Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Pain Needs Painkillers
Caricato da
dominscience10 valutazioniIl 0% ha trovato utile questo documento (0 voti)
16 visualizzazioni3 pagineOverprescribing of opioid painkillers has caused harm to many people. Problems include addiction, loss of social functioning and death. There is lack of evidence of effectiveness for opiates in chronic pain.
Descrizione originale:
Titolo originale
Pain needs painkillers.doc
Copyright
© © All Rights Reserved
Formati disponibili
DOC, PDF, TXT o leggi online da Scribd
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoOverprescribing of opioid painkillers has caused harm to many people. Problems include addiction, loss of social functioning and death. There is lack of evidence of effectiveness for opiates in chronic pain.
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato DOC, PDF, TXT o leggi online su Scribd
0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
16 visualizzazioni3 paginePain Needs Painkillers
Caricato da
dominscience1Overprescribing of opioid painkillers has caused harm to many people. Problems include addiction, loss of social functioning and death. There is lack of evidence of effectiveness for opiates in chronic pain.
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato DOC, PDF, TXT o leggi online su Scribd
Sei sulla pagina 1di 3
Pain needs painkillers right?
Overprescribing of opioid painkillers has caused harm to many people. Problems
include addiction, loss of social functioning and increasingly, though still relatively
uncommonly in the UK, to death.
Concerns have been raised about deaths associated with tramadol in particular. Ive
written before about the lack of evidence of effectiveness for opiates in chronic pain,
but it is hard for clinicians to resist the slippery slope of initiating and then increasing
opioid strength or dose when faced with a patient reporting pain. !here is an e"pectation
that pain needs painkillers # there is arguably a culture of prescribing opiates for
chronic pain. $ut thats %ust common sense # right&
Warnings
'ets not be so fast. (ecently pain specialists and neurologists have become more vocal
about warning against prescribing for chronic non)cancer pain. !he *merican *cademy
of +eurology has %ust issued a review and position paper on the sub%ect written by ,r
-ary .ranklin of the University of /ashington.
!he driver behind the initiative is the 011,111 *mericans who have died, directly or
indirectly, from prescribed opiates in the U2 since the late 0331s. !his is more than died
from (!*s and firearms. !his is far more than the number of U2 military personnel
who died in the 4ietnam war. It truly is an epidemic # a national tragedy # and it looks
like it is one which could have been avoided or one that could at least be ameliorated. It
is one that is caused by non)evidence based prescribing.
Diversion
,iversion and inappropriate use of opioids is a problem. !he paper illustrates the point5
In one population)based study in Ontario, Canada, of all deaths attributable to opioids
during 6117#6118, 9: of patients had died from opioids diverted from friends or
family, and 03: had inappropriately self)administered ;e.g., inhaled, in%ected<. * greater
proportion of deaths may be associated with diversion in rural states.
Risk to benefit balance
!he effectiveness of opiods in chronic pain is uncertain and this is, as the paper
graphically illustrates, grossly outbalanced by the down sides5
=ortality
Overdose morbidity
2erious adverse events
,ependence>*ddiction
'ifelong disability
'oss of family and community
Recommendations
!he paper makes some clear best)practice recommendations which Ill paraphrase5
0. ?ave an agreement with the patient at the outset that identifies the risks and
outlines the patients responsibilities
6. Identify current or past substance misuse
@. Identify risk of depression
A. Use urine to"icology prudently ;identify diversion or misuse of other
substances<. 2creen before starting.
B. Use tools to track pain and function and monitor tolerance
7. !rack the amount of opioids used daily) converted to the eCuivalent dose of
morphine ;=D,<
9. -et further help if the =D, reaches 81)011mg and there is no significant pain
improvement.
8. Use a programme available in most states to monitor Eall sources of controlled
substances.
A different approach to pain
!hese recommendations are solid though I would have liked them to include something
that is mentioned elsewhere in the paper # to address pain in a holistic way. /hy is pain
always seen as something to be instantly medicated, solved by a pill& Pain is a comple"
symptom with biological, psychological and social influences. .ranklin writes5
In addition payers need to offer adeCuate payment incentives for treatment alternatives
to the opioid prescription for acute, subacute, and chronic pain. Cognitive#behavioral
therapy, structured e"ercise, spinal manipulation, and interdisciplinary rehabilitation,
although proven to be moderately effective in treating subacute and chronic low back
pain, are often either not available or not adeCuately funded.
* collaborative care model for the care of patients with chronic pain, not unlike similar
models aimed at chronic disease management of diabetes and other con) ditions, should
be a crucial element in the evolving health care reform environment.
The conclusion?
It seems likely that, in the long run, the use of opioids chronically for most routine
conditions, such as chronic low back pain, chronic headaches, or fibromyalgia, will not
prove to be worth the risk.
*nd the risk for those with a vulnerability to addiction is significant. Prescribing for
pain is a common route of entry into opioid addiction.
Prescribers and patients
$ut we have a lot of work to do to change the prevailing culture. !ime =agaFine picked
up on this paper in a recent article. !hey highlight the challenges around changing the
culture of prescribers5
In 611@, ,r. Gane $allantyne and ,r. Gianren =ao, then at =assachusetts -eneral
?ospital and ?arvard =edical 2chool, published a review of the e"isting data on opioid
use for chronic pain in the New England Journal of Medicine. It was among the first
studies to highlight the fact that the skyrocketing number of prescriptions was doing
little to actually reduce reports of chronic pain.
H!he real problem is physicians who are practicing with the best intentions and not
understanding what the limited role of opiates is,I says $allantyne, now a professor of
anesthesiology and pain medicine at the University of /ashington. H.or 61 years they
have been taught that everybody deserves an opiate, because they really dont know
what else to do. Its a cultural thing and its hard to reverse that.I
In the !ime feature $allantyne continues5
HIn this country we e"pect everything to be fi"ed, and that doctors have the answer and
can take pain awayJ /e shouldnt be resorting to pills as a first resortK they should
very much be a last resortI
.ranklin, -. ;610A<. Opioids for chronic noncancer pain5 * position paper of the
*merican *cademy of +eurology Neurology, 83 ;0A<, 0699)068A ,OI5
Potrebbero piacerti anche
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
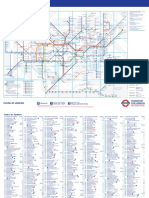
- Standard Tube MapDocumento2 pagineStandard Tube MapBenjamin Zari IIINessuna valutazione finora
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Hines Chaps 1 5 6 10 11Documento19 pagineHines Chaps 1 5 6 10 11dominscience1Nessuna valutazione finora
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Canterbury PDFDocumento1 paginaCanterbury PDFdominscience1Nessuna valutazione finora
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Cognitive PsychologyDocumento10 pagineCognitive Psychologydominscience1Nessuna valutazione finora
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Hansen, G - Deception in PSI ResearchDocumento57 pagineHansen, G - Deception in PSI Researchdominscience1Nessuna valutazione finora
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Moller, L - Pseudoscience or ProtoscienceDocumento3 pagineMoller, L - Pseudoscience or Protosciencedominscience1Nessuna valutazione finora
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Moller, L - Pseudoscience or ProtoscienceDocumento3 pagineMoller, L - Pseudoscience or Protosciencedominscience1Nessuna valutazione finora
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Hansen, G - Deception in PSI ResearchDocumento57 pagineHansen, G - Deception in PSI Researchdominscience1Nessuna valutazione finora
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- DialoguesClinNeurosci 9 173Documento17 pagineDialoguesClinNeurosci 9 173dominscience1Nessuna valutazione finora
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- Cognitive PsychologyDocumento10 pagineCognitive Psychologydominscience1Nessuna valutazione finora
- Reader, C - Khufu Knew The SphinxDocumento19 pagineReader, C - Khufu Knew The Sphinxdominscience1Nessuna valutazione finora
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Cognitive PsychologyDocumento10 pagineCognitive Psychologydominscience1Nessuna valutazione finora
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Spirit Slate Writing and Kindred PhenomenaDocumento89 pagineSpirit Slate Writing and Kindred Phenomenadominscience1Nessuna valutazione finora
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Playing Ground PartIDocumento3 pagineThe Playing Ground PartIdominscience1Nessuna valutazione finora
- Did A Five-Day Camp Without Digital Devices Really Boost Children's Interpersonal Skills?Documento2 pagineDid A Five-Day Camp Without Digital Devices Really Boost Children's Interpersonal Skills?dominscience1Nessuna valutazione finora
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Breaking ResearchDocumento2 pagineBreaking Researchdominscience1Nessuna valutazione finora
- Using "Programmable" Antibiotics To Attack Drug-Resistant MicrobesDocumento3 pagineUsing "Programmable" Antibiotics To Attack Drug-Resistant Microbesdominscience1Nessuna valutazione finora
- The Playing Ground PartDocumento3 pagineThe Playing Ground Partdominscience1Nessuna valutazione finora
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- Tricksy Insects Sing A Song of Love andDocumento2 pagineTricksy Insects Sing A Song of Love anddominscience1Nessuna valutazione finora
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Neurobiological Basis of A HumanDocumento3 pagineThe Neurobiological Basis of A Humandominscience1Nessuna valutazione finora
- Sleeping Brains Understand WordsDocumento2 pagineSleeping Brains Understand Wordsdominscience1Nessuna valutazione finora
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- The GutDocumento2 pagineThe Gutdominscience1Nessuna valutazione finora
- Epidural AnalgesiaDocumento16 pagineEpidural AnalgesiaspreeasNessuna valutazione finora
- MCQ AnaesthesiaDocumento15 pagineMCQ AnaesthesiaProf-Ashraf Emara100% (2)
- Evaluation and Management of Pain in ChildrenDocumento13 pagineEvaluation and Management of Pain in ChildrenOlga MoţpanNessuna valutazione finora
- Jex Review Center Marathon in Criminal Detection and InvestigationDocumento4 pagineJex Review Center Marathon in Criminal Detection and InvestigationArnel Sali-otNessuna valutazione finora
- PharmacologyAnesthesiology RevalidaDocumento166 paginePharmacologyAnesthesiology RevalidaKENT DANIEL SEGUBIENSE100% (1)
- Anes 8 Introduction To Pain ManagementDocumento4 pagineAnes 8 Introduction To Pain ManagementJanica Marie RagsacNessuna valutazione finora
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- GP MCQ 11Documento4 pagineGP MCQ 11Marta MoreiraNessuna valutazione finora
- Xylazine-Involved Overdose Deaths FINAL - 3.8.23Documento5 pagineXylazine-Involved Overdose Deaths FINAL - 3.8.23ActionNewsJaxNessuna valutazione finora
- TCCC Guidelines For Medical Personnel 150603Documento14 pagineTCCC Guidelines For Medical Personnel 150603Vitor Hugo G CorreiaNessuna valutazione finora
- Acute Post-Surgical Pain Management: A Critical Appraisal of Current PracticeDocumento42 pagineAcute Post-Surgical Pain Management: A Critical Appraisal of Current PracticeMmenyeneNessuna valutazione finora
- Drug Study ShenDocumento12 pagineDrug Study ShenLass KazeNessuna valutazione finora
- Case AppendicitisDocumento112 pagineCase AppendicitisChen CobainNessuna valutazione finora
- Summativeassessment 3Documento11 pagineSummativeassessment 3api-522946517Nessuna valutazione finora
- 1756 9966 29 67Documento6 pagine1756 9966 29 67Yogha RyanandaNessuna valutazione finora
- 1 s2.0 S0898656821000693 MainDocumento4 pagine1 s2.0 S0898656821000693 MainLívia MeloNessuna valutazione finora
- Generic Name: Frequent (10%) Baseline Assessment Antiemetic (Assess Intervention/EvaluationDocumento11 pagineGeneric Name: Frequent (10%) Baseline Assessment Antiemetic (Assess Intervention/EvaluationIrene Soriano BayubayNessuna valutazione finora
- Rusan Pharma Product ListDocumento4 pagineRusan Pharma Product ListSanjay SharmaNessuna valutazione finora
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- DS - DutyDocumento19 pagineDS - DutyMarie Kelsey Acena MacaraigNessuna valutazione finora
- Drug TraffickingDocumento20 pagineDrug TraffickingUsman Ahmad TijjaniNessuna valutazione finora
- Concise Guide To Medicine & Drugs, 7th Edition by DKDocumento498 pagineConcise Guide To Medicine & Drugs, 7th Edition by DKJosh MNessuna valutazione finora
- S 006 LBLDocumento21 pagineS 006 LBLEko YuliantoNessuna valutazione finora
- ZOMORPH Capsules 10mgDocumento6 pagineZOMORPH Capsules 10mgFlorexan Malanday PasonNessuna valutazione finora
- Artigo Produtos NaturaisDocumento39 pagineArtigo Produtos NaturaisMillygoNessuna valutazione finora
- Hridae Walia Interaction Design Portfolio PDFDocumento114 pagineHridae Walia Interaction Design Portfolio PDFHridae WaliaNessuna valutazione finora
- Pollice Et Al 2008 Severe Tramadol Addiction in A 61 Year Old Woman Without A History of Substance AbuseDocumento2 paginePollice Et Al 2008 Severe Tramadol Addiction in A 61 Year Old Woman Without A History of Substance Abusefernyz2886Nessuna valutazione finora
- Pain Management JournalDocumento7 paginePain Management JournalPengurus Pusat HipgabiNessuna valutazione finora
- Concept Of: (The Fifth Vital Sign)Documento43 pagineConcept Of: (The Fifth Vital Sign)Mae DacerNessuna valutazione finora
- What Are Drug ClassificationsDocumento5 pagineWhat Are Drug ClassificationsCarl LewisNessuna valutazione finora
- MRQ Base For Final Exam PreparationsDocumento29 pagineMRQ Base For Final Exam PreparationssushmitaNessuna valutazione finora
- Pharmacology NotesDocumento30 paginePharmacology NotesJessica WalkerNessuna valutazione finora
- The Obesity Code: Unlocking the Secrets of Weight LossDa EverandThe Obesity Code: Unlocking the Secrets of Weight LossValutazione: 4 su 5 stelle4/5 (6)
- The Age of Magical Overthinking: Notes on Modern IrrationalityDa EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityValutazione: 4 su 5 stelle4/5 (28)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsDa EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNessuna valutazione finora