Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Nursing Management of The Perioperative Patient
Caricato da
ashdmb2170 valutazioniIl 0% ha trovato utile questo documento (0 voti)
228 visualizzazioni16 pagineNursing Notes
Titolo originale
Nursing Management of the Perioperative Patient
Copyright
© © All Rights Reserved
Formati disponibili
DOCX, PDF, TXT o leggi online da Scribd
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoNursing Notes
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato DOCX, PDF, TXT o leggi online su Scribd
0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
228 visualizzazioni16 pagineNursing Management of The Perioperative Patient
Caricato da
ashdmb217Nursing Notes
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato DOCX, PDF, TXT o leggi online su Scribd
Sei sulla pagina 1di 16
1
NURSING MANAGEMENT OF THE PERIOPERATIVE PATIENT
1. INTRODUCTION
Surgery is an important/expensive area of the Hospital.
Consumes more than the supplies
5 or 6 care givers to 1 patient
How many have had surgery before (including childbirth - although that is more
like emergency than planned surgery)?
Depersonalizing experience
It helps if youve had surgery to focus on some important questions.
o What do our clients expect of us (and how can we provide it in "best" way
possible - cheapest, and most compassionate)?
o How are care givers seen by patients?
o How do care givers think of patients ("is it ready yet?")?
References
http://www.aorn.org Association of OR Nurses
http://www.aana.com American Association of Nurse Anesthetists
http://www.miana.org Michigan Association of Nurse Anesthetists
http://www.asahq.org American Society of Anesthesiologists
http://www.gasnet.org GasNet
http://www.gasnet.org/apsf/ Anesthesia Patient Safety Foundation
http://www.udmercy.edu/crna/ UDM Nurse Anesthesia
http://www.rxlist.com online drug information
Definitions
A perioperative nurse is defined as the registered nurse who, using the nursing process,
designs, coordinates, and delivers care to meet the identified needs of clients whose protective
reflexes or self-care abilities are potentially compromised because they are under the influence of
anesthesia during operative or other invasive procedures. To do his effectively, must understand
the history and physical assessment, pathophysiology, and lab tests; the nature of the planned
procedure; the individual patients likely responses to stress; and the potential risks and
complications of the surgical procedure. Closely fits Roys Self-Care Deficit model.
Invasive Procedures Body is entered by an instrument or device (e.g., a scalpel, tube) or by
ionizing or non-ionizing radiation, and in which protective reflexes or self-care abilities are
potentially compromised.
Standards of practice
Association of Operating Room Nurses (AORN)
American Nurses Association (ANA)
American Association of Nurse Anesthetists (AANA)
American Society for PeriAnesthesia Nursing (ASPAN)
External agencies: State Boards, Amer College of Surgeons, ASA, JCAHO
2
Classification Of Surgery
Major and minor surgery
Major- gen anesth, may be life-threatening
Minor- low risk, outpt, or local/sed
Types of surgery
By purpose of surgery (diagnosis, cure, cosmetic, palliative, prevention,
exploration)
By surgeons specialty
By what type of procedure is being done ie plasty, rraphy otomy etc
Urgency of surgery
Emergency vs scheduled
Settings
Inpatient
o Operating rooms
o Outside the ORRadiology, Labor & Delivery, Endoscopy, ER
Outpatient "ambulatory"
o Hospital outpatient surgery unit, freestanding ambulatory surgery clinic,
doctors office
o General, regional or local anesthesia
o Usually surgery takes < 2 hours
o Usually < 3 hours needed in post-anesthesia care unit (PACU)
o No overnight stay required (for pain control, fluid management, watching
for complications)
3
2. PSYCHOSOCIAL REACTIONS TO SURGERY
Stress Surgery is a stressor in all areas of functioning, physiologic and psychologic.
Preoperative Anxiety is a normal adaptive response
Mild to marked: may be expressed as fear. Pt needs help to decrease anxiety:
o Establish rapport to decrease feelings of depersonalization.
o Humor (sometimes)
o Explain the preoperative and postoperative nursing care to decrease fear
of the unknown.
o Explain that anxiety is a normal reaction.
o Enlist patients active participation in learning and practicing postoperative
activities to give control over the environment.
o When teaching include family and significant other to promote support.
Fear Of The Unknown:
o Patient enters an environment in which they have very little control. Need
to promote an atmosphere where they are free to ask questions.
"Discharge teaching" starts the moment they are admitted to decrease this
problem. Also give them as much control as possible- "Would you like the
IV on your right or your left?"
o Nursing interventions are aimed at decreasing fear of the unknown and
alleviating anxiety.
Coordinate information since patient is frequently not comfortable
asking the surgeon questions. If nurse is unable to answer the
question, they must secure the information for the patient.
Avoid additional anxiety and not give too much information.
Sometimes avoidance is the best defense mechanism.
Other fears
o Pain: pain is common after surgery and fear is common. Chemical
substances are released and nerve endings are stimulated which cause
pain, ischemia and distension.
o Death: psychologic threat of death may be just as frightening for someone
with major, as well as minor, surgery. "If you see a light, dont go towards
it"
o Anesthesia: afraid of what they may disclose, awakening during surgery or
not awakening after. Allay their fears, anything said is confidential, but
rarely say anything (too sleepy).
o Disfigurement and alerted sexuality: almost all surgery will cause some
alteration in body image. If self-perception is affected, patient will
experience a grief reaction.
o Separation and change in roles: feel support systems have lessened.
Finances, income, insurance coverage. Not just meneveryone has an
accustomed role, and they are used to doing for themselves. It may be
4
frustrating, painful, embarrassing etc to have others help. Try social work
consult, or expanded visiting hours for family.
3. PATIENT INTERVIEW / PREOP ASSESSMENT
Purposes: Obtain patient information, Give information, and Get consent. Also
allows assessment of emotional state and expectations. Careful assessment is
necessary in order to prevent operative complications and alert nurse to
postoperative care needs.
History and physical exam (in progress notes, or H&P faxed or brought in by
surgeon from his office) must be completed by the physician, reviewed by the
nurse, and a separate nursing assessment must be completed. Nursing
assessment is holistic - baseline data - identify potential problems. Use lay terms
in your questioning. Annesthesia preop assessment usually in the chart as well.
Vital Signs
Preoperative and baseline. Reveal abnormalities and establish norms.
Past surgical history
Generally, also previous bad outcomes or distressing experiences
Also ask what type anesthesia they have had.
Allergies
Need to be questioned about any allergies to medications, foods, substances.
Clearly identify any allergies on the front of the chart. In OR, must be alert to any
allergic responses since patient will not be able to advocate for self.
In OR, particularly concerned with allergies to tape, latex, iodine.
Distinguish between allergies and adverse reactions. "Garlic onions, and hot
peppers give me indigestion"
Nutritional State
Patients who are healthy will recover better than individual not in homeostasis.
Need to assess nutritional state (ideal body weight, loss of SQ fat, edema,
lymphocyte count, serum albumin).
Protein is essential for tissue repair. CHO provides the necessary energy for
tissue repair. Vitamins necessary (Vit B maintains GI function, Vit C promotes
wound healing and collagen formation, Vit K promotes clotting)
Body Weight
Most are weighed before surgery (basis for anesthetic drug dose)
5
Obesity: more complicated. Increased potential for dehiscence and evisceration,
wound infection. Takes more anesthesia & stored in adipose delaying excretion.
More post-op complications - respiratory, ambulation
Underweight: lack of protein stores. Diet high in PRO, CHO, VIT.
Fluid / Electrolyte Balance
Correction of any imbalance is essential. Patients prone to hypovolemia:
diarrhea, vomiting, bleeding, insufficient fluid intake, GI bleed. Need to assess for
dehydration (skin turgor, mucous membranes, I/O)
Hypervolemia: renal failure, CHF, malnutrition.
Lytes: NA, K, CL, CA, MG. (BUN, Creat for kidney function)
"Routine bloodwork" concept is giving way to minimal labs based on complexity
of procedure and findings in H&P.
Infections
Unless the reason for surgery is an infection (I and D), then surgery will always
be rescheduled if evidence of infection. Assessment, temperature, WBC.
Habits Affecting Anesthesia
ETOH: may delay detoxification by the liver. In addition, withdrawal
postoperatively and malnutrition
Smoker: increase respiratory problems, increase in platelet aggregation and
ahesiveness.
Street Drugs
Chronic Illness
Chronic illness can complicate the postoperative phase
Respiratory (COPD): increase pneumonia, decrease ability to exchange CO
2
and
O
2
Asthma - intraop bronchospasm
Cardiac disease: prosthetic valves increases post op inflammatory process and
potential for infection. PVD impairs tissue and wound healing. Increase risk for
thrombophlebitis
Hematologic disorders: risk of hemorrhage with clotting disorders. Anemia can
compound the surgical loss of blood leading to hypovolemia/shock.
Endocrine disorders: DM may experience hypo/hyperglycemia during the surgical
period. Increase risk of infection, silent MI, peripheral nerve injury, difficult
intubation. Other endocrine disorders can alter the stress response (thyroid,
pheochromocytoma).
Neurological disorders: neuro assessment provides a baseline for post operative.
Incorporate care of chronic neurological disorder into care.
6
GI disorders: adequate liver function is necessary for the detoxification of drugs.
(Hx of PUD, constipation)
Renal disorders: kidneys responsible for excretion of waste and maintenance of
fluid and electrolyte balance. If CRF then need careful assessment of preop: I &
O, specific gravity of urine, and adequate fluid intake.
Musculoskeletal disorders: ROM
Integumentary Status: pressure ulcers from immobility
Drug History: Prescription as well as OTC usage
antibiotics: combine with curare to prolong apnea.
Valvular disease or prosthesis may need antibx prophylaxis (search
http://www.americanheart.org/ ) for Guidelines for the Management of Patients
With Valvular Heart Disease: Executive Summary, Document 1998;71-0154
anticoagulants: increase bleeding time
diuretics: hypokalemia
steroids: decrease adrenal function
aspirin: decreased platelet aggregation
tranquilizers: hypotension and shock
Note: anti-htn medications usually continued through the am of surgery (this used
to be avoided fearing hypotension, now done to promote control without as many
oscillations)
Diagnostic Studies:
Ideally, do only those tests felt necessary based on H&P. No test should be
gotten "for Anesthesia". Not all situations require the same tests.
Several are common: CBC, UA, PT, PTT, ECG, CXR.
Need HCG for all of childbearing age (unless PSH of hysterectomy or tubal ligation)
4. NURSING MANAGEMENT PREOP
Preoperative Teaching
Instruction is essential. Research demonstrates that those who are informed will have
better recovery. Best time to teach is the afternoon or evening before surgery.
Challenging when most are same day admits - even carotids or heart surgery. Important
because it decreases anxiety, influences recovery, promotes patient satisfaction.
General Principles of Preop teaching
1. Some things everyone having surgery has to know
7
2. Reinforce what the patient has been told about surgery. Find out patients
understanding of procedure first. Know enough basic information about common
procedures to anticipate and answer the common questions.
3. Balance telling too little vs too much
4. Avoid anxiety producing words -- "pain" (discomfort)
5. Include family members, if possible
6. Have the patient explain, give return demonstrations
7. Prepare for situations (cold, bright light, never left alone)
Patient Teaching About Postoperative Care
1. Therapeutic devices: indwelling catheter, n/g tube, chest tube
2. Medications for Pain: assured that medication will be available, PCA devices.
3. Postoperative self-care procedures: C & DB, splinting, leg exercises, turning
4. Ambulation- dont bound OOB, dont do a sit up, sit at BS for a moment to check
dizziness
Preop legal preparationthe Operative Permit
It is the surgeons responsibility to explain the surgical procedure, alternatives,
risks, and benefits. Purpose is to ensure the patient is not undergoing a
procedure without informed consent. Helps protect from liability. Adults must be
oriented and not under sedation in order to sign. May take a telephone consent.
Consent is witnessed - that is a witness to the signature.
Related legal and ethical implications.
o Distinguish between paper form and Informed Consent itself.
o What to do if theyre not A&O x 3? How is mental competence
determined?
o Who can sign for a patient (on their behalf)?
o When can surgery be performed in the absence of a signed consent?
o What about children and emancipated minors?
DNRs are on hold while the patient is in the OR
Another related issue is living wills and advance directives.
Important to follow institutional policy regarding site markings
Registered nurse or other healthcare professional responsible for calling time
out to verify patient, procedure, professionals present
Day of surgery preparation
Physical Preparation
8
Nursing responsibilities: orders carried out, final preparations done, records
complete and accompany patient to OR.
Perhaps admitted the evening before. But more trend toward same day
admission.
Diet: Regular light diet. Full liquids in some instances. NPO after midnight (allow
time for the stomach to empty, decrease aspiration) or at least 4-8 hours.
In some cases, if the patient is on a beta-blocker or other hypertension
medications, they will be allowed to take them with small sips of water the
morning of surgery. Check with surgeon if unclear
Skin Preparation: decrease bacteria to a minimum. Mild antiseptic soap and
water the night or day before. Hibiclens scrubs may be given to the patient to
scrub for two days prior to the surgery. Shaving is left to moments before
incision.
Bowel Preparation: type of surgery determines the need for a bowel prep. Enema
or laxative may be administered to permit visualization of the colon and decrease
chance of infection when bowel is resected.
Medications Table
Sedative to ensure adequate rest and to decrease anxiety (midazolam, diazepam,
lorazepam). Preanesthetic agent may be given 30 minutes to 1 hour before surgery to
promote sleep and relaxation. No consent if sedated-- get it signed before giving. Also,
void before giving.
1. Sedatives: decrease the anxiety ie benzodiazepines, barbiturates
2. Narcotic analgesic: reduce the amount of anesthetic needed. Given 30 minutes
to 1 hour before sx, often IM
3. Anticholinergic: reduce secretions. Also cause dry mouth and dilatation of the
pupils. (Atropine or Robinul).
4. Tranquilizer: may be given instead of a narcotic, especially to the elderly. (Valium
or Phenergan).
Note Example of 2,3,4 combined as Demerol-Vistaril-Atropine.
Note Also expect Antibiotics (given within the 1 hr prior to incision).
Note common to see anti-aspiration meds ie Bicitra, Reglan, ranitidine
o Musts: SR up after medication given "Its not fair to leave the SR up, and
the call bell out of reach"
o OOB with help only
o VS before the preop injection (consent signed, etc.)
o Remove dentures, jewelry, contacts, glasses, hearing aids, etc. (In some
cases they may take their hearing aids with them)
Information for the family
9
What time the procedure will be done, how long it will take, that the physician will
communicate progression and recovery until out of anesthetic agent.
Preoperative Checklist / Transportation to the OR
Nursing responsibility to see that the checklist is completed--important, shows that the
patient is ready for transfer to the OR. Unusual observations and abnormal labs are
reported to the physician. "If you want to take care of the patient, take care of the
paperwork"
NPO 6 - 8 hours adults, less for the very tiny. This time frame also depends on
NPO before ALL types of anesthesia. Explain reasons for restriction and
importance, inform other caretakers, dont leave pitcher at bedside. Clear liquid
breakfast may be ok if afternoon surgery
Signed OR Consent
Current history and physical (the surgeons, as opposed to your nsg assessment
and anesthesia assessment)
Completion of physical preparation
VS
Void on call
Prostheses, contacts, dental work etc.
Valuables and their disposition-Make them take rings off! Its not because were
crooks. Its an electrical safety issue.
Recording of preop medication
ID band in proper order
Dont need to remove makeup or nail polish. The text says "Take them off"but
dont worry about cosmetics or nails.
Jewelry should NOT be wornno exceptions (electrical safety hazard in addition
to risk of loss).
10
5. THE INTRAOPERATIVE PHASE
Introduction
Transfer to surgery (preop hold or direct to OR room). Floor RN checks chart and
makes certain the patient is correctly identified ("What is your name?"). Will be
transferred to the OR on a gurney. Family is given instructions.
In holding area, final surgical preparations are made. Preop Hold RN repeats
checks, abdominal prep. prn, IV.
The players & their roles in surgery
Surgeon 1:1 MD or DO
Anesthesiologist 1:1 only if acute. 1:2 to 1:4 the usual, serves as resource and
supervises care in several rooms. MD or DO
Nurse anesthetist CRNA = Certified Registered Nurse Anesthetist 1:1. Directly
provides anesthesia care. Trained to function independently or as team member
with anesthesiologist. Masters prepared advanced-practice nurse.
Circulating nurse 1:1 almost always RN. Manages environment, gopher, protect pt
Scrub nurse 1:1 RN, LPN, SA, Tech. In sterile field, hands tools to surgeon
Anesthesia
Anesthesiologist will visit patient prior or a few days before the procedure
Review of systems, medications, allergies will be discussed
11
Types of anesthesia
Conscious sedation
AKA "local/sed" or "twilight"
Patient is conscious with some alteration of mood
Airway protective reflexes remain intact (gag, cough)
Often combined with local (topical, infiltration, or nerve block) or regional
anesthesia.
Regional Anesthesia
Anesthesia to a body region (as opposed to blocking a single nerve).
Accomplished by injecting local anesthetics near a nerve
Types include: spinal, epidural, axillary block, retrobulbar etc
These patients are conscious and need emotional support; they generally receive
sedation
They need help to maintain position
Check for urinary retention after spinal
Epidural
General anesthesia
Induced by an IV barbiturate and maintained with inhalation agents. Emergence
an active process
Anesthesia machine is used to dispense anesthesia and oxygen. Gases will be
delivered through a gas mask or ET tube (inserted after asleep).
Components:
o Hypnosis (implying amnesia & unconsciousness)
o Reflex suppression
o Analgesia
o Skeletal muscle relaxation
Wound Closure
Contaminated wounds are left open to heal. Otherwise closed in layers.
Sutures: absorbable or non- absorbable - require removal
Sterile adhesive strips
Staples: usually in the sternum, transapically other other sites
12
Retention sutures (provides a secondary suture which relieves undue strain on
the suture line. Suture is passed through a small tube or over a plastic bridge that
is placed on the skin.
Staples: reduces edema and inflammation because manipulation and handling
has been reduced.
6. NURSING MANAGEMENT OF THE POSTOPERATIVE PATIENT
Transfer to Recovery Room (PACU)
Two stressors the patient is recovering from: surgery and anesthesia.
After the surgery is completed and dressing applied, the patients endotracheal
tube is removed. Transferred to recovery room by circulating nurse and CRNA.
Those who do not go to PACU include surgery under local (they can go straight
home or to Phase II) and those going directly to critical care area.
Close observation. 1:1 or 1:2. Standard and emergency equipment are present.
Almost all receive oxygen
Monitoring is individualized to patient need and type of surgery. Continuous, then
up to q15m: EKG, NIBP, pulse oximetry, Intake & output
All preop orders are discontinued postop, rewritten in PACU (vitals, position,
medications, IV, type of PO intake, activity, diagnostic tests, dressing changes).
Immediate postoperative complications "ABC"
Airway obstruction
Causes: effects of anesthestics, effects of narcotics given intraop or postop,
secretions, swelling from a surgical site in the neck
S/S: snoring respirations, "rocking boat", apnea
Treatment: stimulation, chin lift, jaw thrust, nasal or oral airways, reintubation,
mechanical ventilation
Breathing: Respiratory insufficiency
Causes- see above
S/S: shallow respirations, restlessness or other signs of hypoxemia, ABGs, pulse
oximetry < 90%
Treatment: as above
Circulation
Causes: Internal hemorrhage: occur from insecure sutures, erosion of a vessel.
S/S: rapid, deep respirations, rapid thready pulse, hypotension with narrow pulse
pressure, cool, moist, pale skin, restlessness, faintness, dizziness, thirst.
13
Treatment: flat, pressure, IV, blood.
Shock
o Cause: decreased perfusion of tissues. Hemorrhage, trauma, anesthesia,
pooling, or anaphylactic shock.
o Treatment: Change position slowly, avoid Fowlers, raise legs
Hypothermia; Pain; Nausea and vomiting
Neurological problems (delayed emergence, delirium, problems related to the
surgery type i.e. carotid endarterectomy vs lumbar laminectomy)
Transfer to floor
Ready to be discharged to the floor once
patent airway with sufficient ventilation
stable vital signs
normal movement
improving LOC
responds to questions
Admitting the patient to the general nursing unit Nursing Care Plan
Postop care includes:
Immediate rapid assessment, then review all systems
VS and assessments every 15 minutes x4, q30m x 4, q1hrx4, q4h until 24 hrs
has elapsed.
Temperature/Infection. Dont change first dressing, thats the surgeons
prerogative. Reinforce only.
Fluid intake/output (usually until oral intake reestablished)
Safety: ready equipment, raise side rails, call bell, assist OOB, etc.
Comfort and rest
Pulmonary C&DB, early ambulation
Drains are soft rubber tubular structures placed in wounds to
remove fluid (blood, pus)
prevent deep wound infections in areas that may contain purulent material
obliterate dead spaces
Types
o Penrose: open gravity drain. Safety pin placed on the external end of
these drains to prevent them from sliding back into the wound. Usually
14
inserted into a nearby stab wound rather than the surgical wound to allow
the surgical wound to heal properly.
o Perforated catheter and the proximal end is placed into a closed portable
suction device which creates gentle constant suction.
o Hemovac: collapsible collection device. Creates negative pressure to
create suction.
o Jackson Pratt: small reservoir bulb where fluid collects. After emptied it is
compressed and the spout closed to create negative pressure.
Complications Related To Surgery
Stress can cause serious complications and nursing care is aimed at preventing
complications. Vigilant assessment can determine presence of complications, and good
nursing care can help prevent some complications.
Pulmonary Problems
Report fever > 101.5 F. Treat fever < this with C&DB, po intake etc.
Risk factors: general anesthesia, obese, smokers, lung disease, surgery on
upper abdomen, airway, or chest
Atelectasis: collapse of alveoli in a portion of the lung. See more in persons with
upper abdominal surgeries because of the reluctance to C & DB. S/S: decreased
breath sounds, diminished chest expansion (affected side), fever, tachycardia,
decreased cough. TX: antibiotics, decrease viscosity of secretions, C & DB, Turn
q 2h. Dont forget to get them moving even if you feel sorry for them.
Pneumonia: inflammation of the lungs usually due to bacteria. Lower lobes. S/S:
similar to atelectasis. Tx: antibiotics, fluids, C & DB, turn.
Pulmonary embolism: dislodgement of a thrombus from a vein which lodges in
the branch of the lung. S/S: severe, sudden SOB, chest pain, tachypnea,
tachycardia, anxiety. Prevention/Tx: early ambulation (if SBR, leg exercises or
SCD or TEDs), anticoagulants, antibiotics.
Other problems: airway obstruction, hypoxemia, pulmonary edema, aspiration of
gastric contents, bronchospasm, hypoventilation
Cardiovascular Problems
Orthostatic hypotension: a change in BP when changing from supine to upright.
Causes: cardiac, hemorrhage, medications. SS. Hypotension when standing,
tachycardia, faintness. Tx: change positions slowly. Sit at the side of the bed and
dangle until they felt OK. Need to begin early ambulation. Antiembolism
stockings.
Thrombophlebitis may develop from stasis and hypovolemia. S/S: positive
Homans, warm to touch, tender, and firm. Tx: BR with elevation of affected leg.
Other problems: Hypertension, arrhythmias.
15
Neurologic problems
Emergence delirium
Delayed awakening
CVA or decreased LOC related to cerebral blood supply interruptions related to
surgery
Hypothermia
Risk factors: extremes of age, debilitated, intoxicated, long surgery time
Pain
Dont resent their demands or be fearful of addiction
Dont just think of IM drugs-- many other techniques available including PCA,
epidural catheters, NSAIDS
Nausea and vomiting
Post operative nausea/vomiting is a huge problem 30-70% based on population
sampled. Worsened with narcotics, movement, female gender. Tx:
pharmacologic ie droperidol Inapsine, diphenhydramine Benadryl,
dimenhydrinate Dramamine, ondansetron Zofran, etc.
Fluid and electrolyte problems
Hypovolemia: decreased fluid intake: dry mouth, thirst, decreased skin turgor,
decreasing urine output, tachycardia, dry skin. Tx: fluid replacement.
Hypervolemia: IV fluids more than cardiovascular system can handle. Fluids are
retained the first 24 to 48 hours because of stimulation for ADH. s/s: crackles,
increased respiration, pulse, BP, edema, increased urine output. Tx: decreased
fluid intake.
Urinary retention because of trauma from surgery. Other causes include
anesthetics, anticholinergics, positioning. S/S: inability to void, bladder
distension. Tx: catheterization, give privacy, allow to stand, warm water over
perineum, or just the sound of running water.
Renal failure: from inadequate kidney perfusion related to hypotension. S/S:
decreasing urine output in spite of adequate intake. Oliguria, increasing BUN,
creat. Tx: 250-500 ml in 30 minutes, U.O increases then due to hypovolemia.
Hypokalemia: loss of blood, GI fluid
Hyperkalemia: IV fluids
Hyponatremia: loss of body fluids, vomiting, diarrhea
Incisional Problems
16
Wound infection may develop due to 1) surface bacteria, 2) contamination during
sx, 3) tissue infected prior to sx. S/S: wound pain, temperature. Tx: open the
wound and allow to drain.
Dehiscence: partial to total separation of all layers of the incision. Evisceration:
rupture of all layers of the incision with extrusion of abdominal organs. Usually
occur in infected wounds and related to coughing, vomiting, and distension.
Tx: dehiscence - taping or suturing the incision. Evisceration - sudden profuse,
pink drainage, exposed loops of the intestine. Tx: immediate covering of the
loops with sterile towels and saline, notify the MD, low fowlers and knees flexed
to support organs, withhold food and fluids, IV to prevent shock.
Discharge Teaching:
Individualize to the needs of the patient
o diet
o activity
o prescriptions / medications
o elimination
o complications
o sexual activity
o special exercises
o visit with the surgeon
o other follow up appointments
o removal of sutures or staples
o care of the incision
o Infection assessment
o Changes in health
Potrebbero piacerti anche
- The COAT & Review Approach: How to recognise and manage unwell patientsDa EverandThe COAT & Review Approach: How to recognise and manage unwell patientsValutazione: 5 su 5 stelle5/5 (1)
- Leaping the Hurdles: The Essential Companion Guide for International Medical Graduates on their Australian JourneyDa EverandLeaping the Hurdles: The Essential Companion Guide for International Medical Graduates on their Australian JourneyNessuna valutazione finora
- Nsg241 Study Guide Exam 5Documento76 pagineNsg241 Study Guide Exam 5NatalieAndersonNessuna valutazione finora
- Critical Thinking and Nursing ProcessDocumento49 pagineCritical Thinking and Nursing ProcessjeorjNessuna valutazione finora
- Tubes, Lines, and Drains Basics: Harmacy Ompetency Ssessment EnterDocumento11 pagineTubes, Lines, and Drains Basics: Harmacy Ompetency Ssessment EnterJeremy HamptonNessuna valutazione finora
- Interview Questions To PrepareDocumento7 pagineInterview Questions To Prepareico_isNessuna valutazione finora
- W1L1 - Initial Assessment For Trauma - 2Documento44 pagineW1L1 - Initial Assessment For Trauma - 2Baihaqi SaharunNessuna valutazione finora
- Chapter 7 SinghDocumento42 pagineChapter 7 Singhmaa468Nessuna valutazione finora
- 5 Emergency Action Principles - PPTX JuleslectureDocumento55 pagine5 Emergency Action Principles - PPTX JuleslectureBessy Ramos100% (1)
- Entry To Practice RPNDocumento20 pagineEntry To Practice RPNDivina D Galvez-BeronioNessuna valutazione finora
- Nursing BulletsDocumento72 pagineNursing BulletsJoanna Mae Carolino100% (1)
- ATI NotesDocumento2 pagineATI NotesCharlotte Whobrey-Duvall100% (3)
- Nursing Review Bullets HighlightsDocumento65 pagineNursing Review Bullets HighlightsEuanne OrellanoNessuna valutazione finora
- Triage Lecture DR F Mesa GaerlanDocumento55 pagineTriage Lecture DR F Mesa Gaerlanapi-19431894100% (1)
- Clinical Nursing Judgement PaperDocumento6 pagineClinical Nursing Judgement Paperapi-401649778Nessuna valutazione finora
- Bsn-Rs-Careplan 2Documento9 pagineBsn-Rs-Careplan 2api-520841770Nessuna valutazione finora
- Med SurgDocumento9 pagineMed SurgCharlie Gemarino LumasagNessuna valutazione finora
- Mock Osce Midwifery Toc 2021 v2 4 PDFDocumento43 pagineMock Osce Midwifery Toc 2021 v2 4 PDFIsse abdikarim ShaiyeNessuna valutazione finora
- NFDN 2005 Professional PortfolioDocumento2 pagineNFDN 2005 Professional PortfolioTiffany MartellsNessuna valutazione finora
- 1 Perspectives of Pediatric NursingDocumento57 pagine1 Perspectives of Pediatric NursingBluebloodboyNessuna valutazione finora
- Q&A Random - 7Documento15 pagineQ&A Random - 7Filipino Nurses CentralNessuna valutazione finora
- Needs Assessment For Oral Health Program 1Documento16 pagineNeeds Assessment For Oral Health Program 1api-302323771Nessuna valutazione finora
- Class 1 Introduction To Clinical PharmacologyDocumento33 pagineClass 1 Introduction To Clinical Pharmacologymustafa 1Nessuna valutazione finora
- Test Bank For Introduction To Global Health 2nd Edition by JacobsenDocumento5 pagineTest Bank For Introduction To Global Health 2nd Edition by JacobsenjamemaxNessuna valutazione finora
- HIV Practice TestDocumento2 pagineHIV Practice TestJoslyn GrossNessuna valutazione finora
- NRSG 130.01 - Fundamentals of NursingDocumento5 pagineNRSG 130.01 - Fundamentals of NursingJOSHUA DICHOSONessuna valutazione finora
- NCLEXDocumento7 pagineNCLEXmsdrewn30Nessuna valutazione finora
- Fundamentals Note TakingDocumento3 pagineFundamentals Note TakingJero BallesterosNessuna valutazione finora
- SECE Pre-Test 1 - NCLEX - SECEDocumento31 pagineSECE Pre-Test 1 - NCLEX - SECENadesNessuna valutazione finora
- ADEX. MP Resume Template 0604.12 (NY) .6.24.15Documento3 pagineADEX. MP Resume Template 0604.12 (NY) .6.24.15Mjay GuintoNessuna valutazione finora
- LineofinquiryfinaljpDocumento8 pagineLineofinquiryfinaljpapi-456801898Nessuna valutazione finora
- Mock ScenarioDocumento35 pagineMock ScenarioCarla Catrina EstradaNessuna valutazione finora
- Dissiminated Intravascular Coagulation PathoDocumento2 pagineDissiminated Intravascular Coagulation Pathoapi-341263362Nessuna valutazione finora
- (Osborn) Chapter 73 Learning Outcomes (Number and Title)Documento16 pagine(Osborn) Chapter 73 Learning Outcomes (Number and Title)KittiesNessuna valutazione finora
- Nursing in EmergenciesDocumento5 pagineNursing in EmergenciesAvisheel KalsiNessuna valutazione finora
- 11 Test Taking Tips & Strategies For Nurses 101Documento5 pagine11 Test Taking Tips & Strategies For Nurses 101xaileenxNessuna valutazione finora
- RPN Resume 2Documento3 pagineRPN Resume 2api-283946728Nessuna valutazione finora
- Medical EmergenciesDocumento28 pagineMedical EmergenciesmyletterbagNessuna valutazione finora
- Maternity Antepartum Genetic TestingDocumento21 pagineMaternity Antepartum Genetic TestingBobbie N Melinda RussellNessuna valutazione finora
- Clinical Nursing JudgementDocumento6 pagineClinical Nursing Judgementapi-508132058Nessuna valutazione finora
- Aspen Healthcare Online Interview QuestionDocumento5 pagineAspen Healthcare Online Interview QuestionNad DionisioNessuna valutazione finora
- Safe Injection Practices and Handling of SharpsDocumento26 pagineSafe Injection Practices and Handling of SharpsbrightyNessuna valutazione finora
- CBT - Emergency Medicine EditedDocumento14 pagineCBT - Emergency Medicine Editedchristy INessuna valutazione finora
- Student Survival GuideDocumento6 pagineStudent Survival GuideAqua Lake0% (1)
- Analysis of Preconception Healthcare Services Delivered in Selected Medical Officer of Health Areas of Kandy District in Sri LankaDocumento10 pagineAnalysis of Preconception Healthcare Services Delivered in Selected Medical Officer of Health Areas of Kandy District in Sri Lankachamil wijekoonNessuna valutazione finora
- Avant US-RN Recruitment Program: Apply NowDocumento11 pagineAvant US-RN Recruitment Program: Apply Nowrajat mehrotraNessuna valutazione finora
- NCLEX Study GuideDocumento26 pagineNCLEX Study GuideLinda KellyNessuna valutazione finora
- Push 3Documento2 paginePush 3Sandeep SharmaNessuna valutazione finora
- StatementDocumento5 pagineStatementtrinity_brannonNessuna valutazione finora
- Determinants of HealthDocumento9 pagineDeterminants of Healthapi-276860380Nessuna valutazione finora
- Nurse ResumeDocumento1 paginaNurse Resumeapi-266166452Nessuna valutazione finora
- Nurs 253 Preceptor Evaluation Forms-FinalDocumento8 pagineNurs 253 Preceptor Evaluation Forms-Finalapi-284094534Nessuna valutazione finora
- Fetal Alcohol Syndrome Brochure For Nursing SchoolDocumento2 pagineFetal Alcohol Syndrome Brochure For Nursing SchoolKrystal Cowley Miller100% (1)
- Medication Adherence Questionnaire (MAQ) : ARMS ScaleDocumento4 pagineMedication Adherence Questionnaire (MAQ) : ARMS ScaleEnesaHodžićNessuna valutazione finora
- Antihypertension Non AdherenceDocumento16 pagineAntihypertension Non AdherencebezieNessuna valutazione finora
- GCOE Provision 4-6Documento29 pagineGCOE Provision 4-6Justine May GervacioNessuna valutazione finora
- Initial Assessment and ManagementDocumento8 pagineInitial Assessment and ManagementAlvin De LunaNessuna valutazione finora
- NURS 419 Community Health NotesDocumento16 pagineNURS 419 Community Health NotesSarah AnneNessuna valutazione finora
- INFECTION CONTROL: Passbooks Study GuideDa EverandINFECTION CONTROL: Passbooks Study GuideNessuna valutazione finora
- NURSING CARE OF ADULTS II: Passbooks Study GuideDa EverandNURSING CARE OF ADULTS II: Passbooks Study GuideNessuna valutazione finora
- Room: - Name: - Code Status: - AllergiesDocumento2 pagineRoom: - Name: - Code Status: - Allergiesashdmb217Nessuna valutazione finora
- Brain 3Documento3 pagineBrain 3Nurse Betty100% (1)
- Room: - Name: - Code Status: - AllergiesDocumento2 pagineRoom: - Name: - Code Status: - Allergiesashdmb217Nessuna valutazione finora
- Maxwell Quick Medical Reference PDFDocumento35 pagineMaxwell Quick Medical Reference PDFAnonymous fj68Ms100% (10)
- Student Clinical Report SheetDocumento2 pagineStudent Clinical Report SheetMike100% (4)
- Clinical Experience "Tips"Documento5 pagineClinical Experience "Tips"ashdmb217Nessuna valutazione finora
- Nurse Brain Sheet Telemetry Unit SBARDocumento1 paginaNurse Brain Sheet Telemetry Unit SBARashdmb217Nessuna valutazione finora
- AbbreviationsDocumento5 pagineAbbreviationsashdmb217Nessuna valutazione finora
- Histology Exam 2 Review.1Documento18 pagineHistology Exam 2 Review.1ashdmb217Nessuna valutazione finora
- Adventitious Breath SoundsDocumento1 paginaAdventitious Breath Soundsashdmb217Nessuna valutazione finora
- Medical TerminologyDocumento13 pagineMedical Terminologyashdmb217Nessuna valutazione finora
- Information Regarding Family History DocumentDocumento9 pagineInformation Regarding Family History Documentashdmb217Nessuna valutazione finora
- SymbolsDocumento1 paginaSymbolsashdmb217Nessuna valutazione finora
- Useful Spanish Words and PhrasesDocumento32 pagineUseful Spanish Words and Phrasesashdmb217Nessuna valutazione finora
- HCP FormDocumento8 pagineHCP FormMarkNessuna valutazione finora
- Critical Care PhysiologyDocumento287 pagineCritical Care Physiologyashdmb217100% (7)
- Starting Out - New in The ICUDocumento30 pagineStarting Out - New in The ICUashdmb217100% (1)
- Nutrition Review 2.3Documento10 pagineNutrition Review 2.3ashdmb217Nessuna valutazione finora
- Vitamin Chart.2Documento3 pagineVitamin Chart.2ashdmb217Nessuna valutazione finora
- Histology Exam IV Review Part 1Documento36 pagineHistology Exam IV Review Part 1ashdmb217Nessuna valutazione finora
- Histology Exam 3 ReviewDocumento7 pagineHistology Exam 3 Reviewashdmb217Nessuna valutazione finora
- Nutrition Review1.2Documento12 pagineNutrition Review1.2ashdmb217Nessuna valutazione finora
- Histology Exam IV Review Part 2Documento26 pagineHistology Exam IV Review Part 2ashdmb217Nessuna valutazione finora
- Exam 1 Study Guide.2Documento52 pagineExam 1 Study Guide.2ashdmb217Nessuna valutazione finora
- Biochem Exam 2 Review.2Documento31 pagineBiochem Exam 2 Review.2ashdmb217Nessuna valutazione finora
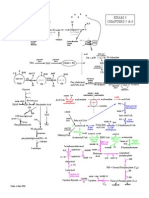
- Exam 3 PathwaysDocumento1 paginaExam 3 Pathwaysashdmb217Nessuna valutazione finora
- Exam IV ReviewDocumento39 pagineExam IV Reviewashdmb217Nessuna valutazione finora
- Exam 4 PathwaysDocumento1 paginaExam 4 Pathwaysashdmb217Nessuna valutazione finora
- Biochem Exam III Review.2Documento24 pagineBiochem Exam III Review.2ashdmb217Nessuna valutazione finora
- Plastic Surgery 2022Documento3 paginePlastic Surgery 2022Plastic SugeryNessuna valutazione finora
- Operating Theatre Efficiency GuidelinesDocumento82 pagineOperating Theatre Efficiency GuidelinesvyshnosudhaNessuna valutazione finora
- Aeon7200A-Service Manual - v0 (1) .7Documento67 pagineAeon7200A-Service Manual - v0 (1) .7Carlito Sales100% (7)
- MirasolDocumento7 pagineMirasolJan Chrispian MirasolNessuna valutazione finora
- American Journal of Clinical HypnosisDocumento6 pagineAmerican Journal of Clinical HypnosisBriando Stevano LinelejanNessuna valutazione finora
- Safe Sedation For All Practitioners A Practical GuideDocumento190 pagineSafe Sedation For All Practitioners A Practical Guidemonir61Nessuna valutazione finora
- Diethyl Ether ReportDocumento24 pagineDiethyl Ether ReportRania 'aciL' Fardyani0% (1)
- Anesthetics: - These Are The Drugs Which Causes - My Be Local or General AnesthesiaDocumento26 pagineAnesthetics: - These Are The Drugs Which Causes - My Be Local or General AnesthesiaKashis SharmaNessuna valutazione finora
- Patient Warming Systems For All Clinical SituationsDocumento8 paginePatient Warming Systems For All Clinical Situationssidmed sidmedNessuna valutazione finora
- Enhanced Recovery After SurgeryDocumento47 pagineEnhanced Recovery After SurgeryPeri HidayatNessuna valutazione finora
- The Introduction of Halothane Into Clinical Practice: The Oxford ExperienceDocumento6 pagineThe Introduction of Halothane Into Clinical Practice: The Oxford Experiencearyati yayaNessuna valutazione finora
- 15 Nursing Care of A Family During Labor and BirthDocumento14 pagine15 Nursing Care of A Family During Labor and BirthNurse UtopiaNessuna valutazione finora
- The Amsterdam Preoperative Anxiety and Information.2Documento7 pagineThe Amsterdam Preoperative Anxiety and Information.2Jose Rafael Villafan BernalNessuna valutazione finora
- Article - Medical NegligenceDocumento4 pagineArticle - Medical NegligenceSimon RajNessuna valutazione finora
- Anesthesia & Analgesia For Labor & DeliveryDocumento30 pagineAnesthesia & Analgesia For Labor & DeliveryPalwasha MalikNessuna valutazione finora
- S M A R T: 201 A TEST #3 Define and Discuss The Purpose of Outcome IdentificationDocumento6 pagineS M A R T: 201 A TEST #3 Define and Discuss The Purpose of Outcome IdentificationLindsay JonesNessuna valutazione finora
- Day Care Centre: Ankit SinghDocumento17 pagineDay Care Centre: Ankit SinghAnonymous ibmeej9Nessuna valutazione finora
- DeliriumDocumento12 pagineDeliriumChrysi TsiouriNessuna valutazione finora
- Alternative Mandibular Nerve Block TechniquesDocumento6 pagineAlternative Mandibular Nerve Block TechniquesAlienformoflifeNessuna valutazione finora
- Annotated Bibliography 1Documento2 pagineAnnotated Bibliography 1api-663775614Nessuna valutazione finora
- Daftar PustakaDocumento6 pagineDaftar PustakaAkhmad Ikhsan Prafita PutraNessuna valutazione finora
- Day Case Surgery 1lDocumento19 pagineDay Case Surgery 1lapi-436678825Nessuna valutazione finora
- Aeu 325Documento2 pagineAeu 325Baha MirzaeifarNessuna valutazione finora
- Professional Anesthesia HandbookDocumento114 pagineProfessional Anesthesia HandbookSooryajith DineshNessuna valutazione finora
- Aidtomultiplechoicequestionsinsurgery20161013 PDFDocumento166 pagineAidtomultiplechoicequestionsinsurgery20161013 PDFAshwin HalaiNessuna valutazione finora
- Statement On Nonoperating Room Anesthetizing LocationsDocumento2 pagineStatement On Nonoperating Room Anesthetizing LocationsJorge QuispeNessuna valutazione finora
- Prevalence, Risk Factors, and Optimized Management of Moderate To Severe Thirst in The Post Anesthesia Care UnitDocumento10 paginePrevalence, Risk Factors, and Optimized Management of Moderate To Severe Thirst in The Post Anesthesia Care Unitpooria shNessuna valutazione finora
- AQUALIPODocumento16 pagineAQUALIPOAvalavenia Molina AbadNessuna valutazione finora
- PharmacologyDocumento84 paginePharmacologyhenrydycoco100% (1)
- Principles Fluid Blood Itaccs Vol18no1-11Documento9 paginePrinciples Fluid Blood Itaccs Vol18no1-11charlietuna1100% (1)