Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Pharmacology Midterm Study Guide
Caricato da
bkearnest0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
848 visualizzazioni17 paginestudy guide for pharm
Copyright
© © All Rights Reserved
Formati disponibili
DOCX, PDF, TXT o leggi online da Scribd
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentostudy guide for pharm
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato DOCX, PDF, TXT o leggi online su Scribd
0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
848 visualizzazioni17 paginePharmacology Midterm Study Guide
Caricato da
bkearneststudy guide for pharm
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato DOCX, PDF, TXT o leggi online su Scribd
Sei sulla pagina 1di 17
Immaculata University Division of Nursing
NUR 301, Nancy Barker
Pharmacology Midterm Exam Study Guide
Thursday June 6
th
; Covers Classes 1 through 6
1
Pharmacology Term Definition
Absorption The uptake of substance by a tissue, such as nutrients, though the
wall of the gastrointestinal tract. Influenced by liver and kidneys.
Active transport The movement of ions or molecules across a cellular membrane
from a lower to a higher concentration, requiring the consumption
of energy. Diffusion high to low (passive transport)
Additive Interactions Two medications with similar therapeutic actions are given together
and a combined response occurs.
Agonist A drug or other chemical that can combine with a receptor on a cell
to produce a physiologic reaction typical of a naturally occurring
substance. Works with
Antagonist A drug that counteracts the effect of another drug. Works against
Antagonistic
Interactions
A second drug decreases the effect or cancels the effect of the first
drug
Bioavailability The fraction of the administered dose that reaches systemic
circulation.
Tablet disintegration time, enteric coatings, and sustained release
formulations can alter.
Oral narrow therapeutic range = concern
Biotransformation The series of chemical changes occurring in a compound, especially
a drug, as a result of enzymatic or other activity by a living organism.
Metabolism liver
Clearance A measure of how well a patient can metabolize or eliminate a drug
per unit of time.
Creatinine clearance A measure of the kidneys ability to eliminate creatinine from the
body.
Monitor BUN and creatinine levels
Diffusion The process by which molecules spread from areas of high
concentration, to areas of low concentration without the use of
energy.
Passive transport
Effective dose (ED50) The dose required to produce a specific therapeutic response in 50%
of the patients.
First-pass effect The resulting decrease in drug concentration in the blood or plasma
following absorption from the gastrointestinal tract before reaching
the systemic circulation.
Occurs when medication is given orally!
Glomerular Filtration
Rate (GFR)
The volume of water filtered out of the plasma through glomerular
capillary walls into Bowmans capsule per unit of time.
Immaculata University Division of Nursing
NUR 301, Nancy Barker
Pharmacology Midterm Exam Study Guide
Thursday June 6
th
; Covers Classes 1 through 6
2
Half-life The time required for the plasma concentration to be reduced to
one-half the original value.
Time for 50% of drug to be eliminated by the body
Incompatibility Usually involves parental drugs, occurs when two drugs and mixed in
solution and cause a reaction such as the formation of precipitate,
color change, or temperature change.
Lethal dose (LD50) A dose that will produce a lethal toxicity in 50% of studied group.
Data obtained from TD50.
Osmosis The tendency of a fluid, usually water, to pass through a
semipermeable membrane into a solution where the solvent
concentration is higher, thus equalizing the concentrations of
materials on either side of the membrane.
Partial agonist A drug that produces a weaker or less efficient response than an
agonist.
Passive transport Diffusion
Peak plasma level Highest plasma level of a specific drug at a specific time.
Trough
Pinocytosis The uptake of fluid and dissolved substances by a cell by
invagination and pinching off of the cell membrane
Receptor A molecular structure or site on the surface or interior of a cell that
binds with substances, such as hormones, antigens, drugs, or
neurotransmitters.
Steady state Rate of drug administration is equal to the rate of drug elimination.
Drug reaches a therapeutic level
Maintain regular dosing intervals to reach
Synergistic Interactions When the effect of two drugs given together is greater than the
expected combined effect.
Toxicity dose (TD50) A dose that will produce a given toxicity in 50% of the studied group.
Therapeutic class A group of drugs with similar mechanism of actions that treat the
same disease state.
Therapeutic index The ratio of the drugs LD50 to its ED50 and measures drug safety
margins.
LD50 = lethal dose
ED50 = effective dose
Trough plasma level The lowest plasma level of a specific drug at a particular time.
Peak
Volume of distribution The apparent volume required to account for the entire drug in the
body in the same concentration as in the sample from the plasma.
Immaculata University Division of Nursing
NUR 301, Nancy Barker
Pharmacology Midterm Exam Study Guide
Thursday June 6
th
; Covers Classes 1 through 6
3
Class #1
Pharmacology
o Draws on information from multiple disciplines
o The study of drugs and their interactions with living systems
Drug
o Any chemical that can affect living processes
o Virtually all chemicals can be considered drugs
o Focus primarily on drugs that have therapeutic applications
Clinical pharmacology
o Study of drugs in humans
o Includes the study of drugs in patients as well as healthy volunteers
(during new drug development)
o Encompasses all aspects of the interaction between drugs and people
primary interest is the use of drug to treat patients
Therapeutics (aka pharmacotherapeutics)
o The use of drugs to diagnose, prevent, or treat disease (or to prevent
pregnancy); medical use of drugs
o Effects of drugs can be either therapeutic or adverse
o Principal concern
Pharmacotherapeutics
o The use of drugs to treat disease
o Take into consideration the condition as well as the drugs effectiveness
o Factors that affect patient response: age, diet, disease, drug interactions,
gender, GI function, liver function, and renal function
o KIDNEY AND LIVER FUNCTION!!
Type of Therapy (6 types)
o 1) Acute: Patients is critically ill and requires active but short-term
therapy
o 2) Empiric: Based on practical experience rather than pure scientific data
Patient presents to emergency room with signs and symptoms of
infection, start antibiotics before testing
Off-label prescribing: using a drug for something other than what
it has been indicated for
Anti-depressants for neuro-pain
o 3) Maintenance: For chronic type conditions such as asthma or diabetes,
take drugs for years related to disease process
o 4) Supplemental: Replenish missing substances in the body such as
hormone replacement therapy.
Example: Post-menopausal women estrogen therapy
Immaculata University Division of Nursing
NUR 301, Nancy Barker
Pharmacology Midterm Exam Study Guide
Thursday June 6
th
; Covers Classes 1 through 6
4
o 5) Supportive: Doesnt treat the cause of the disease but maintains other
threatened body systems until patients condition(s) resolves.
Example: Give insulin to patients on steroids if blood sugars go
high
Doesn't treat disease, treats symptoms!
o 6) Palliative: comfort care, control pain!
To provide comfort to the patient
Goal of HOSPICE CARE!
The Therapeutic Objective
o The objective of drug therapy is to provide maximum benefit with
minimum harm!
o Drugs are not ideal we must exercise skill and care if treatment is to
result in more good than harm
o Nurse has critical role in achieving this; in order to meet this
responsibility, nurse must understand drugs and their effects
(pharmacology)
Pharmacodynamics
o Impact of drugs on the body
o Once a drug reaches site of action, these processes determine the nature
and intensity of the response
o Steps Leading to a Response:
1) Drug-Receptor Interaction
2) Patients functional state (tolerance)
3) Placebo (psychological) effects
Factors that determine the intensity of a drug response:
Prescribed dose administered dose concentration at sites of action
intensity of responses
o 1) Administration
Medication errors
Patient adherence
o 2) Pharmacokinetics
Absorption, distribution, metabolism, excretion (ADME!)
*Sources of Individual Variation
* Physiologic variables
* Pathologic variables
* Genetic variables
* Drug interactions
o 3) Pharmacodynamics
Drug-receptor interaction
Patients functional state
Immaculata University Division of Nursing
NUR 301, Nancy Barker
Pharmacology Midterm Exam Study Guide
Thursday June 6
th
; Covers Classes 1 through 6
5
Placebo effects
Important Properties of Medications = BIG 3
o 1) Effectiveness: does what it is supposed to do
Effective drug: One that elicits the responses for which it is given
Most important property a drug can have
Current US law requires that all new drugs be proven effective
prior to release for marketing
o 2) Safety: does not produce harmful effects
Safe drug: one that cannot produce harmful effects even if
administered in very high does and for a very long time
No such thing all drugs have ability to cause injury, especially
with high doses and prolonged use
Chances of producing adverse effects can be reduced by proper
drug selection and proper dosing can never be eliminated
Pharmakon = (Greek poison)
o 3) Selectivity: elicits response intended
Selective drug: one that elicits only the response for which it is
given; a selective drug would not produce side effects!
No such thing all drugs/medications produce/cause side effects
Most common side effect = nausea
Adverse v. harmful
Choose least invasive option with least amount of side
effects
Six Rights of Medication Administration
o 1) Right Patient
o 2) Right Dose
o 3) Right Drug
o 4) Right Route
o 5) Right Time
o 6) Right Documentation
Pre-administration Assessment All drug therapy begins with assessment of the
patient
o 3 Basic Goals: 1) Collecting base line data needed to evaluate therapeutic
and adverse responses, 2) Identifying high-risk patients, 3) Assessing the
patients capacity for self-care
1&2 Highly specific for each drug, must understand pharmacology
3 Applies generally to all drugs
o Baseline data
Immaculata University Division of Nursing
NUR 301, Nancy Barker
Pharmacology Midterm Exam Study Guide
Thursday June 6
th
; Covers Classes 1 through 6
6
Includes: HR, blood sugar, BP, culture results (Don't give abx
without), allergies (Penicillin most common), liver/kidney
dysfunction (adjust dose)
Needed to evaluate drugs responses, both therapeutic and
adverse
Must first know the effects that our drug is likely to produce
o Identifying High-Risk Patients
Important predisposing factors to adverse reactions from drugs:
pathophysiology (especially liver and kidney impairment), genetic
factors, drug allergies, pregnancy, pregnancy, old age, and
extreme youth
Penicillin allergy Giving penicillin to these people can kill
them!
When planning drug therapy, we must identify patients who are
high-risk for reacting adversely
3 principal tools Patient history, physical examination,
laboratory data
Dosage and Administration
o Consider:
Why you are giving the drug (Certain drugs have more than one
indication, and dosage may differ depending on which indication
the drug is used for)
Aspirin low dose for cardiac issues
Aspirin high does for inflammation
What Route? IV, IM, subcut, PO, PR, gtts, via NGT
Many drugs can be administered by more than one route
and dosage may differ depending upon the route
Morphine: PO vs. injected
o ORAL doses are generally much larger than
INJECTED doses
Routes of Drug Administration (REVIEW!)
Classification:
1) Enteral route
Oral (PO), sublingual (SL), buccal, per rectum (PR)
2) Parenteral route
4 major sites of injection: 1) Intradermal (ID), 2)
subcutaneous (SQ, SC, subcut), 3) Intramuscular (IM), 4)
Intravenous (IV)
OTHERS: epidural, intrathecal, intraosseous,
intraperitoneal, intrapleural, intraarterial
Immaculata University Division of Nursing
NUR 301, Nancy Barker
Pharmacology Midterm Exam Study Guide
Thursday June 6
th
; Covers Classes 1 through 6
7
3) Inhalation
o NGT = nasogastric tube
o Nurses can administer inhaled medications through
nasal and oral passages or through endotracheal or
tracheostomy tubes
4) Topical
Skin, transdermal, mucous membranes
VERIFY!
o Nurse is held responsible/accountable!
If you are unsure as to the order, CLARIFY!
Check ID band/scan
Verify dose
If it doesn't make sense, then don't give it
Generic, Chemical, or Trade
o Generic: nonproprietary name or US Adopted Name; more complex than
trade names, less complex than chemical, preferable to trade names,
each drug only has ONE!
o Chemical: description of a drug using the nomenclature of chemistry,
chemical makeup of medication; long and complex, inappropriate for
everyday use; will NEVER see on doctors order!
o Trade: proprietary name or brand name; the names under which a drug is
marketed; created by drug companies with the intention that they be
easy for nurses, physicians, pharmacists, and consumers to
recall/pronounce; PROBLEM = TOO MANY NAMES FOR SAME DRUG!;
must be approved by FDA no two trade names too similar, cannot be
named to imply unlikely efficacy
Pharmacokinetics
o Absorption of the drug as it moves through the body
Kinetics refers to movement
4 basic pharmacokinetic processes = Absorption, Distribution,
Metabolism, Excretion (ADME); determine the concentration of a
drug at its sites of action
Metabolism + Excretion = Elimination
1) ABSORPTION
o Absorbed taken into the body
o The movement of a drug from its site of
administration into the blood.
o Passive transport needs no cellular energy, goes
from an area of higher concentration to an area of
lower concentration (diffusion)
Immaculata University Division of Nursing
NUR 301, Nancy Barker
Pharmacology Midterm Exam Study Guide
Thursday June 6
th
; Covers Classes 1 through 6
8
o Active transport requires cellular energy to move
the drug (low to high)
o Pinocytosis a cell engulfs a drug particle
Rate of Absorption
o Rate of Absorption determines how soon effects will begin; the amount of
absorption helps determine how intense effects will be.
o The rate at which a drug undergoes absorption is influenced by the
physical and chemical properties of the drug itself and by physiologic and
anatomic factors at the site of absorption
o Fast and furious
IV, SL, or inhalation
Few cells separate the active drug from circulation
o Slow but steady
Oral, IM, or subcut.
Complex membrane systems of GI mucosal layers, muscles, and
skin delay
o Mouth (oral) v. IV doses doses bigger by mouth
o Factors to consider!
First past effect oral
Rate of dissolution, surface area, blood flow, lipid solubility, pH
partitioning
2) Distribution
o Distributed moves into various tissues
o The movement of drugs throughout the body
o Drug distribution is determined by 3 major factors:
1) Blood flow to tissues.
2) The ability of a drug to exit the vascular
system; Typical capillary beds The Blood-
Brain Barrier Placental Drug Transfer
Protein Binding
3) To a lesser extent, the ability of a drug to
enter cells
3) Metabolism (biotransformation)
o Metabolized changed into form that can be
excreted
o The enzymatic alteration of drug structure; most
drug metabolism takes place in the LIVER!
o METABOLISM LIVER!
Things that affect metabolism
o Very young and very old
Immaculata University Division of Nursing
NUR 301, Nancy Barker
Pharmacology Midterm Exam Study Guide
Thursday June 6
th
; Covers Classes 1 through 6
9
Very young immature livers
Very old decline in liver size and blood
flow, function; decreased enzyme
production decrease in metabolism
4) Excretion
o Excreted removed from the body
o The removal of drugs from the body
o Drugs and their metabolities can exit the body in:
urine, bile, sweat, saliva, breast milk, & expired air
o The most important organ for excretion of drugs Is
the KIDNEYS!
o EXCRETION KIDNEYS!
When kidneys are healthy, they serve to
limit the duration of action of many drugs.
Conversely, if renal failure occurs, both the
duration and intensity of drug responses
may increase.
Half-Life: time required for the amount of drug in the body to be decreased by
50% (eliminated); regular dosing intervals = steady state (rate of administration =
rate of excretion)
Onset, peak, duration
o Onset: starts with administration and ends when the therapeutic effect
begins
o Peak: drug concentration rises
o Duration: length of time the drug produces therapeutic effect
Adverse Drug Reactions (ADRs) (also known as adverse drug events (ADEs))
o Any noxious, unintended, and undesired effect that occurs at normal drug
doses (WHO); excludes undesired effects that occur when dose is
excessive (accidental poisoning or medication error)
o Can range in intensity from annoying to life-threatening
o When drugs are used properly, many ADRs can be avoided or at least
minimized.
Common or Serious Adverse Drug Effects
o Can patient tolerate medication without too many adverse effects?
o Adverse effect = undesired response to a drug
CNS, GI, hematologic, hepatic, nephrotoxicity
o Idiosyncratic effect = abnormal/odd/unexpected/uncommon (genetic)
effect of a drug; some decrease over time, some go away
o Hypersensitivity = allergic reaction (Penicillin most common allergy)
Anaphylaxis = life-threatening allergic reaction
Immaculata University Division of Nursing
NUR 301, Nancy Barker
Pharmacology Midterm Exam Study Guide
Thursday June 6
th
; Covers Classes 1 through 6
10
o Toxicity = overdose, one large dose or many small doses over time
Signs and symptoms of liver toxicity: jaundice, dark urine, light-
colored stools, nausea, vomiting, malaise, abdominal discomfort,
loss of appetite
o Mild severe can involve any body system
Adverse drug effects
o Dependence withdrawal effects
o Carcinogenicity (cancer related): refers to the ability of certain
medications and environmental chemicals to cause cancers
o Teratogenicity: drug-induced birth defect; pregnant women or women
who may become pregnant must be very careful
o Black Box Warnings
Highest FDA warning for adverse effects
Significant effect happens relatively frequently
Variables affecting drug action
o Dose/Route
IV, rapid response, most effective
o Drug-drug interactions (or effect)
Increased drug effects
Additive effects:
Synergism/potentiation
Interference
Displacement
Decreased drug effects
Antidote
o Narcan biggest antidote given!
o Drug-diet interactions
Tetracycline: Don't take with dairy; be careful with certain abx &
Grape juice liver/enzyme function
o Pt. related variables
o Tolerance
ANS Drugs
Antibiotics
Class #4
Antiepileptic Drugs (AEDs) prevent seizure
o Think of a seizure as a power surge in the brain
Immaculata University Division of Nursing
NUR 301, Nancy Barker
Pharmacology Midterm Exam Study Guide
Thursday June 6
th
; Covers Classes 1 through 6
11
o Goal of medications is to help brain cells to exercise control, adjust
excitability
o Think of AEDs as a surge protector that prevents sudden bursts of
activity before it can damage
Epilepsy: neurological condition; involves repeated seizures without warning
o Symptoms range from brief staring to unconsciousness with convulsions
o Diagnosed through abnormal wave forms on EEG
Types:
o Gran mal/generalized seizures most common
o Tonic clonic:
Characterized by
Initial rigid posture
Rhythmic and symmetrical jerking movements
Apnea (brief, momentary; stop breathing)
o Absence: blank stare; blinking/Lights on but nobodys home
o Myoclonic: pronounced jerking of muscles or group of muscles, can cause
collapse
o Akinetic: seizures without movement
o Hypermovement: fast and furious moving
Function of AEDs (Anti-Epileptic Drugs): inhibit neurons from firing and stop
excitability of neuron
o Hydantoins; most widely used is Dilantin
Block sodium channels
10 20 mcg/mL (therapeutic serum level)
Above therapeutic level can lead to the following adverse side
effects:
ataxia (staggered gait)
blurred vision
CNS depression sedation
Gingival hyperplasia inflamed, reddened gums
Stick with it:
If taking generic, stay with generic
If taking brand name, stay with brand name
Switching back and forth can cause unforeseen/additional
adverse side effects
Purple Glove Syndrome
Increased severe pain; rare
Stop Dilantin immediately
Stephen Johnson Syndrome
Immaculata University Division of Nursing
NUR 301, Nancy Barker
Pharmacology Midterm Exam Study Guide
Thursday June 6
th
; Covers Classes 1 through 6
12
First appears as rash, severity increases, eventually looks
like a burn
Can be fatal
Commonly seen, unknown cause
Multiple drugs cause
Treated like burn patient
Dilantin stopped
Dilantin
100 mg 3xdaily to maintain therapeutic level
Coumadin (Warfarin)/oral contraceptives effectiveness
o Coumadin: Helps to prevent new blood clots from
forming, and helps to keep existing blood clots
from getting worse. This medicine is a blood
thinner (anticoagulant). Prevent heart
attack/stroke.
Valium, alcohol effects
o Warning/Disclaimer: avoid alcohol while on AEDs
due to CNS depression effect
Not used with pregnancy; highly teratogenic (causing drug-
induced birth effects) pregnant women with epilepsy
need to be extremely careful
Given PO, IV push (very slowly at rate of 50 mg per min;
too fast can lead to cardiac collapse)
Oftentimes used in conjunction with benzodiazepines and
other medications
Zarontin
Drowsiness most common side effect
500 mg/day, increased until seizures controlled
Drug with fewest side effects
Lamictal
Newer drug, broad spectrum
Used in combination
Various types of seizures
Stephen Johnson Syndrome = potentially life-threatening
skin rashes
Given PO
Side effects: dizziness, double vision, nausea, vomiting
Keppra
Used to control partial seizures
Immaculata University Division of Nursing
NUR 301, Nancy Barker
Pharmacology Midterm Exam Study Guide
Thursday June 6
th
; Covers Classes 1 through 6
13
Fast-acting
No liver impairment
Useful in combination
Action unknown
Common adverse effects: drowsiness, agitation, anxiety
No changes in cognitive functions, not as much CNS
depression, mental slowness
Trileptal
Newer AED, used for partial seizures
Renal impairment, decreased renal function lower dose
Block sodium channels
Can lead to dizziness, drowsiness, double vision, nausea
Avoid driving/limit activity until you know the medications
effect on you
Risk of serious hypersensitivity (allergic reaction)
o Multi-organ reaction: fever, rash,
hepatitis/nephritis (indicating kidney/liver
dysfunction)
o Stop immediately!
Assess kidney function monitor BUN and creatinine
sodium levels monitor
Expensive, linked with Stephen Johnson Syndrome
effect oral contraceptives
Dilantin levels
o decrease dose of Dilantin if used in combination
with Trileptal
o monitor carefully dosing/levels
Luminal
Oldest AED
Barbituate
GABA Amount of transmissions sent out
Given IV, IM, PO
Schedule IV drug, dependency
Long half-life, Given 1 time/day
Can cause CNS depression, lethargy, drowsiness,
depression, learning disability
Don't stop abruptly, wean off
Topamax
Conjunctive medication
Immaculata University Division of Nursing
NUR 301, Nancy Barker
Pharmacology Midterm Exam Study Guide
Thursday June 6
th
; Covers Classes 1 through 6
14
Broad spectrum does it all
sweating careful of body temperature, monitor for
potential of overheating
Valproic Acid
Don't use during pregnancy
Also used to treat migraine headache/bipolar disorder
First line drug
Most widely prescribed
Dilantin, watch therapeutic levels
Dont use with impaired liver function
Forms: syrup, injection
o Drug Selection
Most bang for your buck with leas amount of side effects In
other words, best control of seizures with least amount of adverse
effects
Select based on seizure type
Single drug therapy (monotherapy) preferred when possible
AEDs & Pregnancy risk
Not many AEDs safe to be used with pregnant women
Depends on seizure activity whether woman can go off
medication or titrate to lower dose
Ethical question = Mom v. fetus life?
o Nursing
Seizure history
Seizure type
Liver and renal function
Serum drug levels
Med alert ID Epilepsy
Don't abruptly stop medications
Dilantin only mixed with saline
o GABA also connected with bipolar disorder
Drugs for Parkinsons Disease
o Parkinsons disease
Degeneration of area of brain for muscle movement
Dopamine versus Acetylcholine neurotransmitter imbalance
Characterized by:
Slowness in movement
Rigidity
Balance problems
Immaculata University Division of Nursing
NUR 301, Nancy Barker
Pharmacology Midterm Exam Study Guide
Thursday June 6
th
; Covers Classes 1 through 6
15
Specific in cause!
Parkinsons shuffle = distinct gait
Blank affect (display of emotion/facial expression)
Inability for neurotransmission of dopamine
Uncontrolled movement
Affects nearly 1 million Americans; 2
nd
only to Alzheimers as most
common neurodegenerative disease
PROGRESSIVE DISORDER: No cure, goal of drug therapy =
management of symptoms
Dopamine/Ach imbalance in brain
GABA CNS depression
Therapeutic Goals
Restore to highest level of function
Maintain independence for as long as possible
o Drug Therapy
2 categories of drugs
1) Dopaminergic mimics dopamine
2) Anticholinergic
All drugs used to treat directly related to DOPAMINE!
Levadopa
Drug holidays take a break
Converts to dopamine
Dyskinesia: dysfunction of movement, motor dysfunction,
hinder function severely
Wearing off response of Levadopa = on-off effect
Cross BBB converts to dopamine hits dopamine
receptor
Postural hypotension
o Increase sodium and fluid intake to help
manage/prevent
Side effects: head bobbing, tics, nausea, vomiting,
psychosis
Carbidopa
Not effective by itself, has no adverse effects of its own
Only used in combination with Levadopa
Levadopa/Carbidopa
Most effective combination for treatment
For 75% of patients a reduction in 50% of symptoms
Most effective is still only half effective!
Immaculata University Division of Nursing
NUR 301, Nancy Barker
Pharmacology Midterm Exam Study Guide
Thursday June 6
th
; Covers Classes 1 through 6
16
Increased levels of Levadopa with use of Carbidopa
More effective/same effect with lower dose of LD
Helps absorption
Dopamine agonists
2 types:
o Ergot: found in plants
o Non-ergot: synthetic
Most common = Mirapex (Noergot), also
used for restless leg syndrome
Used by themselves in early stages, conjunctive later on
(Levadopa) as disease progresses
Side Effects: nausea, vomiting, drowsiness, daytime
sleepiness, impulse control disorders (ICD) = linked to
function of dopamine
COMT Inhibitors
Inhibit LD metabolism
Given in conjunction
Entacapone (used only with LD) safer/more effective
o Prolongs half-life of LD in blood
Tolcapone
No direct therapeutic effects of their own, but can cause
dyskinesia & ICDs with long-term use
Non-motor symptoms and their management
Affects 90% of patients
Includes: Depression, ANS disturbances, dementia,
psychosis
Amitriptyline only effective drug against depression
Drugs for the Eye
o Glaucoma visual field loss, leading cause of preventable blindness in US
o Forms:
1) Primary Open-Angle Glaucoma (POAG), most common
Progressive optic nerve damage (non-reversible) with
eventual impairment of vision
Elevation of intraocular pressure (IOP)
o Only modifiable risk factor (others include: African
American, family history, advancing age)
Chronic therapy: long-term treatment, life-long
o Drops (topical) most common form of treatment
o Surgical intervention
Immaculata University Division of Nursing
NUR 301, Nancy Barker
Pharmacology Midterm Exam Study Guide
Thursday June 6
th
; Covers Classes 1 through 6
17
o Drug therapy
Timolol (beta-blocker) most common
glaucoma drug
Warn patients drugs may sting
Cycloplegics paralyze ciliary muscles
Oftentimes used in surgeries
Light sensitive, troubled vision
o 2) Acute Angle-Closure Glaucoma
Age-related Macular Degeneration (ARMD)
o Painless, blurs central vision/limits perception of
fine detail
o 2 forms (dry & wet)
o Leading cause of blindness in older Americans
o Progressive disorder stop or slow but not cure!
Drugs for Ear
o Otitis media filled with fluid, red inflamed middle ear
Viral v. bacterial?
Amoxicillin mot common/preferred drug
Tubes prevention of fluid build up in ear, drainage, help to
prevent recurring infection, common in childhood
o Otitis externa = swimmers ear
Oral/topical treatment
Rules for prevention:
Keep ears dry!
Nothing smaller than elbow in ear! even swabs! Don't
remove earwax
Potrebbero piacerti anche
- Nursing Pharmacology COMPLETEDocumento40 pagineNursing Pharmacology COMPLETEMonique Leonardo100% (8)
- PharmacologyDocumento21 paginePharmacologyMaridel Estioco100% (3)
- CHAPTER 1 PharmacologyDocumento21 pagineCHAPTER 1 PharmacologyGia Espinosa OcbeñaNessuna valutazione finora
- Drug Outline: Autonomic Nervous System Drug Class Drug OtherDocumento4 pagineDrug Outline: Autonomic Nervous System Drug Class Drug OtherCess Lagera YbanezNessuna valutazione finora
- Nursing School Drug ChartDocumento13 pagineNursing School Drug ChartEve Lester100% (3)
- Pharmacology Drug ClassificationDocumento4 paginePharmacology Drug ClassificationjetdoctrzNessuna valutazione finora
- Pharm Drug Outline AdrDocumento1 paginaPharm Drug Outline AdrCess Lagera YbanezNessuna valutazione finora
- Pharmacology ReviewDocumento28 paginePharmacology ReviewKathy Wollschleger100% (1)
- Pharmacology Reviewer #01Documento21 paginePharmacology Reviewer #01Cutie Patootie100% (1)
- Nursing MnemonicsDocumento8 pagineNursing Mnemonicsdeeday echavezNessuna valutazione finora
- Pharmacology LectureDocumento45 paginePharmacology LecturebjhilarioNessuna valutazione finora
- Pharmacology SummaryDocumento32 paginePharmacology Summaryminikatiting95% (22)
- Pharmacology Test 1Documento39 paginePharmacology Test 1Niki BolinNessuna valutazione finora
- Introduction To Pharmacology Cheat Sheet: by ViaDocumento2 pagineIntroduction To Pharmacology Cheat Sheet: by Viamamun31100% (1)
- Pharmacology SlidesDocumento114 paginePharmacology Slidesbrandon15000100% (9)
- Nursing PharmacologyDocumento22 pagineNursing PharmacologyDharren Rojan Garvida Agullana100% (2)
- Drugs WorksheetDocumento16 pagineDrugs Worksheetninja-2001Nessuna valutazione finora
- Nursing Pharmacology Inflammation Study GuideDocumento11 pagineNursing Pharmacology Inflammation Study GuideChelsea Smith100% (1)
- Antiinfectives Drug TableDocumento5 pagineAntiinfectives Drug Tablecdp1587100% (3)
- Test Bank For Pharmacology For Pharmacy Technicians 2nd Edition by MoscouDocumento5 pagineTest Bank For Pharmacology For Pharmacy Technicians 2nd Edition by Moscoua493312980100% (1)
- Pharmacology Study Notes - Adrenergic DrugsDocumento2 paginePharmacology Study Notes - Adrenergic Drugsstuckaluck83% (6)
- Learning Packet in Level 1-NCM 106 NURSING PHARMACOLOGY: College of Nursing School Year 2020-2021Documento15 pagineLearning Packet in Level 1-NCM 106 NURSING PHARMACOLOGY: College of Nursing School Year 2020-2021Nur Sanaani100% (1)
- Pharmacology: A ReviewDocumento26 paginePharmacology: A Reviewjava_biscocho122988% (8)
- PHARMACOLOGY Anti Microbial DrugsDocumento17 paginePHARMACOLOGY Anti Microbial DrugsLeilani Sablan100% (2)
- Pharmacology Nursing Mnemonics & Tips - NurseslabsDocumento19 paginePharmacology Nursing Mnemonics & Tips - Nurseslabsmaniz442100% (2)
- Pulmonary Drugs For Nursing PharmacologyDocumento1 paginaPulmonary Drugs For Nursing Pharmacologylhayes123475% (4)
- Nursing PharmacologyDocumento13 pagineNursing PharmacologyRikka Calnea Tabuzo100% (3)
- Pharmacology ChartDocumento6 paginePharmacology ChartPaula67% (3)
- Pharmacology Review For NursesDocumento11 paginePharmacology Review For Nursesisabel_avancena100% (4)
- Exam Cram Cheet SheetDocumento2 pagineExam Cram Cheet SheetSheila Stenson-Roberts100% (1)
- Nursing Lecture PharmacologyDocumento30 pagineNursing Lecture PharmacologyAedge010Nessuna valutazione finora
- Pharmacology Complete Drug TableDocumento6 paginePharmacology Complete Drug Tableninja-2001100% (4)
- m2 Pharmacology Handout 8-25-21Documento7 paginem2 Pharmacology Handout 8-25-21Sheila May SantosNessuna valutazione finora
- Pharmacology ListDocumento2 paginePharmacology ListSareeya Shre100% (1)
- OB Concept MapDocumento2 pagineOB Concept MapJennifer Lewis100% (1)
- Pharmacology Cheat Sheet - Generic Drug Stems - NurseslabsDocumento12 paginePharmacology Cheat Sheet - Generic Drug Stems - NurseslabsKc Mea Paran BorjaNessuna valutazione finora
- Clinical Med CardsDocumento26 pagineClinical Med CardsLila DanielsNessuna valutazione finora
- Pharmacology For Nursing Care 6th Edition Lehne Test BankDocumento2 paginePharmacology For Nursing Care 6th Edition Lehne Test BankStuartCarrsNessuna valutazione finora
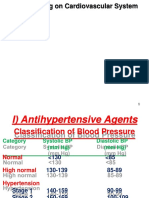
- Drugs Acting On Cardiovascular SystemDocumento18 pagineDrugs Acting On Cardiovascular SystemIbrahem AlNessuna valutazione finora
- Pharmocology Drug Cards: InnovarDocumento33 paginePharmocology Drug Cards: InnovarnamitaNessuna valutazione finora
- PHARMACOLOGY MNEMONICS - PPSXDocumento10 paginePHARMACOLOGY MNEMONICS - PPSXMartin Susanto, MD100% (1)
- Pharmacology Study Guide For NursingDocumento12 paginePharmacology Study Guide For Nursingmadison61404100% (7)
- Pharmacology - Git DrugsDocumento123 paginePharmacology - Git DrugsBenjamin Joel Breboneria75% (4)
- Med Surg Week 6Documento11 pagineMed Surg Week 6Eunice Cortés100% (1)
- 000 Nursing School Necessities Cheat SheetDocumento3 pagine000 Nursing School Necessities Cheat SheetRevNessuna valutazione finora
- PharmacologyDocumento10 paginePharmacologyPrince Mark Badillo100% (2)
- Group 3 Cardiovascular System Complete HandoutDocumento65 pagineGroup 3 Cardiovascular System Complete HandoutNicole LantinNessuna valutazione finora
- Med BundleDocumento36 pagineMed Bundlejamie sealNessuna valutazione finora
- Anti-Infectives and AntibioticsDocumento38 pagineAnti-Infectives and AntibioticsKarel Lu0% (1)
- Dimensional Analysis For Nursing StudentsDa EverandDimensional Analysis For Nursing StudentsNessuna valutazione finora
- Nursing Pharmacology Handouts For ZamboDocumento7 pagineNursing Pharmacology Handouts For ZamboAlexa Abidin Oldenborg100% (8)
- Maternal-Newborn Nursing DeMYSTiFieD: A Self-Teaching GuideDa EverandMaternal-Newborn Nursing DeMYSTiFieD: A Self-Teaching GuideNessuna valutazione finora
- PATHOPHYSIOLOGY: Passbooks Study GuideDa EverandPATHOPHYSIOLOGY: Passbooks Study GuideValutazione: 4.5 su 5 stelle4.5/5 (2)
- Pharmacology Prelims ReviewerDocumento2 paginePharmacology Prelims ReviewerAlthea Aubrey AgbayaniNessuna valutazione finora
- NSG 105 Module 1Documento10 pagineNSG 105 Module 1Alaminah MULOKNessuna valutazione finora
- General Pharmacology NotesDocumento76 pagineGeneral Pharmacology NotesXara Barretto Magadia100% (1)
- Fundamental Concepts of PharmacologyDocumento21 pagineFundamental Concepts of PharmacologyYean Delos ReyesNessuna valutazione finora
- Drug Chemical Name Generic Name Trade Name Drug Classification PharmaceuticsDocumento5 pagineDrug Chemical Name Generic Name Trade Name Drug Classification Pharmaceuticschubbygunny_29776413Nessuna valutazione finora
- IntroductionDocumento66 pagineIntroductionChamique Gelle Kerlin C LingayoNessuna valutazione finora
- Tugas Ujian Tengah SemesterDocumento5 pagineTugas Ujian Tengah SemesterMeta PratamaNessuna valutazione finora
- Peak Expiratory Flow RateDocumento35 paginePeak Expiratory Flow RateLiya RafeekhNessuna valutazione finora
- U7 Ef310matrix Fitt Pros JustinDocumento2 pagineU7 Ef310matrix Fitt Pros Justinapi-252246905Nessuna valutazione finora
- Pharma PrelimDocumento8 paginePharma PrelimNom NomNessuna valutazione finora
- Crash Cart Check ListDocumento2 pagineCrash Cart Check Listkim reyesNessuna valutazione finora
- HiperusemiaDocumento16 pagineHiperusemiasaleh nurazhariNessuna valutazione finora
- Leaflet Paraxyl CR Tablet RangeDocumento1 paginaLeaflet Paraxyl CR Tablet RangeAK GarmentsNessuna valutazione finora
- Exercise No. 1: Determination of Vital SignsDocumento6 pagineExercise No. 1: Determination of Vital SignsJohn smith AlbertoNessuna valutazione finora
- Finish Poster DM TMFDocumento1 paginaFinish Poster DM TMFpratika wardaniNessuna valutazione finora
- Ssi Rabu, 29 Juni 2022Documento49 pagineSsi Rabu, 29 Juni 2022Dhamar SetiaNessuna valutazione finora
- NSO Gastric LavageDocumento3 pagineNSO Gastric Lavagetry dokkNessuna valutazione finora
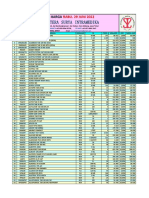
- Stock 21 Juni 2022Documento74 pagineStock 21 Juni 2022Akreditasi Rumah Sakit AndimasNessuna valutazione finora
- Anti Ulcer DrugsDocumento25 pagineAnti Ulcer DrugsPam LalaNessuna valutazione finora
- Medication Review PDFDocumento6 pagineMedication Review PDFRoselyn DawongNessuna valutazione finora
- NR 446 ATI Weekly Tips Week 2 PharmacologyDocumento9 pagineNR 446 ATI Weekly Tips Week 2 PharmacologyChristine Lansdown100% (1)
- Sample OutputDocumento110 pagineSample OutputMohana MuraliNessuna valutazione finora
- Drug Safety Associate Job Interview Questions and AnswersDocumento8 pagineDrug Safety Associate Job Interview Questions and AnswersGaurav Kumar100% (1)
- Laura Ang Resume 23Documento1 paginaLaura Ang Resume 23api-584560790Nessuna valutazione finora
- Concensus For Treatment of SAA v1.7 - AppendixDocumento2 pagineConcensus For Treatment of SAA v1.7 - AppendixSabina-Gabriela MihaiNessuna valutazione finora
- NN Drip ObatDocumento7 pagineNN Drip ObatDioniivanNessuna valutazione finora
- Types of Drug Preparation (Credit To The Rightful Owner)Documento1 paginaTypes of Drug Preparation (Credit To The Rightful Owner)Keren Grace EspirituNessuna valutazione finora
- ParkinsonDocumento12 pagineParkinsonStephanie NieNessuna valutazione finora
- Aroskar PreranaDocumento2 pagineAroskar PreranaKetan VadorNessuna valutazione finora
- Pharm C Exam 10 Drug ListDocumento2 paginePharm C Exam 10 Drug ListVokdadaNessuna valutazione finora
- Medication AdministrationDocumento7 pagineMedication AdministrationMaria Mika Ella RetizaNessuna valutazione finora
- Big Can Be Beautiful, TIVA in The ObeseDocumento7 pagineBig Can Be Beautiful, TIVA in The ObeseHernán GiménezNessuna valutazione finora
- Fajar Ramadhan Burhan (N 101 12 033)Documento4 pagineFajar Ramadhan Burhan (N 101 12 033)ShofaajiNessuna valutazione finora
- Ucm 485112Documento1 paginaUcm 485112worawutNessuna valutazione finora
- Medication Instructions Prior To SurgeryDocumento11 pagineMedication Instructions Prior To Surgeryhohj100% (1)
- Nclexreviewset 2 Fall 09Documento3 pagineNclexreviewset 2 Fall 09Amanda Ashley ZahronNessuna valutazione finora