Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
CL 6050 Medication Administration UPDATED With Changes
Caricato da
Juju FernsDescrizione originale:
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
CL 6050 Medication Administration UPDATED With Changes
Caricato da
Juju FernsCopyright:
Formati disponibili
POLICY/PROCEDURE
TITLE:
WRITING, TRANSCRIBING MEDICAL ORDERS,
AUTHRIZATION AND ADMINISTRATION OF
MEDICATIONS AND RECORDING
ORIGINAL DATE:
AUGUST 2004
IDENTIFICATION
NUMBER:
CL 6050 LAST REVISION DATE:
MAY 2012
NEXT REVIEW DATE:
MAY 2015
HOSPITAL(S)
ALL HMC HOSPITALS / ENTITIES
Sheet No. 1 of 10
Medication Management and Use (MMU) Quality Management Department
Regulatory & Accreditation
1.0 POLICY STATEMENT/PURPOSE:
1.1 This policy is formulated for all Hamad Medical Corporation (HMC) healthcare
providers about ordering, writing and transcribing medical orders, authorization for
medication administration, recording medication in the medical record and on the
safe and accurate administration of medications.
2.0 DEFINTIONS:
2.1 A MEDICAL ORDER An authoritative direction or instruction, issued by a
physician, in writing, or by dictation, verbally or by phone, or otherwise, a rule or a
course of action to be implemented by other health care providers, patient, family,
legal guardians, or significant others, in the treatment, plan of care or service, for the
patient. This may include prescription of medications, diagnostic tests, etc.
2.2 TRANSCRIBING MEDICAL ORDERS -- To copy, write over again, transfer or
translate Information from the physicians medical order or instructions on to the
patients medical records for further medical or nursing action e.g. issuing of the
medication by pharmacy department and administration of the medication to the
patient.
2.3 AUTHORIZATION FOR MEDICATION ADMINISTRATION -- The process of giving
certain health care providers legal and professional permission to provide a patient
with a substance prescribed and intended for the diagnosis, treatment, or prevention
of a medical illness or condition.
2.4 MEDICATION ADMINISTRATION -- The practice of administering medications,
which involves providing the patient with a substance prescribed and intended for
the diagnosis, treatment, or prevention of a medical illness or condition.
2.5 TIME CRITICAL SCHEDULED MEDICATION Are those where early or delayed
administration of maintenance doses of greater than 30 minutes before or after
scheduled dose may cause harm or result in substantial sub-optimal therapy or
pharmacological effect.
POLICY/PROCEDURE
TITLE:
WRITING, TRANSCRIBING MEDICAL ORDERS,
AUTHRIZATION AND ADMINISTRATION OF
MEDICATIONS AND RECORDING
ORIGINAL DATE:
AUGUST 2004
IDENTIFICATION
NUMBER:
CL 6050 LAST REVISION DATE:
MAY 2012
NEXT REVIEW DATE:
MAY 2015
HOSPITAL(S)
ALL HMC HOSPITALS / ENTITIES
Sheet No. 2 of 10
Medication Management and Use (MMU) Quality Management Department
Regulatory & Accreditation
3.0 PROCEDURE/PROCESS:
3.1 All medical orders shall be written on a physician order sheet. These include but are
not limited to diagnostic, therapeutic, treatment and palliative care as well as
referrals to other disciplines and healthcare facilities, and orders for medications.
3.2 Medication orders shall be written on the Physicians Prescription Sheet or through
Computer Physician Order Entry (CPOE).
3.3 Orders shall be accurately transcribed by qualified health care providers.
3.4 Medications administered by HMC qualified health care providers shall be written on
the designated forms, including the date, time, signatures and stamp.
3.5 Writing Medical Orders
3.5.1 Only qualified physicians should write medical orders at HMC.
3.5.2 Only orders written on designated order sheets should be considered valid
to be carried out by health care providers.
3.6 Physicians Prescription Sheet should be used for medications order only and
should be completed only by a privileged physician.
3.6.1 The bottom duplicate copy should serve as the medication prescription that
should be filled by the Pharmacy (See Prescribing of Medications, Policy
No. CL 6048).
3.7 Physician Order Sheet should be used for all orders other than medication orders,
and should be completed only by privileged Physicians.
3.8 Transcription of Medication Orders
3.8.1 The staff nurse who transcribes the medication order should complete the
following:
POLICY/PROCEDURE
TITLE:
WRITING, TRANSCRIBING MEDICAL ORDERS,
AUTHRIZATION AND ADMINISTRATION OF
MEDICATIONS AND RECORDING
ORIGINAL DATE:
AUGUST 2004
IDENTIFICATION
NUMBER:
CL 6050 LAST REVISION DATE:
MAY 2012
NEXT REVIEW DATE:
MAY 2015
HOSPITAL(S)
ALL HMC HOSPITALS / ENTITIES
Sheet No. 3 of 10
Medication Management and Use (MMU) Quality Management Department
Regulatory & Accreditation
3.8.1.1 Order date.
3.8.1.2 Medication.
3.8.1.3 Dosage and Frequency.
3.8.1.4 Route.
3.8.1.5 Time.
3.8.1.6 Commencement date, if applicable.
3.8.1.7 Discontinuation date, if applicable.
3.8.2 Any change in the medication dose, route or frequency should be written as
a new prescription. These changes should then be transcribed as a new
order. Order date should indicate the date when the new prescription is
written.
3.8.3 Transcriptions of all medication orders should require a verification of the
accuracy of the transcribed order by a second nurse and it should be
documented on the Medication Administration Record (MAR).
3.9 Recording Medication Administration
3.9.1 The Medication Administration Record should be utilized in all inpatient
units, Emergency Department (Short Stay Unit), Day Care Unit and
Radiology Department for documenting medications administered by all
routes.
3.9.2 The Intensive Care and Intermediate Care Units should utilize the Intensive
Care or Intermediate Care Flow Sheet for documenting the full details of
medications administered by intravenous infusions.
3.9.3 Procedural areas and the peri-operative areas should document medication
administration on their respective Medication Administration Records or
Flow Sheets.
3.9.4 All health care providers authorized to administer medications should
document the medication administration on the designated administration
recording form immediately after administration with date and time.
POLICY/PROCEDURE
TITLE:
WRITING, TRANSCRIBING MEDICAL ORDERS,
AUTHRIZATION AND ADMINISTRATION OF
MEDICATIONS AND RECORDING
ORIGINAL DATE:
AUGUST 2004
IDENTIFICATION
NUMBER:
CL 6050 LAST REVISION DATE:
MAY 2012
NEXT REVIEW DATE:
MAY 2015
HOSPITAL(S)
ALL HMC HOSPITALS / ENTITIES
Sheet No. 4 of 10
Medication Management and Use (MMU) Quality Management Department
Regulatory & Accreditation
3.10 Authorization for Medication Administration
3.10.1 At Hamad Medical Corporation, medications shall be administered to a
patient by the following staff:
3.10.1.1 Staff Nurses with a validated competency.
3.10.1.2 Anesthesiologist, Dentists and other Physicians who are
licensed and have clinical privileges at Hamad Medical
Corporation.
3.10.1.3 Respiratory Therapist (Respiratory Treatments only), Physical
Therapist, Radiology Technologist and Electro-Encephalogram
(EEG) Technicians shall administer medication within the scope
of their practice, Anesthesia Technicians and/or Technologists
administer medications under the supervision of the
anesthesiologist.
3.10.2 Nursing students should administer oral, intramuscular, subcutaneous and
topical use medications only under the direct supervision of the Preceptor or
Clinical Instructor.
3.10.3 The Clinical Instructor or Preceptor should be a staff nurse who assumes
responsibility for the nursing practice of the student.
3.10.4 The Medication Administration Record (MAR) should be countersigned by
the Preceptor.
3.11 Medication Administration
3.11.1 All medication administration by any route shall be safely and correctly
performed by authorized HMC staff consistent with the seven rights of
medication administration:
3.11.1.1 Right patient.
POLICY/PROCEDURE
TITLE:
WRITING, TRANSCRIBING MEDICAL ORDERS,
AUTHRIZATION AND ADMINISTRATION OF
MEDICATIONS AND RECORDING
ORIGINAL DATE:
AUGUST 2004
IDENTIFICATION
NUMBER:
CL 6050 LAST REVISION DATE:
MAY 2012
NEXT REVIEW DATE:
MAY 2015
HOSPITAL(S)
ALL HMC HOSPITALS / ENTITIES
Sheet No. 5 of 10
Medication Management and Use (MMU) Quality Management Department
Regulatory & Accreditation
3.11.1.2 Right medications.
3.11.1.3 Right dose.
3.11.1.4 Right route.
3.11.1.5 Right time.
3.11.1.6 Patients right to refuse.
3.11.1.7 Right to patient and family education.
3.11.2 All HMC staff administering medications, including Physicians, shall follow
proper procedures as described in this Policy.
3.11.3 Only medications prescribed for the patient based on clinical necessity shall
be administered.
3.11.4 All medications administered to patients shall be recorded in their
Medication Administration Record (MAR) or appropriate flow sheet.
3.11.5 The nurse shall have the right and responsibility to question and to refuse to
carry out the order, until clarified, in the following circumstances:
3.11.5.1 Contraindicated due to drug incompatibility.
3.11.5.2 Inappropriate to the patients condition.
3.11.5.3 Known allergy to the medication.
3.11.5.4 Inappropriate for age and weight.
3.11.5.5 Illegible or any part of the Physicians order is unclear or a
concern; e.g., dosage, route.
3.11.6 A medication order transcription shall clearly indicate the following:
3.11.6.1 The date and time the order was written.
3.11.6.2 The name of the drug in generic or as prescribed.
3.11.6.3 The dose of the drug.
3.11.6.4 The route.
3.11.6.5 The frequency of the doses.
3.11.6.6 The medication discontinuation date.
3.11.6.7 The initials of the transcribing nurse.
3.11.6.8 The initials of the witnessing nurse.
POLICY/PROCEDURE
TITLE:
WRITING, TRANSCRIBING MEDICAL ORDERS,
AUTHRIZATION AND ADMINISTRATION OF
MEDICATIONS AND RECORDING
ORIGINAL DATE:
AUGUST 2004
IDENTIFICATION
NUMBER:
CL 6050 LAST REVISION DATE:
MAY 2012
NEXT REVIEW DATE:
MAY 2015
HOSPITAL(S)
ALL HMC HOSPITALS / ENTITIES
Sheet No. 6 of 10
Medication Management and Use (MMU) Quality Management Department
Regulatory & Accreditation
3.11.7 Nurses shall never administer medications via the following routes or
methods:
3.11.7.1 Intra-cardiac.
3.11.7.2 Intra-pericardial.
3.11.7.3 Intraosseous.
3.11.7.4 Intrathecal.
3.11.7.5 Intraarticular.
3.11.8 A history of medication response, allergies, sensitivities and any substance
abuse should be correctly assessed and recorded by the Physician or nurse
doing the initial assessment process or history and physical examination.
3.11.9 Patients/family or caregivers and next of kin should be educated about
medications they are receiving (Refer to Patient and Family Education,
Policy No. CL 6090).
3.11.10 Patients should be identified prior to drug administration using two identifiers
(Refer to Patient Identification, Policy No. CL 7026).
3.11.11 All medications should be properly labeled (Refer to Dispensing of
Medication, Policy No. CL 6049).
3.11.11.1 Nurses should not re-label any medication.
3.11.12 A valid medication order should be written in English and should be clear
(Refer to Prescribing of Medication, Policy No. CL 6048).
3.11.13 The health care providers administering medications should observe the
patient taking and/or swallowing the drug.
3.11.14 Administered medications must be recorded by the person who administers
the medication and signed by the witness if applicable (Refer to Narcotics
and Controlled Drugs Administration, Storage Maintenance and
Accountability, Policy No. CL 6053).
POLICY/PROCEDURE
TITLE:
WRITING, TRANSCRIBING MEDICAL ORDERS,
AUTHRIZATION AND ADMINISTRATION OF
MEDICATIONS AND RECORDING
ORIGINAL DATE:
AUGUST 2004
IDENTIFICATION
NUMBER:
CL 6050 LAST REVISION DATE:
MAY 2012
NEXT REVIEW DATE:
MAY 2015
HOSPITAL(S)
ALL HMC HOSPITALS / ENTITIES
Sheet No. 7 of 10
Medication Management and Use (MMU) Quality Management Department
Regulatory & Accreditation
3.11.15 The Standard Medication Timing as recommended by the Pharmacy
Department should be followed unless specified by the Physician.
3.11.15.1 If the order is written between the standard medication timing,
the prescriber should clearly specify the initial dose timing and
the subsequent dose.
MEDICATION ADMINISTRATION SCHEDULE
Once Daily 0800 Hours or as prescribed by the
Physician
Twice Daily
0800 Hours and 2000 Hours
Three Times Daily 0800 Hours 1300 Hours 2000 Hours
Every 8 Hours
0600 Hours 1400 Hours 2200 Hours
Four Times Daily
0800 Hours 1200 Hours
1800 Hours 2200 Hours
Every 6 Hours
0600 Hours 1200 Hours
1800 Hours 2400 Hours
Every 4 Hours 6 times a day
0800 Hours 1200 Hours
1600 Hours 2000 Hours
2400 Hours 0400 Hours
Every 12 Hours
0600 Hours 1800 Hours
At bedtime 2000 Hours or 2100 Hours
POLICY/PROCEDURE
TITLE:
WRITING, TRANSCRIBING MEDICAL ORDERS,
AUTHRIZATION AND ADMINISTRATION OF
MEDICATIONS AND RECORDING
ORIGINAL DATE:
AUGUST 2004
IDENTIFICATION
NUMBER:
CL 6050 LAST REVISION DATE:
MAY 2012
NEXT REVIEW DATE:
MAY 2015
HOSPITAL(S)
ALL HMC HOSPITALS / ENTITIES
Sheet No. 8 of 10
Medication Management and Use (MMU) Quality Management Department
Regulatory & Accreditation
3.11.16 Scheduled Medication Administration Time Frame: Scheduled
Medications might be given within one hour (1 hour) before or after the
scheduled time, with the following exceptions:
3.11.16.1 Stat orders.
3.11.16.2 First doses and loading doses.
3.11.16.3 One -time doses.
3.11.16.4 Preoperative drugs.
3.11.16.5 On call doses (e.g., pre-procedure sedation).
3.11.16.6 Time-sequenced or concomitant medications (e.g.
chemotherapy and rescue agents, n-acetaylcysteine and
iodinated contrast media).
3.11.16.7 Drugs administered at specific times to ensure accurate
peak/trough/serum drug levels.
3.11.16.8 Ante and post cibum medication (before and after meals).
3.11.16.9 Surgical Prophylactic Antibiotics should be given one hour of
induction of anesthesia.
3.11.16.10 Febrile Neutropenia patients order is considered as stat order
even if not specified.
3.11.16.11 PRN medications.
3.11.16.12 Time Critical Scheduled Medications (Refer to individual
hospitals list).
3.11.16.13 If administration time specified by the prescriber.
3.11.17 Medications prepared in clinical areas should not be stored in a syringe to
be administered at a later time or date. This excludes procedures under
moderate sedation when a top-up dose may be required (Refer to Moderate
Sedation, Policy No. CL 6029).
3.11.18 The appropriate time to administer oral medications after an NPO (Nil Per
Orum) order should be specified by the Physician.
3.11.19 Intravenous medications administered intermittently via capped vascular
access ports should be flushed with 3 to 6 ml of compatible IV fluid or
heparin lock before and after medication administration.
POLICY/PROCEDURE
TITLE:
WRITING, TRANSCRIBING MEDICAL ORDERS,
AUTHRIZATION AND ADMINISTRATION OF
MEDICATIONS AND RECORDING
ORIGINAL DATE:
AUGUST 2004
IDENTIFICATION
NUMBER:
CL 6050 LAST REVISION DATE:
MAY 2012
NEXT REVIEW DATE:
MAY 2015
HOSPITAL(S)
ALL HMC HOSPITALS / ENTITIES
Sheet No. 9 of 10
Medication Management and Use (MMU) Quality Management Department
Regulatory & Accreditation
3.11.20 Continuous intravenous (IV) medication administration requires special
assessment, monitoring and interpretations.
3.11.21 Intravenous medications should be administered by infusion.
3.11.22 Medications such as IV push through cannula should be performed only by
a physician, competent nurse or a competent paramedical staff.
3.11.23 Midnight audit of the Medication Administration Record should be conducted
by the assigned nurse on the night shift for all patients against the original
top copy of the prescription form for the previous 24 hours. This audit
should be noted and signed by the nurse on the top copy of the prescription
form.
3.11.24 Moderate sedation should be administered by a nurse certified in Immediate
Life Support (ILS), as per Moderate Sedation Policy No. CL 6029.
3.11.25 Nurses or other health care providers should not administer any
experimental or investigational medication unless approved by Research
Committee.
3.11.26 If a patient refuses to take a prescribed medication or if the health care
provider omits to administer a medication, the following actions should be
taken:
3.11.26.1 The incident should be documented.
3.11.26.2 The Physician should be notified.
3.11.26.3 The nurse should complete an Occurrence, Variance and
Accident (OVA) report if the outcome of 3.11.26 above, is likely
to have serious potential or actual consequence to the patient.
POLICY/PROCEDURE
TITLE:
WRITING, TRANSCRIBING MEDICAL ORDERS,
AUTHRIZATION AND ADMINISTRATION OF
MEDICATIONS AND RECORDING
ORIGINAL DATE:
AUGUST 2004
IDENTIFICATION
NUMBER:
CL 6050 LAST REVISION DATE:
MAY 2012
NEXT REVIEW DATE:
MAY 2015
HOSPITAL(S)
ALL HMC HOSPITALS / ENTITIES
Sheet No. 10 of 10
Medication Management and Use (MMU) Quality Management Department
Regulatory & Accreditation
3.11.27 Medication Administration to a Discharged Patient
3.11.27.1 If a patient is discharged but remains in the patient care area,
medications should be given as ordered until the patient
physically leaves the unit, or the Physician writes an order
indicating otherwise.
4.0 DOCUMENTATION:
4.1 Documentation as per Hamad Medical Corporation Guidelines.
5.0 REFERENCES:
5.1 Joint Commission International Accreditation Standards for Hospitals, 4th Edition.
Medication Management and Use Chapter, Standards MMU 6, MMU 6.1, MMU 6.2
5.2 Medication Administration. (2003). American Academy of Pediatrics, Retrieved
December 12, 2008, from http://nrc.uchsc.edu/SPINOFF/MED/Medication.pdf.
5.3 ISMP Guidelines for timely medication administration :response to the CMS (30
minutes rule) www.ismp.org./newsletters/acutecare/articles/20110113.asp
6.0 ATTACHMENTS: Not Applicable.
Potrebbero piacerti anche
- Pharmacology Checklist - Rationale 02Documento30 paginePharmacology Checklist - Rationale 02Tisha DeiparineNessuna valutazione finora
- Narcotic Controlled and Semi-Controlled Medications ManagementDocumento11 pagineNarcotic Controlled and Semi-Controlled Medications Managementshajahanputhusseri100% (1)
- ASHP Guidelines On PreventingDocumento23 pagineASHP Guidelines On PreventingArif RachmatNessuna valutazione finora
- 14 Documented Procedures Exist For Retention Time of Medical Records, Data and Information.Documento4 pagine14 Documented Procedures Exist For Retention Time of Medical Records, Data and Information.Sanjay KadamNessuna valutazione finora
- Drug Therapy Monitoring and Pharmaceutical CareDocumento48 pagineDrug Therapy Monitoring and Pharmaceutical CarePooja agarwalNessuna valutazione finora
- Rights of The PatientDocumento2 pagineRights of The PatientJaymart CostillasNessuna valutazione finora
- Mpp-Verification of Prescription OrdersDocumento6 pagineMpp-Verification of Prescription OrdersMelai Rodriguez IbardalozaNessuna valutazione finora
- TPH TherapheuticsDocumento10 pagineTPH TherapheuticsAl Sah Him100% (2)
- Hospitalist Program Toolkit: A Comprehensive Guide to Implementation of Successful Hospitalist ProgramsDa EverandHospitalist Program Toolkit: A Comprehensive Guide to Implementation of Successful Hospitalist ProgramsNessuna valutazione finora
- Restricted Drugs and Non FormularyDocumento2 pagineRestricted Drugs and Non FormularyChristine Joy De OcampoNessuna valutazione finora
- Pharmacy and Therapeutics Committee Policies and ProceduresDocumento5 paginePharmacy and Therapeutics Committee Policies and ProceduresPHARMACY OLMCMCNessuna valutazione finora
- Procurement and Inventory Management for PharmaceuticalsDocumento43 pagineProcurement and Inventory Management for PharmaceuticalsSAURABH SINGHNessuna valutazione finora
- 31-Nursing Assessment For Out Patient DepartmentDocumento2 pagine31-Nursing Assessment For Out Patient DepartmentakositabonNessuna valutazione finora
- Susan Abbotson - Critical Companion To Arthur Miller - A Literary Reference To His Life and Work-Facts On File (2007) PDFDocumento529 pagineSusan Abbotson - Critical Companion To Arthur Miller - A Literary Reference To His Life and Work-Facts On File (2007) PDFTaha Tariq0% (1)
- Management of MedicationDocumento32 pagineManagement of Medicationsanjay100% (1)
- Protocol Hospital NurseDocumento8 pagineProtocol Hospital NurseDeepak patelNessuna valutazione finora
- Specialty Pharmacy A Complete Guide - 2020 EditionDa EverandSpecialty Pharmacy A Complete Guide - 2020 EditionNessuna valutazione finora
- Look-Alike, Sound-Alike Medication NamesDocumento4 pagineLook-Alike, Sound-Alike Medication NamesBenjel AndayaNessuna valutazione finora
- Assigned on Admission, Transfer, and Discharge ProceduresDocumento12 pagineAssigned on Admission, Transfer, and Discharge ProceduresNagulan Nagul100% (1)
- Hospital PharmacyDocumento25 pagineHospital PharmacyDianie VillapaniaNessuna valutazione finora
- Manual For EndosDocumento19 pagineManual For EndosVarsha MalikNessuna valutazione finora
- Quality Assurance (Autosaved)Documento75 pagineQuality Assurance (Autosaved)OGU CourageNessuna valutazione finora
- 26-Accepted Abbreviations and SymbolsDocumento3 pagine26-Accepted Abbreviations and Symbolsakositabon0% (1)
- Prescription handling and record keeping in retail pharmacyDocumento13 paginePrescription handling and record keeping in retail pharmacyMaryam AzizNessuna valutazione finora
- DispensingDocumento30 pagineDispensingNamanamanaNessuna valutazione finora
- Eastern Laguna Medical Hospital: Antimicrobial Stewardship CommitteeDocumento2 pagineEastern Laguna Medical Hospital: Antimicrobial Stewardship CommitteeKersey Adricula RicaldeNessuna valutazione finora
- Policies and Procedures For Sound-Alike and Look-Alike MedicationsDocumento6 paginePolicies and Procedures For Sound-Alike and Look-Alike Medicationsrelena badrNessuna valutazione finora
- High Alert MedicationsDocumento1 paginaHigh Alert MedicationspucukjayaNessuna valutazione finora
- Nursing Responsibilities In: MedicationsDocumento23 pagineNursing Responsibilities In: MedicationsMarianne LayloNessuna valutazione finora
- Western Australian Patient Identification Policy PDFDocumento14 pagineWestern Australian Patient Identification Policy PDFpuspadiniaNessuna valutazione finora
- Ppg-Gdch-Nur-43 Out On Pass PolicyDocumento5 paginePpg-Gdch-Nur-43 Out On Pass PolicyKenny Josef100% (1)
- 6-Cross Training As A Motivational and ProblemDocumento3 pagine6-Cross Training As A Motivational and Problemakositabon100% (1)
- 28-Nursing Assessment For Admission ofDocumento3 pagine28-Nursing Assessment For Admission ofakositabon100% (1)
- APP KSMC 070 V4 Tel Verbal OrdersDocumento9 pagineAPP KSMC 070 V4 Tel Verbal OrdersKimberly SolisNessuna valutazione finora
- Admistration of Controlled Narcotic and Controlled Non-Narcotic MedicationsDocumento37 pagineAdmistration of Controlled Narcotic and Controlled Non-Narcotic MedicationsKrezielDulosEscobarNessuna valutazione finora
- Discharge Process at Adityavardhan HospitalDocumento6 pagineDischarge Process at Adityavardhan HospitalSanjay Kadam100% (1)
- Case Study - Lilavati: HospitalDocumento39 pagineCase Study - Lilavati: HospitalCharanjeet Singh AroraNessuna valutazione finora
- High Alert MedicationsDocumento1 paginaHigh Alert MedicationsOctaviana SimbolonNessuna valutazione finora
- Habawel V Court of Tax AppealsDocumento1 paginaHabawel V Court of Tax AppealsPerry RubioNessuna valutazione finora
- ASTM Reference RadiographsDocumento3 pagineASTM Reference RadiographsAkbar ShaikNessuna valutazione finora
- Medication Error ReportingDocumento3 pagineMedication Error ReportingBebie MengNessuna valutazione finora
- 34-Physician OrdersDocumento4 pagine34-Physician Ordersakositabon0% (1)
- Antimicrobial Prescribing Policy v3.1Documento20 pagineAntimicrobial Prescribing Policy v3.1craNessuna valutazione finora
- Subin Babu - CVDocumento5 pagineSubin Babu - CVJuju FernsNessuna valutazione finora
- Procedure Manual HospitalDocumento196 pagineProcedure Manual HospitalMarian StrihaNessuna valutazione finora
- Maintenance of Patients Records, Its Security, Sharing of Information and Safe DisposalDocumento7 pagineMaintenance of Patients Records, Its Security, Sharing of Information and Safe DisposalAjay KumarNessuna valutazione finora
- 6 Acop v. OmbudsmanDocumento1 pagina6 Acop v. OmbudsmanChester Santos SoniegaNessuna valutazione finora
- High Alert Medication EnglishDocumento48 pagineHigh Alert Medication Englishassajadda lizikriNessuna valutazione finora
- High Alert Medications 2018Documento30 pagineHigh Alert Medications 2018Eman MohamedNessuna valutazione finora
- NARCOTIC&CONTROLLEDDocumento56 pagineNARCOTIC&CONTROLLEDMelai Rodriguez IbardalozaNessuna valutazione finora
- Writing Medical Orders, Transcribing MedicationDocumento3 pagineWriting Medical Orders, Transcribing MedicationAgus IsmailNessuna valutazione finora
- FARM Note CarePlansDocumento11 pagineFARM Note CarePlansbrain bareNessuna valutazione finora
- Hospital Formulary-Lecture NotesDocumento7 pagineHospital Formulary-Lecture NotesPatras BhattiNessuna valutazione finora
- Patient Database Form, DTPW, PCPDocumento7 paginePatient Database Form, DTPW, PCPClarence100% (1)
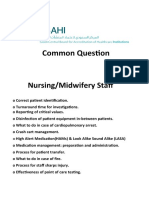
- Nursing Midwifery Staff CBAHI QuestionsDocumento13 pagineNursing Midwifery Staff CBAHI QuestionsnasserjubranNessuna valutazione finora
- Drug AdministrationDocumento30 pagineDrug AdministrationandreabreeNessuna valutazione finora
- Guidelines For The Medicines and Therapeutics CommitteeDocumento20 pagineGuidelines For The Medicines and Therapeutics CommitteeLorezza Miranda Aguilar100% (1)
- A P Policy & Procedure: Ntibiotic OlicyDocumento24 pagineA P Policy & Procedure: Ntibiotic Olicyvijay kumarNessuna valutazione finora
- Administrative Policy for Hospital AdmissionsDocumento8 pagineAdministrative Policy for Hospital AdmissionsHAMMYER ALROKHAMINessuna valutazione finora
- PH 3.2 Prescription AuditDocumento3 paginePH 3.2 Prescription AuditashokNessuna valutazione finora
- ADR Final1Documento10 pagineADR Final1Rubina BisankheNessuna valutazione finora
- Fundamentals of Clinical Pharmacy PracticeDa EverandFundamentals of Clinical Pharmacy PracticeValutazione: 4.5 su 5 stelle4.5/5 (2)
- Healthcare Environmental Services A Complete Guide - 2020 EditionDa EverandHealthcare Environmental Services A Complete Guide - 2020 EditionNessuna valutazione finora
- Mechanisms of Drug Toxicity: Proceedings of the Third International Pharmacological MeetingDa EverandMechanisms of Drug Toxicity: Proceedings of the Third International Pharmacological MeetingH. RaškováNessuna valutazione finora
- Downloaded FromDocumento2 pagineDownloaded FromDuzzysNessuna valutazione finora
- BitLocker Recovery Key 8AABD40C A56C 440D B10D 123305DF1122Documento1 paginaBitLocker Recovery Key 8AABD40C A56C 440D B10D 123305DF1122MuhammadKhalidNessuna valutazione finora
- Downloaded From WWW - ETTV.tvDocumento1 paginaDownloaded From WWW - ETTV.tvJuju FernsNessuna valutazione finora
- How Does Electricity WorkDocumento15 pagineHow Does Electricity WorkJuju FernsNessuna valutazione finora
- Sanitaryware CatalogueDocumento40 pagineSanitaryware CatalogueJuju FernsNessuna valutazione finora
- PLOT NO. 2 - Ground Floor Plan (2781 SQFT)Documento1 paginaPLOT NO. 2 - Ground Floor Plan (2781 SQFT)Juju FernsNessuna valutazione finora
- Texting and Driving Safety PresentationDocumento19 pagineTexting and Driving Safety PresentationJuju Ferns100% (1)
- ZB - 02 - Suspension TraumaDocumento10 pagineZB - 02 - Suspension TraumaJuju FernsNessuna valutazione finora
- Aam Aadmi Series 5Documento16 pagineAam Aadmi Series 5Deepak SharmaNessuna valutazione finora
- SOP08 Occupational Health Plan LUS HSE SP2 446 004 00Documento17 pagineSOP08 Occupational Health Plan LUS HSE SP2 446 004 00Juju FernsNessuna valutazione finora
- Technician cuts extra cables during removal workDocumento1 paginaTechnician cuts extra cables during removal workJuju FernsNessuna valutazione finora
- Emergency Evacuation Layout: Jerry Al Samur Development ProjectDocumento1 paginaEmergency Evacuation Layout: Jerry Al Samur Development ProjectRichu PaliNessuna valutazione finora
- TYGF12Documento1 paginaTYGF12Juju FernsNessuna valutazione finora
- ETA Group - HRP029 - Notice Period PolicyDocumento3 pagineETA Group - HRP029 - Notice Period PolicyJuju FernsNessuna valutazione finora
- TYGF12Documento1 paginaTYGF12Juju FernsNessuna valutazione finora
- JojojoDocumento1 paginaJojojoJuju FernsNessuna valutazione finora
- ETA Group - HRP031 - Exit AdministrationDocumento4 pagineETA Group - HRP031 - Exit AdministrationJuju FernsNessuna valutazione finora
- 5025-11 - Minutes of MEP Weekly Progress Meeting No. 39 PDFDocumento24 pagine5025-11 - Minutes of MEP Weekly Progress Meeting No. 39 PDFJuju FernsNessuna valutazione finora
- HGFYGYDocumento1 paginaHGFYGYJuju FernsNessuna valutazione finora
- TYGF12Documento1 paginaTYGF12Juju FernsNessuna valutazione finora
- HSE Jobs in Saudi Arabia and Qatar - Risk Consultant, Project Manager, Safety OfficerDocumento1 paginaHSE Jobs in Saudi Arabia and Qatar - Risk Consultant, Project Manager, Safety OfficerJuju FernsNessuna valutazione finora
- GFRTDocumento2 pagineGFRTJuju FernsNessuna valutazione finora
- Material Safety Data Sheet: Galva Brite AerosolDocumento6 pagineMaterial Safety Data Sheet: Galva Brite AerosolJuju FernsNessuna valutazione finora
- Scaffolding Inspection Log with Damaged PartsDocumento2 pagineScaffolding Inspection Log with Damaged PartsJuju FernsNessuna valutazione finora
- Dhinesh Nebosh Completed Cv-1Documento4 pagineDhinesh Nebosh Completed Cv-1Juju FernsNessuna valutazione finora
- Approved Form AF 2Documento1 paginaApproved Form AF 2Juju FernsNessuna valutazione finora
- DohaDocumento1 paginaDohaJuju FernsNessuna valutazione finora
- 125Documento2 pagine125Juju FernsNessuna valutazione finora
- QatarDocumento1 paginaQatarJuju FernsNessuna valutazione finora
- AXIS Camera Station Installation and Migration Guide: User ManualDocumento7 pagineAXIS Camera Station Installation and Migration Guide: User ManualCORAL ALONSONessuna valutazione finora
- Newcomb Theodore MDocumento20 pagineNewcomb Theodore MBang Ahmad UstuhriNessuna valutazione finora
- Final Year Project A Report Assessment Form (10%)Documento5 pagineFinal Year Project A Report Assessment Form (10%)Chong Ru YinNessuna valutazione finora
- Culture GuideDocumento44 pagineCulture GuideLeonardo TamburusNessuna valutazione finora
- StarletDocumento16 pagineStarletMohsen SirajNessuna valutazione finora
- Danielle Smith: To Whom It May ConcernDocumento2 pagineDanielle Smith: To Whom It May ConcernDanielle SmithNessuna valutazione finora
- Transmission Line ProtectionDocumento111 pagineTransmission Line ProtectioneccabadNessuna valutazione finora
- Loans and AdvanceDocumento8 pagineLoans and AdvanceDjay SlyNessuna valutazione finora
- SMG Wireless Gateway ManualV2.2.0Documento95 pagineSMG Wireless Gateway ManualV2.2.0shahedctgNessuna valutazione finora
- Machine Problem 6 Securing Cloud Services in The IoTDocumento4 pagineMachine Problem 6 Securing Cloud Services in The IoTJohn Karlo KinkitoNessuna valutazione finora
- Example Italy ItenararyDocumento35 pagineExample Italy ItenararyHafshary D. ThanialNessuna valutazione finora
- Distribution Requirements PlanningDocumento8 pagineDistribution Requirements PlanningnishantchopraNessuna valutazione finora
- Restaurant P&L ReportDocumento4 pagineRestaurant P&L Reportnqobizitha giyaniNessuna valutazione finora
- Hydropneumatic Accumulators Pulsation Dampeners: Certified Company ISO 9001 - 14001Documento70 pagineHydropneumatic Accumulators Pulsation Dampeners: Certified Company ISO 9001 - 14001Matteo RivaNessuna valutazione finora
- CSCI5273 PS3 KiranJojareDocumento11 pagineCSCI5273 PS3 KiranJojareSales TeamNessuna valutazione finora
- Sierra Wireless firmware versions for cellular modulesDocumento20 pagineSierra Wireless firmware versions for cellular modulesjacobbowserNessuna valutazione finora
- An-7004 IGBT Driver Calculation Rev00Documento8 pagineAn-7004 IGBT Driver Calculation Rev00Raghuram YaramatiNessuna valutazione finora
- Break-Even Analysis: Margin of SafetyDocumento2 pagineBreak-Even Analysis: Margin of SafetyNiño Rey LopezNessuna valutazione finora
- Papi AdbDocumento50 paginePapi AdbSilvio Figueiredo0% (1)
- Igbt Irg 4p254sDocumento9 pagineIgbt Irg 4p254sMilagros Mendieta VegaNessuna valutazione finora
- Mecafix 120: Description Technical DataDocumento1 paginaMecafix 120: Description Technical DataJuan Carlos EspinozaNessuna valutazione finora
- Chapter FiveDocumento12 pagineChapter FiveBetel WondifrawNessuna valutazione finora
- PNB V. Se, Et Al.: 18 April 1996 G.R. No. 119231 Hermosisima, JR., J.: Special Laws - Warehouse Receipts LawDocumento3 paginePNB V. Se, Et Al.: 18 April 1996 G.R. No. 119231 Hermosisima, JR., J.: Special Laws - Warehouse Receipts LawKelvin ZabatNessuna valutazione finora
- Naoh Storage Tank Design Description:: Calculations For Tank VolumeDocumento6 pagineNaoh Storage Tank Design Description:: Calculations For Tank VolumeMaria Eloisa Angelie ArellanoNessuna valutazione finora
- Virtual Content SOPDocumento11 pagineVirtual Content SOPAnezwa MpetaNessuna valutazione finora
- The Ball Is Now in Their Hands': Lumumba Responds After City Council Rescinds Emergency DeclarationDocumento2 pagineThe Ball Is Now in Their Hands': Lumumba Responds After City Council Rescinds Emergency DeclarationWLBT NewsNessuna valutazione finora