Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
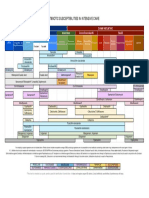
Narrative Chart
Caricato da
hady920100%(1)Il 100% ha trovato utile questo documento (1 voto)
2K visualizzazioni5 pagineNarrative Chart
Copyright
© © All Rights Reserved
Formati disponibili
DOCX, PDF, TXT o leggi online da Scribd
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoNarrative Chart
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato DOCX, PDF, TXT o leggi online su Scribd
100%(1)Il 100% ha trovato utile questo documento (1 voto)
2K visualizzazioni5 pagineNarrative Chart
Caricato da
hady920Narrative Chart
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato DOCX, PDF, TXT o leggi online su Scribd
Sei sulla pagina 1di 5
NARRATIVE CHARTING
05/31/07...2245...Pt 4 hours postoperative: awakens easily: oriented X3 but
groggy. Incision site in front of L ear extending down and around ear and
into neck-approximately 6" in length - without dressing. No swelling or
bleeding, bluish discoloration below L ear noted, sutures intact. Jackson
Pratt drain in L neck below ear with 20 mL bloody drainage measured.
Drain remains secured in place with suture and anchored to L anterior
chest wall with tape. Pt denied pain but stated she felt nauseated and
promptly vomited 100 mL of clear fluid. Pt attempted to get OOB to
ambulate to bathroom with assistance but felt dizzy upon standing.
Assisted to lie down in bed. Voided 200 mL clear, yellow urine in bedpan.
Pt encouraged to deep-breathe and cough QH and turn frequently in bed.
Antiembolism pads applied to both lower extremeties. Explanations given
re: these preventive measures. Pt verbalized understanding.---------------
Joe Schmoe, RN
05/31/07...2255...Pt continues to feel nauseated. Compazine 10mg I.M.
given in R gluteus maximus.----------------------------------------------Joe
Schmoe, RN
05/31/07...2335...Pt states she is no longer nauseated, remains pain free.
No further vomiting. Pt demonstrated taking deep breaths and coughing
effectively.------------------------------------------------------------------Joe
Schmoe, RN
Example for NG insertion. 16 F NGT placed with ease through the
right nares using clean technique after prep with cetacaine spray
and xylocaine jelly for pt comfort. Placement checked per
auscultation and return of gastric contents. 100 ml yellow liquid
gastric contents returned immediately. NG connected to LIWS per
order. Pt tolerated the procedure well and vital signs remain
within normal limits.
Prior to documenting the placement procedure, of course you would also need to
document what the patient looked like ie: why they needed intubated, then any
medications that were given to relax or sedate the patient. Don't forget the soft
restraint documentation if you are using those. Most places require separate papers
for soft restraints or safety devices.
For an ET I will usually chart this: 8.5 ET tube placed successfully after two
attempts per respiratory or MD (whichever). Placement initially checked by
positive breath sounds bi-lat and positive end tidal Co2. Stat x-ray ordered
to confirm placement. Tube placed 22 at the lip and tube secured. Pt's SpO2
now 98% and pt's color is pink, patient is warm and dry.
Then you would chart either the patient is being bagged per RT or pt placed
on a vent and be sure to document the vent settings. If there is anything
suctioned from the lungs you would need to document the consistancy, the
color and the amount.
Narrative Nursing Notes:10/13/2010. 1735. Chief complaint: SOB. Age 28,
Orient x3. HR 70 BPM (pacemaker), Respiration 20,BP: 100/60 mmHg, O2:
95%. Dimished breath sounds, crackles in lower right lung. T 37.0 C. PT
inserted, 600 mL of urine, dark yellow,clear, no odor. Unable to walk
without assistance. Unable to move from chair to bed without
assistance.Breathing with nasal canunli. O2 is humidified. PT states no
pain, 0 on pain scale, but 4-5 when pressureulcer is bothering him.
Pressure ulcer on sacral area. Did not assess. PEARLA. Can respond to
commands.Hearing loss in left year. Motor responses are +2. No facial
drooping noticed. Skin tugor: dehydrated,cool to touch. Notable edema on
lower extremities, Pitting on lower leg. Pedal purse difficult to feel
07:30 Alert, awake, orientated to person place and time. Follows commands. Skin
warm and dry. Respirations
unlabored @18. Apical Pulse = 82, regular. Bowel Sounds absent. Hand grasps equal.
@ 4L via nasal cannula. IV
D5/1/2NS infusing @100 to R forearm via pump. Site clean and dry with no swelling or
redness. Abdominal dressing
dry and intact. Foley draining clear amber urine. Compression boots in place. TEDS in
place. Bed in low position,
call bell in reach, siderails CNS
Documenting diet.
The amount of fluid in CCs is recorded in the I&O sheet. In the narrative note document
the type of diet, percentage
consumed, and any pertinent information :
08:00 Took 100% of low sodium, soft diet. Had difficulty swallowing chopped meat._M.
Nurse, BCNS
Documentation of complete physical assessment.
Complete your assessment before 9 a.m. and before giving any medications or
treatments. It may not all be
actually completed at the same time, but document it in one paragraph making sure that
any abnormal or
critical findings are documented and reported immediately.
Ask the patient specifically when he had last BM. In addition to stating of stating no
complaints of
constipation diarrhea or flatus, describe your patients specific status.
0830 Awake, alert, oriented to person, place & time. Skin warm and dry. Turgor recoil
brisk. Face symmetrical.
PERRLA. EOM intact. Follow spoken commands. Mucous membranes pink & moist.
Swallows without difficulty. Neck supple, trachea midline, carotids equal, no lymph
nodes palpated. JVD (-) @ 45. Respirations even and
unlabored, rate 16. Breath sounds clear bilaterally & A&P. Apical Pulse=72, regular.
Abdomen soft, non-tender, bowel
sounds present in all 4 quadrants. No complaints of constipation, diarrhea, flatus.
States last BM yesterday evening.
Urine amber, no complaints of burning. MAE without difficulty. Peripheral pulses 2+.
Homans sign (-). Capillary
refill brisk. Bed in low position, call light within reach.
SR
BCNS
Documentation of hygiene care:
Most institutions have a check-off list of nursing interventions for hygiene, such as back
care, pedicure, Foley care,
mouth care. However, they should be included in a narrative note. Also indicate how
much of the care the patient
did independently and any pertinent observations.
09:30 Complete bath care given with mouth care, peri-care, Foley care, back care.__M.
Nurse, BCNS
Documenting ambulation:
Describe gait, strength, amount of assistance needed, how tolerated.
09:30 OOB to chair with the assistance of two staff members. Gait steady, but slow.
Ambulated in hallway 5 minutes.
C/O feeling tired., assisted back to
bed________________________________M. Nurse, BCNS
Documenting a problem such as pain:
State the problem, what was done to solve it, and record result.
10:15 States sharp pain points to LLQ of abdomen, 8 on a scale of 1-10. States gets a
little better when lying on left
side. Respirations 20. Demerol 75 mg IM R ventral gluteal site by M. RealNurse, RN.
Side rails
position, call light in reach. M. Nurse, BCNS
and the result (or evaluation of whether your intervention was successful):
11:00 States pain 3 on scale of 1-10. Watching TV.__________________M. Nurse,
BCNS
Documenting a physician visit, a test, therapy, treatment, specimen:
10:30 Dr. Jones in to see patient._________________________________M.
Nurse, BCNS
10:40 To x-ray via w/c for chest x-ray_____________________________M.
Nurse, BCNS
11:45. Sputum Specimen to lab.__________________________________M.
Nurse, BCNS
12:00 Abdominal dressing change. 8" midline, vertical abdominal incision well-
approximated. Staples intact. No
redness, swelling or drainage noted. Dry sterile dressing applied._________M. Nurse,
BCNS
FINAL ENTRY:
Verify status of your patient and include safety check
12:15 States pain almost gone, now a 1 on 1-10 scale. Husband visiting. Watching TV.
Side rail
reach, bed in low position.___________________________________M. Nurse,
BCNS
Potrebbero piacerti anche
- ChartingDocumento3 pagineChartingLorina Lynne ApelacioNessuna valutazione finora
- Head To Toe Narrative ChartingDocumento1 paginaHead To Toe Narrative ChartingDianne Macaraig100% (3)
- Narrative ChartingDocumento2 pagineNarrative Chartingearl_llamas0% (2)
- Head to Toe Assessment ChecklistDocumento6 pagineHead to Toe Assessment Checklistsandra100% (3)
- Gordon's 11 Functional Health PatternsDocumento4 pagineGordon's 11 Functional Health Patternsnina angelaNessuna valutazione finora
- Urinary Incontinence Nursing ManagementDocumento3 pagineUrinary Incontinence Nursing ManagementRnspeakcomNessuna valutazione finora
- Focus Charting Example PDFDocumento1 paginaFocus Charting Example PDFRegine Lorenzana Mey-AngNessuna valutazione finora
- Head To Toe Assessment in 5 Minutes or MoreDocumento12 pagineHead To Toe Assessment in 5 Minutes or MoreTSPANNessuna valutazione finora
- Head To Toe AssessmentDocumento56 pagineHead To Toe AssessmentAna95% (39)
- SAMPLE CHARTING DOCUMENT SUMMARYDocumento1 paginaSAMPLE CHARTING DOCUMENT SUMMARYKatherine Ibarra100% (1)
- PT 2 Nurse NotesDocumento1 paginaPT 2 Nurse NotesAmy67% (3)
- Head To Toe Assessment NRS 111Documento4 pagineHead To Toe Assessment NRS 111Danielle Shull100% (2)
- PHYSICAL ASSESSMENT SKIN, HAIR AND NAILDocumento6 paginePHYSICAL ASSESSMENT SKIN, HAIR AND NAILFerdos Adem100% (9)
- 20Documento24 pagine20Jeremee John Pingco50% (2)
- Gordon'sDocumento2 pagineGordon'sCham Rafaela ConeseNessuna valutazione finora
- Edith Jacobson Care PlanDocumento10 pagineEdith Jacobson Care PlanKarina Rodriguez100% (3)
- Nursing Note For Head To Toe AssessmentDocumento1 paginaNursing Note For Head To Toe Assessmentchoochoopy100% (1)
- Focused AssessmentDocumento3 pagineFocused Assessmentisapatrick8126Nessuna valutazione finora
- Complete Assessment Script Print FormDocumento6 pagineComplete Assessment Script Print Formkeirvyl0% (1)
- Nurses Notes1Documento1 paginaNurses Notes1Wally Cuaresma67% (3)
- Nurses NotesDocumento1 paginaNurses Notesmona_javier100% (4)
- Head To Toe AssessmentDocumento1 paginaHead To Toe AssessmentIdhonna AbihayNessuna valutazione finora
- Personal Nursing PhilosophyDocumento5 paginePersonal Nursing PhilosophyLaura Sotomayor100% (2)
- Nursing Head-to-Toe Assessment Cheat Sheet PDFDocumento7 pagineNursing Head-to-Toe Assessment Cheat Sheet PDFJoebert BangsoyNessuna valutazione finora
- Nursing Care Plan of Client With Fluid and Electrolyte ImbalanceDocumento28 pagineNursing Care Plan of Client With Fluid and Electrolyte ImbalanceCj Aguilar50% (2)
- CEUFast Infection Control and Barrier PrecautionsDocumento90 pagineCEUFast Infection Control and Barrier PrecautionsMeg GalauranNessuna valutazione finora
- Health Assessment Complete 2Documento14 pagineHealth Assessment Complete 2kimberly100% (1)
- Nursing Care Plan Mobility SampleDocumento6 pagineNursing Care Plan Mobility Samplen2biologyNessuna valutazione finora
- Sample Nurses Notes CuDocumento3 pagineSample Nurses Notes Cuapi-1978086589% (19)
- Head-to-Toe Assessment Checklist: Department of Nursing Health AssessmentDocumento2 pagineHead-to-Toe Assessment Checklist: Department of Nursing Health AssessmentRachel Ray100% (2)
- Head To Toe Checklist OlderDocumento1 paginaHead To Toe Checklist Olderspatrick32100% (4)
- Trach care improves vital signs by removing secretionsDocumento1 paginaTrach care improves vital signs by removing secretionsdoirge47100% (8)
- ChartingDocumento1 paginaChartingberhanubedassa100% (2)
- Ethic in NursingDocumento246 pagineEthic in Nursingsyikir100% (1)
- Assessment of The Lungs and ThoraxDocumento21 pagineAssessment of The Lungs and ThoraxNur Rofikoh Bil Karomah100% (2)
- Nurse Assessment ChecklistDocumento3 pagineNurse Assessment Checklistclarimer100% (3)
- Gordon's Functional Health PatternsDocumento2 pagineGordon's Functional Health Patternsserarrist100% (2)
- Gerontologic Health Promotion ActivityDocumento3 pagineGerontologic Health Promotion ActivityCorinne50% (2)
- Nursing Assessment in Tabular FormDocumento38 pagineNursing Assessment in Tabular FormCas Tan100% (1)
- This Study Resource Was: Head-To - Toe Assessment Documentation SampleDocumento2 pagineThis Study Resource Was: Head-To - Toe Assessment Documentation SampleA Sung100% (3)
- Head To Toe Assessment Guide PDFDocumento6 pagineHead To Toe Assessment Guide PDFTashaNessuna valutazione finora
- Cellulitis Concept MapDocumento3 pagineCellulitis Concept MapBien EstrellaNessuna valutazione finora
- Nursing DiagnosisDocumento7 pagineNursing DiagnosisMariya Mikaela Garcia SoledadNessuna valutazione finora
- Nursing Diagnosis & Careplan SamplesDocumento5 pagineNursing Diagnosis & Careplan SamplesE94% (18)
- Methods For Documenting Nurses NotesDocumento2 pagineMethods For Documenting Nurses Notescyndi1709167100% (9)
- Colon Cancer Case Study - 64yo Male Diagnosed After Rectal BleedingDocumento2 pagineColon Cancer Case Study - 64yo Male Diagnosed After Rectal BleedingDragan Djordjevic100% (4)
- Physical AssessmentDocumento19 paginePhysical Assessmentsilentscream0618Nessuna valutazione finora
- Pre-Op Medication Reference SheetDocumento3 paginePre-Op Medication Reference Sheetsabbo morsNessuna valutazione finora
- Nursing Care PlanDocumento10 pagineNursing Care PlanMalou SanNessuna valutazione finora
- Review of Systems SummaryDocumento2 pagineReview of Systems SummaryDiane Gabriel100% (1)
- Nursing management The Ultimate Step-By-Step GuideDa EverandNursing management The Ultimate Step-By-Step GuideNessuna valutazione finora
- Chicago Review Press NCLEX-PN Practice Test and ReviewDa EverandChicago Review Press NCLEX-PN Practice Test and ReviewValutazione: 4 su 5 stelle4/5 (4)
- Talking Therapy: Knowledge and Power in American Psychiatric NursingDa EverandTalking Therapy: Knowledge and Power in American Psychiatric NursingNessuna valutazione finora
- COMMUNITY HEALTH NURSE: Passbooks Study GuideDa EverandCOMMUNITY HEALTH NURSE: Passbooks Study GuideNessuna valutazione finora
- The Battle Against Covid-19 Filipino American Healthcare Workers on the Frontlines of the Pandemic ResponseDa EverandThe Battle Against Covid-19 Filipino American Healthcare Workers on the Frontlines of the Pandemic ResponseNessuna valutazione finora
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideDa EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNessuna valutazione finora
- Easy Nursing Notes For The Registered Nurse.Da EverandEasy Nursing Notes For The Registered Nurse.Valutazione: 4 su 5 stelle4/5 (6)
- Immobilize Injuries with Splinting TechniquesDocumento1 paginaImmobilize Injuries with Splinting Techniqueshady920Nessuna valutazione finora
- Postpartum-First 6 Weeks After: ChildbirthDocumento22 paginePostpartum-First 6 Weeks After: Childbirthhady920100% (1)
- Parkinson's DiseaseDocumento3 pagineParkinson's Diseasehady920Nessuna valutazione finora
- 6th Central Pay Commission Salary CalculatorDocumento15 pagine6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- HAAD Exam BookingDocumento10 pagineHAAD Exam Bookinghady920Nessuna valutazione finora
- ER CasesDocumento1 paginaER Caseshady920Nessuna valutazione finora
- NCLEX - Study Points 1Documento2 pagineNCLEX - Study Points 1hady920Nessuna valutazione finora
- Pearson Vue Scheduling Appointment - Pef CommunityDocumento11 paginePearson Vue Scheduling Appointment - Pef Communityhady920Nessuna valutazione finora
- Nursing Care Plan Nausea & VomitingDocumento3 pagineNursing Care Plan Nausea & Vomitingderic87% (47)
- Maternity ReviewDocumento20 pagineMaternity Reviewhady920Nessuna valutazione finora
- NCLEX-RN Gastrointestinal Health Problems Test DrillDocumento9 pagineNCLEX-RN Gastrointestinal Health Problems Test DrillAko Si PisangNessuna valutazione finora
- Haad Dataflow GuideDocumento16 pagineHaad Dataflow Guidehady920100% (4)
- PrayersDocumento2 paginePrayersshariqhkNessuna valutazione finora
- Delcaration Form by The Sponsoring FacilityDocumento1 paginaDelcaration Form by The Sponsoring FacilityDr-Usman Khan100% (1)
- Haad Dataflow GuideDocumento16 pagineHaad Dataflow Guidehady920100% (4)
- Documentation 123Documento17 pagineDocumentation 123Edmond ChanNessuna valutazione finora
- Experience Letter Salary Sheet Experience LetterDocumento1 paginaExperience Letter Salary Sheet Experience LetterNajmul HasanNessuna valutazione finora
- HAAD Exam SyllabusDocumento2 pagineHAAD Exam SyllabusAnuRavipati75% (4)
- IV Fluid ChartDocumento2 pagineIV Fluid Charthady920Nessuna valutazione finora
- Salah Part1Documento13 pagineSalah Part1hady920Nessuna valutazione finora
- 17-19 Late AdulthoodDocumento52 pagine17-19 Late AdulthoodAlen AlanoNessuna valutazione finora
- NCLEX-RN Gastrointestinal Health Problems Test DrillDocumento9 pagineNCLEX-RN Gastrointestinal Health Problems Test DrillAko Si PisangNessuna valutazione finora
- PSY3370 Chap - 18 - 19Documento13 paginePSY3370 Chap - 18 - 19hady920Nessuna valutazione finora
- Types of SolutionDocumento10 pagineTypes of Solutionhady920Nessuna valutazione finora
- Fluid Management-OnlineDocumento24 pagineFluid Management-Onlinehady920Nessuna valutazione finora
- ReviewerDocumento63 pagineReviewerEdilyn CandelariaNessuna valutazione finora
- Fluid and Electrolyte ImbalanceDocumento25 pagineFluid and Electrolyte Imbalancehady920Nessuna valutazione finora
- Maternity Nursing Lecture PresentationDocumento69 pagineMaternity Nursing Lecture Presentationapi-3764215100% (8)
- Go With The Flow of Chest Tube Therapy: by Arlene M. Coughlin, RN, MSN, and Carolyn Parchinsky, RN, MADocumento14 pagineGo With The Flow of Chest Tube Therapy: by Arlene M. Coughlin, RN, MSN, and Carolyn Parchinsky, RN, MAhady920100% (1)
- Soap Notes HypertensionDocumento6 pagineSoap Notes HypertensionCHRISTINE KARENDINessuna valutazione finora
- ......... NCP CaseDocumento34 pagine......... NCP Casevipnikally80295% (19)
- Co General InformationDocumento13 pagineCo General InformationAndianto IndrawanNessuna valutazione finora
- Transmission Substation Work Practice Manual 2016-07-22Documento499 pagineTransmission Substation Work Practice Manual 2016-07-22Edmund YoongNessuna valutazione finora
- Case Control Study For MedicDocumento41 pagineCase Control Study For Medicnunu ahmedNessuna valutazione finora
- Feasibility of Malunggay & Coconut Vinegar as Natural Cleaning AgentDocumento7 pagineFeasibility of Malunggay & Coconut Vinegar as Natural Cleaning AgentCharles Dave AvenidoNessuna valutazione finora
- ICU antibiotic susceptibilities guideDocumento1 paginaICU antibiotic susceptibilities guideFaisal Reza AdiebNessuna valutazione finora
- Soft Drinks in India: Euromonitor International February 2022Documento27 pagineSoft Drinks in India: Euromonitor International February 2022Gayathri22394Nessuna valutazione finora
- Calculate The Max Doses of Local Anesthesia in DentistryDocumento13 pagineCalculate The Max Doses of Local Anesthesia in DentistryYasser MagramiNessuna valutazione finora
- Brand Analysis of Leading Sanitary Napkin BrandsDocumento21 pagineBrand Analysis of Leading Sanitary Napkin BrandsSoumya PattnaikNessuna valutazione finora
- MalariaDocumento11 pagineMalariaWynli Fullo AncogNessuna valutazione finora
- Updates On Upper Eyelid Blepharoplasty.4Documento8 pagineUpdates On Upper Eyelid Blepharoplasty.4Dimitris RodriguezNessuna valutazione finora
- Fertilizer Use by Crop in The Islamic Republic of IranDocumento78 pagineFertilizer Use by Crop in The Islamic Republic of Iransiamak77Nessuna valutazione finora
- 32 Vol4 EpaperDocumento32 pagine32 Vol4 EpaperThesouthasian TimesNessuna valutazione finora
- Legalizing abortion in the Philippines for women's health and rightsDocumento2 pagineLegalizing abortion in the Philippines for women's health and rightsRosario Antoniete R. Cabilin100% (1)
- Nutrition For Exercise and Sport Exam PDFDocumento6 pagineNutrition For Exercise and Sport Exam PDFAngela BrownNessuna valutazione finora
- MCQ BankDocumento23 pagineMCQ Bankdrmed100% (3)
- Angle Grinder PDFDocumento2 pagineAngle Grinder PDFcityofdarwingisNessuna valutazione finora
- TMH ResumeDocumento2 pagineTMH Resumeapi-257873078Nessuna valutazione finora
- Science of 7 ChakraDocumento6 pagineScience of 7 ChakraSheebaNessuna valutazione finora
- Mind Body PDFDocumento357 pagineMind Body PDFAzhari RahmatNessuna valutazione finora
- 798 3072 1 PBDocumento12 pagine798 3072 1 PBMariana RitaNessuna valutazione finora
- WORKPLACE TB POLICYDocumento4 pagineWORKPLACE TB POLICYGigi CabanaNessuna valutazione finora
- Module 4Documento107 pagineModule 4roseannurakNessuna valutazione finora
- 58-Article Text-228-1-10-20180325Documento11 pagine58-Article Text-228-1-10-20180325mutiara nancyNessuna valutazione finora
- My Study NotebookDocumento40 pagineMy Study NotebookRichyl T. JaymeNessuna valutazione finora
- Methods of Investigating Brain and LanguageDocumento12 pagineMethods of Investigating Brain and Languagekiranjit_123100% (2)
- Detailed Advertisement of Various GR B & C 2023 - 0 PDFDocumento47 pagineDetailed Advertisement of Various GR B & C 2023 - 0 PDFMukul KostaNessuna valutazione finora
- Proximal Humerus Fractures Epidemiology and TrendsDocumento5 pagineProximal Humerus Fractures Epidemiology and TrendsHelena Sofia Fonseca Paiva De Sousa TelesNessuna valutazione finora
- Tailored Health Plans Table of CoverDocumento22 pagineTailored Health Plans Table of CoverAneesh PrabhakaranNessuna valutazione finora