Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Practical Pediatric Regional Anesthesia
Caricato da
Ista Fatimah Kurnia Rahmi0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
30 visualizzazioni31 paginepediatric anesthesia
Copyright
© © All Rights Reserved
Formati disponibili
PDF, TXT o leggi online da Scribd
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentopediatric anesthesia
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato PDF, TXT o leggi online su Scribd
0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
30 visualizzazioni31 paginePractical Pediatric Regional Anesthesia
Caricato da
Ista Fatimah Kurnia Rahmipediatric anesthesia
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato PDF, TXT o leggi online su Scribd
Sei sulla pagina 1di 31
NEW CONCEPTS AND TECHNIQUES IN PEDIATRIC
ANESTHESIA 08898537/02 $16.00 .00
PRACTICAL PEDIATRIC
REGIONAL ANESTHESIA
Santhanam Suresh, MD, and Melissa Wheeler, MD
Change is never made from worse to better
without inconvenience.
BOOKER T. WASHINGTON
Regional anesthetic techniques in children have become more popu-
lar in the past decade. This is in part because of recent research indicat-
ing biobehavioral changes associated with untreated pain in children.
2, 86
Most regional techniques in children are performed under heavy seda-
tion or general anesthesia. Concerns regarding safety and the medico-
legal liability of performing regional blocks under anesthesia must be
weighed against the trauma and potential danger of placing blocks in
awake, uncooperative children. A large body of clinical experience sup-
ports the safety and efcacy of regional blocks placed under general
anesthesia in children.
49
There is evidence-based literature to show that
combined regional and general anesthesia may actually improve out-
come and thereby decrease hospital stay.
61
The availability of better
equipment and safer local anesthetic agents has also improved the safety
of regional anesthetic techniques. Overall, the incidence of complications
with the use of regional techniques in children is not signicantly differ-
ent from that in the adult population. The benets of regional techniques
include avoidance of perioperative opioids and their associated side
effects,
84
early ambulation, and excellent pain control. The preemptive
From the Department of Anesthesiology, Childrens Memorial Hospital, Northwestern Uni-
versity Medical School, Chicago, Illinois
ANESTHESIOLOGY CLINICS OF NORTH AMERICA
VOLUME 20 NUMBER 1 MARCH 2002 83
84 SURESH & WHEELER
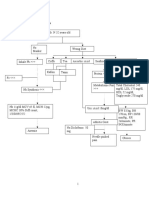
Table 1. DIFFERENCES BETWEEN CENTRAL NEURAXIAL AND PERIPHERAL NERVE
BLOCKS
Central Neuraxial Blocks Peripheral Nerve Blocks
Epidural or intrathecal approach Directed to the area requiring analgesia
Cannot be used for head and neck surgery Applicable for any area that is operated on
Systemic symptoms including hypotension Rarely systemic effects
Lower extremity weakness and delayed Delay in ambulation unlikely (except
ambulation lower extremity block)
Duration of analgesia is limited to Analgesia may last longer than 12 hours
approximately 4 to 6 hours
placement of nerve blocks may also improve postoperative recovery and
decrease postoperative analgesic requirements.
17
This article describes the use of regional anesthetic techniques in
children. They can be divided into two major groups: (1) central neurax-
ial blocks; (2) peripheral nerve blocks. Differences between central neu-
raxial and peripheral nerve blocks are shown in Table 1.
PHARMACOLOGY AND TOXICITY OF LOCAL
ANESTHETICS
The primary local anesthetic agents used in pediatric regional tech-
niques are 2-chloroprocaine, lidocaine, bupivacaine, ropivacaine, mepi-
vacaine, and tetracaine. Levobupivacine has recently been studied and
may replace the racemic mixture of bupivacaine because of its decreased
potential for central nervous system toxicity and cardiotoxicity.
3, 23, 60
All
local anesthetics block the generation and propagation of impulses in
excitable tissues. This action results in effective regional blockade when
these drugs are deposited near peripheral nerves, nerve roots, or the
spinal cord. This also causes the adverse central nervous system and
cardiac effects of local anesthetic toxicity that occur when plasma con-
centrations are elevated by accidental intravenous administration or
increased systemic uptake secondary to relative overdose. The pharma-
cology of local anesthetics in children is similar to that in adults. In
neonates and infants, however, the greater total body water results in a
larger volume of distribution and therefore longer elimination half-life.
Decreased protein binding, both qualitative and quantitative, results in
greater unbound fraction of drug (particularly bupivacaine) and, there-
fore, increased potential for toxicity. In addition, with age, the endoneu-
rium becomes less permeable, so both latency and duration of nerve
blockade increase.
Local Anesthetic Agents
2-Chloroprocaine 2% or 3% has a short time to onset of action and a
short duration of action. It is useful for testing the function of caudal or
PRACTICAL PEDIATRIC REGIONAL ANESTHESIA 85
epidural catheters. Though experience is limited, it has been recom-
mended as a safer alternative for continuous catheter infusion in preterm
and high-risk infants.
37
Lidocaine 0.5% to 2% has a short time to onset and medium duration
of action. It can be used for peripheral blocks or epidural anesthesia.
Bupivacaine 0.1% to 0.5% has a longer onset time and duration of
action than lidocaine or 2-chloroprocaine but has a greater potential for
severe cardiotoxicity than other agents. It can be used for peripheral
blocks, spinal anesthesia, and caudal or epidural anesthesia and analge-
sia.
Levobupivacaine is effective for peripheral nerve block and caudal
block in children.
60
It has less cardiac toxicity potential and may be a
more attractive alternative to bupivacaine.
Ropivacaine 0.2% to 1% is supplied as the pure S-enantiomer and
has an onset time and duration of action comparable with bupivacaine.
It produces less motor blockade and is less toxic than bupivacaine.
41
It
also can be used for peripheral blocks and caudal or epidural anesthesia
and analgesia. Unlike most other local anesthetic agents, onset time,
duration of action, and systemic absorption are not affected by epineph-
rine.
Tetracaine 1% is used for spinal anesthesia.
77
Mepivacaine is approximately equally potent to lidocaine and can
safely be used for peripheral nerve blocks.
20
Mepivacaine can provide a
rapid onset of block, with a shorter duration of motor block, that may
allow for rapid recovery in the postoperative period.
69
Central Neuraxial Blocks
General Principles
Patient Monitoring. Monitors should be applied and function as-
sured before the block is performed. In particular, the electrocardiogram
should be adjusted so that the P wave, QRS complex, and upright T
wave can be seen clearly. Baseline systolic blood pressure and heart rates
should be noted.
Skin Preparation. Bacterial colonization of epidural and caudal
catheters in children occurs at a rate of 6% to 35%.
44, 47, 62
Gram-positive
organisms are most common, though gram-negative colonization may
also occur, particularly with caudal catheters.
47
Children under 3 years
of age are also most likely to have colonization of caudal catheters.
47
Despite high rates of colonization, serious epidural infections are exceed-
ingly rare.
47, 62, 83
Chlorhexidine may be better than povidone iodine for
reducing the risk of catheter colonization in children.
44
Test Dose. The authors strongly recommend the use of a test dose
to decrease the likelihood of intravascular injection. A test dose is not
100% reliable, however, and graded dosing with careful attention to vital
signs is recommended. A test dose should be 0.1 mL/kg of a local
anesthetic solution with 5 g/mL of epinephrine to a maximum volume
86 SURESH & WHEELER
of 3 mL. An increase in heart rate of 10 beats per minute above baseline
occurring within 1 minute of injection is a reasonable predictor of intra-
vascular injection for children anesthetized with sevourane.
88
This sign
is less reliable in children anesthetized with halothane.
88
Pretreatment
with atropine may improve the accuracy of heart rate changes in de-
tecting intravascular injection for both inhalation agents.
87
An increase
in systolic blood pressure of greater than 15 mm Hg within 2 minutes
of injection is further conrmation of intravascular injection, although
less sensitive and specic than changes in heart rate.
48, 88
A 25% change
in the T-wave amplitude (increase or decrease) may be the most reliable
predictor of intravascular injection (Fig. 1).
21, 48
All studies have evaluated
this parameter by strip recording, however, and accuracy by observation
of the monitor alone has not been evaluated. In addition, changes in T-
wave amplitude in response to epinephrine vary with age, and this test,
therefore, may not be valid in children older than 92 months (7.6 years)
of age.
82, 89
Isoproterenol has also been evaluated as an indicator of
intravascular injection.
82
Studies are promising, but isoproterenol has not
been extensively evaluated for neurotoxic potential; supplies of this
medication in the United States are limited because of recent discontinu-
ation of production by several manufacturers.
Sympathetic Tone. A clinically signicant decrease in blood pres-
sure related to sympathectomy from central neuraxial blocks is rare in
children younger than 8 years of age.
65
Volume loading before such
blocks, commonly practiced in adults, is unnecessary in this age group.
In older patients, the sympathetic block results in a slight (20%25%)
but consistent decrease in blood pressure.
65
Even in adolescents, how-
ever, uids or vasopressors are rarely required to treat the hemodynamic
effects of central neuraxial blocks.
Contraindications. Contraindications are few and similar to those
in adults. These include coagulopathy, infection at the insertion site, true
Figure 1. Electrocardiographic changes associated with the intravenous injection of bupiva-
caine and epinephrine 1:200,000. Note the marked increase in the height of the T wave.
(From Freid EB, Bailey AG, Valley RD. Electrocardiographic and hemodynamic changes
associated with unintentional intravascular injection of bupivacaine with epinephrine in
children. Anesthesiology 1993; 79:394398; with permission.)
PRACTICAL PEDIATRIC REGIONAL ANESTHESIA 87
local anesthetic allergy, and abnormal supercial landmarks or lumbo-
sacral myelomeningocele because of the risk of malposition of the cord
or dural sac. Progressive neurologic disease is a relative contraindication
primarily because of medico-legal concerns. The safety of central neurax-
ial techniques in the presence of a ventriculoperitoneal shunt has not
been studied. Risks and benets in these patients should be carefully
considered on an individual basis.
Single-Shot Caudal Block
The single-dose or single-shot caudal technique is the most com-
monly used neuraxial block for children. Developmental anatomy contri-
butes to the ease of caudal needle placement and, therefore, the popular-
ity of the technique in young children compared with adults, for
example, shows that prepubertal children have less presacral fat, making
identication of the bony landmarks easier. Additionally, in children, the
sacral ligament is noncalcied and the hiatus is wide, further contribut-
ing to the ease of caudal needle placement. Caudal block is a useful
adjunct to general anesthesia in most procedures performed below the
umbilicus. In larger volumes (11.25 mL/kg) and in younger children,
it has been described for use in upper abdominal and lower thoracic
procedures.
33
It is the authors experience, however, that analgesia is less
reliable for procedures at this higher level. It is less commonly used as
the sole anesthetic technique, but has been described as an alternative
to spinal or general anesthesia for herniorrhaphy in preterm infants.
33, 37
Anatomy and Landmarks
The posterior superior iliac spines and the sacral hiatus form an
equilateral triangle, the apex of which points inferiorly. The sacral cornua
are easily palpated on either side of the sacral hiatus, approximately 0.5
to 1 cm apart (Fig. 2). The sacrum is the most variable bone in the
human body, hence the sacral foramina may be misidentied as the
sacral hiatus. The proper location is often, but not always, at the begin-
ning of the crease of the buttocks.
Equipment
A variety of needles have been used for single-shot caudal blocks,
including 23-gauge to 18-gauge straight needles, 23-gauge to 19-gauge
buttery needles, 22-gauge or 20-gauge styletted block needles, 22-gauge
spinal needles, and 22-gauge or 20-gauge intravenous needle cathe-
ters. Styletted needles prevent the introduction of a skin plug into the
epidural space that may later develop into an epidermal inclusion cyst.
Intravenous catheters offer the advantage of conrmation of correct
placement if the catheter easily slides off the needle.
88 SURESH & WHEELER
Figure 2. Sacral anatomy. A, Coronal view of the sacrum showing proper needle placement
for performance of a candal epidural block. The needle is advanced at a 45 angle to the
skin until the bone is contacted. The angle is then decreased from 15 to 30 and the
needle is advanced through the sacrococcygeal ligament into the epidural space. B,
Coronal view of the sacral anatomy demonstrating potential improper needle location during
a candal epidural block. (From Deshpande JK, Tobias JD, eds: The Pediatric Pain Hand-
book. St. Louis, Mosby; 1996: 100; with permission.)
PRACTICAL PEDIATRIC REGIONAL ANESTHESIA 89
Technique
The patient is positioned in the lateral decubitus position. After
identication of the sacral hiatus and sterile skin preparation, the needle
is advance at a 45 angle to the skin. A pop or give is felt as the
sacrococcygeal ligament is passed. In infants under 1 year of age, the
dural sac extends to the S4 level. Further needle advancement is not
recommended because of the risk of dural puncture. In older children,
the angle of the needle can be reduced and advanced slightly into the
canal. The needle should be aspirated for blood or cerebrospinal uid
(CSF) and, if negative, a test dose is given. Injection should be easy and
feel similar to injection of an epidural catheter in adults. Palpation of
the skin overlying the sacrum will help rule out supercial injection. Air
injection to check for crepitus is not recommended because of the risk
of air embolism.
31
Dosing and Duration of Block
One milliliter per kilogram of bupivacaine 0.125% with epinephrine
1:200,000 reliably produces 4 to 6 hours of analgesia. Higher concentra-
tions have been used, but motor blockade is signicantly increased
without improving the quality or duration of pain control. Alternatively,
ropivacaine 0.2% can be used in a dose of 1 mL/kg.
54
Clonidine 1 to 2
g/kg appears to prolong bupivacaine block with little additional
risk.
40, 53
Two case reports have suggested clonidine may be responsible
for apnea when used for caudal blocks in neonates, however.
8, 9
The
addition of opioids may increase the potency of the neuraxial block.
Fentanyl 1 to 2 g/kg may also prolong the block, but pruritus and
nausea or vomiting are increased.
13
Morphine (30 g/kg) has also been
used by this route, but side effects (nausea or vomiting and pruritus)
often occur and the increased risk of respiratory depression precludes
its use in outpatients.
Timing of Block
Few young children will cooperate with placement of a regional
block while awake. Blocks are placed after induction of anesthesia and
placement of an intravenous catheter. Prior placement of an intravenous
catheter is mandatory for treatment of complications related to accidental
spinal or intravascular injection. Blockade before the procedure reduces
anesthetic requirements and may have a preemptive analgesic benet.
39
Complications
Complications are unusualabout 1 per 1000 proceduresand usu-
ally minor.
27
Most complications result from misplacement of the needle
into supercial soft tissues or sacral foramina, resulting in block failure;
intrathecal puncture with subsequent spinal anesthesia; or intravascular
90 SURESH & WHEELER
or intraosseous injections, leading to systemic toxicity. Using proper
technique, including incremental injection, minimizes these complica-
tions. Urinary retention and motor blockade are rare with the recom-
mended solutions.
Continuous Caudal Catheter
Equipment
Several companies manufacture kits for caudal catheter placement.
A useful component is a clear plastic drape to better identify landmarks.
An 18- or 19-gauge needle (Crawford type) with a 20- or 21-gauge
catheter is used in patients of all sizes. Smaller catheters tend to kink
either at placement or during postoperative use. A styletted catheter has
been reported to increase the successful passage of catheters to the
thoracic level (discussed subsequently). After placement, care must be
taken to prevent fecal contamination because of the proximity of the
anus to the insertion site. Because of this risk, it is prudent to keep them
in for no longer than 3 days
47
and to discontinue caudal catheters if the
dressing becomes soiled.
Caudal-to-Thoracic Technique
The caudal approach to thoracic epidural anesthesia can be used in
children as old as 10 years of age. Success in this age group is related to
the less densely packed epidural fat that allows for free cephalad passage
of the catheter. Some authors suggest ease of removal of the stylet from
a styletted-type catheter, ease of injection, and negative aspiration and
test doses predict successful placement,
32
whereas others suggest radio-
graphic conrmation.
12
A case report suggests that nerve stimulation
through the catheter (19-gauge epidural catheter, Arrow Flextip Plus,
Arrow International Inc., Reading) using a low electrical current (1
10mA) can be used to identify correct placement.
92
The level of observed
intercostal muscle movement (T9T10 level) predicted catheter tip place-
ment at the T9T10 interspace and this was conrmed by radiographic
imaging.
92
Epidural Block
Anatomy and Landmarks
In adults, the line drawn between the two iliac crests passes over
the fourth lumbar vertebrae or the L3L4 interspace. In children, this
line may pass closer to the fth lumbar vertebrae and in neonates it may
pass over the L5S1 interspace.
10
Until 1 year of age, the spinal cord
ends at a lower level than in adults (L3 versus L1), as does the dural
sac (S4 versus S2). For a lumbar epidural block, it may be safer to select
PRACTICAL PEDIATRIC REGIONAL ANESTHESIA 91
the L4L5 or the L5S1 interspace for infants. Thoracic spine landmarks
are the roots of the scapular spines for T3 and the inferior angle of the
scapula for T7.
Technique and Identication of the Epidural Space
Although the patient can be in the sitting position if awake, the
most common position is lateral, with the surgical side down and the
hips and knees exed by 90. The spine is bent to open the interspinous
space and enlarge the interlaminar space. The midline lumbar interverte-
bral approach is the most common technique of epidural block in chil-
dren. As with adults, loss of resistance (LOR) is used in children for
identication of the epidural space. The site of puncture is in the midline,
midway between the spinous processes of the selected interspace. The
epidural needle is inserted at right angles to the skin until it contacts
the interspinous ligament. The introducer needle is then removed, and
the syringe used for detecting the epidural space is connected. The
epidural needle is then carefully advanced while constant pressure is
exerted on the plunger of the syringe. An increased resistance is detected
when the needle touches the ligamentum avum, followed by a sudden
LOR as the tip of the needle enters the epidural space.
The epidural space is more supercial in children than adults.
Several guidelines for determining epidural depth have been published.
6,
36, 97
None is consistently accurate, though a rough estimate for children
between 6 months and 10 years of age is a depth of 1 mm/kg of body
weight. Other formulas are depth (cm) 1 0.15 age (years) and
depth (cm) 0.8 0.05 weight (kg).
36
The mean depth of epidural
space in neonates has been reported as 1 cm (SD 0.2, range 0.41.5 cm).
36
The best protection against excessive depth and resultant dural puncture
is appropriately short needles and extreme care during advancement of
the needle. Once the needle is in the epidural space, the absence of
blood or CSF reux is veried before insertion of the catheter. A test
dose of the local anesthetic with epinephrine is administered before
every bolus injection.
Whether air or saline should be used to detect LOR continues to be
debated.
75, 80
Air has a long history of use because of its availability,
simplicity, and suitability for identifying the epidural space. Several
severe complications have been reported after injection of air into the
epidural space, including paraplegia
67
and multiradicular syndrome in
adults
63
and air embolism in children.
31, 79, 81
These complications have
led some practitioners to recommend abandoning the air-LOR technique
in favor of a saline-LOR technique.
30, 75
In younger patients, some prac-
titioners believe the saline-LOR technique is not as dependable as the
air-LOR technique.
11
Other possible disadvantages of the saline-LOR
technique are dilution of the local anesthetic and difculty distinguish-
ing a reux of saline from CSF. Because of the limitations of this tech-
nique, some practitioners combine air and saline.
4, 29
In general, the
riskbenet ratio seems to favor the use of saline in most circumstances.
92 SURESH & WHEELER
The most prudent course of action is to always proceed cautiously
and avoid injection of large volumes of any test substrate, whether air
or saline.
Dosing
The recommended volume of anesthetic solution depends on the
upper level of analgesia necessary for completion of the surgery. Many
dosing schemes have been reported. In children older than 10 years of
age, a simple formula calculates the volume (V) necessary to block one
spinal segment
78
:
V (in mL) 1/10 (age in years)
In younger children, the weight of the patient should be considered;
0.04 mL/kg/segment provides an initial bolus-dose estimate. Keep in
mind the maximum dose recommendations (Table 2). If adequate levels
are achieved, redosing after 1 to 2 hours with half the initial volume is
reasonable. Alternatively, a continuous infusion can be started immedi-
ately after the bolus injection. Recommended solutions and infusion
rates are available in standard pediatric anesthesia textbooks.
98
Infants
younger than 12 months of age are prone to accumulation with pro-
longed continuous bupivacaine infusions, so infusion rates should be
reduced in this age group.
51, 72
Lumbar-to-Thoracic Catheter
In contrast to caudal-to-thoracic catheter placement, attempts to
thread a catheter from the lumbar interspaces to the thoracic level are
rarely successful.
5
This is probably related to the more acute angulation
of a catheter placed in the lumbar region. If this technique is attempted,
radiographic conrmation of correct placement is recommended.
Epidural Placement During General Anesthesia
Krane et al
49
have eloquently made the case supporting epidural
placement during general anesthesia in an editorial supported by more
than fty pediatric anesthesiologists from all around the world. For
children, to avoid movement during performance of a block, sedation
or general anesthesia is almost always required. Two concerns regarding
Table 2. LOCAL ANESTHETIC MAXIMUM DOSING GUIDELINES BY WEIGHT
Bolus Dose (mg/kg) Infusion Rates (mg/kg/hour)
Local Anesthetic Infants 6 Months Child Infants 6 Months Child
Bupivacaine 1.5 2.5 0.2 0.4
Chloroprocaine 10 10 18 18
Lidocaine 3 .5 0.8 1.6
PRACTICAL PEDIATRIC REGIONAL ANESTHESIA 93
this practice are reduced reliability of test dose under anesthesia and
neurologic damage secondary to the inability of the patient to report
pain or paresthesia. Data on thousands of pediatric patients do not
support the second concern, and careful attention to technique substan-
tially reduces the possibility of intravascular injection.
22, 27, 66
Complications
The potential complications of epidural anesthesia in children are
the same as those in adults. As in caudal blocks, accidental intrathecal
or intravascular injection may occur. Failure or difculties may occur
because of an inappropriate insertion route, insufcient exion of the
spine, or deformities of the vertebral column. Direct trauma to the spinal
cord can occur during thoracic and upper lumbar approaches and may
result in the same neurologic sequelae as reported in adults. Fortunately,
these sequelae are extremely unusual in children. In the French Lan-
guage Society of Pediatric Anesthesiologists (ADARPEFs) prospective
study, no complication was reported following thoracic epidurals,
whereas the overall morbidity rate was 0.37% and 0.68% for lumbar and
sacral epidurals, respectively.
27
The morbidity rate for thoracic epidurals
may have been skewed because only experienced anesthesiologists per-
formed that block. As for adults, epidural catheters may be malposi-
tioned, disconnected, or broken. Complete failure of the block usually
results from misplacement of the needle or catheter. In a previously
functional catheter, the development of new respiratory depression or
increasing motor weakness may reect migration into the subarachnoid
space. Unilateral blockade is often caused by migration of the catheter
through a spinal foramina. Migration of the catheter into an epidural
vein may cause loss of analgesia and increased sedation if opioids
are being used. The administration of epidural opioids, particularly
morphine, may lead to delayed respiratory depression. All opioids have
the potential to cause nausea, or pruritus. The incidence of urinary
retention is difcult to determine because it is the practice of many
centers to prophylactically place a urinary drainage catheter in these
patients.
Catheter Management for Postoperative Pain
Successful use of continuous catheter techniques for postoperative
pain requires physicians dedicated to their management and an educated
nursing staff comfortable with monitoring and caring for these patients.
Preprinted order sheets indicating infusion solutions and dosing, moni-
toring, patient assessment, and side-effect management increase safety
and success. The article on postoperative pain management in this issue
provides additional information on dosage and catheter management.
94 SURESH & WHEELER
Spinal Anesthesia
In pediatric practice, spinal anesthesia is used mainly for inguinal
hernia repair in former preterm infants to reduce the risk of postopera-
tive apnea. Infants born at less than 37 weeks gestational age and less
than 60 weeks postconceptional age at the time of surgery are at risk for
apnea after general anesthesia. Those presenting with continuing apnea
at home or anemia (hematocrit 30%)
14
are at even greater risk. This
complication appears to be reduced, though not eliminated, following
spinal anesthesia without concomitant sedation.
15, 24, 25, 35, 50, 77
Of note,
apnea may even be increased if regional anesthesia is combined with
sedation (ketamine, midazolam).
94
Spinal anesthesia is less commonly
used in older children in the United States, but several European reports
suggest its safety and efcacy in select cases.
45, 46
Equipment
Short styletted spinal needles, from 22- to 27-gauge, are available
for pediatric spinal anesthesia. In former preterm infants, medications
are best delivered using 1-mL syringes because of the small volumes
required.
Patient Positioning
Lumbar puncture can be performed in the same positions as for
lumbar epidural anesthesia. For the former preterm infant, it is easier
when the infant is in the sitting position. In the sitting position, the
assistant holds the infant so that both arms and legs are bent and the
elbows and knees are brought together. This helps to keep the infant in
position and maximally opens the intervertebral spaces. Attention must
be paid to the position of the head, which must be extended away from
the chest to avoid airway obstruction.
Technique
The technique does not differ from that used in adults. In infants,
puncture is performed in the midline, at the L4L5 interspace, to stay
below the level of the spinal cord. Some practitioners use local anesthesia
at the skin puncture site. The usual depth is several millimeters past
that calculated for depth of the epidural space (discussed earlier). After
reux of CSF from the needle, the syringe is quickly attached to mini-
mize CSF loss and the solution is injected in 10 to 20 seconds. Particu-
larly for infants, in whom the total volume injected are very small, some
practitioners advocate aspiration of spinal uid into the syringe at the
end of the block and then reinjection to assure that the complete dose is
administered. Others intentionally overll the syringe with the volume
of the spinal needle. Patients should be carefully returned to the supine
position, without elevating the legs, after completion of the block.
96
PRACTICAL PEDIATRIC REGIONAL ANESTHESIA 95
Dosing
In general, younger and smaller children require larger doses to
produce the same level of block, but the duration of the effect is shorter.
Dosing recommendations for spinal anesthesia vary and are summarized
in Table 3. Guidelines given are designed to reach an upper limit of block
between T10 and T7. The safety of hyperbaric lidocaine has recently been
questioned in adults because of the high incidence of transient neuro-
logic symptoms (TNS) following its use.
38, 42, 55
These symptoms usually
consist of back and buttock pain. Cauda equina syndrome has been
reported in adults.
26, 55
The US Food and Drug Administration recom-
mends diluting 5% lidocaine with an equal volume of cerebrospinal
uid before injecting the total dose, but at least one study suggests
this does not inuence the incidence of TNS.
76
Although reducing the
concentration of lidocaine to 2% has been found to provide effective
analgesia,
57, 71
the incidence of TNS may be unaffected.
34
In general, for
spinal anesthesia in preterm infants, lidocaine is unsuitable because its
duration of action is too brief.
Complications
Few studies evaluate overall incidence of complications for spinal
anesthesia in children. In the ADARPEFs prospective study, only one
complication (intravascular injection) was reported after 506 spinal anes-
thetics. No headaches were reported.
27
In a retrospective study by the
same association, the incidence of complications after spinal anesthesia
(n705) was 3% and is described as extension of the blockapnea,
seizures.
22
Recently, a report of spinal anesthesia in 100 children, age 2
to 115 months, found few complications using 0.5% isobaric or hypobaric
bupivacaine. Overall, cardiovascular stability was good. A vasopressor
was administered to one child to treat hypotension and atropine to
another to treat bradycardia. Five children developed a mild, position-
dependent headache (2427-gauge needle).
46
A report of experience with
107 spinal anesthetics in children age 7 to 18 years found that six
children required vasopressor and six required atropine to treat brady-
cardia. Nausea (20 patients) and shivering (16 patients) were also re-
ported. Four children had post-dural puncture headaches (27-gauge
needle).
45
High spinal anesthesia has been reported in infants when the
legs are raised shortly after placement of the block.
96
Care must be taken
to avoid this scenario. A report of inguinal hernia repairs in former
preterm infants found 262 of 269 spinal anesthetic placements (97.3%)
were successful.
24
Sixteen patients required two attempts; 56 (21.4%)
required supplemental anesthesia; 34, intravenous anesthesia; six, gen-
eral; 12, local; and four, other regional. One hundred fty-three infants
had histories of apnea. Thirteen episodes of apnea were noted in 13
infants (4.9%); all 13 were inpatients undergoing concomitant therapy
for apnea (mean gestational age [GA] 28 weeks, postconceptional age at
surgery [PCAS], 42.9 weeks). Four of these infants received supplemental
Table 3. RECOMMENDED DOSES AND APPROXIMATE DURATIONS OF LOCAL ANESTHETICS FOR SPINAL ANESTHESIA IN INFANTS AND
CHILDREN
Local Anesthetic 05 kg 515 kg 15 kg Duration
0.75% hyperbaric bupivacaine 0.50.6 mg/kg 0.4 mg/kg 0.3 mg/kg 70 min
(0.060.08 mL/kg) (0.053 mL/kg) (0.04 mL/kg) (similar to 0.5% bupivacaine)
0.5% hyperbaric or isobaric bupivacaine 0.50.6 mg/kg 0.4 mg/kg 0.3 mg/kg 30180 min
(0.10.12 mL/kg) (0.08 mL/kg) (0.06 mL/kg) (avg 80 min)
0.5% hyperbaric tetracaine 0.50.6 mg/kg 0.4 mg/kg 0.3 mg/kg 35240 min
(0.10.12 mL/kg) (0.08 mL/kg) (0.06 mL/kg) (avg 90 min)
5% hyperbaric lidocaine 2.53 mg/kg 2 mg/kg 1.5 mg/kg 60 min
(0.050.06 mL/kg) (0.04 mL/kg) (0.03 mL/kg)
*Adapted from Dalens BJ: Regional anesthesia in children (chapter 44). In Miller RD, (ed): Anesthesia. Philadelphia, Churchill Livingstone, 2000, p 1565; with permission.
9
6
PRACTICAL PEDIATRIC REGIONAL ANESTHESIA 97
anesthesia. This apnea rate is signicantly lower than the published rate
(10%30%) (P .01). Thirty-nine of 103 infants who underwent inguinal
hernia repair on an outpatient basis had histories of apnea. No postoper-
ative episode of apnea was reported, though patients were not moni-
tored for apnea at home. The mean birth weight of this group was 2091
g (weight range, 7103693 g); mean GA, 33 weeks (GA range, 2537
weeks); and mean PCAS, 44.3 weeks (PCAS range, 35.459.2 weeks).
24
Unlike adults, neonates usually tolerate high thoracic spinal anesthesia
with minimal changes in heart rate and arterial blood pressure. This
may be because the sympatholysis from high thoracic spinal anesthesia
is offset by withdrawal of cardiac vagal activity in this age group.
70
Cases of aseptic meningitis after spinal anesthesia in infants have been
reported, but a causative relation cannot be rmly established.
1, 19
PERIPHERAL NERVE BLOCKS
Peripheral nerve blocks used for surgery and postoperative pain
relief are discussed by anatomic regions (Table 4). Very little equipment
is needed to perform these blocksblunt-tip needles and a nerve stimu-
lator capable of providing low-voltage (0.01 mV) electric stimulation.
Local anesthetic selection is based on the duration of the surgical proce-
dure and the desired duration of the block. Lidocaine, mepivacaine,
bupivacaine, ropivacaine and, more recently, levobupivacaine are used
for peripheral nerve blocks. The addition of bicarbonate may enhance
the speed of onset of the nerve block and reduce the pain on injection.
Table 4. PERIPHERAL NERVE BLOCKS
Region Nerve to be Blocked
Head and neck Supraorbital and supratrochlear
Infraorbital nerve
Greater occipital nerve
Great auricular nerve
Chest wall Intercostal nerve
Upper extremities Brachial plexus
Wrist blocks
Elbow (radial, ulnar, and median)
Digital nerve
Abdomen and genitals Ilioinguinal nerve, penile
Lower extremities Femoral nerve
Lateral femoral cutaneous
Sciatic nerve
Ankle block
Digital nerve
Adapted from Polaner D, Suresh S, Cote CJ: Pediatric regional anesthesia. In Cote C, Todres ID,
Ryan JF et al (eds): A Practice of Anesthesia for Infants and Children. Philadelphia, WB Saunders, 2000,
pp 636675; with permission.
98 SURESH & WHEELER
This alters the pKa of the solution, making the local anesthetic available
in the active cationic form.
95
Caution is required to avoid exceeding the
maximum allowable dose of the local anesthetic. The total volume of
local anesthetic required for a peripheral nerve block is extrapolated
from adult experience.
Relative Contraindications to Peripheral Blocks
Though it is rare to encounter opposition to the use of peripheral
nerve blocks, certain conditions may call for a judicious avoidance of
them. Relative contraindications include:
Local infection
Generalized sepsis
Coagulopathy
Predisposition to compartment syndrome
Parental or child dissent
Nerve Stimulator
Though not a substitute for anatomic knowledge, a nerve stimulator
is useful to localize peripheral motor nerves in anesthetized children.
Because paresthesias cannot be elicited in an anesthetized child, the use
of a nerve stimulator may decrease the potential for nerve damage. A
nerve stimulator capable of delivering low voltage is preferred. The
authors prefer stimulation with an insulated needle using a voltage of
0.2 mA with a repetitive single-pole output at a 1-second interval. The
area innervated by the nerve is observed for the appropriate muscle
contraction. When this has been identied, 1 to 2 mL of local anesthetic
agent is injected. Immediate abolishment of muscle movement indicates
correct placement of the needle.
Head and Neck Nerve Blocks
The trigeminal nerve provides sensory innervation to the scalp and
the face. The ophthalmic division of the trigeminal nerve (V
1
) supplies
the scalp anterior to the coronal suture, and the branches of the cervical
nerve (C
2
) supply the scalp posterior to the coronal suture.
Supraorbital and Supratrochlear Nerve. Anatomy and Indication.
These are the terminal branches of the rst branch of the V
1
. The
supraorbital nerve supplies the forehead and the scalp anterior to the
coronal suture after it exits the supraorbital foramen. The supratrochlear
nerve leaves the orbit between the trochlea and the supraorbital foramen
and supplies the forehead (Fig. 3). Blockade of these nerves can be used
for surgical excisions of skin lesions on the scalp
84
and for neurosurgical
PRACTICAL PEDIATRIC REGIONAL ANESTHESIA 99
Figure 3. Supraorbital and supratrochlear nerve blocks. (From Cote CJ, Todres ID, Goud-
souzian NG, et al (eds): A Practice of Anesthesia for Infants and Children, 3rd ed.
Philadelphia: WB Saunders; 2001: 644; with permission.)
procedures that involve incisions on the anterior portion of the scalp.
The authors have also had success treating patients with chronic head-
aches with serial blockades of these nerves.
Technique. Using a sterile technique, the supraorbital notch is identi-
ed, and a 27-gauge needle is inserted perpendicularly. Once resistance
is obtained, the needle is drawn back a few millimeters and 1 mL of
0.25% bupivacaine with 1:200,000 epinephrine is injected to block the
supraorbital nerve. The needle is then withdrawn gently and directed
medially to block the supratrochlear nerve, and an additional 1 mL of
0.25% bupivacaine with 1:200,000 epinephrine is injected.
Complications. Pressure is applied to the supraorbital area after the
block is performed to avoid periorbital edema and ecchymosis secondary
to local anesthetic solution dissecting into the surrounding loose adventi-
tious tissue or from hematoma formation.
Greater Occipital Nerve Block. Anatomy and Indications. The
greater occipital nerve is a terminal branch of the supercial cervical
plexus (dorsal rami of C2). The nerve becomes subcutaneous below the
superior nuchal line by passing above the aponeurotic sling just medial
to the occipital artery (Fig. 4). Blockade of this nerve provides ipsilateral
pain relief for patients undergoing occipital incisions, including craniot-
omies for posterior fossa tumors and posterior ventriculo-peritoneal
100 SURESH & WHEELER
Figure 4. Greater occipital nerve block. (From Cote CJ, Todres ID, Goudsouzian NG, et al
(eds): A Practice of Anesthesia for Infants and Children 3rd ed. Philadelphia, WB Saunders,
2001, p 644; with permission.)
shunts. Blockade can also provide anesthesia for excision of skin lesions
on the scalp.
84
Technique. The head is turned to the side opposite the side to be
blocked. The occipital artery is palpated at the level of the superior
nuchal line. Subcutaneous fanning of 2 mL 0.25% bupivacaine with 1:
200,000 epinephrine is performed.
Complications. Though complications are rare, it is important to
note the proximity to the spinal canal. Particular caution should be
exercised in patients who have had surgery to the posterior fossa.
Intravascular injection can be avoided by careful aspiration.
Infraorbital Block. Anatomy and Indications. The infraorbital nerve
is the terminal branch of the second division of the trigeminal nerve and
is purely sensory. It leaves the skull through the foramen rotundum and
enters the pterygopalatine fossa. Here it exits the infraorbital foramen,
dividing into four branchesthe inferior palpebral, the external nasal,
the internal nasal, and the superior labial. These branches innervate the
lower lid, the lateral inferior portion of the nose and its vestibule, the
upper lip, the mucosa along the upper lip, and the vermilion. This block
can be used to provide postoperative analgesia for procedures performed
to the upper lip and vermilion (e.g., cleft lip repair).
7, 74
It can also
be used for nasal septal reconstruction, rhinoplasty, and in patients
undergoing endoscopic sinus surgery.
PRACTICAL PEDIATRIC REGIONAL ANESTHESIA 101
Technique. Although two approaches are described (intraoral and
extraoral), the authors prefer the intraoral approach. After palpation of
the infraorbital foramen, the upper lip is folded back and a 27-gauge
needle is advanced to the infraorbital foramen parallel to the maxillary
premolar (Fig. 5). By placing a nger at the level of the infraorbital
foramen, the cephalad progression of the needle is checked. A volume
of 0.5 mL to 1 mL of 0.25% bupivacaine with 1:200,000 epinephrine is
injected after careful aspiration.
Complications. Swelling can occur because of loose adventitious
tissue around the eyelid. To prevent this, pressure is applied to the area
for about 5 minutes after the block is performed. Patients and parents
should be informed that the upper lip will be anesthetized after the
block.
Great Auricular Nerve. Anatomy and Indications. This nerve sup-
plies the sensory innervation to the mastoid and the external ear.
84
It is
a branch of the supercial cervical plexus (C3). The nerve wraps around
the posterior border of the belly of the clavicular head of the sternoclei-
Figure 5. Infraorbital nerve block. (From Cote CJ, Todres ID, Goudsouzian NG, et al (eds):
A Practice of Anesthesia for Infants and Children, 3rd ed. Philadelphia: WB Saunders;
2001: 655; with permission.)
102 SURESH & WHEELER
domastoid at the level of the cricoid cartilage (C6)
58
(Fig. 6). Blocking
this nerve provides analgesia for patients undergoing otoplasty repair
16
and tympanomastoid surgery. The authors have found that using this
nerve block, can reduce the postoperative morbidity associated with the
perioperative use of opioids.
Technique. The belly of the clavicular head of the sternocleidomas-
toid is identied, and a line drawn laterally at the level of the cricoid
dissecting the sternocleidomastoid is marked. This is usually about 5 to
6 cm below the bony external auditory canal. Two to 3 mL of 0.25%
bupivacaine with 1:200,000 epinephrine are injected into the area.
Complications. Careful attention to the location of the external
jugular and carotid can prevent intravascular placement. Supercial
needle placement avoids a deep cervical plexus block that can result in
Horners syndrome. Deep injection can also affect the hemidiaphragm
by blocking the phrenic nerve unilaterally or the trapezius by blocking
the spinal accessory nerve.
Figure 6. Great auricular nerve block. (From Cote CJ, Todres ID, Goudsouzian NG, et al
(eds): A Practice of Anesthesia for Infants and Children, 3rd ed. Philadelphia, WB Saunders;
2001, 655; with permission.)
PRACTICAL PEDIATRIC REGIONAL ANESTHESIA 103
Trunk Blocks
Intercostal Nerve Blocks
Anatomy and Indications. The intercostal nerves are derived from
the ventral rami of the rst through the twelfth thoracic nerves. There
are four branches for each intercostal nervethe gray rami communi-
cans that passes to the sympathetic ganglion; the posterior cutaneous
branch, supplying the skin of the paravertebral area; the lateral cutane-
ous branch, supplying the lateral aspect of the lateral and anterior
portions of the chest wall; and the terminal branch, providing sensory
bers to the anterior portions of the chest and abdomen. Intercostal
nerve blocks can be used for isolated surgical elds. They are also used
to manage the pain of postherpetic neuralgia.
Technique. The authors prefer the anterior approach through the
midaxillary line. A 27-gauge needle is placed into the skin over the rib
at the level of the anterior axillary line. The skin is gently pulled caudad.
This allows the needle to fall in the sulcus below the rib. After careful
aspiration, 2 to 3 mL of 0.25% bupivacaine with epinephrine are injected.
For a lesion or surgical eld that covers several dermatomes, however,
the authors choice of analgesia is the placement of a thoracic epidural
catheter (see previous section on central neuraxial blockade).
Complications. Intravascular injection, local anesthetic toxicity with
the use of large volumes of local anesthetic, and pneumothorax from the
needle puncturing the pleural cavity have been reported.
64
With the
posterior approach, there is a risk for subarachnoid injection because the
sheath communicates directly with the subarachnoid space.
Abdomen Blocks
Ilioinguinal and Iliohypogastric Nerve Blocks
Anatomy and Indications. The subcostal nerve (T12) and the ilioin-
guinal and iliohypogastric nerves (derived from L1) innervate the ingui-
nal area. The ilioinguinal and iliohypogastric nerves pass over the ante-
rior superior iliac spine (ASIS) and, after piercing the internal oblique
aponeurosis about 2 to 3 cm medial to the ASIS, travel between the
internal and external oblique aponeurosis. Here they lie in close proxim-
ity to the spermatic cord and accompany the cord structures to the
genitals. This block can be used for hernia repairs and other surgeries
in the groin, including orchidopexy. Recent literature contradicts the
popular belief that this block, when performed preemptively, may lead
to signicant preemptive analgesia.
28
Technique. The ASIS is palpated. A point is marked 1.5 cm below
and medial to the ASIS. The cord structures are palpated and a 27-gauge
needle is placed into the area. Occasionally, a pop may be felt as the
sheath is entered. Five to 10 mL of 0.25% bupivacaine with 1:200,000
epinephrine are injected.
104 SURESH & WHEELER
Complications. Although rare, there is the possibility of a hema-
toma developing in the area after injection.
Penile Blocks
Anatomy and Indications. The nerve supply of the penis is from
the pudendal nerve and the pelvic plexus. Two dorsal nerves of the
penis separate at the level of the symphysis pubis. These are terminal
branches of the pudendal nerve. This block can be used for circumci-
sion
52
and other penile procedures when caudal blocks may be contrain-
dicated.
Techniques. Two methods are commonly useda ring block and
direct blockade of the dorsal nerves of the penis. For either technique,
epinephrine should be avoided in the block solution to prevent ischemia.
Care should be taken to avoid intravascular placement. To place a ring
block, a ring of 0.25% plain bupivacaine is injected around the base of
the penis. To block the dorsal nerves of the penis, a 27-gauge needle is
inserted 1 cm above the symphysis pubis. The needle is advanced 1 cm
after it pierces the penile fascia. After aspiration, 2 mL of 0.25% bupiva-
caine without epinephrine are injected slowly. The needle is then with-
drawn and directed to the 2 oclock position. Two to 3 mL of plain
bupivacaine are injected. The needle is again withdrawn and then di-
rected to the 10 oclock position. Two to 3 mL of local anesthetic solution
are injected.
Complications. There is a mild risk of compromise to organ blood
ow with the ring block. Applying pressure at the base of the penis can
minimize hematoma formation after the block.
Upper Extremity Blocks
Brachial Plexus Block
Several approaches to the brachial plexus are described in adults.
These include the axillary, the interscalene, the supraclavicular, and the
infraclavicular approaches. The axillary approach is the most commonly
used technique for brachial plexus block in children.
Anatomy and Indications. The anatomy of the brachial plexus is
described in detail in many standard anesthesia textbooks. It arises from
the C5, C6, C7, C8, and T1 nerve roots. In children, the axillary sheath,
as well as the axillary artery, are easily palpated.
91
Axillary nerve blocks
can be used for procedures in the hand and arm that require prolonged
pain relief.
69
This can increase blood ow by decreasing the sympathetic
tone. It can be used for placement of an Ilizarov device for the arm as
well as for reimplantation of severed ngers.
Technique. The arm is abducted to a 90 angle. The artery is pal-
pated in the axilla. The use of a nerve stimulator allows accurate place-
ment of the needle in the neurovascular sheath without trying to elicit
PRACTICAL PEDIATRIC REGIONAL ANESTHESIA 105
paresthesia. The axillary sheath is divided into fascial compartments for
each nerve. These may limit spread of the local anesthetic in the sheath.
The transarterial approach involves direct puncture of the axillary artery.
The needle is then advanced further into the sheath. Once blood is no
longer aspirated, half the total volume of local anesthetic is injected. The
needle is then pulled back beyond the artery and the other half of the
local anesthetic is injected. The total dose of local anesthetic injected is 1
mL/kg of 0.25% bupivacaine or 1 mL/kg of 0.2% ropivacaine, up to a
maximum dose of 40 mL. Regardless of technique, careful aspiration
should be carried out before injection to eliminate intravascular local
anesthetic injection. An additional cuff of local anesthetic is injected as
a subcutaneous cuff to block the intercostobrachial nerve so that tourni-
quet pain is not experienced.
Another approach is using multiple injections with the aid of a
nerve stimulator. The needle is advanced into the facial sheath at a 45
angle to the skin above the pulsation of the axillary artery. When a
twitch is elicited in the appropriate muscle group with the nerve stimula-
tor, local anesthetic solution is injected. A ring of local anesthetic should
be injected around the upper aspect of the arm. This will block the
intercostobrachial nerve, which will provide analgesia for tourniquet-
related pain.
Complications. A hematoma may form because of puncture of the
axillary artery. This is usually self contained and can be prevented by
applying pressure to the area.
Lower Extremity Blocks
Caudal blocks are more commonly used for lower extremity proce-
dures, but when a caudal block is contraindicated, a peripheral block
should be considered.
Sciatic Nerve Block
Anatomy and indications. The sciatic nerve arises from the L4, L5,
and S1 roots of the sacral plexus. It passes through the pelvis and is
supercial at the lower margin of the gluteus maximus muscle. It then
descends in the posterior aspect of the thigh, supplying sensory innerva-
tion to the entire posterior thigh and the leg and foot below the ankle,
except the medial aspect, which is supplied by the femoral nerve. This
block can be used for surgery below the knee. In combination with a
femoral nerve block, complete analgesia of the leg and foot can be
obtained. The authors use this block for unilateral club foot repair and
for triple arthrodeses of the foot.
Technique. Although the posterior approach is most commonly
used in adult practice, it may be difcult in the anesthetized pediatric
106 SURESH & WHEELER
patient. The authors prefer the lateral approach to the popliteal fossa to
block the sciatic nerve. This has a longer duration of analgesia in adults.
59
Anatomy and Indications. The popliteal fossa is a diamond-shaped
area located behind the knee, bordered laterally by the biceps femoris
tendon and medially by the semitendinosus and semimembranosus
muscles. The sciatic nerve, in adolescents, divides approximately 5 to 6
cm above the crease of the knee into its two major branches, the tibial
nerve medially and the common peroneal nerve laterally.
Technique. The lower leg is elevated on a pillow. The biceps femoris
tendon is palpated. After sterile preparation, an insulated needle with a
nerve stimulator attached is introduced at about 5 cm above the crease
of the knee. Using low-voltage (0.2 mV0.3 mV) electrical stimulation,
the needle is slowly introduced anterior to the tendon (Fig. 7). Dorsiex-
ion or plantar exion of the foot is seen when the needle is in approxi-
mately the right position. On injection, this response is eliminated,
suggesting correct placement of the needle. Five milliliters (in infants
and toddlers) to 15 mL (in adolescents) of 0.25% bupivacaine with
epinephrine 1:200,000 are injected into the space. Careful aspiration is
carried out to avoid intravascular injection.
Complications. Intraneural placement can be prevented by using a
nerve stimulator. Though rare, intravascular placement should be pre-
vented by careful aspiration.
Figure 7. Lateral popliteal sciatic nerve block. (From Cote CJ, Todres ID, Ryan JF, et al
(eds): A Practice of Anesthesia for Infants and Children, 3rd ed. Philadelphia: WB Saunders;
2001: 655; with permission.)
PRACTICAL PEDIATRIC REGIONAL ANESTHESIA 107
Femoral Nerve Block
Anatomy and Indications. The femoral nerve is located immedi-
ately lateral to the femoral artery in the inguinal area. This block is
useful for surgery on the shaft of the femur.
18, 90
This can be performed
on arrival to the hospital to prevent pain caused by transport and other
manipulations.
Techniques. Because this is a motor nerve, the use of a nerve
stimulator is desirable. Look for movement of the knee and the adduc-
tors. In adolescents, a volume of 10 to 15 mL of 0.25% bupivacaine
with epinephrine 1:200,000 are injected into the fascial sheath. Another
technique is to use a blunt needle to enter the femoral sheath. After the
second pop, the needle will be in the femoral sheath. Following careful
aspiration, 10 to 15 mL of local are anesthetic are injected.
Complications. Bleeding and hematoma formation from the femoral
artery and intraneural placement are the two major complications of
this block.
Lateral Femoral Cutaneous Nerve Block
Anatomy and Indications. This nerve arises from the L2 and L3
roots of the lumbar plexus. It traverses the lateral border of the psoas
muscle and passes obliquely under the fascia iliaca to enter the lateral
aspect of the thigh. It is a pure sensory nerve, providing sensory bers
to the lateral portion of the thigh. Blockade can be used to provide
analgesia to the lateral aspect of the thigh for skin and bone graft
procurement and muscle biopsies.
43, 56
Technique. A point 2-cm caudal and medial to the ASIS is located
on the side to be blocked. The authors prefer using a blunt needle that
is advanced slowly into the sheath. A distinct pop is felt as the needle
enters the fascia iliaca compartment. In adolescents, 10 to 15 mL of
0.25% bupivacaine with epinephrine 1:200,000 are injected after careful
aspiration.
Complications. It is rare to see complications from this nerve block.
Intraneural injection can cause dysesthesia that can last for a few weeks,
however.
Ankle Block
Anatomy and Indications. The nerves for the ankle are primarily
derived from the lumbo-sacral plexus, L4, L5, S1, S2, and S3 roots.
68
Five
nerves supply the ankletibial, supplying the sole of the foot; deep
peroneal, supplying the web between the great toe and the middle toe;
supercial peroneal, supplying the dorsum of the foot; saphenous, a
branch of the femoral nerve supplying the medial aspect of the foot; and
sural, supplying the lateral aspect of the foot.
Technique. Because it is not necessary to elicit paresthesias while
these nerves are located, an ankle block can be performed in the sedated
108 SURESH & WHEELER
patient without the use of a nerve stimulator. A 25-gauge needle is
usually used to inject the local anesthetic. In adolescents, a volume of 5
to 10 mL for each of the nerves to be blocked may be necessary.
Tibial nerve: A 27-gauge needle is inserted at the posterior angle
of the tibia lateral to the pulsation of the tibial artery until bony
contact is made. The needle is then pulled back a few millimeters
and 5 to 10 mL of 0.25% plain bupivacaine are injected.
Deep peroneal nerve: This nerve continues midway between the
malleoli onto the dorsum of the feet. A 27-gauge needle is inserted
between the anterior tibial and the extensor hallucis longus ten-
dons. This is usually lateral to the pulsation of the dorsalis pedis
artery. The needle is advanced until the bony surface of the tibia
is felt. It is then withdrawn a few millimeters and 3 to 5 mL of
0.25% bupivacaine are injected.
Supercial peroneal nerve: This nerve perforates the deep fascia
and runs along the anterior aspect of the dorsum of the foot. A
subcutaneous inltration of 3 to 4 mL of local anesthetic solution
between the medial and lateral malleolus can block this nerve.
Sural nerve: This is a cutaneous nerve that arises from the union
of a branch of the tibial and the common peroneal nerves. It runs
below and lateral to the lateral malleolus. A 27-gauge needle is
inserted below the lateral malleolus toward the bula. Three to 5
mL of plain 0.25% bupivacaine are injected.
Saphenous nerve: This is the terminal sensory branch of the femoral
nerve. A skin wheal placed above and medial to the medial
malleolus will block the saphenous nerve.
Digital Nerve Blocks
Anatomy and Indications. Digital nerves supply all ngers and
toes. In the hand, the common digital nerves are derived from the
median and ulnar nerves and divide in the palm to volar digital nerves
that supply the ngers. All digital nerves have accompanying digital
arteries. The digital nerves of the foot are derived from the plantar
cutaneous branches of the tibial nerve. Digital blocks can be used for
providing analgesia for ingrown toenails, laser treatment of warts,
93
traumatic injuries of the nailbed, and for ischemia secondary to Ray-
nauds phenomenon related to collagen vascular disease.
Techniques. Thumb. With the thumb extended, a 27-gauge needle
is inserted into the palmar surface of the hand between the index nger
and thumb. The needle is advanced to the junction of the web space
and the palmar skin of the hand. One mL of local anesthesia without
epinephrine is injected after careful aspiration to prevent intravascular
placement.
Other ngers. Digital nerves for the other ngers can be blocked by
placing a 27-gauge needle into the web about 3 mm proximal to the
PRACTICAL PEDIATRIC REGIONAL ANESTHESIA 109
junction between the web and the palmar skin; 1 mL of 0.25% bupiva-
caine without epinephrine is injected into each web space.
Toes. These techniques can be difcult to perform because of the
thickness of the overlying skin. A dorsolateral approach is preferred, in
which the web space is accessed from the dorsum of the foot; 1 mL of
local anesthetic without epinephrine is injected into each web space.
Complications. Large volumes can cause ischemia through pressure.
Vasoconstrictors should be avoided because they may lead to ischemia
and necrosis of the digit.
SUMMARY
In children, regional anesthetic techniques are safe and effective
adjuncts to general anesthesia and for postoperative pain relief. Applica-
tion of the techniques described in this article will contribute to im-
proved care for pediatric patients undergoing surgical procedures. The
judicious choice of local anesthetics, along with the blockades of targeted
nerves, decrease the need for supplemental analgesics in the recovery
phase.
References
1. Abouleish A, Nguyen NC, Mayhew JF: Aseptic meningitis after spinal anesthesia in
an infant. Anesthesiology 92:12001201, 2000
2. Anand KJ: Pain, plasticity, and premature birth: A prescription for permanent suffer-
ing? Nat Med 6:971973, 2000
3. Bardsley H, Gristwood R, Baker H, et al: A comparison of the cardiovascular effects of
levobupivacaine and rac- bupivacaine following intravenous administration to healthy
volunteers. Br J Clin Pharmacol 46:245249, 1998
4. Barros S: Loss-of-resistance technique using both air and saline. Reg Anesth 20:
462463, 1995
5. Blanco D, Llamazares J, Rincon R, et al: Thoracic epidural anesthesia via the lumbar
approach in infants and children. Anesthesiology 84:13121316, 1996
6. Bosenberg AT, Gouws E: Skinepidural distance in children. Anaesthesia 50:895897,
1995
7. Bosenberg AT, Kimble FW: Infraorbital nerve block in neonates for cleft lip repair:
Anatomical study and clinical application. Br J Anaesth 74:506508, 1995
8. Bouchut JC, Dubois R, Godard J: Clonidine in preterm-infant caudal anesthesia may
be responsible for postoperative apnea. Reg Anesth Pain Med 26:8385, 2001
9. Breschan C, Krumpholz R, Likar R, et al: Can a dose of 2 microg.kg(1) caudal
clonidine cause respiratory depression in neonates? Paediatr Anaesth 9:8183, 1999
10. Busoni P, Messeri A: Spinal anesthesia in children: Surface anatomy. Anesth Analg 68:
418419, 1989
11. Busoni P, Messeri A: Loss of resistance technique to air for identifying the epidural
space in infants and children. Use an appropriate technique! Paediatr Anaesth 5:
397, 1995
12. Casta A: Attempted placement of a thoracic epidural catheter via the caudal route in
a newborn. Anesthesiology 91:19651966, 1999
13. Constant I, Gall O, Gouyet L, et al: Addition of clonidine or fentanyl to local anaesthet-
ics prolongs the duration of surgical analgesia after single-shot caudal block in chil-
dren. Br J Anaesth 80:294298, 1998
110 SURESH & WHEELER
14. Cote CJ, Zaslavsky A, Downes JJ, et al: Postoperative apnea in former preterm infants
after inguinal herniorrhaphy. A combined analysis. Anesthesiology 82:809822, 1995
15. Cox RG, Goresky GV: Life-threatening apnea following spinal anesthesia in former
premature infants. Anesthesiology 73:345347, 1990
16. Cregg N, Conway F, Casey W: Analgesia after otoplasty: Regional nerve blockade vs
local anaesthetic inltration of the ear. Can J Anaesth 43:141147, 1996
17. Dahl JB, Kehlet H: The value of pre-emptive analgesia in the treatment of postoperative
pain. Br J Anaesth 70:434439, 1993
18. Denton JS, Manning MP: Femoral nerve block for femoral shaft fractures in children:
Brief report. J Bone Joint Surg Br 70:84, 1988
19. Easley RB, George R, Connors D, et al: Aseptic meningitis after spinal anesthesia in
an infant. Anesthesiology 91:305307, 1999
20. Fanelli G, Casati A, Beccaria P, et al: A double-blind comparison of ropivacaine,
bupivacaine, and mepivacaine during sciatic and femoral nerve blockade. Anesth
Analg 87:597600, 1998
21. Fisher QA, Shaffner DH, Yaster M: Detection of intravascular injection of regional
anaesthetics in children. Can J Anaesth 44:592598, 1997
22. Flandin-Blety C, Barrier G: Accidents following extradural analgesia in children. The
results of a retrospective study. Paediatr Anaesth 5:4146, 1995
23. Foster RH, Markham A: Levobupivacaine: A review of its pharmacology and use as a
local anaesthetic. Drugs 59:551579, 2000
24. Frumiento C, Abajian JC, Vane DW: Spinal anesthesia for preterm infants undergoing
inguinal hernia repair. Arch Surg 135:445451, 2000
25. Gallagher TM, Crean PM: Spinal anaesthesia in infants born prematurely. Anaesthesia
44:434436, 1989
26. Gerancher JC: Cauda equina syndrome following a single spinal administration of
5% hyperbaric lidocaine through a 25-gauge Whitacre needle. Anesthesiology 87:
687689, 1997
27. Giaufre E, Dalens B, Gombert A: Epidemiology and morbidity of regional anesthesia
in children: A 1-year prospective survey of the French-Language Society of Pediatric
Anesthesiologists. Anesth Analg 83:904912, 1996
28. Gill P, Kiani S, Victoria BA, et al: Pre-emptive analgesia with local anaesthetic for
herniorrhaphy. Anaesthesia 56:414417, 2001
29. Glantz L, Gozal Y, Gertel M: A loss-of-resistance technique using both air and saline.
Reg Anesth Pain Med 19:294, 1994
30. Goldman LJ: Complications in regional anaesthesia. Paediatr Anaesth 5:39, 1995
31. Guinard JP, Borboen M: Probable venous air embolism during caudal anesthesia in a
child. Anesth Analg 76:11341135, 1993
32. Gunter JB, Eng C: Thoracic epidural anesthesia via the caudal approach in children.
Anesthesiology 76:935938, 1992
33. Gunter JB, Watcha MF, Forestner JE, et al: Caudal epidural anesthesia in conscious
premature and high-risk infants. J Pediatr Surg 26:914, 1991
34. Hampl KF, Schneider MC, Pargger H, et al: A similar incidence of transient neurologic
symptoms after spinal anesthesia with 2% and 5% lidocaine. Anesth Analg 83:1051
1054, 1996
35. Harnik EV, Hoy GR, Potolicchio S, et al: Spinal anesthesia in premature infants
recovering from respiratory distress syndrome. Anesthesiology 64:9599, 1986
36. Hasan MA, Howard RF, Lloyd-Thomas AR: Depth of epidural space in children.
Anaesthesia 49:10851087, 1994
37. Henderson K, Sethna NF, Berde CB: Continuous caudal anesthesia for inguinal hernia
repair in former preterm infants. J Clin Anesth 5:129133, 1993
38. Hiller A, Karjalainen K, Balk M: Transient neurological symptoms after spinal anaes-
thesia with hyperbaric 5% lidocaine or general anaesthesia. Br J Anaesth 82:575579,
1999
39. Holthusen H, Eichwede F, Stevens M, et al: Pre-emptive analgesia: Comparison of
preoperative with postoperative caudal block on postoperative pain in children. Br J
Anaesth 73:440442, 1994
40. Ivani G, De Negri P, Conio A, et al: Ropivacaineclonidine combination for caudal
blockade in children. Acta Anaesthesiol Scand 44:446449, 2000
PRACTICAL PEDIATRIC REGIONAL ANESTHESIA 111
41. Ivani G, Mereto N, Lampugnani E, et al: Ropivacaine in paediatric surgery: Preliminary
results. Paediatr Anaesth 8:127129, 1998
42. Keld DB, Hein L, Dalgaard M, et al: The incidence of transient neurologic symptoms
(TNS) after spinal anaesthesia in patients undergoing surgery in the supine position.
Hyperbaric lidocaine 5% versus hyperbaric bupivacaine 0.5%. Acta Anaesthesiol Scand
44:285290, 2000
43. Khan ML, Hossain MM, Chowdhury AY, et al: Lateral femoral cutaneous nerve block
for split skin grafting. Bangladesh Med Res Counc Bull 24:3234, 1998
44. Kinirons B, Mimoz O, Lafendi L, et al: Chlorhexidine versus povidone iodine in
preventing colonization of continuous epidural catheters in children: A randomized,
controlled trial. Anesthesiology 94:239244, 2001
45. Kokki H, Hendolin H: Hyperbaric bupivacaine for spinal anaesthesia in 718 year old
children: Comparison of bupivacaine 5 mg mL
1
in 0.9% and 8% glucose solutions. Br
J Anaesth 84:5962, 2000
46. Kokki H, Tuovinen K, Hendolin H: Spinal anaesthesia for paediatric day-case surgery:
A double-blind, randomized, parallel-group, prospective comparison of isobaric and
hyperbaric bupivacaine. Br J Anaesth 81:502506, 1998
47. Kost-Byerly S, Tobin JR, Greenberg RS, et al: Bacterial colonization and infection rate
of continuous epidural catheters in children. Anesth Analg 86:712716, 1998
48. Kozek-Langenecker SA, Marhofer P, Jonas K, et al: Cardiovascular criteria for epidural
test dosing in sevouvane and halathane anesthetized in children. Anesth Analg 90:
579583, 2000
49. Krane EJ, Dalens BJ, Murat I, et al: The safety of epidurals placed during general
anesthesia. Reg Anesth Pain Med 23:433438, 1998
50. Krane EJ, Haberkern CM, Jacobson LE: Postoperative apnea, bradycardia, and oxygen
desaturation in formerly premature infants: Prospective comparison of spinal and
general anesthesia. Anesth Analg 80:713, 1995
51. Larsson BA, Lonnqvist PA, Olsson GL: Plasma concentrations of bupivacaine in neo-
nates after continuous epidural infusion. Anesth Analg 84:501505, 1997
52. Lau JT: Penile block for pain relief after circumcision in children. A randomized,
prospective trial. Am J Surg 147:797799, 1984
53. Lee JJ, Rubin AP: Comparison of a bupivacaineclonidine mixture with plain bupiva-
caine for caudal analgesia in children. Br J Anaesth 72:258262, 1994
54. Lonnqvist PA, Westrin P, Larsson BA, et al: Ropivacaine pharmacokinetics after caudal
block in 18 year old children. Br J Anaesth 85:506511, 2000
55. Loo CC, Irestedt L: Cauda equina syndrome after spinal anaesthesia with hyperbaric
5% lignocaine: A review of six cases of cauda equina syndrome reported to the
Swedish Pharmaceutical Insurance, 19931997. Acta Anaesthesiol Scand 43:371379,
1999
56. Maccani RM, Wedel DJ, Melton A, et al: Femoral and lateral femoral cutaneous nerve
block for muscle biopsies in children. Paediatr Anaesth 5:223227, 1995
57. Markey JR, Montiague R, Winnie AP: A comparative efcacy study of hyperbaric 5%
lidocaine and 1.5% lidocaine for spinal anesthesia. Anesth Analg 85:11051107, 1997
58. McKinney P, Gottlieb J: The relationship of the great auricular nerve to the supercial
musculoaponeurotic system. Ann Plast Surg 14:310314, 1985
59. McLeod DH, Wong DH, Vaghadia H, et al: Lateral popliteal sciatic nerve block
compared with ankle block for analgesia following foot surgery. Can J Anaesth 42:
765769, 1995
60. McLeod GA, Burke D: Levobupivacaine. Anaesthesia 56:331341, 2001
61. McNeely JK, Farber NE, Rusy LM, et al: Epidural analgesia improves outcome follow-
ing pediatric fundoplication. A retrospective analysis. Reg Anesth Pain Med 22:1623,
1997
62. McNeely JK, Trentadue NC, Rusy LM, et al: Culture of bacteria from lumbar and
caudal epidural catheters used for postoperative analgesia in children. Reg Anesth
Pain Med 22:428431, 1997
63. Miguel R, Morse S, Murtagh R: Epidural air associated with multiradicular syndrome.
Anesth Analg 73:9294, 1991
64. Moore DC, Bridenbaugh PO: Pneumothorax: Its incidence following intercostal nerve
block. JAMA 174:842, 1960
112 SURESH & WHEELER
65. Murat I, Delleur MM, Esteve C, et al: Continuous extradural anaesthesia in children.
Clinical and haemodynamic implications. Br J Anaesth 59:14411450, 1987
66. Murrell D, Gibson PR, Cohen RC: Continuous epidural analgesia in newborn infants
undergoing major surgery. J Pediatr Surg 28:548552, 1993
67. Nay PG, Milaszkiewicz R, Jothilingam S: Extradural air as a cause of paraplegia
following lumbar analgesia. Anaesthesia 48:402404, 1993
68. Needoff M, Radford P, Costigan P: Local anesthesia for postoperative pain relief after
foot surgery: A prospective clinical trial. Foot Ankle Int 16:1113, 1995
69. Neill RS: Postoperative analgesia following brachial plexus block. Br J Anaesth 50:
379382, 1978
70. Oberlander TF, Berde CB, Lam KH, et al: Infants tolerate spinal anesthesia with
minimal overall autonomic changes: Analysis of heart rate variability in former prema-
ture infants undergoing hernia repair. Anesth Analg 80:2027, 1995
71. Peng PW, Chan VW, Perlas A: Minimum effective anaesthetic concentration of hyper-
baric lidocaine for spinal anaesthesia. Can J Anaesth 45:122129, 1998
72. Peutrell JM, Hughes DG: A grand mal convulsion in a child in association with a
continuous epidural infusion of bupivacaine. Anaesthesia 50:563564, 1995
73. Polaner D, Suresh S, Cote CJ: Pediatric regional anesthesia. In Cote C, Todres ID, Ryan
JF, et al (eds): Pediatric Regional Anesthesia: A Practice Of Anesthesia for Infants and
Children. Philadelphia, WB Saunders, 2000, pp 636675
74. Prabhu KP, Wig J, Grewal S: Bilateral infraorbital nerve block is superior to peri-
incisional inltration for analgesia after repair of cleft lip. Scand J Plast Reconstr Surg
Hand Surg 33:8387, 1999
75. Saberski LR, Kondamuri S, Osinubi OY: Identication of the epidural space: Is loss of
resistance to air a safe technique? A review of the complications related to the use of
air. Reg Anesth Pain Med 22:315, 1997
76. Salmela L, Aromaa U: Transient radicular irritation after spinal anesthesia induced
with hyperbaric solutions of cerebrospinal uid-diluted lidocaine 50 mg/mL or mepi-
vacaine 40 mg/mL or bupivacaine 5 mg/mL. Acta Anaesthesiol Scand 42:765769, 1998
77. Sartorelli KH, Abajian JC, Kreutz JM, et al: Improved outcome utilizing spinal anesthe-
sia in high-risk infants. J Pediatr Surg 27:10221025, 1992
78. Schulte-Steinberg O: Regional anaesthesia for children. Ann Chir Gynaecol 73:158
165, 1984
79. Schwartz N, Eisenkraft JB: Probable venous air embolism during epidural placement
in an infant. Anesth Analg 76:11361138, 1993
80. Scott DB: Identication of the epidural space: Loss of resistance to air or saline? Reg
Anesth Pain Med 22:12, 1997
81. Sethna NF, Berde CB: Venous air embolism during identication of the epidural space
in children. Anesth Analg 76:925927, 1993
82. Shiga M, Nishina K, Mikawa K, et al: Oral clonidine premedication does not change
efcacy of simulated epidural test dose in sevourane-anesthetized children. Anesthe-
siology 93:954958, 2000
83. Strafford MA, Wilder RT, Berde CB: The risk of infection from epidural analgesia in
children: A review of 1620 cases. Anesth Analg 80:234238, 1995
84. Suresh S, Barcelona S, Young N, et al: Postoperative pain management in children
undergoing tympanomastoid surgery: Is a local block better than intravenous opioids?
Anesthesiology 91:A1281, 1999
85. Suresh S, Wagner AM: Scalp excisions: Getting ahead of pain. Pediatr Dermatol 18:
7476, 2001
86. Taddio A, Katz J, Ilersich AL, et al: Effect of neonatal circumcision on pain response
during subsequent routine vaccination. Lancet 349:599603, 1997
87. Tanaka M, Nishikawa T: Simulation of an epidural test dose with intravenous epineph-
rine in sevourane-anesthetized children. Anesth Analg 86:952957, 1998
88. Tanaka M, Nishikawa T: The efcacy of a simulated intravascular test dose in sev-
ourane-anesthetized children: A dose-response study. Anesth Analg 89:632637, 1999
89. Tanaka M, Kimura T, Goyagi T, et al: Evaluating hemodynamic and T wave criteria of
simulated intravascular test doses using bupivacaine or isoproterenol in anesthetized
children. Anesth Analg 91:567572, 2000
PRACTICAL PEDIATRIC REGIONAL ANESTHESIA 113
90. Tobias JD: Continuous femoral nerve block to provide analgesia following femur
fracture in a paediatric ICU population. Anaesth Intensive Care 22:616618, 1994
91. Tobias JD: Brachial plexus anaesthesia in children. Paediatr Anaesth 11:265275, 2001
92. Tsui BC, Seal R, Entwistle L: Thoracic epidural analgesia via the caudal approach
using nerve stimulation in an infant with CATCH22. Can J Anaesth 46:11381142, 1999
93. Wagner AM, Suresh S: Peripheral nerve blocks for warts: Taking the cry out of
cryotherapy and laser. Pediatr Dermatol 15:238241, 1998
94. Welborn LG, Rice LJ, Hannallah RS, et al: Postoperative apnea in former preterm
infants: Prospective comparison of spinal and general anesthesia. Anesthesiology 72:
838842, 1990
95. Wong K, Strichartz GR, Raymond SA: On the mechanisms of potentiation of local
anesthetics by bicarbonate buffer: Drug structure-activity studies on isolated peripheral
nerve. Anesth Analg 76:131143, 1993
96. Wright TE, Orr RJ, Haberkern CM, et al: Complications during spinal anesthesia in
infants: High spinal blockade. Anesthesiology 73:12901292, 1990
97. Yamashita M: Mathematical formula for assessing the depth of the epidural space in
children. Anaesthesia 52:9495, 1997
98. Cote CJ, Todres ID, Goudsouzian NG, et al (eds): A Practice of Anesthesia for Infants
and Children, 3rd ed. Philadelphia, WB Saunders, 2001, p 655
Address reprint requests to
Santhanam Suresh, MD
Department of Anesthesiology, Box #19
Childrens Memorial Hospital
Northwestern University Medical School
Chicago, IL 60614
e-mail: ssuresh@northwestern.edu.
Potrebbero piacerti anche
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (894)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Maximizing Growth Factors for Height IncreaseDocumento29 pagineMaximizing Growth Factors for Height IncreaseMegaV100% (2)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- 4 Daftar PustakaDocumento1 pagina4 Daftar PustakasriwulanrpNessuna valutazione finora
- Daftar Pustaka: Therapeutic Use of Antifungal Agents in Dentistry. Aust DentDocumento2 pagineDaftar Pustaka: Therapeutic Use of Antifungal Agents in Dentistry. Aust DentIsta Fatimah Kurnia RahmiNessuna valutazione finora
- Daftar Pustaka Maffucci SyndromeDocumento2 pagineDaftar Pustaka Maffucci SyndromeIsta Fatimah Kurnia RahmiNessuna valutazione finora
- Journalarticle 0185Documento2 pagineJournalarticle 0185Mahmood AdelNessuna valutazione finora
- Blok 6Documento12 pagineBlok 6Ista Fatimah Kurnia RahmiNessuna valutazione finora
- Kumpulan Soal MCQ Blok 4Documento8 pagineKumpulan Soal MCQ Blok 4Susi SusantiNessuna valutazione finora
- How To ReferencesDocumento23 pagineHow To ReferencesNicharee RangseekajeeNessuna valutazione finora
- MCQ Blok 2Documento16 pagineMCQ Blok 2Ista Fatimah Kurnia RahmiNessuna valutazione finora
- Ovarian Cancer Stage III/IV: Poor Prognostic FactorsDocumento4 pagineOvarian Cancer Stage III/IV: Poor Prognostic Factorsindra_strongNessuna valutazione finora
- Seizure-Related Factors and Non-Verbal Intelligence in Children With Epilepsy A Population-Based Study From Western NorwayDocumento9 pagineSeizure-Related Factors and Non-Verbal Intelligence in Children With Epilepsy A Population-Based Study From Western NorwayIsta Fatimah Kurnia RahmiNessuna valutazione finora
- Journalarticle 0185Documento2 pagineJournalarticle 0185Mahmood AdelNessuna valutazione finora
- Metastatic Spread of Mucinous Cystadenocarcinoma of The Ovaries Into Abdominal WallDocumento3 pagineMetastatic Spread of Mucinous Cystadenocarcinoma of The Ovaries Into Abdominal WallIsta Fatimah Kurnia RahmiNessuna valutazione finora
- Kerangka KonsepDocumento1 paginaKerangka KonsepIsta Fatimah Kurnia RahmiNessuna valutazione finora
- BTLDocumento60 pagineBTLCamiNessuna valutazione finora
- 1.4 The Lymphatic System: Prepared By: Ling Mei TengDocumento15 pagine1.4 The Lymphatic System: Prepared By: Ling Mei TengJuliet LingNessuna valutazione finora
- Paragraph Development ExerciseDocumento6 pagineParagraph Development ExerciseSYAFINAS SALAM100% (1)
- ICSE Class 10 Biology Previous Year Question Paper 2011 PDFDocumento9 pagineICSE Class 10 Biology Previous Year Question Paper 2011 PDFmohammedNessuna valutazione finora
- Excretory System QuizDocumento17 pagineExcretory System QuizShadab HanafiNessuna valutazione finora
- Led Light Therapy GuideDocumento23 pagineLed Light Therapy GuidePeter Freimann100% (4)
- Auxin Controls Seed Dormacy in Arabidopsis (Liu, Et Al.)Documento6 pagineAuxin Controls Seed Dormacy in Arabidopsis (Liu, Et Al.)Jet Lee OlimberioNessuna valutazione finora
- Pass MRCP Part 2 (Sample)Documento26 paginePass MRCP Part 2 (Sample)Ahmad Shokry100% (1)
- He History of ArticulatorsDocumento13 pagineHe History of ArticulatorsrekabiNessuna valutazione finora
- Chapter 6 Cell DivisionDocumento20 pagineChapter 6 Cell DivisionVinash Shka RaoNessuna valutazione finora
- Animal Morphology (GeoZoo Topics)Documento5 pagineAnimal Morphology (GeoZoo Topics)niravhirparaNessuna valutazione finora
- Comprehensive Review of Temporal Lobe EpilepsyDocumento36 pagineComprehensive Review of Temporal Lobe Epilepsyyohanes0gadiNessuna valutazione finora
- Pharmacology Nursing ReviewDocumento19 paginePharmacology Nursing Reviewp_dawg50% (2)
- Chapter 3: Movement of Substance Across The Plasma MembraneDocumento13 pagineChapter 3: Movement of Substance Across The Plasma MembraneEma FatimahNessuna valutazione finora
- Anatomy and Physiology-REVIEWER-Practical ExamDocumento12 pagineAnatomy and Physiology-REVIEWER-Practical ExamDeity Ann ReuterezNessuna valutazione finora
- Anatomy and Diseases of The UveaDocumento102 pagineAnatomy and Diseases of The UveaVishakh IsloorNessuna valutazione finora
- Neurotransmission, Measuring Chemical Events In: Advanced ArticleDocumento12 pagineNeurotransmission, Measuring Chemical Events In: Advanced ArticleazzaassNessuna valutazione finora
- The Science of Laughing - Worksheet 3Documento3 pagineThe Science of Laughing - Worksheet 3Maria Alexandra PoloNessuna valutazione finora
- Checklist FON 1Documento27 pagineChecklist FON 1Hadan KhanNessuna valutazione finora
- Sri Padmavathi Medical College Hospital: APPLICATIONS Are INVITED For The Following Post - 2013-14Documento3 pagineSri Padmavathi Medical College Hospital: APPLICATIONS Are INVITED For The Following Post - 2013-14Birupakshya RoutNessuna valutazione finora
- Seed Germination, Dormancy & Breaking of DormancyDocumento35 pagineSeed Germination, Dormancy & Breaking of DormancySaravananNessuna valutazione finora
- 10th BIOLOGY PPT CH. NO. 8Documento13 pagine10th BIOLOGY PPT CH. NO. 8Aastha BorhadeNessuna valutazione finora
- Arthropod-Plant Interactions Novel Insights and Approaches For IPMDocumento238 pagineArthropod-Plant Interactions Novel Insights and Approaches For IPMAnonymous T9uyM2Nessuna valutazione finora
- Pe Lecture NotesDocumento7 paginePe Lecture NotesAnonymous LJrX4dzNessuna valutazione finora
- Biochem QbankDocumento16 pagineBiochem Qbank786waqar786Nessuna valutazione finora
- CP On AmoebiasisDocumento77 pagineCP On Amoebiasiskathy100% (1)
- Template POMRDocumento8 pagineTemplate POMRPPDS IPD ULMNessuna valutazione finora
- 8 Science NCERT Solutions Chapter 10Documento7 pagine8 Science NCERT Solutions Chapter 10Raj Anand100% (1)