Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
EBOLA
Caricato da
wawa3385Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
EBOLA
Caricato da
wawa3385Copyright:
Formati disponibili
EBOLA
Ebola first appeared in 1976 in 2 simultaneous outbreaks, in Nzara, Sudan, and in Yambuku, Democratic
Republic of Congo. The latter was in a village situated near the Ebola River, from which the disease takes its
name.
Genus Ebolavirus is 1 of 3 members of the Filoviridae family (filovirus), along with genus Marburgvirus
and genus Cuevavirus. Genus Ebolavirus comprises 5 distinct species:
1. Bundibugyo ebolavirus (BDBV)
2. Zaire ebolavirus (EBOV)
3. Reston ebolavirus (RESTV)
4. Sudan ebolavirus (SUDV)
5. Ta Forest ebolavirus (TAFV).
BDBV, EBOV, and SUDV have been associated with large EVD outbreaks in Africa, whereas RESTV and
TAFV have not. The RESTV species, found in Philippines and the Peoples Republic of China, can infect
humans, but no illness or death in humans from this species has been reported to date.
Transmission
Ebola is introduced into the human population through close contact with the blood, secretions, organs or
other bodily fluids of infected animals. In Africa, infection has been documented through the handling of
infected chimpanzees, gorillas, fruit bats, monkeys, forest antelope and porcupines found ill or dead or in the
rainforest.
Ebola then spreads in the community through human-to-human transmission, with infection resulting from
direct contact (through broken skin or mucous membranes) with the blood, secretions, organs or other bodily
fluids of infected people, and indirect contact with environments contaminated with such fluids. Burial
ceremonies in which mourners have direct contact with the body of the deceased person can also play a role
in the transmission of Ebola. Men who have recovered from the disease can still transmit the virus through
their semen for up to 7 weeks after recovery from illness.
Health-care workers have frequently been infected while treating patients with suspected or confirmed EVD.
This has occurred through close contact with patients when infection control precautions are not strictly
practiced.
Among workers in contact with monkeys or pigs infected with Reston ebolavirus, several infections have
been documented in people who were clinically asymptomatic. Thus, RESTV appears less capable of
causing disease in humans than other Ebola species.
However, the only available evidence available comes from healthy adult males. It would be premature to
extrapolate the health effects of the virus to all population groups, such as immuno-compromised persons,
persons with underlying medical conditions, pregnant women and children. More studies of RESTV are
needed before definitive conclusions can be drawn about the pathogenicity and virulence of this virus in
humans.
Signs and symptoms
EVD is a severe acute viral illness often characterized by the sudden onset of fever, intense weakness,
muscle pain, headache and sore throat. This is followed by vomiting, diarrhoea, rash, impaired kidney and
liver function, and in some cases, both internal and external bleeding. Laboratory findings include low white
blood cell and platelet counts and elevated liver enzymes.
People are infectious as long as their blood and secretions contain the virus. Ebola virus was isolated from
semen 61 days after onset of illness in a man who was infected in a laboratory.
The incubation period, that is, the time interval from infection with the virus to onset of symptoms, is 2 to 21
days.
Diagnosis
Other diseases that should be ruled out before a diagnosis of EVD can be made include: malaria, typhoid
fever, shigellosis, cholera, leptospirosis, plague, rickettsiosis, relapsing fever, meningitis, hepatitis and other
viral haemorrhagic fevers.
Ebola virus infections can be diagnosed definitively in a laboratory through several types of tests:
antibody-capture enzyme-linked immunosorbent assay (ELISA)
antigen detection tests
serum neutralization test
reverse transcriptase polymerase chain reaction (RT-PCR) assay
electron microscopy
virus isolation by cell culture.
Samples from patients are an extreme biohazard risk; testing should be conducted under maximum
biological containment conditions.
Vaccine and treatment
No licensed vaccine for EVD is available. Several vaccines are being tested, but none are available for
clinical use.
Severely ill patients require intensive supportive care. Patients are frequently dehydrated and require oral
rehydration with solutions containing electrolytes or intravenous fluids.
No specific treatment is available. New drug therapies are being evaluated.
Natural host of Ebola virus
In Africa, fruit bats, particularly species of the genera Hypsignathus monstrosus, Epomops
franqueti and Myonycteris torquata, are considered possible natural hosts for Ebola virus. As a result, the
geographic distribution of Ebolaviruses may overlap with the range of the fruit bats.
Ebola virus in animals
Although non-human primates have been a source of infection for humans, they are not thought to be the
reservoir but rather an accidental host like human beings. Since 1994, Ebola outbreaks from the EBOV and
TAFV species have been observed in chimpanzees and gorillas.
RESTV has caused severe EVD outbreaks in macaque monkeys (Macaca fascicularis) farmed in Philippines
and detected in monkeys imported into the USA in 1989, 1990 and 1996, and in monkeys imported to Italy
from Philippines in 1992.
Since 2008, RESTV viruses have been detected during several outbreaks of a deadly disease in pigs in
Peoples Republic of China and Philippines. Asymptomatic infection in pigs has been reported and
experimental inoculations have shown that RESTV cannot cause disease in pigs.
Prevention and control
Controlling Reston ebolavirus in domestic animals
No animal vaccine against RESTV is available. Routine cleaning and disinfection of pig or monkey farms
(with sodium hypochlorite or other detergents) should be effective in inactivating the virus.
If an outbreak is suspected, the premises should be quarantined immediately. Culling of infected animals,
with close supervision of burial or incineration of carcasses, may be necessary to reduce the risk of animal-
to-human transmission. Restricting or banning the movement of animals from infected farms to other areas
can reduce the spread of the disease.
As RESTV outbreaks in pigs and monkeys have preceded human infections, the establishment of an active
animal health surveillance system to detect new cases is essential in providing early warning for veterinary
and human public health authorities.
Reducing the risk of Ebola infection in people
In the absence of effective treatment and a human vaccine, raising awareness of the risk factors for Ebola
infection and the protective measures individuals can take is the only way to reduce human infection and
death.
In Africa, during EVD outbreaks, educational public health messages for risk reduction should focus on
several factors:
Reducing the risk of wildlife-to-human transmission from contact with infected fruit bats or monkeys/apes
and the consumption of their raw meat. Animals should be handled with gloves and other appropriate
protective clothing. Animal products (blood and meat) should be thoroughly cooked before consumption.
Reducing the risk of human-to-human transmission in the community arising from direct or close contact
with infected patients, particularly with their bodily fluids. Close physical contact with Ebola patients should
be avoided. Gloves and appropriate personal protective equipment should be worn when taking care of ill
patients at home. Regular hand washing is required after visiting patients in hospital, as well as after taking
care of patients at home.
Communities affected by Ebola should inform the population about the nature of the disease and about
outbreak containment measures, including burial of the dead. People who have died from Ebola should be
promptly and safely buried.
Pig farms in Africa can play a role in the amplification of infection because of the presence of fruit bats on
these farms. Appropriate biosecurity measures should be in place to limit transmission. For RESTV,
educational public health messages should focus on reducing the risk of pig-to-human transmission as a
result of unsafe animal husbandry and slaughtering practices, and unsafe consumption of fresh blood, raw
milk or animal tissue. Gloves and other appropriate protective clothing should be worn when handling sick
animals or their tissues and when slaughtering animals. In regions where RESTV has been reported in pigs,
all animal products (blood, meat and milk) should be thoroughly cooked before eating.
Controlling infection in health-care settings
Human-to-human transmission of the Ebola virus is primarily associated with direct or indirect contact with
blood and body fluids. Transmission to health-care workers has been reported when appropriate infection
control measures have not been observed.
It is not always possible to identify patients with EBV early because initial symptoms may be non-specific.
For this reason, it is important that health-care workers apply standard precautions consistently with all
patients regardless of their diagnosis in all work practices at all times. These include basic hand hygiene,
respiratory hygiene, the use of personal protective equipment (according to the risk of splashes or other
contact with infected materials), safe injection practices and safe burial practices.
Health-care workers caring for patients with suspected or confirmed Ebola virus should apply, in addition to
standard precautions, other infection control measures to avoid any exposure to the patients blood and body
fluids and direct unprotected contact with the possibly contaminated environment. When in close contact
(within 1 metre) of patients with EBV, health-care workers should wear face protection (a face shield or a
medical mask and goggles), a clean, non-sterile long-sleeved gown, and gloves (sterile gloves for some
procedures).
Laboratory workers are also at risk. Samples taken from suspected human and animal Ebola cases for
diagnosis should be handled by trained staff and processed in suitably equipped laboratories.
WHO response
WHO provides expertise and documentation to support disease investigation and control.
Recommendations for infection control while providing care to patients with suspected or confirmed Ebola
haemorrhagic fever are provided in: Interim infection control recommendations for care of patients with
suspected or confirmed Filovirus (Ebola, Marburg) haemorrhagic fever, March 2008. This document is
currently being updated.
WHO has created an aidememoire on standard precautions in health care (currently being updated).
Standard precautions are meant to reduce the risk of transmission of bloodborne and other pathogens. If
universally applied, the precautions would help prevent most transmission through exposure to blood and
body fluids.
Standard precautions are recommended in the care and treatment of all patients regardless of their perceived
or confirmed infectious status. They include the basic level of infection controlhand hygiene, use of
personal protective equipment to avoid direct contact with blood and body fluids, prevention of needle stick
and injuries from other sharp instruments, and a set of environmental controls.
Table: Chronology of previous Ebola virus disease outbreaks
Year Country
Ebolavirus
species Cases Deaths
Case
fatality
Year Country
Ebolavirus
species Cases Deaths
Case
fatality
2012
Democratic Republic of
Congo Bundibugyo 57 29 51%
2012 Uganda Sudan 7 4 57%
2012 Uganda Sudan 24 17 71%
2011 Uganda Sudan 1 1 100%
2008
Democratic Republic of
Congo Zaire 32 14 44%
2007 Uganda Bundibugyo 149 37 25%
2007
Democratic Republic of
Congo Zaire 264 187 71%
2005 Congo Zaire 12 10 83%
2004 Sudan Sudan 17 7 41%
2003 (Nov-
Dec) Congo Zaire 35 29 83%
2003 (Jan-
Apr) Congo Zaire 143 128 90%
2001-2002 Congo Zaire 59 44 75%
2001-2002 Gabon Zaire 65 53 82%
2000 Uganda Sudan 425 224 53%
1996 South Africa (ex-Gabon) Zaire 1 1 100%
1996 (Jul-
Dec) Gabon Zaire 60 45 75%
1996 (Jan-
Apr) Gabon Zaire 31 21 68%
1995
Democratic Republic of
Congo Zaire 315 254 81%
1994 Cote d'Ivoire Ta Forest 1 0 0%
1994 Gabon Zaire 52 31 60%
1979 Sudan Sudan 34 22 65%
1977
Democratic Republic of
Congo Zaire 1 1 100%
1976 Sudan Sudan 284 151 53%
1976
Democratic Republic of
Congo Zaire 318 280 88%
Potrebbero piacerti anche
- Pneumonia Definations & ClassificationsDocumento29 paginePneumonia Definations & ClassificationsJimitNessuna valutazione finora
- A Preschool-Based Intervention For Early ChildhoodDocumento9 pagineA Preschool-Based Intervention For Early Childhoodmohammed MusaNessuna valutazione finora
- Chickenpox What Is Chickenpox?Documento19 pagineChickenpox What Is Chickenpox?s.khan9211rediffmail.comNessuna valutazione finora
- 15.somatization DisorderDocumento13 pagine15.somatization DisorderGERSON RYANTONessuna valutazione finora
- AntraxDocumento17 pagineAntraxEdwin VazquezNessuna valutazione finora
- Communicable Disease Review MaterialDocumento43 pagineCommunicable Disease Review Materialrceponelas1127Nessuna valutazione finora
- Individual Aging Vs Population AgingDocumento74 pagineIndividual Aging Vs Population AgingAnthony RiggsNessuna valutazione finora
- 03 Unit .Self Concept and Self PerceptionDocumento27 pagine03 Unit .Self Concept and Self PerceptionIrfan Ali JunejoNessuna valutazione finora
- Types of PneumoniaDocumento6 pagineTypes of PneumoniasakuraleeshaoranNessuna valutazione finora
- AdulthoodDocumento5 pagineAdulthoodSherwin Purisima TaguesaNessuna valutazione finora
- Introduction To PharmacologyDocumento2 pagineIntroduction To PharmacologyAdri Sinclaire100% (1)
- Obsessive-Compulsive and Related DisordersDocumento16 pagineObsessive-Compulsive and Related DisordersJoanNessuna valutazione finora
- Management of Tuberculosis: A guide for clinicians (eBook edition)Da EverandManagement of Tuberculosis: A guide for clinicians (eBook edition)Nessuna valutazione finora
- TRICHOMONIASISDocumento39 pagineTRICHOMONIASISAlunaficha Melody KiraniaNessuna valutazione finora
- Communicable DiseaseDocumento193 pagineCommunicable DiseaseLuvastranger Auger100% (2)
- EbolaDocumento3 pagineEbolaskrameer100% (1)
- Management of Patients With Neurologic DysfunctionDocumento24 pagineManagement of Patients With Neurologic DysfunctionYahya AL-HelihNessuna valutazione finora
- Cardiopulmonary Resuscitation: College of Nursing Madras Medical CollegeDocumento48 pagineCardiopulmonary Resuscitation: College of Nursing Madras Medical CollegeNithin ManlyNessuna valutazione finora
- Urinary CatheterDocumento4 pagineUrinary CatheterBindu SinghNessuna valutazione finora
- K44 - Nutrition During LactationDocumento26 pagineK44 - Nutrition During Lactationbilli lisanuddinNessuna valutazione finora
- Knowledge, Attitude, and Practices Towards The COVID-19 Pandemic Among Undergraduate StudentsDocumento7 pagineKnowledge, Attitude, and Practices Towards The COVID-19 Pandemic Among Undergraduate StudentsLulu RakhmillaNessuna valutazione finora
- A Study of the Lack of Hiv/Aids Awareness Among African American Women: a Leadership Perspective: Awareness That All Cultures Should Know AboutDa EverandA Study of the Lack of Hiv/Aids Awareness Among African American Women: a Leadership Perspective: Awareness That All Cultures Should Know AboutValutazione: 5 su 5 stelle5/5 (1)
- Layers of The SkinDocumento49 pagineLayers of The SkinBakri MustafaNessuna valutazione finora
- Chloride Deficit LecDocumento2 pagineChloride Deficit Leced123edNessuna valutazione finora
- Assessment of Digestive and Gastrointestinal FunctionDocumento19 pagineAssessment of Digestive and Gastrointestinal FunctionMarichelle Vicente- Delos SantosNessuna valutazione finora
- Burns Rule of Nines 2013Documento1 paginaBurns Rule of Nines 2013ellenningrumNessuna valutazione finora
- Pain Assessment & MGTDocumento16 paginePain Assessment & MGTSitti Mardiya SariolNessuna valutazione finora
- Reproductive Tract InfectionDocumento48 pagineReproductive Tract InfectionSampriti Roy100% (1)
- Dynamics of Disease Transmission: Presented by - Varughese SamDocumento18 pagineDynamics of Disease Transmission: Presented by - Varughese SamVinu Varughese Sam ChemmangattilNessuna valutazione finora
- Dynamics of Disease TransmissionDocumento30 pagineDynamics of Disease TransmissionSyed Sanan shahNessuna valutazione finora
- Screening For DiseaseDocumento29 pagineScreening For DiseaseSrinidhi Nandhini Pandian100% (2)
- Assessment and Management of Patients With Biliary DisorderDocumento50 pagineAssessment and Management of Patients With Biliary DisorderZanida ZainonNessuna valutazione finora
- Nutrition For Preschoolers (NTLC) WordDocumento6 pagineNutrition For Preschoolers (NTLC) WordKeerthana VNessuna valutazione finora
- Concept of Family Nursing Process Part 1Documento14 pagineConcept of Family Nursing Process Part 1Fatima Ysabelle Marie RuizNessuna valutazione finora
- Measles: PGI Nicole Jenne C. TanDocumento40 pagineMeasles: PGI Nicole Jenne C. TanNicole Jenne TanNessuna valutazione finora
- Trichomonas Vaginalis (FINAL)Documento31 pagineTrichomonas Vaginalis (FINAL)Veigner Whyng Cabugayan100% (1)
- Japanese Encephalitis by RobelDocumento2 pagineJapanese Encephalitis by RobelRobel_Saoi_2309Nessuna valutazione finora
- Nasopharyngeal Airway SuctioningDocumento3 pagineNasopharyngeal Airway SuctioningHaitham ZraigatNessuna valutazione finora
- Non Communicable DiseaseDocumento13 pagineNon Communicable DiseaseClancy Anne Garcia Naval100% (1)
- Count, Rate, Ratio, ProportionDocumento51 pagineCount, Rate, Ratio, Proportionprasanna lamaNessuna valutazione finora
- Clinical Case 04 2019Documento12 pagineClinical Case 04 2019Erica Veluz LuyunNessuna valutazione finora
- Food PoisoningDocumento19 pagineFood PoisoningHemanathan PraemNessuna valutazione finora
- AEFIDocumento24 pagineAEFIadiNessuna valutazione finora
- Effectiveness of Structured Teaching Programme On Knowledge Regarding Prevention of Road Traffic Accidents Among Adolescents 13 18 Years in Selected Schools of Baramulla KashmirDocumento4 pagineEffectiveness of Structured Teaching Programme On Knowledge Regarding Prevention of Road Traffic Accidents Among Adolescents 13 18 Years in Selected Schools of Baramulla KashmirIJARP PublicationsNessuna valutazione finora
- The Role of Nurses in Diabetes Care and EducationDocumento16 pagineThe Role of Nurses in Diabetes Care and EducationMakanjuola Osuolale JohnNessuna valutazione finora
- CHAPTER TWO Communicable DssDocumento36 pagineCHAPTER TWO Communicable DssAyro Business CenterNessuna valutazione finora
- CD Summer Review 1Documento157 pagineCD Summer Review 1Nikko MelencionNessuna valutazione finora
- An Interventional Study To Evaluate The Effectiveness of Selected Nutritional Diet On Growth of Pre Schooler at Selected Slums Area of Bhopal M.PDocumento6 pagineAn Interventional Study To Evaluate The Effectiveness of Selected Nutritional Diet On Growth of Pre Schooler at Selected Slums Area of Bhopal M.PEditor IJTSRDNessuna valutazione finora
- Clinical Guidelines (Nursing) - Indwelling Urinary Catheter - Insertion and Ongoing CareDocumento8 pagineClinical Guidelines (Nursing) - Indwelling Urinary Catheter - Insertion and Ongoing CareLeeNessuna valutazione finora
- Dr. Sanjeev GuptaDocumento73 pagineDr. Sanjeev Guptadrsanjeev15Nessuna valutazione finora
- Communicable DiseasesDocumento24 pagineCommunicable DiseasesJanus de LeonNessuna valutazione finora
- Dynamic of DiseaseDocumento8 pagineDynamic of Diseaseachuth29Nessuna valutazione finora
- Japan Gifts GivingDocumento3 pagineJapan Gifts GivingRehan PervaizNessuna valutazione finora
- Drug Resistant TuberculosisDocumento58 pagineDrug Resistant TuberculosisbharatnarayananNessuna valutazione finora
- Concept of Health Disease and PreventionDocumento33 pagineConcept of Health Disease and PreventionitdocNessuna valutazione finora
- Epidemiology 1st PracticalDocumento22 pagineEpidemiology 1st Practicalmichal ben meronNessuna valutazione finora
- NCDDocumento120 pagineNCDBEISAL BABY PNessuna valutazione finora
- ANP Seminar IECDocumento8 pagineANP Seminar IECGinoNessuna valutazione finora
- Personal Data of Patient: Intensive Nursing Practicum - Pediatric Ward (BMC) CASE STUDY 5: Pediatric OncologyDocumento12 paginePersonal Data of Patient: Intensive Nursing Practicum - Pediatric Ward (BMC) CASE STUDY 5: Pediatric OncologyromelynNessuna valutazione finora
- Primary Health Care Maternal & Child HealthDocumento32 paginePrimary Health Care Maternal & Child HealthAbidah Rahmi HilmyNessuna valutazione finora
- TraksiDocumento5 pagineTraksiwawa3385Nessuna valutazione finora
- NeurovascularDocumento10 pagineNeurovascularwawa3385Nessuna valutazione finora
- ReductionDocumento63 pagineReductionwawa3385Nessuna valutazione finora
- Hypertensive RetinopathyDocumento5 pagineHypertensive Retinopathywawa3385Nessuna valutazione finora
- Pneumothorax SXDocumento1 paginaPneumothorax SXwawa3385Nessuna valutazione finora
- NeurovascularDocumento10 pagineNeurovascularwawa3385Nessuna valutazione finora
- Start TriageDocumento12 pagineStart Triagewawa3385Nessuna valutazione finora
- PnemothoraxDocumento1 paginaPnemothoraxwawa3385Nessuna valutazione finora
- Anemia SymptomsDocumento1 paginaAnemia Symptomswawa3385Nessuna valutazione finora
- Causes of AnemiaDocumento2 pagineCauses of Anemiawawa3385Nessuna valutazione finora
- PediculosisDocumento1 paginaPediculosiswawa3385Nessuna valutazione finora
- AnemiaDocumento1 paginaAnemiawawa3385Nessuna valutazione finora
- Anemia: NIH: National Heart, Lung, and Blood InstituteDocumento1 paginaAnemia: NIH: National Heart, Lung, and Blood Institutewawa3385Nessuna valutazione finora
- CDC Ebola Fact SheetDocumento13 pagineCDC Ebola Fact Sheetيوسف سيمنزNessuna valutazione finora
- UrethritisDocumento2 pagineUrethritiswawa3385Nessuna valutazione finora
- Pregnancy - Antenatal Checks of Your Baby: Baby in Vertex - or 'Head' Down PositionDocumento4 paginePregnancy - Antenatal Checks of Your Baby: Baby in Vertex - or 'Head' Down Positionwawa3385Nessuna valutazione finora
- 1 - NICE Guidelines - FullDocumento393 pagine1 - NICE Guidelines - FullangiemerazNessuna valutazione finora
- Hypertensive RetinopathyDocumento5 pagineHypertensive Retinopathywawa3385Nessuna valutazione finora
- Normal Puerperium PDFDocumento22 pagineNormal Puerperium PDFwawa3385100% (1)
- CnoDocumento24 pagineCnotherealoneandonlyoneNessuna valutazione finora
- Addressing Patients' Emotional and Spiritual Needs: Patient CenterednessDocumento12 pagineAddressing Patients' Emotional and Spiritual Needs: Patient Centerednesswawa3385Nessuna valutazione finora
- BookDocumento34 pagineBookwawa33850% (1)
- CnoDocumento24 pagineCnotherealoneandonlyoneNessuna valutazione finora
- Makerere University Is Inviting Applications For Undergraduate Admissions On Private Sponsorship For Academic Year 2015/2016Documento9 pagineMakerere University Is Inviting Applications For Undergraduate Admissions On Private Sponsorship For Academic Year 2015/2016The Campus TimesNessuna valutazione finora
- Islcollective Present SimpleDocumento2 pagineIslcollective Present Simplecrisan mirunaNessuna valutazione finora
- GT I9100g Service SchematicsDocumento8 pagineGT I9100g Service SchematicsMassolo RoyNessuna valutazione finora
- 3.2.1 The Role of Market Research and Methods UsedDocumento42 pagine3.2.1 The Role of Market Research and Methods Usedsana jaleelNessuna valutazione finora
- The Global Entrepreneurship and Development Index 2014 For Web1 PDFDocumento249 pagineThe Global Entrepreneurship and Development Index 2014 For Web1 PDFAlex Yuri Rodriguez100% (1)
- Bai Tap Av 12 Thi Diem Unit TwoDocumento7 pagineBai Tap Av 12 Thi Diem Unit TwonguyenngocquynhchiNessuna valutazione finora
- Model Contract FreelanceDocumento3 pagineModel Contract FreelancemarcosfreyervinnorskNessuna valutazione finora
- Cash Budget Sharpe Corporation S Projected Sales First 8 Month oDocumento1 paginaCash Budget Sharpe Corporation S Projected Sales First 8 Month oAmit PandeyNessuna valutazione finora
- 3 A Sanitary Standards Quick Reference GuideDocumento98 pagine3 A Sanitary Standards Quick Reference GuideLorettaMayNessuna valutazione finora
- The Fluency Course Teacher Instructions PDFDocumento9 pagineThe Fluency Course Teacher Instructions PDFGabriel da RochaNessuna valutazione finora
- El TontoDocumento92 pagineEl TontoRobertNessuna valutazione finora
- Choosing An Effective Visual ToolDocumento9 pagineChoosing An Effective Visual ToolAdil Bin KhalidNessuna valutazione finora
- Zkp8006 Posperu Inc SacDocumento2 pagineZkp8006 Posperu Inc SacANDREA BRUNO SOLANONessuna valutazione finora
- Cutler Hammer Dry Type TransformerDocumento220 pagineCutler Hammer Dry Type TransformernprajanNessuna valutazione finora
- Catalogo HydronixDocumento68 pagineCatalogo HydronixNANCHO77Nessuna valutazione finora
- De On Tap So 4-6Documento8 pagineDe On Tap So 4-6Quy DoNessuna valutazione finora
- CCNP SWITCH 300-115 - Outline of The Official Study GuideDocumento31 pagineCCNP SWITCH 300-115 - Outline of The Official Study GuidehammiesinkNessuna valutazione finora
- CCTV Guidelines - Commission Letter Dated 27.08.2022Documento2 pagineCCTV Guidelines - Commission Letter Dated 27.08.2022Sumeet TripathiNessuna valutazione finora
- Operation of A CRT MonitorDocumento8 pagineOperation of A CRT MonitorHarry W. HadelichNessuna valutazione finora
- Drawbot 1Documento4 pagineDrawbot 1SayanSanyalNessuna valutazione finora
- Onco Case StudyDocumento2 pagineOnco Case StudyAllenNessuna valutazione finora
- Portfolio AdityaDocumento26 paginePortfolio AdityaAditya DisNessuna valutazione finora
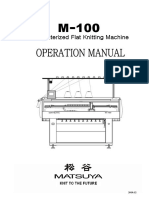
- Computerized Flat Knitting Machine Computerized Flat Knitting Machine Computerized Flat Knitting Machine Computerized Flat Knitting MachineDocumento61 pagineComputerized Flat Knitting Machine Computerized Flat Knitting Machine Computerized Flat Knitting Machine Computerized Flat Knitting MachineAmira's ClothesNessuna valutazione finora
- Sample Valuation ReportDocumento15 pagineSample Valuation Reportayush singlaNessuna valutazione finora
- BBO2020Documento41 pagineBBO2020qiuNessuna valutazione finora
- Catalogue Laboratory Products - Heraeus KulzerDocumento288 pagineCatalogue Laboratory Products - Heraeus KulzerDentaDentNessuna valutazione finora
- Things You Can Do at Burnham ParkDocumento2 pagineThings You Can Do at Burnham ParkBcpo TeuNessuna valutazione finora
- QuerySurge Models Mappings DocumentDocumento28 pagineQuerySurge Models Mappings Documentchiranjeev mishra100% (1)
- Book Review Fiction New HereDocumento7 pagineBook Review Fiction New HereFILZAH SYAUQINA BINTI SUBLY Pelajar KPTM IpohNessuna valutazione finora
- Firing OrderDocumento5 pagineFiring OrderCurtler PaquibotNessuna valutazione finora