Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
1echocardiography and The Neonatologist
Caricato da
AbuAlezzAhmedTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
1echocardiography and The Neonatologist
Caricato da
AbuAlezzAhmedCopyright:
Formati disponibili
Echocardiography and the
neonatologist
Lindsey Hunter
Neil Patel
Abstract
Echocardiographic assessment can be broadly divided into functional and
structural assessment. Functional echocardiography in the hands of an
appropriately trained neonatologist is an accessible and useful modality
in the neonatal intensive care unit. This tool allows the neonatologist
to assess various parameters, e.g. ventricular outputs and SVC ow,
ventricular function, pulmonary pressures and ductus arteriosus and
implement immediate management as result. It is essential that there is
support from the paediatric cardiologist to prevent misdiagnosis of
congenital heart disease and implement further management.
Keywords ductus arteriosus; echocardiography; functional assessment;
neonatal intensive care; structural assessment; SVC ows; ventricular
function
Part 1: overview of practice
Over the past decade echocardiography has increasingly become
both a useful and accessible modality within neonatal units.
Echocardiography (echo) is a powerful tool in the hands of an
appropriately trained operator. Echo assessment can be broadly
divided into functional and structural assessments. There is
a distinct overlap between the two assessment categories, each
will inform the other and neither should be considered in
isolation.
Structural assessment of congenital heart disease is impera-
tive to delineate basic and complex cardiac anatomy including
identifying signicant anomalies.
Functional assessment is an evaluation of myocardial function
and haemodynamics. Although introduced primarily a research
tool, functional echo is increasingly employed at the bedside by
neonatologists. Serial measurements are used to answer specic
and immediate clinical questions in the context of the rapidly
changing haemodynamics of a sick neonate.
Functional echo should be performed as an adjunct or in addi-
tion to existing clinical parameters; e.g. lactate, CRT, heart rate,
blood pressure which are of limited value and are open to observer
variability. Functional echocardiography provides a direct
measure of myocardial function, pulmonary and systemic blood
ows and also intra/extra cardiac shunting.
Who should undertake echocardiograms within the neonatal
intensive care? Practicalities, location and politics can often delay
a cardiology assessment within neonatal units. Traditionally the
diagnosis and management of signicant and complex congenital
heart disease has been the realm of the appropriately skilled and
experienced paediatric cardiologist. However, if functional
echocardiograms are performed by the attending neonatal team
frequent assessment and therapeutic adjustment can be made
without the immediate input of paediatric cardiologist.
The neonatology team must be aware that functional assess-
ment does not exclude structural heart defects. This also high-
lights a potential medico-legal debate surrounding neonatologists
undertaking echocardiograms routinely; the main concern being
the potential to misinterpret or even misdiagnose life threatening
congenital heart disease. Neonatologists must be are aware of
their limitations when structurally assessing the neonatal heart;
in particular there are diagnoses which even an experienced
cardiologist may nd difcult to make or have the potential to
miss including coarctation of the aorta, total anomalous pulmo-
nary venous drainage (TAPVD), anomalous left coronary artery
(ALCAPA), congenitally corrected transposition of the great
arteries and atrial isomerisms.
To ensure neonatologists are adequately trained and that
echocardiography within the neonatal intensive care is safe, open
and easily accessible lines of communication between the
paediatric cardiologists and the neonatologists is desirable. We
recommend a model of support for neonatologists by paediatric
cardiologists at a ward level, continuing medical education
(CME), echocardiography courses, training materials and
ongoing positive feedback. There should be opportunities for the
neonatal trainees to work alongside the cardiologists in the form
of an ofcial placement. In the UK and worldwide, including at
our centre, formally-accredited echocardiography courses are run
which are appropriate for neonatologists and allied professionals.
In our hospital there is a close working relationship between
the paediatric cardiologists and neonatologists with a specialist
interest in cardiology. This allows for prompt and timely
assessment of newborns with abnormal clinical examination
ndings or clinical parameters. Both teams meet weekly to
discuss the ongoing care of those neonates with signicant heart
disease in the NICU.
Part 2
The second part of this article focuses on the specic functional
echocardiographic measures which are used frequently in the
neonatal intensive care unit. It is important to stress that these
should always be accompanied by a complete assessment of
cardiac structure, as discussed above. Whilst we hope to provide
some practical insights into these assessments, it is beyond the
scope of this article to teach these techniques.
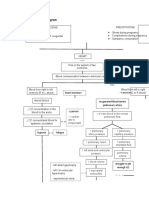
Assessment of the ductus arteriosus (DA)
Assessment of the DA is most frequently performed in pre-term
infants, in whom consideration may be given to closure by
surgical or medical therapies, but is also important in
Lindsey Hunter MBChB MRCPCH is a Paediatric Cardiology Specialist
Trainee in the Cardiology Department Royal Hospital for Sick Children,
Glasgow G3 8SJ, UK. Conicts of interest: none.
Neil Patel BA MBChB MRCPCH MD is a Consultant Neonatologist in Neonatal
Intensive Care at the Royal Hospital for Sick Children, Glasgow G3 8SJ,
UK. Conicts of interest: none.
SYMPOSIUM: NEONATOLOGY
PAEDIATRICS AND CHILD HEALTH 21:6 254 2010 Elsevier Ltd. All rights reserved.
duct-dependent congenital cardiac disease and for assessment of
pulmonary artery pressures.
The DA is typically directly visualized from a high left para-
sternal view. From this position the entire length of the DA can
be demonstrated between proximal descending aorta and
pulmonary artery, and a Doppler of ow velocities and directions
may be performed (Figure 1).
The diameter of the DA may be measured at its insertion into
the pulmonary artery from 2-dimensional and colour Doppler
images. Any constriction of the PDA usually occurs at this point.
Ductal diameters, and the presence of constriction, may assist
prediction of spontaneous duct closure.
There is increasing interest in dening a haemodynamically
signicant ductus arteriosus (HSDA). This depends on combined
echocardiographic and clinical assessment, and may be assisted
by a scoring system such as that proposed by McNamara et al.
(Ref). Echocardiographic ndings in HSDA are of moderate to
large sized ductus withunrestricted left-to-right owof reasonably
high velocity. The echo may also demonstrate reversed diastolic
ow in the proximal descending aorta which may accompany
evidence of impaired abdominal end organ perfusion.
The shunt size through a DA may also be assessed indirectly
by measurement of the left atrium:aortic diameter ratio (LA:Ao).
A left-to-right ductal shunt leads to increased pulmonary venous
return, leading to enlargement of the LA and an increase in the
ratio. Both LA and Ao diameters are obtained from a parasternal,
long-axis m-mode image, the aortic valve diameter is measured
at end diastole and the maximal LA diameter at end systole. A
ratio of greater >1.5:1 is associated with a HSDA.
Management of the HSDA remains controversial and variable.
Early targeted treatment using NSAIDs, ibuprofen or indometh-
acin, is advocated by some authors to achieve greater rates of DA
closure and minimize the pathological consequence of an HSDA.
Serial echocardiography allows more selective, targeted and
shorter courses of NSAID to be given, thereby minimizing the
risks of side effects.
Calculation of ventricular outputs and superior vena cava
(SVC) ows
Measurement of systemic blood ow, combined with blood
pressure allows more informed therapeutic decisions to be made
in the haemodynamically compromised infant. Echocardiography
allows non-invasive measurement of ows in infants where
invasive ow monitoring is too risky or technically challenging.
Calculation of ows requires measurement of a valve diam-
eter, or vessel, to calculate its cross sectional area (CSA). A pulse
wave Doppler ow of velocity against time is then obtained
across the valve, or within the vessel, and the area under this
traced for one cardiac cycle to generate the velocity time integer
(VTI). The ow (in volume/time) is equal to the product of CSA,
VTI and heart rate and is often divided by weight for expression
as ml/kg/min.
Cardiac output Velocity time integer
valve cross sectional area heart rate
Right and left ventricular outputs may be measured this way and
have been shown to change in RDS, PDA and high output states.
In the absence of any shunts right (RVO) and left ventricular
outputs (LVO) are equal to each other and systemic blood ow
(SBF), and are normally between 220 and 250 ml/kg/min.
However, atrial and ductal shunts are common in pre-term
infants (refs) and will lead to differences between RVO and LVO,
such that ventricular outputs cannot be considered equal to SBF.
It has therefore been suggested that measurement of SVC
ow, i.e. blood ow returning to the heart, may provide a better
proportional measure of SBF, independent of shunts. A subcostal
Doppler of SVC ow entering the RA is obtained and combined
with SVC diameter measurements from long-axis views to
calculate SVC ows, which are normally around 80 ml/kg/min.
SVC Flow Velocity time integer SVC cross sectional area
heart rate
SVC ows appear to be low in a proportion of pre-term infants
(newborn low output state) who may be at risk of hypotension,
IVH and neurodevelopmental abnormality (HUNT).
Although not in widespread clinical use, appropriately trained
and equipped neonatal units may routinely measure ventricular
outputs and SVC ows.
It should be appreciated that the error in any ow measure-
ment may be as high as 25%, due to the numerous measure-
ments involved.
Ventricular function
Ventricular function assessment is complicated by the complex
nature of the cardiac cycle and 3-dimensional geometry of the
ventricles.
Rapid clinical assessment of ventricular function is often
based on subjective opinion from 2-dimensional images obtained
in the long and short parasternal axes and apical 4-chamber
views. This technique has the signicant limitations of being
subjective, observer dependent and non-quantitative.
Quantitative volumetric measures of LV function include
ejection fraction and fractional shortening, calculated from
RVOT
MPA
LPA
Descending
aorta
Patent
ductus
Pulse wave
Doppler sample
RPA
Figure 1 Schematic diagram of DA demonstrating position for Doppler of
DA ow.
SYMPOSIUM: NEONATOLOGY
PAEDIATRICS AND CHILD HEALTH 21:6 255 2010 Elsevier Ltd. All rights reserved.
long-axis parasternal m-mode images. Though widely employed
this technique measures systolic function only, is prone to
measurement error and is not independent of changes in loading
conditions. An alternative measure of LV systolic function is the
relationship between LV mean velocity of circumferential bre
shortening (LV MVCF). This technique is said to have the
advantages of being pre-load independent and takes after-load
into account. However, LV MVCF requires measurements of LV
volume, LV wall thickness, ejection time and arterial pressure
and is arguably too cumbersome for routine clinical use.
An alternative global measure of ventricular function is the
Myocardial Performance Index (MPI), or Tei index. This is
derived from time intervals during the cardiac cycle. Though
easily performed in neonates MPI gives no indication of systolic
and diastolic functions, and is also load-dependent i.e. changes
in pre-load or after-load may alter MPI independent of changes in
myocardial function.
Tissue Doppler Imaging, strain and speckle strain imaging are
newer and promising techniques. These have the ability to
directly quantify global and regional systolic and diastolic func-
tion in multiple dimensions. Initial studies have shown the
feasibility of these techniques and their potential for future
clinical use in neonates.
Pulmonary artery pressure
Pulmonary hypertension (PHT) is common in sick newborn
infants and leads to impaired pulmonary blood ow, ventricular
dysfunction due to increased after-load, and pulmonary-systemic
shunting leading to hypoxaemia.
There are two principal echo methods of measuring pulmo-
nary artery pressure (PAP) in newborns; tricuspid regurgitation
jet velocity (TR) and direction and velocity of ductal shunts.
In the TR jet technique the peak TR velocity is inserted into
a modied Bernoulli equation, to calculate the gradient between
the RV and RA:
Pressure gradient 4velocity
2
RV peak pressure (RVp) is obtained by adding this pressure
gradient to an estimate of RA pressure (usually around 5 mmHg).
RVp should be equal to PAP, in the absence of RV outow
obstruction. Previous studies have conrmed that PAP obtained
by the TR method correlates well with gold-standard catheter
measures of PAP.
The TR jet is usually obtained from the apical 4-chamber view,
ensuring a minimal angle of insonation. (Figure 2). The extent of
the TR jet often increases with increasing PAP, even when the
tricuspid valve is otherwise normal and competent. In some
infants, however, TR may be absent, even in the presence of PHT.
An alternative method of estimating PAP is using the direction
and velocity of the ow through a patent DA. These will be
LA RA
LV RV
Doppler beam
Figure 2 Apical 4-chamber view demonstrating position of Doppler sample
for measurement of tricuspid regurgitation velocity.
Figure 3 Doppler waveform demonstrating bidirectional ow in patent ductus arteriosus in an infant with pulmonary hypertension.
SYMPOSIUM: NEONATOLOGY
PAEDIATRICS AND CHILD HEALTH 21:6 256 2010 Elsevier Ltd. All rights reserved.
dependent on the pressure gradient between the pulmonary
artery and aorta at any point in the cardiac cycle. Ductal ow will
be left-to-right if aortic pressure (Ao
p
) exceeds PAP. As PAP
increases ow in the DA may reverse, becoming bidirectional
(Figure 3). If PAP is above aortic pressure throughout the cardiac
cycle, as in severe pulmonary hypertension, then DA ow will be
exclusively right-to-left ow.
The velocity of the DA ow can be inserted into the Bernoulli
equation to calculate the peak pressure gradient between PA and
Ao
p
. However, this peak gradient does not equal the true
difference between peak PA and peak Ao
p
. This is because RV
and LV ejections do not necessarily coincide, and therefore peak
PAP and peak Ao
p
are not simultaneous either.
PAP is not linearly related to RV function, and therefore any
assessment of pulmonary pressures should include an assess-
ment of ventricular function.
Summary
There is an expanding role for functional echocardiography within
the NICU, and for neonatologists performing echocardiograms.
However, neonatologists must be appropriatelytrainedandshould
work in conjunction with, and supported by, their Paediatric
Cardiology colleagues. Neonatal functional cardiology remains an
area of evolving research and discovery with the aimof improving
outcomes for all infants with haemodynamic compromise. A
FURTHER READING
Carmo K, Evans N, Paradisis M. Duration of indomethacin treatment of the
preterm patent ductus arteriosus as directed by echocardiography.
J Pediatr 2009; 155: 819e22.
Evans N. Diagnosis of patent ductus arteriosus in the preterm newborn.
Arch Dis Child 1993; 68: 58e61.
Evans N. Echocardiography on neonatal intensive care units in Australia
and New Zealand. J Paediatr Child Health 2000; 36(2): 169e71.
Evans N, Kluckow M. Early determinants of right and left ventricular
output in ventilated preterm infants. Arch Dis Child Fetal Neonatal Ed
1996; 74: F88e94.
Hiraishi S, Horiguchi Y, Misawa H, et al. Noninvasive Doppler echocar-
diographic evaluation of shunt ow dynamics of the ductus arteriosus.
Circulation 1987; 75: 1146e53.
Iyer P, Evans N. Re-evaluation of the left atrial to aortic root ratio as
a marker of patent ductus arterious. Arch Dis Child Fetal Neonatal Ed
1994; 70: F112e7.
Kluckow M, Evans N. Superior vena cava ow in newborn infants: a novel
marker of systemic blood ow. Arch Dis Child Fetal Neonatal Ed 2000;
82: F182e7.
Kluckow M, Seri I, Evans N. Functional echocardiography an emerging tool
for the neonatologist. J Pediatr 2007; 150: 125e30.
McNamara PJ, Sehgal A. Towards rational management of the patent
ductus arteriosus: the need for disease staging. Arch Dis Child Fetal
Neonatal Ed 2007; 93(6): F424e7.
Mori K, Nakagawa R, Nii M, et al. Pulsed wave Doppler tissue echocar-
diography assessment of the long axis function of the right and left
ventricles during the early neonatal period. Heart 2004; 90: 175e80.
Osborn DA, Evans N, Kluckow M. Left ventricular contractility in extremely
premature infants in the rst day and response to inotropes. Pediatr
Res 2007; 61: 335e40.
Patel N, Mills JF, Cheung MM. Assessment of right ventricular function
using tissue Doppler imaging in infants with pulmonary hypertension.
Neonatology 2009; 96: 193e9.
Patel N, Mills JF, Cheung MM. Use of the myocardial performance index to
assess right ventricular function in infants with pulmonary hyperten-
sion. Pediatr Cardiol 2009; 30: 133e7.
Sehgal A, McNamara PJ. Does point of care functional echocardiography
enhance cardiovascular care in the NICU? J Perinatol 2008; 28:
729e35.
Skinner J, Alverson D, Hunter S. Echocardiography for the neonatologist,
vol. 6. London: Churchill Livingstone, 2000: 133e150.
Skinner JR, Stuart AG, OSullivan J, Heads A, Boys RJ, Hunter S. Right
heart pressure determination by Doppler in infants with tricuspid
regurgitation. Arch Dis Child 1993; 69: 216e20.
Skinner JR, Hunter S, Hey EN. Haemodynamic features at presentation in
persistent pulmonary hypertension of the newborn and outcome. Arch
Dis Child Fetal Neonatal Ed 1996; 74: F26e32.
Tsutsumi T, Ishii M, Eto G, Hota M, Kato H. Serial evaluation for myocardial
performance in fetuses and neonates using a new Doppler index.
Pediatr Int 1999; 41: 722e7.
Ward CJ, Purdie J. Diagnostic accuracy of paediatric echocardiograms
interpreted by individuals other than paediatric cardiologists. J Pae-
diatr Child Health 2001; 37: 3316.
Practice points
C
Echocardiography is a convenient and increasingly important
tool in the assessment and management of newborn infants in
the intensive care unit.
C
Neonatologists performing echocardiography must be
appropriately trained, and should work collaboratively with
a supportive local Paediatric Cardiology team.
C
Neonatal echocardiography includes structural and functional
assessments.
C
Complete structural assessment is imperative to detect
complex cardiac anatomy, which should be managed in
conjunction with the Paediatric Cardiology Team.
C
Functional assessment allows improved understanding of the
mechanisms of cardiovascular compromise infants with and
without structural anomalies.
C
Functional assessment includes measures of ventricular
function, pressures (including pulmonary arterial pressures),
and blood ows in the heart and major vessels.
SYMPOSIUM: NEONATOLOGY
PAEDIATRICS AND CHILD HEALTH 21:6 257 2010 Elsevier Ltd. All rights reserved.
Potrebbero piacerti anche
- 1 s2.0 S1548559521000331 MainDocumento10 pagine1 s2.0 S1548559521000331 MainAchrafNessuna valutazione finora
- Pediatric Echocardiography TechniquesDocumento17 paginePediatric Echocardiography Techniquesraviks34Nessuna valutazione finora
- Debo Ode 2018Documento23 pagineDebo Ode 2018MaluNessuna valutazione finora
- Congenital Heart Disease Presentation and ManagementDocumento4 pagineCongenital Heart Disease Presentation and ManagementCh RajeshNessuna valutazione finora
- Fetal DisritmiaDocumento18 pagineFetal DisritmiaSebastian ChandraNessuna valutazione finora
- Skowno 2019Documento8 pagineSkowno 2019Miguel SánchezNessuna valutazione finora
- Introduction To Echocardiography - (PDF) - in EnglishDocumento16 pagineIntroduction To Echocardiography - (PDF) - in EnglishjedicitoNessuna valutazione finora
- Trans EsophagealDocumento13 pagineTrans EsophagealApril Retno SusiloNessuna valutazione finora
- 1 s2.0 S2772930322004367 MainDocumento15 pagine1 s2.0 S2772930322004367 MainVimal NishadNessuna valutazione finora
- Echocardiography Dissertation IdeasDocumento8 pagineEchocardiography Dissertation IdeasWhoCanWriteMyPaperForMeCanada100% (1)
- Clinical Cases in Chronic Thromboembolic Pulmonary HypertensionDa EverandClinical Cases in Chronic Thromboembolic Pulmonary HypertensionWilliam R. AugerNessuna valutazione finora
- 510732Documento13 pagine510732PaulHerreraNessuna valutazione finora
- Current management and future perspectives of peripartum cardiomyopathyDocumento8 pagineCurrent management and future perspectives of peripartum cardiomyopathyArdisa MeilitaNessuna valutazione finora
- Pediatric Postoperative Cardiac CareDocumento18 paginePediatric Postoperative Cardiac CareChristian MartínezNessuna valutazione finora
- Zuva MuzachimDocumento6 pagineZuva MuzachimZuva MuzachimNessuna valutazione finora
- FetalEcho Statement FINAL publishedinUOGAugust2008 PDFDocumento4 pagineFetalEcho Statement FINAL publishedinUOGAugust2008 PDFLizbeth QuinteroNessuna valutazione finora
- Clinical Review: Hemodynamic Monitoring in The Intensive Care UnitDocumento8 pagineClinical Review: Hemodynamic Monitoring in The Intensive Care Unitmasfak97Nessuna valutazione finora
- Congenital Heart Disease: Education and Practice GapsDocumento18 pagineCongenital Heart Disease: Education and Practice GapsAlvaro Ignacio Lagos SuilNessuna valutazione finora
- 1-s2.0-S1071916423003068-mainDocumento13 pagine1-s2.0-S1071916423003068-mainevelyn.minichNessuna valutazione finora
- Heart Failure ThesisDocumento5 pagineHeart Failure Thesislisastephensfortcollins100% (2)
- Cardiologist: SpecializationsDocumento14 pagineCardiologist: SpecializationsChloe KozumeNessuna valutazione finora
- Enfermedad Valvular CardiacaDocumento10 pagineEnfermedad Valvular CardiacaBrayan HuayraNessuna valutazione finora
- Echo viewsDocumento24 pagineEcho viewsMarina MonulNessuna valutazione finora
- Pediatric Echocardiogram GuidelinesDocumento18 paginePediatric Echocardiogram GuidelinesNorhafizah AhmadNessuna valutazione finora
- Cardiac Anaesthesia Thesis TopicsDocumento6 pagineCardiac Anaesthesia Thesis Topicsfbzgmpm3100% (2)
- Role of non-invasive modalities in diagnosing Congenital Heart DiseaseDocumento33 pagineRole of non-invasive modalities in diagnosing Congenital Heart Diseasezulfantri1983Nessuna valutazione finora
- Monitoring The Critically Ill PatientDocumento4 pagineMonitoring The Critically Ill PatientAh ZhangNessuna valutazione finora
- Anesthesiology Centric ACLSDocumento45 pagineAnesthesiology Centric ACLSAlex ApsokardosNessuna valutazione finora
- Cardiovascular Perfusion ThesisDocumento4 pagineCardiovascular Perfusion Thesisamandagraytulsa100% (2)
- Ductus ArteriosoDocumento17 pagineDuctus ArteriosoJohn Romero CevallosNessuna valutazione finora
- The Role of Echocardiographic Study in Patients With Chronic Kidney DiseaseDocumento9 pagineThe Role of Echocardiographic Study in Patients With Chronic Kidney DiseaseshodhgangaNessuna valutazione finora
- Smith 2013 SMIIDocumento9 pagineSmith 2013 SMIIGryseldaGryGryNessuna valutazione finora
- ISUOG - Fetal Heart ExaminationDocumento12 pagineISUOG - Fetal Heart ExaminationAzucenaNessuna valutazione finora
- SEHGAL 2016 - A New Look at Bronchopulmonary Dysplasia - Post Capillary Pathophysiology and Cardiac DysfunctionDocumento8 pagineSEHGAL 2016 - A New Look at Bronchopulmonary Dysplasia - Post Capillary Pathophysiology and Cardiac DysfunctionRafael JustinoNessuna valutazione finora
- Updated ELSO Pediatric Guidelines 1617997662Documento13 pagineUpdated ELSO Pediatric Guidelines 1617997662Useful StuffNessuna valutazione finora
- Eco DopplerDocumento8 pagineEco DopplerClaudia IsabelNessuna valutazione finora
- 8c99f2 PDFDocumento52 pagine8c99f2 PDFKrisParadajsNessuna valutazione finora
- Noninvasive Hemodynamic Monitoring in The Intensive Care UnitDocumento18 pagineNoninvasive Hemodynamic Monitoring in The Intensive Care UnitmegaNessuna valutazione finora
- 1 s2.0 S1053077019303039 MainDocumento6 pagine1 s2.0 S1053077019303039 MainADELIAADENessuna valutazione finora
- Atwater 2020Documento6 pagineAtwater 2020Vlada SiricNessuna valutazione finora
- Clinical Cases in Heart FailureDa EverandClinical Cases in Heart FailureRavi V. ShahNessuna valutazione finora
- Heart Failure Thesis StatementDocumento5 pagineHeart Failure Thesis StatementLisa Graves100% (2)
- Role of Neonatologist-Performed Echocardiography in The Assessment and T Management of Patent Ductus Arteriosus Physiology in The NewbornDocumento6 pagineRole of Neonatologist-Performed Echocardiography in The Assessment and T Management of Patent Ductus Arteriosus Physiology in The Newbornannie.estdiNessuna valutazione finora
- Cardiac ResuscitationDocumento24 pagineCardiac ResuscitationPaulinaNessuna valutazione finora
- JAIN 2015_PDA diagnosis evaluation and managementDocumento10 pagineJAIN 2015_PDA diagnosis evaluation and managementRafael JustinoNessuna valutazione finora
- Hemodynamic Monitoring ModalitiesDocumento14 pagineHemodynamic Monitoring Modalitiesrudy sanabriaNessuna valutazione finora
- Echocardiography Thesis TopicsDocumento4 pagineEchocardiography Thesis Topicsbsqw6cbt100% (1)
- Research Paper On Congenital Heart DefectsDocumento8 pagineResearch Paper On Congenital Heart Defectspwvgqccnd100% (1)
- Atent Ductus Arteriosus in Preterm InfantsDocumento8 pagineAtent Ductus Arteriosus in Preterm InfantsLissaberti AmaliahNessuna valutazione finora
- Eacvi Recommendations Valvular Regurgitation SummaryDocumento34 pagineEacvi Recommendations Valvular Regurgitation SummaryWilli SotoNessuna valutazione finora
- Sepsis Parte 2Documento12 pagineSepsis Parte 2Maria AlejandraNessuna valutazione finora
- 2022 Non-Cardiac SurgeryDocumento105 pagine2022 Non-Cardiac Surgeryhosameldin ahmedNessuna valutazione finora
- Systolic and Diastolic Function in Congestive Heart Failure Pediatric PatientsDocumento10 pagineSystolic and Diastolic Function in Congestive Heart Failure Pediatric PatientsMiguelNessuna valutazione finora
- Clinical Cases in Right Heart FailureDa EverandClinical Cases in Right Heart FailureLana TsaoNessuna valutazione finora
- Dextrocardia PaperDocumento18 pagineDextrocardia PaperChrismicel GunarsoNessuna valutazione finora
- Ehad 883Documento3 pagineEhad 883nhunhuochachNessuna valutazione finora
- Functional Echocardiography in Assessment of The Cardiovascular System in Asphyxiated NeonatesDocumento6 pagineFunctional Echocardiography in Assessment of The Cardiovascular System in Asphyxiated NeonatesAdrian KhomanNessuna valutazione finora
- Ecocardiografia Monitoreo Hemodinamico en Critico..Documento12 pagineEcocardiografia Monitoreo Hemodinamico en Critico..cositaamorNessuna valutazione finora
- Health 6 Quarter 1 Module6Documento12 pagineHealth 6 Quarter 1 Module6Cindy EsperanzateNessuna valutazione finora
- CardiomyopathyDocumento18 pagineCardiomyopathyDimpal Choudhary100% (1)
- Dịch test - Freedom from Health Anxiety-Rối loạn lo âu bệnh tật-Karen Lynn Cassiday PhDDocumento3 pagineDịch test - Freedom from Health Anxiety-Rối loạn lo âu bệnh tật-Karen Lynn Cassiday PhDĐạt ThânNessuna valutazione finora
- ACS Final DraftDocumento33 pagineACS Final Draftomcm17006Nessuna valutazione finora
- Fetal Echocardiography: Scope, Cardiac Development & AbnormalitiesDocumento28 pagineFetal Echocardiography: Scope, Cardiac Development & Abnormalitiesmerin sunilNessuna valutazione finora
- European J of Heart Fail - 2021 - Moura - Integration of Imaging and Circulating Biomarkers in Heart Failure A ConsensusDocumento20 pagineEuropean J of Heart Fail - 2021 - Moura - Integration of Imaging and Circulating Biomarkers in Heart Failure A ConsensusIsamar AgostoNessuna valutazione finora
- VT and SVTDocumento10 pagineVT and SVTDwi WijayantiNessuna valutazione finora
- Jurnal Mutiple StentDocumento9 pagineJurnal Mutiple StentPrima Anggreini ArinNessuna valutazione finora
- Path o PhysiologyDocumento2 paginePath o PhysiologyPotato BroNessuna valutazione finora
- Congenital-Heart-Disease MidwiferyDocumento16 pagineCongenital-Heart-Disease MidwiferyDrMaxamuud Caqli NuurNessuna valutazione finora
- Tetralogy of FallotDocumento37 pagineTetralogy of Fallottintinlovessu100% (1)
- Amiodarone Infusion GuidelineDocumento3 pagineAmiodarone Infusion GuidelineNur SusiawantyNessuna valutazione finora
- Medical SpecialistDocumento9 pagineMedical SpecialistDhiya MaralinNessuna valutazione finora
- Case Scenario CHFDocumento2 pagineCase Scenario CHFchetankumarbhumireddyNessuna valutazione finora
- The Crash CartDocumento39 pagineThe Crash Cartpramod kumawat100% (1)
- The Sample of PediatricsDocumento47 pagineThe Sample of PediatricsWaseem UllahNessuna valutazione finora
- NCP For HypertensionDocumento1 paginaNCP For Hypertensionrhizalyn1367% (6)
- Heartbeat Health Pitch DeckDocumento24 pagineHeartbeat Health Pitch DeckJordan CrookNessuna valutazione finora
- Diagnosis and Management of Myocardial InfarctionDocumento69 pagineDiagnosis and Management of Myocardial InfarctionSanjana GkNessuna valutazione finora
- Cardiovascular Disease Management Updates from Universitas IndonesiaDocumento22 pagineCardiovascular Disease Management Updates from Universitas IndonesiaAnggit PudjiastutiNessuna valutazione finora
- DS-10249 ACLS PI Sheet 03ts PDFDocumento1 paginaDS-10249 ACLS PI Sheet 03ts PDFAsrini Rizky NasutionNessuna valutazione finora
- Conduction SystemDocumento2 pagineConduction SystemMalik Asif HussainNessuna valutazione finora
- Aha Acls Prep Packet 2020Documento69 pagineAha Acls Prep Packet 2020VP The Hacker100% (2)
- Case Study Heart Attack PDFDocumento30 pagineCase Study Heart Attack PDFtkgoon634950% (2)
- Arrhythmia & Anti-Arrhythmic DrugsDocumento49 pagineArrhythmia & Anti-Arrhythmic DrugsNitesh SinghNessuna valutazione finora
- Electrocardiography: The ECG: A.D. John, MD, Lee A. Fleisher, MDDocumento19 pagineElectrocardiography: The ECG: A.D. John, MD, Lee A. Fleisher, MDCésar Vásquez AguilarNessuna valutazione finora
- Acyanotic Heart DiseaseDocumento20 pagineAcyanotic Heart DiseaseArun GeorgeNessuna valutazione finora
- The Effect of Cilostazol On Right Heart FunctionDocumento43 pagineThe Effect of Cilostazol On Right Heart FunctionGunawan YogaNessuna valutazione finora
- 0 - Anesthetic Management of A Case With Aortic Regurgitation Posted For Laproscopic Hernia Mesh RepairDocumento4 pagine0 - Anesthetic Management of A Case With Aortic Regurgitation Posted For Laproscopic Hernia Mesh RepairAromal SatheeshNessuna valutazione finora
- E Lectrocardiography ECG: Practical Physiology 2020-2021 LabDocumento8 pagineE Lectrocardiography ECG: Practical Physiology 2020-2021 LabBushra AlkaqaniNessuna valutazione finora