Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Tethered Spinal Cord Syndrome Is A Neurological Disorder Caused by Tissue Attachments That Limit The Movement of The Spinal Cord Within The Spinal Column
Caricato da
SitaTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Tethered Spinal Cord Syndrome Is A Neurological Disorder Caused by Tissue Attachments That Limit The Movement of The Spinal Cord Within The Spinal Column
Caricato da
SitaCopyright:
Formati disponibili
Tethered spinal cord syndrome is a neurological disorder caused by tissue attachments that
limit the movement of the spinal cord within the spinal column. Attachments may occur
congenitally at the base of the spinal cord (conus medullaris) or they may develop near the
site of an injury to the spinal cord. These attachments cause an abnormal stretching of the
spinal cord. The course of the disorder is progressive. In children, symptoms may include
lesions, hairy patches, dimples, or fatty tumors on the lower back; foot and spinal
deformities; weakness in the legs; low back pain; scoliosis; and incontinence. This type of
tethered spinal cord syndrome appears to be the result of improper growth of the neural tube
during fetal development, and is closely linked to spina bifida. Tethered spinal cord
syndrome may go undiagnosed until adulthood, when pain, sensory and motor problems, and
loss of bowel and bladder control emerge. This delayed presentation of symptoms is related
to the degree of strain placed on the spinal cord over time and may be exacerbated during
sports or pregnancy, or may be due to narrowing of the spinal column (stenosis) with age.
Tethering may also develop after spinal cord injury and scar tissue can block the flow of
fluids around the spinal cord. Fluid pressure may cause cysts to form in the spinal cord, a
condition called syringomyelia. This can lead to additional loss of movement, feeling or the
onset of pain or autonomic symptoms.
Is there any treatment?
MRI imaging is often used to evaluate individuals with these symptoms, and can be used to
diagnose the location of the tethering, lower than normal position of the conus medullaris, or
presence of a tumor or fatty mass (lipoma). In children, early surgery is recommended to
prevent further neurological deterioration. Regular follow-up is important: retethering may
occur in some individuals during periods of rapid growth and may be seen between five to
nine years of age. If surgery is not advisable, spinal cord nerve roots may be cut to relieve
pain. In adults, surgery to free (detether) the spinal cord can reduce the size and further
development of cysts in the cord and may restore some function or alleviate other symptoms.
Other treatment is symptomatic and supportive.
What is the prognosis?
With treatment, individuals with tethered spinal cord syndrome have a normal life
expectancy. However, some neurological and motor impairments may not be fully
correctable. Surgery soon after symptoms emerge appears to improve chances for recovery
and can prevent further functional decline.
What research is being done?
The NINDS conducts and supports research on disorders of the spinal cord. The goals of this
research are to find ways to prevent, treat, and cure these disorders.
Sindrom sumsum tulang belakang ditambatkan adalah gangguan neurologis yang disebabkan oleh
lampiran jaringan yang membatasi pergerakan dari sumsum tulang belakang dalam kolom tulang
belakang . Lampiran dapat terjadi kongenital di dasar sumsum tulang belakang ( konus medularis )
atau mereka dapat mengembangkan dekat lokasi cedera sumsum tulang belakang . Lampiran ini
menyebabkan abnormal peregangan dari sumsum tulang belakang . Jalannya gangguan yang
progresif . Pada anak-anak , gejala mungkin termasuk lesi , patch berbulu , lesung , atau tumor lemak
pada punggung bawah , kaki dan deformitas tulang belakang , kelemahan di kaki , nyeri pinggang ,
scoliosis , dan inkontinensia . Jenis sindrom sumsum tulang belakang ditambatkan tampaknya
merupakan hasil dari pertumbuhan yang tidak benar dari tabung saraf selama perkembangan janin ,
dan berhubungan erat dengan spina bifida . Sindrom sumsum tulang belakang ditambatkan mungkin
tidak terdiagnosis sampai dewasa , ketika rasa sakit , masalah sensorik dan motorik , dan hilangnya
kontrol usus dan kandung kemih muncul . Ini presentasi tertunda gejala berkaitan dengan tingkat
ketegangan ditempatkan pada sumsum tulang belakang dari waktu ke waktu dan dapat diperburuk
selama olahraga atau kehamilan , atau mungkin karena penyempitan tulang belakang ( stenosis )
dengan usia . Tethering juga dapat berkembang setelah cedera tulang belakang dan jaringan parut
bisa menghalangi aliran cairan di sekitar sumsum tulang belakang . Tekanan fluida dapat
menyebabkan kista terbentuk di sumsum tulang belakang , suatu kondisi yang disebut syringomyelia
. Hal ini dapat mengakibatkan kerugian tambahan gerakan , perasaan atau timbulnya rasa sakit atau
gejala otonom.
Apakah ada pengobatan ?
Pencitraan MRI sering digunakan untuk mengevaluasi individu dengan gejala ini , dan dapat
digunakan untuk mendiagnosa lokasi tethering , lebih rendah dari posisi normal dari konus medularis
, atau adanya tumor atau massa lemak ( lipoma ) . Pada anak-anak , bedah awal dianjurkan untuk
mencegah kerusakan neurologis lanjut . Regular tindak lanjut adalah penting : retethering dapat
terjadi pada beberapa individu selama periode pertumbuhan yang cepat dan dapat dilihat antara 5-9
tahun . Jika operasi ini tidak dianjurkan , akar saraf sumsum tulang belakang dapat dipotong untuk
menghilangkan rasa sakit . Pada orang dewasa , operasi untuk gratis ( detether ) sumsum tulang
belakang dapat mengurangi ukuran dan pengembangan lebih lanjut dari kista di kabel dan dapat
mengembalikan beberapa fungsi atau meringankan gejala lainnya . Pengobatan lainnya adalah
simtomatik dan suportif .
Apa prognosis ?
Dengan pengobatan , individu dengan sindrom sumsum tulang belakang ditambatkan memiliki
harapan hidup normal. Namun, beberapa gangguan neurologis dan motorik mungkin tidak
sepenuhnya diperbaiki . Pembedahan segera setelah gejala muncul tampaknya meningkatkan
peluang untuk pemulihan dan dapat mencegah penurunan lebih lanjut fungsional .
Penelitian apa yang sedang dilakukan ?
The NINDS melakukan dan mendukung penelitian tentang gangguan sumsum tulang belakang .
Tujuan dari penelitian ini adalah untuk menemukan cara untuk mencegah , mengobati , dan
menyembuhkan gangguan ini .
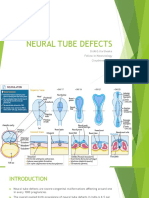
Introduction
When there is disturbed or incomplete closure of the neural tube during embryonic life it
leads to a developmental congenital defect called spina bifida (SB). Some of the vertebrae of
the spinal cord are not completely formed and remain open to produce a defect in the
vertebral column that may or may not be covered by the skin. The most common site of this
defect is the lumber or the sacral segment of the spinal cord. The incidence of SB is about
one in every 1000 births
1,2
.
Disorders associated with spina bifida
There are various disorders which are similar to SB or which may be associated with SB.
These disorders include:
Anencephaly
Encephalocele
Tethered Spinal Cord
Chiari Malformation
Meckel syndrome
Dandy-Walker-Malformation
1. Anencephaly
This disorder refers to the absence of a large portion of the brain or the skull. It is also termed
as aprosencephaly or with an open cranium. It is the neural defect that occurs when the
superior portion of neural the tube fails to close. The possible risk factors for this abnormality
include low folic acid level in pregnant mothers and exposure to certain toxins or drugs
during pregnancy. Its incidence is one in 10,000 births
3
.
Clinical features of anencephaly include:
Absence of the skull or a part with exposure of brain tissue
Absence of the brain or a portion
Facial abnormalities
Valvular defects of the heart
3
Diagnosis: The following tests can be carried out to diagnose this defect in a pregnant
mother:
Abdomenial ultrasonography
Amniocentesis
Alpha-fetoprotein level
Test of pre-pregnancy serum folate level
Urine estriol level
3
Treatment: There is no current therapy except genetic counseling.
Prognosis: The anomaly usually results in death within a few days of birth.
Prevention: Adequate folic acid intake may prevent this malformation from developing
3
.
2. Encephalocele
This is another of the neural tube defects which result from the incomplete closure of superior
part of the neural tube. Its other name is cranium bifidum. It sticks out of the skull through
openings in the form of protrusions of brain tissue with its covering membranes. It has many
similarities with spina bifida. It is a rare anomaly that occurs at a rate of one in 5000 live
births
4,5
.
Types: If the protruded part of encephalocele contains only CSF along with membranes, it
may be termed as meningocele and if the brain tissue also protrudes with it, it is called
encephalomeningocele. Encephaloceles include the following types
4
:
Naso-frontal
Naso-ethmoidal
Naso-orbital
Risk factors: Recent studies show an association of these congenital anomalies with the
following risk factors:
Exposure to cancer causing agents
Exposure to tryptan blue- a stain used to color dead tissues
Decreased level of folic acids
5
Clinical manifestations: Patients with this malformation can have following features:
Hydrocephalus
Weakness of lower limbs
An abnormally small sized head
Disturbed muscle movement
Developmental delay
Vision problems
Mental and growth retardation
Seizures
5
Meningitis, both pre-operative and post operative
Hydrocephalus
Blindness
6
Complications: These include:
Management: The following investigations are conducted with pregnant women to diagnose
this anomaly:
Ultrasonography of the abdomen
MRI
AFP-level
5,6
Reparative surgery is the treatment of choice at an early stage. Other treatment options are
supportive therapy, counseling, physical therapy, psychotherapy etc
5, 6
.
3. Tethered Cord Syndrome
This syndrome is characterized by pulling of the spinal cord at the base of the spinal canal
along with consequent clinical manifestations. It has many different forms like:
Dermiods
Dermal sinus tracts
Cystoceles
Tight filum terminale
Lipomenengiomyelocele
Split cord malformation
7
.
Aetiology: Causes of TCSinclude:
Disturbed growth of the neural tube during fetal development
Spina bifida
Later spinal cord injury
Syringomyelia
8
Clinical manifestations: Clinical manifestations of this anomaly include:
Skin lesions like hairy patches, dimples, or fatty tumors on the lower back
Paralysis of both lower limbs
Spine and feet deformities
Kyphoysis and scoliosis
Backache
Urinary incontinence
Urinary retention
Weakness of muscle and loss of sensations of touch, vibration, temperature, pain and
proprioception
Urinary frequency, urgency, feeling of incomplete urination
Rectal prolapse
Constipation
Bowel control dysfunction
Motor neuron findings like amyotrophy, hypereflexia and up-going planter
Chronic recurrent kidney infections and stones
9, 10
Treatment: Treatment options include:
Untethering by surgery
NSAIDS and opiates to relieve the pain
Antidepressants for severe pain
Muscle relaxing exercises
Treatment of urinary tract infection
Physiotherapy
9,10
4. Chiari Malformation
This is another medical condition associated with neural tube defects. In this instance there is
an extension of the cerebellum into the spinal canal and thus blocking the flow of CSF. There
may be associated symptoms of upper body weakness, difficulty in swallowing and breathing
and hydrocephalus
5
.
5. Meckel syndrome
This problem is associated with neural tube defects and it has following features:
Occipital encephalocele along with micrecephaly
Cleft palate
Polycystic kidney disease
Polydactyly
Ambiguous genitals
5
6. Dandy-Walker-Malformation
It is characterized by enlargement of the 4
th
ventricle along with a cyst that extends into the
posterior cranial fossa. This malformation is also associated with neural tube defects
5
.
Did you enjoy this article?
Help Spina Bifida Awareness!
Tweet
Get free updates
References
1. Davies RW. Congenital vertebral anomalies: aetiology and relationship to spina bifida
cystica. J Med Genet 1975;12(3):280-8.
2. Moris G. Adult Complications of Spina Bifida Occulta [internet]. [last updated 2011
March 25; cited 2013 Aug 23]. Available from:
http://www.livestrong.com/article/244091-adult-complications-of-spina-bifida-occulta/.
Anencephaly [internet]. [last updated 2011 May 1; cited 2013 Aug 23]. Available from:
http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0002547/.
3. Khan AN, Turnbull I, MacDonald S. Encephalocele imaging: review [Internet]. 2011
[lasted updated 2011 May 25; cited 2013 Aug 17]. Available from:
http://emedicine.medscape.com/article/403308-overview.
4. Anthony D, John G, Adam R, Jeffrey V, Geoffrey L. Frontoethmoidal encephaloceles:
reconstruction and refinements. J Caraniofac Surg 2011;12(1):6-18.
5. What are Encephaloceles? [Internet]. [Cited 2013 Aug 17]. Available from:
http://www.bandbacktogether.com/encephalocele-resources/.
6. Yamada S, Lonser RR. Adult tethered cord syndrome. J spinal Disord 2000;13(4):319-23.
7. Agarwalla PK, Dunn IF, Scott RM, Smith ER. Tethered cord syndrome. Neurosurg Clin N
Am 2007;18(3):531-47.
8. Pang D, Wilberger JE. Tethered cord syndrome in adults. J Neurosurg 1982;57(1):32-47.
9. Ratliff J, Mahoney PS, Kline DG. Tethered cord syndrome in adults. South Med J
1999;92(12):1199-203.
Potrebbero piacerti anche
- Nnewfile 2Documento2 pagineNnewfile 2mahariyaNessuna valutazione finora
- A Look at Bipolar Disorder in Michael ClaytonDocumento9 pagineA Look at Bipolar Disorder in Michael ClaytonRichard Moore0% (1)
- Spina Bifida: Causes and Types of Birth DefectDocumento11 pagineSpina Bifida: Causes and Types of Birth DefectErica Joy Algire VillalunaNessuna valutazione finora
- Drug Cards CNSDocumento23 pagineDrug Cards CNSChristine Schroeder100% (2)
- Mcmaster Nursing Anatomy 1H06 Tutorial Assignment 3Documento6 pagineMcmaster Nursing Anatomy 1H06 Tutorial Assignment 3NTRisforthinkersNessuna valutazione finora
- NCP Risk For Activity IntoleranceDocumento4 pagineNCP Risk For Activity IntoleranceBAGUIO CATSNessuna valutazione finora
- Spina Bifida Brochure 508compDocumento20 pagineSpina Bifida Brochure 508compfsaajaNessuna valutazione finora
- Spina Bifida OverviewDocumento26 pagineSpina Bifida OverviewPearl Raiza HadaniNessuna valutazione finora
- Bell's Palsy, MS, Epilepsy 2Documento40 pagineBell's Palsy, MS, Epilepsy 2abdoNessuna valutazione finora
- Neural Tube DefectsDocumento2 pagineNeural Tube DefectsMatthew RyanNessuna valutazione finora
- Genetic Disorders Lec # 6Documento43 pagineGenetic Disorders Lec # 6MISS. COMNessuna valutazione finora
- Tethered Spinal Cord SyndromeDocumento7 pagineTethered Spinal Cord SyndromeeditEonNessuna valutazione finora
- Tethered Cord SyndromeDocumento10 pagineTethered Cord SyndromeLinda SugiartoNessuna valutazione finora
- Down's Syndrome and Spina BifidaDocumento23 pagineDown's Syndrome and Spina BifidaKajal KaliaNessuna valutazione finora
- Different Types of Rare SyndromesDocumento6 pagineDifferent Types of Rare SyndromesAdnan RezaNessuna valutazione finora
- Spina BifidaDocumento18 pagineSpina BifidaIrham KhairiNessuna valutazione finora
- Neural Tube Defects and Folic Acid: Dr. Sukma Sahreni, M.GiziDocumento38 pagineNeural Tube Defects and Folic Acid: Dr. Sukma Sahreni, M.GiziGinanjar Putri SariNessuna valutazione finora
- Spina BifidaDocumento33 pagineSpina BifidaRegine Prongoso DagumanpanNessuna valutazione finora
- Spina Bifida: Causes, Types and TreatmentDocumento41 pagineSpina Bifida: Causes, Types and Treatmenthamza_shoaib99Nessuna valutazione finora
- Spinal Deformities (Congenital)Documento27 pagineSpinal Deformities (Congenital)deathmetal017Nessuna valutazione finora
- Spina BifidaDocumento2 pagineSpina BifidaMI ZINessuna valutazione finora
- Neema Rawat Microteaching (Spina Bifida)Documento67 pagineNeema Rawat Microteaching (Spina Bifida)Dimple GoyalNessuna valutazione finora
- ScoliosisDocumento4 pagineScoliosisDharline Abbygale Garvida AgullanaNessuna valutazione finora
- Physical ImpairmentsDocumento32 paginePhysical Impairmentsabdurehmanasif4gNessuna valutazione finora
- Spina BifidaDocumento2 pagineSpina BifidaTracy100% (2)
- San Filippo SyndromeDocumento3 pagineSan Filippo SyndromerapidoNessuna valutazione finora
- Hypo Tonia Nhs ChoicesDocumento7 pagineHypo Tonia Nhs ChoicesMaryam JamilahNessuna valutazione finora
- Spina Bifida OccultaDocumento2 pagineSpina Bifida OccultasleekchiqueNessuna valutazione finora
- SyringoDocumento3 pagineSyringoSaurabh GandotraNessuna valutazione finora
- Spina BifidaDocumento12 pagineSpina Bifidasalsabil aurellNessuna valutazione finora
- About:: Birth Defects Muscular Dystrophy, Cerebral Palsy Marfan's DiseaseDocumento4 pagineAbout:: Birth Defects Muscular Dystrophy, Cerebral Palsy Marfan's DiseaseAbie BeyNessuna valutazione finora
- Genetic DisordersDocumento26 pagineGenetic DisorderscamsfNessuna valutazione finora
- Cervical SpondylosisDocumento10 pagineCervical Spondylosistaufiq duppa duppaaNessuna valutazione finora
- Surgical Management of Cervical Myelopathy: Clinical EvaulationDocumento10 pagineSurgical Management of Cervical Myelopathy: Clinical EvaulationBaharudin Yusuf RamadhaniNessuna valutazione finora
- Haramaya University: College of Health and Medical Science Department of Midwifery NeurologyDocumento54 pagineHaramaya University: College of Health and Medical Science Department of Midwifery NeurologyMerwan KemalNessuna valutazione finora
- Central Nervous System AbnormalitiesDocumento56 pagineCentral Nervous System AbnormalitiesApin PokhrelNessuna valutazione finora
- Spina BifidaDocumento37 pagineSpina BifidaSyeda Sakina AsgharNessuna valutazione finora
- LimpDocumento7 pagineLimpRakesh DudiNessuna valutazione finora
- Kongenitalni I Razvojni Anomalii Na Rbeten StolbDocumento17 pagineKongenitalni I Razvojni Anomalii Na Rbeten StolbtipharethtNessuna valutazione finora
- Cerebral Palsy Guide: Causes, Symptoms and TreatmentDocumento5 pagineCerebral Palsy Guide: Causes, Symptoms and Treatmentfaye kimNessuna valutazione finora
- Spina Bifida: Causes, Types and TreatmentDocumento17 pagineSpina Bifida: Causes, Types and Treatmentjessy100% (1)
- Spina Bifida - Pediatrics - MSD Manual Professional EditionDocumento4 pagineSpina Bifida - Pediatrics - MSD Manual Professional EditionTONY GO AWAYNessuna valutazione finora
- What To Expect With Spina Bifida Occulta: Find Support For Your Mental HealthDocumento2 pagineWhat To Expect With Spina Bifida Occulta: Find Support For Your Mental Healthmiftah8885Nessuna valutazione finora
- SpondylolisthesisDocumento31 pagineSpondylolisthesisMD ABDUR RAHANNessuna valutazione finora
- Abnormal Spine CurvaturesDocumento7 pagineAbnormal Spine CurvaturesMartin SageNessuna valutazione finora
- ScoliosisDocumento3 pagineScoliosisTracy100% (1)
- MeningomyeloceleDocumento42 pagineMeningomyeloceleSundaraBharathiNessuna valutazione finora
- Neural Tube Defects: Dr.M.G.Kartheeka Fellow in Neonatology Cloudnine, OARDocumento36 pagineNeural Tube Defects: Dr.M.G.Kartheeka Fellow in Neonatology Cloudnine, OARM G KARTHEEKANessuna valutazione finora
- Spinalbifida 121213120324 Phpapp02Documento28 pagineSpinalbifida 121213120324 Phpapp02Silvana María Espinoza CuadrosNessuna valutazione finora
- Kyphosis - Symptoms - Causes - TreatmentDocumento5 pagineKyphosis - Symptoms - Causes - TreatmentMara ColegiuNessuna valutazione finora
- Spina Bifida: Causes, Treatment and PreventionDocumento31 pagineSpina Bifida: Causes, Treatment and PreventionArjun JadejaNessuna valutazione finora
- Spina BifidaDocumento46 pagineSpina BifidaS G100% (1)
- Ankylosing LeafletfaDocumento2 pagineAnkylosing LeafletfaAaron NelsonNessuna valutazione finora
- Pediatric Spine MRI: Occult Spinal DysraphismsDocumento5 paginePediatric Spine MRI: Occult Spinal DysraphismsSilma FarrahaNessuna valutazione finora
- Understanding Muscular Dystrophy: Causes, Symptoms and TreatmentDocumento6 pagineUnderstanding Muscular Dystrophy: Causes, Symptoms and TreatmentKatrina Clarisse HutallaNessuna valutazione finora
- RRLDocumento14 pagineRRLFreisanChenMandumotanNessuna valutazione finora
- 21 - Spondylolisthesis - D3Documento31 pagine21 - Spondylolisthesis - D3Mohamed Magdy El MeligieNessuna valutazione finora
- Myelomeningocele - StatPearls - NCBI BookshelfDocumento13 pagineMyelomeningocele - StatPearls - NCBI BookshelfEmmanuel Andrew Dela CruzNessuna valutazione finora
- Spinal DisDocumento32 pagineSpinal DisAkmal Niam FirdausiNessuna valutazione finora
- Four Myths About Spondylitis: Clinician's GuideDocumento2 pagineFour Myths About Spondylitis: Clinician's GuideAmy YoungNessuna valutazione finora
- Syringomyelia, A Simple Guide To The Condition, Treatment And Related DiseasesDa EverandSyringomyelia, A Simple Guide To The Condition, Treatment And Related DiseasesNessuna valutazione finora
- Spinal Stenosis: A Beginner's Quick Start Guide to Managing the Condition Through Diet and Other Lifestyle Remedies, With Sample RecipesDa EverandSpinal Stenosis: A Beginner's Quick Start Guide to Managing the Condition Through Diet and Other Lifestyle Remedies, With Sample RecipesNessuna valutazione finora
- A Simple Guide to Muscle Dystrophy Disease and Related ConditionsDa EverandA Simple Guide to Muscle Dystrophy Disease and Related ConditionsValutazione: 2 su 5 stelle2/5 (1)
- TETANUS TREATMENT: ANTIBIOTICS, ANTITOXIN, SUPPORTIVE CAREDocumento36 pagineTETANUS TREATMENT: ANTIBIOTICS, ANTITOXIN, SUPPORTIVE CARESitaNessuna valutazione finora
- 1319 FullDocumento9 pagine1319 FullSitaNessuna valutazione finora
- Status Epileptikus DR Dwi Putro SpAK PDFDocumento39 pagineStatus Epileptikus DR Dwi Putro SpAK PDFSitaNessuna valutazione finora
- Status EpileptikusDocumento39 pagineStatus EpileptikusSitaNessuna valutazione finora
- 12 24 1 SMDocumento6 pagine12 24 1 SMSitaNessuna valutazione finora
- Pain, Agitation, DeliriumDocumento5 paginePain, Agitation, DeliriumSitaNessuna valutazione finora
- Post-Streptococcal Acute Glomerulonephritis in Children: Clinical Features and PathogenesisDocumento16 paginePost-Streptococcal Acute Glomerulonephritis in Children: Clinical Features and PathogenesisSitaNessuna valutazione finora
- Infection Control - Bron HenebryDocumento28 pagineInfection Control - Bron HenebryGhazali Ahmad SiregarNessuna valutazione finora
- Chronic Lung DiseaseDocumento59 pagineChronic Lung DiseaseSitaNessuna valutazione finora
- Clinical Practive Guidelines For The Management of Pain Agitation and Delirium in Adult PatientsDocumento44 pagineClinical Practive Guidelines For The Management of Pain Agitation and Delirium in Adult PatientsLuis GuerreroNessuna valutazione finora
- General Spellings Guidelines For IndonesianDocumento3 pagineGeneral Spellings Guidelines For IndonesianSitaNessuna valutazione finora
- Circulation 1977 Gutgesell 457 62Documento7 pagineCirculation 1977 Gutgesell 457 62SitaNessuna valutazione finora
- Power Point EBCR BonnieDocumento51 paginePower Point EBCR BonnieSitaNessuna valutazione finora
- JURNALDocumento9 pagineJURNALSitaNessuna valutazione finora
- Jurnal 3Documento10 pagineJurnal 3SitaNessuna valutazione finora
- Jurnal 1 PDFDocumento13 pagineJurnal 1 PDFSitaNessuna valutazione finora
- Jurnal DengueDocumento3 pagineJurnal DengueSitaNessuna valutazione finora
- Highoutput OstomyDocumento11 pagineHighoutput OstomySitaNessuna valutazione finora
- Kissoon WFPICCS SepsisDocumento10 pagineKissoon WFPICCS SepsisSitaNessuna valutazione finora
- JurnalDocumento6 pagineJurnalSitaNessuna valutazione finora
- CHQ: Child Health Questionnaire: (For Content Review Only)Documento3 pagineCHQ: Child Health Questionnaire: (For Content Review Only)SitaNessuna valutazione finora
- Functional Status QuestionnaireDocumento7 pagineFunctional Status QuestionnaireTO Joss AguilarNessuna valutazione finora
- Jurnal AningDocumento2 pagineJurnal AningSitaNessuna valutazione finora
- 978 FullDocumento7 pagine978 FullSitaNessuna valutazione finora
- Acute Lymphoblastic Leukemia: This Publication Was Sponsored byDocumento52 pagineAcute Lymphoblastic Leukemia: This Publication Was Sponsored bymisbahhari_mdNessuna valutazione finora
- Hypertonic Saline For Treating Raised Intracranial Pressure - Literature Review With Meta-AnalysisDocumento12 pagineHypertonic Saline For Treating Raised Intracranial Pressure - Literature Review With Meta-AnalysisiswanlatifNessuna valutazione finora
- Second-Line Immunosuppressive Treatment of Childhood Nephrotic Syndrome: A Single-Center ExperienceDocumento10 pagineSecond-Line Immunosuppressive Treatment of Childhood Nephrotic Syndrome: A Single-Center ExperienceSitaNessuna valutazione finora
- Neonatal DiabetesDocumento5 pagineNeonatal DiabetesSitaNessuna valutazione finora
- Keywords: Diabetic Ketoacidosis, Neonatal Diabetes, SulphonylureaDocumento1 paginaKeywords: Diabetic Ketoacidosis, Neonatal Diabetes, SulphonylureaSitaNessuna valutazione finora
- Genta HpyloriDocumento7 pagineGenta HpyloriSitaNessuna valutazione finora
- Veterinary AnesthesiaDocumento7 pagineVeterinary AnesthesiaMikeunoe100% (1)
- SBAR Communication GuidelinesDocumento2 pagineSBAR Communication GuidelinesmonabertNessuna valutazione finora
- CHICKENPOX: SIGNS, SYMPTOMS, TREATMENT AND NURSING CAREDocumento16 pagineCHICKENPOX: SIGNS, SYMPTOMS, TREATMENT AND NURSING CAREAlbert TerbioNessuna valutazione finora
- Artificial PancreasDocumento5 pagineArtificial PancreasShreeja SPNessuna valutazione finora
- Anti Thyroid DrugsDocumento22 pagineAnti Thyroid DrugsShahid HameedNessuna valutazione finora
- NRes1 AssignmentDocumento2 pagineNRes1 AssignmentAinee MeuvinNessuna valutazione finora
- A CASE STUDY ON Chronic Renal FailureDocumento2 pagineA CASE STUDY ON Chronic Renal FailureJake Yvan DizonNessuna valutazione finora
- Pharmacovigilance 1Documento28 paginePharmacovigilance 1Gideon AdurojaNessuna valutazione finora
- Joshua Greenlee Mba HT/HTL (Ascp), Scott Webster PHD, Howard Gray Bs MT (Ascp), Patricia Reeves HT (Ascp), Erico Von Bueren PHD MorDocumento1 paginaJoshua Greenlee Mba HT/HTL (Ascp), Scott Webster PHD, Howard Gray Bs MT (Ascp), Patricia Reeves HT (Ascp), Erico Von Bueren PHD MorRashid AliNessuna valutazione finora
- Uses of Inhaler DevicesDocumento39 pagineUses of Inhaler Devicesluis_chubeeNessuna valutazione finora
- Biomechanical Subcomponents Explained - RG 2022Documento6 pagineBiomechanical Subcomponents Explained - RG 2022ashlyn granthamNessuna valutazione finora
- Comparison Between Proprioceptive Neuromuscular Facilitation and Neuromuscular Reeducation For Reducing Facial Disability and Synkinesis in Patients W PDFDocumento8 pagineComparison Between Proprioceptive Neuromuscular Facilitation and Neuromuscular Reeducation For Reducing Facial Disability and Synkinesis in Patients W PDFbenjiNessuna valutazione finora
- CPG - Acute Infectious DiarrheaDocumento52 pagineCPG - Acute Infectious DiarrheaJim Christian EllaserNessuna valutazione finora
- Autonomic FailureDocumento12 pagineAutonomic FailureAndreina AcevedoNessuna valutazione finora
- 525 FullDocumento9 pagine525 FulldianaNessuna valutazione finora
- Amphotericin B Deoxycholate (Conventional) - Drug Information - UpToDate-1Documento4 pagineAmphotericin B Deoxycholate (Conventional) - Drug Information - UpToDate-1Vh TRNessuna valutazione finora
- Quality Assurance in The Blood Transfusion LabDocumento25 pagineQuality Assurance in The Blood Transfusion LabMichelle AnsahNessuna valutazione finora
- Treatment of Knee Meniscus Pathology: Rehabilitation, Surgery, and OrthobiologicsDocumento17 pagineTreatment of Knee Meniscus Pathology: Rehabilitation, Surgery, and OrthobiologicsQuiroprácticaParaTodosNessuna valutazione finora
- Case Study StrokeDocumento5 pagineCase Study StrokelilutzuNessuna valutazione finora
- Hypercalcemia in Dogs Emergent Care Diagnostics and TreatmentsDocumento8 pagineHypercalcemia in Dogs Emergent Care Diagnostics and Treatmentstarilubis277Nessuna valutazione finora
- Medication Therapy StudentDocumento4 pagineMedication Therapy StudentНаталья МурашоваNessuna valutazione finora
- Common Side Effects of OtezlaDocumento57 pagineCommon Side Effects of OtezlaMica JeremijevicNessuna valutazione finora
- Tumor Lysis SyndromeDocumento12 pagineTumor Lysis Syndromeapi-647779956Nessuna valutazione finora
- DR Walsh Autism Ocd Pandas Depression MethylationDocumento6 pagineDR Walsh Autism Ocd Pandas Depression MethylationAnupama PouloseNessuna valutazione finora
- Malaria in Children: Department of Paediatrics and Child Health, Mbarara UniversityDocumento13 pagineMalaria in Children: Department of Paediatrics and Child Health, Mbarara UniversityMwanja MosesNessuna valutazione finora