Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Role of Physiotherapy in ICU
Caricato da
prasanna3k100%(2)Il 100% ha trovato utile questo documento (2 voti)
953 visualizzazioni68 pagineICU
Copyright
© © All Rights Reserved
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documento100%(2)Il 100% ha trovato utile questo documento (2 voti)
953 visualizzazioni68 pagineRole of Physiotherapy in ICU
Caricato da
prasanna3kSei sulla pagina 1di 68
Role of physiotherapy in ICU
Physiotherapy assessment in ICU
MEDICAL CHART READING:
Name, Age, Sex
H\O Present Illness
Past Medical History
Past Surgical History
Drug History
Social/Occupational History
Investigation
BED CHART READING /BEDSIDE MONITORING
Temperature
PR
BP
SpO
2
Hb
Platelets count/INR
CPP
ICP
CVP
PAP/PCWP
Neurological Assessment
Level of consciousness
GCS
Pupil
Size
Reactivity
Equality
CPP(Cerebral Perfusion pressure)
Normal value >70mmHg
Critical value<50 mm Hg
ICP(Intra cranial pressure)
Normal <10mm Hg
Critical >25mm Hg
Physiotherapy with PROM can be used safely
in patients with acute neurological diseases,
even if ICP is elevated before therapy.[1]
1.Roth, C., et al., Effect of early physiotherapy on intracranial pressure and cerebral
perfusion pressure. Neurocrit Care, 2013. 18(1): p. 33-8.
Evidence is compelling that a randomized-
controlled trial is indicated to test the
hypothesis that chest physiotherapy may
actually result in short-term resolution of high
intracranial pressure, and thus provide one
more clinical tool in the management of
elevated intracranial pressure.[2]
2Olson, D.M., et al., Changes in intracranial pressure associated with chest
physiotherapy. Neurocrit Care, 2007. 6(2): p. 100-3
The supine position and Valsalva maneuvers,
however, should be avoided, and ICP should
be monitored closely in patients with severe
intracranial hypertension.[3]
3.Serge Brimioulle, J.-J.M., Danielle,Norrenberg and Robert J Kahn, Effects of Positioning and Exercise on
Intracranial Pressure in a Neurosurgical Intensive Care Unit. Journals of American physical therapy association,
1997. 77: p. 1682-1689.
In situation of high ICP or unstable ICP use
inotropic to maintain MAP
HR(Heart rate and rhythm)
Normal value 50-100bpm
Bradycardia <50
Tachycardia >100
Assess heart rate and basic rhythm by looking
at ECG reading or taking a pulse manually
Sinus bradycardia (< 60 bpm) care should be
taken. Patient should be pre-oxygenated prior
to suction.
Suctioning can cause vagal stimulation and
decrease HR further. Pre-oxygenation helps to
lessen effects of SB and vagal stimulation
Sinus tachycardia (>100bpm) care should be
taken with manual techniques and exercise.
Increased HR may be due to pain/anxiety or
sepsis in response to decreased BP.
Full explanation of treatment and adequate
analgesia should be given
Slow AF is essentially stable fast AF (> 120 bpm)
may contraindicate treatment.
If patient is in SVT or VT treatment is
contraindicated
If the patient is being externally paced, care must
be taken to observe the insertion point of the
wires
Blood Pressure
Assess BP using arterial line (use the recent trend
in BP recordings) or NIBP reading. If BP < 90/60 or
patient is hypotensive in relation to normal BP,
care is required with treatment.
Patient may be hypovolaemic, septic sedated or
have insufficient cardiac function
Treatment techniques could cause BP to decrease
further
Manual hyperinflation can restrict venous
return - reducing cardiac output and can
decrease BP further
Care with suction should be taken hypotensive
patients should be preoxygenated prior to
suction.
Suction can simulate a vaso-vagal response
further reducing BP
If BP is >145/90 or patient is hypertensive in
relation to normal care with treatment is
required.
Patients may be in pain, have anxiety or have
cardiac dysfunction. They may not be
adequately sedated.
If BP suddenly increases or decreases
significantly during treatment stop and
inform nursing staff if they do not settle within
a few minutes and/or intervention is needed
e.g. increase in inotropes
To Treat or not to Treat on Critical Care, Guidelines for Practice 2012---Nottingham University Hospitals
CVP
Circulating blood flows into the right atrium
via the inferior and superior vena cava. The
pressure in the right atrium is known as
central venous pressure (CVP).
Normal value is 3-15cmH
2
0
http://docsm14.webs.com/CVP.pdf
PAP & PCWP
It gives indirect measurement of left atrial
pressure
PAP-10-22mm Hg
PCWP-Normally 8-10 mmHg
High PAP, high pulmonary vascular resistance
and may exacerbated during MHI
INR-international normalized ratio
The prothrombin time (PT) and its derived
measures of prothrombin ratio (PR) and
international normalized ratio (INR) are
measures of the extrinsic pathway of
coagulation
This test is also called "ProTime INR" and
"PT/INR
http://en.wikipedia.org/wiki/Prothrombin_time
Normal range INR in absence of
anticoagulation therapy is 0.8-1.2
If INR is > 1.5 caution with treatment is
required
Check with patients consultant prior to
insertion of NPA,OA
Respiratory support/Mode of
ventialtion
Oxygen therapy
Oxygen is given to treat hypoxaemia. Patients
should initially be given a high concentration.
The amount can then be adjusted according to
the results of pulse oximetry and arterial
blood gas analysis.
Oxygen range vary from21%(FiO
2
0.21)to
100%(FiO
2
1.0)*
HELLY, M. P. & NIGHTINGALE, P. 1999. ABC of intensive care Respiratory support. British Medical Journals, 319, 16741677.
PRYOR, J. A. & PRASAD, A. S. 2008. Physiotherapy for Respiratory and Cardiac Problems: Adults and Paediatrics, Elsevier
Sp0
2
normal 94%-100%
http://www.amperordirect.com/pc/help-pulse-oximeter/z-interpreting-
results.html
Oxygen is usually given
1. Fixed performance device-Venturi Mask
2. Variable performance device-face mask,
nasal prongs or cannulas
http://www.ccmtutorials.com/rs/oxygen/page13.htm
Fi0
2
: Fraction of Inspired Oxygen
Nasal canula
O2 Flow rate (l/min) FiO2
1 24%
2 28%
3 32%
4 36%
5 40%
6 44%
Over 4 l/min cause mucosal drying and nasal bleeding
Oxygen face mask
simple oxygen mask has open side ports that
allow room air to enter the mask and dilute
the oxygen, as well as allowing exhaled carbon
dioxide to leave the containment space
Mary Elizabeth Martelli R.N., B.S.The Gale Group Inc., Gale. Gale Encyclopedia of
Nursing and Allied Health, 2002
Oxygen face mask -cntd
partial rebreather oxygen mask
similar to a simple face mask, however, the
side ports are covered with one-way discs to
prevent room air from entering the mask.
Mary Elizabeth Martelli R.N., B.S.The Gale Group Inc., Gale. Gale Encyclopedia of
Nursing and Allied Health, 2002
Oxygen face mask -cntd
This mask is called a rebreather because it has
a soft plastic reservoir bag connected to the
mask that conserves the first third of the
patient's exhaled air while the rest escapes
through the side ports.
Mary Elizabeth Martelli R.N., B.S.The Gale Group Inc., Gale. Gale Encyclopedia of
Nursing and Allied Health, 2002
Oxygen face mask -cntd
Non-rebreather oxygen mask
similar to a simple face mask but has multiple
one-way valves in the side ports. These valves
prevent room air from entering the mask but
allow exhaled air to leave the mask.
Mary Elizabeth Martelli R.N., B.S.The Gale Group Inc., Gale. Gale Encyclopedia of
Nursing and Allied Health, 2002
Oxygen face mask -cntd
It has a reservoir bag like a partial rebreather
mask but the reservoir bag has a one-way
valve that prevents exhaled air from entering
the reservoir.
Mary Elizabeth Martelli R.N., B.S.The Gale Group Inc., Gale. Gale Encyclopedia of
Nursing and Allied Health, 2002
Oxygen face mask -cntd
This allows larger concentrations of oxygen to
collect in the reservoir bag for the patient to
inhale.
Mary Elizabeth Martelli R.N., B.S.The Gale Group Inc., Gale. Gale Encyclopedia of
Nursing and Allied Health, 2002
CPAP/Bi PAP
Continuous positive airway pressure (CPAP) is
the use of continuous positive pressure to
maintain a continuous level of positive airway
pressure. It is functionally similar to positive
end-expiratory pressure (PEEP),
CPAP also may be used to treat preterm
infants whose lungs have not yet fully
developed.
Eg-segmental lung collapse, ARDS, Pneumonia
CPAP is used when lung volumes are reduced
specially FRC
It will improve the lung compliance and
reduce the work of breathing
Conventional mechanical ventilation
Continuous mandatory ventilation
Assist-control ventilation
Intermittent mandatory ventilation
Synchronous intermittent mandatory
ventilation
Pressure support ventilation
CMV
Breaths are delivered at preset intervals,
regardless of patient effort.
This mode is used most often in the paralyzed
or apneic patient because it can increase the
work of breathing if respiratory effort is
present.
The hallmark of CMV is that the ventilator
makes no effort to sense patient effort
Assist-control ventilation
The ventilator delivers preset breaths in
coordination with the respiratory effort of the
patient.
With each inspiratory effort, the ventilator
delivers a full assisted tidal volume.
Spontaneous breathing independent of the
ventilator between A/C breaths is not allowed
http://www.lakesidepress.com/pulmonary/books/physiology/chap10b.
htm
IMV
With intermittent mandatory ventilation
(IMV), breaths are delivered at a preset
interval
Spontaneous breathing is allowed between
ventilator-administered breaths.
Spontaneous breathing occurs against the
resistance of the airway tubing and ventilator
valves, which may be formidable.
http://www.lakesidepress.com/pulmonary/books/physiology/chap10b.htm
SIMV
The ventilator delivers preset breaths in
coordination with the respiratory effort of the
patient.
Spontaneous breathing is allowed between
breaths.
Synchronization attempts to limit barotrauma
that may occur with IMV when a preset breath is
delivered to a patient who is already maximally
inhaled (breath stacking) or is forcefully exhaling.
Positive end-expiratory pressure
(PEEP)
PEEP can be used to increase oxygenation in
either AC or SIMV mode. The effect of PEEP on
the lungs is similar to blowing up a balloon
and not letting it completely deflate before.
http://www.modernmedicine.com/modern-medicine/news/quick-guide-vent-
essentials#sthash.7ljg63Wo.dpuf
Pressure support
For the spontaneously breathing patient, pressure
support ventilation (PSV) has been advocated to limit
barotrauma and to decrease the work of breathing.
Used alone or added to SIMV, this provides a small
amount of pressure during inspiration to help the
patient draw in a spontaneous breath.
http://www.modernmedicine.com/modern-medicine/news/quick-guide-vent-
essentials#sthash.7ljg63Wo.dpuf
auscultation
If patient is ventilated normal breath sounds
tend to be harsh
Percussion note
Plural effusion-stony dull
Atelectasis- consolidation dull
Pneumothorax - Hyperresonant
Chest expansion
Middle lobe & lingula motion
Upper lobe motion
Lower lobe motion
(>5cm)
Position of trachea
Vocal Fremitus(tactile)
Hand placement same as chest excursion.
Compare bilaterally
Ask pt to say k or 99
Note sound transmission under palm
Decrease transmission = air/emphysema
Increase transmission = consolidation, fluid
ABG-arterial blood gas
It is a blood test that is performed using blood
from an artery.
An ABG is a test that measures the arterial
oxygen tension (PaO
2
), carbon dioxide tension
(PaCO
2
), and acidity (pH).
http://en.wikipedia.org/wiki/Arterial_blood_gas
Sputum analysis
Bloody
inflammation of throat, bronchi; lung cancer;
sputum evenly mixed with blood, from alveoli, small
bronchi;
massive blood tuberculosis of lung, lung abscess,
bronchiectasis ,infarction, embolism.
Rusty colored - usually caused by
pneumococcal bacteria (in pneumonia)
Purulent - containing pus.
Foamy white - may come from obstruction or
even edema.
Frothy pink - pulmonary edema
MHI-Manual Hyper Ventilation
MHI sometimes known as "bagging" is a
technique that can be used as part of the
management of mechanically ventilated and
tracheostomy patients.
The physiotherapeutic technique involves the use
of a 2 liter, single patient use resuscitation bag
that is squeezed with a series of larger than
baseline peak airway pressures and tidal volume
at a slow inflation rate, with the addition of a
pause
A bag valve mask, abbreviated to BVM and
sometimes known by the proprietary name
Ambu bag or generically as a manual
resuscitator or self-inflating bag
Absolute Contraindications
1. Extra-alveolar air e.g. Bullae or Undrained
Pneumothorax
2. Subcutaneous emphysema of unknown
cause
3. Severe/widespread bronchospasm
Precautions
Pneumothorax, with a bubbling chest drain
Low, high or labile blood pressure
Labile ICP
Some lung diseases, especially emphysema/
hyperinflated lungs
Cardiac arrhythmias
Post Lung surgery
High PEEP requirements combined with high Fi02
requirement
PEEP > 10cmH20 on mechanical ventilation
Effects
Optimise alveolar ventilation. By reducing
atelectasis, this reduces ventilation perfusion
mismatch and improves gas exchange (Rothen et
al., 1993 and 1995)
Mobilise pulmonary secretions (Jones et al.,
1992)
Improve lung compliance (Hodgson et al., 1996)
A PEEP valve may be used when the patient is
on a PEEP > 10cmH2O and shows clinical signs
of desaturation.
Disconnect patient from the ventilator, attach
the bagging circuit to the catheter mount,
attach the reservoir bag to the ventilator
tubing and mute the alarm or switch the
ventilator to standby as per local policy in the
Unit
Using 1 or 2 hands, co-ordinate the delivery of
the breaths with any respiratory efforts of the
patient. Allow the patient to acclimatise by
using small TVs initially
Care should be taken to minimise movement
of the endotracheal or tracheostomy tube
during MHI
Use 10-15l of O
2
Common technique is slow inspiration and
inspiratory hold followed by quick expiratory
release.
Long inspiratory hold is contraindicated in a
patient who is already hyperinflated
If indicated apply manual techniques such as
shaking or vibration at the end of expiration
and during expiration
Repeat the procedure several times as
indicated(6-8 times)
Suctioning
Limb physiotherapy
Passive/Active movement
Positioning
Positioning for physiotherapy with the good
lung down is associated with improved
ventilation perfusion ratios and oxygenation
Side to side turning improves oxygenation
Prone positioning improves oxygenation in
patients with atelectatic superior and
posterior lower lobe segments
Ventilation/perfusion ratio
It is defined as: the ratio of the amount of air
reaching the alveoli to the amount of blood
reaching the alveoli.
"V" ventilation the air that reaches the alveoli
"Q" perfusion the blood that reaches the
alveoli
http://en.wikipedia.org/wiki/Ventilation/perfusion_ratio
1 liter of blood can hold about 200 mL of oxygen;
1 liter of dry air has about 210 mL of oxygen.
Therefore, under these conditions, the ideal
ventilation perfusion ratio would be about 1.05.
V/Q ratio-1.05
The actual values in the lung vary depending on
the position within the lung. If taken as a whole,
the typical value is approximately 0.8
Potrebbero piacerti anche
- Recent Advances in PhysiotherapyDa EverandRecent Advances in PhysiotherapyCecily PartridgeNessuna valutazione finora
- Physiotherapy in IcuDocumento18 paginePhysiotherapy in Icu_darkangel26_0% (1)
- Physiotherapy For Vascular PatientDocumento44 paginePhysiotherapy For Vascular PatientHaengbokaeyo Hua Min100% (4)
- Physiotherapy For ChildrenDocumento2 paginePhysiotherapy For ChildrenSuleiman AbdallahNessuna valutazione finora
- Principles of Chest Physiotherapy in ICUDocumento42 paginePrinciples of Chest Physiotherapy in ICUKapil Lakhwara100% (3)
- PepDocumento8 paginePepUdayakrishnan P Kanhangad100% (1)
- Physiotherapy in General Surgical ConditionDocumento7 paginePhysiotherapy in General Surgical Conditionprofpt98100% (8)
- Chest Physiotherapy in Intensive Care Unit (ICU) PDFDocumento399 pagineChest Physiotherapy in Intensive Care Unit (ICU) PDFGuillermo Sasso Pacheco83% (6)
- Cardiorespiratory AssessmentDocumento7 pagineCardiorespiratory AssessmentHanna SofiaNessuna valutazione finora
- Physiotherapy in The ICUDocumento10 paginePhysiotherapy in The ICUakheel ahammedNessuna valutazione finora
- Physiotherapy ManagementDocumento137 paginePhysiotherapy ManagementLavanya AuthimooalmNessuna valutazione finora
- Traumatic Brain Injury Physiotherapy AssessmentDocumento20 pagineTraumatic Brain Injury Physiotherapy AssessmentNithin Nair100% (1)
- Suspension TherapyDocumento39 pagineSuspension TherapyFarrukh Shahzad100% (5)
- Complications of Bed Rest 1Documento4 pagineComplications of Bed Rest 1Geetha Bhavani100% (2)
- Chest PhysiotherapyDocumento16 pagineChest Physiotherapyhemaanandhy75% (4)
- Physiotherapy Management of Vascular DisordersDocumento55 paginePhysiotherapy Management of Vascular DisordersAkheel AhammedNessuna valutazione finora
- Tendon Transfers - RehabilitationDocumento4 pagineTendon Transfers - RehabilitationPankaj Malik100% (4)
- Joint MobilizationDocumento42 pagineJoint MobilizationSérgio Xavier Silva100% (1)
- Manual Hyper InflationDocumento39 pagineManual Hyper InflationDeepa SuvarnaNessuna valutazione finora
- Peripheral Vascular DiseaseDocumento32 paginePeripheral Vascular DiseaseShy PatelNessuna valutazione finora
- PT Management of Spinal Cord InjuryDocumento20 paginePT Management of Spinal Cord InjuryJen Passilan100% (1)
- Orthopedic Physiotherapy AssessmentDocumento2 pagineOrthopedic Physiotherapy AssessmentVijaya KrishnaNessuna valutazione finora
- Icu and PhysiotherapyDocumento81 pagineIcu and PhysiotherapyLakshmi Prasanna100% (2)
- Positive Expiratory PressureDocumento21 paginePositive Expiratory PressureVijayalaxmi KathareNessuna valutazione finora
- MPT Books ListDocumento3 pagineMPT Books ListImran KhanNessuna valutazione finora
- Vertebrobasilar SyndromeDocumento14 pagineVertebrobasilar SyndromeHitesh RohitNessuna valutazione finora
- Musculoskeletal - Physiotherapy - Amy WashbrookDocumento35 pagineMusculoskeletal - Physiotherapy - Amy WashbrookRaluca Andreea100% (1)
- Cardio Pulmonary AssessmentDocumento7 pagineCardio Pulmonary AssessmentRaj KannanNessuna valutazione finora
- Post operative physiotherapy management for flail chest or Multiple ribs fracture or Cardio-pulmonary rehabilitation or physiotherapy or physical therapy or flail chest or BPT or MPT or PT or project report or case study or medical field or MGR medical university or Senthil Kumar BPTDocumento67 paginePost operative physiotherapy management for flail chest or Multiple ribs fracture or Cardio-pulmonary rehabilitation or physiotherapy or physical therapy or flail chest or BPT or MPT or PT or project report or case study or medical field or MGR medical university or Senthil Kumar BPTdskmpt88% (8)
- Mastectomy and Physiotherapy Management Final YearDocumento24 pagineMastectomy and Physiotherapy Management Final YearNithin Nair57% (7)
- Books PhysiotherapyDocumento22 pagineBooks Physiotherapyroyalviren100% (2)
- Active and Passive MovementsDocumento20 pagineActive and Passive MovementsSajida Bibi Noonari57% (7)
- Thoracic Surgeries: Types Description IndicationsDocumento32 pagineThoracic Surgeries: Types Description IndicationsAnusha Verghese100% (1)
- ORTHOPAEDIC ASSESSMENT FORM - YoburajDocumento3 pagineORTHOPAEDIC ASSESSMENT FORM - Yoburajsundar_kumar0Nessuna valutazione finora
- Cardio Alexandra Hough 2nd EditionDocumento376 pagineCardio Alexandra Hough 2nd EditionManoj M100% (1)
- Physiotherapy in Gastrectomy CholecystectomyDocumento19 paginePhysiotherapy in Gastrectomy Cholecystectomyakheel ahammedNessuna valutazione finora
- Physiotherapy Guidelines For Manual HyperinflationDocumento5 paginePhysiotherapy Guidelines For Manual HyperinflationAhmed Abd Elrauf100% (2)
- Physiotherapy in AmputationsDocumento6 paginePhysiotherapy in Amputationskrissh20Nessuna valutazione finora
- Diabetes and PhysiotherapyDocumento15 pagineDiabetes and Physiotherapyane2saNessuna valutazione finora
- Hari Subedi Physiotherapist: Physiotherapy Equipment ChecklistDocumento7 pagineHari Subedi Physiotherapist: Physiotherapy Equipment ChecklistdinuNessuna valutazione finora
- Cardiac Rehabilitation ProtocolDocumento5 pagineCardiac Rehabilitation Protocolmarkhabm100% (1)
- Cardiopulmonary PhysiotherapyDocumento181 pagineCardiopulmonary PhysiotherapyOana Moza100% (3)
- PNF - TechniquesDocumento34 paginePNF - Techniquesbpt2100% (4)
- Neurological Physiotherapy Evaluation Form Wm-2Documento15 pagineNeurological Physiotherapy Evaluation Form Wm-2Mohamed HarithNessuna valutazione finora
- Physiotherapy Assessment For Orthopedic ConditionsDocumento6 paginePhysiotherapy Assessment For Orthopedic ConditionsSHAIK SHABEENA100% (3)
- Role of Physiotherapy in Management of Burns-HshDocumento25 pagineRole of Physiotherapy in Management of Burns-HshChristopher Chibueze Igbo100% (1)
- Physiotherapy For Stroke Patients - Physiotherapy Remedies For Victims of StrokeDocumento9 paginePhysiotherapy For Stroke Patients - Physiotherapy Remedies For Victims of StrokeHumaira RahmanNessuna valutazione finora
- Physiotherapy Care Protocol For Low Back PainDocumento29 paginePhysiotherapy Care Protocol For Low Back Painaliaarif75% (4)
- The Indian Association of Physiotherapists - IAP Constitutions PDFDocumento17 pagineThe Indian Association of Physiotherapists - IAP Constitutions PDFHasan RahmanNessuna valutazione finora
- Specialist Physiotherapy Assessment FormDocumento4 pagineSpecialist Physiotherapy Assessment FormSathish Kumar100% (2)
- Cardiac RehabilitationDocumento125 pagineCardiac RehabilitationHiral vankar100% (1)
- Pulmonary Rehabilitation (S)Documento79 paginePulmonary Rehabilitation (S)liz100% (3)
- Neurological Physiotherapy Evaluation FormDocumento6 pagineNeurological Physiotherapy Evaluation FormAsif Khan100% (4)
- Physiotherapy in Pediatrics - NEURO MUSCULAR CONDITIONSDocumento28 paginePhysiotherapy in Pediatrics - NEURO MUSCULAR CONDITIONSKumar G PalaniNessuna valutazione finora
- DeQuervain Disease, A Simple Guide To The Condition, Treatment And Related ConditionsDa EverandDeQuervain Disease, A Simple Guide To The Condition, Treatment And Related ConditionsNessuna valutazione finora
- Everything You Wanted to Know About the Back: A Consumers Guide to the Diagnosis and Treatment of Lower Back PainDa EverandEverything You Wanted to Know About the Back: A Consumers Guide to the Diagnosis and Treatment of Lower Back PainNessuna valutazione finora
- Length Tension Testing Book 2, Upper Quadrant: A Workbook of Manual Therapy TechniquesDa EverandLength Tension Testing Book 2, Upper Quadrant: A Workbook of Manual Therapy TechniquesValutazione: 1 su 5 stelle1/5 (1)
- Common Diseases in NCLEXDocumento15 pagineCommon Diseases in NCLEXdecsag06Nessuna valutazione finora
- 1 s2.0 S0883944118304246 Main PDFDocumento7 pagine1 s2.0 S0883944118304246 Main PDFfitrianiNessuna valutazione finora
- Deep BreathingDocumento10 pagineDeep BreathingfarhaanrazzakNessuna valutazione finora
- ATELECTASISDocumento27 pagineATELECTASISBrian100% (1)
- Essentials of Physiotherapy After Thoracic Surgery - What Physiotherapists Need To Know. A Narrative ReviewDocumento15 pagineEssentials of Physiotherapy After Thoracic Surgery - What Physiotherapists Need To Know. A Narrative ReviewMariana MadridNessuna valutazione finora
- Presentation2.Ppt P&CDocumento38 paginePresentation2.Ppt P&CElla CaroNessuna valutazione finora
- Occupational Lung DiseaseDocumento31 pagineOccupational Lung DiseaseRapid Medicine100% (2)
- Lesson 1 Oxygenation Suctioning Bronchial HygieneDocumento14 pagineLesson 1 Oxygenation Suctioning Bronchial HygieneRENEROSE TORRESNessuna valutazione finora
- 3.causes of Opacified CXRDocumento20 pagine3.causes of Opacified CXRStashia EquinaNessuna valutazione finora
- SuctioningDocumento6 pagineSuctioningCriselda Ultado100% (2)
- Nursing Care Plan: Holy Name University College of Health Sciences Department of Nursing Tagbilaran City, BoholDocumento4 pagineNursing Care Plan: Holy Name University College of Health Sciences Department of Nursing Tagbilaran City, BoholAllison CrookeNessuna valutazione finora
- Asthma and COPD NCLEXDocumento17 pagineAsthma and COPD NCLEXPotchiee PfizerNessuna valutazione finora
- Pulmozyme Mue PosterDocumento1 paginaPulmozyme Mue Posterapi-290231811Nessuna valutazione finora
- Winninghams Critical Thinking Cases in Nursing 5th Edition Harding Solutions ManualDocumento66 pagineWinninghams Critical Thinking Cases in Nursing 5th Edition Harding Solutions ManualTiglao, Camile Ann C.0% (1)
- Fisiologia Respiratoria para Anestesiologos 2019 PDFDocumento14 pagineFisiologia Respiratoria para Anestesiologos 2019 PDFAlvarez Flores GilmerNessuna valutazione finora
- Shi Et Al-2019-Intensive Care MedicineDocumento11 pagineShi Et Al-2019-Intensive Care MedicineJavier BlancNessuna valutazione finora
- Basic Chest UltrasoundDocumento60 pagineBasic Chest UltrasoundAdriana Villarreal100% (1)
- Plain Chest X RayDocumento154 paginePlain Chest X RaySamuel Gamadey100% (3)
- Chest PT in Icu 1996@609.full PDFDocumento17 pagineChest PT in Icu 1996@609.full PDFDyah SafitriNessuna valutazione finora
- 02 Incentive SpirometryDocumento5 pagine02 Incentive SpirometrygireeshsachinNessuna valutazione finora
- Postural DrainageDocumento19 paginePostural Drainagenkarthikraj100% (1)
- Study Notes PediatricsDocumento86 pagineStudy Notes PediatricsMedShare100% (19)
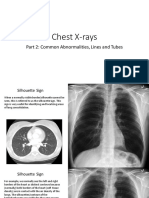
- Chest Xray PT 2Documento41 pagineChest Xray PT 2pvs5155Nessuna valutazione finora
- Care of Clients With Physiologic and Psychosocial AlterationsDocumento34 pagineCare of Clients With Physiologic and Psychosocial AlterationsChloie Marie RosalejosNessuna valutazione finora
- Bronchiolitis in ChildrenDocumento16 pagineBronchiolitis in ChildrenDhan RamadhanNessuna valutazione finora
- Postural DrainageDocumento7 paginePostural DrainageBiway RegalaNessuna valutazione finora
- Blue Protocol. Lung Ultrasound in The Critically IllDocumento12 pagineBlue Protocol. Lung Ultrasound in The Critically IllRomina Alfonsina Decap CarrascoNessuna valutazione finora
- Postural DrainageDocumento19 paginePostural DrainageAtul SrivastavaNessuna valutazione finora
- ATELEKTASISDocumento37 pagineATELEKTASISGalih Arief Harimurti WawolumajaNessuna valutazione finora
- Chest Physical Therapy For Patients in The Intensive Care Unit (APTA Journal)Documento19 pagineChest Physical Therapy For Patients in The Intensive Care Unit (APTA Journal)Physio EbookNessuna valutazione finora