Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Nutrition
Caricato da
vijaya_ojha0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
22 visualizzazioni7 pagineOverview Mineral
Copyright
© © All Rights Reserved
Formati disponibili
PDF, TXT o leggi online da Scribd
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoOverview Mineral
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato PDF, TXT o leggi online su Scribd
0 valutazioniIl 0% ha trovato utile questo documento (0 voti)
22 visualizzazioni7 pagineNutrition
Caricato da
vijaya_ojhaOverview Mineral
Copyright:
© All Rights Reserved
Formati disponibili
Scarica in formato PDF, TXT o leggi online su Scribd
Sei sulla pagina 1di 7
1
University of Papua New Guinea
School of Medicine and Health Sciences
Division of Basic Medical Sciences
M. Med Part I
Lecture: Some Aspects of Nutrition
Micronutrient deficiency, now referred to as Vitamin and Mineral Deficiency (VMD), is
widespread among women and children in resource limited (developing) countries
VMD deprives about a billion people world-wide of their Intellect, Strength and Vitality
Individuals with multiple deficiencies are in a state of Micronutrient Starvation
o They suffer from the Hidden Hunger that secretly suppresses their immune
response, increasing the risk of developing infectious diseases
Adequate amount of Micronutrients are needed at all ages,
Effects of inadequate intake are particularly serious during periods of rapid growth,
pregnancy, lactation and early childhood
Iron, Zinc, Iodine and Selenium among others are very important for Physical and Cognitive
development of children
How important is Iodine?
Iodine is essential for biosynthesis of Thyroid hormones:
o Thyroxine (T 4) and Tri-Iodothyronine (T 3)
Inadequate intake of dietary iodine or regular consumption of diet containing anti-metabolites
(Goitrogens) of Iodine metabolism can impair biosynthesis of Thyroid hormones, leading to a
Spectrum of diseases: Iodine Deficiency Disorders (IDD)
Iodine Deficiency (ID) is regarded as the single most common cause of preventable mental
retardation and brain damage in a population where the intake of iodine is insufficient
Severe ID that leads to Endemic Cretinism has been reduced World-wide because of
implementation of dietary iodine supplementation programs {Universal Salt Iodization (USI)
strategy}
What are some of the consequences of Iodine deficiency?
Some clinical consequences of ID:
o Severity can vary from Mild Intellectual Blunting to Frank Cretinism,
May include Gross Mental Retardation, Deaf Mutism, Short Stature, and various
other defects
o Mild to Moderate ID is prevalent in several countries including PNG
o Of great prevalence are the more subtle degrees of mental impairment, which occur in
apparently normal children with low dietary intake of iodine
Manifestations range from small neurological changes, to impaired learning
ability and underperformance in school, including poor performance on formal
tests of Psychomotor functions
Dietary ID in Pregnant and Lactating women may have serious consequences:
o Maternal ID can compromise the Thyroid status of the Fetus and Neonate
Maternal Thyroxine (T4) is required for Neurodevelopment of Fetus during the
first half of gestation
Fetal Neurodevelopment is most vulnerable to damage during early gestation in
women with Mild to Moderate ID
Maternal milk is major source of Iodine for Thyroid hormone in Neonates
Importance of adequate intake of Iodine by Lactating mothers cannot be overemphasized
2
In women of childbearing age: ID can cause Infertility and set the stage for Miscarriage,
Abortion, or Stillbirth during pregnancy
What are some of the metabolic functions of Zinc?
Zinc is present in over 300 Metallo-proteins with wide range of biochemical functions
Metallo-proteins that require Zinc for normal functioning include:
Regulatory and transport proteins such as:
o Gustin:
Polypeptide in Saliva that is essential for normal development of Taste buds,
(this account for the decreased taste acuity in Zn deficient individuals)
o Metallothionein: (Zn induces biosynthesis of MT in GIT)
o Gene-Regulatory Proteins (e.g., Zinc fingers involved in sequence-specific
DNA recognition and Gene expression)
Nucleoproteins that are involved in DNA Replication and Transcription
Zn as Co-factors for many Enzymes:
o Carbonic Anhydrase (regulation of HCO
3
-
ion),
o Alcohol Dehydrogenase:
Alcohol causes increase loss of Zinc in urine
o Nucleoside Phosphorylase:
Decrease activity cause by Zinc deficiency may result in accumulation of
toxic levels of Nucleotides, leading to impaired cell division or cell death
o Alkaline Phosphatase (ALP); Lactate Dehydrogenase (LDH),
o Glutamine Synthetase; Glutamate Dehydrogenase (GDH),
o Prolyl Hydroxylase:
Plays major role in post-translational modification of Collagen
o Porphobilinogen (PBG) Synthase:
Plays major role in biosynthesis of Heme,
o RNA and DNA Polymerases,
Zn acts to modulate metabolism of Vitamin A:
o Biosynthesis of Retinol-binding protein
o Conversion of Retinol to Retinal:
o A process that is necessary for vision, thus the impaired dark adaptation in
Zn deficient individuals
o Transportation of Retinol from Liver, to other organs is possible only if
hepatocellular secretion can take place via Zinc accumulation on Retinol-binding
protein
ZINC NUTRITURE IN INFANTS:
First Six months of life: Period of rapid growth, and Zn intake varies with the mode of
feeding
Relatively high Zinc requirements during this period can be met satisfactory from breast -
milk alone for most healthy infants
o Healthy breast-fed infants usually do not develop Zinc deficiency, because of the
High Bioavailability (80%) of Zinc in breast milk,
3
Cows milk contains higher Zinc content than human breast milk, but the bioavailability
(35%) is lower
o Difference in Bioavailability is due to higher levels of Citrate and Lactoferin in
Human breast milk, compared to high Phytates, Calcium and Casein in Cows milk
From Six months to two years of age, adequacy of Zinc intake becomes highly dependent
on the amount and bioavailability of Zinc from Complementary foods
o Breast-fed infants, and Low birth weight infants may be at risk for Zinc deficiency
because of:
Increased requirements,
Potentially lower intake and/or
Lower absorption efficiency
Zinc content of breast milk falls with duration of lactation
Prolonged breast-feeding without adequately prepared Complementary foods may reduce
Zinc intake, thereby increasing the risk of Zinc deficiency in infants
Zinc deficiency may occur in children fed with Cows milk, because of the high levels of
Phytate, Calcium and Casein that impairs Zinc absorption
Same holds true for Soymilk, which contains high levels of Phytate
NB:
Zinc supplementation enhances Linear Growth and significantly reduces incidence of
Anemia in children
o Stunted children benefit more than non-stunted children;
o Children up to 24 months of age benefit more than older children
SELENIUM (Se):
Selenium is a co-factor in Glutathione Peroxidase, a major Antioxidant in cells
Selenium is an essential component of De-Iodinase (Type 1) that catalyzes conversion of
Thyroxine (T
4
) to Tri-Iodothyronine (T
3
)
o De-Iodinase contains a specific Amino Acid called Seleno-Cysteine
Conversion of T4 to Reverse T3 is catalyzed by enzyme called 5-De-Iodinase that does not
require Selenium
o Deficiency of Selenium results in decreased conversion of T4 to T3,
which at the same time causes an increase in the conversion of T4 to reverse
T3 (rT3), by 5-Deiodinase that does not contain Seleno-Cysteine
Deficiency of both Selenium and Iodine causes severe condition Myxoedematous Cretinism
How is Vitamin A transported in blood?
Vitamin A in blood is transported bound to Retinol Binding Protein (RBP) and
Transthyrethrin (TTR) in 1:1:1 molar ratio
RBP is produced in liver as Apo-RBP
RBP in circulation with vitamin A is called Holo-RBP
In individual with normal status of Vitamin A, Apo-RBP is not released in significant
amount from liver unless vitamin A is available to form Holo-RBP
In well-nourished individuals 85 90% of Vitamin A is transported in blood as Holo-RBP
What are some of the functions of Vitamin A?
Vitamin A is involved in Visual cycle
o Rhodopsin = 11-cis-Retinal + Opsin
4
Vitamin A is involved in biosynthesis of Transferrin (Iron transporter)
o Vitamin A deficiency causes non-responsive Iron deficiency anemia
Vitamin A is involved in regulation of growth and differentiation
o It is essential for biosynthesis of:
Glycoproteins required for normal growth regulation
Glycosaminoglycans (GAGs), which are components of Mucus (Mucin)
secreted by epithelial cells
In Vitamin A deficiency status:
o Differentiation process slows down,
o Keratin producing cells replace Mucin-producing cells in epithelial tissues in the
Eyes, Lungs and Gut
o Reduction in Mucus secretion leads to drying of epithelial tissues in the Eyes, Lungs
and Gut,
o Excess Keratin production causes Keratinization (e.g., in eye causing
Xerophthalmia (dry eye) which can result in blindness
Water soluble Vitamins: Biological active forms and Metabolic Functions
Common Names &
Chemical Nature
Biologically Active /
Coenzyme forms
Metabolic functions of biologically
active forms
Thiamine or
Vitamin B
1
Thiamine Pyrophosphate
(TPP)
Coenzyme in Oxidative Decarboxylase
reactions (Pyruvate, Alpha-Oxo-Glutarate,
Alpha-Ketobutyrate
Riboflavin or
Vitamin B
2
Flavin Adenine-
Dinucleotide (FAD),
Flavin Adenine-
Mononucleotide
(FMN)
Coenzyme in some Dehydrogenase
reactions, and in some Red-Ox reactions
Niacin: Nicotinic
Acid; Nicotinamide
Nicotinamide
Adenine-Dinucleotide
(NAD)
Nicotinamide
Adenine Dinucleotide
Phosphate (NADP)
Coenzyme in several Dehydrogenase
reactions, and in several Red-Ox reactions
Pyridoxine,
Pyridoxal,
Pyridoxamine
(Vitamin B
6
)
Pyridoxal-Phosphate
(B
6
-Phosphate)
Coenzyme in several enzymes: Amino
Acid Decarboxylase, Transaminases,
Delta-amino-Laevulinic Acid Synthetase
(ALA-Synthase)
Pantothenic Acid Coenzyme A,
Acyl-carrier Protein
(ACP)
Carrier of Acyl groups in Acylation
reactions
Cobalamin
(Vitamin B
12
)
Methyl-Cobalamin,
5-Deoxyadenosyl
Cobalamin
Coenzyme for One-carbon transfer
reactions (-CH
3
)
Folic Acid, Folate,
Foliacin (Vitamin M)
Tetra-hydro-folic acid, Tetra-
hydro-Folate (FH
4
, or THF)
Coenzyme for One-carbon transfer
reactions
Ascorbic Acid,
(Vitamin C)
L-Ascorbic Acid, Dehydro-
Ascorbate
Reducing Agent (electron donor),
Antioxidant
Biotin Prosthetic group of
Carboxylases
Carrier of active CO
2
in carboxylation
reactions
5
Fat Soluble Vitamins: Biological active forms and Metabolic Functions
Common Names &
Chemical Nature
Biological Active Forms Metabolic functions of Active
forms
Retinol (Vitamin A),
All trans Retinol
11-cis Retinal, Prosthetic group in visual
pigments,
Cofactor role in biosynthesis
of Cholesterol,
Role in membrane
biogenesis
Role in cell differentiation
Cholecalciferol
(Vitamin D
3
)
Calciferol or
Ergocalciferol
(Vitamin D
2
)
1,25-Dihydroxy-
Cholecalciferol,
1,25-DihydroxyVitamin D
3
Absorption of Calcium in
GIT,
Reabsorption &
Mobilization of Calcium
and Phosphate in Bone
Tocopherols (Vitamin E) Alpha-Tocopherol, Beta-
Tocopherol
Antioxidants protecting
polyunsaturated fatty acids in
membranes,
Phytomenadione (Vitamin K) Vitamin K Cofactor in Post-translational
gamma-carboxylation of N-terminal
Glutamic acid residue in blood
clotting factors
What is the energy and macronutrient intake for People living with HIV/AIDS?
HIV/AIDS specifically affects Nutritional status of PLWHA because it:
o Increases energy requirements, Reduces food intake, and Adversely affecting
nutrient absorption and metabolism
Responsiveness of PLWHA to nutritional interventions depends on:
o Viral load, Stage of the disease, Concurrent treatment, Body Mass Index and
Presence or absence of Opportunistic Infections
PLWHA have greater energy needs than uninfected individuals,
o Extent of increased energy needs depends on progression and stage of HIV infection
In Asymptomatic PLWHA:
o Energy needs are 10% higher than the accepted levels for healthy non-HIV infected
persons of the same age, sex and physical activity level
o Increase energy is needed to maintain body weight and physical activity, which are
highly desirable for preserving quality of life
In PLWHA with symptoms or any opportunistic infection:
o Energy needs are 20% to 30% higher than the acceptable level for health non-HIV
infected persons of the same age, sex and physical activity level
Increase energy is needed to support weight recovery during and after HIV
related illnesses
6
The 20 to 30% increase in energy intake may not be easily achievable because of poor
appetite, inadequate dietary intake or other reasons caused by acute infection/illness
However, food intake should be encouraged and increased to the extent possible,
particularly during the period of recovery
Estimated increased energy requirements are to:
Compensate for increased level of Resting Energy Expenditure (REE)
Allow for normal Activity-related Energy Expenditure (AEE),
Both of which together represent the Total Energy Expenditure (TEE)
o TEE = REE + AEE
Amount of Macronutrients consumed by PLWHA should be the same as for non-HIV
infected adults
Recommended ranges of values are that:
Proteins should contribute 12% to 15% of total energy intake;
Fat should contribute about 30% to 35% of total energy intake
Carbohydrates should contribute about 50 55% of total energy intake
UNGASS Declaration:
o Declaration of the commitment by United Nations General Assembly Special Session
(UNGASS) dedicated to HIV/AIDS recognizes the need to integrate Food Support as part of a
Comprehensive Response to HIV/AIDS
o UNGASS Declaration of June 2006, Article 28 States that:
all people at all times, will have access to Sufficient, Safe, and Nutritious Food
to meet their dietary needs and food preferences for an Active and Healthy Life, as
part of a comprehensive response to HIV/AIDS
o According to the UNGASS Declaration:
All member states of the United Nations General Assembly MUST recognized that
where Anti-Retroviral Therapy is necessary, Food is a Key Element in Strategies to
Promote Adherence to it and its efficacy
o Efficacy of HAART treatment partly depends on the nutritional status of PLWHA
o Therefore, Nutritional Assessment and Counseling should be an integral part of all HIV/AIDS
treatment programs
ANTHROPOMETRY: Nutritional Status of infants using WHO Anthro 2005 Software:
Please See the attached CD containing the WHO Anthro 2005 Software
Read the two papers attached to this lecture notes
Reference:
1. Textbook of Biochemistry with Clinical Correlations, 4
th
Ed, Edited by T. M. Delvin,
Wiley-Liss, Brisbane, 1993; 1127 1128.
2. Shils ME, Olson JA, Shike M, Ross AC, eds. Modern Nutrition in Health and Disease 9
th
Edition. Lippincott Williams & Wilkins, Sydney 1998; 223 239, 741 742.
7
3. Briefing Paper No. 7: WHO document on-line Publications@odi.com: World Health
Organization, Geneva August 2006: 1 3
4. Castleman T, Seamon-Fosso E, Cogill B. Food and nutrition implications of antiretroviral
therapy in resource limited setting. Food and Nutrition Technical Assistance; Technical
Notes No. 7, Revised May 2004; 2 13.
5. WHO; Nutrient Requirements for People Living with HIV/AID: Report of a Technical
Consultation, World Health Organization, Geneva, 13 15 May 2003
6. WHO; Nutrition and HIV/AIDS: Report by the Secretariat. 59
th
World Health Assembly;
Provisional Agenda Item 11.3; A59/7, May 2006.
7. U. S. Presidents Emergency Plan for AIDS Relief (US PEPAR): Report on Food and
Nutrition for People Living with HIV/AIDS. Submitted by the office of the U.S. Global
AIDS Coordinator, U.S. Department of State: May 2006
Potrebbero piacerti anche
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceDa EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceValutazione: 4 su 5 stelle4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeDa EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeValutazione: 4 su 5 stelle4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeDa EverandShoe Dog: A Memoir by the Creator of NikeValutazione: 4.5 su 5 stelle4.5/5 (537)
- Grit: The Power of Passion and PerseveranceDa EverandGrit: The Power of Passion and PerseveranceValutazione: 4 su 5 stelle4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)Da EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Valutazione: 4 su 5 stelle4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingDa EverandThe Little Book of Hygge: Danish Secrets to Happy LivingValutazione: 3.5 su 5 stelle3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItDa EverandNever Split the Difference: Negotiating As If Your Life Depended On ItValutazione: 4.5 su 5 stelle4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureDa EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureValutazione: 4.5 su 5 stelle4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryDa EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryValutazione: 3.5 su 5 stelle3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerDa EverandThe Emperor of All Maladies: A Biography of CancerValutazione: 4.5 su 5 stelle4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaDa EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaValutazione: 4.5 su 5 stelle4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersDa EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersValutazione: 4.5 su 5 stelle4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealDa EverandOn Fire: The (Burning) Case for a Green New DealValutazione: 4 su 5 stelle4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyDa EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyValutazione: 3.5 su 5 stelle3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnDa EverandTeam of Rivals: The Political Genius of Abraham LincolnValutazione: 4.5 su 5 stelle4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaDa EverandThe Unwinding: An Inner History of the New AmericaValutazione: 4 su 5 stelle4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreDa EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreValutazione: 4 su 5 stelle4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Da EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Valutazione: 4.5 su 5 stelle4.5/5 (121)
- Her Body and Other Parties: StoriesDa EverandHer Body and Other Parties: StoriesValutazione: 4 su 5 stelle4/5 (821)
- Self-Operated Temperature Regulators Temperature Regulator Type 1Documento6 pagineSelf-Operated Temperature Regulators Temperature Regulator Type 1Pocola AdrianNessuna valutazione finora
- Operator'S Manual Px01X-Xxx-Xxx-Axxx: 1/4" Diaphragm PumpDocumento12 pagineOperator'S Manual Px01X-Xxx-Xxx-Axxx: 1/4" Diaphragm PumpAir PumpingNessuna valutazione finora
- 11 Iajps11072017Documento7 pagine11 Iajps11072017Baru Chandrasekhar RaoNessuna valutazione finora
- 0653 - w12 - QP - 11 (Combined)Documento20 pagine0653 - w12 - QP - 11 (Combined)MCHNessuna valutazione finora
- Experiments 11 15 NotesDocumento16 pagineExperiments 11 15 Notesforisko05Nessuna valutazione finora
- Sodium Metabisulphite RPTDocumento51 pagineSodium Metabisulphite RPTGodolias WoldemariamNessuna valutazione finora
- Endothermic and Exothermic Reactions WorksheetDocumento4 pagineEndothermic and Exothermic Reactions Worksheetabdulhakim100% (1)
- Tugas 1 PPADocumento29 pagineTugas 1 PPAlulalalaNessuna valutazione finora
- Stainless EnstainlessDocumento27 pagineStainless EnstainlessVinaya Almane DattathreyaNessuna valutazione finora
- YLAA InstallationDocumento62 pagineYLAA InstallationJoe YoungNessuna valutazione finora
- Applsci 08 01960 PDFDocumento17 pagineApplsci 08 01960 PDFphillynovitaNessuna valutazione finora
- Experimental Detemination of Crystal StructureDocumento40 pagineExperimental Detemination of Crystal StructureAASHIR AHMAD JASKANINessuna valutazione finora
- High Risk Medication PolicyDocumento44 pagineHigh Risk Medication PolicyDewi Ratna SariNessuna valutazione finora
- ASTM Method D5134-92Documento1 paginaASTM Method D5134-92Sylab InstrumentsNessuna valutazione finora
- Green Building Plumbing: Mohammed Athar Mansury Farjana Priyanka Sengar Mohammed Waseem RezaDocumento20 pagineGreen Building Plumbing: Mohammed Athar Mansury Farjana Priyanka Sengar Mohammed Waseem RezaAthar MansuryNessuna valutazione finora
- Major Intermediates in Organophosphate Synthesis (PCL, Pocl, PSCL, and Their Diethyl Esters) Are Anticholinesterase Agents Directly or On ActivationDocumento7 pagineMajor Intermediates in Organophosphate Synthesis (PCL, Pocl, PSCL, and Their Diethyl Esters) Are Anticholinesterase Agents Directly or On ActivationYancy JuanNessuna valutazione finora
- Semester/Concrete Technology (9021) /experiment-02 PDFDocumento14 pagineSemester/Concrete Technology (9021) /experiment-02 PDFjestinvthomasNessuna valutazione finora
- College of Nursing: Cebu Normal UniversityDocumento5 pagineCollege of Nursing: Cebu Normal UniversityChelsea WuNessuna valutazione finora
- Lin Jingwei - A Nomadic Furniture For College StudentsDocumento129 pagineLin Jingwei - A Nomadic Furniture For College StudentsAarish Netarwala100% (2)
- Material Safety Data Sheet Visco ActDocumento4 pagineMaterial Safety Data Sheet Visco Actfs1640Nessuna valutazione finora
- GUIDE-MQA-017-006 (Good Manufacturing Practice For Assemblers of Medicinal Products)Documento15 pagineGUIDE-MQA-017-006 (Good Manufacturing Practice For Assemblers of Medicinal Products)William ChandraNessuna valutazione finora
- CFM SPM 70-48-00Documento8 pagineCFM SPM 70-48-00ZakiHaunaNessuna valutazione finora
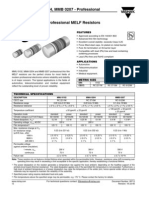
- MMU 0102, MMA 0204, MMB 0207 - Professional: Vishay BeyschlagDocumento13 pagineMMU 0102, MMA 0204, MMB 0207 - Professional: Vishay BeyschlagJan KowalskiNessuna valutazione finora
- Component in Making Fiber Board As Substitute For HardiflexDocumento9 pagineComponent in Making Fiber Board As Substitute For Hardiflexxiniac_1Nessuna valutazione finora
- Medidor Caudal Kobold Flotador UrkDocumento4 pagineMedidor Caudal Kobold Flotador UrkBase SistemasNessuna valutazione finora
- Ethylenediamine Complexes of ChromiumDocumento5 pagineEthylenediamine Complexes of ChromiumMatt PraterNessuna valutazione finora
- SilicaMix Product Brochure2Documento12 pagineSilicaMix Product Brochure2rajni phNessuna valutazione finora
- Conjugate Acid Base Pairs WorksheetDocumento1 paginaConjugate Acid Base Pairs WorksheetFrank Massiah100% (3)
- Soil1 PDFDocumento80 pagineSoil1 PDFSumit KumarNessuna valutazione finora
- Praktikum Biofarmasetika: Data Penetrasi TransdermalDocumento6 paginePraktikum Biofarmasetika: Data Penetrasi TransdermalCindy Riana Putri FebrianiNessuna valutazione finora