Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
The Effects of Dose, Route of Administration, Drug Scheduling and MDR-1 Gene
Caricato da
Aleine Leilanie Oro0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
10 visualizzazioni7 pagineOral Gavage
Drug Scheduling
MDR-1 Gene
Copyright
© © All Rights Reserved
Formati disponibili
PDF, TXT o leggi online da Scribd
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoOral Gavage
Drug Scheduling
MDR-1 Gene
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato PDF, TXT o leggi online su Scribd
0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
10 visualizzazioni7 pagineThe Effects of Dose, Route of Administration, Drug Scheduling and MDR-1 Gene
Caricato da
Aleine Leilanie OroOral Gavage
Drug Scheduling
MDR-1 Gene
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato PDF, TXT o leggi online su Scribd
Sei sulla pagina 1di 7
Leukemia (2000) 14, 17961802
2000 Macmillan Publishers Ltd All rights reserved 0887-6924/00 $15.00
www.nature.com/leu
The effects of dose, route of administration, drug scheduling and MDR-1 gene
transfer on the genotoxicity of etoposide in bone marrow
SD Turner
1
, JA Rafferty
1
, LJ Fairbairn
1
, J Ashby
3
, H Tinwell
3
, H-G Eckert
4,5
, C Baum
4
and LS Lashford
1,2
1
Department of Experimental Haematology, Paterson Institute for Cancer Research,
2
Academic Unit of Paediatric Oncology, Christie Hospital
(NHS Trust), Manchester, UK;
3
Central Toxicology Laboratory, AstraZeneca, Maccleseld, UK; and
4
Heinrich-Pette Institute, Hamburg,
Germany
We have used the bone marrow micronucleus assay (BMMN)
as a measure of clastogenicity, in response to etoposide
exposure in murine bone marrow. Oral delivery of etoposide
resulted in a reduced number of micronucleated polychromatic
erythrocytes (MPE) relative to the same dose delivered intra-
peritoneally (P 0.001). Daily fractionation of the oral schedule
of etoposide led to a more than six-fold increase in cumulative
MPE frequency over that observed with the same total, unfrac-
tionated dose, with the potency of the response increasing with
serial exposure (r = 0.79). Retrovirally-mediated expression of
MDR1 in murine bone marrow resulted in partial protection
against the clastogenic activity of etoposide relative to mock
transduced control mice. The model system developed has
indicated a variety of factors able to inuence the genotoxicity
of etoposide. It should now be possible to further exploit this
model in order to dene other factors governing haemopoietic
sensitivity to etoposide. Leukemia (2000) 14, 17961802.
Keywords: multidrug resistance; etoposide dose schedule; bone
marrow; gene transfer; micronucleus
Introduction
The epipodophyllotoxins etoposide and teniposide are chem-
otherapeutic agents that are widely used in the management
of solid tumours and haematological malignancies.
1
Both
compounds form cleavable complexes with DNA topoisomer-
ase II and therefore induce double-stranded DNA breaks
which, if unrepaired, are responsible for cell death both in
tumour and in dose-limiting tissues such as the bone mar-
row.
26
Persistent DNA damage in surviving cells is implicated
in the genesis of a therapy-related secondary leukaemia
(tAML) which is characterised by a translocation involving the
MLL1 gene at 11q23.
7
Although tAML is a relatively rare event
there is a signicant body of evidence indicating that the risk
of developing secondary leukaemia increases with the fre-
quency of administration and cumulative exposure to these
drugs.
813
The frequency of tAML appears to rise after cumu-
lative doses in excess of 2000 mg/m
2,811
and other studies,
most notably in childhood leukaemia, have indicated that
twice weekly or weekly administration of etoposide is associa-
ted with a cumulative risk of tAML approaching 12%.
13
While these retrospective studies demonstrate the associ-
ation between etoposide exposure and tAML, they are unable
to elucidate and predict additional factors which may inu-
ence the frequency of persistent DNA damage. This may
include effects of other DNA damaging agents such as cispla-
tin
14,15
and alkylating agents,
12,16
anti-metabolites,
13,17
growth
factors
18
and therapeutic manoeuvres such as genetic manipu-
Correspondence: LS Lashford, Academic Unit of Paediatric Oncology,
Christie Hospital (NHS Trust), Wilmslow Road, Manchester M20 4BX,
UK; Fax: 44 161 446 3092
5
Current address: EUFETS GmbH, Vollmersbachstrae 66, 55743
Idar-Oberstein, Germany
Received 27 September 1999; accepted 1 March 2000
lation of drug resistance which aim to increase bone marrow
tolerance to chemotherapy.
19
The latter two factors may be
particularly important, as there may be a correlation between
reducing acute cytotoxicity and promoting survival of geneti-
cally damaged cells. To investigate this concept further we
have established a murine model in which a single genotoxic
endpoint can be quantied in the context of different treat-
ment strategies aimed at improving the therapeutic index of
etoposide. Thus it is possible to relate dose, schedule and
other factors including the expression of drug resistance func-
tions such as MDR1, to a dened measure of DNA damage.
A number of assays for genotoxicity is available and follow-
ing initial investigation the bone marrow micronucleus
(BMMN) assay was chosen as an appropriate measure of DNA
damage.
20
This assay detects clastogenic damage which per-
sists after one full cycle of erythrocyte replication (Figure 1)
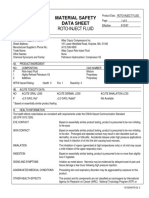
Figure 1 The BMMN assay detects clastogenic activity in the
erythropoietic lineage of the haemopoietic compartment in the form
of MPE. PE lack a nucleus and therefore MN are easily detectable in
these cells. The PE and MPE mature into normocytes, which may
senesce in the bone marrow or migrate into the peripheral blood
along with the immature MPE and PCE.
Genotoxicity of etoposide in bone marrow
SD Turner et al
1797
and is considered to be a good surrogate marker for the car-
cinogenic potential of any genotoxin. The current study
describes the sensitivity of the BMMN assay following etopo-
side exposure, and considers the inuence of dose, route and
schedule of etoposide administration on micronucleus induc-
tion. Furthermore, given the current interest in protecting bone
marrow from the acute cytotoxic effects of chemotherapy by
overexpression of MDR1,
21
we have used the mouse model
to investigate the impact of this strategy on etoposide-induced
micronucleus frequency.
Materials and methods
Chemicals
A clinical preparation of etoposide was purchased from Bristol
Myers (Hounslow, UK) and contained etoposide at a concen-
tration of 20 mg/ml, as well as citric acid (2 mg/ml), polyethyl-
ene glycol 300 (650 mg/ml), benzyl alcohol (30 mg/ml),
Tween 80 (80 mg/ml) and ethanol (30.5% v/v). Etoposide was
diluted to the required concentrations (0.11.0 mg/ml) in
physiological saline and was prepared immediately before
administration to animals.
Mice
Male and female B6D2F1 mice aged 8 to 10 weeks old were
obtained from the Paterson Institute breeding colony. All
experimental procedures were performed in accordance with
the Animals (Scientic Procedures) Act (1986).
Bone marrow micronucleus assay
Groups of mice were treated with drug and were sacriced
by cervical dislocation 24 h after treatment. The bone marrow
from one femur of each mouse was ushed into 1 ml of foetal
calf serum. Smears were prepared on glass microscope slides,
were stained with acridine orange as described previously
22
and assessed for micronucleated polychromatic erythrocyte
(MPE) frequency amongst 2000 polychromatic erythrocytes
(PCE). The ratio of PCE to normochromatic erythrocytes (NE)
amongst 1000 cells was also analysed for each mouse as an
indicator of the toxicity of etoposide to the erythroid compart-
ment of the bone marrow.
The frequency of micronucleated peripheral blood reticulo-
cytes was determined by smearing a drop of blood (removed
via cardiac puncture) from the treated mice 48 h after drug
administration and on to a pre-coated microscope slide under
a coverslip. Cells were stained super vitally with acridine
orange as previously described.
23
The slides were analysed for
the frequency of micronucleated reticulocytes amongst 1000
reticulocytes (see Tables 1 and 2 for the dosing regimens
employed).
Reconstitution of mice with MDR-1 transduced bone
marrow
Bone marrow was harvested from both femurs of 100 male
mice 48 h after treatment with 150 mg/kg of 5-uorouracil
(David Bull Laboratories, Warwick, UK) intravenously. The
bone marrow cells were then cultured in prestimulation
Leukemia
Table 1 Regimen of etoposide administration
Group Delivery vehicle Etoposide (mg/kg)
1 10
2 10 (1)
3 2 8 (1.25)
4 6 4 (2.5)
5 8 2 (5)
6 9 1 (10)
Male B62DF1 mice aged 810 weeks old were administered the
indicated number of treatments p.o. Each dose was given 24 h
apart and all of the mice were sacriced 24 h following the nal
treatment.
Table 2 Regimen of etoposide administration
Group No. Delivery vehicle Etoposide (2.5 mg/kg)
1, 6 4
2, 7 3 1
3, 8 2 2
4, 9 1 3
5, 10 4
Male B62DF1 mice aged 810 weeks old were administered the
indicated number of treatments of delivery vehicle and etoposide
spaced 24 h apart. Groups 15 were sacriced 24 h after the nal
dose and were entered into the BMMN assay. Groups 610 were
sacriced 48 h following the nal treatment and were entered into
the BMMN and PBR assays.
medium (DMEM supplemented with 20% foetal calf serum,
0.1% BSA, 2 mM glutamine, 200 U/ml recombinant human
IL-6 (Sandoz, Basle, Switzerland)), 10 ng/ml recombinant
murine IL-3 (R&D Systems, Abingdon, UK) and 100 ng/ml
recombinant rat stem cell factor (Amgen, Thousand Oaks, CA,
USA) for 48 h at 37C. Bone marrow cell cultures were then
overlaid on to amphotropic MDR-1 retroviral producers
24
or
-iduronidase producers
25
(mock transduction) for 48 h in the
same medium with the addition of 5 g/ml polybrene. Bone
marrow cells were harvested by gentle shaking of the culture
asks and after a wash in serum-free medium were injected
into the tail vein of 100 female marrow ablated recipients
(irradiated at 15 Gy using a
60
Co source over 16 h) at 5
10
6
cells/mouse.
26
After a period of 46 weeks the mice were
entered into the BMMN assay.
Granulocytemacrophage colony-forming unit plating
An aliquot of 10
5
bone marrow cells from pooled group
samples, 4 weeks after transduction and transplantation was
suspended in 0.5 ml of IMDM supplemented with 20% FCS,
10% BSA and 1% IL-3. Next, 0.5 ml of methylcellulose was
added and the solution was mixed with a blunt-ended needle.
The mixture was then plated into three wells of a 24-well
microtitre plate which was then incubated at 37C for 1 week
in an atmosphere of 5% CO
2
, 5% O
2
, 90% N
2
. Colonies were
picked into 50 l of K buffer (100 l 10 PCR buffer, 900 l
0.5% Tween 20 and 5 l proteinase K (20 mg/ml)), ash
frozen in liquid nitrogen and stored at 80C prior to analysis
by PCR for human MDR-1 and murine Y-chromosome DNA
sequence.
Genotoxicity of etoposide in bone marrow
SD Turner et al
1798
Leukemia
Figure 2 The micronucleus frequency (bars) and polychromatic to normochromatic erythrocyte ratio (PCE:NE, line) in the bone marrow of
male B6D2F1 mice treated with increasing i.p. doses of etoposide (n = 5). The number of MPE amongst 2000 PCE and the ratio of PCE:NE
among 1000 cells were counted. Results represent the means and standard errors of the individual animal data. These data were reproduced
in a second experiment employing the same number of mice and dosing regimen (data not shown).
PCR to detect human MDR-1 and murine Y-
chromosome sequence
PCR of human MDR-1 cDNA was carried out using primers
that span a 523 bp fragment of DNA (sense, 5 AGA TCA ACT
CGT AGG AGT GTC 3, antisense, 5 GTT TCT GTA TGG
TAC CTG CAA 3) with 35 cycles of 94C for 1 min, 59C for
1 min and 72C for 1 min followed by 5 min at 72C. As a
control for ampliable DNA in GM-CFC colonies, PCR was
carried out using primers specic for regions of murine Y-
chromosome DNA according to a standard protocol.
27
Statistical analysis
Results were analysed for statistical signicance using the Stu-
dents t-test except for the experiment analysing both 24 h
bone marrow and 48 h bone marrow and blood, where results
were analysed by Spearmans correlation.
Results
Sensitivity of the bone marrow micronucleus assay to
etoposide
Etoposide causes a dose-dependent suppression of bone mar-
row function. This is manifest in the erythrocyte compartment
as a block in production of polychromatic erythrocytes and
hence depression in the PCE:NE ratio (Figure 2). For the pur-
pose of the BMMN assay a PCE:NE ratio of 1 indicates a
level of toxicity above which the dose dependence of
micronucleus induction is lost due to the impact of toxicity
on polychromatic erythrocyte production.
20
When etoposide
was administered via the intraperitoneal (i.p.) route, a PCE:NE
ratio of 1 was reached at doses between 0.5 and 1 mg/kg.
This is consistent with the observed rise in MPE frequency at
etoposide doses up to 1 mg/kg. For this reason, 1 mg/kg was
selected as the reference dose for micronucleus induction in
subsequent studies involving i.p. administration of etoposide.
Determination of the effect of route of administration
on etoposide-induced micronucleus formation
The route of administration of etoposide had a profound effect
on the frequency of micronucleus induction. As expected, 1
mg/kg of etoposide administered i.p., produced a potent
response and at a level consistent with those described before
(Figure 3). Oral (p.o.) administration of 1 mg/kg etoposide
resulted in a major reduction in the number of micronuclei
observed (P 0.001) compared to the same dose given by
the i.p. route. This difference is not explained by toxicity as
the PCE:NE ratio following either route of exposure remained
above 1 (Table 3) (ie in the range where no adverse effects of
toxicity on the reproducibility of the assay are seen
20
). At a
higher dose (10 mg/kg), i.p. administration of etoposide
resulted in major toxicity and this precluded analysis of the
frequency of MPE. However, following oral administration of
10 mg/kg etoposide, there was a signicant rise in the fre-
quency of MPE (P 0.01) relative to the 1 mg/kg p.o. dose.
Figure 3 The frequency of MPE in the bone marrow of mice 24 h
following treatment with the indicated doses of etoposide by both i.p.
(open bars) and p.o. (solid bars) routes of administration.
Genotoxicity of etoposide in bone marrow
SD Turner et al
1799
Table 3 The ratio of PCE:NE in the bone marrow of mice 24 h after administration of the indicated doses of etoposide
Effect of route of administration Effect of fractionated Mechanism of the Inuence of MDR 1 overexpression
(Figure 3) schedule (Figure 4) schedule effect (Figure 5) (Figure 6)
Etoposide Route of Average Schedule Average Schedule Average Transduced Etoposide Average
(mg/kg) administration PCE:NE of PCE:NE of PCE:NE gene (mg/kg) PCE:NE
s.d. etoposide s.d. etoposide s.d. s.d.
(mg/kg) (mg/kg)
0 i.p. 1.41 0.17 0 1.41 0.22 0 1.41 0.23 Mock 0 1.43 0.21
p.p. 1.34 0.25 10 10 1.36 0.13 1 2.5 1.19 0.11 MDR1 0 1.45 0.22
1 i.p. 1.06 0.17 8 1.25 1.35 0.11 2 2.5 1.14 0.09 Mock 1 1.41 0.14
p.o. 1.43 0.12 4 2.5 1.39 0.14 3 2.5 1.12 0.14 MDR1 1 1.43 0.20
10 i.p. 0.21 0.04 2 5 0.33 0.13 4 2.5 1.13 0.11
p.o. 1.30 0.15 1 10 1.05 0.12
This Table demonstrates the results obtained in all of the experiments performed employing the BMMN assay.
Determination of the effect of fractionated schedule
on etoposide-induced micronucleus induction
To determine whether the micronucleus assay can discrimi-
nate between different schedules of etoposide, animals were
administered drug to a maximal cumulative oral dose of 10
mg/kg in varying daily fractions (see Figure 4). Administration
of a single dose of 10 mg/kg in this experiment produced a
comparable frequency of MPE to that demonstrated in Figure
3. However, fractionating the dose to 2 5 mg/kg and 4
2.5 mg/kg led to a signicant (two-fold) elevation (P 0.01)
in the frequency of MPE measured 24 h after delivery of the
nal dose of etoposide. Further fractionation of the dose did
not show any signicant increase in MPE over a single dose
of 10 mg/kg. However, the number of MPE seen 24 h after the
last administration of 10 1 mg/kg etoposide was signicantly
higher (P 0.05) than that seen following a single dose of 1
mg/kg of this agent (Figure 3). Possible explanations for this
result might include persistence of MPE in the bone marrow
over the time course of the experiment or some priming event
which leads to increased sensitivity to subsequent doses of
drug. To try to distinguish between these two possibilities we
determined whether MPE accumulated in bone marrow or
peripheral blood at serial time points in the 4 2.5 mg/kg
schedule, 48 h following the last exposure to etoposide.
The effect of treating mice with 1, 2, 3 or 4 consecutive
doses of 2.5 mg/kg of etoposide are shown in Figure 5. With
each serial exposure there was a trend towards increasing
MPE frequency at 24 h after treatment (r = 0.79, P 0.001)
although the differences between consecutive treatments were
not statistically signicant (P 0.05). There was no evidence
of persistence of MPE in the bone marrow nor that micron-
Figure 4 The frequency of MPE in the bone marrow of mice 24 h
following administration of the nal dose of etoposide given p.o.
Leukemia
Figure 5 The frequency of MPE in the bone marrow of mice
treated with the indicated doses of etoposide 24 (solid bars) and 48
h (open bars) following administration of the nal dose in the bone
marrow and 48 h following the nal dose in peripheral blood
(hatched bars).
ucleated reticulocytes migrated into the peripheral blood 48
h after the last dose, indicating that the increased frequency
of MPE seen with dose fractionation was not due to accumu-
lation of these cells. Calculation of the total number of MPE
seen over the experiment indicated that not only did dose
fractionation lead to an increase in genotoxic damage detect-
able 24 h following the nal dose of etoposide administered,
but the cumulative damage over the dosing period was more
than six times that resulting from a single dose of 10 mg/kg.
Inuence of overexpression of MDR1 on
micronucleus induction following etoposide exposure
In order to investigate the inuence of MDR1 overexpression
on MPE induction by etoposide, bone marrow from male mice
were transduced with a retrovirus containing either the human
MDR1 cDNA (experimental) or an irrelevant control cDNA
(mock transduced). The cells were then transplanted back into
female myeloablated recipients. Analysis of colony-forming
cells from recipient mice indicated that a transduction
efciency of around 18% (9/50 PCR-positive colonies) had
been achieved, and subsequent micronucleus assay demon-
strated that MDR1 transduction conferred a statistically sig-
nicant protection (P 0.05) against micronucleus induction
by etoposide (Figures 6 and 7).
Genotoxicity of etoposide in bone marrow
SD Turner et al
1800
Leukemia
Figure 6 Treatment-induced clastogenicity in human MDR-1 and
mock transduced mice following exposure to etoposide (1 mg/kg,
open bars) or delivery vehicle (solid bars) administered intraperitone-
ally.
Figure 7 (a) Y-chromosome PCR of isolated GM-CFU colonies
plated from femoral bone marrow; +, positive control. (b) MDR-1 PCR
of K buffer extracts of isolated GM-CFU colonies plated from femoral
bone marrow; +, positive control.
Discussion
Although etoposide is widely recognised as a powerful leuka-
emogen,
713
it remains an important drug in cancer therapy.
A number of factors increase the risk of secondary malignancy
and these include cumulative exposure to drug and rapid
scheduling of etoposide pulses.
813
A recent review of the
modes of etoposide administration in UK paediatric practice
revealed 21 different schedules in multiple drug combi-
nations.
28
The most common method of drug delivery is intra-
venously at doses of 360450 mg/m
2
fractionated over 3 days,
and repeated every 3 weeks, although protracted oral fraction-
ated schedules, eg 50 mg/m
2
daily for 21 days have also been
used extensively. The latter schedule is a well tolerated out-
patient treatment, is associated with little haematological tox-
icity and, because of the maintenance of signicant serum lev-
els of drug over many days, may have increased efcacy.
29,30
Most reports of etoposide-associated secondary leukaemia
have followed pulsed intravenous therapy.
13
Recently, con-
cern has been expressed over orally administered etoposide,
although in the report of this work patients have been heavily
pre-treated with other DNA damaging agents, thus making it
difcult to determine the specic contribution of etoposide.
31
The inuence of such confounding variables on cancer risk
are difcult to assess and consequently this study set out to
establish a model in which the interaction of such factors
could be studied. The initial objectives were to identify a sur-
rogate endpoint for relevant DNA damage following etoposide
exposure (DNA strand breaks/translocation events), which
was also sufciently sensitive to detect damage over a clini-
cally relevant dose range (1.76.7 mg/kg/day).
28
Following
initial assessment of three different assays, the comet assay,
32
the MutaMouse model
33
and the BMMN assay,
20
we concen-
trated on the latter since it provided a reliable and reproduc-
ible measure of DNA damage at clinically-relevant dose
ranges.
A number of studies have shown that the BMMN assay is
a robust measure of the clastogenic activity of a variety of
compounds, including etoposide.
34,35
Moreover, given that
micronuclei result from the lag of chromosomal fragments on
the mitotic spindle, induction of these reects damage that
persists through at least one full cycle of DNA synthesis and
repair. Our results demonstrate that the assay is very sensitive
to the effects of etoposide exposure, with a signicant induc-
tion of MPE at doses as low as 0.1 mg/kg i.p. A dose-depen-
dent rise in MPE induction was seen up to 1 mg/kg i.p. after
which the balance between sublethal and cytotoxic events
was shifted towards bone marrow toxicity (as evidenced by
a reduction in the ratio of PE/NE to below one). The dose
dependency of MPE induction was also demonstrated for the
oral route of exposure, although neither maximal MPE induc-
tion nor toxicity were demonstrated. The explanation for this
observation may rest in part with the differences in bio-avail-
ability of etoposide following oral and i.p. administration, as
absorption of orally delivered etoposide may be as little as
17% of the administered dose.
36
Thus the route of drug deliv-
ery is an important factor in the routine assessment of drug-
induced clastogenicity using the BMMN assay, although for a
specied route of exposure this is a relatively sensitive and
consistent marker of DNA damage.
Given the apparent importance of schedule on the risk of
therapy-induced leukaemia, we investigated if the BMMN
assay was able to detect different levels of DNA damage fol-
lowing fractionated delivery of etoposide. An increased level
of MPE induction has been reported following fractionated
delivery of other drugs such as 1--D-arabinofuranosyl cyto-
sine (Ara-C) or methotrexate (MTX).
37
For the purpose of this
study etoposide was delivered orally as this route has found
increasing favour in clinical practice and is administered as a
highly fractionated schedule (i.e. twice daily over 21 consecu-
tive days).
Two conclusions can be drawn regarding the impact of frac-
tionating the dose. Firstly, as for a single pulse of etoposide
administration there is a dose-dependent rise in MPE induc-
tion measured 24 h after the last dose in any schedule unless
bone marrow toxicity is seen. The dose dependency of frac-
tion size is most clearly seen for the schedules of 10 1 mg,
8 1.25 mg and 4 2.5 mg where the PCE:NE ratio remains
above one. Therefore it is not unreasonable to conclude that
daily fractionation of etoposide administration is more clastog-
enic than a single high dose administration, and through sur-
vival of sublethally damaged cells is more likely to lead to the
genesis of a secondary leukaemia. However, this is unlikely
to be a simple relationship. Figure 5 illustrates that each
administered fraction engenders a clastogenic response and
that the response increases with sequential fractions. Thus the
overall risk of persistent generating DNA damage must relate
to the cumulative potency of the micronucleus response. Hya-
shi et al
38
accounted for the effect of cumulative exposure to
drug by a model whereby MPE resulting from a previous dose
remain in the bone marrow 48 h after administration and are
detected along with those caused by a subsequent dose of
agent resulting in an accumulation of MPE. This model was
applied to a number different compounds and held true for
Genotoxicity of etoposide in bone marrow
SD Turner et al
1801
some, although not for all agents tested.
38
Such a model can-
not, however, be used to explain the increase in MPE as a
result of exposure to multiple doses of etoposide, as the num-
ber of MPE at 48 h following the last dose of any series drops
to background levels. For these same reasons the increased
clastogenicity of subsequent doses cannot be easily explained
by the persistence of occult DNA damage, which is then
manifest as micronuclei following progression of cells through
cycle. Were this the case, signicant levels of MPE would be
expected at 48 h following the last dose of etoposide in any
series. Given that our data cannot be reconciled by a model
where persistence and accumulation of MPE occurs during the
dosing period, this points to an effect of etoposide adminis-
tration which leads to sensitisation of the bone marrow to sub-
sequent doses of this agent. A number of possibilities seem
worthy of consideration. Firstly, that the etoposide-induced
damage leads to increased cycling in the target compartment
for micronucleus induction (the erythroid lineage).
39
If etopo-
side induces cells into cycle, then this may in turn result in a
greater number of cells undergoing division in the presence of
this clastogen and thus displaying the results of drug-induced
injury. Another explanation for the observed effect might be
that treatment with etoposide increases topoisomerase II levels
in cells.
40
If this were the case, etoposide would be able to
interact with more enzyme, resulting in higher levels of DNA
strand breakage within target cells, and thus result in a higher
incidence of MPE. Alternatively, it is possible that some
element of long-term genomic instability occurs, similar to
that seen following -radiation damage to bone marrow.
41
Further experimentation will obviously be required to deter-
mine whether any of these mechanisms contribute to the
observed effects.
Notwithstanding the mechanism of schedule-dependent
exacerbation of etoposide- induced genotoxic damage to
bone marrow, it is clear that some schedules are likely to be
more genotoxic than others and that this is likely to reect the
clinical impact of etoposide administration. The model
described here provides a relatively robust means of determin-
ing the impact of etoposide scheduling on the bone marrow
compartment. Thus it may be possible, using this model, to
derive a protocol for etoposide administration/scheduling that
will achieve maximum tumour kill with minimum adverse
effects on bone marrow.
Alternatively it may be the case that genotoxicity in bone
marrow will always mirror tumour kill. If so, an alternative
means of minimising bone marrow toxicity will be required.
One alternative to modifying the dose/scheduling of etoposide
to ameliorate long-term effects in bone marrow might be to
modify the sensitivity of this tissue to etoposide. The MDR-1
gene product is known to confer resistance to the cytotoxic
effects of etoposide and related agents by acting as a mem-
brane pump that expels drug from cells, thus effectively lower-
ing the concentration of active agent in these cells.
42
Whilst
this undoubtedly leads to increased survival of cells, the
effects on other endpoints of genotoxic damage are undocu-
mented. In particular, one worry is that expression of MDR-1
in bone marrow cells which do not normally express this pro-
tein might lead to the increased survival of cells carrying sub-
lethal, but potentially mutagenic and carcinogenic damage.
19
Our data, however, show a clear protective effect against the
clastogenic activity of etoposide conferred by transfer of the
human MDR-1 gene into bone marrow. This rst ever demon-
stration of protection against clastogenicity by transfer and
expression of the human MDR1 gene suggests that it may also
be possible to reduce the mutagenic and potentially carcino-
Leukemia
genic effects of etoposide exposure using this approach. In
this scenario, it may be the case that the exact nature of the
scheduling of etoposide will become less important in terms
of reducing the development of iatrogenic haemopoietic
tumours and more emphasis may be put on maximising
tumour kill.
Acknowledgements
SDT is in receipt of an MRC studentship award and a Zeneca
case award. Research undertaken in the Paterson Institute was
supported by the Cancer Research Campaign (UK) and the
NHS Research and Development Levy. CB is funded by the
Deutsche Krebshilfe (101456 Ba2). We thank L Woolford, M
Willington and T McNally for technical assistance and Prof
OB Eden for his generous support and advice.
References
1 Pizzo PA, Poplack DG (eds). General principles of chemotherapy.
In: Principles and Practice of Paediatric Oncology. 2nd edn. Lip-
pincott-Raven: Philadelphia, Chapter 1:9, 1997, pp 215272.
2 Chen GL, Yang L, Rowe TC, Halligan BD, Tewey KM, Liu LF.
Non-intercalative antitumour drugs interfere with the breakage
reunion of mammalian DNA topoisomerase II. J Biol Chem 1984;
259: 1356013566.
3 Ross W, Rowe T, Glisson B, Yalowich J, Liu L. Role of topoisomer-
ase II in mediating epipodophyllotoxin-induced DNA cleavage.
Cancer Res 1984; 44: 58575860.
4 Markovits J, Pommier Y, Kerrigan D, Covey JM, Tilchen EJ, Kolm
KW. Topoisomerase II mediated DNA breaks and cytotoxicity in
relation with proliferation and the cell cycle in NIH3T3 broblasts
and L1210 leukaemia cells. Cancer Res 1987; 47: 20502055.
5 Pommier Y, Kerrigan D, Civey JM, Kao-Shan C, Whang-Peng J.
Sister chromatid exchanges, chromosomal aberrations and cyto-
toxicity produced by antitumour topoisomerase II inhibitors in
sensitive (DC3F) and resistant (DC3F/9-OHE) Chinese hamster
cells. Cancer Res 1988; 48: 512516.
6 Chatterjee S, Trivedi D, Petzold SJ, Berger NA. Mechanism of epi-
podophyllotoxin-induced cell death in poly(adenosine diphos-
phate-ribose) synthesis-decient V79 Chinese hamster cell lines.
Cancer Res 1990; 50: 27132718.
7 Hunger SP, Tkachuk DC, Amylon MD, Link MP, Carroll AJ, Wel-
born JL, Willman CL, Cleary ML. HRX involvement in de novo
and secondary leukaemias with diverse chromosome 11q23
abnormalities. Blood 1993; 81: 31973203.
8 Ratain MJ, Kaminer LS, Bitran JD. Actue non-lymphocytic leu-
kaemia following etoposide and cisplatin combination chemo-
therapy for advanced non-small cell carcinoma of the lung. Blood
1987; 70: 14121417.
9 Pederson-Bjergaard J, Daugaard J, Daugaard G, Hansen SW.
Increased risk of myelodysplasia and leukaemia after etoposide,
cisplatin and bleomycin for germ-cell tumours. Lancet 1991; 338:
359363.
10 Nichols CR, Breeden SE, Loehrer PJ. Secondary leukaemia asso-
ciated with a conventional dose of etoposide: review of serial
germ cell tumour protocols. J Natl Cancer Inst 1993; 85: 3640.
11 Bjorin DF, Motzer RJ, Rodriguez E. Acute non-lymphocytic leu-
kaemia in germ cell tumour patients treated with etoposide-con-
taining chemotherapy. J Natl Cancer Inst 1993; 85: 6062.
12 Hawkins MM, Wilson NMK, Stovall MA, Marsden HB, Potok
MHN, Kingston JE, Chessels JM. Epipodophyllotoxins, alkylating
agents and radiation risk of secondary leukaemia after childhood
cancer. Br Med J 1992; 304: 951958.
13 Pui C-H, Ribeiro RC, Hancock ML, Rivera GK, Evans WE, Rai-
mondi SC, Head DR, Behm FG, Mahmoud MH, Sandlund GT,
Crist WM. Acute myeloid leukaemia in children treated with epi-
podophyllotoxins for acute lymphoblastic leukaemia. New Engl J
Med 1991; 325: 16821687.
14 Wang L, Setlow R. Inactivation of O
6
-alkylguanine-DNA-alkyl-
Genotoxicity of etoposide in bone marrow
SD Turner et al
1802
Leukemia
transferase in HeLa cells by cisplatin. Carcinogenesis 1989; 10:
16811684.
15 Trey J, Gerson S. The role of O
6
-alkylguanine-DNA-alkyltransfer-
ase in limiting nitrosourea-induced sister chromatid exchanges in
proliferating human lymphocytes. Cancer Res 1989; 49: 1899
1903.
16 Le Beau MM, Albain KS, Larson RA, Vardiman JW, Davis EM,
Blough RR, Golomb HM, Rowley JD. Clinical and cytogenetic cor-
relations in 63 patients with therapy-related myelodysplastic syn-
dromes and acute non-lymphocytic leukaemia: further evidence
for characteristic abnormalities of chromosomes No. 5 and 7. J
Clin Oncol 1986; 4: 325345.
17 Winick NJ, McKenna RW, Shuster JJ, Schneider NR, Borowitz MJ,
Bowman WP, Jacaruso D, Kamen BA, Buchanen GR. Secondary
acute myeloid leukaemia in children with acute lymphoblastic
leukaemia treated with etoposide. J Clin Oncol 1993; 11: 209
217.
18 Van Os R, Robinson S, Sheridan T, Mislow JMK, Dawes D, Mauch
PM. Granulocyte colony-stimulating factor enhances bone mar-
row stem cell damage caused by repeated administration of cyto-
toxic agents. Blood 1998; 92: 19501956.
19 Rafferty JA, Hickson I, Chinnasamy N, Lashford LS, Margison GP,
Dexter TM, Fairbairn LJ. Chemoprotection of normal tissues by
transfer of drug resistance genes. Cancer Metast Rev 1996; 15:
365383.
20 Scmid W. The micronucleus test. Mutat Res 1975; 31: 915.
21 Rafferty JA, Lashford LS, Turner SD, Fairbairn LJ. Genetic chemo-
protection of bone marrow from the dose-limiting toxicities of
chemotherapy. Prog Growth Fact 1999; 5: 37.
22 Tinwell H, Ashby J. Comparison of acridine orange and giesma
stains in several mouse bone marrow studies including a triple
dose experiment. Mutagenesis 1989; 4: 477482.
23 Hyashi M, Morita T, Kodama Y, Sofuni T, Ishidate M. The
micronucleus assay with mouse peripheral blood reticulocytes
using acridine orange coated slides. Mutat Res 1990; 245: 245
249.
24 Eckert H, Stockschlader M, Just U, Hegewisch-Becker S, Grez M,
Uhde A, Zander A, Ostertag W, Baum C. High dose multidrug
resistance in primary human hematopoietic cells transduced with
optimized retroviral vectors. Blood 1996; 88: 34073415.
25 Fairbairn LJ, Lashford LS, Spooncer E, McDermott RH, Lebens G,
Arrand LE, Arrand JR, Bellantuono I, Holt R, Hatton CE, Cooper
A, Besley GTN, Wriath JE, Anson DS, Hopwood JJ, Dexter TM.
Long-term in vitro correction of -iduronidase deciency (Hurler
syndrome) in human bone marrow. Proc Natl Acad Sci USA 1996;
93: 20252030.
26 Chinnasamy N, Rafferty JA, Hickson I, Lashford LS, Longhurst SJ,
Thatcher N, Margison GP, Dexter TM, Fairbairn LJ. Chemoprotec-
tive gene transfer II: multilineage in vitro protection of haemopo-
iesis against the effects of an antitumour agent by expression of a
mutant human O
6
-alkylguanine-DNA alkyltransferase. Gene Ther-
apy 1998; 5: 842847.
27 Han YM, Yoo OJ, Lee KK. Sex determination in single mouse
blastomeres by polymerase chain reaction. J Assist Reprod Genet
1993; 10: 151156.
28 UKCCSG Chemotherapy Standardisation Working Group. 1994.
Personal communication: L Lashford.
29 Davidson A, Gowing R, Lowis L, Newell D, Lewis I, Dicks-
Mireaux C, Pinkerton CR. Phase II study of 21 day oral etoposide
in children. New agents group of the United Kingdoms Childrens
Cancer Study Group (UKCCSG). Eur J Cancer 1997; 33: 1816
1822.
30 Clark PL, Cottier B. The activity of 10, 14 and 21 day schedules
of single agent etoposide in previously untreated patients with
extensive SCLC. Semin Oncol 1992; 19 (Suppl. 14): 3639.
31 Bertholt F. University of Cologne, Germany. Personal communi-
cation.
32 Singh SP, McCoy MT, Tice RR, Schneider EL. A simple technique
for quantitation of low levels of DNA damage in individual cells.
Exp Cell Res 1988; 175: 184191.
33 Hoorn AJW, Custer LL, Myhr BC, Brusick D, Gossen J, Vigj J.
Detection of chemical mutagens using MutaMouse: a transgenic
mouse model. Mutagenesis 1993; 8: 710.
34 Ashby J, Tinwell H, Glover P, Poorman-Allen P, Krehl R, Callander
RD, Clive D. Potent clastogenicity of the human carcinogen eto-
poside to the mouse bone marrow and mouse lymphoma L5178Y
cells: comparison to Salmonella responses. Environ Mol Mutagen
1994; 24: 5160.
35 Larripa IB, Carballo MA, Mudry MM, Laball de Vinusa L. Etopo-
side and teniposide: in vitro and in vivo genotoxicity studies. Drug
Invest 1992; 4: 365375.
36 Stewart DJ, Nundy D, Maroun JA, Tetreault L, Prior J. Bioavail-
ability, pharmacokinetics and clinical effects of an oral prep-
aration of etoposide. Cancer Treat Rep 1985; 69: 269273.
37 Collaborative Study Group for the Micronucleus Test, The Mam-
malian Mutagenesis Study Group of the Environmental Mutagen
Society, Japan (CSGMT/JEMS.MMS). Single vs multiple dosing in
the micronucleus test: the summary of the fourth collaborative
study by CSGMT/JEMS.MMS. Mutat Res 1990; 234: 205222.
38 Hayashi M, Sofuni T, Morita T. Simulation study of the effects of
multiple treatments in the mouse bone marrow micronucleus test.
Mutat Res 1991; 252: 281287.
39 Hoand K, Peterson BO, Helin K, Jensen PB, Sehested M.
Response of cellular DNA topoisomerases to induction of full
length E2F-1/DP-1 transcription factor. Proc Am Assoc Cancer Res
1997; 38: 62.
40 Isaacs RJ, Davies SL, Sandri MI, Redwood C, Wells NJ, Hickson
ID. Physiological regulation of eukaryotic topoisomerase II.
Biochim Biophys Acta 1998; 1400: 121137.
41 Wright EG. Radiation-induced genomic instability in haemopo-
ietic cells. Int J Radiat Biol 1998; 74: 681687.
42 Spiers AD. Multiple drug resistance, the MDR gene, and the law
of maximum perversity as it applies to oncology: an hypothesis.
Haematol Oncol 1994; 12: 155161.
Potrebbero piacerti anche
- Waste QuestionnaireDocumento6 pagineWaste QuestionnaireAleine Leilanie OroNessuna valutazione finora
- 21 Slide Pitch Deck Template: Quickly and Efficiently Showcase Your Business To InvestorsDocumento49 pagine21 Slide Pitch Deck Template: Quickly and Efficiently Showcase Your Business To InvestorsAleine Leilanie Oro100% (3)
- Gri 1-2Documento2 pagineGri 1-2Aleine Leilanie OroNessuna valutazione finora
- GRI Index 3Documento1 paginaGRI Index 3Aleine Leilanie OroNessuna valutazione finora
- Ebrd Aesr Template (2010) SWDocumento9 pagineEbrd Aesr Template (2010) SWAleine Leilanie OroNessuna valutazione finora
- Career Hunter Recruitment Solutions: Unit Ground Flr. Alfonso de Oro BLDG Brgy Malamig, Mandaluyong CityDocumento1 paginaCareer Hunter Recruitment Solutions: Unit Ground Flr. Alfonso de Oro BLDG Brgy Malamig, Mandaluyong CityAleine Leilanie OroNessuna valutazione finora
- Gerardo's CA Cafe: Buffet MenuDocumento2 pagineGerardo's CA Cafe: Buffet MenuAleine Leilanie OroNessuna valutazione finora
- Pagcor Registry LocalDocumento7 paginePagcor Registry LocalAleine Leilanie OroNessuna valutazione finora
- LAE PointersDocumento2 pagineLAE PointersAleine Leilanie Oro100% (2)
- HW: Procedure On How Ip'S Iccs Can Claim To Their Ancestral Land and AncestralDocumento1 paginaHW: Procedure On How Ip'S Iccs Can Claim To Their Ancestral Land and AncestralAleine Leilanie OroNessuna valutazione finora
- Art 448 Carrascoso JR Vs CA - 123672 - December 14, 2005 - JDocumento23 pagineArt 448 Carrascoso JR Vs CA - 123672 - December 14, 2005 - JAleine Leilanie OroNessuna valutazione finora
- The Writs: Oro, Aleine Leilanie BDocumento23 pagineThe Writs: Oro, Aleine Leilanie BAleine Leilanie OroNessuna valutazione finora
- Art 448 Geminiano Vs CADocumento4 pagineArt 448 Geminiano Vs CAAleine Leilanie OroNessuna valutazione finora
- Judicial Ethics - Revised SyllabusDocumento3 pagineJudicial Ethics - Revised SyllabusAleine Leilanie OroNessuna valutazione finora
- Zuellig PDFDocumento10 pagineZuellig PDFAleine Leilanie OroNessuna valutazione finora
- BOA Vs MeralcoDocumento4 pagineBOA Vs MeralcoAleine Leilanie OroNessuna valutazione finora
- 3 People Vs Puedan - 139576 - September 2, 2002 - JDocumento9 pagine3 People Vs Puedan - 139576 - September 2, 2002 - JAleine Leilanie OroNessuna valutazione finora
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Catalog en Eurocoustic 0Documento132 pagineCatalog en Eurocoustic 0Vikash KumarNessuna valutazione finora
- Material Safety Data Sheet Roto-Inject FluidDocumento5 pagineMaterial Safety Data Sheet Roto-Inject FluidQuintana JoseNessuna valutazione finora
- Punjab National BankDocumento4 paginePunjab National BankShubham RajNessuna valutazione finora
- Astm D 1142Documento11 pagineAstm D 1142yusria1982Nessuna valutazione finora
- Endovascular Skills CourseDocumento20 pagineEndovascular Skills CourseAbdullah JibawiNessuna valutazione finora
- Assessment 2 Vital Signs Normal ValuesDocumento4 pagineAssessment 2 Vital Signs Normal Valuesthannikkotte12345Nessuna valutazione finora
- Rotating Driver S Workstation and Rotating Cab: Reliable Solutions For More Ergonomic and Effective WorkingDocumento12 pagineRotating Driver S Workstation and Rotating Cab: Reliable Solutions For More Ergonomic and Effective WorkingEduardo CapeletiNessuna valutazione finora
- Automobile Air Conditioning SystemDocumento8 pagineAutomobile Air Conditioning SystemAyyan Gaonkhadkar100% (1)
- Leoline Installation and MaintenanceDocumento8 pagineLeoline Installation and MaintenanceFloorkitNessuna valutazione finora
- AE Board Review Part3 - MSWord2003 Long Paper 2011Documento12 pagineAE Board Review Part3 - MSWord2003 Long Paper 2011Jan14Nessuna valutazione finora
- Comparative Study of DEA and MDEADocumento4 pagineComparative Study of DEA and MDEAsaleh4060Nessuna valutazione finora
- La Paz National High SchoolDocumento19 pagineLa Paz National High SchoolBon Ivan FirmezaNessuna valutazione finora
- Quorum Sensing PDFDocumento9 pagineQuorum Sensing PDFShareenMuneebNessuna valutazione finora
- References: ProblemsDocumento14 pagineReferences: ProblemsDiego AlejandroNessuna valutazione finora
- Standardization 1 PDFDocumento7 pagineStandardization 1 PDFmazharul HasanNessuna valutazione finora
- How Hydraulic Valve Lifters WorkDocumento1 paginaHow Hydraulic Valve Lifters WorkSanket Sabale100% (1)
- Jokes and Their Relation To The Unconscious: Laurence HenkelmanDocumento3 pagineJokes and Their Relation To The Unconscious: Laurence HenkelmanMilos VisnjicNessuna valutazione finora
- 2016 Specimen Paper 1 PDFDocumento16 pagine2016 Specimen Paper 1 PDFBioScMentor-1Nessuna valutazione finora
- FMDS0289 Pipe Friction LossDocumento64 pagineFMDS0289 Pipe Friction Lossdaniela hritucNessuna valutazione finora
- Preparation of Stick Type Solid Glue As Paper AdheDocumento9 paginePreparation of Stick Type Solid Glue As Paper AdheAhmad AlShahrourNessuna valutazione finora
- Lesson 3.3 Inside An AtomDocumento42 pagineLesson 3.3 Inside An AtomReign CallosNessuna valutazione finora
- Jurnal Aquaponik Jada BahrinDocumento36 pagineJurnal Aquaponik Jada BahrinbrentozNessuna valutazione finora
- Vocabulary June v22Documento2 pagineVocabulary June v22Wiston TonwisNessuna valutazione finora
- ISKCON Desire Tree - Brahma Vimohana LeelaDocumento34 pagineISKCON Desire Tree - Brahma Vimohana LeelaISKCON desire treeNessuna valutazione finora
- Summary (Adjuncts)Documento2 pagineSummary (Adjuncts)Ngọc MinhNessuna valutazione finora
- 10.4324 9781315717289 PreviewpdfDocumento179 pagine10.4324 9781315717289 PreviewpdfMahdi GargouriNessuna valutazione finora
- Leader Ship Assessment: Student No 374212036Documento4 pagineLeader Ship Assessment: Student No 374212036Emily KimNessuna valutazione finora
- Good Boys Go To Heaven, Bad Boys Go EverywhereDocumento32 pagineGood Boys Go To Heaven, Bad Boys Go Everywherealcantaravic2006Nessuna valutazione finora
- What Is Primary Health Care and Its Relation To Universal Health Care? As A Medical Student, What Impact Can I Create in Implementing PHC and UHC?Documento2 pagineWhat Is Primary Health Care and Its Relation To Universal Health Care? As A Medical Student, What Impact Can I Create in Implementing PHC and UHC?Aubrey Unique EvangelistaNessuna valutazione finora
- The Jewish Way in Death and MourningDocumento67 pagineThe Jewish Way in Death and Mourningizzy212100% (1)