Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Discrepancy of Blood Pressure Between The Brachial Artery and Radial Artery
Caricato da
kalashkamitaTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Discrepancy of Blood Pressure Between The Brachial Artery and Radial Artery
Caricato da
kalashkamitaCopyright:
Formati disponibili
www.wjem.
org
294 World J Emerg Med, Vol 4, No 4, 2013 Li et al
Discrepancy of blood pressure between the brachial
artery and radial artery
Wen-yuan Li
1
, Xiao-hai Wang
2
, Li-chong Lu
3
, Hao Li
4
1
Department of Anesthesiology, Second Afliated Hospital of Nanjing Medical University, Nanjing, China
2
Department of Anesthesiology, Afliated Drum-Tower Hospital of Medical College of Nanjing University, Nanjing, China
3
Department of Cardio-Thoracic Surgery, Affiliated Drum-Tower Hospital of Medical College of Nanjing University,
Nanjing, China
4
Department of Anesthesiology, First People's Hospital of Yancheng, Yancheng, China
Corresponding Author: Xiao-hai Wang, Email: wxh32@jlonline.com
Original Article
INTRODUCTION
Blood pressure (BP) is a vital sign indicating
general health of critically ill patients and guiding their
treatment. It is well known that the accurate method for
monitoring BP is passing a transducer connected to a
catheter directly into the ascending aorta. However, this
technique is invasive and not suitable for all patients.
In general, non-invasive blood pressure monitoring is
commonly used in the clinic. Systemic blood pressure
is usually estimated by conventional measurements of
brachial artery blood pressure with a brachial cuff using
oscillometric devices.
However, when patients have some difficulties in
monitoring BP on the upper arm, such as the wound on
the skin or infection of subcutaneous tissues of the upper
arm, brachial blood pressure (bBP) is not suitable for
measurement. Meanwhile, looking for another way to
monitor BP will be necessary. Under this condition, we
found that in many patients with intact forearms, the radial
blood pressure (rBP) on the wrist is easy to be measured.
Therefore, we investigated the relationship between bBP
and rBP using appropriate cuffs and intended to nd that
whether rBP can substitute bBP clinically.
2013 World Journal of Emergency Medicine
BACKGROUND: In this study, we attempted to nd the relations between blood pressure (BP)
measured on the brachial artery (bBP) and BP assessed on the radial artery (rBP) in the right arm.
METHODS: Three hundred and fifteen patients were enrolled in this study. Those who had
peripheral vascular disease, wounds of arm skin or subcutaneous tissue infection were excluded.
After a 15-minute equilibration and stabilization period after inducation of anesthesia, three bBP and
rBP records were obtained sequentially using an oscillometric device with an adult cuff and infant cuff,
respectively. Order for each BP was randomized.
RESULTS: The bBP was signicantly lower than the rBP (P<0.05). The difference between the
two values varied from 13 to 18 mmHg in systolic BP (SBP), diastolic BP (DBP) and mean blood
pressure (MAP) respectively. And the rBP was positively correlated with the bBP (r=0.872, 0.754,
0.765; P<0.001, <0.001, <0.001; SBP, DBP, MAP, respectively).
CONCLUSION: The bBP value can be evaluated by the noninvasive measurements of rBP
using an appropriate cuff in clinical practice.
KEY WORDS: Blood pressure; Brachial artery; Radial artery; Correlation; Linear regression
World J Emerg Med 2013;4(4):294297
DOI: 10.5847/ wjem.j.19208642.2013.04.010
www.wjem.org
295 World J Emerg Med, Vol 4, No 4, 2013
bSBP (mmHg) 9099 100109 110119 120129 130139 140149 90149
rSBP-bSBP 1713 1710 177 189 1711 2111 1810
n 22 42 74 63 69 45 315
Table 2. Absolute differences of SBP between rBP and bBP in different intervals
t=0.929, P=0.462.
Location SBP DBP MAP
Upper arm 127.919.5 79.612.6 94.614.9
Forearm 145.222.7 92.113.3 108.417.0
P <0.001 <0.001 <0.001
Table 1. BP values of the two measuring locations (mmHg)
Data are given as meanSD; *Paired t test.
bDBP (mmHg) 5059 6069 7079 8089 9099 100109 50109
rDBP-bDBP 1713 158 136 126 105 1413 137
n 16 61 99 98 34 7 315
Table 3. Absolute differences of DBP between rBP and bBP in different intervals
t=2.176, P=0.057.
bMAP (mmHg) 6069 7079 8089 9099 100109 110119 120129 60129
rMAP-bMAP 147 1511 156 157 157 138 148 157
n 6 38 106 75 66 22 2 315
Table 4. Absolute differences of MAP between rBP and bBP in different intervals
t=0.311, P=0.931.
METHODS
This study was approved by the Institutional Ethics
Committee at Drum-Tower Hospital. A total of 315
patients, 149 males and 166 females, aged 1879 years,
were enrolled in this study. They all provided the written
informed consent.
Participants were excluded if they had upper limb
amputation, cuts or bruising of the skin at measurement
sites. In addition, those with hypertension, arrhythmia,
aortic coarctation, aortic dissection, peripheral vascular
disease, congenital heart disease, and vasculitis were all
excluded.
Under the condition of general anesthesia, the right
upper limbs of all patients (in a supine position) were
exposed. The upper arm and forearm were kept at heart
level. Appropriate-sized cuffs were chosen according to
the circumferences measured at the midpoint of the upper
arm and forearm. Then we placed the two cuff bladders
over the arterial pulsation and wrapped the cuffs snugly
around the patients' upper arm and forearm with the
cuff bladders encircling at least 80 % of circumferences,
because too small a cuff size leads to false high BPs
and too large leads to false low BPs.
[1,2]
After induction
of anesthesia and a 15-minute stabilization period, BP
was recorded sequentially on the upper arm and forearm
using two automated oscillometric BP monitors (Datex-
Ohmeda, Madison, WI, USA). Order for site to be
measured was first decided randomly, measurement
should be repeated twice at intervals of at least 1 minute,
and the 2 readings were averaged. When the two readings
at the same site differed by >4 mmHg, the recording was
removed, and additional readings should be obtained.
[3]
Statistical analysis
Data were presented as mean and standard deviations
(meanSD). Statistical analysis was performed using
SPSS v.13 (SPSS, Inc. Chicago, IL, USA.). bBP and
rBP were compared using paired t-test. The association
between bBP and rBP was evaluated using the intraclass
correlation coefficient. We used one-way analysis of
variance (ANOVA) to compare BPs of each interval. A P
value of <0.05 was considered statistically signicant.
RESULTS
Mean BMI was 23.23.5 kg/m
2
(range 18.530.7
kg/m
2
), mean circumference of arm and forearm was
25.32.8 cm (range 2234 cm) and 16.31.4 cm (range
1320 cm), respectively. An infant cuff (appropriate
circumference 1020 cm) was used to measure rBP. We
used various sizes of adult cuffs to measure bBP (12
cm22 cm, for arm circumference of 22 to 26 cm; 16
cm30 cm, for arm circumference of 27 to 34 cm).
We obtained 1890 valid pressure readings from 315
patients. The mean BP value for each measurement of
location is shown in Table 1. The mean SBP and DBP in
the upper arm were both significantly higher than those
www.wjem.org
296 World J Emerg Med, Vol 4, No 4, 2013 Li et al
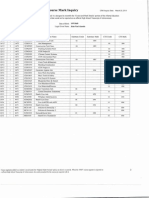
Figure 1. Scatterplots of rSBP, rDBP, and rMAP between rBP and bBP
after general anesthesia. The x-axis indicates the mean of two readings
of the bronchial artery; y-axis, the mean of BP values of the radial
artery. Linear regression analysis showed a significant correlation
between rBP and bBP.
rSBP (mmHg)
0 50 100 150 200 250
200
180
160
140
120
100
80
60
40
20
0
b
S
B
P
(
m
m
H
g
)
y=0.749x+19.13
r=0.872
P<0.001
y=0.673x+21.51
r=0.765
P<0.001
rMAP (mmHg)
0 50 100 150 200
160
140
120
100
80
60
40
20
0
b
M
A
P
(
m
m
H
g
)
y=0.712x+13.96
r=0.754
P<0.001
rDBP (mmHg)
0 20 40 60 80 100 120 140 160
140
120
100
80
60
40
20
0
b
D
B
P
(
m
m
H
g
)
in the forearm respectively (P<0.001).
Scatterplots of BP between the upper arm and
forearm rSBP and bSBP were significantly correlated
(r=0.872, P<0.001), and rDBP and bDBP were also
signicantly correlated (r=0.754, P<0.001) in addition to
rMAP and bMAP (r=0.765, P<0.001) (Figure 1). Linear
regression analysis showed a significant correlation
between rBP and bBP.
The absolute differences between rBP and bBP in
SBP, DBP and MAP are shown in Tables 24. We divided
bBP into several intervals for every 10 mmHg. There
were no signicant differences in absolute difference of
rBP and bBP between the intervals (P=0.462, P=0.057,
P=0.931). bBP could be obtained by subtracting 18, 13,
13 mmHg from rBP in SBP, DBP, and MAP, respectively.
DISCUSSION
Usually, the BP of the brachial artery is measured
using an oscillometric device with an appropriate cuff in a
clinic. But in some patients, BP can't be monitored on their
upper arms because of the wound of skin or infection.
Some studies
[4,5]
considered oscillometric devices for wrist
measurement, but most studies have shown that these
devices are inaccurate.
[68]
BPs at the wrist measured by
oscillometric devices generally overestimate BP compared
with conventional sphygmomanometry on the upper arm,
and the differences could be substantial.
[3]
It was reported
that systemic pressure increased as the measurement
location was moved toward the periphery of the body
away from the heart, whereas diastolic pressure was not
different.
[9]
Nevertheless, our study showed that rDBP was
much higher than bDBP. We thought this disparity might
be due to the patients' state. In Lee's study,
[9]
the patients
were measured before the induction of anesthesia, but
our patients were measured during the maintainence of
anesthesia.
Researchers
[10,11]
reported that there were marked
differences between SBP of the radial artery and that
of the brachial artery, and they were also correlated
significantly with BMI. In our study, we found the
differences between rBP and bBP, and also a strong
linear relationship between them. Therefore, we can
calculate bBP from the linear equation. Obviously, it is
impractical to calculate bBP in the clinic. According to
the absolute differences of BP values in the two sites, we
could estimate dSBP, dDBP and dMAP by subtracting
18, 13, 13 mmHg from rSBP, rDBP, rMAP, respectively.
And there was no significant difference between the
calculated values and the measured values.
To avoid these inuences of "white coat effect", cold,
tension, movement of arms, muscle fasciculation, blood
pressure was measured in the maintenance of general
anesthesia with room temperature at 2426 C during
the experiment.
[12,13]
The position of the measured site
could affect the values, i.e. the BP readings would be
high if the arm was below the right atrium, whereas the
readings would be low when the arm was above the heart
level. These differences might be attributed to the effects
of hydrostatic pressure and could be about 2 mmHg for
every inch above or below the heart level.
[2]
Hence the
midpoint of both upper arm and forearm was placed at
the level of the heart in this study.
[2,14]
From this study, we conclude that when BP value
is difficult to be measured from the upper arm, it can
be estimated by the measurement of the forearm as rBP
using an appropriate cuff in clinical practice.
www.wjem.org
297 World J Emerg Med, Vol 4, No 4, 2013
Funding: None.
Ethical approval: This study was approved by the Institutional
Ethics Committee at Drum-Tower Hospital, Nanjing, China.
Conicts of interest: The authors state that there is no conict of
interest invoving the study.
Contributors: All the authors contributed to the concept of the
study, performance of the study, data collection, and writing of the
manuscript.
REFERENCES
1 Amoore JN. Oscillometric sphygmomanometers: a critical
appraisal of current technology. Blood Press Monit 2012; 17:
8088.
2 Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill
MN, et al. Recommendations for blood pressure measurement
in humans and experimental animals part 1: blood pressure
measurement in humans. A statement for professionals from
the subcommittee of professional and public education of the
American Heart Association Council on high blood pressure
research. Circulation 2005; 111: 697716.
3 O'Brien E, Pickering T, Asmar R, Myers M, Parati G, Staessen
J, et al. Working group on blood pressure moiroring of the
European society of hypertension international protocol for
validation of blood pressure measuring devices in adults. Blood
Press Monit 2002; 7: 317.
4 Zeng WF, Huang QF, Sheng CS, Li Y, Wang JG. Validation of
the Kingyield BP210 wrist blood pressure monitor for home
blood pressure monitoring according to the European Society of
Hypertension International Protocol. Blood Press Monit 2012;
17: 4246.
5 Lu Y, Li CS, Wang S. Effect of hypertransfusion on the
gastrointestinal tract after cardiac arrest in a porcine model.
World J Emerg Med 2012; 3: 4954.
6 O' Brien E. Ambulatory blood pressure measurement is
indispensable to good clinical practice. J Hypertens Suppl 2003;
21: S1118.
7 Akpolat T, Aydogdu T, Erdem E, Karatas A. Inaccuracy of home
sphygmomanometers: a perspective from clinical practice. Blood
Press Monit 2011; 16: 168171.
8 Latman NS, Latman A. Evaluation of instruments for
noninvasive blood pressure monitoring of the wrist. Biomed
Instrum Technol 1997; 31: 6368.
9 Lee JH, Kim JM, Ahn KR, Kim CS, Kang KS, Chung JH,
et al. Study for the discrepancy of arterial blood pressure in
accordance with method, age, body part of measurement during
general anesthesia using sevourane. Korean J Anesthesiol 2011;
60: 323328. Epub 2011 May 31.
10 van der Hoeven NV, van den Born BJ, van Montfrans GA.
Reliability of palpation of the radial artery compared with
auscultation of the brachial artery in measuring SBP. J Hypertens
2011; 29: 5155.
11 Tomlinson LA, Wikinson IB. Does it matter where we measure
blood pressure? Br J Clin Pharmacol 2012; 74: 241245.
12 Dourmap C, Girerd X, Marquand A, Fourcade J, Hottelard C,
Begasse F, et al. Systolic blood pressure is depending on the
arm position when home blood pressure is measured with a
wrist or an arm validated monitor. Blood Press Monit 2010; 14:
181183.
13 O'Brien E, Waeber B, Parati G, Staessen G, Myers MG. On
behalf of the European Society of Hypertension Working Group
on Blood Pressure Monitoring. Blood pressure measuring
devices: validated instruments. BMJ 2001; 322: 531536.
14 McAlister FA, Straus SE. Evidence based treatment of
hypertension. Measurement of blood pressure: an evidence based
review. BMJ 2001; 322: 908911.
Received April 7, 2013
Accepted after revision July 20, 2013
Potrebbero piacerti anche
- 13 Calibration WassertheurerDocumento7 pagine13 Calibration WassertheurerYasmine AbbaouiNessuna valutazione finora
- The Usefulness of A Laser Doppler in The Measurement of Toe Blood PressuresDocumento8 pagineThe Usefulness of A Laser Doppler in The Measurement of Toe Blood PressuressalemNessuna valutazione finora
- Ankle-Brachial Index For Assessment of Peripheral Arterial DiseaseDocumento3 pagineAnkle-Brachial Index For Assessment of Peripheral Arterial DiseaseKukuh Rizwido PrasetyoNessuna valutazione finora
- CufflessDocumento4 pagineCufflessShruti ShreeNessuna valutazione finora
- Directions For Use of An Aneroid Sphygmomanometer PDFDocumento6 pagineDirections For Use of An Aneroid Sphygmomanometer PDFNana AkwaboahNessuna valutazione finora
- Januario2018 Arm Muscle in BP MeasurementDocumento10 pagineJanuario2018 Arm Muscle in BP MeasurementMumtaz MaulanaNessuna valutazione finora
- The Value of The Peak Systolic Velocity RatioDocumento5 pagineThe Value of The Peak Systolic Velocity RatioRikyo LunaNessuna valutazione finora
- Accuracy and Trending of Non Invasive Oscillometric - 2020 - Anaesthesia CriticaDocumento7 pagineAccuracy and Trending of Non Invasive Oscillometric - 2020 - Anaesthesia CriticaRicardoNessuna valutazione finora
- Blood Pressure: I. Theoretical BackgroundDocumento9 pagineBlood Pressure: I. Theoretical BackgroundkereklovagNessuna valutazione finora
- Ankle-Brachial Index For Assessment of Peripheral Arterial DiseaseDocumento5 pagineAnkle-Brachial Index For Assessment of Peripheral Arterial DiseaseindrawepeNessuna valutazione finora
- Arterial Blood Pressure Feature Estimation Using PlethysomographDocumento12 pagineArterial Blood Pressure Feature Estimation Using PlethysomographLevente BalázsNessuna valutazione finora
- Starling Resistor in Sitting Position in APSF NewsletterDocumento2 pagineStarling Resistor in Sitting Position in APSF NewsletterJennifer PraneviciusNessuna valutazione finora
- Both Body and Arm Position Significantly Influence Blood Pressure MeasurementDocumento4 pagineBoth Body and Arm Position Significantly Influence Blood Pressure MeasurementRey DudutzNessuna valutazione finora
- Oscillometric Blood Pressure A Review For CliniciansDocumento9 pagineOscillometric Blood Pressure A Review For CliniciansicastrocemNessuna valutazione finora
- Diagnosis2 (1) 1 PDFDocumento9 pagineDiagnosis2 (1) 1 PDFRobin WilliamsNessuna valutazione finora
- Jvs 17 243Documento10 pagineJvs 17 243Dr.Lázár AttilaNessuna valutazione finora
- Non-Invasive Blood Pressure Monitoring Underestimates Hypertensive Response To Exercise in Suspected Heart Failure With Preserved Ejection FractionDocumento3 pagineNon-Invasive Blood Pressure Monitoring Underestimates Hypertensive Response To Exercise in Suspected Heart Failure With Preserved Ejection FractionEffendi UChinNessuna valutazione finora
- Effect Blood Pressure Alteration Pulse Wave Velocity: THE OF ON THEDocumento5 pagineEffect Blood Pressure Alteration Pulse Wave Velocity: THE OF ON THECoral PlantNessuna valutazione finora
- Noninvasive Cuffless Estimation of Blood Pressure Using Photoplethysmography Without Electrocardiograph MeasurementDocumento4 pagineNoninvasive Cuffless Estimation of Blood Pressure Using Photoplethysmography Without Electrocardiograph MeasurementTensing RodriguesNessuna valutazione finora
- Bi Vins 1985Documento3 pagineBi Vins 1985Jorge MontenegroNessuna valutazione finora
- 2007 - CAVI - Carotid Atherosclerosis - Pts With Essential Hypertension - HypertResDocumento6 pagine2007 - CAVI - Carotid Atherosclerosis - Pts With Essential Hypertension - HypertResMichail PapafaklisNessuna valutazione finora
- Diastolic Blood PressureDocumento7 pagineDiastolic Blood PressureElena MadalinaNessuna valutazione finora
- Measurement of BPDocumento6 pagineMeasurement of BPNiko DagunoNessuna valutazione finora
- Math ProjectDocumento16 pagineMath ProjectMuhammad Hasaan ChaudhryNessuna valutazione finora
- 36814803Documento5 pagine36814803Fernando CardiologíaNessuna valutazione finora
- Angina Pectoris in Patients With Aortic Stenosis and Normal Coronary Arteries - CirculationDocumento24 pagineAngina Pectoris in Patients With Aortic Stenosis and Normal Coronary Arteries - CirculationOscar F RojasNessuna valutazione finora
- DIAZ2017 Relation Btween CRF and BP in Young Adult Mediation AnalysisDocumento5 pagineDIAZ2017 Relation Btween CRF and BP in Young Adult Mediation AnalysisMumtaz MaulanaNessuna valutazione finora
- 16-sbp Amp Pheno SharmanDocumento26 pagine16-sbp Amp Pheno SharmanYasmine AbbaouiNessuna valutazione finora
- Correlation Between Home and Ambulatory Blood Pressure Measurement Diagnosis and MonitoringDocumento1 paginaCorrelation Between Home and Ambulatory Blood Pressure Measurement Diagnosis and MonitoringAchref HamdaniNessuna valutazione finora
- JurnalDocumento5 pagineJurnalKardio JuliNessuna valutazione finora
- Tension Arterial..Trabajo en InglesDocumento4 pagineTension Arterial..Trabajo en InglesMari Alvarado BravoNessuna valutazione finora
- Application of Dynamic Thermogram For Diagnosis of HypertensionDocumento9 pagineApplication of Dynamic Thermogram For Diagnosis of HypertensionJayanthi ThiruvengadamNessuna valutazione finora
- Research Article: ECG Markers of Hemodynamic Improvement in Patients With Pulmonary HypertensionDocumento11 pagineResearch Article: ECG Markers of Hemodynamic Improvement in Patients With Pulmonary HypertensionFaradilla NovaNessuna valutazione finora
- A Simple Method For Noninvasive Estimation of Pulmonary Vascular ResistanceDocumento7 pagineA Simple Method For Noninvasive Estimation of Pulmonary Vascular ResistanceJorge KlyverNessuna valutazione finora
- 10-Mog Vs SPH in InvasiveDocumento8 pagine10-Mog Vs SPH in InvasiveYasmine AbbaouiNessuna valutazione finora
- A Valuable Echocardiographic Indicator For The Optimal Tightness of Bilateral Pulmonary Artery BandingDocumento8 pagineA Valuable Echocardiographic Indicator For The Optimal Tightness of Bilateral Pulmonary Artery BandingRafailiaNessuna valutazione finora
- Tonometria PDFDocumento9 pagineTonometria PDFAdán LópezNessuna valutazione finora
- TBPI Information PDFDocumento8 pagineTBPI Information PDFxtraqrkyNessuna valutazione finora
- 1 s2.0 S1746809418302209 MainDocumento11 pagine1 s2.0 S1746809418302209 MainRajesh SudiNessuna valutazione finora
- Appendix A: Doppler Ultrasound and Ankle-Brachial Pressure IndexDocumento26 pagineAppendix A: Doppler Ultrasound and Ankle-Brachial Pressure IndexabigailNessuna valutazione finora
- A Tale of Three Cuffs The Hemodynamics of Blood Flow RestrictionDocumento7 pagineA Tale of Three Cuffs The Hemodynamics of Blood Flow RestrictionAugusto Felipe Benavides MejiasNessuna valutazione finora
- PlethysmographyDocumento9 paginePlethysmographyTensing RodriguesNessuna valutazione finora
- Characterization of Right Ventricular Deformation in Pulmonary Arterial Hypertension Using Three-Dimensional Principal Strain AnalysisDocumento9 pagineCharacterization of Right Ventricular Deformation in Pulmonary Arterial Hypertension Using Three-Dimensional Principal Strain AnalysisErtanNessuna valutazione finora
- What Is New in Hemodynamic Monitoring and ManagementDocumento9 pagineWhat Is New in Hemodynamic Monitoring and ManagementMarcelo EspinheiraNessuna valutazione finora
- Paper Grupo 2Documento9 paginePaper Grupo 2Fiorella LeyvaNessuna valutazione finora
- J of Clinical Hypertension - 2020 - Candan - The Relationship Between Nocturnal Blood Pressure Drop and Body CompositionDocumento7 pagineJ of Clinical Hypertension - 2020 - Candan - The Relationship Between Nocturnal Blood Pressure Drop and Body Compositionanthony.teggNessuna valutazione finora
- End 2014 0019Documento6 pagineEnd 2014 0019Manolin KinNessuna valutazione finora
- 2023 - Improved Transcranial Doppler Waveform Analysis For Intracranial Hypertension Assessment in Patients With Traumatic Brain InjuryDocumento10 pagine2023 - Improved Transcranial Doppler Waveform Analysis For Intracranial Hypertension Assessment in Patients With Traumatic Brain InjuryOlga Manco GuzmánNessuna valutazione finora
- Bedside Hemodynamic MonitoringDocumento26 pagineBedside Hemodynamic MonitoringBrad F LeeNessuna valutazione finora
- A Quantitative Real-Time Assessment of Buerger (2016) GS PUBMEDDocumento5 pagineA Quantitative Real-Time Assessment of Buerger (2016) GS PUBMEDFitriani FitrianiNessuna valutazione finora
- Epidemiology of Hypertension: 8/10 Pts Continued To Show Improvement. Four of 6Documento1 paginaEpidemiology of Hypertension: 8/10 Pts Continued To Show Improvement. Four of 6Eko PrasNessuna valutazione finora
- Jurnal Internasional Peb Nifas 5Documento10 pagineJurnal Internasional Peb Nifas 5Herdian KurniawanNessuna valutazione finora
- Relationship Between Hypertension and Obesity Anthropometric Indices in Adults of Mashhad CityDocumento4 pagineRelationship Between Hypertension and Obesity Anthropometric Indices in Adults of Mashhad CityLudwig Jonathan Rivero OrtizNessuna valutazione finora
- How To Define Pulmonary Hypertension Due To Left Heart DiseaseDocumento3 pagineHow To Define Pulmonary Hypertension Due To Left Heart DiseaseLê HoangNessuna valutazione finora
- 01-Dolan 2006 AASI Rationale and MethodologyDocumento3 pagine01-Dolan 2006 AASI Rationale and MethodologyRafael Yokoyama FecchioNessuna valutazione finora
- Robert C. Bourge, M.D., PH.D.: Director Division of Cardiovascular Disease University of AlabamaDocumento48 pagineRobert C. Bourge, M.D., PH.D.: Director Division of Cardiovascular Disease University of AlabamaUtomo FemtomNessuna valutazione finora
- BloodDocumento4 pagineBloodLajir LuriahkNessuna valutazione finora
- Retrospective Study PAHDocumento4 pagineRetrospective Study PAHAfifah Nur KartikasariNessuna valutazione finora
- Acid-Base Disorders: Clinical Evaluation and ManagementDa EverandAcid-Base Disorders: Clinical Evaluation and ManagementNessuna valutazione finora
- Football, The Challenge: Video CDocumento1 paginaFootball, The Challenge: Video CkalashkamitaNessuna valutazione finora
- Paul Yellin Aspen RecipesDocumento4 paginePaul Yellin Aspen RecipeskalashkamitaNessuna valutazione finora
- GingerDocumento14 pagineGingerkalashkamitaNessuna valutazione finora
- Axillary: Variation in The Origins of The Branches of The ArteryDocumento9 pagineAxillary: Variation in The Origins of The Branches of The ArterykalashkamitaNessuna valutazione finora
- Work: Video ADocumento2 pagineWork: Video AkalashkamitaNessuna valutazione finora
- These Notes Accompany The Podcast Lesson That You May Access by Going ToDocumento2 pagineThese Notes Accompany The Podcast Lesson That You May Access by Going TokalashkamitaNessuna valutazione finora
- ch9 NotesDocumento31 paginech9 NotesChris Baden HadawayNessuna valutazione finora
- These Notes Accompany The Podcast Lesson That You Can Access atDocumento4 pagineThese Notes Accompany The Podcast Lesson That You Can Access atkalashkamitaNessuna valutazione finora
- These Notes Accompany The Podcast Lesson That You May Access by ClickingDocumento2 pagineThese Notes Accompany The Podcast Lesson That You May Access by ClickingkalashkamitaNessuna valutazione finora
- These Notes Accompany The Podcast Lesson That You Can Access atDocumento3 pagineThese Notes Accompany The Podcast Lesson That You Can Access atkalashkamitaNessuna valutazione finora
- These Notes Accompany The Podcast Lesson That You Can Access atDocumento3 pagineThese Notes Accompany The Podcast Lesson That You Can Access atkalashkamitaNessuna valutazione finora
- These Notes Accompany The Podcast Lesson That You Can Access atDocumento3 pagineThese Notes Accompany The Podcast Lesson That You Can Access atkalashkamitaNessuna valutazione finora
- Chris Gough. English Vocabulary OrganiserDocumento226 pagineChris Gough. English Vocabulary Organisernatalia8186100% (1)
- Hare and Hyena: Mutugi KamundiDocumento18 pagineHare and Hyena: Mutugi KamundiAndresileNessuna valutazione finora
- CH-5 Further Percentages AnswersDocumento5 pagineCH-5 Further Percentages AnswersMaram MohanNessuna valutazione finora
- Smart Door Lock System Using Face RecognitionDocumento5 pagineSmart Door Lock System Using Face RecognitionIJRASETPublicationsNessuna valutazione finora
- Csir Life Sciences Fresh Instant NotesDocumento4 pagineCsir Life Sciences Fresh Instant NotesAlps Ana33% (3)
- Test Physics Chapter# 12,13,14 (2 Year) NameDocumento1 paginaTest Physics Chapter# 12,13,14 (2 Year) NameStay FocusedNessuna valutazione finora
- SCERT Kerala State Syllabus 9th Standard English Textbooks Part 1-1Documento104 pagineSCERT Kerala State Syllabus 9th Standard English Textbooks Part 1-1Athulya ThondangattilNessuna valutazione finora
- Magic Bullet Theory - PPTDocumento5 pagineMagic Bullet Theory - PPTThe Bengal ChariotNessuna valutazione finora
- CHAPTER IV The PSYCHOLOGY of YOGA Yoga, One Among The Six Orthodox Schools of Indian ... (PDFDrive)Documento64 pagineCHAPTER IV The PSYCHOLOGY of YOGA Yoga, One Among The Six Orthodox Schools of Indian ... (PDFDrive)kriti madhokNessuna valutazione finora
- Derma Notes 22pages. DR - Vishwa Medical CoachingDocumento23 pagineDerma Notes 22pages. DR - Vishwa Medical CoachingΝίκος ΣυρίγοςNessuna valutazione finora
- Img 20201010 0005Documento1 paginaImg 20201010 0005Tarek SalehNessuna valutazione finora
- Subject OrientationDocumento15 pagineSubject OrientationPearl OgayonNessuna valutazione finora
- Studies On Drying Kinetics of Solids in A Rotary DryerDocumento6 pagineStudies On Drying Kinetics of Solids in A Rotary DryerVinh Do ThanhNessuna valutazione finora
- Lodge at The Ancient City Information Kit / Great ZimbabweDocumento37 pagineLodge at The Ancient City Information Kit / Great ZimbabwecitysolutionsNessuna valutazione finora
- SDSSSSDDocumento1 paginaSDSSSSDmirfanjpcgmailcomNessuna valutazione finora
- XII CS Material Chap7 2012 13Documento21 pagineXII CS Material Chap7 2012 13Ashis PradhanNessuna valutazione finora
- Img 20150510 0001Documento2 pagineImg 20150510 0001api-284663984Nessuna valutazione finora
- Sample REVISION QUESTION BANK. ACCA Paper F5 PERFORMANCE MANAGEMENTDocumento43 pagineSample REVISION QUESTION BANK. ACCA Paper F5 PERFORMANCE MANAGEMENTAbayneh Assefa75% (4)
- Worst of Autocall Certificate With Memory EffectDocumento1 paginaWorst of Autocall Certificate With Memory Effectapi-25889552Nessuna valutazione finora
- BiografijaDocumento36 pagineBiografijaStjepan ŠkalicNessuna valutazione finora
- AMICO Bar Grating CatalogDocumento57 pagineAMICO Bar Grating CatalogAdnanNessuna valutazione finora
- 2500 Valve BrochureDocumento12 pagine2500 Valve BrochureJurie_sk3608Nessuna valutazione finora
- Nutridiet-Enteral and Parenteral FeedingDocumento3 pagineNutridiet-Enteral and Parenteral FeedingBSN 1-N CASTRO, RicciNessuna valutazione finora
- SafetyRelay CR30Documento3 pagineSafetyRelay CR30Luis GuardiaNessuna valutazione finora
- Dialectical Relationship Between Translation Theory and PracticeDocumento5 pagineDialectical Relationship Between Translation Theory and PracticeEverything Under the sunNessuna valutazione finora
- Leadership and Management in Different Arts FieldsDocumento10 pagineLeadership and Management in Different Arts Fieldsjay jayNessuna valutazione finora
- Gis Data Creation in Bih: Digital Topographic Maps For Bosnia and HerzegovinaDocumento9 pagineGis Data Creation in Bih: Digital Topographic Maps For Bosnia and HerzegovinaGrantNessuna valutazione finora
- MH5-C Prospekt PDFDocumento16 pagineMH5-C Prospekt PDFvatasaNessuna valutazione finora
- KPI AssignmentDocumento7 pagineKPI AssignmentErfan Ahmed100% (1)
- Manuel SYL233 700 EDocumento2 pagineManuel SYL233 700 ESiddiqui SarfarazNessuna valutazione finora
- Modular Q1 WK3-4Documento3 pagineModular Q1 WK3-4JENIFFER DE LEONNessuna valutazione finora