soap, in comparison to 99.3% in
Kuzu et al., (2005) study and only
31.7% used alcohol hand rub in
comparison to Wendt et al., (2004)
(52.2%) who had conducted his study
in a university hospital in Heidelberg,
Germany.(17,24) Hand hygiene through
alcohol hand rub need to be increased
through
increase
supply
and
continuous education. Whitby et al.,
(2008) had found that introduction of
Alcohol based hand rub without an
Vol. 26
No. 2
April 2008
Khaled M. Abd Elaziz and Iman M. Bakr
associated
program
Assessment of knowledge, Attitude
behavioral modification
proved
ineffective.(25)
As regard washing hands before and
after doing different procedures, 20.6%
and 7.9% of HCW wash their hands
before and after invasive procedures in
comparison to 13.8% and 35.6% in
Arenas et al., (2005) study who had
conducted their study among HCW in
haemodialysis units in Spain.(26) HCW
should be keen not to transmit
infection to their patients and raising
the awareness of HCW in this issue is
very important. Kim et al., (2003) had
found a positive association between
glove use and subsequent hand
disinfection.(12) 22.5%, 38.6% and
70.4% of the nurses in Hassan and
Aboul-Asm, (2007) study performed
hand washing after removing gloves,
patient contact and after body fluid
contact in comparison to 61.4%, 43.9%
and
39.8%
of
the
observed
opportunities among HCW in our
study.(27) Differences in the health team
covered and the method of the
assessment might have created the
discrepancy in the results.
Our results showed a higher positive
attitude among nurses (96.0%) towards
HW protection of health care personnel
in comparison to 86.2% in Nobile et
al., (2002) study in Italy among HCWS
in ICUs.(28)
97.3% of the nurses in our study
believe HW practices can be improved
by administrative orders and this
contradicts Harris et al.,(2000) who
found that healthcare workers are not
in favor of interventions involving
rewards and punishments, but are more
attracted to interventions that make
hand-washing easier.(29)
Using hand hygiene as a sole measure
to reduce infection is unlikely to be
successful when other factors in
The Egyptian Journal of Community Medicine
infection
control,
such
as
environmental hygiene, crowding, stuff
levels and education are inadequate (9).
Only 70% of the 10 wards observed in
our study, their stuff received formal
education on hand washing hygiene.
All HCW should have continuous
education to raise their awareness and
compliance towards hand washing
hygiene. Also only 30% of the
observed wards had written hand
hygiene guidelines. These guidelines
should be generalized to all wards of
the hospital.
Recommendations
Implementation
of
multifaceted
interventional behavioral hand hygiene
program is important for improving the
compliance
to
hand
hygiene
guidelines.
Implementation of hand washing
training programs for undergraduate
doctors, house officers and nurses.
Those training programs should be
done at intervals and assessed for the
improvement of hand washing
practices
Continuous
monitoring
and
performance feedback is beneficial
beside increase in supplies necessary
for hand washing and institutional
support.
References
1)Anderson JL, Warren CA, Perez
E, Louis RI, Phillips S, Wheeler J,
Cole
M,
Misra
R.
Gender and ethnic differences in hand
hygiene practices among college
students. Am J Infect Control. 2008
Jun;36(5):361-8.
2)Haas
JP,
Larson
EL.
Compliance with hand hygiene
guidelines: where are we in 2008? Am
J Nurs. 2008 Aug;108(8):40-4; quiz
45.
3) WHO (2004).
Vol. 26
No. 2
April 2008
Khaled M. Abd Elaziz and Iman M. Bakr
Assessment of knowledge, Attitude
Practical guidelines for infection
control in health care facilities.2004;
Annex1:76-80
4) Won SP, Chou HC, Hsieh WS,
Chen CY, Huang SM, Tsou KI, Tsao
PN
Hand-washing program for the
prevention of nosocomial infections in
a neonatal intensive care unit. Infect
control Hosp Epidemiology. 2004
Sep;25(9):742-6.
5) Gould D, Drey N.
Hand hygiene technique. Nurs Stand.
2008 Apr 30-May; 6;22(34):42-6.
6) Creedon SA
Healthcare
workers'
hand
decontamination practices: compliance
with recommended guidelines. J Adv
Nur 2005 August; 51(3):208-16.
7) Basuurah MM, Madani TA.
Hand washing and gloving practice
among health care workers in medical
and surgical wards in a tertiary care
center in Riyadh, Saudi Arabia. Scand
J Infect Dis. 2006; 38(8):620-4
8) Chistiaens G, Barbier C, Mutsers
J, Warnotte J, De Mol P, Bouffioux
C.
Hand hygiene: first measure to control
nosocomial infection. Rev Med Liege.
2006 Jan; 61(1):31-6
9) Akyol A, Ulusoy H, Ozen I
Hand washing: a simple, economic and
effective method for preventing
nosocomial infections in intensive care
units. J Hosp Infect.2006 Apr;
62(4):395-405.
10) Patarakul K, TanKhum A,
Kanha
S,
Pandungpean
D,
Jaichaiyapum OO.
Crosssectional survey of hand-hygiene
compliance and attitudes of health care
workers and isitors in the intensie care
units at King Chulalongkorn Memorial
Hospital. Med Assoc Thai. 2005 Sep;
suppl 4: S287-93.
11) Pittet D, Hugonnet S, Harbarth
S, Mourouga P, Sauan , Touveneau
S, Perneger TV.
The Egyptian Journal of Community Medicine
Effectiveness of a hospital wide
programme to impove compliance with
hand hygiene. Infection Control
Program.
Lancet.
2000
Oct;
356(9238): 1307-12.
12) Kim PW, Roghmann MC,
Perencevich EN, Harris AD.
Rates of hand disinfection associated
with glove use, patient isolation, and
changes between exposure to various
body sites. Am J Infect Conrol. 2003
Apr; 31(2): 97-103.
13) Rosenthal VD, Guzman S,
Pezzotto SM, Crnich CJ.
Effect of an infection control program
using education and performance
feedback on rates of intravascular
device
associated
bloodstream
infections in intensive care units in
Argentina. Am J Infect Control. 2003
Nov; 31(7): 405-9.
14) Lipsett PA, Swoboda SM. (2001).
Hand washing compliance depends on
professional status. Surg Infect
(Larchmt). 2001 Fall; 2(3):241-5.
15) Zakzouk HS, El- Senousy T,
Hussain M.
Infection control standards in burn
unit. The new Egyptian J of medicine.
2004 Sept; 31(3):7-17
16) Mohamed M.
Sources of infection in intensive care
unit& a suggested control system.
Master degree thesis in medical
surgical nursing.1999 High institute of
nursing. Ain Shams University.
17) Kuzu N, Ozer F, Aydemir S,
Yalcin AN, Zencir M.
Compliance with hand hygiene and
glove use in a university-affiliated
hospital.
Infect
Contol
Hosp
Epidemiol. 2005 Mar; 26(3):312-5.
18) Talaat E.
Tracheostomy care self learning
package, its effect on nurses
knowledge and performance, medical
surgical nursing, Doctorate Degree,
2001 High Institute of nursing, Ain
Shams University
Vol. 26
No. 2
April 2008
Khaled M. Abd Elaziz and Iman M. Bakr
Assessment of knowledge, Attitude
19) Samuel R, Almedom AM, Hagos
G, Mutungi A.
Promotion of hand washing as a
measure of quality of care and
prevention
of
hospital-acquired
infections in Eritea: the Keren study.
Afr Health Sci. 2005 Mar; 5(1):4-13
20) Stein AD, Makarawo TP, Ahmad
MF.
A survey of doctor's and nurse's
knowledge, attitudes and compliance
with infection control guidelines in
Birmingham teaching hospital. J Hosp
Infect. 2003 May;54 (1):68-73
21) Ji G, Yin H, Chen Y.
Prevalence of and risk factors for noncompliance with glove utilization and
hand hygiene among obstetrics and
gynecology workers in rural China. J
Hosp Infect. 2005 Mar; 59(3):235-41
22) Karabay O, Sencan I, Sahin I,
Alpteker H, Ozcan A, Oksuz S.
Compliance and efficacy of hand
rubbing during in- hospital practice.
Med Princ Pract. 2005 Sep Oct; 14(5):
313-7.
23) Kac G, Podglajen I, Gueneret M,
Vaupr S, Bissery A, Meyer
G.(2006)
Microbiological evaluation of two
hand hygiene procedures achieved by
healthcare workers during routine
patient care: a randomized study. J
Hosp Infect. 2006 Jan;62(1):129.
24) Wendt C, Knautz D, Von Baum
H.
Differences in hand hygiene behavior
related to the contamination risk of
healthcare activities in different groups
of healthcare workers. Infect Control
The Egyptian Journal of Community Medicine
Hosp Epidemiol. 2004 Mar; 25(3):
203-6
25) Whitby M, McLaws ML, Slater
K,
Tong
E,
Johnson
B.
Three successful interventions in
health care workers that improve
compliance with hand hygiene: is
sustained replication possible?Am J
Infect Control. 2008 Jun;36(5):349-55.
26) Arenas MD, Sanchez-Paya J,
Bail G, Garcia- Valdecasas J, Goriz
JL, Soriano A, Antolin A, Lacueva J,
GarciaS, Sirvent A, Espinosa M,
Angoso M.
A multicentric survey of the practice of
hand hygiene in haemodialysis units:
factors affecting compliance. Nephrol
Dial Transplant. 2005 Jun;20(6):116471. Epub 2005 Mar15.
27) Hassan HE, Aboul Asm SF.
Infection control education: A creative
Approach. The new Egyptian J of
medicine. 2007 Jan; 36 (1):67-73
28) Nobile C, Diac E, Mantuori P,
Villari P.
Healthcare personnel and hand
decontamination in intensive care
units: knowledge, attitudes, and
behaviour in Italy . Journal of Hospital
Infection , 2002; 51 (3 ): 226 232
29) Harris A, Nafziger R, Samore M,
DiRosario K, Roghmann M, Carmeli
Y.
A survey on handwashing practices
and opinions of healthcare workers .
Journal of Hospital Infection , 2000; 45
(4): 318 321.
Vol. 26
No. 2
April 2008
Khaled M. Abd Elaziz and Iman M. Bakr
Assessment of knowledge, Attitude
(A) Observation of hand- washing (HW)opportunities
Table 1: Compliance to hand hygiene among different groups of health care
workers in Ain Shams University
Health care
workers
Doctors
Nurses
Housekeepers
Others*
Total
Opportunities
Observed
Total
465
1180
296
248
2189
No.
174
429
67
75
745
Done
(%)
37.5
36.4
22.6
30.2
34.0
Hand Washing
Appropriate
No.
(%)
54
11.6
44
3.7
1
0.3
12
4.8
111
5.1
X2=23.9
P=0.000
X2=52.5
P=0.000
*Others include waste disposal workers and janitors
Table 2: Compliance to hand hygiene among different departments and in
different procedures in Ain Shams university hospitals
Opportunities
Observed
Departments:
Orthopedic
Neurosurgery
Plastic surgery
General surgery 7
NICU Pediatric
NICU Gynecology
Hematology
Chest ICU
Procedures:
Invasive procedures
Non-invasive procedures
Personal contact
Body fluids contact
Contaminated inanimate objects
Waste handling
After using gloves
Total
The Egyptian Journal of Community Medicine
No.
Hand Washing
Appropriate
%
No.
%
115
157
294
156
480
345
274
368
16
2
32
63
300
136
73
123
13.9
1.3
10.9
40.4
62.5
39.4
26.6
33.4
8
0
4
0
67
29
3
0
6.9
0
1.3
0
13.9
8.4
1.1
0
753
501
157
191
249
224
114
2189
258
160
69
76
52
60
70
745
34.3
31.9
43.9
39.8
20.9
26.8
61.4
34.0
34
39
7
22
3
3
3
111
4.5
7.7
4.4
11.5
1.2
1.3
2.6
5.1
Vol. 26
Done
No. 2
April 2008
Khaled M. Abd Elaziz and Iman M. Bakr
Assessment of knowledge, Attitude
Table 3: Appropriateness of hand washing in different types of hand washing
and before and after different procedures among HCW in Ain Shams University
hospitals
HW done
Appropriate
HW
No
%
Types of hand washing (HW):
No
%
17
3.5
480
64.2
Routine HW
8
27.6
29
3.9
Antiseptic HW
86
36.4
236
31.7
Alcohol hand rub
111
14.9
745
100
Total
Appropriate HW before &after interventions
No. of H.W. done
1- Invasive Procedure
22
20.6
107
Before
12
7.9
151
After
34
13.1
258
Total
2- Non invasive Procedure
16
23.9
67
Before
23
24.7
93
After
39
24.4
160
Total
3- Personal contact
4
18.2
22
Before
3
6.4
47
After
7
10.2
69
Total
4- Body fluids contact
12
63.2
19
Before
10
17.5
57
After
22
28.9
76
Total
5- Contaminated inanimate objects
2
14.3
14
Before
1
2.6
38
After
3
5.8
52
Total
6- Wastes handling
1
25.0
4
Before
2
3.6
56
After
3
5.0
60
Total
7- Using gloves
1
50
2
Before
2
2.9
68
After
3
4.3
70
Total
The Egyptian Journal of Community Medicine
Vol. 26
No. 2
April 2008
Khaled M. Abd Elaziz and Iman M. Bakr
Assessment of knowledge, Attitude
B) Knowledge assessment of hand washing practices
Table 4: Comparison between the mean knowledge scores of HCWS, doctors,
nurses and workers in different departments in Ain Shams University
Department
HCWS
Doctors
Nurses
N=152
N=42
N=75
Mean+ SD
Orthopedic
36.715.2
25.8 8.0
44.215.3
Neurosurgery
42.910.1
44.010.4
33.3 2.8
Plastic surgery
41.811.9
40.0 7.0
37.711.9
General Surgery 7
42.29.5
47.5 8.6
41.49.8
NICU Pediatric
51.89.5
46.6 5.7
48.02.7
ICU Pediatric
41.28.5
41.2 8.5
NICU gynecology
41.710.4
43.311.7
42.5 9.5
ICU gynecology
44.114.8
45.010.0
45.0 17.7
Hematology
44.713.4
42.716.6
42.0
2.7
Chest ICU
36.012.8
41.510.8
35.0 9.3
Collective mean knowledge score of doctors, nurses and workers= 39.110.5,
42.611.7 and 44.215.0 respectively
Table (5): Assessment of attitude towards hand washing of Nurses in Ain shams
university
Attitude of nurses
1-HW is protective to health
care personnel
2-HW can be improved by
administrative orders and
continuous observation
3-HW lowers nosocomial
infections more than any
other methods of IC
4-HW can be improved by
role models
No.
72
96.0
73
97.3
69
92.0
53
70.7
The Egyptian Journal of Community Medicine
Vol. 26
No. 2
April 2008
Workers
N=35
50.00
47.59.5
55.05.7
40.010.0
63.311.5
37.59.5
40.028.2
52.010.9
26.015.1
Khaled M. Abd Elaziz and Iman M. Bakr
Assessment of knowledge, Attitude
Table 6: Ward assessment in different departments in Ain Shams University
hospitals (n=10)
Items
No. (%)
Number of available sinks
8 (80)
Number of sinks where soap is available
4 (40)
Availability of hand drying material
1 (10)
Availability of paper towel
0 (0)
Availability of cloth towel
1 (10)
Availability of alcohol hand rub
4 (40)
Availability of automatic sinks
1 (10)
Availability of gloves at point of care
7 (70)
Written hand hygiene guidelines
3 (30)
Availability of communication material for hand hygiene(HH)
5 (50)
Staff formally educated on HH
7 (70)
A product selection process has been implemented
1 (10)
Feedback performance provided to staff
1 (10)
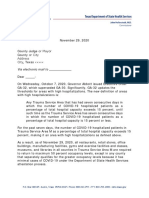
25
23.2
20
18.8
15.7
15
14.5
9.9
10
7.9
5.6
4.3
5
0
A+
B+
A+
B+
d
B
ne
A+
ea
cl
rs
es
c
he
rfa
Ot
su
e
ll
im
ta
tt
No
ac
Cnt
o
tc
ng
or
yi
Sh
dr
Ber
op
pr
Im
A-
Figure 1: Forms of inappropriate hand hygiene among observed opportunities
(Total 605)
A- Improper drying is any method of dying other than dying in fresh clean towel
B- Short contact time is below 30 seconds in routine hand washing and alcohol hand
rub, or less than 2 minutes in hygiene wash.
C-Not all surfaces cleaned
D-Others
The Egyptian Journal of Community Medicine
Vol. 26
No. 2
April 2008
Potrebbero piacerti anche
- Practice of Five Moments of Hand Hygiene Amongthe Nurses in Selected Hospitals in UaeDocumento7 paginePractice of Five Moments of Hand Hygiene Amongthe Nurses in Selected Hospitals in UaeAJHSSR JournalNessuna valutazione finora
- Handhygiene 2Documento7 pagineHandhygiene 2aby sugaraNessuna valutazione finora
- Research ArticleDocumento8 pagineResearch ArticleVian HertaminaNessuna valutazione finora
- Hand Hygiene Practice Among Pharmacy Staffs in Miri General Hospital 102 112Documento11 pagineHand Hygiene Practice Among Pharmacy Staffs in Miri General Hospital 102 112Maizura Syahirah MohtadaNessuna valutazione finora
- The Impact of Gown-Use Requirement On Hand Hygiene ComplianceDocumento7 pagineThe Impact of Gown-Use Requirement On Hand Hygiene Compliancebouchra8blsNessuna valutazione finora
- ART2016631Documento7 pagineART2016631Tmanoj PraveenNessuna valutazione finora
- HandhygieneDocumento21 pagineHandhygieneAberaNessuna valutazione finora
- Artikel 1Documento29 pagineArtikel 1Nophienyagigghz Luphmoepolephel Anyun'nyuntamaNessuna valutazione finora
- Article - Text 20050 1 10 20220916Documento5 pagineArticle - Text 20050 1 10 20220916NaveedNessuna valutazione finora
- Knowledge of Hand Hygiene and Compliance Among Clinicians - at A Level Six Hospital in Kenya: A Cross Sectional StudyDocumento20 pagineKnowledge of Hand Hygiene and Compliance Among Clinicians - at A Level Six Hospital in Kenya: A Cross Sectional StudyIJAR JOURNALNessuna valutazione finora
- Hand Hygiene Journal HelminaDocumento12 pagineHand Hygiene Journal Helminajoko samudro100% (1)
- Hand Hygiene Compliance in Healthcare WorkersDocumento6 pagineHand Hygiene Compliance in Healthcare WorkersRiska IndrianiNessuna valutazione finora
- Research PaperDocumento10 pagineResearch Paperapi-345759649Nessuna valutazione finora
- Evidence-Based Solution Research Has Proved That Maintaining Hand Hygiene Is EssentialDocumento4 pagineEvidence-Based Solution Research Has Proved That Maintaining Hand Hygiene Is Essentialcate karanjaNessuna valutazione finora
- INFECTION CONTROL: CAN NURSES IMPROVE HAND HYGIENE PRACTICES? by Jacqueline M. Smith, RN, BN, Dyan B. Lokhorst, RN, CHPCN (C), BN (November, 2009) University of Calgary, Faculty of Nursing June, 2009Documento6 pagineINFECTION CONTROL: CAN NURSES IMPROVE HAND HYGIENE PRACTICES? by Jacqueline M. Smith, RN, BN, Dyan B. Lokhorst, RN, CHPCN (C), BN (November, 2009) University of Calgary, Faculty of Nursing June, 2009Rusida LiyaniNessuna valutazione finora
- Faktor Perilaku Cuci Tangan Pakai Sabun CTPS Di SMDocumento8 pagineFaktor Perilaku Cuci Tangan Pakai Sabun CTPS Di SMDwi NopriyantoNessuna valutazione finora
- 2-Article Text-128-2-10-20200328Documento8 pagine2-Article Text-128-2-10-20200328Siti HamsyiahNessuna valutazione finora
- Handwashing NSG Research Paper 2022Documento7 pagineHandwashing NSG Research Paper 2022Kathy LaminackNessuna valutazione finora
- Hand Hygiene Practices Among-19042023-1Documento8 pagineHand Hygiene Practices Among-19042023-1AbigailNessuna valutazione finora
- Strategies To Prevent Healthcareassociated Infections Through Hand HygieneDocumento24 pagineStrategies To Prevent Healthcareassociated Infections Through Hand HygieneRonald CeliNessuna valutazione finora
- Literature Review Hand HygieneDocumento7 pagineLiterature Review Hand Hygienecjxfjjvkg100% (1)
- Hand WashingDocumento11 pagineHand Washinglo99988Nessuna valutazione finora
- Knowledge and Hand Hygiene Practice of Healthcare Workers inDocumento11 pagineKnowledge and Hand Hygiene Practice of Healthcare Workers inBarangay MotibotNessuna valutazione finora
- 44 Iajps44052018 PDFDocumento5 pagine44 Iajps44052018 PDFiajpsNessuna valutazione finora
- ResearchDocumento15 pagineResearchRijelNessuna valutazione finora
- AJN The American Journal of NursingDocumento21 pagineAJN The American Journal of NursingAzman HariffinNessuna valutazione finora
- Compliance With Handwashing in Intensive Care Unit in University Hospitals of La HavanaDocumento4 pagineCompliance With Handwashing in Intensive Care Unit in University Hospitals of La HavanaRomelia E QuiloNessuna valutazione finora
- Baseline Evaluation of Hand Hygiene Compliance in Three Major Hospitals, Isfahan, IranDocumento4 pagineBaseline Evaluation of Hand Hygiene Compliance in Three Major Hospitals, Isfahan, IranIka Yuki HikariNessuna valutazione finora
- Hand Hygiene Study - PITTET !!! 1-s2.0-S0195670109001868-MainDocumento11 pagineHand Hygiene Study - PITTET !!! 1-s2.0-S0195670109001868-MainAgil DaruNessuna valutazione finora
- Hpmij 03 00153Documento6 pagineHpmij 03 00153Azmi SevenfoldismNessuna valutazione finora
- A Study To Assess The Knowledge and Practices of Hand Hygiene Among Nursing Staff in Different Department of The Hospitals in Uttar PradeshDocumento24 pagineA Study To Assess The Knowledge and Practices of Hand Hygiene Among Nursing Staff in Different Department of The Hospitals in Uttar PradeshEditor IJTSRD100% (1)
- Handhygiene GR3Documento8 pagineHandhygiene GR3rivera.alieyaclaireNessuna valutazione finora
- The Problem and Its Setting: "Hand Washing Is Associated With Voluntary Individualistic Behavior." Dean David HolyoakeDocumento3 pagineThe Problem and Its Setting: "Hand Washing Is Associated With Voluntary Individualistic Behavior." Dean David HolyoakeKathleen Camille ManiagoNessuna valutazione finora
- Special Issue 1 3Documento129 pagineSpecial Issue 1 3Amit PasiNessuna valutazione finora
- Observational StudyDocumento5 pagineObservational StudyasumaacocoNessuna valutazione finora
- Hand WashingDocumento9 pagineHand WashingAlexDormanNessuna valutazione finora
- Hand Hygiene ArticleDocumento7 pagineHand Hygiene ArticlechijNessuna valutazione finora
- G H H H - C S: R H I C P A C Hicpac/Shea/Apic/Idsa H H T FDocumento39 pagineG H H H - C S: R H I C P A C Hicpac/Shea/Apic/Idsa H H T FAbidi HichemNessuna valutazione finora
- Pittet, 2003Documento9 paginePittet, 2003Rusida LiyaniNessuna valutazione finora
- Copy1-Okeke Chidima ProjectDocumento38 pagineCopy1-Okeke Chidima Projectmmdt2v544qNessuna valutazione finora
- A Qualitative Exploration of Reasons For Poor Hand HygieneDocumento5 pagineA Qualitative Exploration of Reasons For Poor Hand HygieneMarsha WilliamsNessuna valutazione finora
- Simplifying The World Health Organization Protocol 3 Steps Versus 6 Steps For Performance of Hand Hygiene in A Cluster-Randomized TrialDocumento7 pagineSimplifying The World Health Organization Protocol 3 Steps Versus 6 Steps For Performance of Hand Hygiene in A Cluster-Randomized TrialManuel GuzmanNessuna valutazione finora
- MotivasiDocumento5 pagineMotivasiIrfan MadamangNessuna valutazione finora
- ASurveyof Handwashing Knowledgeand Attitudesamongthe Healthcare Professionalsin Lahore PakistanDocumento7 pagineASurveyof Handwashing Knowledgeand Attitudesamongthe Healthcare Professionalsin Lahore PakistankhadeejakhurshidNessuna valutazione finora
- Effect of Antiseptic Handwashing Vs Alcohol Sanitizer On Health Care-Associated Infections in Neonatal Intensive Care UnitsDocumento7 pagineEffect of Antiseptic Handwashing Vs Alcohol Sanitizer On Health Care-Associated Infections in Neonatal Intensive Care UnitselitamahaputriNessuna valutazione finora
- Smartphone Text Message Service To Foster Hand Hygiene ComplianceDocumento6 pagineSmartphone Text Message Service To Foster Hand Hygiene ComplianceEszter TóthNessuna valutazione finora
- Hand Washing (ABAYOMI OLATUNDE SAMUELDocumento38 pagineHand Washing (ABAYOMI OLATUNDE SAMUELgowon love odiriNessuna valutazione finora
- Patient Safety and Medical ErrorsDocumento8 paginePatient Safety and Medical ErrorsVũ Tuấn TùngNessuna valutazione finora
- Patient-Centered Hand Hygiene. The Next Step in Infection Prevention PDFDocumento7 paginePatient-Centered Hand Hygiene. The Next Step in Infection Prevention PDFJessica SilvaNessuna valutazione finora
- A Study On Knowledge and Practice of Nursing Staff Towards Infection Control MeasuresDocumento17 pagineA Study On Knowledge and Practice of Nursing Staff Towards Infection Control MeasuresPriyanka SatalkarNessuna valutazione finora
- Handrub Vs HandscrubDocumento7 pagineHandrub Vs HandscrubElisya KharuniawatiNessuna valutazione finora
- An Investigation of Nurses ' Knowledge, Attitudes, and Practices Regarding Disinfection Procedures in ItalyDocumento7 pagineAn Investigation of Nurses ' Knowledge, Attitudes, and Practices Regarding Disinfection Procedures in ItalyAlex SemusuNessuna valutazione finora
- Best SoapDocumento8 pagineBest Soapdebby claudiNessuna valutazione finora
- Sarani2015Documento6 pagineSarani2015Mastifa HanasitaNessuna valutazione finora
- 5Documento8 pagine5Hidayat ArifinNessuna valutazione finora
- N014445456 PDFDocumento3 pagineN014445456 PDFIOSRjournalNessuna valutazione finora
- Journal of Hospital Infection: B. Marjadi, M.-L. MclawsDocumento5 pagineJournal of Hospital Infection: B. Marjadi, M.-L. Mclawseman sulaimanNessuna valutazione finora
- Problem-Based Research PaperDocumento12 pagineProblem-Based Research Paperapi-349372265Nessuna valutazione finora
- Fundamental Aspects of Infection Prevention and ControlDa EverandFundamental Aspects of Infection Prevention and ControlNessuna valutazione finora
- Five Disciplines for Zero Patient Harm: How High Reliability HappensDa EverandFive Disciplines for Zero Patient Harm: How High Reliability HappensValutazione: 2 su 5 stelle2/5 (1)
- OJPsych 2014011010170851 PDFDocumento4 pagineOJPsych 2014011010170851 PDFRusida LiyaniNessuna valutazione finora
- Proo Fonly: Healthcare Providers ' Knowledge of Standard Precautions at The Primary Healthcare Level in Saudi ArabiaDocumento8 pagineProo Fonly: Healthcare Providers ' Knowledge of Standard Precautions at The Primary Healthcare Level in Saudi ArabiaRusida LiyaniNessuna valutazione finora
- Hand Disinfectant Practice: The Impact of An Education InterventionDocumento5 pagineHand Disinfectant Practice: The Impact of An Education InterventionRusida LiyaniNessuna valutazione finora
- INFECTION CONTROL: CAN NURSES IMPROVE HAND HYGIENE PRACTICES? by Jacqueline M. Smith, RN, BN, Dyan B. Lokhorst, RN, CHPCN (C), BN (November, 2009) University of Calgary, Faculty of Nursing June, 2009Documento6 pagineINFECTION CONTROL: CAN NURSES IMPROVE HAND HYGIENE PRACTICES? by Jacqueline M. Smith, RN, BN, Dyan B. Lokhorst, RN, CHPCN (C), BN (November, 2009) University of Calgary, Faculty of Nursing June, 2009Rusida LiyaniNessuna valutazione finora
- IPAMS Healthcare and Medical Services Evaluation FormDocumento2 pagineIPAMS Healthcare and Medical Services Evaluation FormManases VelasquezNessuna valutazione finora
- Mega Pa TakafulDocumento12 pagineMega Pa TakafulFarah WahidaNessuna valutazione finora
- Permission LetterDocumento3 paginePermission LetterLouise AxalanNessuna valutazione finora
- DSHS Letter To County Judge GA-32 50 Percent Occupational Capacity in BusinessesDocumento2 pagineDSHS Letter To County Judge GA-32 50 Percent Occupational Capacity in BusinessesMark Schnyder100% (1)
- Colorado COVID-19 Public Health Order April 15, 2021Documento7 pagineColorado COVID-19 Public Health Order April 15, 2021Michael_Roberts2019Nessuna valutazione finora
- Carilion Clinic Announces CEO Murphy's Departure, Agee's SuccessionDocumento5 pagineCarilion Clinic Announces CEO Murphy's Departure, Agee's SuccessionThe Roanoke TimesNessuna valutazione finora
- RLE DR CASES MarcelinoDocumento8 pagineRLE DR CASES MarcelinoArlyn MarcelinoNessuna valutazione finora
- History Taking in Patients With Diabetes - The Hands On Guide To Diabetes Care in Hospital - Wiley Online LibraryDocumento2 pagineHistory Taking in Patients With Diabetes - The Hands On Guide To Diabetes Care in Hospital - Wiley Online Librarymaha altweileyNessuna valutazione finora
- Hospital Management System ProposalDocumento11 pagineHospital Management System ProposalAce WolverineNessuna valutazione finora
- HOSPITAL AssignmentDocumento4 pagineHOSPITAL AssignmentPrity DeviNessuna valutazione finora
- City Limits Magazine, November 1998 IssueDocumento40 pagineCity Limits Magazine, November 1998 IssueCity Limits (New York)Nessuna valutazione finora
- Resume Medis B.inggrisDocumento5 pagineResume Medis B.inggrisgenzizuNessuna valutazione finora
- Personal StatementDocumento2 paginePersonal Statementapi-289732318Nessuna valutazione finora
- Lesson 3 Patient Classification SystemDocumento22 pagineLesson 3 Patient Classification SystemTanya WilliamsNessuna valutazione finora
- Evaluation of The Exit Proformas in Use at Special Wards of A Public Sector Tertiary Care HospitalDocumento14 pagineEvaluation of The Exit Proformas in Use at Special Wards of A Public Sector Tertiary Care HospitalchouguleNessuna valutazione finora
- StarHealthAssureInsurancePolicy PolicyDocumento20 pagineStarHealthAssureInsurancePolicy PolicyAnirudh SagaNessuna valutazione finora
- MAPO Index For Risk Assessment of Patient Manual Handling in Hospital Wards: A Validation StudyDocumento17 pagineMAPO Index For Risk Assessment of Patient Manual Handling in Hospital Wards: A Validation StudySebastian LoperaNessuna valutazione finora
- Handouts 1684Documento26 pagineHandouts 1684Cristine PaningbatanNessuna valutazione finora
- RFP PresentationDocumento6 pagineRFP Presentationssreya80Nessuna valutazione finora
- Model Agreement Insurance Model EHCPDocumento43 pagineModel Agreement Insurance Model EHCPvandana singhNessuna valutazione finora
- Universal Charity: Samael Aun Weor Third EditionDocumento14 pagineUniversal Charity: Samael Aun Weor Third Editionmmmm100% (1)
- Assessing Top Management Commitment, Workforce Management, and Quality Performance of Malaysian HospitalsDocumento10 pagineAssessing Top Management Commitment, Workforce Management, and Quality Performance of Malaysian HospitalsWilmer UcedaNessuna valutazione finora
- Curriculum VitaDocumento2 pagineCurriculum VitaAjusshuwaNessuna valutazione finora
- CBAHI New StandardDocumento267 pagineCBAHI New StandardJack Patag100% (2)
- CSR Project in MCLDocumento77 pagineCSR Project in MCLChinmaya Meher100% (3)
- Formulary Book - Hajer (1) Final To Print1 MOH HospitalDocumento115 pagineFormulary Book - Hajer (1) Final To Print1 MOH HospitalspiderNessuna valutazione finora
- UPMC Children's Hospital of Pittsburgh Process Improvement Proposal.Documento14 pagineUPMC Children's Hospital of Pittsburgh Process Improvement Proposal.lindsey02grayNessuna valutazione finora
- QLM Insurance BenefitsDocumento13 pagineQLM Insurance BenefitsJasmin RacaNessuna valutazione finora
- Ghop 2013Documento65 pagineGhop 2013petal80Nessuna valutazione finora
- Health Report 1Documento106 pagineHealth Report 1Senthil KumarNessuna valutazione finora