Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Hemostasis Dysproteinemias
Caricato da
Shaz ChindhyCopyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Hemostasis Dysproteinemias
Caricato da
Shaz ChindhyCopyright:
Formati disponibili
Hemostatic Dysfunction in Paraproteinemias
and Amyloidosis
Maurizio Zangari, M.D.,
1
Francesca Elice, M.D.,
1
Louis Fink, M.D.,
2
and Guido Tricot, M.D., Ph.D.
1
ABSTRACT
Thrombotic and hemorrhagic complications frequently have been observed in
patients with monoclonal gammopathy, Waldenstrom macroglobulinemia, amyloidosis,
multiple myeloma (MM), and myeloma. Chemotherapy in combination with the use of
antiangiogenic agents can further enhance the risk of cardiovascular complications. A
malignancy-associated thrombophilic state (in particular, cytokine-induced high levels of
factor VIII and von Willebrand factor) can also explain the high rate of thrombosis
reported in these patients. Impaired brinolysis and a transient downregulation of the
protein C system are recently discovered pathogenetic mechanisms. At diagnosis, when
the highest VTE risk is present, baseline coagulation tests such activated protein C
resistance may be helpful to identify patients who can benet the most from anti-
coagulation; with the emerging evidence of a positive effect on survival of low molecular
weight heparin, prospective trials are needed in this group of diseases.
KEYWORDS: Myeloma, paraproteinemia, amyloidosis, bleeding diathesis, thrombosis
INCIDENCE OF THROMBOEMBOLIC
COMPLICATIONS
Thrombosis is nowrecognizedas one of the most common
complications faced by cancer patients. In addition to
common risk factors for venous thromboembolism
(VTE) such as age, immobility, surgery, inammatory
response, and chemotherapy, disease-specic mechanisms
are involved in the pathogenesis of the phenomenon. The
overall incidence of VTE in the general population is 117
per 100,000 person-years. Incidence rates for both deep
vein thrombosis (DVT) and pulmonary embolism (PE)
increase dramatically withadvancing age among both men
and women. Thromboembolic complications frequently
have beenreportedinpatients withparaproteinemias, as in
many other hematologic malignancies. Monoclonal
gammopathy of undetermined signicance (MGUS) has
been associated with an increased risk of VTE: the VTE
rate was 6.1% (1.3 per 100 patient-years) in a prospective
analysis of 310 MGUS patients
1
and 7.5% in a retrospec-
tive study with 174 patients observed during a 10-year
period.
2
With the knowledge that specic intervention
can affect the hemostatic system differently, multiple
myeloma (MM) patients treated with vincristine 0.5 mg,
doxorubicin (doxo) 10 mg/m
2
, and dexamethasone 40 mg
daily for 4 days (VAD) with or without radiotherapy
showed a VTE incidence of 10%.
2,3
In a population
with a median age of 61 years, two recent large phase III
trials in the relapse setting have shown that single-agent
dexamethasone is associated with a lowrate of thrombosis
(3.5%in the MM-009 trial, 4.5%in the MM-010 trial).
4,5
Similar incidence (3%) has been observed with dexame-
thasone in the newly diagnosed setting.
6
1
Myeloma Institute for Research and Therapy, University of Arkansas
for Medical Sciences, Little Rock, Arkansas;
2
Nevada Cancer Institute,
Las Vegas, Nevada.
Address for correspondence and reprint requests: Maurizio Zangari,
M.D., Myeloma Institute for Research and Therapy, 4301 West
Markham, 816 Little Rock, AR72205. E-mail: zangarimaurizio@uams.
edu.
Hemostatic Dysfunction in Malignant Hematologic Disorders; Guest
Editor, Hau C. Kwaan, M.D., Ph.D.
Semin Thromb Hemost 2007;33:339349. Copyright # 2007 by
Thieme Medical Publishers, Inc., 333 Seventh Avenue, New York, NY
10001, USA. Tel: +1(212) 5844662.
DOI 10.1055/s-2007-976169. ISSN 0094-6176.
339
The recent introduction of effective antiangio-
genic agents in cancer treatment has heightened the
medical attention on this phenomenon. Thalidomide,
the rst antiangiogenic drug tested in MM, was associ-
ated to an unexpected high rate of VTE (27%) when
combined with dexamethasone and chemotherapy.
7
This
complication was not apparent when used as single agent:
VTE incidence was <5% in 169 extensively pretreated
MM patients receiving single-agent thalidomide
8
; a
similar experience was reported by other investigators.
9,10
Compared with single-agent thalidomide, a modest in-
crease of the thrombotic risk was described in relapsed or
refractory patients treated with the combination of dex-
amethasone and thalidomide (VTE rate 8%),
11
but this
risk became more prominent when the same regimen was
applied to newly diagnosed subjects (VTE rate 20 to
26%).
6,12
The potential thrombogenicity of the thalido-
mide/chemotherapy combination was conrmed further
in a phase III trial with upfront random assignment to
chemotherapy with or without thalidomide: incidence of
thrombosis was statistically higher in the thalidomide
arm(p 0.002).
13
Among 232 MM patients treated with
chemotherapy and thalidomide in two protocols that
differed only by the inclusion of doxo in one, VTE
incidence was signicantly different in the two groups
(doxo 16 versus 3.5%; p 0.02).
14
The synergistic prothrombotic effect of doxo/
thalidomide combination was also conrmed in an ex-
perimental model of thrombosis in rabbits.
15
In a multi-
variate analysis of 535 patients treated with thalidomide
in various trials, newly diagnosed status, thalidomide/
doxo combination, and presence of chromosome 11
abnormalities were the only independent risk factors
associated with DVT development.
16
The early onset
of thrombosis, when the highest tumor load is present
(50% of cases within 2 months),
12
indicates a possible
release of thrombogenic factors from cancer cells. Low
VTE rate (8%) has been reported in the United King-
dom Myeloma Forum T-VAD trial, in which thalido-
mide was added to VAD chemotherapy (T-VAD) only
after an initial debulking with two chemotherapy
cycles.
17
The low VTE incidence associated with the
brief delay in thalidomide administration suggests that
the drug could act as a precipitating factor only in the
presence of a baseline prothrombophilic state. The
immunomodulatory drug lenalidomide is a thalidomide
analogue that retains direct anticancer toxicity and
immunological activity of the parent compound but
with different toxicity prole. Deep venous thrombosis
was not a frequent event in phase I and II studies.
18,19
However, grade 3 or 4 VTE were observed in 18% of
patients enrolled in a phase II trial which compared
two different lenalidomide dexamethasone schedules.
20
Preliminary reports of two multicenter double blind
phase III trials which compared lenalidomide plus
dexamethasone versus dexamethasone and placebo in
relapsed/refractory setting (MM-009 study in North
America and MM-010 study internationally) indicate
statistically higher DVT incidence in the lenalidomide/
dexamethasone arms of both the studies (MM-009 15%
vs 3.5% & MM-010 8.5% vs 4.5%).
4,5
Frequent throm-
botic episodes were reported in an ongoing SWOG trial
which compared dexamethasone alone versus dexame-
thasone plus lenalidomide in newly diagnosed patients; 9
of the rst 12 patients (75%) enrolled in the lenalido-
mide/dexamethasone arm without anticoagulation de-
veloped thrombosis, including one ischemic stroke,
while no events were reported in 9 patients assigned to
the dexamethasone arm.
21
The addition of aspirin (80
mg or 325 mg) reduced such incidence to 19%. More
contained DVT incidence was reported in a similar
setting by Rajkumar
22
with aspirin prophylaxis (3%).
Among other paraproteinemias, venous and arte-
rial thrombotic events have been frequently associated
with amyloidosis. In a group of 56 amyloidosis patients
with a median age of 67 years, 11% developed VTE.
23
The presence of circulating monoclonal protein was not
a risk factor for VTE development, whereas older age,
immobility, and personal history of DVT were found to
increase the thrombotic risk. In patients with acute
leukemia and amyloidosis, a thrombotic event appears
to confer a substantial morbidity and mortality and
complicates the management of an already complex
clinical condition: median survival for patients with
arterial and venous thrombosis was 3 and thrombosis
was 16 months respectively.
24
Recent studies indicate
that cancer prothrombogenicity is involved intrinsically
in tumor cell growth, angiogenesis, metastasis, and
associated with a poorer prognosis.
25
These observations
have led to the hypothesis that anticoagulant treatment
could affect the survival of cancer patients.
26
We have
analyzed the prognostic impact of the development of a
thrombotic episode in newly diagnosed MM patients
who received chemotherapy either with or without
thalidomide on our Total Therapy 2 protocol.
27
Of
668 patients enrolled, 155 developed VTE complication
during treatment. The overall and event-free survival of
patients who experience VTE was not inferior. Indeed,
we observed that patients who received intensive chemo-
therapy without thalidomide and developed thrombosis
experienced a signicantly longer event-free survival
compared with those without VTE (p 0.02), suggest-
ing a benecial effect of low molecular weight heparin
(LMWH) on disease progression.
28
PATHOGENETIC MECHANISMS OF
THROMBOSIS IN PARAPROTEINEMIAS
Multiple and interdependent mechanisms are responsi-
ble for the hypercoagulable state in patients with
cancer. Tumor procoagulant activity, host inammatory
responses, and extrinsic factors, which frequently are
340 SEMINARS IN THROMBOSIS AND HEMOSTASIS/VOLUME 33, NUMBER 4 2007
iatrogenic, are involved. Classic risk factors such as
surgery, prolonged immobilization, fractures, and use
of oral contraceptives not only predispose apparently
normal individuals to thrombosis but also are likely to
trigger this condition in people with inherited and
acquired thrombophilic abnormalities. Abnormally
high plasma levels of immunoglobulin and associated
increased blood viscosity can impair brin polymeriza-
tion.
29
The abnormally structured brin interferes with
the binding site for plasmin and factor XIII (FXIII).
30
Defective binding with FXIII causes a decit in clot
retraction and bulky clot formation, which can more
easily occlude small blood vessels.
31
Abnormally as-
sembled brin produces thinner and weaker strands
that are more resistant to brinolytic activity of plasmin.
In fact, brin structure is a major determinant of bri-
nolysis that can be impaired in a manner dependent on
the dose of immunoglobulin G (IgG).
3234
Yagci et al
33
have observed a signicant negative correlation between
global brinolytic capacity (GFC) with levels of plasmi-
nogen activator inhibitor type 1 (PAI-1) and C-reactive
protein (CRP), suggesting that decreased GFC is caused
mainly by high PAI-1 activity. In MM, the increased
PAI-1 activity seems to be related to an increased CRP
and interleukin-6 (IL-6) levels. These observations in-
dicate that inammatory cytokines associated with mye-
loma (in particular, IL-6 and its downstream target
CRP) not only have a direct effect on coagulation, but
can also inhibit brinolysis.
The monoclonal paraprotein itself may have in-
trinsic prothrombotic properties: several authors have
described monoclonal paraproteins with lupus antico-
agulant activity in patients who developed thromboem-
bolic events.
35
Bellotti et al
36
described three patients
with immunoglobulins against thromboplastin phos-
pholipid that showed lupus anticoagulantlike activity:
the strongest interaction was demonstrated in the patient
with the most basic antibody. Takamiya et al
37
described
an IgG lambda paraprotein derived from a myeloma
patient with lupus anticoagulantlike activity in mixing
studies; such immunoglobulin lost its activity when
degraded by pepsin, suggesting that the interaction
with coagulation factors and phospholipids was not
immunologically mediated. These observations indicate
that negatively charged immunoglobulins can interact
with acid phospholipid on the platelet surface by an
electrostatic mechanism. IL-6, CRP, and tumor necrosis
factor alpha (TNF-a) are acute-phase reactant proteins
frequently elevated in patients with MM.
IL-6 plays is an important role as a survival and
antiapoptotic factor for MM cells in the bone marrow
microenvironment and has been implicated in both auto-
crine and paracrine growth of the malignant clone.
38
IL-6
induces not only B lymphocyte differentiation into ter-
minally differentiated plasma cells but also acts as a
survival and growth factor for MM. IL-6 is able to induce
the growth of plasma cells isolated from patients and to
inhibit myeloma cell apoptosis induced by dexamethasone
and anti-Fas antibodies, but it cannot inhibit apoptosis
induced by irradiation.
39
Serum levels of IL-6 and CRP
have been associated with the proliferative activity of the
disease and used as prognostic factors in MM patients.
40
IL-6 is produced not only by plasma cells, but mainly by
osteoblasts and stromal cells, resulting in paracrine stim-
ulation of the malignant clone. This stimulation depends
on both direct cellcell contact and on the release of
soluble factors such as TNF-a, soluble IL-6Ra, and
vascular endothelial growth factor (VEGF).
41
The pro-
duction of VEGF in this cytokine loop is of particular
interest because VEGF enhances angiogenesis and upre-
gulates the expression of tissue factor on endothelial
cells,
42
thus contributing to the disease-associated throm-
bophilic state. Under normal conditions, the anticoagu-
lant-to-procoagulant balance of the endothelium allows
blood cells and platelets to owwithout adhering to vessel
walls. Excessive cytokine concentration during the in-
ammatory- or acute-phase response states can alter this
ne balance, producing procoagulant endothelial condi-
tions.
43
The cytokine network associated with MMalso is
an example of such an imbalance. In particular, elevated
IL-6 levels are able to increase brinogen, tissue factor,
and FVIII plasma levels.
44,45
These in vitro observations
also have been conrmed in the clinical setting, where
high levels of FVIII and von Willebrand factor (vWF)
antigen have been associated with IL-6 levels in patients
with active disease.
46
In this background of impaired brinolysis and
cytokine-induced activation of the coagulation system,
the deciency of natural anticoagulant mechanisms can
further alter the hemostatic balance in a thrombophilic
direction. In MM, an impaired activity of the protein C
system has been suggested by the observation of abnor-
mal resistance to activated protein C (APC) and by a
reduced protein S function.
Indeed, the presence of acquired resistance to
APC without FV Leiden mutation has been observed
in cancer patients who experienced a thrombotic epi-
sode.
47,48
After reporting a high incidence (23%) of
acquired APC resistance in a group of 62 newly diag-
nosed myeloma patients with active disease,
49
we con-
ducted an analysis of 1178 newly diagnosed or newly
treated myeloma patients: APC resistance was detected
in 109 patients (9%) and in two thirds of them the
alteration was not related to FV Leiden mutation.
50
Patients carrying such an acquired abnormality developed
a statistically higher incidence (p 0.008) of thrombosis
during treatment. Acquired APC resistance was not
observed in a series of 51 patients with MGUS that
were tested at our institution (unpublished data) support-
ing the idea that cancer activity along with inammatory
cytokine release plays a crucial role in inducing abnor-
malities in the APC system. Similar experiences have
HEMOSTATIC DYSFUNCTION IN PARAPROTEINEMIAS AND AMYLOIDOSIS/ZANGARI ET AL 341
been reported by Hugo and Jeanet,
51
who conducted a
prospective study with 50 symptomatic MM patients
treated with thalidomide in combination with VAD
(20 patients), dexamethasone (24 patients), or melpha-
lan/prednisone (six patients).
51
Atransient acquired APC
resistance was observed in 12% of patients and was
associated with a high incidence (66%) of DVT.
Protein S is an important APC cofactor for the
inactivation FVa and FVIIIa; levels of protein S are
known to be reduced in inammatory conditions.
52
Indeed, in a group of 78 newly diagnosed myeloma
patients, we found a correlation between acquired
APC resistance and decreased protein S activity
(p 0.012), which was present in 27% of patients
(Table 1).
50
The binding of the IgG paraprotein with
free protein S, which resulted in a severe acquired
deciency of protein S activity, has also been described
in a myeloma patient.
53
The role of inherited thrombophilic factors seems
to be marginal in patients with neoplasia
54
and in
particular with MM.
55
In an analysis of 1178 myeloma
patients conducted at our institution, 3% were carriers of
the FV Leiden mutation.
50
FV Leiden mutation is the
most common thrombophilic mutation that is found in 1
to 7% of a normal white population,
56
and determines a
7-fold increase of VTE risk in heterozygous carriers,
whereas this risk is up to 80-fold higher in homozygous
patients.
57,58
In our series, patients carrying FV Leiden
mutation appear to have higher VTE incidence com-
pared with controls (22% v 12%), but this difference did
not reach statistical signicance.
50
The prothrombotic
mutation 20210A of the prothrombin gene occurs in 2%
of the general population, but it is more frequent in
patients with VTE.
59
This mutation has been observed
in 4% of newly diagnosed myeloma patients (Table 2).
Methylenetetrahydrofolate reductase (MTHFR) gene
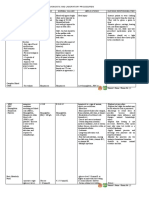
Table 1 Coagulation Factors at Baseline and during Therapy in Myeloma Patients
Baseline (% abnormal)
After
Treatment Therapy Reference
D-dimer Increased (63%) T CHT Elice et al
50
PAI-1 Normal TD Corso et al
60
Homocysteine Increased (56%) T and TD Weber et al
61
Increased (814%) T CHT Elice et al
50
Antithrombin Decreased (42%) In 19 of
20 patients
T or TD Weber et al
61
Decreased (32%) T CHT Elice et al
50
Protein C activity Decreased (18%) T and TD Weber et al
61
Decreased (9%) T CHT Elice et al
50
Protein S activity Decreased (12%) T and TD Weber et al
61
Decreased (27%) T CHT Elice et al
50
APC sensitivity ratio Decreased (9%) T CHT Elice et al
50
Thrombomodulin Decreased # TD Corso et al
60
von Willebrand antigen Increased (49%) T CHT Elice et al
50
Increased T CHT Minnema et al
46
Factor VIII:C Increased T CHT Minnema et al
46
Anticardiolipin IgG Positive (3%) T CHT Elice et al
50
Anticardiolipin IgA Positive (20%) Negative T and TD Weber et al
61
VEGF Increased T and TD Weber et al
105
Increased T Neben et al
106
# in RP T Bertolini et al
107
# in RP T Dmoszynska et al
108
b-FGF # in RP T Bertolini et al
107
# in RP T Dmoszynska et al
108
T, thalidomide; CHT, chemotherapy; PAI-1, plasminogen activator inhibitor type 1; , no change; TD, thalidomide and dexamethesone; APC,
activated protein C; #, decreased levels with therapy compared with baseline; C, coagulant activity; Ig, immunoglobulin; VEGF, vascular
endothelial growth factor; RP, responding patients; b-FGF, basic fibroblast growth factor.
342 SEMINARS IN THROMBOSIS AND HEMOSTASIS/VOLUME 33, NUMBER 4 2007
T
a
b
l
e
2
S
t
r
a
t
e
g
i
e
s
o
f
T
h
r
o
m
b
o
p
r
o
p
h
y
l
a
x
i
s
i
n
M
y
e
l
o
m
a
P
a
t
i
e
n
t
s
S
t
a
t
u
s
(
N
/
R
)
N
o
P
r
o
p
h
y
l
a
x
i
s
W
a
r
f
a
r
i
n
1
1
.
2
5
m
g
/
d
L
o
w
M
o
l
e
c
u
l
a
r
W
e
i
g
h
t
H
e
p
a
r
i
n
A
s
p
i
r
i
n
%
V
T
E
N
o
.
R
e
f
e
r
e
n
c
e
%
V
T
E
N
o
.
R
e
f
e
r
e
n
c
e
%
V
T
E
N
o
.
R
e
f
e
r
e
n
c
e
%
V
T
E
N
o
.
R
e
f
e
r
e
n
c
e
(
d
o
s
e
o
f
a
s
p
i
r
i
n
)
T
h
a
l
i
d
o
m
i
d
e
d
e
x
a
m
e
t
h
a
s
o
n
e
N
2
6
1
9
C
a
v
o
e
t
a
l
1
2
2
5
2
4
W
e
b
e
r
e
t
a
l
6
8
7
4
2
H
a
s
s
o
u
n
1
0
9
(
8
1
m
g
)
*
2
0
1
0
2
R
a
j
k
u
m
a
r
e
t
a
l
6
1
3
5
2
C
a
v
o
e
t
a
l
1
2
R
2
1
2
0
P
a
l
u
m
b
o
e
t
a
l
1
1
0
8
4
7
A
n
a
g
n
o
t
o
p
o
u
l
o
s
e
t
a
l
1
1
T
h
a
l
i
d
o
m
i
d
e
m
e
l
p
h
a
l
a
n
/
p
r
e
d
n
i
s
o
n
e
N
1
2
1
2
4
F
a
c
o
n
e
t
a
l
1
1
1
1
8
6
5
P
a
l
u
m
b
o
e
t
a
l
1
1
2
5
7
8
P
a
l
u
m
b
o
e
t
a
l
1
1
2
T
h
a
l
i
d
o
m
i
d
e
c
h
e
m
o
t
h
e
r
a
p
y
w
i
t
h
d
o
x
o
r
u
b
i
c
i
n
N
3
4
8
7
Z
a
n
g
a
r
i
e
t
a
l
7
1
3
1
3
5
Z
a
n
g
a
r
i
e
t
a
l
7
1
1
5
6
8
Z
a
n
g
a
r
i
e
t
a
l
7
1
1
0
3
9
Z
e
r
v
a
s
e
t
a
l
1
1
3
1
0
2
1
1
M
i
n
n
e
m
a
e
t
a
l
7
3
1
2
1
6
C
h
a
n
a
n
-
K
h
a
n
e
t
a
l
1
1
4
1
8
5
8
B
a
z
e
t
a
l
7
5
(
8
1
m
g
)
R
1
6
1
9
2
Z
a
n
g
a
r
i
e
t
a
l
4
9
L
e
n
a
l
i
d
o
m
i
d
e
d
e
x
a
m
e
t
h
a
s
o
n
e
N
3
3
4
R
a
j
k
u
m
a
r
e
t
a
l
2
2
(
8
0
3
2
5
m
g
)
7
5
1
2
Z
o
n
d
e
r
e
t
a
l
2
1
1
9
3
2
Z
o
n
d
e
r
e
t
a
l
2
1
(
3
2
5
m
g
)
R
8
3
5
1
D
i
m
o
p
o
u
l
o
s
e
t
a
l
5
L
e
n
a
l
i
d
o
m
i
d
e
m
e
l
p
h
a
l
a
n
a
n
d
p
r
e
d
n
i
s
o
n
e
R
2
3
8
P
a
l
u
m
b
o
e
t
a
l
1
1
2
(
1
0
0
m
g
)
L
e
n
a
l
i
d
o
m
i
d
e
c
h
e
m
o
t
h
e
r
a
p
y
w
i
t
h
d
o
x
o
r
u
b
i
c
i
n
R
9
5
8
B
a
z
e
t
a
l
7
5
(
8
2
m
g
)
*
T
h
a
l
i
d
o
m
i
d
e
a
n
d
d
e
x
a
m
e
t
h
a
s
o
n
e
w
e
r
e
a
d
m
i
n
i
s
t
e
r
e
d
t
o
n
e
w
l
y
d
i
a
g
n
o
s
e
d
p
a
t
i
e
n
t
s
a
f
t
e
r
a
n
i
n
i
t
i
a
l
d
e
b
u
l
k
i
n
g
c
h
e
m
o
t
h
e
r
a
p
y
.
R
,
r
e
l
a
p
s
e
d
/
r
e
f
r
a
c
t
o
r
y
;
V
T
E
,
v
e
n
o
u
s
t
h
r
o
m
b
o
e
m
b
o
l
i
s
m
;
N
,
n
e
w
l
y
d
i
a
g
n
o
s
e
d
.
HEMOSTATIC DYSFUNCTION IN PARAPROTEINEMIAS AND AMYLOIDOSIS/ZANGARI ET AL 343
mutations have been described in up to 50% of MM
individuals and overall not different from general pop-
ulation.
60,61
In myeloma patients, inherited thrombo-
philic factors seem to have a marginal impact on VTE
risk. Prophylactic strategies, and selected testing (APC)
rather than extensive screening for thrombophilic factors
are recommended in patients with paraproteinemias.
EFFECT OF MYELOMA THERAPY ON
COAGULATION AND ANGIOGENIC
FACTORS
Activation of coagulation system and brinolysis, in-
creased angiogenesis, and reduction of natural antico-
agulants has been observed in patients with myeloma
during the course of the disease (Table 1). Several
investigators reported transient elevations of FVIII and
vWF levels during therapy with thalidomide.
46,62
Minema et al
46
also described an association between
FVIII and vWF levels and VTE development. Clinical
evidence of an elevated plasma level of vWF and FVIII
was described in a patient with hereditary von Willebrand
disease type 2A, who experienced a temporary remission
of bleeding symptoms at onset of MM. The reappearance
of symptoms, after achieving remission, suggests that an
effective myeloma therapy can downregulate the levels of
these factors.
63
The knowledge of a correlation between
FVIII levels and VTE risk
64
could be important for the
assessment of the thrombotic risk of patients receiving
thrombogenic therapies. Levels of vWF and platelet
aggregation tests were obtained in a group of individuals
at baseline and after therapy with liposomal doxo, vin-
cristine, dexamethasone, and thalidomide. Higher vWF
levels and increased platelet sensitivity to ristocetin dur-
ing treatment suggest a possible interaction between
platelets and endothelial cells.
65
The increased level of
such factors could be related not only to therapy, but also
could be associated with disease activity, given that many
patients with active disease had elevated baseline FVIII
and vWF levels, irrespective of thalidomide treatment.
Because vWF is synthesized by endothelial cells, the level
of vWF may indicate bone marrow neovascularization, or
could be the result of cytokines release. Indeed, interleu-
kin-11 upregulates clotting factor levels.
46
A group of 31
myeloma patients with acquired APC resistance had the
test repeated at least twice during treatment. Response to
therapy was associated with normalization of APC values
in two thirds of these patients. Disease status (active
disease versus partial or complete response) and level of
monoclonal component were the two factors associated
with the presence of APC resistance.
50
Reduction of thrombomodulin plasma concentra-
tion and variation of angiogenic factors also have been
reported during thalidomide therapy
60,66
(Table 2). A
decrease of VEGF and basic broblast growth factor (b-
FGF) was only observed in responding patients. Similar
changes in angiogenic molecules were also described with
conventional chemotherapy, indicating that tumor bur-
den reduction rather than thalidomide-dependent inhib-
ition of angiogenic cytokine secretion is the most likely
explanation for this phenomenon. In a bone marrow
endothelial cell system derived from active myeloma
patients, thalidomide has been shown to downregulate
the expression of angiogenic genes such as VEGF, b-
FGF, and hepatocyte growth factor. A similar effect was
not observed on endothelial systems derived frominactive
MM or monoclonal gammopathy.
67
It is conceivable that
the antiangiogenic properties associated to thalidomide
are depending on the disease and microenvironment,
explaining the contrasting results obtained regarding
the antiangiogenic activity of thalidomide in vivo.
EFFECT OF ANTICOAGULANTS ON
THROMBOTIC COMPLICATIONS IN
PARAPROTEINEMIAS
The best strategy to prevent thromboembolic complica-
tions in paraproteinemias has not been established yet,
mainly because of limited data available. Although it is
difcult to introduce a systematic thromboprophylaxis in
a population of patients who are often thrombocytopenic
and have an increased risk of bleeding, the high rate of
thromboembolic complications during the treatment
with new agents warrants the use of prophylaxis in those
patients with the highest risk. Denition of the treat-
ment-associated thrombotic risk in a specic cancer
population and identication of reliable markers for
VTE development are fundamental for the evaluation
of the riskbenet ratio of an anticoagulant therapy.
Table 2 summarizes the strategies for thrombo-
prophylaxis used in myeloma patients treated with tha-
lidomide and lenalidomide in different combinations
with dexamethasone or chemotherapy. Effective anti-
coagulation with warfarin has the advantage of oral
administration, but it requires regular monitoring to
keep international normalized ratio (INR) values within
a dened range and it has many interactions with food or
other drugs. With the use of therapeutic anticoagulation
with warfarin (INR range 2 to 3), thrombosis was a rare
event in newly diagnosed patients treated with thalido-
mide and dexamethasone.
68
The use of xed low-dose
warfarin derives from the experience in VTE prophylaxis
for patients with indwelling catheters or with atrial
brillation. Although this strategy does not require blood
monitoring, efcacy results were contrasting.
69,70
Similar
opposing results were obtained in MM: Although Cavo
et al
12
showed a signicant reduction in VTE incidence
in newly diagnosed patients treated with upfront thali-
domide and dexamethasone, Weber et al
68
and Zangari
et al
71
did not conrmthis risk reduction. Different doses
of warfarin (1.25 versus 1 mg/d) or different patient
populations may account for the discordant results.
344 SEMINARS IN THROMBOSIS AND HEMOSTASIS/VOLUME 33, NUMBER 4 2007
The superiority of LMWH compared with war-
farin for recurrent VTE prophylaxis in cancer patients
72
inspired the use of these drugs for thromboprophylaxis
in MM patients with the highest VTE risk.
The prothrombotic effect of doxo-containing
chemotherapy combined with thalidomide was abro-
gated completely by the prophylactic use of enoxaparin
(40 mg/d) or nadroparin (2850 IU anti-Xa), as listed in
Table 2.
71,73
For the treatment of responding patients
who developed VTE, available data suggest that it is
reasonable to resume the therapy with thalidomide when
full anticoagulation has been established and continued
for the total duration of therapy.
71
The rate of VTE
recurrence was overall 11% and not signicantly differ-
ent from the rate observed in other cancers (9 to 17%).
74
Recent data suggesting a possible role of platelet
dysfunction in the pathogenesis of VTE have led to test
aspirin as thromboprophylaxis in clinical trials.
65
Although only a modest reduction of VTE incidence
was obtained with prophylactic xed low dose aspirin in
patients treated with thalidomide, dexamethasone and
chemotherapy,
75
aspirin appears more efcacious in
protocols including lenalidomide/dexamethasone, as
shown in Table 2.
21,22
BLEEDING DIATHESIS IN
PARAPROTEINEMIAS
Evidence of bleeding, often conned to purpura, epis-
taxis, or hematuria, manifests in less than 10% of
patients with MGUS, MM, Waldenstrom macroglobu-
linemia, and primary AL amyloidosis. Interactions be-
tween plasma paraprotein, platelets, and coagulation
factors (reviewed by Liebman
76
) are the common path-
ophysiologic mechanisms.
In a series of 62 patients with paraproteinemia,
correlation between specic immunoglobulins and ab-
normalities of the coagulation system or frequency of
bleeding episodes were described.
77
Platelet count and
thrombin time were more frequently altered in IgG and
IgA paraproteinemias, whereas platelet adhesiveness test,
FVIII levels, prothrombin time (PT), and partial throm-
boplastin time (PTT) were often abnormal in IgA and
IgM paraproteinemias. Bleeding episodes were more
frequent in Waldenstrom macroglobulinemia (36%) and
IgA myeloma (33%). Mixing studies with normal plasma
indicated the presence of an inhibitory paraprotein that
caused reduced levels of coagulation factors or prolonga-
tion of thrombin time (TT), PT, and PTT times.
Bleeding diathesis is more commonly observed in
patients with amyloidosis: at diagnosis, 15% of patients
show purpura, particularly in periorbital and facial
areas.
78
Severe hemorrhages are rare, but they can be
life threatening. In a series of 36 patients with amyloi-
dosis and monoclonal gammopathy, laboratory clotting
abnormalities were found in most cases and hemorrhagic
manifestations were found in one third of patients (nine
mild to moderate episodes of purpura or ecchymoses and
fatal mucosa hemorrhage).
79
Prolongation of TT, repti-
lase time (RT), and Russel viper venom time (RVVT) are
the most common abnormalities found; low plasma levels
of FX are also common and do not correlate with RVVT.
The presence of a plasma inhibitor has been hypothesized
to be the cause of TT, RT, and RVVT prolongation but
abnormal tests values can also be observed in the absence
of an abnormal paraprotein. Paraprotein can inhibit brin
polymerization, resulting in prolonged TT and abnormal
clot formation.
30
Inhibition of brin monomer aggrega-
tion by the paraprotein also has been postulated in a
patient with MM with prolonged TT and RT, where TT
but not RT was corrected by the mixing of patients and
normal plasma.
80
Despite the relatively frequent abnor-
mal TT time, clinical bleeding manifestations are ob-
served only in a minority of patients, who possibly have
other associated hemostatic defects, such as a decreased
FX level, enhanced brinolysis due to a
2
-antiplasmin
deciency,
79
or vessel wall amyloid deposition.
81
The
primary role of plasma factors in the bleeding diathesis
is also suggested by the clinical response observed with
plasma exchange or large-volume plasmapheresis, in
particular in patients with Waldenstrom macroglobuli-
nemia.
82,83
The presence of circulating paraproteins with
vWF or FVIII inhibitory activity have been described
in patients with MGUS,
84
MM, Waldenstrom macro-
globulinemia, lymphoma, chronic lymphocytic leuke-
mia, and amyloidosis.
85,86
The presence of such factors
was associated with clinical symptoms of acquired von
Willebrand disease or hemophilia.
87,88
The addition of puried paraprotein to platelet-
rich plasma can impair platelet aggregation and release of
platelet factor 3.
89,90
A lambda dimeric protein puried
in a patient with IgD/lambda myeloma, who rapidly
developed a subcutaneous hematoma after puncture of
the inguinal artery, retained the ability to prolong PTT
and RVVT and to inhibit ristocetin-induced platelet
aggregation.
91
This lambda dimer showed both lupus
anticoagulant activity and inhibitory effect on vWF
glycoprotein Iba binding on the platelet surface, induc-
ing an acquired von Willebrand state.
91
The coexistence
of these two hemostatic alterations caused by the same
monoclonal protein is rare, but it has been observed in
several cases of paraproteinemias.
84
Other paraprotein-independent mechanisms can
determine laboratory or clinical hemostatic abnormalities.
Heparin-like anticoagulants have been identied in pa-
tients with MM with a prolonged TT, which was cor-
rected by addition of heparinase or protamine sulfate; the
latter was also able to control bleeding in one patient.
92,93
Excessive brinolysis has been reported in several
cases of MM and amyloidosis that manifested bleed-
ing diathesis and abnormal coagulation tests, such as
HEMOSTATIC DYSFUNCTION IN PARAPROTEINEMIAS AND AMYLOIDOSIS/ZANGARI ET AL 345
shortened clot lysis and elevated brin/brinogen deg-
radation products.
94
The pathogenesis of hyperbrinol-
ysis could be related to a reduced levels of a
2
-antiplasmin
or may be secondary to complex formation with plasmin;
increased urokinase-type plasminogen activator activity
also has been observed in a few other cases.
95
Treatment
with e-aminocaproic acid was efcacious in controlling
bleeding symptoms in some patients.
96
Accelerated clearance of coagulation proteins can
explain the hemostatic abnormalities in same cases. An
increased binding of vWF with monomeric IgM on the
surface of malignant cells has been described to induce
acquired von Willebrand disease in a patient with
Waldenstrom macroglobulinemia.
97
Bleeding symptoms
associated to acquired deciency of FX is a relatively
common feature in amyloidosis.
98
No evidence of a FX
inhibitor was demonstrated, but a rapid clearing from
circulation of I
131
-labeled FX and accumulation in areas
involved by amyloid deposits were shown by Furie
et al.
99
Quantitative afnity chromatography analysis
demonstrated that FX binds frequently to amyloid brils
in the spleen.
100,101
Splenectomy can produce resolution
of bleeding diathesis in some cases.
102,103
Hemorrhagic symptoms, in particular retinal
hemorrhages, epistaxis, and gingival bleeding, are char-
acteristic of the hyperviscosity syndrome, frequently
observed in Waldenstrom macroglobulinemia and less
commonly in MM.
104
Plasma exchange is an effective
treatment to reduce plasma viscosity and bleeding.
CONCLUSIONS
Hemostatic dysfunctions leading to thrombotic or hem-
orrhagic complications are common in patients with
paraproteinemias and amyloidosis. The use of antian-
giogenic agents in combination with steroids or chemo-
therapy further enhances the thrombotic risk.
The inammatory response associated with these
conditions and reduced natural anticoagulant mecha-
nisms are important factors that determine the thrombo-
philic state, even though specic paraprotein-linked
effects (such as lupus anticoagulant activity or inhibition
of brin polymerization) also are involved in several cases.
The coagulation abnormalities that are more frequently
observed in the presence of active disease can normalize
with effective treatment. Emerging data indicate that the
effect of LMWH in cancer and in MM is not conned to
the anticoagulant activity but extends to survival.
ABBREVIATIONS
APC activated protein C
b-FGF basic broblast growth factor
CRP C-reactive protein
doxo doxorubicin
GFC global brinolytic capacity
IL-6 interleukin 6
LMWH low molecular weight heparin
MGUS monoclonal gammopathy of undetermined
signicance
MM multiple myeloma
PT prothrombin time
PTT partial thromboplastin time
TNF-a tumor necrosis factor alpha
TT thrombin time
VAD vincristine/ adriamycin/dexamethasone
VEGF vascular endothelial growth factor
VTE venous thromboembolism
REFERENCES
1. Sallah S, Husain A, Wan J, Vos P, Nguyen NP. The risk of
venous thromboembolic disease in patients with monoclonal
gammopathy of undetermined signicance. Ann Oncol
2004;15(10):14901494
2. Srkalovic G, Cameron MG, Rybicki L, et al. Monoclonal
gammopathy of undetermined signicance and multiple
myeloma are associated with an increased incidence of
venothromboembolic disease. Cancer 2004;101(3):558566
3. Barlogie B, Desikan R, Eddlemon P, et al. Extended survival
in advanced and refractory multiple myeloma after single-
agent thalidomide: identication of prognostic factors in a
phase 2 study of 169 patients. Blood 2001;98(2):492494
4. Weber DM, Chen C, Niesvizky R, et al. Lenalidomide plus
high-dose dexamethasone provides improved overall survival
compared to high-dose dexamethasone alone for relapsed or
refractory multiple myeloma (MM): Results of a North
American phase III study (MM-009). J Clin Oncol 2006;
24(18S):7521 (abst)
5. Dimopoulos MA, Spencer A, Attal M, et al. Study of
lenalidomide plus dexamethasone versus dexamethasone
alone in relapsed or refractory multiple myeloma (MM):
results of a phase 3 study (MM-010). Blood 2005;106:6 (abst)
6. Rajkumar SV, Blood E, Vesole D, Fonseca R, Greipp PR, for
the Eastern Cooperative Oncology Group. Phase III clinical
trial of thalidomide plus dexamethasone compared with
dexamethasone alone in newly diagnosed multiple myeloma: a
clinical trial coordinated by the Eastern Cooperative Oncol-
ogy Group. J Clin Oncol 2006;24(3):431436
7. Osman K, Comenzo R, Rajkumar SV. Deep venous
thrombosis and thalidomide therapy for multiple myeloma.
N Engl J Med 2001;344(25):19511952
8. Singhal S, Mehta J, Desikan R, et al. Antitumor activity of
thalidomide in refractory multiple myeloma. N Engl J Med
1999;341(21):15651571
9. Tosi P, Zamagni E, Cellini C, et al. Salvage therapy with
thalidomide in patients with advanced relapsed/refractory
multiple myeloma. Haematologica 2002;87(4):408414
10. Kumar S, Gertz MA, Dispenzieri A, et al. Response rate,
durability of response, and survival after thalidomide therapy
for relapsed multiple myeloma. Mayo Clin Proc 2003;78(1):
3439
11. Anagnostopoulos A, Weber D, Rankin K, Delasalle K,
Alexanian R. Thalidomide and dexamethasone for resistant
multiple myeloma. Br J Haematol 2003;121(5):768771
12. Cavo M, Zamagni E, Tosi P, et al. First-line therapy with
thalidomide and dexamethasone in preparation for autologous
346 SEMINARS IN THROMBOSIS AND HEMOSTASIS/VOLUME 33, NUMBER 4 2007
stem cell transplantation for multiple myeloma. Haemato-
logica 2004;89(7):826831
13. Zangari M, Anaissie E, Barlogie B, et al. Increased risk of
deep-vein thrombosis in patients with multiple myeloma
receiving thalidomide and chemotherapy. Blood 2001;98(5):
16141615
14. Zangari M, Siegel E, Barlogie B, et al. Thrombogenic
activity of doxorubicin in myeloma patients receiving
thalidomide: implications for therapy. Blood 2002;100(4):
11681171
15. Biemond BJ, Havik SR, Meijers JCM, et al. Strong
thrombogenic activity of the combined administration of
thalidomide and doxorubicin in experimental thrombosis in
the rabbit. Blood 2003;102(11):554 (abst 2036)
16. Zangari M, Barlogie B, Thertulien R, et al. Thalidomide
and deep vein thrombosis in multiple myeloma: risk factors
and effect on survival. Clin Lymphoma 2003;4(1):3235
17. Cavenagh JD, Oakervee H, for the UK Myeloma Forum
and the BCSH Haematology/Oncology Task Forces.
Thalidomide in multiple myeloma: current status and future
prospects. Br J Haematol 2003;120(1):1826
18. Richardson PG, Schlossman RL, Weller E, et al. Immu-
nomodulatory drug CC-5013 overcomes drug resistance and
is well tolerated in patients with relapsed multiple myeloma.
Blood 2002;100(9):30633067
19. Richardson PG, Blood E, Mitsiades CS, et al. A
randomized phase 2 study of lenalidomide therapy for
patients with relapsed or relapsed and refractory multiple
myeloma. Blood 2006;108:34583464
20. Zangari M, Elice F, Tricot G. Immunomodulatory drugs in
multiple myeloma. Expert Opin Investig Drugs 2005;
14(11):14111418
21. Zonder JA, Barlogie B, Durie BG, et al. Thrombotic
complications in patients with newly diagnosed multiple
myeloma treated with lenalidomide and dexamethasone:
benet of aspirin prophylaxis. Blood 2006;108(1):403
22. Rajkumar SV, Hayman SR, Lacy MQ, et al. Combination
therapy with lenalidomide plus dexamethasone (Rev/Dex) for
newly diagnosed myeloma. Blood 2005;106(13):40504053
23. Srkalovic G, Cameron MG, Deitcher SR, Kattke-Marchant
K, Hussein MA. Incidence and risk factors of venous
thromboembolism (VTD) in patients with amyloidosis. Int
Semin Surg Oncol 2005;2:17
24. Halligan CS, Lacy MQ, Vincent Rajkumar S, et al. Natural
history of thromboembolism in AL amyloidosis. Amyloid
2006;13(1):3136
25. Sorensen HT, Mellemkjaer L, Olsen JH, Baron JA.
Prognosis of cancers associated with venous thromboemb-
olism. N Engl J Med 2000;343(25):18461850
26. Zacharski LR, Henderson WG, Rickles FR, et al. Effect of
warfarin anticoagulation on survival in carcinoma of the
lung, colon, head and neck, and prostate. Final report of VA
Cooperative Study #75. Cancer 1984;53(10):20462052
27. Barlogie B, Tricot G, Anaissie E, et al. Thalidomide and
hematopoietic-cell transplantation for multiple myeloma.
N Engl J Med 2006;354(10):10211031
28. Zangari M, Barlogie B, Cavallo F, et al. Effect on survival of
treatment associated venous thromboembolism in newly
diagnosed multiple myeloma patients. Blood Coagul
Fibrinolysis 2006. In press
29. OKane MJ, Wisdom GB, Desai ZR, Archbold GP.
Inhibition of brin monomer polymerisation by myeloma
immunoglobulin. J Clin Pathol 1994;47(3):266268
30. Gabriel DA, Smith LA, Folds JD, Davis L, Cancelosi SE.
The inuence of immunoglobulin (IgG) on the assembly of
brin gels. J Lab Clin Med 1983;101(4):545552
31. Carr ME Jr, Zekert SL. Abnormal clot retraction, altered
brin structure, and normal platelet function in multiple
myeloma. Am J Physiol 1994;266(3 Pt 2):H1195H1201
32. Carr ME Jr, Dent RM, Carr SL. Abnormal brin structure
and inhibition of brinolysis in patients with multiple
myeloma. J Lab Clin Med 1996;128(1):8388
33. Yagci M, Sucak GT, Haznedar R. Fibrinolytic activity in
multiple myeloma. Am J Hematol 2003;74(4):231237
34. van Marion AM, Auwerda JJ, Minnema MC, et al.
Hypobrinolysis during induction treatment of multiple
myeloma may increase the risk of venous thrombosis.
Thromb Haemost 2005;94(6):13411343
35. Duhren U, Paar D, Kolbel C, et al. Lupus anticoagulant
associated syndrome in benign and malignant systemic
diseaseanalysis of ten observations. Klin Wochenschr
1987; 65(18):852859
36. Bellotti V, Gambo G, Merlini G, et al. Study of three
patients with monoclonal gammopathies and lupus-like
anticoagulants. Br J Haematol 1989;73(2):221227
37. Takamiya O, Machida S, Okuda M, et al. A non-
immunological phospholipid-dependent coagulation inhib-
itor associated with IgG lambda-type multiple myeloma.
Am J Hematol 2004;75(1):3439
38. Tricot G. New insights into role of microenvironment in
multiple myeloma. Lancet 2000;355(9200):248250
39. Anderson K. Advances in the biology of multiple myeloma:
therapeutic applications. Semin Oncol 1999;26(5 suppl 13):
1022
40. Yasui H, Hideshima T, Richardson PG, et al. Novel
therapeutic strategies targeting growth factor signaling casca-
des in multiple myeloma. Br J Haematol 2006;132(4):385397
41. Barille S, Bataille R, Amiot M. The role of interleukin-6
and interleukin-6/interleukin-6 receptor-alpha complex in
the pathogenesis of multiple myeloma. Eur Cytokine Netw
2000;11(4):546551
42. Mechtcheriakova D, Wlachos A, Holzmuller H, et al.
Vascular endothelial cell growth factor-induced tissue factor
expression in endothelial cells is mediated by EGR-1. Blood
1999;93:38113823
43. Esmon CT. Possible involvement of cytokines in diffuse
intravascular coagulation and thrombosis. Baillieres Best
Pract Res Clin Haematol 1999;12(3):343359
44. Amrani DL. Regulation of brinogen biosynthesis: gluco-
corticoid and interleukin-6 control. Blood Coagul Fibrinol-
ysis 1990;1(45):443446
45. Stirling D, Hannant WA, Ludlam CA. Transcriptional
activation of the factor VIII gene in liver cell lines by
interleukin-6. Thromb Haemost 1998;79(1):7478
46. Minnema MC, Fijnheer R, De Groot PG, Lokhorst HM.
Extremely high levels of von Willebrand factor antigen and of
procoagulant factor VIII found in multiple myeloma patients
are associated with activity status but not with thalidomide
treatment. J Thromb Haemost 2003;1(3):445449
47. Green D, Maliekel K, Sushko E, Akhtar R, Soff GA.
Activated-protein-C resistance in cancer patients. Haemo-
stasis 1997;27(3):112118
48. Haim N, Lanir N, Hoffman R, Haim A, Tsalik M, Brenner
B. Acquired activated protein C resistance is common in
cancer patients and is associated with venous thromboemb-
olism. Am J Med 2001;110(2):9196
HEMOSTATIC DYSFUNCTION IN PARAPROTEINEMIAS AND AMYLOIDOSIS/ZANGARI ET AL 347
49. Zangari M, Saghafar F, Anaissie E, et al. Activated protein
C resistance in the absence of factor V Leiden mutation is a
common nding in multiple myeloma and is associated with
an increased risk of thrombotic complications. Blood Coagul
Fibrinolysis 2002;13(3):187192
50. Elice F, Fink L, Tricot G, Barlogie B, Zangari M. Acquired
resistance to activated protein C (aAPCR) in multiple
myeloma is a transitory abnormality associated with an
increased risk of venous thromboembolism. Br J Haematol
2006;134(4):399405
51. Hugo JZ, Jeanet DM. Acquired activated protein C
resistance and thrombosis in multiple myeloma patients.
Thromb J 2006;4:11
52. Esmon CT. The impact of the inammatory response on
coagulation. Thromb Res 2004;114(56):321327
53. Deitcher SR, Erban JK, Limentani SA. Acquired free
protein S deciency associated with multiple myeloma: a
case report. Am J Hematol 1996;51(4):319323
54. Otterson GA, Monahan BP, Harold N, et al. Clinical
signicance of the FV: Q506 mutation in unselected
oncology patients. Am J Med 1996;101(4):406412
55. Santos AB, Llamas P, Roman A, et al. Evaluation of throm-
bophilic states in myeloma patients receiving thalidomide: a
reasonable doubt. Br J Haematol 2003;122(1):159160
56. Rees DC, Cox M, Clegg JB. World distribution of factor V
Leiden. Lancet 1995;346(8983):11331134
57. Koster T, Rosendaal FR, de Ronde H, et al. Venous
thrombosis due to poor anticoagulant response to activated
protein C: Leiden Thrombophilia Study. Lancet 1993;
342(88868887):15031506
58. Rosendaal FR, Koster T, Vandenbroucke JP, Reitsma PH.
High risk of thrombosis in patients homozygous for factor V
Leiden (activated protein C resistance). Blood 1995;85(6):
15041508
59. Poort SR, Rosendaal FR, Reitsma PH, Bertina RM. A
common genetic variation in the 3
0
-untranslated region of
the prothrombin gene is associated with elevated plasma
prothrombin levels and an increase in venous thrombosis.
Blood 1996;88(10):36983703
60. Corso A, Lorenzi A, Terulla V, et al. Modication of
thrombomodulin plasma levels in refractory myeloma
patients during treatment with thalidomide and dexame-
thasone. Ann Hematol 2004;83(9):588591
61. Weber D, Ginsberg C, Walker P, et al. Correlation of
thrombotic/embolic events (T/E) with features of hyper-
coagulability in previously untreated patients before and
after treatment with thalidomide (T) or thalidomide-
dexamethasone (TD). Blood 2002;100(11):(abst 787)
62. Ward CM, Yen T, Harvie R, Pavlakis N. Elevated levels of
factor VIII and von Willebrand factor after thalidomide
treatment for malignancy: relationship to thromboembolic
events. Hematol J 2003;4(suppl 1):265 (abst)
63. Auwerda JJ, Sonneveld P, Leebeek FW. Temporary relief of
symptomatic Von Willebrand disease by multiple myeloma.
J Thromb Haemost 2005;3(5):10881089
64. Kyrle PA, Minar E, Hirschl M, et al. High plasma levels of
factor VIII and the risk of recurrent venous thromboemb-
olism. N Engl J Med 2000;343(7):457462
65. Hussein MA. Thromboembolism risk reduction in multiple
myeloma patients treated with immunomodulatory drug
combinations. Thromb Haemost 2006;95(6):924930
66. Sezer O, Jakob C, Eucker J, et al. Serum levels of the
angiogenic cytokines basic broblast growth factor (bFGF),
vascular endothelial growth factor (VEGF) and hepatocyte
growth factor (HGF) in multiple myeloma. Eur J Haematol
2001;66(2):8388
67. Vacca A, Scavelli C, Montefusco V, et al. Thalidomide
downregulates angiogenic genes in bone marrow endothelial
cells of patients with active multiple myeloma. J Clin Oncol
2005;23(23):53345346
68. Weber D, Rankin K, Gavino M, et al. Thalidomide alone or
with dexamethasone for previously untreated multiple
myeloma. J Clin Oncol 2003;21:1619
69. Cunningham MS, White B, Hollywood D, ODonnell J.
Primary thromboprophylaxis for cancer patients with central
venous cathetersa reappraisal of the evidence. Br J Cancer
2006;94(2):189194
70. Perret-Guillaume C, Wahl DG. Low-dose warfarin in
atrial brillation leads to more thromboembolic events
without reducing major bleeding when compared to
adjusted-dosea meta-analysis. Thromb Haemost 2004;
91(2):394402
71. Zangari M, Barlogie B, Anaissie E, et al. Deep vein
thrombosis in patients with multiple myeloma treated with
thalidomide and chemotherapy: effects of prophylactic and
therapeutic anticoagulation. Br J Haematol 2004;126(5):
715721
72. Lee AY, Levine MN. Venous thromboembolism and cancer:
risks and outcomes. Circulation 2003;107(23 suppl 1):I17I21
73. Minnema MC, Breitkreutz I, Auwerda JJ, et al. Prevention of
venous thromboembolism with low molecular-weight heparin
in patients with multiple myeloma treated with thalidomide
and chemotherapy. Leukemia 2004;18(12): 20442046
74. Lee AY, Levine MN, Baker RI, et al. Randomized
Comparison of Low-Molecular-Weight Heparin versus
Oral Anticoagulant Therapy for the Prevention of Recurrent
Venous Thromboembolism in Patients with Cancer
(CLOT) Investigators. Low-molecular-weight heparin ver-
sus a coumarin for the prevention of recurrent venous
thromboembolism in patients with cancer. N Engl J Med
2003;349(2):146153
75. Baz R, Li L, Kottke-Marchant K, et al. The role of aspirin
in the prevention of thrombotic complications of thalido-
mide and anthracycline-based chemotherapy for multiple
myeloma. Mayo Clin Proc 2005;80(12):15681574
76. Liebman HA, Benz EJJ, Shattil SJ, et al. Hemostatic defects
associated with dysproteinemias. In: Hoffman R, et al, eds.
Hematology: Basic Principles and Practice. 3rd ed. New
York: Churchill Livingstone; 2000:19962000
77. Perkins HA, MacKenzie MR, Fudenberg HH. Hemostatic
defects in dysproteinemias. Blood 1970;35(5):695707
78. Kyle RA, Gertz MA. Primary systemic amyloidosis: clinical
and laboratory features in 474 cases. Semin Hematol 1995;
32:4559
79. Gamba G, Montani N, Anesi E, et al. Clotting alterations
in primary systemic amyloidosis. Haematologica 2000;85(3):
289292
80. Saif MW, Allegra CJ, Greenberg B. Bleeding diathesis in
multiple myeloma. J Hematother Stem Cell Res 2001;10(5):
657660
81. Hoshino Y, Hatake K, Muroi K, et al. Bleeding tendency
caused by the deposit of amyloid substance in the
perivascular region. Intern Med 1993;32(11):879881
82. Beardell FV, Varma M, Martinez J. Normalization of
plasma factor X levels in amyloidosis after plasma exchange.
Am J Hematol 1997;54(1):6871
348 SEMINARS IN THROMBOSIS AND HEMOSTASIS/VOLUME 33, NUMBER 4 2007
83. Gertz MA, Kyle RA. Hyperviscosity syndrome. J Intensive
Care Med 1995;10:128141
84. Taher A, Abiad R, Uthman I. Coexistence of lupus
anticoagulant and acquired haemophilia in a patient with
monoclonal gammopathy of unknown signicance. Lupus
2003;12(11):854856
85. Mohri H, Noguchi T, Kodama F, Itoh A, Ohkubo T.
Acquired von Willebrand disease due to inhibitor of human
myeloma protein specic for von Willebrand factor. Am J
Clin Pathol 1987;87(5):663668
86. Loftus LS, Arnold WN. Acquired hemophilia in a patient
with myeloma. West J Med 1994;160(2):173176
87. Federici AB, Stabile F, Castaman G, Canciani MT,
Mannucci PM. Treatment of acquired von Willebrand
syndrome in patients with monoclonal gammopathy of
uncertain signicance: comparison of three different ther-
apeutic approaches. Blood 1998;92(8):270727011
88. Hayashi T, Yagi H, Suzuki H, et al. Low-dosage intra-
venous immunoglobulin in the management of a patient
with acquired von Willebrand syndrome associated with
monoclonal gammopathy of undetermined signicance.
Pathophysiol Haemost Thromb 2002;32(1):3339
89. Cohen I, Amir J, Ben-Shaul Y, Pick A, De Vries A. Plasma
cell myeloma associated with an unusual myeloma protein
causing impairment of brin aggregation and platelet
function in a patient with multiple malignancy. Am J Med
1970;48(6):766776
90. Penny R, Castaldi PA, Whitsed HM. Inammation and
haemostasis in paraproteinaemias. Br J Haematol 1971;
20(1):3544
91. Shinagawa A, Kojima H, Berndt MC, et al. Character-
ization of a myeloma patient with a life-threatening
hemorrhagic diathesis: presence of a lambda dimer protein
inhibiting shear-induced platelet aggregation by binding to
the A1 domain of von Willebrand factor. Thromb Haemost
2005;93(5):889896
92. Chapman GS, George CB, Danley DL. Heparinlike
anticoagulant associated with plasma cell myeloma. Am J
Clin Pathol 1985;83:764766
93. Kaufman PA, Gockerman JP, Greenberg CS. Production of a
novel anticoagulant by neoplastic plasma cells: report of a case
and review of the literature. Am J Med 1989;86(5):612616
94. Liebman H, Chinowsky M, Valdin J, Kenoyer G, Feinstein
D. Increased brinolysis and amyloidosis. Arch Intern Med
1983;143(4):678682
95. Liebman HA, Carfagno MK, Weitz IC, et al. Excessive
brinolysis in amyloidosis associated with elevated plasma
single-chain urokinase. AmJ Clin Pathol 1992;98(5):534541
96. Sane DC, Pizzo SV, Greenberg CS. Elevated urokinase-
type plasminogen activator level and bleeding in amyloi-
dosis: case report and literature review. Am J Hematol 1989;
31(1):5357
97. Brody JI, Haidar ME, Rossman RE. A hemorrhagic
syndrome in Waldenstro ms macroglobulinemia secondary
to immunoadsorption of factor VIII. Recovery after
splenectomy. N Engl J Med 1979;300(8):408410
98. Greipp PR, Kyle RA, Bowie EJ. Factor-X deciency in
amyloidosis: a critical review. Am J Hematol 1981;11(4):
443450
99. Furie B, Greene E, Furie BC. Syndrome of acquired factor
X deciency and systemic amyloidosis in vivo studies of the
metabolic fate of factor X. N Engl J Med 1977;297(2):8185
100. Furie B, Voo L, McAdam KP, Furie BC. Mechanism of
factor X deciency in systemic amyloidosis. N Engl J Med
1981;304(14):827830
101. Galbraith PA, Sharma N, Parker WL, Kilgour JM.
Acquired factor X deciency. Altered plasma antithrombin
activity and association with amyloidosis. JAMA 1974;
230(12):16581660
102. Greipp PR, Kyle RA, Bowie EJ. Factor X deciency in
primary amyloidosis: resolution after splenectomy. N Engl J
Med 1979;301(19):10501051
103. Rosenstein ED, Itzkowitz SH, Penziner AS, Cohen JI,
Mornaghi RA. Resolution of factor X deciency in primary
amyloidosis following splenectomy. Arch Intern Med 1983;
143(3):597599
104. Gertz MA, Fonseca R, Rajkumar SV. Waldenstroms
macroglobulinemia. Oncologist 2000;5(1):6367
105. Weber D, Albitar M, Delasalle K, et al. Correlation of
peripheral blood plasma levels of angiogenesis factors with
treatment of thalidomide (T) or thalidomide - dexame-
thasone (TD) in previously untreated patients with
multiple myeloma (MM). Blood 2002;100(11):808809
(abst 3193)
106. Neben K, Moehler T, Kraemer A, et al. Response to
thalidomide in progressive multiple myeloma is not mediated
by inhibition of angiogenic cytokine secretion. Br J Haematol
2001;115(3):605608
107. Bertolini F, Mingrone W, Alietti A, et al. Thalidomide in
multiple myeloma, myelodysplastic syndromes and histio-
cytosis. Analysis of clinical results and of surrogate angio-
genesis markers. Ann Oncol 2001;12(7):987990
108. Dmoszynska A, Bojarska-Junak A, Domanski D, et al.
Production of proangiogenic cytokines during thalidomide
treatment of multiple myeloma. Leuk Lymphoma 2002;
43(2):401406
109. Hassoun H, Reich L, Klimek VM, et al. Doxorubicin and
dexamethasone followed by thalidomide and dexamethasone
is an effective well tolerated initial therapy for multiple
myeloma. Br J Haematol 2006;132(2):155161
110. Palumbo A, Betrola A, Falco P, et al. Efcacy of low-dose
thalidomide and dexamethasone as rst salvage regimen in
multiple myeloma. Hematol J 2004;5(4):318324
111. Facon T, Mary JY, Hulin C, et al. Major superiority of
melphalanprednisone (MP) thalidomide (THAL) over
MP and autologous stem cell transplantation in the
treatment of newly diagnosed elderly patients with multiple
myeloma. Blood 2005;106:230 (abst 780)
112. Palumbo A, Rus C, Zeldis JB, Rodeghiero F, Boccadoro M.
Italian Multiple Myeloma Network, Gimema. Enoxaparin
or aspirin for the prevention of recurrent thromboembolism
in newly diagnosed myeloma patients treated with melpha-
lan and prednisone plus thalidomide or lenalidomide.
J Thromb Haemost 2006;4(8):18421845
113. Zervas K, Dimopoulos MA, Hatzicharissi E, et al. Greek
Myeloma Study Group. Primary treatment of multiple
myeloma with thalidomide, vincristine, liposomal doxor-
ubicin and dexamethasone (T-VAD doxil): a phase II
multicenter study. Ann Oncol 2004;15(1):134138
114. Chanan-Khan AA, Miller KC, McCarthy P, et al. VAD-t
(vincristine, adriamycin, dexamethasone and low-dose
thalidomide) is an effective initial therapy with high
response rates for patients with treatment naive multiple
myeloma (MM). Blood 2004;104:943944 (abst 3463)
HEMOSTATIC DYSFUNCTION IN PARAPROTEINEMIAS AND AMYLOIDOSIS/ZANGARI ET AL 349
Potrebbero piacerti anche
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Pericardial Disease: Adel Hasanin Ahmed 1Documento5 paginePericardial Disease: Adel Hasanin Ahmed 1Shaz ChindhyNessuna valutazione finora
- ACCP Board Review 21st EditionDocumento491 pagineACCP Board Review 21st Editionphathands_311721694100% (2)
- Cong HeartDocumento7 pagineCong HeartShaz ChindhyNessuna valutazione finora
- Me 1Documento74 pagineMe 1Shaz ChindhyNessuna valutazione finora
- Lac+Usc Internal Medicine Residency Survival Guide 2013-2014Documento226 pagineLac+Usc Internal Medicine Residency Survival Guide 2013-2014Shaz ChindhyNessuna valutazione finora
- Endocrine Learning ObjDocumento2 pagineEndocrine Learning ObjShaz ChindhyNessuna valutazione finora
- ST NoDocumento89 pagineST NoShaz Chindhy100% (1)
- MKSAPDocumento2 pagineMKSAPShaz ChindhyNessuna valutazione finora
- Alcohol Dependednce Vs Abuse: Best TX Is Conseling + Drug. Combining Drugs Is NOT More EfficatiousDocumento4 pagineAlcohol Dependednce Vs Abuse: Best TX Is Conseling + Drug. Combining Drugs Is NOT More EfficatiousShaz ChindhyNessuna valutazione finora
- I. Definition/General Considerations: Colon CancerDocumento2 pagineI. Definition/General Considerations: Colon CancerShaz ChindhyNessuna valutazione finora
- I. Definition/General Consideration: Acute Asthma ExacerbationDocumento2 pagineI. Definition/General Consideration: Acute Asthma ExacerbationShaz ChindhyNessuna valutazione finora
- IMDocumento128 pagineIMShaz ChindhyNessuna valutazione finora
- All of Medicine FlashcardsDocumento142 pagineAll of Medicine FlashcardsShaz Chindhy100% (2)
- Cardio AnswersDocumento26 pagineCardio AnswersShaz ChindhyNessuna valutazione finora
- I. Definition/General Considerations: HypercalcemiaDocumento2 pagineI. Definition/General Considerations: HypercalcemiaShaz ChindhyNessuna valutazione finora
- Diabetes: Foot ExamDocumento4 pagineDiabetes: Foot ExamShaz ChindhyNessuna valutazione finora
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- CC CM Isbb Histopath Mtlaw ReviewerDocumento26 pagineCC CM Isbb Histopath Mtlaw ReviewerAnne MorenoNessuna valutazione finora
- XN-1500 10p ENDocumento5 pagineXN-1500 10p ENHarika PutraNessuna valutazione finora
- Bleeding DisordersDocumento10 pagineBleeding Disorderslyli Star AngeloNessuna valutazione finora
- Gambaran Asuhan Keperawatan Pada Pasien Hipertensi Dengan Gangguan Kebutuhan Rasa Nyaman NyeriDocumento8 pagineGambaran Asuhan Keperawatan Pada Pasien Hipertensi Dengan Gangguan Kebutuhan Rasa Nyaman NyeriGhaniNessuna valutazione finora
- The Epiphyseal Plate: Physiology, Anatomy, and TraumaDocumento12 pagineThe Epiphyseal Plate: Physiology, Anatomy, and TraumaLaura Mérida CáceresNessuna valutazione finora
- Platelet Rich Plasma (PRP) and Platelet Rich Fibrin (PRF) : Rencana Pengajuan Penelitian TesisDocumento10 paginePlatelet Rich Plasma (PRP) and Platelet Rich Fibrin (PRF) : Rencana Pengajuan Penelitian TesisrachmadyNessuna valutazione finora
- ReportDocumento4 pagineReportRancho AmithNessuna valutazione finora
- VKDBDocumento34 pagineVKDBCHANDREN ARUMUGAMNessuna valutazione finora
- BC-5300 VetDocumento2 pagineBC-5300 VetlijianaNessuna valutazione finora
- Extending The Reach of Cardiovascular AutotransfusionDocumento6 pagineExtending The Reach of Cardiovascular AutotransfusionManigandan DhamodhiranNessuna valutazione finora
- Virtual Long Bone Dissection-2Documento2 pagineVirtual Long Bone Dissection-2api-435871995Nessuna valutazione finora
- Blood Groups Assignment AaaDocumento3 pagineBlood Groups Assignment AaaLoro JDNessuna valutazione finora
- Quality Assurance in The Blood BankDocumento41 pagineQuality Assurance in The Blood Bankgauravmahajan4480% (5)
- IMHM321 Lecture Trans 3Documento9 pagineIMHM321 Lecture Trans 3Brix BrixNessuna valutazione finora
- Evaluation of The Ruminant Complete Blood Dell CountDocumento26 pagineEvaluation of The Ruminant Complete Blood Dell CountDirección Científica Laboratorio VitalabNessuna valutazione finora
- Blood GroupDocumento12 pagineBlood Groupalive computerNessuna valutazione finora
- CH 6 Muscular SystemDocumento51 pagineCH 6 Muscular SystemNAMERAH GOTENessuna valutazione finora
- Blood Bank Nca-Cls Q'S: Terms in This SetDocumento18 pagineBlood Bank Nca-Cls Q'S: Terms in This SetjustinNessuna valutazione finora
- Haematology AnalyzerDocumento78 pagineHaematology Analyzerswaraj sharmaNessuna valutazione finora
- The Man With The Golden Blood - MosaicDocumento11 pagineThe Man With The Golden Blood - MosaicagxzNessuna valutazione finora
- Important Tables of Oral PathologyDocumento17 pagineImportant Tables of Oral PathologyEasy Med LecturesNessuna valutazione finora
- Coagulation TestsDocumento25 pagineCoagulation Testsdave_1128Nessuna valutazione finora
- Blood WorksheetDocumento5 pagineBlood Worksheetapi-296199660100% (1)
- Case 5 - (Salimbagat) Diagnostic and Laboratory ProceduresDocumento12 pagineCase 5 - (Salimbagat) Diagnostic and Laboratory ProceduresChristine Pialan SalimbagatNessuna valutazione finora
- Grafik QC Hematologi 2023 BaruDocumento125 pagineGrafik QC Hematologi 2023 BaruSyifa nurfitriNessuna valutazione finora
- Activity 11 Discussion Serum Plasma Preparation Centrifuging and TransferringDocumento3 pagineActivity 11 Discussion Serum Plasma Preparation Centrifuging and TransferringErin De LaraNessuna valutazione finora
- Anatomy Lec 9 (Muscles)Documento21 pagineAnatomy Lec 9 (Muscles)HumrazNessuna valutazione finora
- Lab ReportDocumento2 pagineLab ReportSamir Kumar DashNessuna valutazione finora
- UNIT 1 (Anatomy & Physiology)Documento11 pagineUNIT 1 (Anatomy & Physiology)Workinesh Kaynabo KambaloNessuna valutazione finora
- Reference For Assignment 2Documento2 pagineReference For Assignment 2chrisNessuna valutazione finora