Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Neuro Questions
Caricato da
sarasmith1988Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Neuro Questions
Caricato da
sarasmith1988Copyright:
Formati disponibili
NEUROMUSCULAR DISORDERS
7. A patient with Guillain-Barr syndrome asks the nurse what has caused the disease. In
responding to the patient, the nurse explains that Guillain-Barr syndrome
a. results from an acute infection and inflammation of the peripheral nerves.
b. is due to an immune reaction that attacks the covering of the peripheral nerves.
c. is caused by destruction of the peripheral nerves after exposure to a viral infection.
d. results from degeneration of the peripheral nerve caused by viral attacks.
Correct Answer: B
8. A 24-year-old patient is hospitalized with the onset of Guillain-Barr syndrome. During
this phase of the patient's illness, the most essential assessment for the nurse to carry out is
a. monitoring the cardiac rhythm continuously.
b. determining the level of consciousness q2hr.
c. evaluating sensation and strength of the extremities.
d. performing constant evaluation of respiratory function.
Correct Answer: D
10. A patient who has numbness and weakness of both feet is hospitalized with Guillain-
Barr syndrome. The nurse will anticipate that collaborative interventions at this time will
include
a. intubation and mechanical ventilation.
b. insertion of a nasogastric (NG) feeding tube.
c. administration of methylprednisolone (Solu-Medrol).
d. IV infusion of immunoglobulin (Sandoglobulin).
Correct Answer: D
25. Which of these nursing actions for a patient with Guillain-Barr syndrome is most
appropriate for the nurse to delegate to an experienced nursing assistant?
a. Nasogastric tube feeding q4hr
b. Artificial tear administration q2hr
c. Assessment for bladder distension q2hr
d. Passive range of motion to extremities q8hr
Correct Answer: D
When caring for a patient who has Guillain-Barr syndrome, which assessment data
obtained by the nurse will require the most immediate action?
a. The patient complains of severe tingling pain in the feet.
b. The patient has continuous drooling of saliva.
c. The patient's blood pressure (BP) is 106/50 mm Hg.
d. The patient's quadriceps and triceps reflexes are absent.
Correct Answer: B
When teaching the patient with newly diagnosed multiple sclerosis (MS) about the
disease, the nurse explains that
a. MS is a congenitally acquired illness that causes progressive neurologic deterioration.
b. impulses travel too fast over nerves that have lost their myelin coat and cause
overstimulation of muscle fibers.
c. autoimmune processes cause gradual destruction of the myelin sheath of nerves in
the brain and spinal cord.
d. antibodies are produced against acetylcholine receptors at the synapse and result in
blocked muscle contraction.
Correct Answer: C
When obtaining a health history and physical assessment for a patient with possible
multiple sclerosis (MS), the nurse should
a. confirm patient information with family members.
b. ask about a recent history of temperature spikes.
c. question the patient about any leg weakness or spasm.
d. determine whether hypersexuality has caused problems.
Correct Answer: C
A 28-year-old woman has had multiple sclerosis (MS) for 3 years and wants to have
children before her disease worsens. When she asks about the risks associated with
pregnancy, the nurse explains that
a. MS is associated with a slightly increased risk for congenital defects.
b. symptoms of MS are likely to become worse during her pregnancy.
c. women with MS frequently have premature labor.
d. MS symptoms may be worse after the pregnancy.
Correct Answer: D
16. A patient with multiple sclerosis (MS) is to begin treatment with glatiramer acetate
(Copaxone). In planning the patient teaching necessary with the use of the drug, the
nurse recognizes that the patient will need to be taught
a. how to draw up and administer injections of the medication.
b. use of contraceptive methods other than oral contraceptives for birth control.
c. to plan laboratory monitoring of CBC, chemistries, and liver function every 3 months.
d. that the drug will control symptoms but has no effect on the progression of the
disease.
Correct Answer: A
17. When planning care for a patient with MS who has a nursing diagnosis of risk for
activity intolerance related to extremity weakness secondary to stress, the most
appropriate patient goal is
a. "The patient will express minimal stress level."
b. "Strength in arms and legs will be maintained."
c. "The patient will complete ADLs without fatigue."
d. "Intake of high-nutrition foods will be adequate."
Correct Answer: C
18. A patient with multiple sclerosis (MS) has a nursing diagnosis of urinary retention
related to sensorimotor deficits. An appropriate nursing intervention for this problem is to
a. decrease fluid intake in the evening.
b. teach the patient how to use the Cred method.
c. suggest the use of incontinence briefs for nighttime use only.
d. assist the patient to the commode every 2 hours during the day.
Correct Answer: B
19. The nurse identifies the nursing diagnosis of impaired physical mobility related to
bradykinesia for a patient with Parkinson's disease. To assist the patient to ambulate
safely, the nurse should
a. allow the patient to ambulate only with assistance.
b. instruct the patient to rock from side to side to initiate leg movement.
c. have the patient take small steps in a straight line directly in front of the feet.
d. teach the patient to keep the feet in contact with the floor and slide them forward.
Correct Answer: B
20. A patient who has been taking bromocriptine (Parlodel) and benztropine (Cogentin)
for Parkinson's disease is experiencing a worsening of symptoms. The nurse will anticipate
that patient may benefit from
a. complete drug withdrawal for a few weeks.
b. use of levodopa (L-dopa)-carbidopa (Sinemet).
c. withdrawal of anticholinergic therapy.
d. increasing the dose of bromocriptine.
Correct Answer: B
21. A patient with Parkinson's disease has decreased tongue mobility and an inability to
move the facial muscles. The nurse recognizes that these impairments commonly
contribute to the nursing diagnosis of
a. disuse syndrome related to loss of muscle control.
b. self-care deficit related to bradykinesia and rigidity.
c. impaired verbal communication related to difficulty articulating.
d. impaired oral mucous membranes related to inability to swallow.
Correct Answer: C
22. A patient has a new prescription for levodopa (L-dopa) to control symptoms of
Parkinson's disease. Which assessment data obtained by the nurse may indicate a need
for a decrease in the dose?
a. The patient has a chronic dry cough.
b. The patient has 4 loose stools in a day.
c. The patient develops a deep vein thrombosis.
d. The patient's blood pressure is 90/46 mm Hg.
Correct Answer: D
23. A patient with myasthenia gravis (MG) is admitted to the hospital with severe
weakness and acute respiratory insufficiency. The health care provider performs a
Tensilon test to distinguish between myasthenic crisis and cholinergic crisis. During the
test, it will be most important to monitor the patient's
a. pupillary size.
b. muscle strength.
c. respiratory function.
d. level of consciousness (LOC).
Correct Answer: C
24. When teaching a patient with myasthenia gravis (MG) about management of the
disease, the nurse advises the patient to
a. anticipate the need for weekly plasmapheresis treatments.
b. protect the extremities from injury due to poor sensory perception.
c. do frequent weight-bearing exercise to prevent muscle atrophy.
d. perform necessary physically demanding activities in the morning.
Correct Answer: D
25. A hospitalized patient with myasthenia gravis (MG) has a nursing diagnosis of
imbalanced nutrition: less than body requirements related to impaired swallowing. To
promote nutrition, the nurse suggests that before meals the patient should avoid
a. watching television.
b. talking on the phone.
c. typing on the computer.
d. ambulating in the halls.
Correct Answer: B
27. A patient with amyotrophic lateral sclerosis (ALS) is hospitalized with pneumonia.
Which nursing action will be included in the plan of care?
a. Observing for agitation and paranoia
b. Assisting the patient with active range of motion (ROM)
c. Using simple words and phrases to explain procedures
d. Administer muscle relaxants as needed for muscle spasms
Correct Answer: B
31. A patient is seen in the health clinic with symptoms of a stooped posture, shuffling
gait, and pill rolling-type tremor. The nurse will anticipate teaching the patient about
a. preparation for an MRI.
b. purpose of EEG testing.
c. antiparkinsonian drugs.
d. oral corticosteroids.
Correct Answer: C
SPINAL CORD INJURY/TBI
5. A patient has a lesion that affects lower motor neurons. During assessment of the
patient's lower extremities, the nurse expects to find
a. spasticity.
b. flaccidity.
c. hyperactive reflexes.
d. loss of sensation.
Answer: B
2. When interviewing an acutely confused patient with a head injury, which of these
questions will provide the most useful information?
a. "Have you ever been hospitalized for a neurologic problem?"
b. "Do you have any pain at the present time?"
c. "What have you had to eat in the last 24 hours?"
d. "Can you describe you usual pattern for coping with injury?"
Answer: B
9. When admitting a patient with acute confusion to the hospital, the nurse will interview
the patient about health problems and health history primarily to
a. determine the patient's motivation for self-care.
b. include the patient in health care decisions.
c. use the information given by the patient to guide care.
d. assess the patient's baseline cognitive abilities.
Answer: D
13. The following orders are received for a patient who is unconscious after a head injury
caused by an automobile accident. Which one should the nurse question?
a. Perform neurologic checks every 15 minutes.
b. Prepare the patient for lumbar puncture.
c. Obtain x-rays of the skull and spine.
d. Do computed tomography (CT) scan with and without contrast.
Answer: B
8. When obtaining a health history from a patient with a neurologic problem, which
question by the nurse will elicit the most useful response from the patient?
a. "Do you ever have any nausea or dizziness?"
b. "Does the pain radiate from your back into your legs?"
c. "Do you have any sensations of pins and needles in your feet?"
d. "Can you describe the sensations you are having in your chest?"
Answer: D
4. In a patient who has a corticospinal tract lesion, the nurse should assess for
a. extremity movement and strength.
b. cranial nerve function.
c. peripheral sensitivity to pain.
d. level of consciousness (LOC).
Answer: A
2. When admitting a patient who has a history of paraplegia as a result of a spinal cord
injury, the nurse will plan to
a. check the patient for urinary incontinence every 2 hours to maintain skin integrity.
b. assist the patient to the toilet on a scheduled basis to help ensure bladder emptying.
c. use intermittent catheterization on a regular schedule to avoid the risk of infection.
d. ask the patient about the usual urinary pattern and measures used for bladder control.
Answer: D
12. Neurologic testing of the patient by the nurse indicates impaired functioning of the
left glossopharyngeal nerve (CN IX) and the vagus nerve (CN X). Based on these findings,
the nurse plans to
a. insert an oral airway.
b. withhold oral fluid or foods.
c. provide highly seasoned foods.
d. apply artificial tears every hour.
Answer: B
11. To assess the functioning of the optic nerve (CN II), the nurse should
a. apply a cotton wisp strand to the cornea.
b. have the patient read a magazine.
c. shine a bright light into the patient's pupil.
d. check for equal opening of the eyelids.
Answer: B
13. The following orders are received for a patient who is unconscious after a head injury
caused by an automobile accident. Which one should the nurse question?
a. Perform neurologic checks every 15 minutes.
b. Prepare the patient for lumbar puncture.
c. Obtain x-rays of the skull and spine.
d. Do computed tomography (CT) scan with and without contrast.
Answer: B
14. The charge nurse is observing a new staff nurse who is assessing a patient with a
possible spinal cord lesion for sensation. Which action indicates a need for further
teaching about neurologic assessment?
a. The new nurse tests for light touch before testing for pain.
b. The new nurse has the patient close the eyes during testing.
c. The new nurse tells the patient, "You may feel a pinprick now."
d. The new nurse uses an irregular pattern to test for intact touch.
Answer: C
16. When reviewing the results of a patient's cerebrospinal fluid analysis, the nurse will
notify the health care provider about
a. pH of 7.35.
b. white blood cell count (WBC) of 4/ml (0.004/L).
c. protein 30 mg/dl (0.30 g/L).
d. glucose 30 mg/dl (1.7 mmol/L).
Answer: D
13. A patient with a neck fracture at the C5 level is admitted to the intensive care unit
(ICU) following initial treatment in the emergency room. During initial assessment of the
patient, the nurse recognizes the presence of spinal shock on finding
a. hypotension, bradycardia, and warm extremities.
b. involuntary, spastic movements of the arms and legs.
c. the presence of hyperactive reflex activity below the level of the injury.
d. flaccid paralysis and lack of sensation below the level of the injury.
Correct Answer: D
14. When caring for a patient who had a C8 spinal cord injury 10 days ago and has a
weak cough effort, bibasilar crackles, and decreased breath sounds, the initial
intervention by the nurse should be to
a. administer oxygen at 7 to 9 L/min with a face mask.
b. place the hands on the epigastric area and push upward when the patient coughs.
c. encourage the patient to use an incentive spirometer every 2 hours during the day.
d. suction the patient's oral and pharyngeal airway.
Correct Answer: B
15. As a result of a gunshot wound, a patient has an incomplete right spinal cord lesion
at the level of T7, resulting in Brown-Squard syndrome. Which nursing action should be
included in the plan of care?
a. Assessment of the patient for left leg pain
b. Assessment of the patient for left arm weakness
c. Positioning the patient's right leg when turning the patient
d. Teaching the patient to look at the left leg to verify its position
Correct Answer: C
16. A patient with a T1 spinal cord injury is admitted to the intensive care unit (ICU). The
nurse will teach the patient and family that
a. use of the shoulders will be preserved.
b. full function of the patient's arms will be retained.
c. total loss of respiratory function may occur temporarily.
d. elevations in heart rate are common with this type of injury.
Correct Answer: B
17. The health care provider orders administration of IV methylprednisolone (Solu-Medrol)
for the first 24 hours to a patient who experienced a spinal cord injury at the T10 level 3
hours ago. When evaluating the effectiveness of the medication the nurse will assess
a. blood pressure and heart rate.
b. respiratory effort and O2 saturation.
c. motor and sensory function of the legs.
d. bowel sounds and abdominal distension.
Correct Answer: C
18. A patient with a paraplegia resulting from a T10 spinal cord injury has a neurogenic
reflex bladder. When the nurse develops a plan of care for this problem, which nursing
action will be most appropriate?
a. Teaching the patient how to self-catheterize
b. Assisting the patient to the toilet q2-3hr
c. Use of the Cred method to empty the bladder
d. Catheterization for residual urine after voiding
Correct Answer: A
19. A patient with a history of a T2 spinal cord tells the nurse, "I feel awful today. My head
is throbbing, and I feel sick to my stomach." Which action should the nurse take first?
a. Notify the patient's health care provider.
b. Check the blood pressure (BP).
c. Give the ordered antiemetic.
d. Assess for a fecal impaction.
Correct Answer: B
Rationale: The BP should be assessed immediately in a patient with an injury at the T6
level or higher who complains of a headache to determine whether autonomic
dysreflexia is causing the symptoms, including hypertension. Notification of the patient's
health care provider is appropriate after the BP is obtained. Administration of an
antiemetic is indicated after autonomic dysreflexia is ruled out as the cause of the
nausea. The nurse may assess for a fecal impaction, but this should be done after
checking the BP and lidocaine jelly should be used to prevent further increases in the BP.
20. The nurse discusses long-range goals with a patient with a C6 spinal cord injury. An
appropriate patient outcome is
a. transfers independently to a wheelchair.
b. drives a car with powered hand controls.
c. turns and repositions self independently when in bed.
d. pushes a manual wheelchair on flat, smooth surfaces.
Correct Answer: D
21. A patient who sustained a T1 spinal cord injury a week ago refuses to discuss the injury
and becomes verbally abusive to the nurses and other staff. The patient demands to be
transferred to another hospital, where "they know what they are doing." The best
response by the nurse to the patient's behavior is to
a. ask for the patient's input into the plan for care.
b. clarify that abusive behavior will not be tolerated.
c. reassure the patient that the anger will pass and rehabilitation will then progress.
d. ignore the patient's anger and continue to perform needed assessments and care.
Correct Answer: A
22. A 26-year-old patient with a C8 spinal cord injury tells the nurse, "My wife and I have
always had a very active sex life, and I am worried that she may leave me if I cannot
function sexually." The most appropriate response by the nurse to the patient's comment
is to
a. advise the patient to talk to his wife to determine how she feels about his sexual
function.
b. tell the patient that sildenafil (Viagra) helps to decrease erectile dysfunction in
patients with spinal cord injury.
c. inform the patient that most patients with upper motor neuron injuries have reflex
erections.
d. suggest that the patient and his wife work with a nurse specially trained in sexual
counseling.
Correct Answer: D
23. A 25-year-old patient has returned home following extensive rehabilitation for a C8
spinal cord injury. The home care nurse visits and notices that the patient's spouse and
parents are performing many of the activities of daily living (ADLs) that the patient had
been managing during rehabilitation. The most appropriate action by the nurse at this
time is to
a. tell the family members that the patient can perform ADLs independently.
b. remind the patient about the importance of independence in daily activities.
c. recognize that it is important for the patient's family to be involved in the patient's care
and support their activities.
d. develop a plan to increase the patient's independence in consultation with the with
the patient, spouse, and parents.
Correct Answer: D
27. When caring for a patient who was admitted 24 hours previously with a C5 spinal
cord injury, which nursing action has the highest priority?
a. Continuous cardiac monitoring for bradycardia
b. Administration of methylprednisolone (Solu-Medrol) infusion
c. Assessment of respiratory rate and depth
d. Application of pneumatic compression devices to both legs
Correct Answer: C
SEIZURES
7. A patient has a tonic-clonic seizure while the nurse is in the patient's room. During the
seizure, it is important for the nurse to
a. insert an oral airway during the seizure to maintain a patent airway.
b. restrain the patient's arms and legs to prevent injury during the seizure.
c. avoid touching the patient to prevent further nervous system stimulation.
d. time and observe and record the details of the seizure and postictal state.
Correct Answer: D
Rationale: Because diagnosis and treatment of seizures frequently are based on the
description of the seizure, recording the length and details of the seizure is important.
Insertion of an oral airway and restraining the patient during the seizure are
contraindicated. The nurse may need to move the patient to decrease the risk of injury
during the seizure.
8. The nurse witnesses a patient with a seizure disorder as the patient suddenly jerks the
arms and legs, falls to the floor, and regains consciousness immediately. It will be most
important for the nurse to
a. document the timing and description of the seizure.
b. notify the patient's health care provider about the seizure.
c. give the scheduled dose of divalproex (Depakote).
d. assess the patient for a possible head injury.
Correct Answer: D
9. After experiencing a generalized tonic-clonic seizure in the classroom, an elementary
school teacher is evaluated and diagnosed with idiopathic epilepsy. The patient cries
and tells the nurse, "I can not teach anymore. It will be too difficult for the students if this
happens again at work." The most appropriate nursing diagnosis for the patient is
a. anxiety related to loss of control during seizures.
b. hopelessness related to diagnosis of chronic illness.
c. disturbed body image related to new diagnosis of a seizure disorder.
d. ineffective role performance related to misinformation about epilepsy.
Correct Answer: D
10. The health care provider prescribes phenytoin (Dilantin) for control of complex partial
seizures. After the nurse has taught the patient about phenytoin, which patient
statement indicates understanding of the medication?
a. "I should use soft swabs rather than a toothbrush to clean my mouth."
b. "After I have a seizure, I should call an ambulance to take me to the hospital."
c. "I may need to have my blood taken frequently to check the level of the Dilantin."
d. "I will take the medication at the beginning of the seizure when I experience an aura."
Correct Answer: C
11. When a patient experiences a generalized tonic-clonic seizure in the emergency
department after a head injury, all of the following orders are received. Which one will
the nurse implement first?
a. Send to radiology for computed tomography (CT) scan.
b. Administer midazolam (Versed).
c. Check capillary blood glucose.
d. Monitor level of consciousness (LOC).
Correct Answer: B
12. A patient found in a tonic-clonic seizure reports afterward that the seizure was
preceded by numbness and tingling of the arm. The nurse knows that this finding
indicates a(n) _____ seizure.
a. absence
b. simple partial
c. complex partial
d. generalized myoclonic
Correct Answer: C
STROKE
The nurse obtains all of the following information about a 65-year-old patient in the clinic.
When developing a plan to decrease stroke risk, which risk factor is most important for
the nurse to address?
a.
The patient smokes a pack of cigarettes daily.
b.
The patient's blood pressure (BP) is chronically between 150/80 to 170/90 mm Hg.
c.
The patient works at a desk and relaxes by watching television.
d.
The patient is 25 pounds above the ideal weight.
Correct Answer: B
Rationale: Hypertension is the most important modifiable risk factor. Smoking, physical
inactivity, and obesity all contribute to stroke risk but not so much as hypertension.
A patient with right-sided weakness that started 1 hour ago is admitted to the
emergency department and all these diagnostic tests are ordered. Which order should
the nurse act on first?
a.
Noncontrast computed tomography (CT) scan
b.
Chest radiograph
c.
Complete blood count (CBC)
d.
Electrocardiogram (ECG)
Correct Answer: A
Rationale: Rapid screening with a noncontrast CT scan is needed before administration
of tissue plasminogen activator (tPA), which must be given within 3 hours of the onset of
clinical manifestations of the stroke. The sooner the tPA is given, the smaller the area of
brain injury. The other diagnostic tests give information about possible causes of the
stroke and do not need to be completed as urgently as the CT scan.
The nurse expects that management of the patient who experiences a brief episode of
tinnitus, diplopia, and dysarthria with no residual effects will include
a.
heparin via continuous intravenous infusion.
b.
prophylactic clipping of cerebral aneurysms.
c.
therapy with tissue plasminogen activator (tPA).
d.
oral administration of ticlopidine (Ticlid).
Correct Answer: D
Rationale: The patient's symptoms are consistent with transient ischemic attack (TIA), and
drugs that inhibit platelet aggregation are prescribed after a TIA to prevent stroke.
Continuous heparin infusion is not routinely used after TIA or with acute ischemic stroke.
The patient's symptoms are not consistent with a cerebral aneurysm. tPA is used only for
acute ischemic stroke, but not for TIA.
Aspirin is ordered for a patient who is admitted with a possible stroke. Which information
obtained during the admission assessment indicates that the nurse should consult with
the health care provider before giving the aspirin?
a.
The patient has atrial fibrillation.
b.
The patient has dysphasia.
c.
The patient states, "I suddenly developed a terrible headache."
d.
The patient has a history of brief episodes of right hemiplegia.
Correct Answer: C
Rationale: A sudden-onset headache is typical of a subarachnoid hemorrhage, and
aspirin is contraindicated. Atrial fibrillation, dysphasia, and transient ischemic attack (TIA)
are not contraindications to aspirin use, so the nurse can administer the aspirin.
A patient with a stroke experiences right-sided arm and leg paralysis and facial drooping
on the right side. When obtaining admission assessment data about the patient's clinical
manifestations, it is most important the nurse assess the patient's
a.
ability to follow commands.
b.
visual fields.
c.
right-sided reflexes.
d.
emotional state.
Correct Answer: A
Rationale: Because the patient with a left-sided brain stroke may also have difficulty with
comprehension and use of language, so it is important to obtain baseline data about
the ability to follow commands. This will impact on patient safety and nursing care. The
visual fields are not typically affected by a left-sided stroke. Information about reflexes
and emotional state will be collected but is not as high a priority as information about
language abilities.
6. The nurse on the medical unit receives a verbal report from the emergency
department nurse that a patient has an occlusion of the left posterior cerebral artery.
When admitting the patient to the medical floor, the nurse will anticipate that the patient
may have
a.
visual deficits.
b.
dysphasia.
c.
confusion.
d.
poor judgment.
Correct Answer: A
Rationale: Visual disturbances are expected with posterior cerebral artery occlusion.
Aphasia occurs with middle cerebral artery involvement. Cognitive deficits and changes
in judgment are more typical of anterior cerebral artery occlusion.
The health care provider prescribes clopidogrel (Plavix) for a patient with cerebral
atherosclerosis. When teaching about the new medication, the nurse will tell the patient
a.
that Plavix will reduce cerebral artery plaque formation.
b.
to monitor and record the blood pressure daily.
c.
to call the health care provider if stools are tarry.
d.
that Plavix will dissolve clots in the cerebral arteries.
Correct Answer: C
Rationale: Plavix inhibits platelet function and increases the risk for gastrointestinal
bleeding, so patients should be advised to notify the health care provider about any
signs of bleeding. The medication does not lower blood pressure, decrease plaque
formation, or dissolve clots.
The health care provider recommends a carotid endarterectomy for a patient with
carotid atherosclerosis and a history of transient ischemic attacks (TIA). The patient asks
the nurse to describe the procedure. Which response by the nurse is appropriate?
a.
"The diseased portion of the artery in the brain is removed and replaced with a synthetic
graft."
b.
"The carotid endarterectomy involves surgical removal of plaque from an artery in the
neck."
c.
"A catheter with a deflated balloon is positioned at the narrow area, and the balloon is
inflated to flatten the plaque."
d.
"A wire is threaded through an artery in the leg to the clots in the carotid artery and the
clots are removed."
Correct Answer: B
Rationale: In a carotid endarterectomy, the carotid artery is incised and the plaque is
removed. The response beginning, "The diseased portion of the artery in the brain is
removed" describes an arterial graft procedure. The answer beginning, "A catheter with
a deflated balloon is positioned at the narrow area" describes an angioplasty. The final
response (beginning, "A wire is threaded through the artery") describes the Merci
procedure.
On initial assessment of a patient hospitalized following a stroke, the nurse finds the
patient's blood pressure to be 180/90 mm Hg. Which of the following orders by the health
care provider should the nurse question?
a.
Infuse normal saline at 75 ml/hr.
b.
Keep head of bed elevated at least 30 degrees.
c.
Administer tissue plasminogen activator (tPA) per protocol.
d.
Titrate labetolol (Normodyne) drip to keep BP less than 140/90 mm Hg.
Correct Answer: D
Rationale: Since elevated BP may be a protective response to maintain cerebral
perfusion, antihypertensive therapy is recommended only if MAP is >130 mm Hg or
systolic pressure is >220 mm Hg. Fluid intake should be 1500 to 2000 ml daily to maintain
cerebral blood flow. The head of the bed should be elevated to at least 30 degrees
unless the patient has symptoms of poor tissue perfusion. tPA may be administered if the
patient meets the other criteria for tPA use.
A patient with a history of several transient ischemic attacks (TIAs) arrives in the
emergency room with hemiparesis and dysarthria that started 2 hours previously. The
nurse anticipates the need to prepare the patient for
a.
intravenous heparin administration.
b.
transluminal angioplasty.
c.
surgical endarterectomy.
d.
tissue plasminogen activator (tPA) infusion.
Correct Answer: D
Rationale: The patient's history and clinical manifestations suggest an acute ischemic
stroke and a patient who is seen within 3 hours of stroke onset is likely to receive tPA (after
screening with a CT scan). Heparin administration in the emergency phase is not
indicated. Emergent carotid transluminal angioplasty or endarterectomy are not
indicated for the patient who is having an acute ischemic stroke.
The nurse identifies the nursing diagnosis of impaired verbal communication for a patient
with expressive aphasia. An appropriate nursing intervention to help the patient
communicate is to
a.
ask simple questions that the patient can answer with "yes" or "no."
b.
develop a list of words that the patient can read and practice reciting.
c.
have the patient practice facial and tongue exercises to improve motor control
necessary for speech.
d.
prevent embarrassing the patient by changing the subject if the patient does not
respond in a timely manner.
Correct Answer: A
Rationale: Communication will be facilitated and less frustrating to the patient when
questions that require a "yes" or "no" response are used. When the language areas of the
brain are injured, the patient might not be able to read or recite words, which will
frustrate the patient without improving communication. Expressive aphasia is caused by
damage to the language areas of the brain, not by the areas that control the motor
aspects of speech. The nurse should allow time for the patient to respond.
A patient with a stroke has progressive development of neurologic deficits with
increasing weakness and decreased level of consciousness (LOC). The priority nursing
diagnosis for the patient is
a.
risk for impaired skin integrity related to immobility.
b.
disturbed sensory perception related to brain injury.
c.
risk for aspiration related to inability to protect airway.
d.
impaired physical mobility related to weakness.
Correct Answer: C
Rationale: Protection of the airway is the priority of nursing care for a patient having an
acute stroke. The other diagnoses are also appropriate, but interventions to prevent
aspiration are the priority at this time.
A patient has a stroke affecting the right hemisphere of the brain. Based on knowledge
of the effects of right brain damage, the nurse establishes a nursing diagnosis of
a.
impaired physical mobility related to right hemiplegia.
b.
impaired verbal communication related to speech-language deficits.
c.
risk for injury related to denial of deficits and impulsiveness.
d.
ineffective coping related to depression and distress about disability.
Correct Answer: C
Rationale: Right-sided brain damage typically causes denial of any deficits and poor
impulse control, leading to risk for injury when the patient attempts activities such as
transferring from a bed to a chair. Right-sided brain damage causes left hemiplegia. Left-
sided brain damage typically causes language deficits. Left-sided brain damage is
associated with depression and distress about the disability.
14. A patient with homonymous hemianopsia resulting from a stroke has a nursing
diagnosis of disturbed sensory perception related to hemianopsia. To help the patient
learn to compensate for the deficit during the rehabilitation period, the nurse should
a.
apply an eye patch to the affected eye.
b.
approach the patient on the unaffected side.
c.
place objects necessary for activities of daily living on the patient's affected side.
d.
have the patient use the eye muscles to move the eyes through the entire visual field.
Correct Answer: C
Rationale: During the rehabilitation period, placing objects on the affected side will
encourage the patient to use the scanning technique to visualize the affected side.
Because homonymous hemianopsia affects half the visual field in each eye, use of an
eye patch is not appropriate. Approaching the patient on the affected side is
appropriate during the acute period but does not help the patient learn skills needed to
compensate for the visual defect. The problem is with the visual field, not with the eye
muscles, so practice moving the eyes through the visual field will not be effective.
A patient who has had a subarachnoid hemorrhage is being cared for in the intensive
care unit. Which information about the patient is most important to communicate to the
health care provider?
a.
The patient complains of an ongoing severe headache.
b.
The patient's blood pressure is 90/50 mm Hg.
c.
The cerebrospinal fluid (CFS) report shows red blood cells (RBCs).
d.
The patient complains about having a stiff neck.
Correct Answer: B
Rationale: To prevent cerebral vasospasm and maintain cerebral perfusion, blood
pressure needs to be maintained at a high level after a subarachnoid hemorrhage. A
low or drop in BP indicates a need to administer fluids and/or vasopressors to increase
the BP An ongoing headache, RBCs in the CSF, and a stiff neck are all typical clinical
manifestations of a subarachnoid hemorrhage and do not need to be rapidly
communicated to the health care provider.
The nurse identifies the nursing diagnosis of imbalanced nutrition: less than body
requirements related to inability to feed self for a patient with right-sided hemiplegia. An
appropriate nursing intervention is to
a.
assist the patient to eat with the left hand.
b.
provide oral care before and after meals.
c.
teach the patient the "chin-tuck" technique.
d.
provide a wide variety of food choices.
Correct Answer: A
Rationale: Because the nursing diagnosis indicates that the patient's imbalanced
nutrition is related to the right-sided hemiplegia, the appropriate interventions will focus
on teaching the patient to use the left hand for self-feeding. The other interventions are
appropriate for patients with other etiologies for the imbalanced nutrition.
17. The nurse is assisting the patient who is recovering from an acute stroke and has right-
side hemiplegia to transfer from the bed to the wheelchair. Which action by the nurse is
appropriate?
a.
Positioning the wheelchair next to the bed on the patient's right side
b.
Placing the wheelchair parallel to the bed on the patient's left side
c.
Setting the wheelchair directly in front of the patient, who is sitting on the side of the bed
d.
Moving the wheelchair a few steps from the bed and having the patient walk to the
chair
Correct Answer: B
Rationale: Placing the wheelchair on the patient's left side will allow the patient to use
the left hand to grasp the left arm of the chair to transfer. If the chair is placed on the
patient's right side or in front of the patient, it will be awkward to use the strong arm, and
the patient will be at increased risk for a fall. Because the patient has hemiplegia, it is not
appropriate to place the chair where the patient will need to walk to it.
A 32-year-old patient has a stroke resulting from a ruptured aneurysm and subarachnoid
hemorrhage. Which intervention will be included in the care plan?
a.
Encouraging patient to cough and deep breath every 4 hours
b.
Inserting an oropharyngeal airway to prevent airway obstruction
c.
Assisting to dangle on edge of bed and assess for dizziness
d.
Applying intermittent pneumatic compression stockings
Correct Answer: D
Rationale: The patient with a subarachnoid hemorrhage usually has minimal activity to
prevent cerebral vasospasm or further bleeding and is at risk for deep vein thrombosis
(DVT). Activities (such as coughing and sitting up) that might increase intracranial
pressure (ICP) or decrease cerebral blood flow are avoided. Because there is no
indication that the patient is unconscious, an oropharyngeal airway is inappropriate.
A patient who has had a stroke has a new order to attempt oral feedings. The nurse
should assess the gag reflex and then
a.
offer the patient a sip of juice.
b.
order a varied pureed diet.
c.
assess the patient's appetite.
d.
assist the patient into a chair.
Correct Answer: D
Rationale: The patient should be as upright as possible before attempting feeding to
make swallowing easier and decrease aspiration risk. To assess swallowing ability, the
nurse should initially offer water or ice to the patient. Pureed diets are not recommended
because the texture is too smooth. The patient may have a poor appetite, but the oral
feeding should be attempted regardless.
A patient has right-sided weakness and aphasia as a result of a stroke but is attempting
to use the left hand for feeding and other activities. The patient's wife insists on feeding
and dressing him, telling the nurse, "I just don't like to see him struggle." A nursing diagnosis
that is most appropriate in this situation is
a.
situational low self-esteem related to increasing dependence on others.
b.
interrupted family processes related to effects of illness of a family member.
c.
disabled family coping related to inadequate understanding by patient's spouse.
d.
ineffective therapeutic regimen management related to hemiplegia and aphasia.
Correct Answer: C
Rationale: The information supports the diagnosis of disabled family coping because the
wife does not understand the rehabilitation program. There are no data supporting low
self-esteem, and the patient is attempting independence. The data do not support an
interruption in family processes because this may be a typical pattern for the couple. The
patient's attempts to use the left hand indicate that he is managing the therapeutic
regimen appropriately.
Several weeks after a stroke, a patient has urinary incontinence resulting from an
impaired awareness of bladder fullness. A bladder retraining program for the patient
should include
a.
limiting fluid intake to 1000 ml daily to reduce urine volume.
b.
assisting the patient onto the bedside commode every 2 hours.
c.
performing intermittent catheterization after each voiding to check for residual urine.
d.
using an external "condom" catheter to protect the skin and prevent embarrassment.
Correct Answer: B
Rationale: Developing a regular voiding schedule will prevent incontinence and may
increase patient awareness of a full bladder. A 1000-ml fluid intake is too restricted and
will lead to dehydration. Intermittent catheterization and use of a condom catheter are
appropriate in the acute phase of stroke but should not be considered solutions for long-
term management because of the risks for urinary tract infection (UTI) and skin
breakdown.
A 72-year-old is being discharged home following a stroke. The patient is able to walk
with assistance but needs help with hygiene, dressing, and eating. Which statement by
the patient's wife indicates that discharge planning goals have been met?
a.
"I can provide the care my husband needs if I use the support and resources available in
the community."
b.
"Because my husband will have continuous improvement in his condition, I won't need
outside assistance in his care for very long."
c.
"I can handle all of my husband's needs thanks to the instructions you've given me."
d.
"I have arranged for a home health aide to provide all the care my husband will need."
Correct Answer: A
Rationale: The statement that community resources will be used indicates a realistic
outcome. The patient is unlikely to continue to improve to the point of needing no
assistance. The wife is likely to be overwhelmed by the patient's needs if she attempts to
manage without assistance. There is no indication that the patient will need a home
health aide to meet all of his care needs.
A patient who has a history of a transient ischemic attack (TIA) has an order for aspirin
160 mg daily. When the nurse is administering the medications, the patient says, "I don't
need the aspirin today. I don't have any aches or pains." Which action should the nurse
take?
a.
Document that the aspirin was refused by the patient.
b.
Call the health care provider to clarify the medication order.
c.
Explain that the aspirin is ordered to decrease stroke risk.
d.
Tell the patient that the aspirin is used to prevent aches.
Correct Answer: C
Rationale: Aspirin is ordered to prevent stroke in patients who have experienced TIAs.
Documentation of the patient's refusal to take the medication is an inadequate response
by the nurse. There is no need to clarify the order with the health care provider. The
aspirin is not ordered to prevent aches and pains.
A patient is admitted to the hospital with dysphasia and right-sided weakness that
resolves in a few hours. The nurse will anticipate teaching the patient about
a.
alteplase (tPA).
b.
aspirin (Ecotrin).
c.
warfarin (Coumadin).
d.
nimodipine (Nimotop).
Correct Answer: B
Rationale: Following a TIA, patients typically are started on medications such as aspirin to
inhibit platelet function and decrease stroke risk. tPA is used for acute ischemic stroke.
Coumadin is usually used for patients with atrial fibrillation. Nimodipine is used to prevent
cerebral vasospasm after a subarachnoid hemorrhage.
The nurse is caring for a patient with carotid artery narrowing who has just returned after
having left carotid artery angioplasty and stenting. Which assessment information is of
most concern to the nurse?
a.
The pulse rate is 104 beats/min.
b.
There are fine crackles at the lung bases.
c.
The patient has difficulty talking.
d.
The blood pressure is 142/88 mm Hg.
Correct Answer: C
Rationale: Small emboli can occur during carotid artery angioplasty and stenting, and
the aphasia indicates a possible stroke during the procedure. Slightly elevated pulse rate
and blood pressure are not unusual as a result of anxiety associated with the procedure.
Fine crackles at the lung bases may indicate atelectasis caused by immobility during the
procedure; the nurse should have the patient take some deep breaths.
A patient with left-sided hemiparesis arrives by ambulance to the emergency
department. Which action should the nurse take first?
a.
Obtain the Glasgow Coma Scale score.
b.
Check the respiratory rate.
c.
Monitor the blood pressure.
d.
Send the patient for a CT scan.
Correct Answer: B
Rationale: The initial nursing action should be to assess the airway and take any needed
actions to assure a patent airway. The other activities should take place quickly after the
ABCs (airway, breathing, circulation) are completed.
A patient with sudden-onset right-sided weakness has a CT scan and is diagnosed with
an intracerebral hemorrhage. Which information about the patient is most important to
communicate to the health care provider?
a.
The patient has atrial fibrillation and takes warfarin (Coumadin).
b.
The patient takes a diuretic because of a history of hypertension.
c.
The patient's blood pressure is 144/90 mm Hg.
d.
The patient's speech is difficult to under
Correct Answer: A
Rationale: The use of warfarin will have contributed to the intracerebral bleeding and
remains a risk factor for further bleeding. Administration of vitamin K is needed to reverse
the effects of the warfarin, especially if the patient is to have surgery to correct the
bleeding. The history of hypertension is a risk factor for the patient but has no immediate
effect on the patient's care. The BP of 144/90 indicates the need for ongoing monitoring
but not for any immediate change in therapy. Slurred speech is consistent with a left-
sided stroke, and no change in therapy is indicated.
A patient with a left-sided brain stroke suddenly bursts into tears when family members
visit. The nurse should
a.
explain to the family that depression is normal following a stroke.
b.
have the family members leave the patient alone for a few minutes.
c.
teach the family that emotional outbursts are common after strokes.
d.
use a calm voice to ask the patient to stop the crying behavior.
Correct Answer: C
Rationale: Patients who have left-sided brain stroke are prone to emotional outbursts,
which are not necessarily related to the emotional state of the patient. Depression after
a stroke is common, but the suddenness of the patient's outburst suggests that depression
is not the major cause of the behavior. The family should stay with the patient. The crying
is not within the patient's control and asking the patient to stop will lead to
embarrassment.
Potrebbero piacerti anche
- Medical Surgical Nursing Nclex Questions Neuro2Documento12 pagineMedical Surgical Nursing Nclex Questions Neuro2dee_day_8Nessuna valutazione finora
- Neuro Nursing Diagnosis and CareDocumento47 pagineNeuro Nursing Diagnosis and CareMeredith Caitlyn Fernandez100% (1)
- Nle NPDocumento4 pagineNle NPHamad KristinNessuna valutazione finora
- MS Exam SampleDocumento17 pagineMS Exam SampleAllen Bugarin CabadingNessuna valutazione finora
- NCLEX Neurology Practice Test Part IDocumento6 pagineNCLEX Neurology Practice Test Part IAngelica Superable Nacion100% (2)
- Question NEURODocumento39 pagineQuestion NEUROjondelacruz19100% (1)
- Pharmacology ExamDocumento9 paginePharmacology ExamEranio Jr Ang BorjaNessuna valutazione finora
- Review Notes in Infection Control - NCLEXDocumento1 paginaReview Notes in Infection Control - NCLEXwyndz100% (10)
- Medical-Surgical Nursing OverviewDocumento64 pagineMedical-Surgical Nursing OverviewRAYMUND IAN ABALOS100% (2)
- Medical-Surgical Nursing Exam 3 (50 Items)Documento5 pagineMedical-Surgical Nursing Exam 3 (50 Items)lovely_omega100% (1)
- Endocrine Nclex QuestionsDocumento9 pagineEndocrine Nclex QuestionsTiffany Fain Noles100% (1)
- Neurologic NCLEX Practice Test Part 1Documento10 pagineNeurologic NCLEX Practice Test Part 1mpasague100% (2)
- Medical Surgical Nursing Nclex Questions 5Documento18 pagineMedical Surgical Nursing Nclex Questions 5dee_day_8Nessuna valutazione finora
- Nursing-Exam-Questions-12-AR 2Documento122 pagineNursing-Exam-Questions-12-AR 2Cristel Estampador-AlcedoNessuna valutazione finora
- Mental Health and Substance Abuse Nursing ConceptsDocumento10 pagineMental Health and Substance Abuse Nursing ConceptsJenny Torreda100% (1)
- NLE - Practice TestsDocumento25 pagineNLE - Practice TestsBen0% (1)
- Quiz OncologyDocumento20 pagineQuiz OncologyJona Joyce JunsayNessuna valutazione finora
- Chapter 30: Hematologic Disorders Linton: Medical-Surgical Nursing, 7th EditionDocumento5 pagineChapter 30: Hematologic Disorders Linton: Medical-Surgical Nursing, 7th EditionStaceyNessuna valutazione finora
- Exam Questions Samples - NCLEXDocumento7 pagineExam Questions Samples - NCLEXJusta Victorin100% (4)
- NCLEX QuestionsDocumento5 pagineNCLEX QuestionsMeganNessuna valutazione finora
- Pharmacology NCLEX QuestionsDocumento128 paginePharmacology NCLEX QuestionsChristine Williams100% (2)
- Special - NCLEX - Exam - Jakarta - Students - PDF Filename UTF-8''Special NCLEX Exam - Jakarta StudentsDocumento23 pagineSpecial - NCLEX - Exam - Jakarta - Students - PDF Filename UTF-8''Special NCLEX Exam - Jakarta Studentsrizqi100% (1)
- Nle ms1Documento32 pagineNle ms1Neil AlviarNessuna valutazione finora
- P1 RleDocumento34 pagineP1 RleMary Jean GicaNessuna valutazione finora
- 500 Item Free Nursing Board Exam ReviewerDocumento149 pagine500 Item Free Nursing Board Exam ReviewerMichael Montaño100% (3)
- Med Surg ReviewDocumento6 pagineMed Surg ReviewSabhi Sandhu75% (4)
- 100 Item Comprehensive Exam II With Answers and RationaleDocumento16 pagine100 Item Comprehensive Exam II With Answers and RationaleVJ DeeNessuna valutazione finora
- Board Exam 4Documento20 pagineBoard Exam 4Kira100% (9)
- Test Bank CardioDocumento16 pagineTest Bank CardioLudwigJayBarayuga86% (7)
- NCLEX RN Practice Questions 17Documento6 pagineNCLEX RN Practice Questions 17RI NANessuna valutazione finora
- CHAPTER 16 MEDICAL Û SURGICAL EMERGENCIESDocumento10 pagineCHAPTER 16 MEDICAL Û SURGICAL EMERGENCIESjev_belardoNessuna valutazione finora
- MedSurg NeuroDocumento8 pagineMedSurg NeuroZachary T Hall100% (1)
- CA2 Pediatric Nursing Review Post TestDocumento5 pagineCA2 Pediatric Nursing Review Post Testgabby100% (2)
- NP3 ExamDocumento14 pagineNP3 ExamArnie Jude CaridoNessuna valutazione finora
- Gregorio, A 54 Year Old Client Diagnosed WithDocumento81 pagineGregorio, A 54 Year Old Client Diagnosed WithFreeNursingNotesNessuna valutazione finora
- Endocrine NCLEX PN Pract & ANS Questions IIDocumento13 pagineEndocrine NCLEX PN Pract & ANS Questions IIYA HONessuna valutazione finora
- Medical Surgical Nursing BulletsDocumento75 pagineMedical Surgical Nursing Bulletsmervilyn100% (3)
- A Client Is Scheduled For InsertionDocumento31 pagineA Client Is Scheduled For Insertionjenelle_0509100% (2)
- Comprehensive Exam 1Documento19 pagineComprehensive Exam 1karenkaren09100% (1)
- Medical Surgical NursingDocumento21 pagineMedical Surgical Nursingicy431Nessuna valutazione finora
- Psychiatric Nursing Questionares With Rationale 1Documento23 paginePsychiatric Nursing Questionares With Rationale 1Tsuyoshi Bang100% (2)
- M 2Documento8 pagineM 2Aijem RyanNessuna valutazione finora
- Prelims Pedia 102Documento10 paginePrelims Pedia 102quidditch07Nessuna valutazione finora
- Nursing Practice 1 (Dec 2006)Documento12 pagineNursing Practice 1 (Dec 2006)ɹǝʍdןnos100% (1)
- 300 Items QuestionnaireDocumento62 pagine300 Items Questionnairestuffednurse100% (5)
- Pedia NotesDocumento7 paginePedia NotesFreeNursingNotes100% (1)
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideDa EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNessuna valutazione finora
- Neclex Questions Test 3Documento16 pagineNeclex Questions Test 3Brittany Worrall100% (13)
- Neurosensory test knowledge questionnaire 3Documento5 pagineNeurosensory test knowledge questionnaire 3Ebenezer Manguerra Diala Gube Jr.Nessuna valutazione finora
- NCM 104 Midterm Exams - 1Documento21 pagineNCM 104 Midterm Exams - 1Bing58Nessuna valutazione finora
- Neuro and Onco ExamsDocumento19 pagineNeuro and Onco Examsquidditch07Nessuna valutazione finora
- Prometric Mock TestDocumento36 paginePrometric Mock TestDhakshina PriyaNessuna valutazione finora
- Advanced Medsurg Final ExamDocumento113 pagineAdvanced Medsurg Final Examanahmburu966Nessuna valutazione finora
- Page - 1Documento21 paginePage - 1AnnizaNessuna valutazione finora
- When Assessi-WPS OfficeDocumento7 pagineWhen Assessi-WPS OfficeJocelyn AndresNessuna valutazione finora
- Medical Surgical Challenge and Practice TestDocumento12 pagineMedical Surgical Challenge and Practice TestLim Eric100% (1)
- Neurologic ProblemsDocumento11 pagineNeurologic ProblemsFilipino Nurses Central67% (3)
- Chapter 08 - Neurologic ProblemsDocumento12 pagineChapter 08 - Neurologic Problemscari100% (1)
- A Client Who Weighs 90 KG and Had A 50% Burn Injury at 10 AM Arrives at The Hospital Atnoon. Using The Parkland Formula, Calculate The Rate That The Nurse Should UsekdhsfaDocumento1 paginaA Client Who Weighs 90 KG and Had A 50% Burn Injury at 10 AM Arrives at The Hospital Atnoon. Using The Parkland Formula, Calculate The Rate That The Nurse Should Usekdhsfasarasmith1988Nessuna valutazione finora
- Chapter 031Documento3 pagineChapter 031sarasmith1988Nessuna valutazione finora
- SjdnsDocumento1 paginaSjdnssarasmith1988Nessuna valutazione finora
- Mod GDocumento1 paginaMod Gsarasmith1988Nessuna valutazione finora
- Chapter 29 Management of Patients With Structural Infectious andDocumento15 pagineChapter 29 Management of Patients With Structural Infectious andsarasmith1988Nessuna valutazione finora
- Respiratory DisorderDocumento15 pagineRespiratory Disordersarasmith1988Nessuna valutazione finora
- Cardiac - MI and HFDocumento20 pagineCardiac - MI and HFKadijha SingletonNessuna valutazione finora
- A Client Who Weighs 90 KG and Had A 50% Burn Injury at 10 AM Arrives at The Hospital Atnoon. Using The Parkland Formula, Calculate The Rate That The Nurse Should UseDocumento1 paginaA Client Who Weighs 90 KG and Had A 50% Burn Injury at 10 AM Arrives at The Hospital Atnoon. Using The Parkland Formula, Calculate The Rate That The Nurse Should Usesarasmith1988Nessuna valutazione finora
- NUR201 VocabularyDocumento1 paginaNUR201 Vocabularysarasmith1988Nessuna valutazione finora
- More Nclex From Evolve ResourcesDocumento18 pagineMore Nclex From Evolve Resourcessarasmith1988Nessuna valutazione finora
- Chapter 16Documento6 pagineChapter 16sarasmith1988Nessuna valutazione finora
- Cardiovascular: Common Lab Tests For Cardiovascular DisordersDocumento49 pagineCardiovascular: Common Lab Tests For Cardiovascular Disorderssarasmith1988Nessuna valutazione finora
- Which Nursing Intervention Would Be Most Appropriate When Caring For An Acutely Agitated Client Diagnosed With Paranoid SchizophreniaDocumento1 paginaWhich Nursing Intervention Would Be Most Appropriate When Caring For An Acutely Agitated Client Diagnosed With Paranoid Schizophreniasarasmith1988Nessuna valutazione finora
- Mod GDocumento1 paginaMod Gsarasmith1988Nessuna valutazione finora
- Chapter 16Documento6 pagineChapter 16sarasmith1988Nessuna valutazione finora
- NUR201 VocabularyDocumento1 paginaNUR201 Vocabularysarasmith1988Nessuna valutazione finora
- Cardiovascular: Common Lab Tests For Cardiovascular DisordersDocumento49 pagineCardiovascular: Common Lab Tests For Cardiovascular Disorderssarasmith1988Nessuna valutazione finora
- Chapter 16Documento6 pagineChapter 16sarasmith1988Nessuna valutazione finora
- Heart Failure Mechanisms and Assessment FindingsDocumento9 pagineHeart Failure Mechanisms and Assessment Findingssarasmith1988Nessuna valutazione finora
- Cardiovascular: Common Lab Tests For Cardiovascular DisordersDocumento49 pagineCardiovascular: Common Lab Tests For Cardiovascular Disorderssarasmith1988Nessuna valutazione finora
- Nclex CVDocumento6 pagineNclex CVsarasmith1988Nessuna valutazione finora
- Cardiac - MI and HFDocumento20 pagineCardiac - MI and HFKadijha SingletonNessuna valutazione finora
- Chapter 29 Management of Patients With Structural Infectious andDocumento15 pagineChapter 29 Management of Patients With Structural Infectious andsarasmith1988Nessuna valutazione finora
- Chapter 020Documento3 pagineChapter 020sarasmith1988Nessuna valutazione finora
- Chapter 16Documento6 pagineChapter 16sarasmith1988Nessuna valutazione finora
- Chapter 019Documento2 pagineChapter 019sarasmith1988Nessuna valutazione finora
- Chapter 16Documento6 pagineChapter 16sarasmith1988Nessuna valutazione finora
- Mod - C - Study 202Documento3 pagineMod - C - Study 202sarasmith1988Nessuna valutazione finora
- Chapter 012Documento3 pagineChapter 012sarasmith1988Nessuna valutazione finora
- Fetal Blood Sampling: 1. PurposeDocumento7 pagineFetal Blood Sampling: 1. PurposeMuathNessuna valutazione finora
- Comparative Study of Hepatoprotective Activity of Proprietary Polyherbal Preparations Against paraDocumento5 pagineComparative Study of Hepatoprotective Activity of Proprietary Polyherbal Preparations Against paraassemNessuna valutazione finora
- Effects of Vasopressors On Cerebral Circulation.6Documento11 pagineEffects of Vasopressors On Cerebral Circulation.6diego morenoNessuna valutazione finora
- Laboratory Handbook PDFDocumento184 pagineLaboratory Handbook PDFReymi Then50% (2)
- F 16 CLINNeurologicalObservationChartDocumento2 pagineF 16 CLINNeurologicalObservationChartRani100% (1)
- Smriti Mishra BCG NCCDocumento1 paginaSmriti Mishra BCG NCCashish bondiaNessuna valutazione finora
- Clsi 2012Documento50 pagineClsi 2012niluh suwasanti100% (1)
- Artificial MethodsDocumento23 pagineArtificial MethodsJanna Broqueza RodriguezNessuna valutazione finora
- 2018 01 Early Pregnancy Loss LightDocumento41 pagine2018 01 Early Pregnancy Loss LightMishal FatimaNessuna valutazione finora
- 1 Hygene and SanitationDocumento22 pagine1 Hygene and SanitationJammil Ud-ulonNessuna valutazione finora
- Science: Quarter 2 - Module 1Documento20 pagineScience: Quarter 2 - Module 1Kate BatacNessuna valutazione finora
- CA Mega Brochure 1090-Rev-B EngDocumento6 pagineCA Mega Brochure 1090-Rev-B EngMuhammad Mahbøøb SadiqNessuna valutazione finora
- Gingival Periodontal IndexDocumento23 pagineGingival Periodontal Indexxodia_04100% (3)
- MESOTHERAPYDocumento39 pagineMESOTHERAPYAtid Amanda100% (2)
- List of ReferencesDocumento3 pagineList of ReferencesRave MiradoraNessuna valutazione finora
- Cleaning Allergen Polyurethane 1Documento128 pagineCleaning Allergen Polyurethane 1Yudhi AdiNessuna valutazione finora
- Management of Infants BornDocumento6 pagineManagement of Infants BornDiana FlorezNessuna valutazione finora
- Abbas Et Al. 2020 - Nature Immunology-2020-Abbas-TomaselloDocumento33 pagineAbbas Et Al. 2020 - Nature Immunology-2020-Abbas-TomaselloAchille BroggiNessuna valutazione finora
- Energy ThumpsDocumento3 pagineEnergy ThumpsTink De NeverlandNessuna valutazione finora
- Review 02Documento2 pagineReview 02Vicki KimNessuna valutazione finora
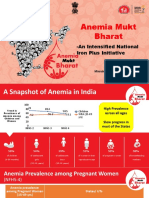
- Anemia Mukt Bharat: - An Intensified National Iron Plus InitiativeDocumento23 pagineAnemia Mukt Bharat: - An Intensified National Iron Plus InitiativeAnggun100% (1)
- Drug Study NifedipineDocumento3 pagineDrug Study NifedipineJanzelvine Lee MontenegroNessuna valutazione finora
- Nursing Care Plan: Change in Health Status As Evidence by Excessive Shaking After 1hour, The Patient Will Be Able ToDocumento1 paginaNursing Care Plan: Change in Health Status As Evidence by Excessive Shaking After 1hour, The Patient Will Be Able ToVoid LessNessuna valutazione finora
- Cheat Sheet 2Documento5 pagineCheat Sheet 2Katelyn HillNessuna valutazione finora
- Microbiology Quick TableDocumento2 pagineMicrobiology Quick TableCoy Nuñez100% (2)
- Hormone Levels For Fertility Patients1Documento4 pagineHormone Levels For Fertility Patients1Kunbi Santos-ArinzeNessuna valutazione finora
- Pain Pada SyringomyeliaDocumento6 paginePain Pada Syringomyeliavico julendiNessuna valutazione finora
- G128 0066721 MSDSDocumento8 pagineG128 0066721 MSDSfiguev2208Nessuna valutazione finora
- Prosthetic Management - Transtibial Amputation Part 12Documento25 pagineProsthetic Management - Transtibial Amputation Part 12Marizandi BothaNessuna valutazione finora
- Biochemistry Importance for NursesDocumento15 pagineBiochemistry Importance for NursesJulius Memeg PanayoNessuna valutazione finora