Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Pancreatic Hormones & Antidiabetic Agents: A. Insulin
Caricato da
Usman Ali AkbarTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Pancreatic Hormones & Antidiabetic Agents: A. Insulin
Caricato da
Usman Ali AkbarCopyright:
Formati disponibili
PANCREATIC HORMONES & ANTIDIABETIC AGENTS
A. Insulin
1. Structure and synthesis a. Insulin is a polypeptide hormone produced by the pancreatic b cell. Insulin consists of two
chains, A and B, linked by two disulfide bridges.
b. Human insulin contains 51 amino acids. Bovine insulin differs from human insulin at three amino acid sites; porcine
insulin differs in only one amino acid.
c. Insulin is stored as a complex with Zn2+; two molecules of zinc complex six molecules of insulin.
d. Insulin synthesis and release are modulated by the following:
(1) The most important stimulus is glucose. Amino acids, fatty acids, and ketone bodies also stimulate release.
(2) The islets of Langerhans contain several cell types besides b cells that synthesize and
release peptide humoral agents (including glucagon and somatostatin) that can modulate insulin secretion.
(3) a-Adrenergic pathways inhibit secretion of insulin; this is the predominant inhibitory mechanism.
e. b-Adrenergic stimulation increases insulin release.
f. Elevated intracellular Ca2+ acts as an insulin secretagogue.
2. Mechanism of action
a. Insulin binds to specific high-affinity receptors with tyrosine kinase activity located in the plasma membrane. Specific
tyrosine residues of the insulin receptor become phosphorylated (autophosphorylation); other substrates for
phosphorylation include IRS-14 (insulin receptor substrates-1 to -4). The increase in glucose transport inmuscle and
adipose tissue is mediated by the recruitmentof hexose transport molecules (GLUT-1 andGLUT-4) into the plasma
membrane.
b. Insulin alters the phosphorylation state of key metabolic enzymes, leading to enzymatic activation or inactivation.
c. Insulin induces the transcription of several genes involved in increasing glucose catabolism and specifically inhibits
transcription of other genes involved in gluconeogenesis
.
3. Actions. Insulin promotes systemic cellular K+ uptake.
a. Liver
(1) Inhibits glucose production and increases glycolysis
(2) Inhibits glycogenolysis and stimulates glycogen synthesis
(3) Increases the synthesis of triglycerides
(4) Increases protein synthesis
b. Muscle
(1) Increases glucose transport and glycolysis
(2) Increases glycogen deposition
(3) Increases protein synthesis
c. Adipose tissue
(1) Increases glucose transport
(2) Increases lipogenesis and lipoprotein lipase
(3) Decreases intracellular lipolysis
4. Pharmacologic properties
a. Insulin has a t1/2 of 510 minutes.
b. Insulin is degraded by hepatic glutathioneinsulin transhydrogenase, which reduces the di disulfide
linkages between the A and B chains, producing two biologically inactive peptides.
5. Insulin preparations
(1) Rapid acting 3 Insulin analogs :
Insulin lispro, insulin aspart , insulin glulisine
*rapid onset and early peaks
*Control of postprandial glucose levels
*Immediately injected after meals
*For treatment of uncomplicated diabetic ketoacidosis.
(2) Short acting. Regular insulin (IV) emergency/ SC ordinary
Control postprandial glucose concentrations.
1 h before meal
(3) Intermediate acting Neutral Protamin Hagedorn Insulin ( NPH)
Regular insulin + Protamine
Delayed onset and peak of action
(4) Long acting Insulin glargine and Insulin detemir
Peakless basal insulin level
Last > 20h : Control glucose level without producing hypoglycemia
Insulin Delivery systems
1) Pen devices containing prefilled regular, lispro, NPH, glargine, premixed lispro protamine-lispro, or premixed
aspart protamine-aspart
2) Jet injector systems
3) Insulin pumps (continuous SC insulin infusion devices, CSII)
Inhaled insulin: Afrezza
Is a rapid-acting inhaled insulin to be administered prior to meals or within 20 minutes of starting a meal
The most common ADRs associated with Afrezza in clinical trials were hypoglycemia, cough, and throat pain or
irritation
It is not a substitute for long-acting insulin and must be used in combination with long-acting insulin in patients
with type 1 diabetes
It is not recommended for the treatment of diabetic ketoacidosis or in patients who smoke or who have chronic
lung disease
Adverse Effects :
1. Hypoglycemia
2. Insulin allergy and resistance
a) Insulin allergy
b) Insulin resistance
3. Lipohypertrophy
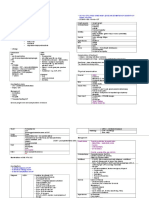
NON INSULIN ANTIDIABETIC DRUGS
Insulin Secretogogues Biguanides Thiazolidinedones
Drugs :
Older:
Chloropromide
Tolbutamide
Intermediate:
Glimepride
Glipize
Glyburide
Fast acting:
Repaglinide
Nateglinide
MOA :
Stimulate the release of endogenous
insulin by promoting closure of K+
channels -> deplorization -> insulin
release
Drugs :
Metformin
MOA:
Reduces postprandial and fasting
glucose
*inhibit hepatic and renal
gluconeogenesis
Stimulation of glucose uptake and
glycolysis and slowing of glucose
absorption from GIT, Reduction of
glucagon
All thru activation of AMP stimulated
kinases.
Reduces endogenous insulin
production through enhanced insulin
sensitivity
Restore fertitlity in anovulatory
women with POCD.
MOA: binds to the PPAR-gamma
(peroxisome proliferators activated
receptor) in cell nuclei esp in
adipocytes transcription of
multiple genes affecting lipid
homeostasis ( lipolysis, TG
accumulation, plasma free fa
concs) glu uptake in muscle,
gluconeogensis & hepatic glu
output by insulin. sensitivity of
adipocytes to insulin pt will gain
wt
Uses:
Monotherapy (up to 8mg bd) in type
2 DM
Combine with metformin or
sulphonyurea if there is insufficient
in fasting bld glu
Toxicities :
*hypoglycemia
* rash/allergic reactions
*Weight gain
Toxicities :
Do not cause hypoglycemia
GIT distress
Lactic acidosis
SEs:
Hepatic impairment. Avoid in pts
with hx of liver impairment or if basal
ALT is >2.5x upper limit of normal. If
give drug & LFT >3x, stop drug.
Fluid retention monitor carefully
for HF in pt with cardiac problems
Hb & hematocrit & wbc cos of in
bld vol due to fluid retention
Ovulation may be induced in
premenopausal/anovulatory women
with insulin resistance. May need
contraception
LDL & HDL over time, but HDL
more improve lipid profile
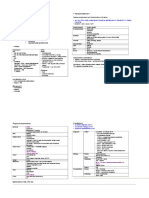
@Glucosidase Inhibitors Pramlintide Exenatide Sitagliptin
MOA: binds to the PPAR-
gamma (peroxisome
proliferators activated
receptor) in cell nuclei
esp in adipocytes
transcription of multiple
genes affecting lipid
homeostasis ( lipolysis,
TG accumulation,
plasma free fa concs)
glu uptake in muscle,
gluconeogensis &
hepatic glu output by
insulin. sensitivity of
adipocytes to insulin
pt will gain wt
Uses:
o Monotherapy (up to
8mg bd) in type 2 DM
o Combine with
metformin or
sulphonyurea if there
is insufficient in
fasting bld glu
SEs:
a. Hepatic impairment.
Avoid in pts with hx of
liver impairment or if
basal ALT is >2.5x upper
limit of normal. If give
drug & LFT >3x, stop
drug.
b. Fluid retention monitor
Synthetic analog of amylin
(hormone produced by
pancreatic B cells)
Activates high affinity
receptors ( complex of
calcitonin and Receptor
activity modifying
receptor(RANK(
Suppresses glucagon
release
Slow gastric emptying
Reduce appetite.
Use to treat DM type 1
and type 2
SE:
GI Disturbances
Headache
hypoglycemia
Glucagon like peptide-1
Incretin family.
Agument glucose
stimulated insulin rease
From pancreatic B cells
Retard gastric emptying
Inhibit glucagon secretion
Feeling of satiety
GLP-1 increase cAMp
Ca2+
Exenatide :
*Used in combination with
metformin , sulfonylurea
for type 1 and 2
SE: GIT disturbances
Nausea
Hypoglycemia
Fata acute
pancreatitis(Rare)
Oral inhibitor of
dipeptidyl peptidase 4
(DPP40
Type 2 diabetes
Used with metformin or
thiazolidinedione.
Sitaglipti :
Insulin release
Inhibit glucagon secretion
Anorexic effect
SE:
Headache
Nasopharyngitis
Upper Resp Track
Infection.
carefully for HF in pt with
cardiac problems
c. Hb & hematocrit & wbc
cos of in bld vol due to
fluid retention
d. Ovulation may be
induced in
premenopausal/anovulat
ory women with insulin
resistance. May need
contraception
e. LDL & HDL over time,
but HDL more
improve lipid profile
Glucagon :
Glucagon
a. Structure and synthesis
(1) Glucagon is a single-chain polypeptide of 29 amino acids produced by the a cells of the pancreas.
(2) Glucagon shares a structural homology with secretin, VIP, and gastric inhibitory peptide.
(3) Secretion of glucagon is inhibited by elevated plasma glucose, insulin, and somatostatin.
(4) Secretion of glucagon is stimulated by amino acids, sympathetic stimulation, and sympathetic secretion.
b. Actions and pharmacologic properties
(1) Membrane-bound receptors are most abundant in the liver; response is coupled to an
increase in cAMP.
(2) Glucagon stimulates the use of glycogen stores and gluconeogenesis; in general, its
actions oppose those of insulin.
(3) Large doses produce marked relaxation of smooth muscle.
(4) Glucagon is extensively degraded in the liver and kidney and is also subject to hydrolysis
in plasma. Plasma t1/2 of glucagon is approximately 35 minutes.
c. Therapeutic uses
(1) Glucagon produces rescue from hypoglycemic crisis. Glucagon rapidly increases blood
glucose in insulin-induced hypoglycemia if hepatic glycogen stores are adequate.
(2) Glucagon provides intestinal relaxation prior to radiologic examination.
(3) Glucagon causes b-cell stimulation of insulin secretion; it is used to assess pancreatic
reserves.
d. Adverse effects. The adverse effects of glucagon are minimal; there is a low incidence of
nausea and vomiting.
Potrebbero piacerti anche
- Endocrine PharmacologyDocumento42 pagineEndocrine PharmacologyAhmed El SharkawyNessuna valutazione finora
- Hypoglycemia, A Simple Guide To The Condition, Treatment And Related ConditionsDa EverandHypoglycemia, A Simple Guide To The Condition, Treatment And Related ConditionsNessuna valutazione finora
- Naplex Complete Study Outline A Topic-Wise Approach DiabetesDa EverandNaplex Complete Study Outline A Topic-Wise Approach DiabetesValutazione: 4 su 5 stelle4/5 (2)
- Pancreatic Hormones by KatzungDocumento3 paginePancreatic Hormones by KatzungChristian DeeNessuna valutazione finora
- Insulin and Oral AntidiabeticsDocumento24 pagineInsulin and Oral AntidiabeticsMirza Shaharyar Baig100% (1)
- Organophosphate PoisoningDocumento23 pagineOrganophosphate PoisoningUsman Ali AkbarNessuna valutazione finora
- Insulin and Oral Hypoglycemic AgentsDocumento27 pagineInsulin and Oral Hypoglycemic Agentsapi-19916399100% (1)
- Pancreas 2021Documento32 paginePancreas 2021Dr. AliNessuna valutazione finora
- Diabetes Mellitus.Documento42 pagineDiabetes Mellitus.betablockers100% (1)
- Physiology of Diabetes: Dr. Solomon Sathishkumar. MDDocumento36 paginePhysiology of Diabetes: Dr. Solomon Sathishkumar. MDKhaled LajmiNessuna valutazione finora
- MBS2-K7-Pharmacology of Endocrine PancreasDocumento55 pagineMBS2-K7-Pharmacology of Endocrine PancreasZoga Pratantia TohariNessuna valutazione finora
- What Are The Cellular and Molecular Actions of Insulin?Documento13 pagineWhat Are The Cellular and Molecular Actions of Insulin?Elle ReyesNessuna valutazione finora
- Insulin and The Oral HypoglycemicsDocumento9 pagineInsulin and The Oral HypoglycemicsHasibNessuna valutazione finora
- Pharmacology - Section 25 - Insulin and HypoglycaemicsDocumento3 paginePharmacology - Section 25 - Insulin and HypoglycaemicsPathalee ThalpavilaNessuna valutazione finora
- Dr. Solomon Sathishkumar, MD Department of Physiology Christian Medical College Vellore, IndiaDocumento48 pagineDr. Solomon Sathishkumar, MD Department of Physiology Christian Medical College Vellore, IndiaKrairat KomdeeNessuna valutazione finora
- Unit 1 Antidiabetic Drugs Pharmacy-IIDocumento69 pagineUnit 1 Antidiabetic Drugs Pharmacy-IIAsad MirajNessuna valutazione finora
- Pancreatic HormonesDocumento41 paginePancreatic HormonesBodea Doru100% (1)
- #3 Pancreatic Hormones & Antidiabetic Drugs 14 PDFDocumento14 pagine#3 Pancreatic Hormones & Antidiabetic Drugs 14 PDFOmar BasimNessuna valutazione finora
- Metabolic Syndrome and Diabetes - 200918Documento80 pagineMetabolic Syndrome and Diabetes - 200918helena.lovrincevicNessuna valutazione finora
- End PancreasDocumento29 pagineEnd Pancreasahmed alkramyNessuna valutazione finora
- Insulin & Oral Hypoglycemic Agents.: Pharmacology-2Documento33 pagineInsulin & Oral Hypoglycemic Agents.: Pharmacology-2maxi noveloNessuna valutazione finora
- AntidiabetesDocumento51 pagineAntidiabetesPuri Ratna KartiniNessuna valutazione finora
- GI and Reproductive HormoneDocumento74 pagineGI and Reproductive Hormonepranutan739Nessuna valutazione finora
- Richa Chauhan PPT 5 21Documento13 pagineRicha Chauhan PPT 5 21Richa ChauhanNessuna valutazione finora
- Group 3 Concepcion Contacto Cordero Cornejo Cornell Cortez CruzDocumento62 pagineGroup 3 Concepcion Contacto Cordero Cornejo Cornell Cortez CruzConcepcion Kevin ChuckNessuna valutazione finora
- Physio 7Documento12 paginePhysio 7amjadNessuna valutazione finora
- InsulinDocumento50 pagineInsulinTandin SonamNessuna valutazione finora
- Physiology, Endocrine, Pancreas - StatPearls - NCBI BookshelfDocumento5 paginePhysiology, Endocrine, Pancreas - StatPearls - NCBI Bookshelfdrpaez27Nessuna valutazione finora
- Hormones in Metabolism (DR - Ani Retno)Documento45 pagineHormones in Metabolism (DR - Ani Retno)AciNessuna valutazione finora
- Insulin, Oral Hypoglycemic Agents-1Documento23 pagineInsulin, Oral Hypoglycemic Agents-1IbrahimNessuna valutazione finora
- Diabetes Mellitus and Laboratory Tests of DiabetesDocumento24 pagineDiabetes Mellitus and Laboratory Tests of DiabetesturkiNessuna valutazione finora
- Anti-Diabetic Drugs Part A-2Documento35 pagineAnti-Diabetic Drugs Part A-2rimsha waseemNessuna valutazione finora
- Classifications of Insulin2Documento116 pagineClassifications of Insulin2loglesb1Nessuna valutazione finora
- Pathophysiology Notes: Diabetes Mellitus Is A Group of Metabolic Disorders Characterized HyperglycemiaDocumento14 paginePathophysiology Notes: Diabetes Mellitus Is A Group of Metabolic Disorders Characterized HyperglycemiaHaifa ibrahimNessuna valutazione finora
- Diabetes Mellitus: Regulation of Blood GlucoseDocumento65 pagineDiabetes Mellitus: Regulation of Blood GlucoseReggae BautistaNessuna valutazione finora
- I. METABOLISM (Intro) : Quiz/Test Review Notes Section 1 Short Term Metabolism (Metabolism)Documento7 pagineI. METABOLISM (Intro) : Quiz/Test Review Notes Section 1 Short Term Metabolism (Metabolism)parthpatel007Nessuna valutazione finora
- The Pancreas: Dr.H.Gusbakti, MSC, PKK, Aifm Professor of Physiology University Islamic North SumateraDocumento54 pagineThe Pancreas: Dr.H.Gusbakti, MSC, PKK, Aifm Professor of Physiology University Islamic North SumateraandreNessuna valutazione finora
- Pancreas Aug 4Documento53 paginePancreas Aug 4Dr.Gomathi sivakumarNessuna valutazione finora
- Endocrine Pancreas & Fuel Homeostasis: Learning ObjectivesDocumento7 pagineEndocrine Pancreas & Fuel Homeostasis: Learning ObjectivesMaggieLockeNessuna valutazione finora
- INSULIN Dan Obat Hipoglikemik OralDocumento35 pagineINSULIN Dan Obat Hipoglikemik OralSwietenia Rambu SabatiNessuna valutazione finora
- Endo Pancrease ElhDocumento27 pagineEndo Pancrease Elhodiodi57Nessuna valutazione finora
- Week 3 Pharmaco - Part 1Documento44 pagineWeek 3 Pharmaco - Part 1Tiko JomidavaNessuna valutazione finora
- Current Modalities in The Treatment of Non-Insulin Dependent DMDocumento6 pagineCurrent Modalities in The Treatment of Non-Insulin Dependent DMSemir1989Nessuna valutazione finora
- Physiologic Response To Hypoglycemia in Healthy Individuals and Patients With Diabetes MellitusDocumento14 paginePhysiologic Response To Hypoglycemia in Healthy Individuals and Patients With Diabetes Mellitus11. Nguyễn Võ Như HuỳnhNessuna valutazione finora
- DiabetesDocumento10 pagineDiabetesLyNessuna valutazione finora
- 5 Parathyroid & PancreasDocumento13 pagine5 Parathyroid & Pancreasapi-3706483Nessuna valutazione finora
- DR - Mohammed Qasim 2017-2018 4 GradeDocumento40 pagineDR - Mohammed Qasim 2017-2018 4 GradeFarah Bashar Al-RawachyNessuna valutazione finora
- Lecture 7 Diabetes Mellitus 2021Documento39 pagineLecture 7 Diabetes Mellitus 2021Ahmed ShakerNessuna valutazione finora
- Type I Diabetes MellitesDocumento71 pagineType I Diabetes MellitesMuthu LakshmiNessuna valutazione finora
- Unit Fourteen: Endocrinology and Reproduction: Chapter 78: Insulin, Glucagon, and Diabetes MellitusDocumento27 pagineUnit Fourteen: Endocrinology and Reproduction: Chapter 78: Insulin, Glucagon, and Diabetes MellitusPatrick CommettantNessuna valutazione finora
- ANTI-DIABETIC AGENTS (OHAs)Documento42 pagineANTI-DIABETIC AGENTS (OHAs)Prajwal Rao KNessuna valutazione finora
- Endocrin E Pancreas: DR - Sabri.S.EltaybeDocumento43 pagineEndocrin E Pancreas: DR - Sabri.S.EltaybehamidNessuna valutazione finora
- CC 11 GlucoseDocumento9 pagineCC 11 GlucoseJohn OgunsolaNessuna valutazione finora
- MS3 Review NotesDocumento11 pagineMS3 Review NotesPaul Anthony LoricaNessuna valutazione finora
- 14 - Blood Glucose HomeostasisDocumento34 pagine14 - Blood Glucose HomeostasischeckmateNessuna valutazione finora
- Endocrine Pancreas & Fuel Homeostasis: Learning ObjectivesDocumento7 pagineEndocrine Pancreas & Fuel Homeostasis: Learning ObjectivesEmmanuel NhandaraNessuna valutazione finora
- Anti HyperglycemeaDocumento17 pagineAnti HyperglycemeaMuhammad KhalilNessuna valutazione finora
- Diabetes Mellitus Type 11Documento44 pagineDiabetes Mellitus Type 11MARICRIS NEBIARNessuna valutazione finora
- Antidiabetic Chapter34 (This)Documento93 pagineAntidiabetic Chapter34 (This)hamidNessuna valutazione finora
- InsulinDocumento6 pagineInsulinAmbroseNessuna valutazione finora
- Insuline HormoneDocumento36 pagineInsuline HormoneF ParikhNessuna valutazione finora
- Nephrotic SyndromeDocumento2 pagineNephrotic SyndromeUsman Ali AkbarNessuna valutazione finora
- Chronic Renal Failure Long CaseDocumento2 pagineChronic Renal Failure Long CaseUsman Ali AkbarNessuna valutazione finora
- Polycystic Kidneys: Adult PKD: ComplicationsDocumento1 paginaPolycystic Kidneys: Adult PKD: ComplicationsUsman Ali AkbarNessuna valutazione finora
- CRF Wtih Fluid Overload MX PathwayDocumento1 paginaCRF Wtih Fluid Overload MX PathwayUsman Ali AkbarNessuna valutazione finora
- Urinary Tract Infection & PyelonephritisDocumento3 pagineUrinary Tract Infection & PyelonephritisUsman Ali AkbarNessuna valutazione finora
- Chronic Renal Failure: Concise Long Case ApproachDocumento3 pagineChronic Renal Failure: Concise Long Case ApproachUsman Ali AkbarNessuna valutazione finora
- GI Bleeding Team Work - 2nd EditionDocumento9 pagineGI Bleeding Team Work - 2nd EditionUsman Ali AkbarNessuna valutazione finora
- Renal TransplantDocumento2 pagineRenal TransplantUsman Ali AkbarNessuna valutazione finora
- Renal Tubular Acidosis Summary - AdjDocumento1 paginaRenal Tubular Acidosis Summary - AdjUsman Ali AkbarNessuna valutazione finora
- CRF Wtih Fluid Overload MX Pathway - AdjDocumento1 paginaCRF Wtih Fluid Overload MX Pathway - AdjUsman Ali AkbarNessuna valutazione finora
- DialysisDocumento2 pagineDialysisUsman Ali AkbarNessuna valutazione finora
- Subject: Permission For Badminton Court NID, Multan: TH THDocumento1 paginaSubject: Permission For Badminton Court NID, Multan: TH THUsman Ali AkbarNessuna valutazione finora
- Renal Tubular Acidosis SummaryDocumento1 paginaRenal Tubular Acidosis SummaryUsman Ali AkbarNessuna valutazione finora
- Obstructive Airway Disease: Dr. Khalid Al-Mobaireek King Khalid University HospitalDocumento53 pagineObstructive Airway Disease: Dr. Khalid Al-Mobaireek King Khalid University HospitalUsman Ali AkbarNessuna valutazione finora
- 2017-2018 Clerkship Calendar - FinalDocumento3 pagine2017-2018 Clerkship Calendar - FinalNickNessuna valutazione finora
- King Khalid University Hospital Department of Obstetrics & Gyncology Course 481Documento40 pagineKing Khalid University Hospital Department of Obstetrics & Gyncology Course 481Usman Ali AkbarNessuna valutazione finora
- GI Bleeding Team Work - 2nd EditionDocumento9 pagineGI Bleeding Team Work - 2nd EditionUsman Ali AkbarNessuna valutazione finora
- Anaemia in PregnancyDocumento13 pagineAnaemia in PregnancyUsman Ali AkbarNessuna valutazione finora
- Anaemia in PregnancyDocumento13 pagineAnaemia in PregnancyUsman Ali AkbarNessuna valutazione finora
- Ibs Presentation PDFDocumento18 pagineIbs Presentation PDFUsman Ali AkbarNessuna valutazione finora
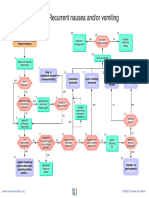
- Recurrent VomitingDocumento16 pagineRecurrent VomitingUsman Ali AkbarNessuna valutazione finora
- Cord ProlapseDocumento2 pagineCord ProlapseUsman Ali AkbarNessuna valutazione finora
- Recurrent Nausea Andor VomitingDocumento8 pagineRecurrent Nausea Andor VomitingUsman Ali AkbarNessuna valutazione finora
- DR Othman Alharbi, MBBS FRCPC Assistance Professor & Consultant Gastroenterology College of Medicine King Saud UniversityDocumento18 pagineDR Othman Alharbi, MBBS FRCPC Assistance Professor & Consultant Gastroenterology College of Medicine King Saud UniversityUsman Ali AkbarNessuna valutazione finora
- GRAM NEGATIVE RODS (5) Fastidious Organisms From Animal Sources (A)Documento1 paginaGRAM NEGATIVE RODS (5) Fastidious Organisms From Animal Sources (A)Usman Ali AkbarNessuna valutazione finora
- Foreign Visiting Student Medical Status Form PDFDocumento1 paginaForeign Visiting Student Medical Status Form PDFUsman Ali AkbarNessuna valutazione finora
- When Hope DiesDocumento2 pagineWhen Hope DiesUsman Ali AkbarNessuna valutazione finora
- TSMEntry 2Documento1 paginaTSMEntry 2Usman Ali AkbarNessuna valutazione finora
- Diseases of The StomachDocumento17 pagineDiseases of The StomachUsman Ali AkbarNessuna valutazione finora