Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Lim Et Al. - 2012 - Validation of The Paediatric Hearing Impairment Caregiver Experience (PHICE) Questionnaire
Caricato da
LiRuijie0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
47 visualizzazioni1 paginaLim, L. H. Y., Xiang, L., Li, R., Wong, N. L. Y., & Yuen, K. C. P. (2012). Validation of the Paediatric Hearing Impairment Caregiver Experience (PHICE) Questionnaire. Presented at the International Society for Pharmacoeconomics and Outcomes Research (ISPOR) 17th Annual International Meeting, Washington, D.C. doi:10.13140/2.1.4922.0488
Titolo originale
Lim et al. - 2012 - Validation of the Paediatric Hearing Impairment Caregiver Experience (PHICE) Questionnaire
Copyright
© © All Rights Reserved
Formati disponibili
PDF, TXT o leggi online da Scribd
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoLim, L. H. Y., Xiang, L., Li, R., Wong, N. L. Y., & Yuen, K. C. P. (2012). Validation of the Paediatric Hearing Impairment Caregiver Experience (PHICE) Questionnaire. Presented at the International Society for Pharmacoeconomics and Outcomes Research (ISPOR) 17th Annual International Meeting, Washington, D.C. doi:10.13140/2.1.4922.0488
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato PDF, TXT o leggi online su Scribd
0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
47 visualizzazioni1 paginaLim Et Al. - 2012 - Validation of The Paediatric Hearing Impairment Caregiver Experience (PHICE) Questionnaire
Caricato da
LiRuijieLim, L. H. Y., Xiang, L., Li, R., Wong, N. L. Y., & Yuen, K. C. P. (2012). Validation of the Paediatric Hearing Impairment Caregiver Experience (PHICE) Questionnaire. Presented at the International Society for Pharmacoeconomics and Outcomes Research (ISPOR) 17th Annual International Meeting, Washington, D.C. doi:10.13140/2.1.4922.0488
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato PDF, TXT o leggi online su Scribd
Sei sulla pagina 1di 1
Validation of the Paediatric Hearing Impairment Caregiver Experience
Questionnaire in Singapore Population
Hsueh Yee LynneLIM
1
, MBBS, FRCS, MPH, Ling XIANG
2
, MBBS, MMed, MSc, Ruijie Li
3
, MSc, Naomi Wong
1
, BSpPath (Hons), Chi Pun Kevin Yuen
4
, PhD
1
Otolaryngology - Head Neck Surgery Department, National University Health System, Singapore,
2
National University of Singapore,
3
Health Services & Outcomes Research, National Healthcare Group, Singapore,
4
Department of Special Education and Counselling, The Hong Kong Institute of Education
Corresponding author:
LI Ruijie (Ruijie_li@nhg.com.sg)
Research Analyst,
Health Services & Outcomes Research,
National Healthcare Group,
Singapore
Background
The stress experienced by parents of children with hearing loss has been studied over the past 2 decades. Increased parenting
stress is often associated with developmental problems such as delay in acquisition of language, social and emotional
problems. The stress that parents endure is also subjected to fluctuation as they go through the process of meeting and
overcoming various challenges associated with their childs hearing impairment. An instrument, the Paediatric Hearing
Impairment Caregiver Experience Questionnaire (PHICE) was therefore developed to document the levels of stress as
experienced by parents of children with hearing impairment
1
. While this instrument has been validated in the United States, it
use would not be appropriate for use in a Singapore context due to the varying infrastructures and culture of the hearing
impaired in the 2 countries. This study therefore aims to modify and validate the PHICE questionnaire to make it relevant for
use in Singapore.
The PHICE questionnaire is a 68 item instrument spanning across the domains: communication, education, emotional well-
being, equipment, financial, healthcare, social, and support. The item is scored on an 8 point Likert scale with the following
descriptors: "Not applicable", "No stress", "Very low stress", "Low stress", "Moderate stress", "High stress", "Very high stress"
and "Extremely high stress". Given its length, it takes a considerable amount of time to complete the questionnaire. Therefore,
another aim of this study is to create a shorter version of the questionnaire.
Methods & Analysis
Expert panel review
Prior to administering the questionnaire on the local population, an expert panel was convened to assess each item on the
questionnaire for its suitability for use in Singapore. The expert panel consisted of an otolaryngology surgeon, an audiologist
and two speech-language therapists. After a round of review, 7 questions were removed.
These 7 questions were removed primarily because of the focus on sign language. These items were considered irrelevant
because in the Singapore, only a limited number of children with hearing loss are attending the Singapore School for the Deaf,
the only school whose primary medium of instruction is sign language in Singapore.
Administering of the questionnaire
125 caregivers of children with permanent hearing loss for at least 6 months attending the otolaryngology, audiology and
aural rehabilitation clinic were recruited into the study. Informed consent was sought and a total of 125 completed PHICE
questionnaires were collected between January 2006 and December 2008. The questionnaire was self-administered.
Scaling
The items were recoded such that the Not applicable entries were mapped to No stress. This is on the assumption that if it
is not applicable to a caregiver, they should not face stress in that particular area. This recoding is necessary in order to
preserve the inherent assumption of equidistant between points on the Likert scale.
Missing data
Missing data was filled by cross validation imputation using the package missMDA
2
through R
3
. The amount of missing
data was deemed to be small at 0.72%. The imputed data was rounded off to the nearest integer to maintain the ordinal
nature of the scale and to make the data interpretable
4
.
Exploratory factor analysis
Factor analysis using principal axis factoring was conducted the using the package psych
5
through R
3
. Oblique rotation was
used as the latent factors are expected to correlate with each other
6
. Oblimin was selected as the rotation of choice.
Number of factors to retain
Non-graphical solutions to the scree test
7
including parallel analysis, optimal coordinates and acceleration factor was used to
help decide on the appropriate number of factors to retain. The number of factors suggested to retain is 3, 3 and 1
respectively.
The suggested factor solutions were studied but none of them yield any interpretable solution. A more thorough search for an
interpretable solution was conducted for a 4 13 factor structure. A 6 factor solution was eventually adopted as the most
interpretable factor solution yielding the factors Adapting to hearing loss, Support, Education, Healthcare, Policy and
Expectation.
Cross-loadings
Cross-loadings for each item were assessed. A cross-loading difference threshold of less than 0.1 between the 2 highest
factors loading was set as the criteria for removal of items. The solution however had a factor, Expectation, with only 2 items
left after the removal. A decision was then made to move the items to the next factor on which it loaded heaviest on. This
resulted in a new 5 factor solution.
Adjustment of factors to improve interpretability and clinical relevance
Using the new 5 factor solution, changes were further made to it. 6 questions were reassigned to other factors. This was done
to ensure congruence between the meanings of the factors and the questions contained within. This would also improve
interpretability of the factors.
Health and Education
Both the health and education subscales have more than half of the items in the new factors belonging to the old factor. This
implies that these 2 subscales have changed little qualitatively. The new items added to these 2 subscales were most likely due
to the probable attribution to 1 or more of the subscales at the inception of the questionnaire. Factor analysis in this instance
has helped to clarify under which subscale the items would more appropriately belong. Furthermore, the new items are
coherent with the implied meaning of the subscale.
Non-overlapping factors
5 other subscales from the old factor structure have been regrouped into 2 subscales. The reassignments of the subscales help
better define the meaning of each subscale by the new composition of the items and are supported by the confirmatory
analysis.
Conclusion
In conclusion, the PHICE has been revised, reorganised in terms of the subscales composition and the resulting instrument is
deemed to be structurally valid and internally consistent.
References
1. Meinzen-Derr J, Lim LHY, Choo DI, Buyniski S, Wiley S. Pediatric hearing impairment caregiver experience: Impact of
duration of hearing loss on parental stress. International Journal of Pediatric Otorhinolaryngology. 2008;72(11):16931703.
2. Husson F, Josse J. missMDA: Handling missing values with/in multivariate data analysis principal component methods). 2010.
3. R Development Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for
Statistical Computing; 2011. Available at: http://www.R-project.org. Accessed May 1, 2010.
4. Schafer JL. Analysis of Incomplete Multivariate Data. Chapman and Hall/CRC; 1997.
5. Revelle W. psych: Procedures for Psychological, Psychometric, and Personality Research. Evanston, Illinois: Northwestern
University; 2011. Available at: http://personality-project.org/r/psych.manual.pdf.
6. Tabachnick BG, Fidell LS. Using Multivariate Statistics. 5th ed. Allyn & Bacon; 2006.
7. Rache G, Riopel M, Blais J-G. Non Graphical Solutions for the Cattells Scree Test. In: Montral, Canada: Psychometric
Society; 2006.
8. Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives.
Structural Equation Modeling: A Multidisciplinary Journal. 1999;6(1):155.
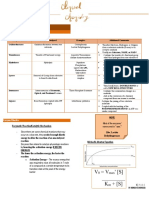
Confirmatory factor analysis
Confirmatory factor analysis was conducted on the
original 8 factor model, the 5 factor model suggested
in the exploratory factor analysis and the modified 5
factor model. Table 3 lists the various goodness-of-fit
indices proposed by Hu & Bentler
8
for assessing
goodness-of-fit indices.
From the various indices, we can see that the original 5
factor solution is a superior fit for the data and fulfils
the criteria set out by Hu & Bentler for a good fit. The
changes made to the 5 factor model increased the
levels of misfits as indicated by the indices. However,
this is a trade-off that has to be made to improve
interpretability. Furthermore, the change between the
original and the modified 5 factor model is deemed to
be minimal.
The confirmatory factor analysis suggests that after
refactoring and reducing the number of items, the new
factor structure is able to better explain the underlying
phenomenon as expressed by the data.
Internal consistency
Cronbachs was computed for the new subscales
within the 5 factor structure to determine its internal
consistency. Both the value for the original and the
modified 5 factor solution was computed as presented
in Table 4. All subscales had an alpha value of more
than 0.73 suggesting good internal consistency. The
change from the original 5 factor solution to the
modified 5 factor solution is also minimal.
Discussion
The factor structure of the original questionnaire has
been changed significantly from an 8 factor structure
to a 5 factor structure with only 3 overlapping factors.
Given the large reassignment of items, it may be
suggested that the new structure could an artefact of
factor analysis and may not be meaningful in clinical
usage. This discussion would look at the overlapping
and non-overlapping factors (Table 6) and explore the
qualitative changes in the reassignment.
Overlapping factors
The overlapping factors are as shown in Table 6. The
table is formulated after removal of items removed in
the new factor structure from the old factor structure.
This allows for a fairer comparison of the changes
made to the new factor structure.
The number of shared items between these shared items
varies between 2 5 items suggesting that qualitatively, the
factors share some similarity.
Support
The support factor expanded from the original 6 items
to the current 12 items. The original support subscale
consisted of items that suggests as direct need for
support such as 10.
3 questions that were removed due to high
cross loadings were reintroduced. This
reintroduction was a result of feedback from
clinicians that these questions were pertinent
to the care of the patient. While these
questions could be scored separately, a
decision was made to group them under
existing factors based on their content after
examining the change in model fit statistics
as presented in the subsequent portions. The
results that were reassigned and reintroduced
are as presented in Table 1. The factor
solution derived is presented in Table 2.
Inadequate support or understanding
from an employer.. The new subscale
support contains items that are less
direct in nature such as 15. Obtaining
special learning materials for my child
(e.g., books, captioned videos).. A close
look at the various items under the new
subscale reveals this difference. This
suggests that support in the context of
caregiver stress may be homogenous,
whether they are direct or indirect.
Potrebbero piacerti anche
- Regulation of Heart RateDocumento30 pagineRegulation of Heart RateTripat Singh67% (3)
- How Do Phagocytes Work in The BodyDocumento2 pagineHow Do Phagocytes Work in The Bodykei04086100% (1)
- MegakaryopoiesisDocumento13 pagineMegakaryopoiesisAezel CruzNessuna valutazione finora
- Basic Principles of HemostasisDocumento5 pagineBasic Principles of HemostasisSean Matthew100% (1)
- Complexometric Titration Lab Report"TITLE "TITLE Redox Titration Pre-Lab QuestionsDocumento4 pagineComplexometric Titration Lab Report"TITLE "TITLE Redox Titration Pre-Lab Questionsbrian batuanNessuna valutazione finora
- VIRO2Documento11 pagineVIRO2AntonyJoseNessuna valutazione finora
- Acute Myeloid Leukemia in Children 2016Documento10 pagineAcute Myeloid Leukemia in Children 2016Jorge Eduardo Espinoza RiosNessuna valutazione finora
- RBC MembraneDocumento41 pagineRBC MembranemwambungupNessuna valutazione finora
- Portfolio Clinical Case Study 3 Lymphoma FinalDocumento27 paginePortfolio Clinical Case Study 3 Lymphoma Finalapi-277136509Nessuna valutazione finora
- Introduction To HaemostasisDocumento18 pagineIntroduction To Haemostasiswatchme3Nessuna valutazione finora
- FerritinDocumento4 pagineFerritinNIGHT tubeNessuna valutazione finora
- Blood Smears and The Use of Wrights StainDocumento5 pagineBlood Smears and The Use of Wrights Stainkaleb16_2Nessuna valutazione finora
- Experiment 3Documento8 pagineExperiment 3Fatimah NazliaNessuna valutazione finora
- Ziehl Neelsen Staining - Principle, Procedure and Interpretations - HowMedDocumento4 pagineZiehl Neelsen Staining - Principle, Procedure and Interpretations - HowMedMeenachi ChidambaramNessuna valutazione finora
- UNIT 3.0 Medical Technology CurriculumDocumento12 pagineUNIT 3.0 Medical Technology CurriculumJean Carmelette BalalloNessuna valutazione finora
- Diagnostic Procedures For Primary HemostasisDocumento2 pagineDiagnostic Procedures For Primary HemostasisAezel CruzNessuna valutazione finora
- Lymphoma Diagnosis BCSH 042010Documento59 pagineLymphoma Diagnosis BCSH 042010DR_Alaa_FakhriNessuna valutazione finora
- Pap Smear: Dr. Monika NemaDocumento114 paginePap Smear: Dr. Monika NemafadoNessuna valutazione finora
- Clinical & Hematological Profile of Anemia Among Male Patients: A Snapshot Study From Tertiary Care Centre of Western IndiaDocumento8 pagineClinical & Hematological Profile of Anemia Among Male Patients: A Snapshot Study From Tertiary Care Centre of Western IndiaIJAR JOURNALNessuna valutazione finora
- Radioimmunoassay (Ria) 3Documento21 pagineRadioimmunoassay (Ria) 3Sapna JainNessuna valutazione finora
- The Philippines Biosafety Guidelines For Contained Use of Genetically Modified OrganismsDocumento186 pagineThe Philippines Biosafety Guidelines For Contained Use of Genetically Modified Organismsvinlava100% (1)
- Antinuclear Antibodies Marker of Diagnosis and Evolution in Autoimmune DiseasesDocumento12 pagineAntinuclear Antibodies Marker of Diagnosis and Evolution in Autoimmune DiseasesFAIZAN KHANNessuna valutazione finora
- Comprehensive Report On Rapid Plasma Reagin Test (RPR)Documento3 pagineComprehensive Report On Rapid Plasma Reagin Test (RPR)Kim RuizNessuna valutazione finora
- AKC Histo Drawings PDFDocumento130 pagineAKC Histo Drawings PDFDanDeleanuNessuna valutazione finora
- Monoclonal Antibody: Engineering and TherapyDocumento39 pagineMonoclonal Antibody: Engineering and TherapyAugusta Rizki AnandaNessuna valutazione finora
- Kirby BauerDocumento1 paginaKirby BauerFighter_ace_97Nessuna valutazione finora
- Medical TechnologistDocumento2 pagineMedical Technologistapi-329932534Nessuna valutazione finora
- Manual and Semiautomatic Hematology TestingDocumento10 pagineManual and Semiautomatic Hematology TestingNathaniel Sim100% (1)
- Performance Rubrics For EtsDocumento2 paginePerformance Rubrics For EtsKim G. SarongNessuna valutazione finora
- Guide to Crossmatch Testing PhasesDocumento4 pagineGuide to Crossmatch Testing PhasesEl Marie SalungaNessuna valutazione finora
- Chapter 18 Anemia HematologyDocumento30 pagineChapter 18 Anemia HematologyYelnats DatsimaNessuna valutazione finora
- MPhil BBS Guide 2020Documento14 pagineMPhil BBS Guide 2020swasahmedNessuna valutazione finora
- Research Paper Writing and Presentation TipsDocumento49 pagineResearch Paper Writing and Presentation TipsAbdul KarimNessuna valutazione finora
- CC Partii&III NotesDocumento30 pagineCC Partii&III NotesAnielle Mongaya100% (1)
- Principles of serodiagnosis techniquesDocumento26 paginePrinciples of serodiagnosis techniquesNipun ShamikaNessuna valutazione finora
- Acid Fast Bacteria: M. Tuberculosis, M. LepraeDocumento22 pagineAcid Fast Bacteria: M. Tuberculosis, M. LepraeelaNessuna valutazione finora
- Rapid Plasma Reagin (RPR)Documento7 pagineRapid Plasma Reagin (RPR)Gakwaya Jules CesarNessuna valutazione finora
- Virology lab diagnosis methodsDocumento31 pagineVirology lab diagnosis methodsjamsthemack100% (1)
- ImmunotechniquesDocumento32 pagineImmunotechniquesKarthik Rajendran100% (2)
- Laboratory Diagnosis of Virus InfectionDocumento14 pagineLaboratory Diagnosis of Virus Infectionherry2swNessuna valutazione finora
- Laboratory Diagnosis of MalariaDocumento6 pagineLaboratory Diagnosis of MalariaRam Sharma PaudelNessuna valutazione finora
- LJ MediaDocumento3 pagineLJ MediaJerry ThompsonNessuna valutazione finora
- Systemic Mycoses: Key Features of Five Fungal PathogensDocumento12 pagineSystemic Mycoses: Key Features of Five Fungal Pathogensdrunken monkeyNessuna valutazione finora
- Count the sperm in the central grid and multiply by 10,000 to obtain the sperm concentration per mLDocumento81 pagineCount the sperm in the central grid and multiply by 10,000 to obtain the sperm concentration per mLAris ResurreccionNessuna valutazione finora
- 6476 Formulation of Alternative Culture Media For Bacterial and Fungal GrowthDocumento6 pagine6476 Formulation of Alternative Culture Media For Bacterial and Fungal GrowthHanief MitsukhaNessuna valutazione finora
- Antinuclear Antibody TestDocumento3 pagineAntinuclear Antibody TestElise Señadoza Aulmo-BarcenasNessuna valutazione finora
- Principles in Medical Laboratory Science 2Documento2 paginePrinciples in Medical Laboratory Science 2lai cruzNessuna valutazione finora
- Gravimetric Analysis: Classical Method of Chemical Analysis Based on Mass MeasurementsDocumento20 pagineGravimetric Analysis: Classical Method of Chemical Analysis Based on Mass MeasurementsLen-Len CobsilenNessuna valutazione finora
- Guide To Pipetting: Third EditionDocumento29 pagineGuide To Pipetting: Third EditionNhật Vy HuyênNessuna valutazione finora
- Activity 2.1 - Manual Pipetting PDFDocumento10 pagineActivity 2.1 - Manual Pipetting PDFno veNessuna valutazione finora
- Solubility, Solubility Product, Precipitation Titration, GravimetryDocumento10 pagineSolubility, Solubility Product, Precipitation Titration, GravimetrySURESH100% (3)
- StainigDocumento38 pagineStainigyuppie_raj2175Nessuna valutazione finora
- BSL Level 1-2 Lab SafetyDocumento30 pagineBSL Level 1-2 Lab SafetyEriani WulandariNessuna valutazione finora
- Mycology: Specimen Collection & HandlingDocumento46 pagineMycology: Specimen Collection & Handlingbetty kassawNessuna valutazione finora
- Chemiluminescence NotesDocumento7 pagineChemiluminescence NotesSavarinathan Maria RayappanNessuna valutazione finora
- Scrub Typhus Clinical StudyDocumento17 pagineScrub Typhus Clinical StudyRajesh PadhiNessuna valutazione finora
- Coombs TestDocumento11 pagineCoombs TestunilabreynosaNessuna valutazione finora
- 68th AACC Annual Scientific Meeting Abstract eBookDa Everand68th AACC Annual Scientific Meeting Abstract eBookNessuna valutazione finora
- The Pyridine Nucleotide CoenzymesDa EverandThe Pyridine Nucleotide CoenzymesJohannes EverseNessuna valutazione finora
- Li - 2011 - TCM's Unverifiable DrawbackDocumento1 paginaLi - 2011 - TCM's Unverifiable DrawbackLiRuijieNessuna valutazione finora
- Li Et Al. - 2014 - Worry About Caregiving Performance: A Confirmatory AnalysisDocumento1 paginaLi Et Al. - 2014 - Worry About Caregiving Performance: A Confirmatory AnalysisLiRuijieNessuna valutazione finora
- Lim Et Al. - 2012 - Validation of The Paediatric Hearing Impairment CADocumento1 paginaLim Et Al. - 2012 - Validation of The Paediatric Hearing Impairment CALiRuijieNessuna valutazione finora
- Lim Et Al. - 2012 - PSS19 Validation of The Paediatric Hearing Impairment Caregiver Experience (PHICE) InstrumentDocumento1 paginaLim Et Al. - 2012 - PSS19 Validation of The Paediatric Hearing Impairment Caregiver Experience (PHICE) InstrumentLiRuijieNessuna valutazione finora
- Li Et Al. - 2013 - Home Safety in Falls Prevention: A Closer Look at The CHEP ProgrammeDocumento57 pagineLi Et Al. - 2013 - Home Safety in Falls Prevention: A Closer Look at The CHEP ProgrammeLiRuijieNessuna valutazione finora
- Ang Et Al. - 2011 - A Projection of Progression of Normal and Impaired Glucose Tolerance To Type 2 Diabetes Mellitus in Singapore Using Markov ModellingDocumento1 paginaAng Et Al. - 2011 - A Projection of Progression of Normal and Impaired Glucose Tolerance To Type 2 Diabetes Mellitus in Singapore Using Markov ModellingLiRuijieNessuna valutazione finora
- Li Et Al. - 2014 - Worry About Caregiving Performance: A Confirmatory AnalysisDocumento37 pagineLi Et Al. - 2014 - Worry About Caregiving Performance: A Confirmatory AnalysisLiRuijieNessuna valutazione finora
- Li Et Al. - 2014 - Refactoring of The SAFER-HOME To Represent The Occupational Context of A PersonDocumento32 pagineLi Et Al. - 2014 - Refactoring of The SAFER-HOME To Represent The Occupational Context of A PersonLiRuijieNessuna valutazione finora
- Lim Et Al. - 2012 - Effectiveness of A Multifaceted Cognitive Training Programme For People With Mild Cognitive Impairment: A One-Group Pre - and Posttest DesignDocumento6 pagineLim Et Al. - 2012 - Effectiveness of A Multifaceted Cognitive Training Programme For People With Mild Cognitive Impairment: A One-Group Pre - and Posttest DesignLiRuijieNessuna valutazione finora
- Li and Liu - 2012 - The Use of Errorless Learning Strategies For Patients With Alzheimer's DiseaseDocumento7 pagineLi and Liu - 2012 - The Use of Errorless Learning Strategies For Patients With Alzheimer's DiseaseLiRuijieNessuna valutazione finora
- Lim Et Al. - 2014 - Validation of The Paediatric Hearing Impairment Caregiver Experience (PHICE) Questionnaire in The Singapore PopulationDocumento9 pagineLim Et Al. - 2014 - Validation of The Paediatric Hearing Impairment Caregiver Experience (PHICE) Questionnaire in The Singapore PopulationLiRuijieNessuna valutazione finora
- Solution Manual For Dosage Calculations A Multi Method Approach 0132158620Documento13 pagineSolution Manual For Dosage Calculations A Multi Method Approach 0132158620RandallValdezypfqw100% (86)
- Formulalrium PanduanDocumento64 pagineFormulalrium Panduananon_939732770Nessuna valutazione finora
- Care Study CAESARIAN SECTIONDocumento29 pagineCare Study CAESARIAN SECTIONNoreen EndinoNessuna valutazione finora
- Star HealthDocumento451 pagineStar Healthsanjay prasadNessuna valutazione finora
- ns3360 Lesson Plans Spring2014Documento11 paginens3360 Lesson Plans Spring2014api-232466940Nessuna valutazione finora
- 7 Day Free Guide PDFDocumento14 pagine7 Day Free Guide PDFGuille RodriguezNessuna valutazione finora
- 837 Institutional 5010 PDFDocumento610 pagine837 Institutional 5010 PDFtrkreddyNessuna valutazione finora
- Geriatric Nursing MidtermDocumento67 pagineGeriatric Nursing MidtermMadeline N. Gerzon100% (2)
- Seminar on Concepts and Foundations of RehabilitationDocumento13 pagineSeminar on Concepts and Foundations of Rehabilitationamitesh_mpthNessuna valutazione finora
- A Client With A Brain Tumor: Nursing Care PlanDocumento1 paginaA Client With A Brain Tumor: Nursing Care Planshabatat2002Nessuna valutazione finora
- A New Drug-Shelf Arrangement For Reducing MedicatiDocumento9 pagineA New Drug-Shelf Arrangement For Reducing MedicatiEmmanuel LawerNessuna valutazione finora
- 3.mechanical VentilationDocumento33 pagine3.mechanical Ventilationisapatrick8126Nessuna valutazione finora
- Pathophysiology of Rheumatic Heart Disease to CardiomegalyDocumento2 paginePathophysiology of Rheumatic Heart Disease to CardiomegalyRj Avila100% (1)
- Eucalyptus The Genus Eucalyptus PDFDocumento433 pagineEucalyptus The Genus Eucalyptus PDFPeter Wilhelmsen100% (5)
- Melanoma Cancer PresentationDocumento13 pagineMelanoma Cancer PresentationMerlyn JeejoNessuna valutazione finora
- DR, OR, WardDocumento14 pagineDR, OR, WardjanNessuna valutazione finora
- Scientific Validation of Urakka Varmam Stimulation With Special Reference To Baroreflex Activation TherapyDocumento5 pagineScientific Validation of Urakka Varmam Stimulation With Special Reference To Baroreflex Activation TherapyMurali SmatNessuna valutazione finora
- Healing Stories of People Final EditingDocumento53 pagineHealing Stories of People Final Editinggabyk6867% (3)
- Antenatal & Postnatal Care: 1. General InformationDocumento7 pagineAntenatal & Postnatal Care: 1. General InformationanishnithaNessuna valutazione finora
- Regulation5362014 Qa enDocumento143 pagineRegulation5362014 Qa enmeiNessuna valutazione finora
- PMLS ReviewerDocumento26 paginePMLS ReviewerEkoy TheRealNessuna valutazione finora
- Stress Dose SteroidsDocumento4 pagineStress Dose SteroidsTitien fitria sholihati100% (1)
- Phobic EncounterDocumento1 paginaPhobic EncounterEmanuel PeraltaNessuna valutazione finora
- 1413272524world10 15 14 PDFDocumento38 pagine1413272524world10 15 14 PDFCoolerAdsNessuna valutazione finora
- Chest X-RayDocumento125 pagineChest X-RayRusda Syawie100% (1)
- PR Menarini PDX Ab RBCDocumento2 paginePR Menarini PDX Ab RBCvyasakandarpNessuna valutazione finora
- CAE-UOE Part1Documento4 pagineCAE-UOE Part1nikitsaNessuna valutazione finora
- Rubbing Alcohol BrochureDocumento2 pagineRubbing Alcohol BrochureShabab HuqNessuna valutazione finora
- HAADStatisticsEng2013 PDFDocumento91 pagineHAADStatisticsEng2013 PDFHitesh MotwaniiNessuna valutazione finora