Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Liver Physiology and Pathophysiology
Caricato da
Muhammad Rosyid RidloCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Liver Physiology and Pathophysiology
Caricato da
Muhammad Rosyid RidloCopyright:
Formati disponibili
Ovid: Principles and Practice of Pediatric Surgery
Copyright 2005 Lippincott Williams & Wilkins
Oldham, Keith T., Colombani, Paul M., Foglia, Robert P., Skinner, Michael A.
Principles and Practice of Pediatric Surgery, 4th Edition
Chapter 90
Liver Physiology and Pathophysiology
Edward P. Tagge
Patrick B. Thomas
Derya U. Tagge
Medical University of South Carolina, Department of Surgery, Divisions of Pediatric Surgery and General
Surgery, Charleston, South Carolina 29425.
Medical University of South Carolina, Department of Surgery, Divisions of Pediatric Surgery and General
Surgery, Charleston, South Carolina 29425.
Medical University of South Carolina, Department of Surgery, Divisions of Pediatric Surgery and General
Surgery, Charleston, South Carolina 29425.
The liver serves a key role in many critical metabolic pathways. As the first organ to receive a nutrient-enriched
blood supply from the portal system, it is strategically situated to perform a large number of diverse metabolic
functions. In addition, the unique vascular structure of the liver provides unparalleled access to nutrients and
xenobiotics absorbed from the intestinal lumen. Processing, redistribution, and storage of metabolic fuels such
as glucose and fatty acids are a major responsibility of the liver. Protein production, particularly albumin and the
coagulation factors, is an extremely important function of the liver. The liver also contains a host of biochemical
pathways for the modification and detoxification of compounds absorbed from the small intestine.
ANATOMY
Morphogenesis
The liver and the biliary system originate from the primitive foregut. The hepatic anlage appears during the
fourth week of gestation as a duodenal diverticulum. The hepatic lobules are identifiable at the sixth gestational
week, and the cystic duct and the gallbladder are fully recanalized by the seventh to eighth week. The liver
reaches a peak relative size of about 10% of fetal weight at the ninth week, dropping to 5% of body weight at
birth and eventually 2% in an adult. Early in gestation, hematopoietic cells outnumber functioning hepatocytes
in the hepatic anlage. Near term, the hepatocytes dominate the organ, and hematopoiesis is virtually absent by
the second postnatal month in full-term infants.
Fetal hepatic blood flow is derived from the hepatic artery and from the portal and umbilical veins, which form
the portal sinus. The portal venous inflow is directed mainly to the right lobe of the liver; and umbilical flow is
directed primarily to the left. The ductus venosus shunts blood from the portal and umbilical veins to the hepatic
vein, bypassing the sinusoidal network. Because the oxygen saturation is lower in portal than in umbilical
venous blood, the right hepatic lobe has lower oxygenation and greater hematopoietic activity than the left
hepatic lobe. The ductus venosus obliterates when oral feedings are initiated, ensuring all blood traverse the
hepatic vascular sinusoidal system.
Ultrastructure
The fundamental unit in the liver is the hepatic acinus, which can be envisioned as a wheel, with the central vein
http://gateway.ut.ovid.com/gw2/ovidweb.cgi (1 of 31)1/2/2006 10:18:21 PM
Ovid: Principles and Practice of Pediatric Surgery
comprising the hub and four to six portal triads representing the rim. The transport and metabolic activities of
the liver are facilitated by the structural arrangement of liver cell cords, which are formed by rows of
hepatocytes, separated by sinusoids that converge toward the tributaries of the central vein. This relationship
establishes the patterns of flow for substances to and from the liver. Plasma proteins and other plasma
components are secreted by the liver. Absorbed and circulating nutrients arrive through the portal vein or the
hepatic artery, pass through the sinusoids where they are modified by the hepatocytes, and are
P.1438
returned to the systemic circulation at the central vein. Biliary components are transported via the series of
enlarging channels from the bile canaliculi through the bile ductule to the common bile duct.
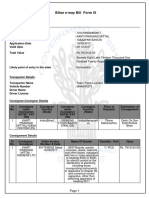
FI GURE 90- 1. Liver lobule. (Adapted from Anatomical Charts, Co.)
Our understanding of the ultrastructural anatomy of the hepatocyte has been made possible through electron
microscopy and cell fractionation techniques (Fig. 90-1). Hepatocytes are epithelial cells that are bounded by
three separate membrane domains: (1) the basolateral membrane, which abuts the sinusoidal space; (2) the
apical membrane, which circumscribes the canaliculus; and (3) the lateral hepatic membrane between adjacent
hepatocytes (1). The liver's unique sinusoidal structure is well suited for the bidirectional transfer of a variety of
solutes, including macromolecules, across the sinusoidal membrane. The low pressure allows blood to percolate
slowly through the sinusoids and hepatic acinus. Fenestrae within the sinusoidal endothelium and the absence of
a basement membrane permit direct contact of the portal blood with the hepatic sinusoidal surface in the space
of Disse. Canalicular membranes of adjacent hepatocytes form bile canaliculi, which are bounded by tight
http://gateway.ut.ovid.com/gw2/ovidweb.cgi (2 of 31)1/2/2006 10:18:21 PM
Ovid: Principles and Practice of Pediatric Surgery
junctions preventing transfer of secreted compounds back into the sinusoid. There are abundant mitochondria,
which are the sites of substrate metabolism, of key processes in gluconeogenesis, and of storage and release of
energy. An extensive endoplasmic reticulum is the site of protein and triglyceride synthesis and drug
metabolism. The prominent golgi apparatus is active in protein packaging and possibly in bile secretion.
There are a variety of nonparenchymal cells in the liver, which serve other important physiologic roles. The
sinusoidal space houses macrophage-derived Kupffer cells, which are phagocytic cells. These cells are important
mediators of the hepatic inflammatory response. The lipocyte, identified phenotypically by its high lipid content,
is the major site for vitamin A storage. It is also the major cell type responsible for synthesis of extracellular
collagen, and is a critical component of the fibrogenic response to liver injury.
P.1439
METABOLIC FUNCTIONS
A major responsibility of the liver is to provide a continual source of energy for the body. The liver regulates
nutrient flux during periods of nutrient absorption, digestion, and modification for storage. It also makes
nutrients available systemically during periods of fasting. The regulation of these metabolic pathways involves
complex interactions among the nutrient content of the blood, end products of nutrient metabolism, and
hormonal regulation.
Carbohydrate Metabolism
Glucose is the central component of all metabolic pathways because it can be converted to amino acids, fatty
acids, or glycogen (the major storage form of glucose). Maintaining adequate circulating levels of glucose is
essential for the central nervous system. The brain normally uses glucose as its major metabolic fuel, and
hepatic glycogen is the main storage site for the glucose-dependent brain, erythrocytes, retina, and renal
medulla (2). The liver serves a key role in maintaining total carbohydrate stores because of its ability to store
glycogen and synthesize glucose from precursors (3). Glycogen constitutes approximately 10% of liver weight.
The liver can store approximately a 2-day supply of glucose in the form of glycogen before gluconeogenesis
occurs. By gluconeogenesis, the liver is able to produce up to 240 g of glucose a day, which is approximately
twice the metabolic needs of the retina, red blood cells, and brain.
Immediately after birth, an infant is dependent on hepatic glycogenolysis; thereafter, an infant is capable of
both glycogenolysis and gluconeogenesis. The fluctuations in serum glucose concentration in preterm infants are
due in part to the fact that efficient regulation of the synthesis, storage, and degradation of glycogen develops
only near the end of full-term gestation.
Fatty Acids Metabolism
The liver plays a central role in regulating the body's total fatty acid needs. Oxidation of fatty acids to carbon
dioxide and water yields the highest adenosine triphosphate (ATP) production of any metabolic fuel. Fatty acids
are thus the most efficient long-term storage form of energy. Fatty acid oxidation particularly provides a major
source of energy in early life, complementing glycogenolysis and gluconeogenesis. Newborn infants are relatively
intolerant of prolonged fasting, owing in part to a restricted capacity for hepatic ketogenesis. Rapid maturation
of the ability of the liver to oxidize fatty acid occurs during the first few days of life. Because milk provides the
major source of calories in early life, this high-fat, low-carbohydrate diet mandates active gluconeogenesis to
maintain blood sugar levels. When the glucose supply is limited, ketone body production from endogenous fatty
acids provides substrate for hepatic gluconeogenesis and an alternative fuel for brain metabolism. Excess
glucose can be converted to fatty acid for future use and stored in distal sites such as adipose tissue.
Fatty acids are also involved in various physiologic functions. For instance, fatty acids are constituent parts of
various cellular structural components such as membranes. Furthermore, they are involved in regulatory
functions in intracellular communication, golgi function, and anchoring of membrane proteins. The liver serves a
http://gateway.ut.ovid.com/gw2/ovidweb.cgi (3 of 31)1/2/2006 10:18:21 PM
Ovid: Principles and Practice of Pediatric Surgery
central role in the synthesis of fatty acid for storage in distal sites and the trafficking of lipids within the body.
For lipids to be transferred between different locations, the liver synthesizes a large number of apolipoproteins.
Lipids may be stored temporarily in the liver as fat droplets, excreted directly into bile, or metabolized into bile
acids. The liver is the major site of sterol excretion from the body and is the site of bile acid synthesis. The
production and metabolism of sterols require complex regulation of multiple enzymatic pathways, and bile acids
play a critical role in modulating these enzyme activities. Bile acids are recirculated 20 to 30 times per day via a
unique enterohepatic circulation that requires specific active transport processes (4) (Fig. 90-2). In the terminal
ileum, a unique sodium-dependent bile acid transporter prevents loss of bile acids in the stool (5), and in the
liver the activity of specific transmembrane transporters and intracellular binding proteins are required to
capture and recirculate the bile acids. Bile acids also play an important role in micellization of fats for intestinal
absorption.
Protein Metabolism
Formation of plasma proteins is a vital function of the liver (Table 90-1). Because protein metabolism is such an
important part of liver function, the synthetic capability of the liver is routinely assessed by measurement of
specific serum proteins it produces. The liver synthesizes blood coagulation proteins factor II (prothrombin),
factor VII, factor IX, factor X, protein C, and protein S. All these proteins undergo a unique, vitamin K-
dependent gamma-carboxylation of specific glutamic acid residues, which is essential for normal activity.
More than 95% of serum
1
-antitrypsin (
1
-AT), a member of the serine protease inhibitor family, is synthesized
by the liver. Absent or reduced
1
-AT activity is manifested clinically by destruction of the lung parenchyma with
the early onset of emphysema. The liver also synthesizes carrier proteins albumin and alpha-fetoprotein (AFP).
Albumin functions as a nonspecific carrier protein that binds fatty acids, bile acids, and numerous other
compounds, as well as providing serum oncotic pressure that opposes hydrostatic pressure. AFP serves a similar
function in the
P.1440
P.1441
developing organism. Synthesis of albumin appears at approximately the seventh and eighth gestational week
and increases in inverse proportion to that of AFP, which is a dominant fetal protein. By the third and fourth
month of gestation, the fetal liver is able to produce each of the major protein classes, at concentrations
considerably below those achieved at maturity. AFP is entirely replaced by serum albumin at the end of the first
year of life. During liver regeneration, as in acute viral hepatitis, and in liver tumors such as hepatoblastoma and
hepatocellular carcinoma, serum AFP levels may be elevated.
http://gateway.ut.ovid.com/gw2/ovidweb.cgi (4 of 31)1/2/2006 10:18:21 PM
Ovid: Principles and Practice of Pediatric Surgery
FI GURE 90- 2. Enterohepatic circulation of bile acids. (From Carey MC. The enterohepatic circulation. In: Arias
IM, Popper H, Schacter D, et al., ed. The liver: biology and pathobiology. New York: Raven Press, 1982:430,
with permission.)
TABLE 90-1 Important Proteins Produced by the Liver.
Category Protein Function
Coagulation proteins Fibrinogen (factor 1) Forms fibrin
Prothrombin (factor II) Converts fibrinogen to fibrin
Factors V, VII, IX, X, XI, and XII Serves as extrinisic and intrinsic pathway
Plasminogen Forms plasmin
Antithrombin III Acts as protease inhibitor
Protein S Acts as protein C cofactor
Protein C Acts as anticoagulant
Transport proteins Albumin Acts as carrier protein, provides oncotic
pressure
Transferrin Transports iron
Ceruloplasmin Transports copper
Haptoglobin Transports free hemoglobin
Thyroxin-binding globulin Transports thyroid hormone
Retinol-binding protein Transports vitamin A
Vitamin D-binding protein Transports vitamin D
Acute-phase reactants
2
-Macroglobulin Binds endopeptidases
1
-Antitrypsin Inhibits serine proteases
C-reactive protein Modifies inflammation
Lipoprotein metabolism Apolipoprotein AI and AII Acts as Lecithin cholesterol
acyltransferase (LCAT) cofactors
Apolipoprotein CI, CII, and CIII Inhibits binding to liver
http://gateway.ut.ovid.com/gw2/ovidweb.cgi (5 of 31)1/2/2006 10:18:21 PM
Ovid: Principles and Practice of Pediatric Surgery
Apolipoprotein E Recognizes receptor
Apo B100 Synthesizes and secretes very low-
density lipoprotein
Biotransformation
The liver plays a major role in the biotransformation of drugs, particularly those poorly excreted in the urine.
This occurs in two phases. Phase I uses microsomal enzymes such as the cytochrome P450 enzymes to make
the drugs more polar. In phase II, the drugs are conjugated with other moieties to facilitate their excretion in
bile or urine. Newborn infants have a decreased capacity to metabolize metabolic byproducts and detoxify
certain drugs, owing to underdevelopment of these hepatic enzyme systems. For example, newborn infants have
decreased activity of uridine diphosphate (UDP)-glucuronyl transferase (rate-limiting enzyme in bilirubin
excretion), which converts unconjugated bilirubin to the readily excreted glucuronide conjugate. Microsomal
activity can be stimulated by the administration of phenobarbital or other inducers of cytochrome P450.
Hepatic Excretory Function
Bile acids are the major product of degradation of cholesterol, and their secretion is the major determinant of
bile flow. Incorporation of bile acids into micelles with cholesterol and phospholipid creates an efficient vehicle
for solubilization and intestinal absorption of lipophilic compounds, such as dietary fats and fat-soluble vitamins.
The primary bile acids, cholic acid and chenodeoxycholic acid, are synthesized in the liver. In response to a
meal, contraction of the gallbladder delivers bile acids to the intestine. After mediating fat digestion, the bile
acids enter the enterohepatic recirculation as described previously. Bile acids are reabsorbed from the terminal
ileum and returned to the liver via portal blood, where they are taken up by liver cells and reexcreted in bile. In
an adult, this enterohepatic circulation involves 90% to 95% of the circulating bile acid pool. Bile acids that
escape ileal reabsorption reach the colon, where the bacterial flora, through dehydroxylation and deconjugation,
produces the secondary bile acids, deoxycholate and lithocholate.
Neonates have inefficient ileal reabsorption and a low rate of hepatic clearance of bile acids from portal blood.
The latter results in elevated serum concentrations of bile acids in healthy newborns, often to levels that would
suggest liver disease in older individuals. The size of the bile acid pool in a neonate is about one-half that of an
adult, and the bile acid concentration in the proximal intestinal lumen is similarly decreased to levels that are
frequently below the concentration required for micelle formation (2 mM); accordingly, absorption of dietary fats
and fat-soluble vitamins is reduced, but not sufficiently to produce malabsorption. Transient phases of
physiologic cholestasis and physiologic steatorrhea have a role in the nutrition of low birth weight infants,
but are otherwise of minor importance.
CLINICAL MANIFESTATIONS OF LIVER DISEASE
Acute or chronic liver injury can reduce the metabolic and synthetic capabilities of the liver, thereby resulting in
diverse clinical disorders and a variety of clinical presentations. Liver enlargement, although not pathognomonic,
is one of the more common presentations of liver disease. In a newborn infant, extension of the liver edge more
than 3.5 cm below the costal margin in the midclavicular line suggests hepatic enlargement. In children, the
normal liver edge can be felt up to 2 cm below the right costal margin. The downward displacement of the liver
by the diaphragm or thoracic organs can create an erroneous impression of hepatomegaly. Examination of the
liver should note the consistency, contour, tenderness, or the presence of any masses or bruits, as well as
assessing splenic size. Ultrasonography can often help in evaluating unexplained hepatomegaly.
Jaundice becomes clinically apparent in children and adults when the serum concentration of bilirubin reaches 2
to 3 mg per dL. Bilirubin occurs in four forms: (1) unconjugated bilirubin tightly bound to albumin, (2) free or
unbound bilirubin (the form responsible for kernicterus), (3) conjugated bilirubin, and (4) delta fraction (bilirubin
covalently bound to albumin). Jaundice may reflect accumulation of either unconjugated or conjugated bilirubin.
An increase in unconjugated bilirubin may indicate increased production, hemolysis, reduced hepatic removal, or
http://gateway.ut.ovid.com/gw2/ovidweb.cgi (6 of 31)1/2/2006 10:18:21 PM
Ovid: Principles and Practice of Pediatric Surgery
altered metabolism of bilirubin. Significant accumulations of conjugated bilirubin (more than 20% of total)
reflect decreased excretion by damaged hepatic parenchymal cells or disease of biliary tract. Cholestasis is a
more general term, defined as accumulation in serum of substances normally excreted in bile, such as bilirubin,
cholesterol, bile acids, and trace elements.
Cirrhosis is an advanced form of liver disease, and may result from hepatitis, toxic injury, or chronic biliary
obstruction. Cirrhosis is defined histologically by the presence of bands of fibrous tissue linking portal areas, thus
forming parenchymal nodules. Cirrhosis may be macronodular, with nodules of various sizes (up to 5 cm)
P.1442
separated by broad septa, or micronodular, with nodules of uniform size (less than 1 cm) separated by fine
septa. The progressive scarring of cirrhosis leads to altered hepatic blood flow, further impairing liver cell
function and causing the development of portal hypertension (PH).
PH is defined as an increase in portal venous pressure to greater than 20 mm Hg. Because the portal vein drains
the splanchnic area into the hepatic sinusoids, pressure is normally slightly higher (5 to 10 mm Hg) in the portal
vein than in other venous systems in order to overcome the resistance of the sinusoidal system. However, in
liver disease, a combination of increased hepatic resistance and increased circulating blood volume can lead to
hypertension in the portal system, manifesting as gastrointestinal (GI) bleeding at points of portosystemic
collaterals.
Ascites is a common manifestation of end-stage liver disease. In patients with significant hepatic disease,
sinusoidal blockade caused by cirrhosis increases hydrostatic pressure and transudation of fluid.
Metabolic abnormalities may complicate acute or chronic liver disorders, leading to encephalopathy. This
neuropsychiatric disturbance can present in a variety of ways, including restless, altered mentation, varying
levels of consciousness, or even coma. With chronic liver disease, hepatic encephalopathy may be recurrent,
precipitated by bleeding, infection, drugs or electrolyte and acidbase disturbances.
There is a close relationship between hepatic and renal dysfunction. Systemic disease may affect both organs
individually and/or simultaneously, or parenchymal liver disease may produce secondary impairment of renal
function. Hepatorenal syndrome is defined as renal failure in a patient with cirrhosis and no other demonstrable
cause of renal failure. The pathophysiology is poorly defined, but seems to involve altered hormonal metabolism
that leads to abnormalities of renal blood flow.
EVALUATION OF LIVER DISEASE
Adequate evaluation of a child with suspected liver disease starts with an accurate history and a careful physical
examination. Further evaluation is aided by judicious selection of diagnostic tests, followed by imaging studies
and potentially a liver biopsy. Any single biochemical assay provides limited information, which must be placed
in the context of the entire clinical picture.
Biochemical Liver Tests
The liver performs a diverse array of biochemical, synthetic, and excretory functions, and as a result, no single
biochemical test is capable of providing an accurate assessment of hepatic function. Biochemical liver tests have
limited sensitivity and specificity, and do not all reflect liver function as the common misnomer liver function
tests implies (6).
The aminotransferases include aspartate aminotransferase (AST, formerly SGOT) and alanine aminotransferase
(ALT, formerly SGPT). These enzymes are elevated in many forms of liver disease, especially those that are
associated with significant hepatocyte necrosis, such as seen in ischemic injury. Although ALT is relatively liver
specific, AST is also found in skeletal and cardiac muscle, kidney, brain, pancreas, and blood cells. Lactate
dehydrogenase (LDH) is a very nonspecific assay, as elevated levels are seen with skeletal or cardiac muscle
injury, hemolysis, stroke, and renal infarction, in addition to acute and chronic liver disease.
http://gateway.ut.ovid.com/gw2/ovidweb.cgi (7 of 31)1/2/2006 10:18:21 PM
Ovid: Principles and Practice of Pediatric Surgery
Alkaline phosphatase (AP) comprises a group of enzymes present in a large variety of tissues, particularly bone
and liver. Elevation of AP in the setting of liver disease results from increased synthesis and from release of the
enzyme into serum, rather than from impaired biliary secretion. Levels of AP up to three times normal are
relatively nonspecific. Because marked elevations of AP can be seen with both infiltrative hepatic disorders and
biliary obstruction (intra- or extrahepatic), the level of AP cannot be used to distinguish between them. Elevation
of AP is commonly seen in neonatal liver disease of various causes. Hepatic gamma glutamyl transpeptidase
(GGTP) is derived from hepatocytes and biliary epithelia. Like AP, GGTP is found in the liver and many
extrahepatic tissues, including the kidney and pancreas. However, it is not found in appreciable quantities in
bone, and it is thus helpful in confirming the hepatic origin of an elevated AP level. The normal serum GGTP level
is significantly higher in infants than in adults. Benign recurrent intrahepatic cholestasis and Byler's syndrome,
both rare cholestatic liver diseases that often present in infancy, are characterized by elevation of the serum AP
without an elevated GGTP.
Bilirubin is an organic anion that is derived primarily from the catabolism of hemoglobin. Serum bilirubin consists
of two major forms, a water-soluble, conjugated, direct fraction and a lipid-soluble, unconjugated, indirect
fraction. The serum bilirubin level is normally almost entirely unconjugated, reflecting a balance between the
rates of production and hepatobiliary excretion. Unconjugated hyperbilirubinemia (i.e., indirect bilirubin fraction
greater than 85% of the total serum bilirubin) results from either increased bilirubin production (most likely by
hemolysis) or from defects in hepatic uptake or conjugation. Conjugated hyperbilirubinemia (i.e., direct bilirubin
fraction greater than 50% of the total serum bilirubin) occurs as a result of a defect in hepatic excretion, with
subsequent regurgitation of conjugated bilirubin from hepatocytes into the serum. This impaired biliary excretion
occurs in both parenchymal liver disease and biliary tract obstruction (7). Thus, measurement of the conjugated
fraction does not reliably distinguish biliary obstruction from parenchymal
P.1443
liver disease. Because conjugated bilirubin is cleared by the kidney, serum concentrations of bilirubin rarely
exceed 30 mg per dL in the absence of hemolysis or renal failure.
The liver plays a crucial role in hemostasis. All major coagulation factors except factor VIII are synthesized in
hepatocytes (see Chapter 16, Fig. 16-2) The prothrombin time (PT) measures the rate of conversion of
prothrombin to thrombin and reflects the activity of several of the factors involved in the extrinsic coagulation
pathway, including factors II, V, VII, and X. Vitamin K is required for the gamma-carboxylation of factors II, VII,
IX, and X, which is essential for the normal function of these factors. Prolongation of the PT may occur in
decompensated liver disease with hepatocellular dysfunction and in chronic cholestatic disease with fat
malabsorption and concomitant vitamin K deficiency.
Approximately 10 g of albumin is synthesized and secreted by hepatocytes each day. With progressive
parenchymal liver disease, albumin synthetic capacity decreases. Thus, albumin concentrations are believed to
reflect one of the important synthetic functions of the liver. However, the serum albumin concentration reflects a
variety of extrahepatic factors, including nutritional and volume status, vascular integrity, catabolism, hormonal
factors, and loss in the urine or stool. Therefore, a low serum albumin level is not specific for liver disease.
Liver Biopsy
Because the morphologic features of specific hepatic diseases are frequently distinctive, liver biopsy combined
with clinical data can suggest an etiology. Tissue obtained by percutaneous liver biopsy can be used for
histologic examination, for enzyme analysis to detect inborn errors of metabolism, and for analysis of stored
material (e.g., iron, copper). In infants and children, needle biopsy of the liver is easily accomplished through
the percutaneous approach. The procedure can be performed safely in infants as young as 1 week, and patients
usually require only sedation and local anesthesia. The risk of development of a complication such as
hemorrhage, hematoma, creation of an arteriovenous fistula, pneumothorax, or bile peritonitis is very small. In
patients with significant liver disease, correction of any associated coagulopathy is strongly encouraged prior to
percutaneous liver biopsy. If the coagulopathy is not correctable, liver biopsy under direct visualization is a
relatively straightforward procedure.
http://gateway.ut.ovid.com/gw2/ovidweb.cgi (8 of 31)1/2/2006 10:18:21 PM
Ovid: Principles and Practice of Pediatric Surgery
Imaging Procedures
Various techniques help define the size, shape, and architecture of the liver, as well as the anatomy of the
biliary system. A plain roentgenographic study may suggest hepatomegaly. Calcifications or collections of gas
may be evident within the liver, biliary tract, or portal circulation.
Ultrasonography provides extremely useful information about the size, composition, and blood flow of the liver.
Ultrasound is particularly useful in children because it can be done at the bedside without the need for sedation
or general anesthesia. Even in neonates, ultrasonography can assess gallbladder size, visualize gallstones,
detect dilatation of the biliary tract, and define a choledochal cyst. In patients with PH, ultrasonography can
evaluate patency of the portal vein or demonstrate collateral circulation. Small amounts of ascitic fluid can be
easily seen on ultrasound, as can mass lesions as small as 1 to 2 cm.
Computed tomography (CT) scanning provides more detailed information, but is less suitable for use in younger
patients because of the small size of structures and the paucity of intraabdominal fat for contrast. When a
hepatic tumor is suspected, CT scanning is the best method to define anatomic extent, solid or cystic nature,
and vascularity. Either CT scanning or ultrasonography may be used to guide percutaneously placed fine needles
for biopsies or aspiration of specific lesions.
Occasionally, direct visualization of the intrahepatic and extrahepatic biliary tree may be required in some
patients to evaluate the cause, location, or extent of biliary obstruction. Gastroduodenoscopy with endoscopic
retrograde cholangiopancreatography (ERCP) has been performed in children for more than 20 years (8). The
technique has been quite successful in managing children with a large number of biliary disorders (9,10). More
recently ERCP has even been used in some centers to delineate the extrahepatic ductal anatomy in infants, and
has been successful in making a differential diagnosis of neonatal hepatitis from extrahepatic biliary atresia (BA)
(11,12). Occasionally, percutaneous transhepatic cholangiography has been used to outline the biliary ductal
system in infants and young children. Magnetic resonance imaging (MRI) is receiving increasing attention as an
alternative imaging technology; magnetic resonance cholangiopancreatography can be of value in differentiating
biliary tract lesions (13).
Radionuclide scanning relies on selective uptake of a radiopharmaceutical agent. Commonly used agents include
(1) technetium 99m-labeled sulfur colloid, which undergoes phagocytosis by Kupffer cells and (2)
99m
Tc-
iminodiacetic acid agents, which are taken up by hepatocytes and excreted into bile. The
99m
Tc-sulfur colloid
scan may detect focal lesions (e.g., tumors, cysts, or abscesses) greater than 2 to 3 cm in diameter. The
99m
Tc-
substituted iminodiacetic acid dyes may differentiate intrahepatic cholestasis from extrahepatic obstruction in
neonates. Imaging results are best when scanning is preceded by a 5- to 7-day period of treatment with
phenobarbital to stimulate bile flow.
Selective angiography of the celiac, superior mesenteric, or hepatic artery may be used to visualize the hepatic
or portal circulation. Angiography is occasionally used to
P.1444
define the blood supply of tumors before surgery and is useful in the study of patients with known or presumed
PH. The patency of the portal system, the extent of collateral circulation, and the caliber of vessels under
consideration for a shunting procedure can be evaluated. MRI and variations on CT scanning can now provide
similar information.
CHOLESTASIS
Neonatal Cholestasis
Neonatal cholestasis must always be considered in a newborn who is jaundiced for more than 14 to 21 days;
measurement of the serum total and conjugated bilirubin in these infants is mandatory (14). Conjugated
hyperbilirubinemia, dark urine, and pale stools are pathognomonic of the neonatal hepatitis syndrome that
http://gateway.ut.ovid.com/gw2/ovidweb.cgi (9 of 31)1/2/2006 10:18:21 PM
Ovid: Principles and Practice of Pediatric Surgery
should be investigated urgently. This neonatal hepatitis syndrome has many causesinfectious, genetic,
metabolic, or miscellaneous. These abnormalities give rise either to mechanical obstruction of bile flow or to
functional impairment of hepatic excretory function and bile secretion (Table 90-2). Neonatal cholestasis may be
divided into extrahepatic and intrahepatic disease. The most important condition in the differential diagnosis is
BA because these infants require expeditious surgical drainage. However, differentiation among extrahepatic BA,
idiopathic neonatal hepatitis, and intrahepatic cholestasis is often particularly difficult.
TABLE 90-2 Causes of Neonatal Cholestasis Syndrome.
Surgically correctable
obstructive lesions
Extrahepatic biliary atresia
Choledochal cyst
Spontaneous bile duct perforation
Surgically noncorrectable
obstructive lesion
Alagille's syndrome
Inborn errors of metabolism
Disorders of carbohydrate
metabolism
Galactosemia
Hereditary fructose intolerance
Fructose-1,6 diphosphatase
deficiency
Glycogen storage disease (Ia, Ib,
III, IV, VI) Disorders of amino acid and
protein metabolism Tyrosinemia
Carbamoyl phosphate synthetase
(CPS)
deficiency
Ornithine transcarbamylase (OTC)
deficiency
Citrullinemia
Argininosuccinic aciduria
Disorders of lipid metabolism
Gaucher disease
Niemann-Pick type C
Disorders of bile acid metabolism
Isomerase deficiency
Reductase deficiency
Zellweger syndrome
Disorders of metal metabolism
Wilson's disease
Perinatal hemochromatosis
Disorders of bilirubin metabolism
Crigler-Najjar syndrome
Gilbert disease
Dubin-Johnson rotor syndrome Congenital infections Cytomegalovirus
Rubella virus
Herpes virus
Hepatitis B virus
Echovirus 14, 19
Coxsackievirus B
http://gateway.ut.ovid.com/gw2/ovidweb.cgi (10 of 31)1/2/2006 10:18:21 PM
Ovid: Principles and Practice of Pediatric Surgery
Toxoplasmosis
Syphilis
Miscellaneous
Idiopathic giant cell hepatitis
Cystic fibrosis
Hemolytic disease
Neonatal hypopituitarism
Inspissated bile syndrome
The clinical features of infants with neonatal cholestasis provide very few clues about etiology (15). The initial
step is prompt recognition of any specific or treatable primary causes of cholestasis, such as sepsis, an
endocrinopathy (hypothyroidism or panhypopituitarism), nutritional hepatotoxicity caused by a specific
metabolic illness (galactosemia), or other metabolic diseases (tyrosinemia). Recognition of such entities allows
institution of appropriate therapy and may possibly prevent further injury. Hepatobiliary disease may be the
initial manifestation of homozygous
1
-AT deficiency or of cystic fibrosis. Neonatal liver disease may also be
associated with congenital syphilis and specific viral infections, notably echo virus, herpes virus, and the
hepatitis viruses. Additional cholestatic disorders include neonatal iron storage disease and inborn errors of bile
acid biosynthesis.
BA is a disorder of the infant liver in which there is obliteration or discontinuity of the extrahepatic biliary
system, resulting in obstruction of bile flow. Untreated, the resulting cholestasis leads to progressive conjugated
hyperbilirubinemia, cirrhosis, hepatic failure, and subsequent death within 2 years. The natural history of BA has
been favorably altered by the Kasai portoenterostomy; approximately one-fourth of patients who undergo a
Kasai portoenterostomy will survive more than 10 years without liver transplantation, one-fourth drain bile but
develop cirrhosis, and the remaining one-half of patients never experience adequate bile flow (16). The
portoenterostomy should be performed before there is irreversible sclerosis of the intrahepatic bile ducts; this is
before the child reaches 3 months of age (17). BA represents the most common indication for pediatric liver
transplantation (18,19,20).
No single biochemical test or imaging procedure can clearly differentiate clearly infants with BA from those with
neonatal hepatitis. Ultrasonography should be carried out because it may detect a choledochal cyst, common
bile duct stone, or another unusual cause of dilatation of the biliary tract. Hepatobiliary scintigraphy using
iminodiacetic acid analogs after phenobarbital stimulation can be helpful to differentiate BA from neonatal
hepatitis (21). Liver biopsy can occasionally provide reliable discriminatory evidence because BA is characterized
by bile duct proliferation, whereas neonatal hepatitis has diffuse hepatocellular disease and giant cell
transformation. However, unless another disease is clearly diagnosed with these tests, the child should undergo
expeditious exploratory laparotomy and intraoperative cholangiogram by a surgeon who has experience doing
the Kasai portoenteostomy.
Cholestasis in the Older Child
Acute viral hepatitis accounts for most cases of cholestasis after the neonatal period, although many of the
conditions causing neonatal cholestasis may also cause chronic cholestasis in older patients. An adolescent with
conjugated hyperbilirubinemia should be evaluated for acute and chronic hepatitis,
1
-AT deficiency, Wilson's
disease, liver disease associated with inflammatory bowel disease, and the syndromes of intrahepatic cholestasis
(with or without bile duct paucity). Other causes include cholelithiasis (22) and abdominal tumors.
INHERITED METABOLIC DISORDERS
Inborn errors of metabolism encompass a vast variety of maladies with varied presentations and
pathophysiology. Metabolic liver disease may present as an acute, life-threatening illness in the neonatal period
or may be manifested as chronic liver disease in adolescence, progressing to liver failure, cirrhosis, or
hepatocellular carcinoma.
http://gateway.ut.ovid.com/gw2/ovidweb.cgi (11 of 31)1/2/2006 10:18:21 PM
Ovid: Principles and Practice of Pediatric Surgery
1
-ANTITRYPSIN DEFICIENCY
Deficiency of
1
-AT is the most common metabolic disease affecting the liver, affecting 1 in 2,000 live births in
the U.S. white population. It is also associated with chronic liver disease and hepatocellular carcinoma in adults,
and is a well-known cause of pulmonary emphysema. It is transmitted in an autosomal recessive fashion with
codominant expression.
1
-AT binds with and promotes the degradation of serine proteases, most important,
neutrophil elastase, which are responsible for triggering inflammatory
P.1445
cascades and activating complement.
1
-AT is normally responsible for more than 90% of antielastase activity in
alveolar lavage fluid. Eight percent to 12% of newborns and 3% to 7% of older children with
1
-AT deficiency
(PiZZ) present with cholestasis (23). Emphysema develops in all persons with null
1
-AT phenotypes by age 20
to 30 years. Although emphysema is due to uninhibited proteolytic destruction of the connective tissue matrix of
the lung, liver disease is believed to result from the toxic effects of the mutant
1
-AT molecule retained within
the endoplasmic reticulum of liver cells (24). The prognosis of patients with liver disease presenting in infancy
secondary to
1
-AT
P.1446
deficiency is variable; not all patients progress to end-stage liver disease.
Presenting symptoms of neonatal hepatic involvement can include jaundice, slow weight gain, irritability,
lethargy, acholic stools, or a bleeding diathesis. Later presentation can include abdominal distention,
hepatosplenomegaly, ascites, or an upper GI bleed secondary to esophageal varices. The initial treatment of the
patient with
1
-AT deficiency is symptomatic. It has been suggested that breastfeeding until the end of the first
year of life may decrease the manifestations of cholestatic liver disease, as may administration of
ursodeoxycholic acid. The importance of the use of fat-soluble vitamins, adequate nutrition, and counseling
regarding the avoidance of second-hand smoke cannot be overemphasized. Although treatment of
1
-AT
deficiency-associated liver disease is mostly supportive, orthotopic liver transplantation (OLT) has been
employed as a treatment for patients who have progressed to end-stage liver disease;
1
-AT deficiency is the
most common metabolic liver disease for which transplantation is performed. In addition to replacing the injured
organ, transplantation corrects the metabolic defect, thereby avoiding progression of systemic disease (25).
Glycogen Storage Disease
More than ten distinct disorders of glycogen metabolism have been described in the literature. The overall
incidence of glycogen storage disease (GSD) is estimated to range from 1 in 50,000 to 1 in 100,000. GSD type
I, resulting from the deficiency of glucose-6-phosphatase activity, is the most common of the errors in glycogen
metabolism. Most patients present in infancy with hypoglycemic seizures and growth failure. Physical signs
invariably include hepatomegaly (secondary to vastly increased glycogen storage), short stature, and adiposity.
These patients demonstrate mild elevations in serum aminotransferase levels, but generally do not progress to
cirrhosis or liver failure. By age 15, most patients develop hepatic adenomas, although adenomas have been
described in patients as young as 3 years of age.
Medical therapy includes a formula that does not contain fructose or galactose, with frequent daytime feedings
and continuous nocturnal administration (26). As solids are introduced, high-carbohydrate foods should be
emphasized. These patients require special attention during acute illnesses that may affect intake or metabolism
because they can become hypoglycemic quickly. Liver transplantation has successfully corrected the metabolic
error in patients with GSD type I and allowed catch-up growth, even into the third decade. As survival is
extended, these patients may demonstrate signs of other systemic complications, such as progressive kidney
http://gateway.ut.ovid.com/gw2/ovidweb.cgi (12 of 31)1/2/2006 10:18:21 PM
Ovid: Principles and Practice of Pediatric Surgery
disease, cardiovascular disease, and malignancy (27).
Tyrosinemia
There are four known human diseases involving enzymatic deficiencies in the catabolic pathway for the amino
acid tyrosine: alkaptonuria and hereditary tyrosinemia types I, II, and III. Only hereditary tyrosinemia type I
(HTI) leads to progressive liver dysfunction. HTI is an autosomal recessive-transmitted disease with a worldwide
incidence of about 1 in 100,000 (28). The enzymatic defect in patients with tyrosinemia has been identified as a
deficiency of fumarylacetate hydrolase (FAH). FAH deficiency leads to accumulation of the upstream metabolites
fumarylacetoacetate and maleylacetoacetate, which are then converted to the toxic intermediates
succinylacetoacetate and succinylacetone (SA). Patients with HTI can present acutely with liver failure or with
chronic disease and hepatocellular carcinoma. In the acute form, patients manifest liver disease in the first 6
months of life, with hypoglycemia, ascites, jaundice, and a bleeding diathesis. The acute form of HTI is usually
fatal within the first 2 years of life due to recurrent bleeding and liver failure (35 of 47 deaths); however,
hepatocellular carcinoma (7 of 47) and neurologic crisis (3 of 47) accounted for some deaths (29). Patients with
the chronic form of HTI classically show similar but milder symptoms, presenting after 1 year of age with
hepatomegaly, rickets, nephromegaly, and growth retardation. These patients also are likely to have neurologic
problems and hepatocellular carcinoma.
The diagnosis of tyrosinemia should be suspected in any child with neonatal liver disease or a bleeding diathesis
or in any child older than 1 year of age with undiagnosed liver disease or rickets. Elevated serum and urine
succinylacetone (SA) and urine -aminolevulinic acid (ALA) levels are regarded as pathognomonic for
tyrosinemia, although the diagnosis can be confirmed with an assay for FAH using lymphocytes, erythrocytes, or
liver tissue.
Historically, the treatment of tyrosinemia has been dietary management, based on the restriction of tyrosine and
phenylalanine. Dietary restriction has been shown to reverse the renal damage and improve the metabolic bone
disease; however, the liver disease progresses. Nevertheless, an adequate intake of these amino acids is
necessary to ensure normal growth and development. OLT has become a mainstay therapy for patients with
tyrosinemia (30).
Porphyrias
This diverse group of metabolic derangements stems from errors in the synthesis of heme, with many forms
associated with primary expression in the liver or direct hepatic toxicity. The porphyrias are usually classified
either by the site of major biochemical abnormality or by the clinical features. In five of the porphyrias, the liver
is the major site of expression, and in two others, both the liver and bone marrow are involved. The porphyrias
are divided clinically into those that are acute, with dramatic and
P.1447
potentially life-threatening neurologic symptoms, and those with only cutaneous symptoms.
The term acute porphyria refers to the nature of the neurologic attacks, which are recurrent, dramatic, and life
threatening. Abdominal pain is present in more than 90% of patients, followed in frequency by tachycardia and
dark urine in about 80% of patients (31). Acute intermittent porphyria is the most common of the acute
porphyrias, occurring in approximately 1 in 10,000 people, and in as many as 1 in 500 patients with psychiatric
disorders. Hepatic involvement is variable; elevated serum aminotransferase and bile acids levels may be seen,
and patients are at increased risk of developing hepatocellular carcinoma (32). The overall survival for patients
with acute porphyria is good. Treatment is based on avoidance of drugs and other precipitating factors.
Intravenous administration of hematin, a congener of heme, can have a dramatic effect on the neurologic
symptoms, especially if given early in an attack (33). OLT has been attempted for several of the porphyrias, with
mixed results (34).
http://gateway.ut.ovid.com/gw2/ovidweb.cgi (13 of 31)1/2/2006 10:18:21 PM
Ovid: Principles and Practice of Pediatric Surgery
Wilson's Disease
Wilson's disease, a disorder of copper metabolism, is a progressive neurologic disease with chronic liver disease
and a corneal abnormality, the Kayser-Fleischer ring. Wilson's disease is an autosomal recessive disorder
resulting from the dysfunction of a copper ATPase responsible for transporting copper into the secretory pathway
for incorporation into ceruloplasmin and excretion into the bile. The incidence is approximately 1 in 30,000. In
Wilson's disease, inadequate biliary copper excretion leads to copper accumulation in the liver, brain, kidney,
and cornea. Copper, a component of several essential enzymes, is toxic to tissues when present in excess.
The clinical presentation of Wilson's disease is extremely variable. The age at onset of symptoms is usually
between 5 and 35 years. The presentation may be as chronic or fulminant liver disease, a progressive neurologic
disorder without hepatic dysfunction, isolated acute hemolysis, or psychiatric illness. The hepatic presentation of
Wilson's disease is more common in children than in adult patients. Wilson's disease should be considered as a
possible diagnosis in any child with hepatomegaly, persistently elevated serum aminotransferase levels, or
evidence of fatty liver. Recurrent bouts of hemolysis may predispose to the development of gallstones, and thus
children with unexplained cholelithiasis should be tested for Wilson's disease. Unlike other types of chronic liver
disease, Wilson's disease is rarely complicated by hepatocellular carcinoma. In patients who have predominantly
hepatic disease, evidence of subtle neurologic involvement can often be found. Changes in school performance,
dexterity, and even handwriting may be seen. A soft whispery voice (hypophonia) is another early feature of
neurologic involvement.
Because a diagnosis of Wilson's disease has not usually been made, fulminant viral hepatitis is usually the
working diagnosis. Slit-lamp examination may reveal Kayser-Fleischer rings, copper deposition in Descemet's
membrane in the cornea; however, Kayser-Fleischer rings may be absent in 15% to 50% of patients with
exclusively hepatic involvement. The laboratory diagnosis of Wilson's disease is confirmed by decreased serum
ceruloplasmin, increased urinary copper content, and elevated hepatic copper concentration. Molecular genetic
analysis is complex because more than 100 unique mutations have been identified, and most individuals are
compound heterozygotes. These patients may respond to chelation treatment with penicillamine (35). For those
with irreversible liver failure, hepatic transplantation is curative.
Cystic Fibrosis
Liver disease can be the presenting symptom of cystic fibrosis (CF) in the newborn, and CF-associated liver
disease has been associated with meconium ileus syndrome (36). The diagnosis should be considered in any
infant with neonatal cholestasis, although only 2% of such patients have CF. Liver disease may become more
prevalent as the mean age of survival for patients with CF increases; however, liver involvement is not universal
and seems to peak during the adolescent years. The diagnosis of significant liver disease in this patient
population can be difficult because the presenting signs are subtle. Hepatomegaly, present in approximately
30% of patients, has been shown to correlate well with the presence of cirrhosis and is often the first finding of
liver disease. Liver biochemical test results may remain relatively normal despite histologic evidence of cirrhosis.
Treatment of patients with CF with ursodeoxycholic acid improves the biochemical indices of liver injury;
however, conclusive evidence that the drug halts the progression to cirrhosis is not yet available (37).
Portosystemic shunts can be effective treatment for patients with PH. Liver transplantation has been performed
successfully for patients with decompensating liver and stable pulmonary function (38).
VIRAL HEPATITIS
Six viruses have been identified that produce liver disease as their major clinical manifestation: five are RNA
viruses (hepatitis A, C, D, E, and G) and hepatitis B is a DNA virus.
Hepatitis A Virus
Hepatitis A virus (HAV) is an RNA virus that infects per the oral route. Once absorbed in the intestine, the virus
reaches the liver, where replication takes place in the hepatocyte cytoplasm. Antigenic detection is possible 1 to
http://gateway.ut.ovid.com/gw2/ovidweb.cgi (14 of 31)1/2/2006 10:18:21 PM
Ovid: Principles and Practice of Pediatric Surgery
2 weeks after inoculation and persists up to 8 weeks. New
P.1448
virions are excreted via bile to the intestine, where it is shed into the stool in high titers. Because it is relatively
resistant to degradation by environmental conditions, the virus is spread easily within a population, with a very
high attack rate (80% of those exposed become infected).
HAV results in acute infection only, and the clinical spectrum of disease ranges from silent asymptomatic
infection to fulminant hepatitis. Prodromal symptoms include fatigue and weakness, anorexia, nausea and
vomiting, and abdominal pain. The development of jaundice and dark urine occurs within 1 to 2 weeks of the
onset of prodromal symptoms, although anicteric infections are three times more likely than icteric infections in
children (39). Although more than 90% of children younger than the age of 5 are asymptomatic, 70% to 80% of
adults are symptomatic. Overall, HAV is typically a benign, self-limited infection, with the majority of patients
exhibiting complete recovery within 2 months of the onset of disease.
Hepatitis B Virus
Hepatitis B virus (HBV) is a partially double-stranded DNA that is predominantly hepatotropic. In contrast to
classical retroviruses such as HIV, HBV transcripts are synthesized entirely from episomal DNA. Integration of
HBV DNA does occur in chronic infection and may be important for hepatic carcinogenesis. In the United States,
approximately 1.25 million people are chronically infected with HBV and spread of infection is predominantly by
horizontal routes. Adults and adolescents are at greatest risk of infection in the United States because of
acquisition from sexual activity, injection drug use, and blood transfusion (40). Although only 1% to 3% of all
reported cases of HBV infection in the United States are believed to occur in children, 20% to 30% of all chronic
HBV infections in the United States occur in children younger than age 5 years. Infants born to HBeAg-positive
mothers with high viral loads have an 80% risk of perinatal acquisition in the absence of interventions.
Interestingly, children of HBsAg-positive mothers who are not infected at birth remain at high risk, as 60%
become infected by the age of 5 years (41). The mechanism of this later infection is unknown, although
breastfeeding is not believed to be an important mode of transmission.
Clinical observations suggest that the immune response of the host is more important than viral factors in the
pathogenesis of liver injury caused by HBV. For instance, infants with immature immune systems who acquire
HBV infection at birth typically have only mild liver injury. Conversely, HBV-induced fulminant hepatic failure is
associated with a vigorous immune response, low serum levels of virus, and massive hepatocellular necrosis.
The incubation period of hepatitis B varies from 16 months. Clinical presentation varies from asymptomatic
infection to liver failure.
Current serologic assays for the diagnosis of acute and chronic HBV infection are both sensitive and specific. In
acute infection, HbsAg, indicating active HBV infection, becomes detectable approximately 6 weeks after
inoculation, before the onset of clinical symptoms or biochemical abnormalities. Biochemical abnormalities
usually coincide with the prodromal phase of the acute illness and may persist for several months. The serum
ALT level is typically higher than the serum AST level, and levels of both aminotransferases are usually 500 U
per L or greater. Bilirubin elevations are usually modest (5 to 10 mg per dL). With the onset of symptoms, IgM
anti-HBc becomes detectable. IgM anti-HBc may persist for many months, and IgG anti-HBc may persist for
many years, if not a lifetime. Anti-HBs is the last serologic test to become positive and is a marker of resolving
infection.
Treatment of acute HBV infection is largely supportive. The most profound complication of acute HBV infection is
fulminant hepatic failure, defined as the onset of hepatic encephalopathy within 8 weeks of the onset of
symptoms. Although this complication is infrequent (occurring in less than 1% of cases), the prognosis is poor.
If clinical symptoms of hepatic failure develop, patients should be referred for consideration of liver
transplantation. Chronic HBV infection is usually defined as detectable HPV surface antigenemia for a period of 6
months or more. The risk of chronicity after neonatally acquired infection is extremely high (up to 90%), and the
risk of developing hepatocellular carcinoma (HCC) is markedly increased in those patients. Patients with chronic
HBV appear to derive long-term benefit from interferon (42), although patients with PH, variceal bleeding, or
http://gateway.ut.ovid.com/gw2/ovidweb.cgi (15 of 31)1/2/2006 10:18:21 PM
Ovid: Principles and Practice of Pediatric Surgery
hepatorenal syndrome should be referred for liver transplantation. Because of many improvements in the
treatment of HPV after transplantation, orthotopic liver transplantation is now the standard of care for patients
with decompensated HBV-induced liver disease (43).
Hepatitis C Virus
Hepatitis C virus (HCV) is an important public health problem because it is a major cause of chronic hepatitis,
cirrhosis, and HCC. The most striking feature of this virus is its ability to induce persistent infection in at least
85% of infected persons, despite a vigorous humoral and cellular host immune response. HCV is a single-
stranded RNA virus. Its modes of transmission can be divided into percutaneous (blood transfusion and needle
stick inoculation) and nonpercutaneous (sexual contact, perinatal exposure). Perinatal transmission occurs
exclusively from mothers who are HCV RNA positive at the time of delivery (44); the risk posed to the infant
from breastfeeding is minimal. In contrast to the high efficiency of perinatal transmission of HBV, the efficiency
of perinatal transmission of HCV is low (0% to 10%).
Acute infection is rarely seen in clinical practice because the majority of patients experience no clinical
symptoms. Jaundice may develop in 25% of these patients, whereas
P.1449
10% to 20% may present with nonspecific symptoms such as fatigue, nausea, and vomiting. Infection with HCV,
once established, persists in the vast majority of patients. Disease progression is largely silent, and patients
often are identified only on routine biochemical screening or blood assay.
The primary goal of therapy for HCV infection is to eradicate the infection early in the course of the disease to
prevent progression to end-stage liver disease and eventually to HCC. Interferon-based regimens constitute
the cornerstone of current antiviral therapies (42). Several trials have shown that treatment with a combination
of interferon- plus ribavirin (an oral antiviral agent with activity against DNA and RNA viruses) results in a
higher frequency of sustained biochemical and virologic response than does treatment with interferon alone
(45). New formulations of interferon, pegylated interferons, have been developed more recently, which are able
to sustain more uniform plasma levels and consequently enhance viral suppression (46,47).
PORTAL HYPERTENSION AND VARICEAL BLEEDING
PH, defined as an elevation of portal pressure higher than 10 to 12 mm Hg, is a major cause of morbidity and
mortality in children with liver disease. Although there have been considerable advances in treatment since the
mid-1990s, the complications of PHGI hemorrhage, ascites, and encephalopathycontinue to pose difficult
challenges.
Etiology
The causes of PH are conventionally classified according to the localization of the site of maximal resistance to
portal flow. The three major categories of PH are prehepatic, intrahepatic, and posthepatic. Portal vein
obstruction is the major cause of prehepatic PH in childhood. Umbilical infection secondary to umbilical vein
catherization spreads to the left branch of the portal vein, which then leads to formation of thrombus in the
portal vein. Fibroblasts transform the clot into a firm, collagenous plug in which tortuous venous channels
develop, the so-called cavernous transformation. Pressure rises in the portal vein remnant, transforming usually
small venous collaterals into esophageal, gastric, duodenal, and jejunal varices. Portal vein thrombosis has also
been associated with neonatal dehydration, intraabdominal infections, inflammatory bowel disease, sclerosing
cholangitis, and hypercoagulable states, such as factor V Leiden deficiency or protein C and protein S
deficiencies. At least one-half of reported cases have no defined cause.
The intrahepatic causes of PH are numerous, with the site of resistance conventionally divided into presinusoidal,
sinusoidal, and postsinusoidal. Presinusoidal hypertension can be caused by increased flow, as a result of an
arteriovenous fistula or by obstruction to flow, as in congenital hepatic fibrosis. Cirrhosis is the predominant
http://gateway.ut.ovid.com/gw2/ovidweb.cgi (16 of 31)1/2/2006 10:18:21 PM
Ovid: Principles and Practice of Pediatric Surgery
cause of sinusoidal PH and is related to obstruction of blood through the portal vein. There are numerous causes
of childhood cirrhosis, including BA, 1-AT deficiency, Wilson's disease, GSD, and CF.
Postsinusoidal causes also occur in childhood. The Budd-Chiari syndrome involves obstruction to hepatic vein
drainage, and can occur anywhere between the efferent hepatic veins and the right atrium. Venoocclusive
disease seen after total body irradiation and/or chemotherapy is the most frequent cause of hepatic vein
obstruction in children.
Pathophysiology
The initial hemodynamic abnormality in PH is increased resistance to portal blood flow. Curiously, despite the
development of significant collaterals diverting portal blood into systemic veins, increased portal pressures are
maintained by an overall increase in portal venous flow. Clinically, a hyperdynamic circulation is achieved by
tachycardia, an increase in cardiac output, and decreased systemic vascular resistance. The increase in portal
blood flow is related to the contribution of hepatic and collateral flow; the actual portal blood flow reaching the
liver is reduced.
Normal, uncorrected pressure in the portal vein ranges from 5 to 10 mm Hg. Portal pressure is usually
expressed as a portal pressure gradient (P) and is most often determined in patients with cirrhosis as the
hepatic venous pressure gradient (HVPG). A pressure measurement is made via a catheter wedged into a
hepatic vein; this measurement is termed the wedged hepatic venous pressure (WHVP). After withdrawal of the
catheter tip into the hepatic vein, a free hepatic vein pressure (FHVP) is obtained. The HVPG is obtained by
subtracting the value of the WHVP from the FHVP.
Anatomic Sites of Collateral Formation
Spontaneous portosystemic collaterals develop in a number of anatomic sites: (1) squamocolumnar junctions of
the GI tract, (2) recanalized umbilical vein, (3) retroperitoneum, (4) and sites of previous abdominal surgery or
intraabdominal trauma (Fig. 90-3). Esophageal varices are the most important site of bleeding in PH and are
supplied mainly by an enlarged coronary (left gastric) vein and the short gastric veins. They generally achieve
their greatest prominence 2 to 3 cm above the gastroesophageal junction and in time may extend cephalad to
the midesophagus. The next most common site for the formation of clinically significant varices is the stomach,
either in obvious continuity with esophageal varices or as free-standing gastric varices. These superficial
submucosal collaterals are prone to rupture and bleed. In addition to varices, the vascularity of the stomach is
also abnormal, demonstrating prominent
P.1450
submucosal arteriovenous communications. The resulting vascular ectasia has been called congestive
gastropathy and contributes to a significant risk of bleeding from the stomach.
http://gateway.ut.ovid.com/gw2/ovidweb.cgi (17 of 31)1/2/2006 10:18:21 PM
Ovid: Principles and Practice of Pediatric Surgery
FI GURE 90- 3. Potential venous collaterals that develop with portal hypertension. The veins of Sappey drain
portal blood through the base areas of the diaphragm and through paraumbilical vein collaterals to the
umbilicus. The veins of Retzius form in the retroperitoneum and shunt portal blood from the bowel and other
organs to the vena cava. (From Marvin MR, Emond JC. Cirrhosis and portal hypertension. In: Greenfield LJ,
Mulholland MW, Oldham KT, et al., eds. Surgery: scientific principles and practice, 3rd ed. Philadelphia:
Lippincott Williams & Wilkins, 2001, with permission.)
Diagnosis
Children with PH, regardless of the underlying cause, may have recurrent bouts of life-threatening hemorrhage.
Variceal bleeding accounts for approximately one-fifth to one-third of all deaths in cirrhotic patients. The most
important determinant of survival is the patient's level of hepatic function; prognosis is generally much better in
patients without significant liver impairment, such as those with portal vein thrombosis.
Physical examination may show hepatomegaly, jaundice, palmar erythema, ascites, and periumbilical
vascularity, a caput medusae. However, GI bleeding, either as melena or hematemesis, is the most frequent
manifestation of PH.
Doppler flow ultrasonography can demonstrate the patency of the portal vein and flow within the portal system,
in addition to detecting the presence of esophageal varices. An upper GI can also diagnose esophageal varices.
Selective arteriography of the celiac axis, superior mesenteric artery, and splenic vein can map the involved
vascular anatomy and measure portal pressure. However, endoscopy is the most reliable method for detecting
esophageal varices. Endoscopy is undertaken after initial hemodynamic resuscitation and is essential for the
precise diagnosis because only 60% to 80% of bleeding episodes in these patients are from esophageal varices.
Once a diagnosis of PH has been established, several endoscopic features of esophageal varices may predict a
risk for
P.1451
hemorrhage: variceal size and the presence of so-called red signs. Red signs, including cherry red spots and red
wale markings (longitudinal, raised, red streaks), are usually associated with the most advanced grade of
http://gateway.ut.ovid.com/gw2/ovidweb.cgi (18 of 31)1/2/2006 10:18:21 PM
Ovid: Principles and Practice of Pediatric Surgery
varices and are believed to represent focal weaknesses in the variceal wall (48).
Treatment
The management of children with PH has substantially changed more recently, owing to the good results and
broader application of both endoscopic sclerotherapy and orthotopic liver transplantation (49). The therapy of PH
consists of emergency treatment of potentially life-threatening hemorrhage and prophylaxis directed at
prevention of initial or subsequent bleeding. Prompt and appropriate hemodynamic resuscitation should be
followed by implementation of measures aimed at arresting and preventing the recurrence of bleeding. The
major therapies available for the achievement of these goals rely on one of two fundamental approaches:
lowering of portal pressure or local obliteration of the varices.
Treatment of patients with variceal hemorrhage must initially focus on fluid resuscitation and blood transfusion,
as needed. Correction of coagulopathy by administration of vitamin K, platelets, or fresh frozen plasma
transfusion is essential. A nasogastric tube should be placed to document the presence of blood within the
stomach and to monitor for ongoing bleeding. An H
2
receptor blocker such as ranitidine should be given
intravenously to reduce the risk of bleeding from gastric erosions.
Pharmacologic therapy to decrease portal pressure may be considered in patients who do not stop bleeding
spontaneously. Propanolol has been used to directly decrease portal pressures. Vasopressin or one of its analogs
is commonly used, due to its ability to increase splanchnic vascular tone and thus decrease portal blood flow.
Vasopressin is administered initially with a bolus of 0.33 U per kg followed by a continued infusion, but its use is
occasionally limited by its vasoconstrictive side effects. The somatostatin analog octreotide decreases splanchnic
blood flow with fewer side effects. Although studies in adults are promising, its use and efficacy in children have
not been well evaluated.
Balloon tamponade, using Sengstaken-Blakemore or Minnesota tubes, has been used for many years to diminish
variceal flow and control bleeding by compressing the varices. These balloons can control active bleeding in
more than 90% of cases. However, there is a high rate of rebleeding when the balloon is deflated, and thus
balloon tamponade is considered a temporizing measure in patients who have active, life-threatening
hemorrhage. Other potential serious complications include esophageal perforation and aspiration pneumonia.
Thus, patients should be intubated for airway protection before insertion of the tube, and the position of the
gastric balloon should be confirmed radiographically before being fully inflated.
Endoscopy is the cornerstone of the management of GI hemorrhage, as both a diagnostic and a therapeutic
modality. Treatment options include injection sclerotherapy and variceal band ligation (50). Injections may be
directed into the veins (intravariceal injection) or adjacent to the variceal channels (paravariceal injection);
different sclerosants are available, including 5% sodium morrhuate, 1% to 3% sodium tetradecyl sulfate, 5%
ethanolamine oleate, and absolute alcohol. Although bleeding may be controlled acutely in most cases, further
sessions of sclerotherapy are required and treatments can be associated with further bleeding, esophageal
ulceration, and stricture formation. These complications led to the development of an alternative endoscopic
therapy referred to as variceal banding, based on the principles of hemorrhoidal banding. However, the use of
banding in the actively bleeding patient is a technically challenging procedure and experience with the technique
in children is limited.
Until the early 1980s, the treatment of choice of bleeding esophageal varices was based on two main types of
open surgery: portosystemic shunts and devascularization procedures (49,51,52,53). Shunt operations have
traditionally been classified as total, partial, or selective, on the basis of their intended impact on portal blood
flow. Total shunts divert all portal blood flow into the inferior vena cava; end-to-side portacaval shunt is the best
example. The side-to-side portacaval shunt differed in that theoretically only part of the portal stream was
diverted into the vena cava. However, in reality, not only did the side-to-side portacaval shunt allow total
diversion of portal blood flow, but it also facilitated diversion of part of the hepatic arterial blood backward into
the vena cava, leading to hepatic encephalopathy and liver failure. Other nonselective shunts have used large
diameter portacaval prosthetic H grafts, small diameter grafts, and mesocaval shunts. Selective shunts, a shunt
http://gateway.ut.ovid.com/gw2/ovidweb.cgi (19 of 31)1/2/2006 10:18:21 PM
Ovid: Principles and Practice of Pediatric Surgery
engineered to decompress variceal flow while preserving prograde portal blood flow, were designed to avoid the
encephalopathy seen with total shunts. The Warren or distal splenorenal shunt, the best example of a selective
shunt, decompresses varices through the splenic vein to the left renal vein and disconnects other potential
portosystemic connections (Fig. 90-4). This procedure yielded good results in children, even when applied in
toddlers (49,54). Direct surgical devascularization of the varices offers the potential for control of bleeding
without the shunt-related complication of encephalopathy and can be applied when the anatomy is unfavorable
for a shunt. Improved long-term control of bleeding has been reported with the Sugiura operation, a more
extensive procedure consisting of transthoracic paraesophageal devascularization, esophageal transection,
splenectomy, esophagogastric devascularization, pyloroplasty, and vagotomy (53). However, since the
introduction of
P.1452
sclerotherapy for the treatment of bleeding esophageal varices, the number of surgical procedures has sharply
decreased.
FI GURE 90- 4. Distal splenorenal Warren shunt. The splenic vein is divided near its junction with the superior
mesenteric vein. The distal end of the splenic vein is anastomosed to the renal vein. Varices are selectively
decompressed through the stomach and short gastric veins into the splenic vein and then into the vena cava
through the renal vein. Portal hypertension is maintained in the portal and superior mesenteric veins to provide
enough pressure to drive portal blood through the diseased liver. (From Marvin MR, Emond JC. Cirrhosis and
portal hypertension. In: Greenfield LJ, Mulholland MW, Oldham KT, et al., eds. Surgery: scientific principles and
practice, 3rd ed. Philadelphia: Lippincott Williams & Wilkins, 2001, with permission.)
As noted previously, all surgical options have the potential for significant morbidity and mortality. Attempts to
devise a less invasive approach to portal decompression led to the development of a nonsurgical shunt, the
transjugular intrahepatic portosystemic shunt (TIPS) (Fig. 90-5). TIPS is a percutaneous method of creating a
http://gateway.ut.ovid.com/gw2/ovidweb.cgi (20 of 31)1/2/2006 10:18:21 PM
Ovid: Principles and Practice of Pediatric Surgery
side-to-side portacaval shunt by the deployment of an expandable metallic stent placed by an interventional
radiologist (55). The potential advantages of this technique include avoidance of general anesthesia, decreased
procedural morbidity and mortality rates, and avoidance of surgery in the region of the hepatic hilum, which
may be important in potential liver transplantation candidates. However, the TIPS procedure is prone to
thrombosis, particularly in younger children, and may precipitate the hepatic arterial steal phenomenon known
to cause hepatic encephalopathy.
Orthotopic liver transplantation represents the definite therapy for PH (56,57). A prior portosystemic shunting
operation does not preclude a successful liver transplantation, although it does make the operation technically
more difficult. However, liver transplantation is expensive, requires lifelong immunosuppression, and is limited
by a significant donor shortage. Thus, there remains the need for managing PH in patients who are awaiting
transplantation or who are not considered transplantation candidates.
ASCITES AND SPONTANEOUS BACTERIAL PERITONITIS
Ascites
Ascites is an accumulation of serous fluid within the peritoneal cavity. There are multiple causes of ascites;
hepatic, renal, and cardiac disease are the most common causes in children (Table 90-3). The clinical hallmark
of ascites is abdominal distention, although considerable intraperitoneal fluid may accumulate before ascites is
detectable by the classic physical signs of bulging flanks, shifting dullness, and a fluid wave. The course,
prognosis, and treatment of ascites depend entirely on the cause. Patients with any type of ascites are at
increased risk for spontaneous bacterial peritonitis.
Chylous ascites can result from obstruction or injury to the intraabdominal portion of the lymphatic system.
Causes include lymphangiomatosis, congenital malformations, tumors, enlarged lymph nodes, previous
abdominal surgery, or trauma. Because of loss of serum proteins (and thus oncotic pressure), not only will the
child present with abdominal distension, but he or she may also have
P.1453
P.1454
peripheral edema. Diagnosis of chylous ascites depends on paracentesis. If the patient has not eaten, the fluid
will appear serous; however, if the child has recently had a fat-containing meal, it will be milky. Fluid analysis
will disclose a high cell count that is predominantly lymphocytic, an elevated triglyceride level, and high protein
content. Serum hypoalbuminemia and lymphopenia are commonly seen. Treatment includes feedings of a high-
protein, low-fat diet supplemented with medium-chain triglycerides (absorbed directly into the portal
circulation). Parenteral alimentation may be necessary to decrease lymph flow to facilitate sealing of the leak.
Laparotomy may be indicated to search for the site of the leak if a trial of dietary management has been
unsuccessful, particularly in cases secondary to trauma or previous surgery.
http://gateway.ut.ovid.com/gw2/ovidweb.cgi (21 of 31)1/2/2006 10:18:21 PM
Ovid: Principles and Practice of Pediatric Surgery
FI GURE 90- 5. Schematic representation of the creation of a transjugular intrahepatic portosystemic shunt.
(A) Needle is advanced from supraheptic vena cava into portal vein using fluoroscopy. (B) Wire is advanced
through needle into the superior mesenteric vein. (C) The tract between hepatic and portal vein is dilated with
andioplasty balloon catheter. (D) Balloon-expandable stents are placed in the tract between hepatic and portal
vein. (E) Final appearance of stent, with intrahepatic shunt from portal vein to hepatic vein. (From Zemel G,
Katzen BT, Becker GJ, et al. Percutaneous transjugular portosystemic shunt. JAMA 1991;266:390, with
permission.)
TABLE 90-3 Causes of Childhood Ascites.
http://gateway.ut.ovid.com/gw2/ovidweb.cgi (22 of 31)1/2/2006 10:18:21 PM
Ovid: Principles and Practice of Pediatric Surgery
Serous ascites
Cirrhosis
Nephrosis
Right-sided heart failure
Budd-Chiari syndrome
Postop (venous pressure shunt, peritoneal dialysis)
Biliary ascites
Neonatal bile duct perforation
Hepatitis
Cystic fibrosis
Chylous ascites
Malrotation with volvulus
Lymphangioma
Small bowel obstruction
Trauma
Urinary ascites
Posterior urethral valves
Bladder perforation
Ureterocele
Pancreatic ascites
Acute pancreatitis
Pancreatic pseudocyst
Ovarian ascites
Cyst (torsion, rupture)
Tumors
Malignant ascites
Any intraperitoneal neoplasm
The presence of ascites in conjunction with palmar erythema and/or abdominal wall collateral veins is suggestive
of parenchymal liver disease. In ascites secondary to liver disease, vasopressin, renin-aldosterone, and
sympathetic nervous systems are activated (58,59). These changes lead to renal vasoconstriction and
subsequent sodium and water retention. Fluid then weeps from the congested hepatic sinusoids as ascites.
The mainstay of therapy for children with cirrhotic ascites is dietary sodium restriction and diuretics. Fluid loss
and weight change are related directly to sodium balance. In the presence of avid renal retention of sodium,
sodium intake is limited to 1 to 2 mEq per kg per day. Aggressive restriction of fluid is inappropriate, except for
patients with severe hyponatremia. Diuresis may be maintained by the use of agents such as furosemide alone
or in combination with spironolactone (3 to 5 mg per kg day in four doses). Importantly, patients with ascites
without peripheral edema are at risk for reduced plasma volume, and thus diuretic doses and dietary sodium
intake must be carefully adjusted to achieve weight loss and negative sodium balance.
Refractory ascites is defined as ascites unresponsive to a sodium-restricted diet and high-dose diuretic
treatment. Refractoriness may be manifested by minimal weight loss despite diuretics, diuretic complications, or
the development of tense ascites (60). Tense ascites alters renal blood flow and systemic hemodynamics, and
requires urgent therapy. In the 1960s, portacaval shunts were used to treat refractory ascites, but operative
hemorrhagic complications and portosystemic encephalopathy led to the abandonment of this approach.
Presently, treatment options for refractory ascites include serial therapeutic paracenteses, peritoneovenous
shunts, TIPS, and liver transplantation. Large-volume paracentesis and intravenous albumin infusion may
improve hemodynamics, renal perfusion, and symptoms (61). TIPS is now considered the second-line treatment
for these patients (62,63,64). A more recent randomized trial in diuretic-resistant patients has demonstrated a
survival advantage for TIPS compared with serial paracenteses (65). Although there was initial enthusiasm for
peritoneovenous shunting, high complication and failure rates, as well as randomized trials demonstrating no
survival advantage, have led to the relegation of this procedure to third-line therapy. Finally, for patients with no
psychosocial or medical contraindications, evaluation for liver transplantation is essential once ascites has
become diuretic resistant.
Spontaneous Bacterial Peritonitis
http://gateway.ut.ovid.com/gw2/ovidweb.cgi (23 of 31)1/2/2006 10:18:21 PM
Ovid: Principles and Practice of Pediatric Surgery
Spontaneous bacterial peritonitis (SBP) is the most common cause of inflammation of ascitic fluid. Spontaneous
forms of ascitic fluid infection are believed to be the result of overgrowth of a specific organism in the gut,
translocation of that microbe from the gut to mesenteric lymph nodes, and resulting spontaneous bacteremia
and subsequent colonization of susceptible ascitic fluid (66). The diagnosis of SBP is made when there is a
positive ascitic fluid culture and an elevated ascitic fluid absolute polymorphonucleocyte count, without evidence
of an intraabdominal surgically treatable source of infection. The most common bacterial infection of ascitic fluid
is monomicrobial, with a low bacterial concentration (median colony count of only 1 organism per milliliter).
Thus, the decision to begin empiric antibiotic treatment is not
P.1455
routinely based on culture, but on the cell count and differential.
Although SBP is approximately six times as common as surgical peritonitis in a patient with ascites, secondary
peritonitis should be considered in any patient with neutrocytic ascites because clinical symptoms and signs will
not distinguish between them. Ascitic fluid total protein, glucose, and LDH can be of some value in distinguishing
SBP from intestinal perforation. Patients who meet two of the following three criteria are likely to have surgical
peritonitis: total protein greater than 1 g per dL, glucose less than 50 mg per dL, and LDH greater than the
upper limit of normal for serum. The most apparent difference between the spontaneous forms of ascitic fluid
infection and the secondary forms is that the former are always monomicrobial and the latter are usually
polymicrobial.
Escherichia coli, streptococci (mostly pneumococci), and Klebsiella cause most episodes of SBP. Timely diagnosis
requires a high index of suspicion and a low threshold for performing a paracentesis because the symptoms and
signs of infection are often subtle. A slight change in mental status, fever, or abdominal pain in a patient with
ascites should raise the suspicion of infection and prompt a paracentesis. Cefotaxime or a similar third-
generation cephalosporin appears to be the treatment of choice for suspected SBP. Anaerobic coverage is not
needed, nor is coverage for Pseudomonas or Staphylococcus. Less than 5% of patients die of infection if
appropriate antibiotics are administered in a timely fashion. However, spontaneous ascitic fluid infection is a
good marker of end-stage liver disease and has been proposed as an indication for liver transplantation.
ACUTE LIVER FAILURE
Acute liver failure (ALF) arises from loss of hepatic parenchyma or severe functional impairment that may result
from a variety of insults to the liver. ALF has been defined by three criteria: (1) rapid development of
hepatocellular dysfunction, (2) encephalopathy, and (3) absence of a prior liver disease. The clinical features of
ALF result directly from loss of critical hepatocellular functions (protein synthesis, intermediary metabolism, and
detoxification). The disorder usually evolves over a very short period.
Etiology
ALF is a rare condition in the pediatric population. Patients who present with severe failure of liver synthetic
function have a high mortality with medical therapy alone. The main causes of death are cerebral edema,
hemorrhage, renal failure, and sepsis. The etiology of ALF is age specific, with a significant number due to
inborn errors of metabolism, especially in neonates and infants. Treatment of children with ALF is supportive,
aimed at preventing and managing associated complications until the native liver recovers or until liver
transplantation. Sedation should not be administered unless a decision for artificial ventilation has been made.
Because all children are potential transplant candidates, transfer to and management in a liver transplant centre
is recommended. Prognostic criteria for mortality are less well defined compared with the adult population,
although a significantly elevated international normalized ratio (INR) greater than or equal to 4 carries a high
chance of death, and liver transplantation should be considered at this stage. Auxiliary transplantation is an
attractive option in selected individuals and provides the chance to stop immunosuppression if sufficient hepatic
regeneration occurs. The use of various liver assist devices and hepatocyte transplantation as a bridge to liver
transplantation show promise, although when used in isolation, they do not have an impact on overall patient
survival (67).
http://gateway.ut.ovid.com/gw2/ovidweb.cgi (24 of 31)1/2/2006 10:18:21 PM
Ovid: Principles and Practice of Pediatric Surgery
Fulminant hepatic failure is most commonly a complication of viral hepatitis, and there is a high risk of fulminant
hepatic failure in young people with combined hepatitis B and D infections. A large number of other viruses,
including but not exclusively Epstein-Barr virus, adenovirus, and cytomegalovirus, may produce fulminant
hepatitis in children. Various hepatotoxic drugs and chemicals may also cause acute fulminant hepatic failure.
Acetaminophen is directly hepatotoxic and predictably produces hepatocellular necrosis with an overdose. Even
recommended therapeutic dosages of acetaminophen can sometimes result in ALF in patients who are fasting or
who chronically use alcohol or drugs that induce cytochrome oxidases. Predictable liver injury may occur after
exposure to Amanita mushrooms or carbon tetrachloride. Idiosyncratic damage may follow the use of drugs such
as halothane or sodium valproate. Ischemia and hypoxia may produce liver failure. A large number of metabolic
disorders can rarely be associated with hepatic failure, including Wilson's disease, galactosemia, tyrosinemia,
neonatal iron storage disease, and deficiencies of mitochondrial electron transport.
The mechanisms that lead to fulminant hepatic failure are poorly understood. It is unknown why only about 1%
to 2% of patients with viral hepatitis experience liver failure, but it is speculated that a hyperimmune response
to the virus underlies the massive liver necrosis. Whatever the initial cause of hepatocyte injury, various factors
may contribute to the pathogenesis of liver failure, including impaired hepatocyte regeneration, endotoxemia,
and decreased hepatic reticuloendothelial function.
Clinical Presentation
The initial presentation of ALF may include nonspecific complaints such as nausea, vomiting, and fatigue.
However, hepatocellular injury soon leads to impaired elimination of bilirubin, depressed synthesis of coagulation
P.1456
factors (I, II, V, VII, IX, and X), diminished glucose synthesis, and increased lactate levels. Coagulopathy
increases the risk of GI and intracranial hemorrhage, hypoglycemia contributes to brain injury, and acidosis can
produce cardiovascular dysfunction.
Encephalopathy is a defining criterion for ALF. In infants, irritability, poor feeding, and a change in sleep rhythm
may be the only findings. Patients are often somnolent or combative on arousal, and may rapidly progress to
deeper stages of coma in which extensor responses and decerebrate and decorticate posturing appear. A staging
system has been developed to help monitor change and identify potential transplantation candidates. This
system consists of stage 1subtle changes in affect, stage 2drowsiness and asterixis, stage 3marked
somnolence and extensor reflex rigidity, and stage 4frank coma. Progressive cerebral edema will produce
intracranial hypertension, which can impair cerebral perfusion, leading to irreversible neurologic damage or even
uncal herniation and death.
Infections develop in as many as 80% of patients with ALF, and respiratory failure and renal failure are
commonly associated with ALF. A potential consequence of ALF is the syndrome of multiple organ failure, which
manifests clinically as hypotension, pulmonary edema, acute tubular necrosis, and disseminated intravascular
coagulation. Multiple organ failure is a significant contributor to patient mortality.
Laboratory Findings
Initially, serum aminotransferase activities may be markedly elevated, followed by elevation of the direct and
indirect bilirubin levels. The blood ammonia concentration is usually increased, and PT is always prolonged and
often does not improve after parenteral administration of vitamin K. Hypoglycemia can occur, particularly in
infants, as can metabolic acidosis or respiratory alkalosis. Liver biopsy reveals confluent massive necrosis of
hepatocytes. Bridging necrosis may be seen, and a particular zonal pattern of necrosis may be observed with
certain insults (e.g., centrilobular damage is associated with acetaminophen hepatotoxicity or with circulatory
shock).
Treatment
http://gateway.ut.ovid.com/gw2/ovidweb.cgi (25 of 31)1/2/2006 10:18:21 PM
Ovid: Principles and Practice of Pediatric Surgery
Patients with ALF fall into two broad categories: (1) those in whom intensive medical care enables recovery of
hepatic function, and (2) those who require liver transplantation to survive. Thus, it is critical to rapidly
determine to which group a particular patient belongs. The following characteristics have been demonstrated to
be associated with a poor outcome: negative serology for hepatitis A or B, younger age (younger than 10 years)
or older age (older than 40 years), markedly elevated serum bilirubin level, marked prolongation of the
prothrombin time, acidosis, and an elevated serum creatinine level. Among patients with a cause of ALF other
than acetaminophen toxicity, the presence of any single adverse prognostic characteristic was associated with a
mortality rate of 80%, and the presence of three adverse characteristics was associated with a mortality rate of
more than 95%. Because these mortality rates vastly exceed those associated with liver transplantation, the
presence of any single indicator of a poor prognosis should prompt serious consideration for liver transplantation.
The initial management of ALF should include an attempt to identify the cause of ALF because a small number of
causes of ALF can be treated specifically. For example, acetaminophen toxicity can be treated with N-
acetylcysteine, and herpes-induced fulminant hepatitis has been reported to respond to intravenous acyclovir.
Otherwise, management of fulminant hepatic failure is supportive because no therapy is known to reverse
hepatocyte injury or to promote hepatic regeneration. Intensive medical care is warranted in all patients with
ALF. Patients with profound encephalopathy (i.e., stage 3 and stage 4) should undergo endotracheal intubation
to prevent aspiration, to reduce cerebral edema by hyperventilation, and to facilitate pulmonary toilet.
Intracranial pressure monitoring and treatment with osmotherapy and barbiturates are two options for treating
intracranial hypertension, although cerebral edema is an extremely serious complication that responds poorly to
those measures. GI hemorrhage, infection, and hypovolemia may precipitate encephalopathy and should be
identified and corrected. Protein intake should be restricted or eliminated. Lactulose should be given every 2 to 4
hr orally or by nasogastric tube in doses (10 to 50 mL) sufficient to cause diarrhea. Oral or rectal administration
of a nonabsorbable antibiotic such as neomycin may reduce enteric bacteria responsible for ammonia
production. Because clinical recognition of infection may be difficult, surveillance cultures in patients with ALF
are extremely helpful. If renal failure is present, measurement of central pressures provides a direct guide to
fluid therapy. Because patients with ALF have a propensity to develop adult respiratory distress syndrome, early
measurement of central venous or pulmonary arterial pressure in oliguric patients is preferable to empiric
administration of fluid boluses. If oliguria persists in the face of adequate central filling pressures, continuous
arteriovenous hemofiltration should be initiated.
Liver transplantation has improved the outcome for some patients with ALF. Before the era of liver
transplantation, less than one-half of patients with ALF survived. In contrast, survival rates for patients with ALF
who undergo liver transplantation have been substantially higher, with an overall survival rate greater than 70%
in some centers. Reduced-size allografts and living donor transplantation have been important advances in the
treatment of infants
P.1457
with hepatic failure (68). Partial auxiliary orthotopic or heterotopic liver transplantation has also been successful
in a small number of children, allowing regeneration of the native liver and eventual withdrawal of
immunosupression. However, transplantation is not always successful. In one series, patients who presented
with multisystem organ failure had 100% mortality rate, despite liver transplantation (69). Another series noted
that ALF during the first year of life is a severe condition with poor prognosis, despite the advent of liver
transplantation (70). Many patients with irreversible ALF never have the chance to undergo transplantation
because of medical contraindications or the unavailability of donor livers. More recent advances in the
experimental therapy of ALF have been limited. Treatment strategies, such as charcoal hemoperfusion and
administration of prostaglandin E
1
, which showed early promise, have not been shown to be superior to
standard care.
Prognosis
Children with hepatic failure may fare somewhat better than adults, but overall mortality exceeds 70%. The
prognosis may vary considerably with the cause of liver failure and stage of hepatic encephalopathy. With
http://gateway.ut.ovid.com/gw2/ovidweb.cgi (26 of 31)1/2/2006 10:18:21 PM
Ovid: Principles and Practice of Pediatric Surgery
intensive medical support, survival rates of 50% to 60% occur with hepatic failure complicating acetaminophen
overdose and with fulminant HAV or HBV infection. In contrast, recovery can be expected in only 10% to 20% of
patients with liver failure caused by non-A, non-B, or non-C hepatitis, or an acute onset of Wilson's disease.
Survival of 50% to 75% is being achieved in patients with the poorest prognosis after orthotopic liver
transplantation.
REFERENCES
1. LeBlanc GA. Hepatic vectorial transport of xenobiotics. Chem Biol Interact 1994;90:101120.
2. McGarry JD, Kuwajima M, Newgard CB, et al. From dietary glucose to liver glycogen: the full circle round.
Ann Rev Nutr 1987;7:5173.
3. Alonso MD, Lomako J, Lomako WM, et al. A new look at the biogenesis of glycogen. FASEB J 1995;9:1126
1137.
4. Bahar RJ, Stolz A. Bile acid transport. Gastroenterol Clin North Am 1999;28:2758.
5. Wong MH, Oelkers P, Craddock AL, et al. Expression cloning and characterization of the hamster ileal
sodium-dependent bile acid transporter. J Biol Chem 1994;269:13401347.
6. Rosenthal P. Assessing liver function and hyperbilirubinemia in the newborn. National Academy of Clinical
Biochemistry. Clin Chem 1997;43:228234.
7. Rosenthal P, Henton D, Felber S, et al. Distribution of serum bilirubin conjugates in pediatric hepatobiliary
diseases. J Pediatr 1987;110:201205.
8. Cotton PB, Laage NJ. Endoscopic retrograde cholangiopancreatography in children. Arch Dis Child
1982;57:131136.
9. Ashida K, Nagita A, Sakaguchi M, et al. Endoscopic retrograde cholangiopancreatography in paediatric
patients with biliary disorders. J Gastroenterol Hepatol 1998;13:598603.
10. Tagge EP, Tarnasky PR, Chandler J, et al. Multidisciplinary approach to the treatment of pediatric
pancreaticobiliary disorders. J Pediatr Surg 1997;32:158164.
11. Guelrud M, Jaen D, Mendoza S, et al. ERCP in the diagnosis of extrahepatic biliary atresia. Gastrointest
Endosc 1991;37:522526.
12. Ohnuma N, Takahashi T, Tanabe M, et al. The role of ERCP in biliary atresia. Gastrointest Endosc
1997;45:365370.
13. Ng KK, Wan YL, Lui KW, et al. Three-dimensional magnetic resonance cholangiopancreatography for
evaluation of obstructive jaundice. J Formosan Med Assoc 1997;96:586592.
http://gateway.ut.ovid.com/gw2/ovidweb.cgi (27 of 31)1/2/2006 10:18:21 PM
Ovid: Principles and Practice of Pediatric Surgery
14. McKiernan PJ. Neonatal cholestasis. Semin Neonatol 2002;7:153165.
15. Trauner M, Meier PJ, Boyer JL. Molecular pathogenesis of cholestasis. N Engl J Med 1998;339:12171227.
16. Bates MD, Bucuvalas JC, Alonso MH, et al. Biliary atresia: pathogenesis and treatment. Semin Liver Dis
1998;18:281293.
17. Tagge DU, Tagge EP, Drongowski RA, et al. A long-term experience with biliary atresia. Reassessment of
prognostic factors. Ann Surg 1991;214:590598.
18. Laurent J, Gauthier F, Bernard O, et al. Long-term outcome after surgery for biliary atresia. Study of 40
patients surviving for more than 10 years. Gastroenterology 1990;99:17931797.
19. Ryckman F, Fisher R, Pedersen S, et al. Improved survival in biliary atresia patients in the present era of
liver transplantation. J Pediatr Surg 1993;28:382385.
20. Whitington PF, Balistreri WF. Liver transplantation in pediatrics: indications, contraindications, and
pretransplant management. J Pediatr 1991;118:169177.
21. Lin WY, Lin CC, Changlai SP, et al. Comparison technetium of Tc-99m disofenin cholescintigraphy with
ultrasonography in the differentiation of biliary atresia from other forms of neonatal jaundice. Pediatr Surg Int
1997;12:3033.
22. Tagge EP, Othersen HB Jr, Jackson SM, et al. Impact of laparoscopic cholecystectomy on the management
of cholelithiasis in children with sickle cell disease. J Pediatr Surg 1994;29:209212.
23. Mowat AP. Alpha 1-antitrypsin deficiency (PiZZ): features of liver involvement in childhood. Acta Paediatr
Suppl 1994;393:1317.
24. Perlmutter DH. Alpha-1-antitrypsin deficiency. Semin Liver Dis 1998;18:217225.
25. Vennarecci G, Gunson BK, Ismail T, et al. Transplantation for end stage liver disease related to alpha 1
antitrypsin. Transplantation 1996;61:14881495.
26. Goldberg T, Slonim AE. Nutrition therapy for hepatic glycogen storage diseases. J Am Diet Assoc
1993;93:14231430.
27. Lee PJ, Leonard JV. The hepatic glycogen storage diseasesproblems beyond childhood. J Inherited Metab
Dis 1995;18:462472.
28. Grompe M. The pathophysiology and treatment of hereditary tyrosinemia type 1. Semin Liver Dis
2001;21:563571.
http://gateway.ut.ovid.com/gw2/ovidweb.cgi (28 of 31)1/2/2006 10:18:21 PM
Ovid: Principles and Practice of Pediatric Surgery
29. van Spronsen FJ, Thomasse Y, Smit GP, et al. Hereditary tyrosinemia type I: a new clinical classification
with difference in prognosis on dietary treatment. Hepatology 1994;20:11871191.
30. Mohan N, McKiernan P, Preece MA, et al. Indications and outcome of liver transplantation in tyrosinaemia
type 1. Eur J Pediatr 1999;158. Suppl 2:S4954.
31. Elder GH, Hift RJ, Meissner PN. The acute porphyrias. Lancet 1997;349:16131617.
32. Andant C, Puy H, Bogard C, et al. Hepatocellular carcinoma in patients with acute hepatic porphyria:
frequency of occurrence and related factors. J Hepatol 2000;32:933939.
33. Badminton MN, Elder GH. Management of acute and cutaneous porphyrias. Int J Clin Pract 2002;56:272
278.
34. Polson RJ, Lim CK, Rolles K, et al. The effect of liver transplantation in a 13-year-old boy with
erythropoietic protoporphyria [Comment]. Transplantation 1988;46:386389.
35. Loudianos G, Gitlin JD. Wilson's disease. Semin Liver Dis 2000;20:353364.
36. Lykavieris P, Bernard O, Hadchouel M. Neonatal cholestasis as the presenting feature in cystic fibrosis.
Arch Dis Child 1996;75:6770.
37. Sokol RJ, Durie PR. Recommendations for management of liver and biliary tract disease in cystic fibrosis.
Cystic Fibrosis Foundation Hepatobiliary Disease Consensus Group. J Pediatr Gastroenterol Nutr 1999;28.
38. Noble-Jamieson G, Barnes N, Jamieson N, et al. Liver transplantation for hepatic cirrhosis in cystic fibrosis.
J Roy Soc Med 1996;27:3137.
39. Romero R, Lavine JE. Viral hepatitis in children. Semin Liver Dis 1994;14:289302.
P.1458
40. Alter MJ, Mast EE. The epidemiology of viral hepatitis in the United States. Gastroenterol Clin North Am
1994;23:437455.
41. Beasley RP, Hwang LY. Postnatal infectivity of hepatitis B surface antigen-carrier mothers. J Infect Dis
1983;147:185190.
42. Fishman LN, Jonas MM, Lavine JE. Update on viral hepatitis in children. Pediatr Clin North Am 1996;43:57
74.
43. Shouval D, Samuel D. Hepatitis B immune globulin to prevent hepatitis B virus graft reinfection following
liver transplantation: a concise review. Hepatology 2000;32:11891195.
http://gateway.ut.ovid.com/gw2/ovidweb.cgi (29 of 31)1/2/2006 10:18:21 PM
Ovid: Principles and Practice of Pediatric Surgery
44. Ohto H, Terazawa S, Sasaki N, et al. Transmission of hepatitis C virus from mothers to infants. The
Vertical Transmission of Hepatitis C Virus Collaborative Study Group [Comment]. N Engl J Med 1994;330:744
750.
45. Poynard T, Marcellin P, Lee SS, et al. Randomised trial of interferon alpha2b plus ribavirin for 48 weeks or
for 24 weeks versus interferon alpha2b plus placebo for 48 weeks for treatment of chronic infection with
hepatitis C virus. International Hepatitis Interventional Therapy Group (IHIT). Lancet 1998;352:14261432.
46. Zeuzem S, Feinman SV, Rasenack J, et al. Peginterferon alfa-2a in patients with chronic hepatitis C. N
Engl J Med 2000;343:16661672.
47. Heathcote EJ, Shiffman ML, Cooksley WG, et al. Peginterferon alfa-2a in patients with chronic hepatitis C
and cirrhosis. N Engl J Med 2000;343:16731680.
48. North Italian Endoscopic Club for the study and treatment of esophageal varices. Prediction of the first
variceal hemorrhage in patients with cirrhosis of the liver and esophageal varices. A prospective multicenter
study. The North Italian Endoscopic Club for the Study and Treatment of Esophageal Varices. N Engl J Med
1988;319:983989.
49. Maksoud JG, Goncalves ME. Treatment of portal hypertension in children. World J Surg 1994;18:251258.
50. de Franchis R, Primignani M. Endoscopic treatments for portal hypertension. Semin Liver Dis 1999;19:439
455.
51. Alvarez F, Bernard O, Brunelle F, et al. Portal obstruction in children. II. Results of surgical portosystemic
shunts. J Pediatr 1983;103:703707.
52. Shun A, Delaney DP, Martin HC, et al. Portosystemic shunting for paediatric portal hypertension. J Pediatr
Surg 1997;32:489493.
53. Shah SR, Nagral SS, Mathur SK. Results of a modified Sugiura's devascularisation in the management of
unshuntable portal hypertension. HPB Surg 1999;11:235239.
54. Renard TH, Andrews WS, Rollins N, et al. Use of distal splenorenal shunt in children referred for liver
transplant evaluation. J Pediatr Surg 1994;29:403406.
55. Heyman MB, LaBerge JM. Role of transjugular intrahepatic portosystemic shunt in the treatment of portal
hypertension in pediatric patients. J Pediatr Gastroenterol Nutr 1999;29:240249.
56. Reyes J, Iwatsuki S. Current management of portal hypertension with liver transplantation. Adv Surg
1992;25:189208.
57. Knechtle SJ, Kalayoglu M, D'Alessandro AM, et al. Portal hypertension: surgical management in the 1990s.
Surgery 1994;116:687693.
http://gateway.ut.ovid.com/gw2/ovidweb.cgi (30 of 31)1/2/2006 10:18:21 PM
Ovid: Principles and Practice of Pediatric Surgery
58. Schrier RW. Pathogenesis of sodium and water retention in high-output and low-output cardiac failure,
nephrotic syndrome, cirrhosis, and pregnancy (1). N Engl J Med 1988;319:10651072.
59. Schrier RW. Pathogenesis of sodium and water retention in high-output and low-output cardiac failure,
nephrotic syndrome, cirrhosis, and pregnancy (2). N Engl J Med 1988;319:11271134.
60. Arroyo V, Gines P, Gerbes AL, et al. Definition and diagnostic criteria of refractory ascites and hepatorenal
syndrome in cirrhosis. International Ascites Club. Hepatology 1996;23:164176.
61. Kramer RE, Sokol RJ, Yerushalmi B, et al. Large-volume paracentesis in the management of ascites in
children. J Pediatr Gastroenterol Nutr 2001;33:245249.
62. Nazarian GK, Bjarnason H, Dietz CA Jr, et al. Refractory ascites: midterm results of treatment with a
transjugular intrahepatic portosystemic shunt. Radiology 1997;205:173180.
63. Sergent G, Gottrand F, Delemazure O, et al. Transjugular intrahepatic portosystemic shunt in an infant.
Pediatr Radiol 1997;27:588590.
64. van Buuren HR, Cheng KH, Pieterman H, et al. Transjugular intrahepatic portosystemic shunt. Requiem for
the surgical portosystemic shunt? Scand J Gastroenterol Suppl 1993;200:4852.
65. Rossle M, Ochs A, Gulberg V, et al. A comparison of paracentesis and transjugular intrahepatic
portosystemic shunting in patients with ascites. N Engl J Med 2000;342:17011707.
66. Runyon BA, Squier S, Borzio M. Translocation of gut bacteria in rats with cirrhosis to mesenteric lymph
nodes partially explains the pathogenesis of spontaneous bacterial peritonitis. J Hepatol 1994;21:792796.
67. Aw MM, Dhawan A. Acute liver failure. Indian J Pediatr 2002;69:8791.
68. Miwa S, Hashikura Y, Mita A, et al. Living-related liver transplantation for patients with fulminant and
subfulminant hepatic failure. Hepatology 1991;30:15211526.
69. Nicolette L, Billmire D, Faulkenstein K, et al. Transplantation for acute hepatic failure in children. J Pediatr
Surg 1998;33:9981002.
70. Durand P, Debray D, Mandel R, et al. Acute liver failure in infancy: a 14-year experience of a pediatric
liver transplantation center. J Pediatr 2001;139:871876.
http://gateway.ut.ovid.com/gw2/ovidweb.cgi (31 of 31)1/2/2006 10:18:21 PM
Potrebbero piacerti anche
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Cell Structure, Function Practice Test With AnswersDocumento16 pagineCell Structure, Function Practice Test With AnswersDJ ISAACSNessuna valutazione finora
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- Intel Stratix 10 Avalon - MM Interface For PCI Express Solutions User GuideDocumento173 pagineIntel Stratix 10 Avalon - MM Interface For PCI Express Solutions User Guideenoch richardNessuna valutazione finora
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- SR6 Core Rulebook Errata Feb 2020Documento6 pagineSR6 Core Rulebook Errata Feb 2020yrtalienNessuna valutazione finora
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- 2 Contoh Narative TextDocumento9 pagine2 Contoh Narative TextRini RienzNessuna valutazione finora
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- Aluminium Alloy - Wikipedia, The Free EncyclopediaDocumento12 pagineAluminium Alloy - Wikipedia, The Free EncyclopediaAshishJoshi100% (1)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Product Stock Exchange Learn BookDocumento1 paginaProduct Stock Exchange Learn BookSujit MauryaNessuna valutazione finora
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- Case StudyDocumento61 pagineCase StudyA GNessuna valutazione finora
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Me8072 Renewable Sources of EnergyDocumento13 pagineMe8072 Renewable Sources of EnergyNallappan Rajj ANessuna valutazione finora
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- SPM 1449 2006 Mathematics p2 BerjawapanDocumento18 pagineSPM 1449 2006 Mathematics p2 Berjawapanpss smk selandar71% (7)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- 40 RT-flex Control-System Rev01Documento68 pagine40 RT-flex Control-System Rev01Mayvon Botelho100% (2)
- PAG7.1 Student The Effects of Antibiotics On Microbial Growth - v0.3Documento3 paginePAG7.1 Student The Effects of Antibiotics On Microbial Growth - v0.3Habib UddinNessuna valutazione finora
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Viscous Fluid Flow Frank M White Third Edition - Compress PDFDocumento4 pagineViscous Fluid Flow Frank M White Third Edition - Compress PDFDenielNessuna valutazione finora
- Module in Pe 103Documento79 pagineModule in Pe 103Kym Dacudao100% (1)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- Sample Dilapidation ReportDocumento8 pagineSample Dilapidation ReportczarusNessuna valutazione finora
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (73)
- Eliminating Oscillation Between Parallel MnosfetsDocumento6 pagineEliminating Oscillation Between Parallel MnosfetsCiprian BirisNessuna valutazione finora
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (344)
- Easergy PS100 48VDC Power SupplyDocumento2 pagineEasergy PS100 48VDC Power SupplyRichard SyNessuna valutazione finora
- Class 12 Maths Project On Prime NumbersDocumento13 pagineClass 12 Maths Project On Prime Numbersanon_3835245630% (1)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- LPG GasDocumento39 pagineLPG Gasv prasanthNessuna valutazione finora
- Raspberry Pi 3 and BeagleBone Black For Engineers - UpSkill Learning 124Documento124 pagineRaspberry Pi 3 and BeagleBone Black For Engineers - UpSkill Learning 124Dragan IvanovNessuna valutazione finora
- JHS 182Documento137 pagineJHS 182harbhajan singhNessuna valutazione finora
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- Tsel Manual ThermoselDocumento25 pagineTsel Manual ThermoselPedro AlvelaisNessuna valutazione finora
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- Comparative Performance of Some Cattle Breeds Under Barani Conditions of PakistanDocumento4 pagineComparative Performance of Some Cattle Breeds Under Barani Conditions of PakistanMasood HassanNessuna valutazione finora
- Food Biotechnology in Ethical PerspectiveDocumento340 pagineFood Biotechnology in Ethical Perspectivemojtaba2500100% (2)
- Electrical Power System Device Function NumberDocumento2 pagineElectrical Power System Device Function Numberdan_teegardenNessuna valutazione finora
- Sci NB Mod 2 LSN 3Documento4 pagineSci NB Mod 2 LSN 3Ramses octavio Rodriguez ocanasNessuna valutazione finora
- (G. Lakshmi Narasaiah) Finite Element Analysis PDFDocumento349 pagine(G. Lakshmi Narasaiah) Finite Element Analysis PDFmoljaime1326Nessuna valutazione finora
- Serial Analysis of Gene Expression (SAGE)Documento34 pagineSerial Analysis of Gene Expression (SAGE)Rohit PhalakNessuna valutazione finora
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Uji Efektivitas Mikroba Rumpun BambuDocumento7 pagineUji Efektivitas Mikroba Rumpun BambuUse Real ProjectNessuna valutazione finora
- Complete Processing Lines For Extruded Pet FoodDocumento13 pagineComplete Processing Lines For Extruded Pet FoodденисNessuna valutazione finora
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)