Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Section 3: Cancer Drugs and Stem Cells
Caricato da
Edward HanDescrizione originale:
Titolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Section 3: Cancer Drugs and Stem Cells
Caricato da
Edward HanCopyright:
Formati disponibili
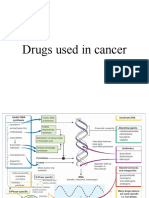
Section 3: Cancer drugs and Stem Cells
Since cancer is a heterogeneous disease, many drugs have been discovered and developed to
combat various aspects of cancer. Cancer therapies are discussed below along with how they can benefit
from utilizing stem cells.
3.1.1 Chemotherapy.
Chemotherapy is the most commonly used type of cancer drug. A few examples include
alkylating agents, anti-neoplastics, and anti-metabolites. They can be administered orally, intravenously,
and directly into tissues. Although chemotherapy is a systemic treatment and can combat metastasis, it
also affects all rapidly proliferating cells and will cause systemic toxicity resulting in side effects such as
fatigue, nausea, pain, depression, numbness, weakness, hair loss, and overall decrease in quality of life.
Side effects can be minimized through tumor targeting which will result in higher concentrations at
diseased sites and lower concentrations systemically. For example, antibody targeted chemotherapies
conjugating cytotoxic chemotherapeutics to tumor associated antigens have been shown to have tumor
specific cytotoxic effects[69]. Use of tumor specific antigens for targeting is imperfect, however, and is
not applicable to all sorts of cancers. Fortunately, stem cells are able to home to all sorts of tumors due to
the inherent characteristics of cancer. As such, engineering stem cells to secrete chemotherapeutics can
significantly increase efficacy and safety. However, some cancer cells are resistant to chemotherapeutics,
necessitating efforts which utilizing other pathways to treat cancer.
3.1.2 Anti-cancer stem cell drugs
Rather than target cancer in general, some drugs also specifically focus on targeting cancer stem
cells These cancer stem cells are oftentimes more resistant to chemotherapy and radiation therapies and
cancer relapse occurs if the traditional treatments fail to kill all cancer stem cells[70]. In relapsed patients,
cancer stem cells account for a greater proportion of the tumors which makes the cancer even more
difficult to treat in a breast cancer model, the population of breast cancer initiating cells has been shown
to increase from 9% to 74% in tumors after traditional treatments[71].
3.1.3 Pro-apoptotic proteins
Apoptosis is a pathway naturally found on cancer cells that can be triggered to induce cell death
and cancer regression. Most notably, tumor necrosis factor-related apoptosis induced ligand (TRAIL)
directly attaches to receptors on tumor cells and activates apoptosis proteases to kill the cancer cell [72].
This is highly effective against all cancers types but creating cancer specific pro-apoptosis proteins is
essential. Similar to other drugs, any non specific activation can be minimized through targeting using
stem cell vehicles. MSCs designed to deliver specially engineered secretable TRAIL have been showed to
cause apoptosis in in vivo glioma models. Importantly, it has been shown that MSCs are resistant to
apoptosis from TRAIL making them viable targeting candidates[73].
3.1.4 Prodrugs
Another way to increase cancer specificity in drugs is to utilize prodrugs. Prodrugs are normally
non toxic. However, they are designed to respond to tumor specific enzymes which activate the prodrug
into its toxic form[74]. Thus, prodrugs provide a more targeted approach towards cancer therapy since
greater concentrations of cytotoxic drug will be located at sites of cancer than in healthy tissues[75].
Another benefit of prodrug systems is the bystandard effect which kills all local cancer cells in a given
region through diffusion of the activated prodrug agent[76]. Stem cells can further increase local
concentration of drug at tumor sites and thus increase therapeutic efficiency. Prodrugs also exhibit higher
specificity than many conventional drugs which further reduces systemic toxicity even if stem cell
vehicles become lodged in organs such as the liver or lungs. The prodrug system can even be used in
cancers that do not have specific activating enxymes through suicide gene therapy (discussed in section
4.1.4).
3.1.5 Anti-angiogenesic agents
Aside from killing cancer cells, tumor growth can be hindered via antiangiogenic agents. As a
mass of proliferating cells, tumors require blood vessels to carry oxygen and nutrients to cells past the
oxygen diffusion limit which are at risk of hypoxia. Studies have shown that utilizing anti-angiogenic
VEGF receptor inhibitors transiently normalized tumor vessels in glioblastoma patients [77].
Intravenously delivered stem cells can be used as vehicles for these agents. In addition, since certain types
of stem cells, such as MSCs, can become embedded pericytes, using continuous release delivery
mechanisms can reduce the transience of anti-angiogenesis cancer therapy[78].
3.1.6 Growth factor limiting agents
Similar to angiogenic proteins, growth factors are also important to the development of cancer.
Many drugs such as NK4 which inhibits hepatocyte growth factor are used to combat cancer. Delivery of
NK4 using MSCs has been shown to significantly increase survival of mice in a lung metastasis
model[79].
Potrebbero piacerti anche
- ChemotherapyDocumento29 pagineChemotherapyatifzeaNessuna valutazione finora
- En Wikipedia OrgDocumento5 pagineEn Wikipedia OrgKueh Wee RockNessuna valutazione finora
- The Concept of Killing Tumours With The Assistance of Transdermal Patches and Nano Aptamer BioconjugatesDocumento17 pagineThe Concept of Killing Tumours With The Assistance of Transdermal Patches and Nano Aptamer BioconjugateskmdevrajNessuna valutazione finora
- Pharmacology ChemotherapyDocumento28 paginePharmacology ChemotherapyDartiguesNessuna valutazione finora
- Targeting TerapyDocumento10 pagineTargeting TerapyWisnuardhyHendrawardhanaNessuna valutazione finora
- Presentation 4Documento26 paginePresentation 4sai projectNessuna valutazione finora
- Assignment On Anticancer Antimetabolites Antifungal Course Title: Pharmacology II Course Code: BPH-3013Documento17 pagineAssignment On Anticancer Antimetabolites Antifungal Course Title: Pharmacology II Course Code: BPH-3013Nargish SultanaNessuna valutazione finora
- Oncotarget 08 38022 PDFDocumento22 pagineOncotarget 08 38022 PDFmpl12345678Nessuna valutazione finora
- Anticancer DrugsDocumento57 pagineAnticancer Drugsn4pnjfk6rbNessuna valutazione finora
- Antineoplastic Agents 2011 Dental MARCH-1Documento41 pagineAntineoplastic Agents 2011 Dental MARCH-1BinayakSwainNessuna valutazione finora
- CancerBooklest FinalDocumento15 pagineCancerBooklest Finalrafael alvarizNessuna valutazione finora
- Nikita Sharma Practice School ProjectDocumento10 pagineNikita Sharma Practice School ProjectNikita sharmaNessuna valutazione finora
- TS2 Cancer TherapiesDocumento1 paginaTS2 Cancer Therapiesndeye yarame diopNessuna valutazione finora
- Drug Delivery Proposal For Ovarian CancerDocumento13 pagineDrug Delivery Proposal For Ovarian Cancerapi-316362096Nessuna valutazione finora
- Chemo PamphletDocumento3 pagineChemo PamphletPowpOw SangalangNessuna valutazione finora
- How Cancer Cells Resist ChemotherapyDocumento15 pagineHow Cancer Cells Resist ChemotherapyKerim SabicNessuna valutazione finora
- (Acero) Week 4 PT - Research Report On Immunotherapy and Its AdvancementsDocumento3 pagine(Acero) Week 4 PT - Research Report On Immunotherapy and Its AdvancementsPaul AceroNessuna valutazione finora
- Biochemical and Biophysical Research Communications: ReviewDocumento5 pagineBiochemical and Biophysical Research Communications: ReviewYudhi AuliaNessuna valutazione finora
- Microenvironment Chronic Inflammation Oxygen Free Radicals: Nat GenetDocumento6 pagineMicroenvironment Chronic Inflammation Oxygen Free Radicals: Nat GenetGwyneth Cartalla100% (1)
- Celular Dormancy MechanismsDocumento17 pagineCelular Dormancy MechanismsJoão FrancoNessuna valutazione finora
- Anti CancerDocumento11 pagineAnti Cancerali ahmedNessuna valutazione finora
- Cancer Chemotherapy ModuleDocumento3 pagineCancer Chemotherapy ModuleSheril MarekNessuna valutazione finora
- Targetet Therapy InteresantDocumento10 pagineTargetet Therapy InteresantpopeataNessuna valutazione finora
- Anjali SudhaDocumento8 pagineAnjali Sudhagaurav saxenaNessuna valutazione finora
- 1st StudyDocumento14 pagine1st StudyWeeaboo Franz VlogsNessuna valutazione finora
- Cancer: Treatments and PreventionDocumento5 pagineCancer: Treatments and PreventionMukesh PandeyNessuna valutazione finora
- Chemotheraphy JournalsDocumento5 pagineChemotheraphy JournalsSutria N. SyatiNessuna valutazione finora
- Current Status and Future Directions of Cancer ImmunotherapyDocumento7 pagineCurrent Status and Future Directions of Cancer ImmunotherapyDesire EstevesNessuna valutazione finora
- Molecules: A Review On Cancer Immunotherapy and Applications of Nanotechnology To Chemoimmunotherapy of Different CancersDocumento24 pagineMolecules: A Review On Cancer Immunotherapy and Applications of Nanotechnology To Chemoimmunotherapy of Different CancersJuan Vera SanchezNessuna valutazione finora
- 9.lecturer 18 Biochemistry Effect On Tumor and Tumor MarkersDocumento19 pagine9.lecturer 18 Biochemistry Effect On Tumor and Tumor MarkersAbdulRahman MuthannaNessuna valutazione finora
- Drugs Used in CancerDocumento46 pagineDrugs Used in CancerRENTI NOVITANessuna valutazione finora
- Research Journal of Pharmaceutical, Biological and Chemical SciencesDocumento9 pagineResearch Journal of Pharmaceutical, Biological and Chemical SciencesObaid Ullah KhanNessuna valutazione finora
- New Approaches To Treat Cancer - What They Can and Cannot DoDocumento10 pagineNew Approaches To Treat Cancer - What They Can and Cannot DoMuhammad ImranNessuna valutazione finora
- Method Development and Pharmacological Study of Chemotherapeutic Agents OAJT - ms.ID.555568 DrkrishnasarmapathyDocumento1 paginaMethod Development and Pharmacological Study of Chemotherapeutic Agents OAJT - ms.ID.555568 DrkrishnasarmapathyDrkrishnasarma pathyNessuna valutazione finora
- NCM106Documento23 pagineNCM106Angel JagongNessuna valutazione finora
- Molecules 23 02334Documento17 pagineMolecules 23 02334Lady GonzabayNessuna valutazione finora
- Molecular Basis of Cancer TherapyDocumento8 pagineMolecular Basis of Cancer TherapySenthereng MoaisiNessuna valutazione finora
- Advantages of ChemotherapyDocumento13 pagineAdvantages of ChemotherapyMohammad SafiqulNessuna valutazione finora
- Antineoplastics (FINAL)Documento118 pagineAntineoplastics (FINAL)judd wilsonNessuna valutazione finora
- Cancer Textbook 4 (Cancer Treatment and Ovarian Cancer)Da EverandCancer Textbook 4 (Cancer Treatment and Ovarian Cancer)Nessuna valutazione finora
- Ijms 23 15455Documento19 pagineIjms 23 15455Ignacio SanchoNessuna valutazione finora
- Anticancer For MedicineDocumento81 pagineAnticancer For MedicineYusra SanyNessuna valutazione finora
- RahultDocumento1 paginaRahultAjay SharmaNessuna valutazione finora
- Targeted Therapy in CancerDocumento51 pagineTargeted Therapy in CancerSatya WangsaNessuna valutazione finora
- Antineoplastic Agents by Rajarshi Patel - PPSXDocumento41 pagineAntineoplastic Agents by Rajarshi Patel - PPSXRajarshi PatelNessuna valutazione finora
- Gene Therapy For Cancer Treatment Past Present FutureDocumento10 pagineGene Therapy For Cancer Treatment Past Present FuturefrancoismullierNessuna valutazione finora
- Exosome-Based Immunotherapy: A Promising Approach For Cancer TreatmentDocumento16 pagineExosome-Based Immunotherapy: A Promising Approach For Cancer Treatment1810 15Marvin LionelNessuna valutazione finora
- A Summary Report On Cancer ImmunotherapyDocumento3 pagineA Summary Report On Cancer ImmunotherapyAubrey Rose Flores100% (1)
- Table Differniation Between Tumor and BenignDocumento7 pagineTable Differniation Between Tumor and BenignAhmed AlrkabeNessuna valutazione finora
- TTT of CancerDocumento10 pagineTTT of Cancerali ahmedNessuna valutazione finora
- Anticancer Drugs: Consumer ChemistryDocumento24 pagineAnticancer Drugs: Consumer ChemistryAshlie AbalaNessuna valutazione finora
- Seminário 4.2-An Overview of Cancer Treatment ModalitiesDocumento20 pagineSeminário 4.2-An Overview of Cancer Treatment ModalitiesAngellique NiyiragiraNessuna valutazione finora
- 9.3.2 Targeted Cancer TherapiesDocumento8 pagine9.3.2 Targeted Cancer TherapiesFivi KurniawatiNessuna valutazione finora
- Definition of Cancer and ChemotherapyDocumento1 paginaDefinition of Cancer and ChemotherapymegamarwaNessuna valutazione finora
- Drug ResistanceDocumento39 pagineDrug ResistanceJalal EltabibNessuna valutazione finora
- Understanding Chemotherapy: Mechanisms, Agents, and Nursing CareDocumento89 pagineUnderstanding Chemotherapy: Mechanisms, Agents, and Nursing CareNurse NotesNessuna valutazione finora
- What Is Targeted Therapy?Documento27 pagineWhat Is Targeted Therapy?Raxter ErNessuna valutazione finora
- Immuno TherapyDocumento20 pagineImmuno TherapyAttis PhrygiaNessuna valutazione finora
- Cancer Drug ResistanceDocumento9 pagineCancer Drug Resistancemrezvani1992Nessuna valutazione finora
- Activity 13 ImmunochemistryDocumento28 pagineActivity 13 ImmunochemistryKendrix Aguiluz FlorendoNessuna valutazione finora
- Flu A-B PCRDocumento53 pagineFlu A-B PCRyousrazeidan1979Nessuna valutazione finora
- How Does Forensic Identification Work?: Some Examples of DNA Uses For Forensic IdentificationDocumento22 pagineHow Does Forensic Identification Work?: Some Examples of DNA Uses For Forensic IdentificationKonigAndy007Nessuna valutazione finora
- BSC 6 Sem Applied Zoology 2 Zoology Summer 2018Documento1 paginaBSC 6 Sem Applied Zoology 2 Zoology Summer 2018Ujjwala KumbhalkarNessuna valutazione finora
- Genetically Modified Foods A Critical Review of Their Promise and ProblemsDocumento8 pagineGenetically Modified Foods A Critical Review of Their Promise and ProblemsIoana MoldovanNessuna valutazione finora
- Research ProjectsDocumento2 pagineResearch Projectsapi-143464694Nessuna valutazione finora
- CH 5 - Virology 1Documento60 pagineCH 5 - Virology 1Tariku TadesaNessuna valutazione finora
- Lifespan: Why We Age - and Why We Don't Have To - David A. SinclairDocumento5 pagineLifespan: Why We Age - and Why We Don't Have To - David A. Sinclairzoxowalu0% (3)
- Frequently Asked Questions On Immunization (English) : 1. What Is A Vaccine?Documento6 pagineFrequently Asked Questions On Immunization (English) : 1. What Is A Vaccine?L Jossenel Mejido-AñanoNessuna valutazione finora
- Biology AnalysisDocumento6 pagineBiology AnalysisPrivateNessuna valutazione finora
- Vce Unit 3Documento6 pagineVce Unit 3api-323688225Nessuna valutazione finora
- PlasmidsDocumento14 paginePlasmidsMagesh RamasamyNessuna valutazione finora
- Ch-1. of Class 12 BioDocumento6 pagineCh-1. of Class 12 BioAnshulKumarNessuna valutazione finora
- Agri CuliDocumento11 pagineAgri CuliAdriel MendozaNessuna valutazione finora
- Pharma Data Calling DetailDocumento1 paginaPharma Data Calling Detailprajay3536Nessuna valutazione finora
- GPB 121 Most Probable Que PaperDocumento2 pagineGPB 121 Most Probable Que Paperpratikwagh112002Nessuna valutazione finora
- NanoCellect Biomedical Begins Distribution To EuropeDocumento2 pagineNanoCellect Biomedical Begins Distribution To EuropePR.comNessuna valutazione finora
- Progress in Drug Discovery & Biomedical ScienceDocumento21 pagineProgress in Drug Discovery & Biomedical SciencenishiNessuna valutazione finora
- Unit 1 Cell Biology Practice 1: (72 Marks)Documento17 pagineUnit 1 Cell Biology Practice 1: (72 Marks)Rita LimNessuna valutazione finora
- Genetics) SyllabusDocumento33 pagineGenetics) Syllabusb.duttaNessuna valutazione finora
- Epigenetics in NursingDocumento10 pagineEpigenetics in NursingJoe RobinsonNessuna valutazione finora
- Lab Report 10Documento6 pagineLab Report 10api-301352285Nessuna valutazione finora
- Scale-Up of Protein Purification Downstream Processing Issues PDFDocumento13 pagineScale-Up of Protein Purification Downstream Processing Issues PDFCapNessuna valutazione finora
- Southern Blotting TechniqueDocumento5 pagineSouthern Blotting TechniqueVĩnh Nguyễn VănNessuna valutazione finora
- Genexpert Mtb-Rif: Naadira Vanker - Regional Workshop On Laboratory Methods For The Diagnosis of Tuberculosis - KcriDocumento23 pagineGenexpert Mtb-Rif: Naadira Vanker - Regional Workshop On Laboratory Methods For The Diagnosis of Tuberculosis - KcriIsah Mohammed100% (1)
- Functional Matrix Theory Revisited: Presented By: DR H M Manisha PG1 YearDocumento48 pagineFunctional Matrix Theory Revisited: Presented By: DR H M Manisha PG1 YearH. M Manisha100% (1)
- Cell Biology Test - 70 Possible Points: Prokaryotic and Eukaryotic Cells (2 Points Per Question)Documento3 pagineCell Biology Test - 70 Possible Points: Prokaryotic and Eukaryotic Cells (2 Points Per Question)Vienne MonroidNessuna valutazione finora
- Bio May Exam 2014 - Paper 2Documento8 pagineBio May Exam 2014 - Paper 2Eva MayseNessuna valutazione finora
- Drosophila Dihybrid Cross Lab Genetics f13Documento6 pagineDrosophila Dihybrid Cross Lab Genetics f13api-2497729890% (1)
- Pharmacokinetics, Pharmacodynamics and Pharmacogenetics of Tacrolimus in Kidney TransplantationDocumento10 paginePharmacokinetics, Pharmacodynamics and Pharmacogenetics of Tacrolimus in Kidney TransplantationSarah Gita SinagaNessuna valutazione finora