Documenti di Didattica
Documenti di Professioni
Documenti di Cultura
Nagle Notes On Pharmacology
Caricato da
relyessTitolo originale
Copyright
Formati disponibili
Condividi questo documento
Condividi o incorpora il documento
Hai trovato utile questo documento?
Questo contenuto è inappropriato?
Segnala questo documentoCopyright:
Formati disponibili
Nagle Notes On Pharmacology
Caricato da
relyessCopyright:
Formati disponibili
Pharm Assessment 2
(addl/background info on slides: 82-86, 88-89, 100-102, 106, 119-123, 130-131, 165)
DRUGS ACTING ON AMINE SYNTHESIS, UPTAKE, OR METABOLISM
Metyrosine (Demser) blocks tyrosine hydroxylase
Carbidopa (Lodosyn) blocks DOPA decarboxylase in periphery; used w/ L-DOPA to treat Parkinsons
o DOPA decarboxylase is also in the periphery (does NOT cross BBB), so this decreases metab of L-
DOPA in peripheral tissues (and GI tract), so more can get to the brain.
o Allows decreased dosage of L-DOPA good b/c high dose can cause nausea & vomiting
o Does not block completely; still making sufficient amount of NE
* You canNOT just give pt DA b/c it does not cross the BBB; so give L-DOPA, which enters brain, in to
dopaminergic neurons, and then ! DA.
Disulfiram (Antabuse) blocks DA hydroxylase and acetaldehyde dehydrogenase (in the metabolism
of alcohol) because it chelates the Cu that these enzymes need! Used to treat alcoholism.
o so this drug decreases NE, but
o the MAIN POINT: causes a buildup of acetaldehyde (intermed in metab of alcohol) ! vasodilation !
hypotension ! feel very sick.
Entacapone (COMTan) blocks COMT (liver & kidney); used w/ L-DOPA to treat Parkinsons
o Similarly to Carbidopa, this decreases metab of L-DOPA in the periphery and allows decreased dosage
of L-DOPA, avoiding nausea and vomiting.
Reserpine (Serpasil) inhibits DA & NE into synaptic vesicles; Tx hyperT and psychosis.
o After ~12 hrs, damages vesicles and they cannot be released, so get depletion of NE from
noradrenergic n terminals fx like a sympathectomy (like cutting the nn). ! block symp fx
(and therefore increase parasymp fx).
o Takes ~48 hrs to reform vesicles.
o BUT w/ exogenous NE administration, Reserpine will potentiate fx.
o CONTRAINDICATIONS: depression and peptic ulcers
" In brain, blocks DA, NE, and Serotonin uptake, which can lead to depression.
Cocaine inhibits amine pump in nerve endings; uses: Tx depression, local anesthetic
o ! inhibits reuptake by the amine pump of NE, DA, GABA, Serotonin, and Epi!!
o Tx of depression and as a local anesthetic
o DA buildup ! increased libido, NE buildup ! increased symp fx, Serotonin buildup ! euphoria.
o recall that 70% or more of NE is usually taken back up, so this increases NE in cleft a LOT; can ! MI.
Tyrosine !(tyr hydroxylase)! DOPA !(DOPA decarboxylase)! DA !(DA hydroxylase)! NE
in periphery: L-DOPA !(DOPA decarboxylase)! DA
liver/kidney: L-DOPA !(COMT)! 3-0-MD
TCAs (e.g. Desipramine or Amitriptyline) also block the amine pump; Tx depression
o Mech not fully understood, but increases NE in brain. Takes a few weeks.
o Also increase NE overall and ! increased basal BP. If give NE w/ TCA, will see potentiated response.
!-Methyldopa (Aldomet) false nt w/ NE; Tx hypertension
o
o !-Methyl-NE is the active agent here, on !
2
receptors in RVLM. It is a false neurotransmitter, i.e. it is
taken up in nn, then stored w/, released w/, and acts like NE
* acts like NE, but treats hypertension??
" An injection in the periphery would increase BP by acting on vessel !
2
receptors, but
" It is given so that it acts centrally, on the RVLM (rostral ventrolateral medulla), reducing
impulses from the brain that signal NE release, to decrease BP.
o [compare to Clonidine and Guanabenz below, w/ direct axn on !
2
in RVLM]
Enzymatic Degradation of Catecholamines:
" Enzymes:
o MAO-A (GI tract and liver) metabolizes Epi, NE, serotonin, and Tyramine (see below)
o MAO-B (esp. brain, and platelets) metabolizes DA
o COMT (liver and kidney) metabolizes L-DOPA, Epi, and NE
" blocked by Entacapone (see above)
" Urinary metabolites:
o Epi and NE ! VMA, MHPG, MOPEG
o NE ! normetanephrine; Epi ! metanephrine (Dx pheochromocytoma)
o DA ! HVA and DOPAC (homovanillic acid and dihydroxyphenylacetic acid)
Tranylcypromine (Parnate) and Phenelzine (Nardil) inhibit MAO-A & MAO-B
o Tx: depression and panic disorders
Selegiline (Eldepryl) inhibits MAO-B
o Tx Parkinsons, +/- L-DOPA
_______________________________________________________________________
Pre-Junctional Adrenergic Receptor Actions (*slide 102 pic)
!
2
"
2
On adrenergic n: inhibits release of NE On adrenergic n: increases release of NE
On parasymp n: inhibits Ach release
On serotoninergic n: inhibits serotonin
!-Methyldopa !(Dopa decarboxylase)! !-Methyldopamine!(DA #-hydroxylase)! !-Methyl-NE
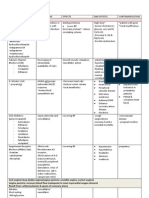
Post-Junctional Adrenergic Receptor Actions, Agonists, & Antagonists
!
1
!
2
#
1
"
2
(NE does not bind!!)
Vessels: constrict Vessels: constrict
* Hypotension in RVLM
Heart: Increase HR
(also contractility and
conduction velocity)
Vessels: dilate
Decrease GI motility &
tone;
* cntrxn of sphincter mm
in GI and bladder
Decrease GI motility &
tone
Decrease GI motility & tone Decrease GI motility & tone;
* relax bladder detrussor
Pancreas:
inhibit Insulin secretion
Pancreas:
increase Insulin secretion
Also: increase
Glucagon secretion
Liver: increase
glycogenolysis
Liver & Muscle:
increase glycogenolysis
and gluconeogenesis
Fat cell:
decrease lipolysis
Adipose tissue:
FA mobilization
Bronchial smooth m: relax
Contract Radial m in eye
(dilation, mydriasis)
Platelets: aggregation Kidney:
increase renin release
Pregnant uterus:
relax (prevent premies)
(Ritodrine)
Specific:
Phenylephrine,
Methoxamine
Metaraminol (mixed action,
so also get fx of NE!)
Specific:
Clonidine (Catapress)
Specific:
Dobutamine (Dobutrex)
Short-acting: (all Tx asthma)
Metaproterenol (Alupent)
Terbutaline (Brethin)
Albuterol (Proventil)
Bitolterol (Tornalate)
Pirbuterol (Maxidair)
Long-acting:
Salmeterol (Serevent)
Formoterol (Foradil)
Epi (!
1
!
2
#
1
#
2
)
NE (!
1
!
2
#
1
)
Ephedrine (!
1
#
2
)
(mixed action!)
Epi (!
1
!
2
#
1
#
2
)
NE (!
1
!
2
#
1
)
Epi (!
1
!
2
#
1
#
2
)
NE (!
1
!
2
#
1
)
Isoproterenol (#
1
#
2
)
Ephedrine (mixed action!)
Short-acting:
Epi (!
1
!
2
#
1
#
2
)
Isoproterenol (#
1
#
2
)
Prazosin (Minipress)
Terazosin
Doxazosin
Rauwolscine
(not on list; not used clinic.)
Acebutolol, Atenolol (low
)
Metoprolol (Lopressor)
(moderate)
Butoxamine
(not approved, not on list)
Phenoxybenzamine (!
1
!
2
)
Phentolamine (!
1
!
2
)
Carvediolol (!
1
!
2
#
1
#
2
)
Labetalol (!
1
!
2
#
1
#
2
)
Phenoxybenzamine (!
1
!
2
)
Phentolamine (!
1
!
2
)
Carvediolol (!
1
!
2
#
1
#
2
) !
Labetalol (!
1
!
2
#
1
#
2
) !
Pindolol
!
, Nadolol (low)
Timolol (low-moderate)
Propranolol
!
(High)
Penbutolol (High) (all #
1
#
2
)
Pindolol, Nadolol (low)
Timolol (low-moderate)
Propranolol, Penbutolol (High)
(all #
1
#
2
)
#-blockers used to treat hypertension b/c they decrease renin release !! decrease Angio II ! decrease BP.
Detrussor m does not have adrenergic innerv, but does have #
2
receptors.
Low/moderate/high indicates lipid solubility. Low - slow into CNS and slow out; High fast into CNS and fast out.
Pindolol also a partial agonist good for very senstive pts that may get bradycardia w/ B
1
blocked.
!
Pindolol and Propranolol stabilize membranes w/ direct effect on membrane Na conductors prevent arrhythmias.
Note: also have #
3
receptors, which are involved in lipolysis in brown adipose tissue.
DIRECT SYMPATHOMIMETICS
Note: There are ! receptor subtypes (slide 113), but we dont have drugs (yet) that are subtype-specific.
Epinephrine (Propine) acts on !
1
!
2
#
1
#
2
[Note: Propine is a prodrug and is converted to Epi in the body.]
o Relative effect on !
receptors: Epi > NE
o Small dose Epi ! vasodilation via #
2
(decreased peripheral resistance)
o Normal doses ! vasoconstriction via !
1
!
2
o Fx on HR unpredictable may see increase, decrease, or no change depending on whether the Epi or
reflex predominates.
o Increase systolic, decrease diastolic BP ! no change in MAP.
o Used in dentistry w/ local anesthetic given locally in high dose to ! vasocnstrxn (! effects
predominate) ! reduce systemic absorption of anesthetic and reduce bleeding.
o Tx A-V heart block.
o Tx open-angle Glaucoma, along w/ #-blocker Timolol (see Timolol below) Epi reduces prdxn of aq humor
by ciliary processes and increases outflow.
Norepinephrine (Levarterenol) acts on !
1
!
2
#
1
(NOT #
2
)
o ! REFLEX decrease in HR due to marked increase in BP; most prominent w/ !
1
agonists
" i.e. symp outflow is decreased; parasymp is increased, and Ach overpowers NE fx on heart
" if give Atropine, fx of Ach blocked, so NE increases BP and HR
" also have vasodilation of coronary vessels due to local mediators (lactic acid, PGI
2
, NO, etc.)
o Increase systolic and diastolic BP.
" #-blocker does not change its BP fx b/c does not act on #
2
and no #
1
in vessels.
o Increase peripheral resistance.
o Would NOT give to decrease HR in tachycardia b/c combo of no cholinergic innerv to ventricles (no
parasymp), plus NE acting directly on ventricles ! induce 2
o
pacemakers in ventricles ! ventricular
tachycardia and arrhythmias.
Phenylephrine (Neo-synephrine) - !
1
selective agonist ! vasocnstrxn and increased BP.
o Will ! REFLEX decrease in HR with increased BP.
" But here, if you give Atropine and then Phenylephrine, will see increased BP but no change in HR!
b/c no direct fx on HR (no #
1
).
o Tx paroxysmal atrial tachycardia (if pt NOT hypertensive) b/c increases parasymp activity
" Will also cause increased BP though.
o DIRECT, i.e. not taken up by nn to exert its fx...
* therefore, fx will NOT be altered by cocaine/TCAs or reserpine.
o Decongestant (any !
1
agonist) b/c nasal mucosa is highly vascularized.
o Blocked by Prazosin
Methoxamine (Vasoxyl) - !
1
o Like NE and Phenylephrine, will see increased BP and REFLEX decreased HR.
o Decongestant (any !
1
agonist) b/c nasal mucosa is highly vascularized.
o Blocked by Prazosin
Clonidine (Catapress) and Guanabenz (Wytensin) !
2
o Clonidine crosses the BBB, so can give injection. It will cause an initial increase in BP by acting on
vessels, then once it crosses the BBB, will act on RVLM and decrease BP by reducing flow of impulses
from brain that signal release of NE. (Symps account for 40-60 mm Hg of total BP.)
o Used as preanesthetic drug (sedative, antianxiety, pain).
o Used for Heroin and Nicotine w/drawal b/c pts in w/drawal have increased symp activity, want to
decrease it.
o Relative effect on !
2
: Clonidine = Guanabenz > NE
o Both blocked by Rauwolscine (not on drug list & not used clinically)
Isoproterenol (Isuprel) acts on #
1
and #
2
o Decrease peripheral resistance; increase systolic and decrease diastolic ! decrease MAP
o Large increase in HR b/c direct and reflex mechanisms
o Tx A-V heart block.
o Increased HR fx blocked by Propanolol (#
1
)
* Relative effect on # receptors: Isoproterenol >> Epi > NE
Dobutamine (Dobutrex) acts on #
1
! increases HR; @ high doses, #
2
and !
1
also
o Tx cardiac decompensation after surgery or in CHF
o Blocked by Metoprolol
Albuterol (Proventil), Bitolterol (Tornadate), Metaproterenol (Alupent), Terbutaline
(Brethin), Pirbuterol (Maxidair) - act on #
2
; Tx asthma
o Blocked by Butoxamine (NOT on list)
Salmeterol (Serevent), Formoterol (Foradil)- acts on #
2
; long-acting
Ritodrine (Yutopar) - #
2
; prevents premature labor
Side effects and Toxicity:
Throbbing headache
Precordial pain
Cerebral hemmorhage
(due to excessive increase in BP)
Palpitations
Cardiac arrhythmias
Restlessness
Panic, Anxiety, Tremor,
Respiratory difficulties
(due to CNS stimulation)
Pulmonary edema
(after prolonged drug use)
Contraindications:
Hyperthyroidism
" b/c have increased #
1
receptor density in heart.
Heart disease
Severe hypertension
" could use e.g. Clonidine or
!-Methyldopa, but nothing
that increases BP.
Inhalation anesthesia -
(arrhythmias) b/c sensitizes
heart to the effects of NE and
Epi.
INDIRECT SYMPATHOMIMETICS
Indirect i.e. they do not act on adrenergic receptors, but act presynaptically to release nts that can then act
on their respective receptors postsynaptically.
Amphetamine taken up by amine pump at nerve terminal; then pushes the nts out
o Primary: increases NE ! alertness
o Then: increases DA ! euphoria
o Then: increases Serotonin ! hallucination
o Passes BBB! (*except for amphetamine and ephedrine, sympathomimetics have little CNS fx)
o Tx psychogenic disorders
o Tx narcolepsy (NE fx) b/c NE is low in these pts brains; can also counteract barbiturates.
Tyramine taken up by amine pump at nerve terminal; releases NE
o Found in many foods (cheese, wine, fish), * normally metabolized by MAO-A * (GI tract and liver)
o If blocking MAO-A w/ drug (e.g. Tranylcypromine or Phenelzine) tyramine absorbed in intestine, into n
via amine pump, releases NE ! hypertensive crisis.
* If give Amphetamine/Tyramine after cocaine/TCA, will NOT be taken up b/c amine pump blocked.
* Amphetamine and Tyramine do NOT promote the influx of Ca
2+
in the nerve terminal and do NOT need an AP
to push out or release the other nts.
* If give Amphetamine/Tyramine after Reserpine, no effects of NE seen b/c Reserpine blocks the storage of
NE (and DA) in the vesicles.
MIXED-ACTION SYMPATHOMIMETICS
Ephedrine (Pretz-D) mixed action: direct on !
1
and #
2
, indirect by increasing release of NE.
o so indirectly has axn on !
1
!
2
#
1
via NE release
* Given w/ Reserpine, will see decreased fx b/c Reserpine depletes NE in n terminals.
o Passes BBB! (*except for amphetamine and ephedrine, sympathomimetics have little CNS fx)
o Tx narcolepsy (NE fx) b/c NE is low in these pts brains
Metaraminol (Aramine) mixed action: direct on !
1
, indirect by increasing NE (!
1
!
2
#
1
)
* Is a false nt i.e. it is taken up, stored in vesicles, and released w/ NE.
o Tx when want to temporarily increase BP, e.g for drug-induced hypoT, excision of pheochromocytoma,
orthostatic hypotension. (NOTE: can use any !
1
agonist to increase BP!)
Comparison of Directly & Indirectly Acting Sympathomimetics:
Direct Axn: Post-Synaptic Indirect Axn: Pre-Synaptic
BP response after sympathectomy,
Cocaine, or Reserpine
##
(NE >> E)
$ or none
COMT Effect Inactivated (shorter duration) Resistant (Amphetamine or Ephedrine)
MAO Effect Inactivated (shorter duration) Resistant (Amphetamine or Ephedrine)
Effect Duration Shorter Longer
Oral Activity No Yes (Amphetamine or Ephedrine)
Receptor Blockade $ Response $ Response
!-ADRENERGIC ANTAGONISTS
See Chart above!
Pharmacological Effects:
o Heart & Vasculature (pic slide 149):
" Do NOT block the chronotropic fx of catecholamines/symp stimulation (#
1
).
" $BP:
" Orthostatic hypotension (normally have reflex # symp activity upon standing, but if !
blocked, vessels do not constrict) esp do NOT give to pts on vasodilators!! (e.g. NO)
o Note: Clonidine and Aldomet cause $ symp output, do NOT cause this b/c they
dont block the receptors.
" Venous pooling ! $ preload ! $ CO
" ! REFLEX tachycardia
" # Na
+
and H
2
O retention b/c increased symp to #
1
receptors in JG renal cells.
* This is called pseduo-tolerance b/c eventually you will have plasma expansion,
and the BP will not be lowered anymore.
* ! blockers are given with # blockers to block the reflex tachycardia and pseudo-tolerance!!
o Other:
" Eye: radial muscle miosis w/o loss of accomodation. (accomodation is ciliary m, parasymp)
* Urinary: !
1
blockage relaxes sphincter; can help in benign prostatic hypertrophy (BPH).
[The zosin drugs.]
Therapeutic Uses:
o Hypertension only if given w/ # blockers
o Pheochromocytoma use w/ metyrosine (blocks syn of catecholamines); may also add # blockers.
" Used pre-op to make sure pt has endogenously high levels of catecholamines
" Used post-op to prevent severe symp fx of circulating catecholamines still present.
o Peripheral Vascular Disease: Raynauds and Buergers syndrome intense vasocnstrxn in fingers
and toes, commonly seen in teens exposed to cold.
o Shock: NOT a primary Tx!
" First choice is to replace fluid and give DA (see below).
" Given as a last resort if vasocnstrxn persists after other Tx.
o BPH, hyperreflexia, incomplete urinary voiding: !
2
blockers used to relax sphincters.
o Pulmonary Congestion (CHF): b/c decreases BP (indirect effect, and only a temporary soln).
Side effects:
Postural hypotension
Tachycardia (REFLEX)
Arrhythmia
Abdominal Pain
Nausea and vomiting
Diarrhea
Contraindications:
Hypotension e.g. on NO, nitroglycerin,
Cialis, Viagra will pass out if standing up!
Heart disease (b/c will ! tachycardia)
Peptic ulcer
$-ADRENERGIC ANTAGONISTS -olol
See chart above!
Pindolol #
1
#
2
and
special:
o Membrane stabilizer DIRECT effect on Na
+
channels in heart, has a depressant effect and
prevents arrhythmias.
o Also has partial agonist activity advantage b/c some pts very sensitive to blocking #
1
Propranolol (Inderal) #
1
#
2
and
special
o Membrane stabilizer DIRECT effect on Na
+
channels in heart, has a depressant effect and
prevents arrhythmias.
Timolol (Blocadren) blocks #; used w/ Epi to treat open-angle Glaucoma
o Open-angle glaucoma is the most common form of glaucoma; gradual, painless, but inevitably leads to
vision loss due to optic n damage if not treated.
o Timolol primarily reduces the prdxn of aq humor (Epi does this but also increases outflow).
o Also: Tx migraines
* Carvediolol, Labetalol - ! AND #!
o Tx hypertension recall ! blockers used w/ # blockers to treat hyperT, and this already has both!
Pharmacological Effects:
o Heart & Vasculature (slide 155):
" Decrease HR, contractility, CO, cndxn velocity, and O
2
consumption: all primarily due to
blockade of catecholamine fx on #
1
. [neg chrono-, dromo-, and iono-tropic fx]
" May ! direct myocardial depressant w/ membrane stabilizing (Pindolol, Propranolol)
" Anti-arrhythmic
" Decreased periph vasc resistance ! decrease BP, esp in pts w/ high renin and CO.
o Other:
" Resp System: may ! bronchocnstrxn and block #
2
relaxation fx.
" Metab:
" Inhibit glycogenolysis in heart and skel m (#
2
)
" Increase insulin secretion (#
2
)
" Block FFA release (#
1
)
" CNS: decrease in BP partly due to CNS fx.
" Kidney: decreases renin release from JG (#
1
).
Therapeutic Uses:
o Cardiac arrhythmias catecholamine OD; during anesthesia; digitalis toxicity (narrow Tx winodow).
o Angina pectoris combine w/ NO to decrease workload of heart.
o Hypertrophic obstructive cardiomyopathies large heart with increased O
2
demand
o MI to decrease risk of 2
nd
MI
o Marfans use to decrease incidence of acute dissecting aortic aneurysm
o in CHF (*use in low doses and NOT in severe cases*) b/c ! upreg of #
1
receptors and then remove
the antagonist to get a rebound effect.
o Fallots tetralogy (pulmonary stenosis, IV septal defect, ventric hypertrophy, aortal juxtaposition)
to decrease workload on heart.
o Tx tachycardia: reflex, stress- or fear-induced.
o Hypertension
o Hyperthyroidism pts have increased #
1
receptors in heart via hormonal stimulation of synthesis
o Pheochromocytoma
o Glaucoma:
" Timolol decreases formation of aq humor by ciliary processes.
o Migraine headache Propanolol, Timolol
" Only effective as a prophylactive before headache starts; mech unknown
Side fx and Toxicity:
Decrease cardiac cndxn (#
1
),
Bradycardia, Hypotension
Exacerbation of periph vasc
disease
Bronchospasm (#
2
)
Hypoglycemia (#
2
)
Nightmares common
Depression, Fatigue
Contraindications:
Severe CHF
A-V heart block
Diabetics on Insulin does not allow
tachycardic sensing of max insulin
injxns; can lead to seizure and
convulsions
Periph Vasc Disease
Renal Insufficiency do NOT give to
pt with renal a. stenosis; prevents
monitoring of BP via JG cells and
inhibits release of renin and
restoration of BP ! renal failure.
Bronchial asthma avoid # blockers in
general, but if necessary use #
1
specific blockers. (e.g. Metoprolol)
DOPAMINERGICS
D
1
Post. (~D
5
) D
2
Post. (~D
3
, D
4
) D
2
Pre.
Renal and Mesenteric vessels:
relaxation
Pituitary gland:
inhibit PL release
Adrenergic nn:
inhibit NE release
Kidney:
natriuresis and diuresis
(i.e. # Na
+
and overall urine output)
DA-ergic nn (CNS):
Inhibit DA release
Parathyroid gland:
PTH release
(D
1
): Fenoldopam
(D
2
): Bromocriptine
Pramipexole
(D
1
D
2
): Dopamine
Apomorphine
Pergolide
(D
1
D
2
): Dopamine
Apomorphine
Pergolide
(D
2
): Domperidone
(D
1
D
2
): Haloperidol (D
1
D
2
): Haloperidol
NON-SELECTIVE AGONISTS (D
1
and D
2
):
o Dopamine (Inotropin)
* Tx for SHOCK: b/c low doses also stimulate #
1
receptors in heart to increase HR and CO;
also good b/c increases coronary and renal perfusion a major advantage over Epi!
" High doses acts much like Epi.
o Apomorphine (Apokyn) Tx Parkinsons
" Acts on DA receptors in hypothalamus
o Pergolide (Peremax)
SELECTIVE AGONISTS:
o Fenoldopam (Corlopam) D
1
promotes diuresis and natriuresis in renal failure and shock !
lowers BP
o Bromocriptine (Parlodel) D
2
Tx Parkinsons and impotency
o Pramipexole (Mirapex) D
2
ANTAGONISTS:
o Haloperidol (Haldol) D
1
and D
2
- Tx psychogenic disorders (e.g. schizophrenia)
o Domperidone (Moltilium) D
2
Antiemetic (i.e. alleviates nausea/vomiting)
" Think: need it after Dom Perignon
Which of the following statements regarding efficacy (intrinsic
activity) of a drug is CORRECT?
A. The efficacy of a drug is the dose that is required to produce
50 percent of the maximal response
B. The efficacy of a drug is the minimal dose of a drug that
produces a quantal response
C. The efficacy of a drug is directly related to its potency and
affinity
D. The efficacy of a drug can be accurately estimated from the
slope of a dose-response curve
E. The efficacy of a drug is the intrinsic activity by which an
agonist produces the maximal effect
Quantal dose-response curves describes:
A. the relationship between the concentration of the drug and the
progressive increment in the magnitude of the response
B. the relationship between the concentration of the drug and the
number of receptors occupied by the drug
D. the relationship between the concentration of the drug and the
number of receptors activated by the drug
F. the relationship between the concentration of the drug and the
frequency of the individuals responding in a given population
E. the relationship between the concentration of the drug and the
rate at which drug activates the receptor
Which statement describing a drug receptor interaction
studied by radioligand binding is CORRECT?
A. The ED
50
represents the dose of a drug that produces
the maximal biological response
B. The lower the IC
50
of the drug, the lower the drugs
affinity for its receptor will be
C. The IC50 denotes the concentration of a nonradio-
labeled ligand required to displace a radioligand by
50% from its receptor
D. The Bmax determined from radioligand binding studies
denote the lowest number of receptors involved in the
biological response to an agonist
Which of the following drugs inhibits the activity of
dopamine-beta-hydroxylase and acetaldehyde
dehydrogenase?
A) Carbidopa [Lodosyn]
B) Disulfiram [Antabuse]
C) Tyramine
D) alpha-methyl-para-tyrosine [Demser]
E) alpha-methyldopa [Aldomet]
Reserpine:
A) inhibits the activity of dopamine beta-hydroxylase
C) inhibits the transport of norepinephrine and dopamine into
synaptic vesicles in adrenergic nerves
E) depletes norepinephrine from adrenergic nerves by inhibiting
the activity of tyrosine hydroxylase
D) does not deplete epinephrine from the adrenal gland
E) prevents the re-uptake of norephinephrine and dopamine into
varicosities through amine pump in adrenergic nerves
B.P.
Mm, Hg
Drug X
ISO PHE TYR NE E
ISO PHE TYR NE E
Mean
arterial
B.P.
100
0
H.R.
200
50
4
0
Intestinal
contraction
Drug X
Which of the following drugs is useful in the treatment of
paroxysmal tachycardia?
A. Isoproterenol (Isuprel)
B. Epinephrine
C. Propranolol (Inderal)
D. Methoxamine (Vasoxyl)
E. Metaproterenol (Alupent )
A 67-year-old woman is admitted to the ICU with sepsis
secondary to a urinary tract infection. She is tachycardic, BP
is 80/40, and renal output is low. Antibiotic therapy is
instituted, together with iv fluids and a low-dose infusion of
dopamine. Which of the following drugs would directly
antagonize the action of this agent at D1 and D2 receptors?
A) alpha-methyl-para-tyrosine [Metyrosine]
B) entacapone [Comtan]
C) carbidopa [Lodosyn]
D) Pindolol (Visken)
E) haloperidol [Haldol]
Cholinergic Drugs
Organ Muscarinic Agonist
Muscarinic Antagonist
Ganglionic Agonist
N1
Ganglionic Antagonist
Block N1
Eye
* iris Contraction (Miosis) Mydriasis Mydriasis
* ciliary
muscle
Accommodation Cycloplegia cycloplegia
Heart ! HR, ! BP Initial !HR ! " HR Initial " HR! ! HR Moderate " HR, ! CO
Blood
Vessels
Dilation Block of agonist Ax. Constriction
(NE & EPI adrenal
release)
Orthostatic hypotension,
Dilation,
" peripheral blood flow
Veins Dilation ! venous return
Lung
* Muscles Bronchoconstriction Bronchodilation
* Glands " secretion & motility ! secretion
GI Tract " motility ! motility & tone
* Sphincters ! tone=Relaxation
* Secretion
" !
" motility & tone=
nausea,
Vomiting, diarrhea
! motility=constipation
Bladder " urination Relaxation=retention ! contraction=retention
* Detrussor " tone=Contraction
* Sphincters ! tone =Relaxation
Glands " secretion ! secretion
Xerostomia, anhidrosis
Skeletal
Muscle
+ Neuro end plates ---- Stimulation!paralysis Relaxation
CNS --- Sedation, antiparkinsons,
Prevention of motion sickness,
Hallucinations
+ vomiting center
+ ADH release
analgesia
Ach, Carbachol,
Methacholine,
Bethacholine, Cevimeline,
Pilocarpine
Atropine, Scopoline, Glycopyrrolate,
Ipratropium, Oxybutynin,
Trihexphenidyl HCL, Benztropine,
Tropicamide
Acetylcholine,
Nicotine
Hexamethonium,
Mecamylamine
1/8
Pharm Assessment 3
INHIBITORS OF Ach (synthesis, storage, and release)
Hemicholinium - inhibits choline transport into neuron ! inhibits Ach synthesis.
o Active uptake of choline is RLS in Ach synthesis, NOT activity of ChAT. Uptake
mediated by [Na], so normally increases with depolarization.
Vesamicol inhibits storage of Ach in vesicles; NOT used clinically.
Botulinum Toxin inhibits fusion of Ach vesicles at presynaptic membrane.
o Contains proteases that degrade VAMPs and SNAPs, which are necessary
for fusion.
o Clinical uses:
" Facial wrinkles
" Strabismus (eyes not properly aligned)
" Blepharospasm (abnl tic/twitch of mm around eye)
" Meiges syndrome (unilat spasm due to facial n. inflammation)
" Spasmodic torticollis (invol cntrxn of neck mm)
*[slides 174-178: effects on BP with combos of Ach, Nicotine, NE, Atropine,
Hexamethonium, and Phentolamine]
" Small dose Ach IV ! decrease BP, unless blocked by Atropine
" Large dose Ach IV ! decrease BP
! w/ Atropine, then will ! increase BP (relase of Epi and NE)
! w/ Atropine and Hexamethonium ! no effect on BP (block M and N
1
)
! w/ Atropine and Phentolamine ! no effect on BP
! w/ Hexamethonium only ! decrease BP (direct axn on M)
" Nicotine ! increase in BP (release Epi and NE),
! w/ Hexamethonium (N
1
) ! no effect on BP
! w/ Phentolamine ! no effect on BP
" NE ! increase in BP
! w/ Phentolamine ! no effect on BP
2/8
MUSCARINIC AGONISTS
(aka parasympathomimetics)
[Beth Cevim Carries Methylated Pillows.]
Acetylcholine (Miochol-E) binds to M and N receptors. (*slide 172 diagram)
o No Tx uses
o Does NOT cross BBB
o Muscarinic
" Actions: Think parasympathetics: axns similar to those seen w/ postgang
parasymps (for all, see slides 185, 187, 194) ; vessel dilation via NO.
! Accomodation (close-up vision), myosis (pupil cntrxn)
! Atrium: can ! atrial flutter/fibrillation b/c decrease refractory
periods and duration of each AP, increase conduction velocity.
* opposite of axns in AV node
! Glands (sweat, salivary, lacrimal, nasopharyng, bronch) increase
secretion.
" Receptors = GPCRs, M1-M5
! M1: Nerves, G
q
! M2: Heart (and nerves, smooth muscle), G
i
! M3: Endothelium (and glands, smooth muscle), G
q
" Locations:
! Postgang parasymps
! Blood vessel smooth muscle (NOT innervated, but have M
3
receptors: Ach ! release NO ! relaxation).
! Sweat glands (except soles, palms, and axillae, which are NE).
" Blocked by Atropine
o Nicotinic
" Actions: many, see below.
" Receptors = Na ion channels, classified by sensitivity to !-bungarotoxin.
" N1 Locations:
! Autonomic ganglia of symp AND parasymp (see below)
! Adrenal medulla ! release Epi
! Adrenergic nerve terminals ! NE
! Blocked by Hexamethonium
" N2 Location:
! NMJ (skeletal mm.)
! Blocked by Curare (and others, see below)
o Small dose Ach IV ! NO release in endothelium ! decrease BP.
" Will not see other effects.
" If give atropine first, will see no effect!
o Large dose Ach
" Direct effect on M
2
and effect on parasymp ganglia ! decrease HR
" Symp ganglia (N
1
) ! release NE
" Adrenal Medulla (N
1
) ! release Epi
" NMJ (N
2
) ! cntrxn of skel m
* have BOTH vasodilators and constrictors released, but Ach effects
predominate ! decrease BP!!
Note:
Subtypes of
GPCRs not
covered in
class but for
boards
3/8
Carbachol (Carbacol) urinary retention and post-op atonic bowel
o Also has some N action give w/ atropine! increase BP.
o NOT hydrolyzed by cholinesterase.
Methacholine (Mecholyl) Dx asthma
o Also has some N action give w/ atropine! increase BP.
Bethanechol (Urecholine) urinary retention and post-op atonic bowel
o no N action!! ONLY Muscarinic so if give w/ atropine, no effects.
o NOT hydrolyzed by cholinesterase.
Cevimeline (Evoxac) Tx: Sjogrens syndrome, Mikuliczs syndrome, and Sicca
syndrome
" Sjogrens = dry mouth, dry eyes, AND arthritis
" Sicca = dry mouth, dry eyes (xerostomia, xerophthalmia)
" Mikuliczs = bilat enlargement of lacrimal and salivary glands, no arthritis
o no N action!! ONLY Muscarinic so if give w/ atropine, no effects.
Pilocarpine (Salagen) (an alkaloid) Tx closed-angle glaucoma, applied topically
! increase outflow of aqueous humor.
o Common cause is dilation of pupil due to an emotional crisis, w/ symp discharge;
drugs like NE, E, and atropine can also cause if pt is very susceptible to mydriasis.
o Rapid onset accompanied by pain (oppo. of open-angle glaucoma).
o also increases saliva
o no N action!! ONLY Muscarinic so if give w/ atropine, no effects.
RECALL:
- Only M axn: Bethanechol, Cevimeline, Pilocarpine
- M and N axns: Ach, Carbachol, Methacholine
- Not hydrolyzed by cholinesterase: Bethanechol, Carbachol (note these have the same
uses, too)
ALSO:
- All w/ chol in the name (i.e. the choline esters) do NOT give IV b/c ! hypotension !
coronary insufficiency; give oral or subQ.
- SIDE EFFECTS are ~same as the axns (slide 199). *effects on heart!
- Atropine is an antidote for the side effects.
CONTRAINDICATIONS (200): asthma, hyperthyroid (atrial fib), coronary insufficiency (hypoT),
peptic ulcer disease
4/8
MUSCARINIC ANTAGONISTS
compete w/ Ach and M agonists for M receptors
[After Trying a hex (Trihex.), Ben and Ipra Glistened on the pier (Glycopyrrolate),
Scooping up the Oxygen of the Tropics.]
Atropine blocks M receptors, naturally occurring
o Selected Effects (for all, see 204-205):
" Cycloplegia (lack of accommodation due to paralysis of ciliary m.), mydriasis
" Atropine flush vasodilation in cutaneous vessels, esp. of the face and
neck, as a rxn to hyperthermia. NO cholinergic innerv to blood vessels!
" Bronchodilation, but not as effective as
2
-blockers b/c density of M
decreases from trachea to bronchioles, while density of
2
increases.
" CNS atropine and scopolamine can cause hallucinations and euphoria;
stimulates medullary centers/ depression in larger doses.
o Tx:
" exposure to anticholinesterases or organophosphates (decrease Ach fx)
" Decrease salivation and resp secretion for endotrach tubing
" *acute MI when bradycardia is associated w/ hypotension w/o arrhythmias
b/c ! increased HR.
" Digitalis toxicity (digitalis stimulates the vagus n.)
o Contraindications:
" Glaucoma - b/c dilate pupil. - *can cause acute glaucoma in sensitive pts.
" Hypertension
" Alzheimers b/c cholinergic NS is imp for cognition, and these pts already
have some loss of cholinergic fnxn.
Scopolamine Tx motion sickness; naturally-occurring
o Lipid soluble crosses BBB, patches avail.
Glycopyrrolate (Robinul) decrease gastric hypermotility.
Ipratropium (Atrovent) Tx asthma/ COPD; inhaled
o NOT absorbed from GI; does NOT cross BBB.
Oxybutynin (Ditropan) inhibit hyperactive bladder
Trihexphenidyl HCl (Artane) and Benztropine (Cogentin) Tx Parkinsons
Tropicamide (Mydriacyl) examination of fundus
o Shorter duration than atropine.
o Reverse fx with pilocarpine.
RECAP:
- note that the naturally-occurring agents (Atropine & Scopolamine) are well absorbed and
widely distributed (i.e. go to CNS).
- Quaternary cpds not well-absorbed, limited distribution (i.e. Ipratropium)
5/8
GANGLIONIC AGONISTS (acting on N
1
)
Acetylcholine (recall no Tx uses, does NOT cross BBB)
Nicotine binds N
1
(and N
2
at NMJ); crosses BBB.
o FX:
" CV: - Small dose: increase HR
! Large dose: first increase HR, then
decrease HR (via modulation of
medullary center).
! Vessels: constriction (release NE and
Epi)
" Skel m.:
! Stimulation, followed by paralysis
when Rs are desensitized
" CNS:
! Stim then inhib of medullary centers
! Vomitting (chemoreceptors)
! Release ADH antidiuretic
! ~analgesia
o NICOTINE TOXICITY: acute, w/ rapid onset
" Nausea, vomitting, diarrhea, hypotension,
mental confusion
* death from respiratory paralysis
" Tx: gastric lavage w/ KMNO
4
soln; ventilation and anticonvulsant
" Chronic tobacco toxicity: many S&S not due to nicotine, but some are.
(slide 211)
GANGLIONIC ANTAGONISTS
Hexamethonium blocks N
1
receptors, NOT used clinically.
o (i.e. autonomic ganglia including parasymp (Ach) and symp: NE, adrenal medulla (Epi)
and sweat glands(Ach)).
o Does NOT cross BBB (a quaternary ammonium cpd)
o Hexamethonium Man (slide 216)
Mecamylamine (Inversine) blocks N
1
receptors, used clinically.
o Crosses BBB!
o Tx severe hypertension and hypertensive crisis: Tourettes Syndrome only
Mecamylamine b/c hexamethonium does not cross BBB.
o ACTIONS & SIDE EFFECTS see 214-215.
* Parasymps dominate (& therefore will see opposite fx w/ this drug)
everywhere except vessels and sweat glands.
" Also impotence, CNS effects (Meca only), and Tolerance.
o CONTRAINDICATIONS: Renal, cerebrovascular, and coronary insufficiency
(b/c ! marked hypotension; blood will pool away from these organs).
Therapeutic:
Analgesia
Cognitive
Enhancement
(release of Ach)
Neuroprotection
Anxiolytic (release
of GABA)
Antipsychotic
Harmful
GI distress
Hypothermia
Emesis
Hypertension
Seizures (release
of Glu in brain)
Resp distress
6/8
NON-DEPOLARIZING NEUROMUSCULAR BLOCKERS
a.k.a. competitive
-cur-
All non-depolarizing:
- Locally-acting, @ the NMJ (bind N
2
); prevent binding of Ach ! no APs.
- Produce a competitive, reversible block - can reverse with anticholinesterases, b/c
increase amt of Ach to compete.
*** NONE of the NM blockers cross the BBB; NONE ! analgesia.
D-Tubocurarine (Curare) Short onset (min), long duration (1-1.5hrs)
o Releases histamine may cause hypoT, decreased CO, bronchospasm, and urticaria.
o Muscle paralysis: face/neck ! limbs ! trunk ! intercostal mm ! diaphragm!
(Recover in reverse order.)
o Treat O.D. w/ assisted ventilation, and anticholinesterases (e.g. neostigmine,
pyridostigmine)
o Some X-rxn w/ autonomic ganglia ! some blockade in Tx doses.
o Tx use:
" w/ general anesthesia; can then decrease dose of anesthestics.
" Treat convulsions tetanus, epilepsy, *electroshock therapy*
* Assisted ventilation should be avail. immediately as a precaution.
o CV effects due to: histamine, auto gang N
1
Pancuronium (Pavulon) short onset, long duration
o does NOT release histamine so does NOT ! hypoT; is M-specific!!
o M. relaxant for endotrach intubation (as are many of the others!)
o Renal/hepatic degradation
Vecuronium (Norcuron) short onset, intermed duration
o congener of Pancuronium
o Hepatic/Renal degradation
o No CV fx (does not release histamine)
Atracurium (Tracrium) short onset, intermed duration
o Undergoes Hoffman degradation (spontaneous!)
o CV effects due to: (minimal) histamine release in Tx doses
Rocuronium (Zemuron) short onset, intermed duration
o Hepatic/renal degradation
o No CV fx (does not release histamine)
Mivacurium (Mivacron) short onset, short duration
* degraded by pseudocholinesterase, so if pt doesnt have that enzyme, drug will have
increased action BAD.
7/8
DEPOLARIZING NEUROMUSCULAR BLOCKERS
Locally-acting, @ the NMJ (bind N
2
).
Succinylcholine (Anectine) rapid onset, ultra-short dur.
o CV effects due to: Histamine, SA node M receptors, and
Autonomic Ganglia fx
o When combine w/ N
2
, two phases:
" PHASE 1: Depolarizing block ! muscle activation
(fasciculations)
! Action would be like super-potent Ach
! Antagonized by curare
! Intensified by anticholinesterases
" PHASE 2: Desensitized block (acting like the
competitive NM blockers)
! Antagonized by anticholinesterases
! Intensified by curare.
RECALL:
- S.T.A.M. release hiSTAMine!
- V.A.R. intermediate duration
- V.R. no CV fx
NOTE: not on list, but in slides and some in review session
Benzoquinonium BOTH competitive and depolarizing NM blocker.
o A synthetic, quaternary ammonium cpd.
o Also has considerable anticholinesterase activity.
Drug-drug Interaxns that ! Enhanced NM Blockade
o Inhalational Anesthetics: Ether, Halothane, Isoflurane
" Have curare-like axn i.e. act on CNS and cause relaxation (must decrease
amt curare if given w/ these).
" Synergize w/ competitive NM blockers.
o Antibiotics: Streptomycin, neomycin, Polymyxin
" Cause competitive NM blockade decrease release of Ach; can have
synergistic fx w/ competitive NM blockers.
" Similar effects w/ colistin and kanamycin
Advantages:
Rapid onset
Ultra-short duration
IM injxn
Disadvantages:
Hyperkalemia (due to
depolarizations)
Cardiac dysrhythmias (due
to hyperkalemia)
Masseter spasm
* Malignant Hyperthermia:
some have big release of
Ca and activate a lot of
enzymes, e.g. patients w/o
pseudocholin-esterase.
Increased ICP, IOP, IGP
8/8
ANTICHOLINESTERASES
They inhibit cholinesterase ! increase Ach ! *enhance activity of cholinergic NS*
Potential sites of axn:
- postgang parasymp neuroeffector jnxns (M)
- postgang symp cholinergic sites, (i.e. sweat glands EXCEPT palms, soles, and axillae) (M)
- symp and parasymp ganglia (N
1
)
- skeletal NMJ (N
2
)
- adrenal medulla (N
1
)
- CNS many cross BBB
REVERSIBLE:
o Edrophonium (Tensilon) Dx myasthenia gravis (pt has decreased Ach Rs)
" Rapid onset, short duration so NOT used for Tx
" Stimulates skel mm by a direct axn (But primary effect is block of Ach-ase)
" [example pt shows improvement of ptosis and weak smile]
o Physostigmine (Eserine) for certain types of glaucoma and atropine O.D.
" Readily absorbed from GI, subQ, and mucous membs
" Crosses BBB ! CNS stim then depression
* ! M and N axns (INdirectly by inhib. of Ach-ase, NOT directly on N or M)
o Neostigmine (Prostigmin)
" Clinical Uses:
! Dx and Tx of myasthenia gravis
! post-op bladder and bowel atony
! to reverse non-depolarizing NM blockers (-cur-)
" No CNS fx
* ! M and N axns, w/ DIRECT axn on skeletal m via stim of N
2
o Pyridostigmine (Mestinon) Tx of myasthenia gravis
" same axns as neostigmine (w/ direct axn on N
2
)
" lasts longer, fewer side fx
IRREVERSIBLE
o Echothiophate (Phospholine) [and DFP, not on list] Tx Glaucoma
An organophosphorous cpd
Long duration of axn
not preferred but used when other Rx not helping
* can cause CATARACTS in older pts
o Toxicity ! M, N, and CNS fx
o Pyridostigmine given as prophylaxis to block irreversible binding.
o Tx of Intoxication:
! Atropine (blocks M axn), Assisted ventilation, Remove source
! Tremethadone or thiopental
! CHOLINESTERASE REACTIVATORS (Pralidoxime (2-PAM) and
DAM)
Not on drug list:
- Nerve gases
(Sarin, Tabun,
Soman)
- Insecticides
1
Pharmacology Assessment 4 (start of Block 2)
AUTOCOIDS
Local hormones produced by various tissues that act on same or nearby tissues.
5 Categories: Eicosanoids, Kinins, Natriuritic peptides, Endothelins, and Other
Eicosanoids
Some specific eicosanoids and their actions
System PGE
2
PGI
2
PGH
2
PGF
2
! TxA
2
Cardio " BP,
dilate # vessel
" BP, "platelet
aggregation,
dilate # vessel
$ platelet
aggregation
-- $BP, $ platelet
aggregation,
constrict # vs
Renal Vasodilation % $ blood flow
$ natriuresis, kaluresis, " Cl
-
$ renin; " ADH
-- -- --
Respiratory dilate bronchioles -- bronchoconstriction
Gastro " acid secretn,
$ peristalsis
" acid secretn
(esp in fundus)
-- $ peristalsis --
Reproductive relax empty
uterus,
contract gravid
uterus,
induce abortion
-- -- contracts
every
uterus;
Corpus Leut
regression;
induce abort.
--
CNS $hyperthermia -- -- -- --
Autonomics " NE release %"BV constriction
that was caused by NE,ADH,A2.
-- -- --
Metabolism " lipolysis (in adipose + heart) -- -- --
Other hyperalgesic;
PGE1 (synth)
$ erection
hyperalgesic -- -- --
Associated
DRUGS
Dinoprostone Epoprostenol
(other analogs)
Dinoprost
Carbaprost
Major Synthetic Steps: (see slide 250)
o Phospholipids & arachidonic acid
o COX I and COX II convert arachidonic acid to PGG
2
! inhibited by aspirin and ibuprofen
! COX I constituitively present
! COX II induced in most tissues by two things (??)
Selective COX II inhibitors: Celecoxib (Celebrex) & Rofecoxib (Vioxx)
o PGG
2
is a precursor for:
prostaglandins
prostacyclin (PGI
2
) " platelet aggregation
thromboxane - $ platelet aggregation
o Synthesized as needed (not stored in tissues)
2
Eicosanoids and their Analogs
PGI
2
= Epoprostenol (Flolan) very unstable
o Tx: severe Pulmonary Arterial HTN; congenital heart defects. Can be substituted
for heparin during dialysis in renal disease (why?).
o PGI
2
analogs:
! Carbacyclin & Iloprost - more stable; used for tx gastric ulcers
! Trepostinil and Beraprost same uses as Epoprostenol
o Side efx: jaw and muscle pain; very expensive
PGE
1
= Alprostadil
o Used to tx congenital heart defects & erectile dysfunction
o Misoprostol, Rioprostil PGE
1
analogs for tx gastric ulcers
o Gemeprost PGE
1
analog dilation of cervix for uterine exam
PGE
2
Dinoprostone (Cervidil) dilation of cervix for uterine exam; induce abortion in
gravid uterus; decrease postpartum hemorrhage
PGF
2
! (Dinoprost) and 15-methyl-PGF
2
! (Carbaprost) induce labor and abortion
Latanoprost (Xalatan) preferred tx for glaucoma
o PGF
2
! prodrug that $ outflow of aqueous humor via uvulosclera output
o side efx: permanent change of eye color (brown)
o Combo: Latanoprost + Timolol = Xalacom.
Niacin
o tx: atherosclerosis by $ HDL levels
o Side efx: skin flushing
Cordaptive - PGD2-1 receptor antagonist combo (Niacin + Laropiprant)
o Tx atherosclerosis without flushing.
Lets Review:
' Drugs to tx gastric ulcers: Carbacyclin, Iloprost, Misoprostol, Rioprostil
' Drugs with Gynecological uses: Dinoprostone (PGE
2
), Gemeprost, Dinoprost & Carbaprost
' Good tx for glaucoma: Latanoprost
' Drugs to tx atherosclerosis: Niacin, Cordaptive
' Drugs to tx ductus arteriosis: Epoprostenol, Alprostadil
Other Notes:
' NEVER prescribe anti-inflamms or COX inhibitors to CHF patients!!! (but baby aspirin is OK
b/c it blocks TxA
2
without blocking those protective prostaglandins).
' hyperalgesic this is why antiinflamm like COX inhibs " pain.
' in Cirrhosis with ascites, have # PG syn.
3
The Other Autacoids
Kinins
Major Synthetic Steps (see slide 263)
' Kininogen gets metabolized by Kalikrein (enzyme) into Bradykinin (or Kallidin)
' Bradykinin actions: venoconstriction, pain, $catecholamines, bronchoconstriction, dieuresis,
natriuresis
' ACE (Angiotensin Converting Enzyme) has 2 functions:
o $ Angiotensin II
o " Bradykinin
ACE Inhibitors (slide 263)
o Preferred HTN Rx for pts with diabetes mellitus (with good renal fxn).
o Side efx: cough
Aprotinin (Trasylol) - Inhibits kallikrein
o (not common use) reduce blood loss in patients undergoing coronary bypass surgery
o side efx: anaphylactic shock
Natriuretic Peptides
Endogenous Types:
o ANP (atriopeptin) synthesized 1 in atrium
o BNP (brain natriuretic peptide) synth. in ventricles & brain
o CNP (C-type) synth. in brain and endothelial cells.
Stimuli that release them (slide 269): $BP, $AngioII, endothelin, sympathetic stimulation
Effects (slide 270): diuresis, natriuresis, vasodilation, "aldosterone
Inactivated by neutral endopeptidase (so inhibiting endopeptidase would prolong NP actions)
Nesiritide (Natrecor) recombinant BNP; tx dyspnea due to CHF (compare to
nitroglycerine); side efx: hypotension
Endothelins most potent vasoconstrictors in the body whoa
Endopeptidases are needed for cleavage/activation. Different isoforms are pharmalogicly distinct.
Actions are mediated through endothelin receptor sub-types (ETA, ETB1, ETB2).
Endothelin Receptor Antagonists: Tx pulmonary HTN (but all have bad side efx)
Bosentan (Tracleer) blocks ET1 A+B receptors (hepatotoxic, peripheral edema)
Sitaxentan (Thelin) selective ET1A blocker (hepatotoxic; flushing; Warfarin interaction)
Ambrisentan (Letairis) selective AT1 receptor blocker (flushing, but less hepatotoxic)
Other Substances
Substance P & Calcitonin vasodilator; neurotransmitter (pain signals)
VIP (Vasoactive Intestinal Peptide) vasodilator, NTM
Histamine, Angiotensin II, and Serotonin to be covered later in the course
4
DIURETICS
Drugs that affect the Kidney so that you excrete more fluid. Many are used as Anti-Hypertensives
Review: pathway through the kidney and key facts about each
' Glomerulus: things that influence GFR:
o Capillary permeability
o Filtration pressure regulated by afferent
arterioles
o Renal blood flow
o Plasma oncotic pressure
' Proximal convoluted tubule: bicarbonate reabsorption
' Loop of Henle: in the medulla
' Thick Ascending Limb: Na-K-2Cl symport; water
impermeable
' Distal convoluted tubule: macula densa; aquaporin-2
(regulated by ADH); 3 more segments
o Na-K-aldosterone independent (has Na-Cl symport)
o Aldosterone sensitive segment
o Sodium load segment
' Collecting Duct: one last chance for water reabsorption
Proximal Convoluted Tubule Diuretics:
Acetazolamide (Diamox) - Carbonic Anhydrase Inhibitor
o Action: inhibit C.A & HCO
3
-
loss in urine (alkaline)
! Cl
-
is reabsorbed instead
! Also $ excretion of NaCl & H
2
O
o Tx is limited, but may be used for: glaucoma; cysteinurea (alkaline urine $cysteine
excretion); seizures ("pH helps), and occasionally liver sirrhosis & renal failure
o Side Efx: metabolic acidosis, hyperchloremia, drowsiness, $ sensitivity to thiazides
Mannitol - Osmotic Diuretic (10-fold $ urine flow)
o Tx: prophylaxis of acute renal failure when there is low GFR (ex: trauma, shock)
o Inert; $ osmolarity of plasma & tubular fluid so more water flows into PCT.
o side efx: volume overload may &heart failure
Loop Diuretics:
o inhibit Na-K-2Cl symporter; $renin; maintain GFR
o causes $$diuresis w/ significant NaCl losses; venodilator
o General Tx: edema, hypercalcemia, washout toxins, prophylaxis for renal failure,
dieuretic for HTN used w/ other drugs.
o Side efx:$BUN, hypokalemia, alkalosis, ototoxicity, drug interactions
Furosemide (Lasix) - inhibits NaCl resorption; high safety margin; interacts with Warfarin
5
Bumetanide (Bumex) - 40x more potent than furosemide (and doesnt interact with
warfarin)
Torsemide (Demadex) - longer half-life (dose once daily)
Distal Convoluted Tubule Diuretics:
Thiazide Diuretics
o Tx: HTN (but not with diabetes mellitus), edema from CHF, liver cirrhosis, renal
failure, nephrogenic diabetes insipidus (b/c "receptors mean Desmopressin no help).
o Action: inhibit Na/Cl symporter in the Na-K-Aldo independent segment, causing
natriuresis and dieuresis (and many other side efx).
! Short Term Effects: dieuresis, hypokalemia, "CO and "BP
! Long Term Effects: " hypervolemia & direct vasodilation (unknown mech.)
o Side efx: (a lot, see slide 38) Hypokalemia, hypo-Mg, hyper-Ca, hyperuricemia,
hypercholesterolemia
o Class 1 used when GFR is high (>40 ml/min)
! HYDROCHLOROTHIAZIDE (Esidrex) short-acting; tx HTN,
nephrogenic diabetes insipidus
! CHLORTHALIDONE (Hygroton) long-acting, tx HTN
! Quinethazone -
o Class 2 used when GFR is lower (20<40)
! Metolazone - $ potency, tx HTN even if renal insufficiency is present
! Indapamide - $$ potency, tx HTN; also has direct vasodilatory effects
K-sparing Diuretics inhibit Na resorption in DCT. Often used with HCTZ to normalize K
+
.
o SPIRONOLACTONE (Aldactone) aldosterone antagonist (competitive
inhibitor)
o Eplenerone (Inspra) aldosterone antagonist
o AMILORIDE (Midamor) and TRIAMTERENE (Dyrenium)
! inhibit Na reabsorption in late distal tubule
! used with other diuretics like HCTZ
! side efx: hyperkalemia, anemia
ANTI-DIURETICS -Act on Collecting Ducts
ADH = 8-Argenine Vasopressin - acts on 2 receptors
o V
1
receptor: vasopressor (via IP
3
and Ca
++
release)
o V
2
receptor: activates aquaporin for $ water reabsorption
Desmopressin (DDAVP) V
2
receptor agonist; tx central diabetes insipidus and bleeding
Demeclocycline (Declocyclin) pro-diuretic, anti-ADH
o use with OPC-31260
o action: antagonizes ADH at V
2
receptors
o tx Syndrome of Inappropriate Secretion of ADH
6
HYPERTENSION
Defined as:
Contraction of Vascular Smooth Muscle: Calcium and Important Receptors
An $ in intracellular Ca
++
is required for contraction
o Ca
++
can be released from the Golgi
o Ca
++
can enter the cell via L-Type Ca Channel
Now, Ca
++
can bind calmodulin& move troponin& free myosin head to grab actin
filament& contraction of muscle fiber& vasoconstriction.
Important Receptors:
o Gq coupled receptors & IP
3
& $ Ca
++
release
! !1 adrenergics, Angiotensin II receptors, and endothelin-1 receptors
o Gs and Gi coupled receptors regulate cAMP
! (-adrenergic receptors $ cAMP & $PKA & $Ca
++
! M
2
muscarinic receptors " cAMP & "PKA & "Ca
++
Control of Blood Pressure
Baroreflexes rapid adjustment of BP
o Baroreceptors in carotid sinus signal the
o Solitary Nucleus in the brainstem, which signals the...
o Vasomotor Center in the medulla, which is tonically active and will $or" tone.
Kidney slow but long-term adjustment of BP
o Juxtaglomerular cells are stretch sensors in afferent arteriole: lack of
stretch & signal Renal Nerves ((1-adrenergics) & $ Renin.
o Macula Densa senses osmolarity in distal tubules: low osmolarity & $ Renin.
BP Classification SBP mmHg DBP mmHg
Normal <120 and <80
Pre-HTN 120-139 or 80-89
Stage 1 HTN (drug tx advised) 140-159 or 90-99
Stage 2 HTN >160 or >100
7
ANTI-HYPERTENSIVES that interfere with the Sympathetics
Centrally Acting Agents
General: They stimulate central postsynaptic !
2
receptors in the RVLM, which causes "symp output
& "HR, "perif vascular resistance
!-Methyldopa (Aldomet) false NTM, mimics NE.
o Only used for severe HTN in preeclampsia during pregnancy b/c severe side efx.
(but not teratogenic)
o Side Efx: sedation, sleep disturbance, Na + H
2
O retention; immunological dysfxn.
Clonidine (Catapres), Guanfacine (Tenex), and Guanabenz (Wytensin)
o !2 agonists in RVLM
o Side efx: sedation, drowsiness, fatigue, anxiety, Na + H
2
O retention, xerostomia
o Clonidine is also analgesic.
o Guanabenz also lowers plasma cholesterol (and doesnt retain H
2
O).
Peripheral Sympatholytics
Reserpine
o Tx: inhibits NE uptake into vesicles % endogenous NE is depleted
o Side Efx: do NOT use in pts with peptic ulcers or hx of depression/suicide!!!
o Note: it may be cheap, but its a generic drug from India, so theres no drug company
buffer if tx goes bad and the patient wants to sue somebody. Hmm.
Guanadrel not discussed in lecture.
!-adrenergic Antagonists
General: cause "arterial pressure & small reflex $HR
Prazocin (Minipress) !
1
specific antag.; tx HTN
o short acting, so $dose gradually to prevent postural hypotension
o Other benefits: $HDL & improves insulin resistance
Doxazocin (Cardura) and Terazocin (Hytrin) - !
1
specific antag.
o Tx: HTN + BPH (enlarged prostate)
o Side efx: orthostatic hypotension
Phenoxybenzamine and Phentolamine non-selective !-antagonists
o Obsolete for tx HTN. Used for Pheochromocytoma.
8
Beta-Blockers (slide 50)
General Tx: HTN, esp associated with CHF or previous MI (prophylactic b/c protects against CAD).
(Can be used to treat CHF, but dose must start LOW and titrate upward b/c of initial "CO)
General Action: " CO by "HR + "contractility; inhibits reflex tachycardia
General Side Efx: Raynauds, bradycardia, bronchospasm, depression/CNS efx, drug interaction w/
conduction blockers, fatigue, "GFR
Non-Selective (-blockers: (slide 48)
Propanolol (Inderol) also anti-arrhytmia
Carvedilol (Coreg) blocks !+( receptors non-selectively
o 1 drug for CHF
o Also "ROS production.
Pindolol (Visken) and Acebutol (Sectral) partial agonists
o ISA (increased sympathetic activity) & less drastic "CO and HR
Timolol (Blocadren) very slight ISA
Labetalol (Normodyne) -
Selective (
1
Blockers
Metoprolol (Lopressor) and Atenolol (Tenormin) cardioselective ((1) % OK for
asthmatics
Betaxolol (Kerlone) and Bisoprolol (Zebeta) long-acting
Esmolol (Brevibloc) very short half-life; used to tx tachycardia
Nebivolol (Bystolic) newest; claims to exhibit vasodilation b/c $ NO
Direct Vasodilators (mnemonic? MSNDFH)
Usually Rxd only after 2 or 3 other drugs have been tried without success.
Minoxidil (Loniten) a pro-drug (liver sulfation) that opens K
+
/ATP channels in smooth muscle
o dilates arterioles (not veins)
o Side efx: reflex tachycardia; hirsutism & topical cream sold as Rogaine
Sodium Nitroprusside (Nitropress) prodrug for NO
o Dilates both arteries and veins via $cGMP & "TPR & "afterload
o Tx: great for HTN crisis and Left-sided HF.
o Side efx: hypotension, tachycardia, palpitations, metabolism into cyanide, nausea
Diazoxide (Hyperstat IV) opens K
+
channels in smooth muscle
o Tx HTN crisis
o Effect augmented in combo with (-Blocker (b/c BB prevents reflex tachycardia)
o Side efx: tachycardian, fluid retention, hyperglycemia (inhibits insulin release)
Fenoldopam (Corlopram) D
1
receptor agonist; short half-life
o tx HTN crisis; contraindicated for glaucoma.
Hydralazine (generic) tx CHF
9
Interfere with Renin/Angiotensin
ACE Inhibitors = (-pril)
Improves prognosis for CHF by reducing afterload!!!
First choice anti-HTN for diabetics.
Mechanism of Action: block ACE enzyme that 1) converts Angio1&Angio2 & 2) degrades bradykinin
Side Efx: orthostatic hypotention (first dose), hyperkalemia, dry cough, angioedema, fetotoxicity
Captopril (Capoten) short half-life; $synthesis of prostaglandins & $vasodilation
Enalapril (Vasotec) prodrug & (de-esterification) & elanaprilat (active)
Lisinopril (Zestril) lysine derivative of elanaprilat
Ramipril (Altace) prodrug with long half-life
Fosinopril (Monopril) ideal for CHF pts with renal disease (b/c 100% hepatic metabolism)
Angiotensin II Receptor Blockers = (-sartan)
Advantages over ACE-I: no cough, "angioedema
Disadvantages compared to ACE-I: dont affect ($) bradykinin (% no vasodilaton)
Mechanism of Action: blocks Angio2-1 Receptor (AT1)
- more effective angio stopper than ACE-I % better $ vasodilation and duresis.
Side Efx: orthostatic hypotension, hyperkalemia, fetotoxicity, hepatic dysfunction
Losartan (Cozaar) prodrug & active metabolite is non-competitive inhibitor of receptor
o Also $ uric acid excretion & inhibits CYP450
Irbesartan (Avapro) and Valsartan (Diovan)
Telmisartan (Micardis) longest half-life; not excreted by kidneys
Renin Inibitor
Aliskiren (Tekturna) nonpeptide inhibitor of renin & no Angio1
o NEVER used alone; usually used with A2RB (like Valsartan)
L-type Calcium Channel Blockers (CCBs)
Verapamil a phenylalkylamine; tx angina and arrhythmias; "" contractility + AV conduction
o Good Tx for healthy patients with HTN + arrhythmias or angina.
Diltiazem benzothiazepine; good intermediate (can "P without $$ reflex tachychardia)
Dihydropyridines: Amlodipine (long acting), Nifedipine (short acting), Nicardipine, etc
o Tx HTN (may use with diuretic to " edema)
o $ selectivity for L-type vascular smooth muscle (not cardiac)
10
Congestive Heart Failure (CHF)
The Death Spiral:
1) something causes activation of sympathetics and renin/aldo system
- may be "CO, MI, HTN, or other problem with volume or pressure overload
2) $NE, Angio2, Aldo, Vasopressin, Endothelin
- $ contractility and HR via vasoconstriction ($preload + afterload) and fluid
retention (note that this also $O
2
demand).
3) Initially helpful, but prolonged presence causes problems = Maladaptive responses:
- myocyte hypertrophy prevents effective contractility AND $O
2
demand.
- peripheral and pulmonary edema (from vasoconstriction) & orthopnea + PND
- interstitial fibrosis, apoptosis, and arrhythmias.
$ Many of the above drugs are used for Tx!!!
Which one do you use???
$ ACE Inhibitors are #1
o clinically proven to reduce
morbidity/mortality in CHF!!!
o They balance vasodilation (via Bradykinin) and " myocyte hypertrophy.
$ Use AT2-Blockers instead of ACE-I (maybe equally effective) if cough develops
Digoxin (Lanoxin) a digitalis glycoside that $Ca
++
intracellularly for $contractility.
o Mechanism of Action: blocks Na
+
/K
+
-ATPase causing $Na intracellularly, which
allows $ activity of Na
+
/Ca
++
exchanger, which $Ca
++
intracellularly & $ contractility.
o 1 Tx: severe CHF w/ low EjFr.
o Side efx: many drug interactions, including diuretics ($arrythmias), warfarin;
Individual response to digoxin is highly variable.
Milrinone (Primacor) phosphodiesterase inhibitor & $cAMP; short-term IV use only
Bosentan (Tracleer) competitive Endothelin-1 Receptor antagonist & vasodilation
o Tx: CHF, pulmonary arterial HTN (fatal w/ no great tx)
o Side efx: teratogenic, hepatotoxicity, hole in wallet (very expensive!)
Bepridil (Vasocor) a miscellaneous anti-HTN that inhibits both L-type Ca
++
& Na
+
channels
o Side efx: arrhythmias, agranulocyosis
Vasopeptidase Inhibitors: Omapatrilat & Sampatrilat
1
A 73 A 73- -year year- -old woman with congestive heart old woman with congestive heart
failure requires treatment with failure requires treatment with digoxin digoxin
[ [Lanoxin Lanoxin] to improve cardiac muscle ] to improve cardiac muscle
contractility and reduce her SOB. contractility and reduce her SOB. Digoxin Digoxin
works by: works by:
A. A. Activating beta Activating beta- -adrenergic receptor in the adrenergic receptor in the
heart heart
B. B. Increasing the synthesis of Increasing the synthesis of cAMP cAMP
C. C. Directly activating G proteins Directly activating G proteins
D. D. Releasing mitochondrial calcium from Releasing mitochondrial calcium from
storage storage
E. E. Inhibiting the sodium/potassium Inhibiting the sodium/potassium ATPase ATPase
A 50 year A 50 year- -old man with well old man with well- -controlled type II controlled type II
diabetes and normal renal function requires an diabetes and normal renal function requires an
oral agent to treat his hypertension. Select the oral agent to treat his hypertension. Select the
best agent from this group of drugs. best agent from this group of drugs.
A. A. Atenolol Atenolol
B. B. Nifedipine Nifedipine
C. Hydrochlorothiazide C. Hydrochlorothiazide
D. D. Captopril Captopril
E. E. Verapamil Verapamil
Which of the following drugs would be most Which of the following drugs would be most
likely to trigger an attack of gout in an likely to trigger an attack of gout in an
individual who is individual who is hyperuricemic hyperuricemic? ?
A. A. Atenolol Atenolol
B. B. Nifedipine Nifedipine
C. C. Hydrochlorothiazide Hydrochlorothiazide
D. D. Captopril Captopril
E. E. Verapamil Verapamil
Which of the following is representative of
a class of agents that is contraindicated in
pregnancy by virtue of teratogenicity?
A. A. Atenolol Atenolol
B. B. Nifedipine Nifedipine
C. Hydrochlorothiazide C. Hydrochlorothiazide
D. D. Captopril Captopril
E. E. Verapamil Verapamil
Which of the following would be a poor choice Which of the following would be a poor choice
as an antihypertensive in an individual with as an antihypertensive in an individual with
insulin insulin- -dependent diabetes because it masks the dependent diabetes because it masks the
symptoms of hypoglycemia and may delay symptoms of hypoglycemia and may delay
recovery from a hypoglycemic episode? recovery from a hypoglycemic episode?
A. A. Atenolol Atenolol
B. B. Nifedipine Nifedipine
C. Hydrochlorothiazide C. Hydrochlorothiazide
D. D. Captopril Captopril
E. E. Verapamil Verapamil
An asthmatic requires antihypertensive An asthmatic requires antihypertensive
therapy. Which of the following potential drug therapy. Which of the following potential drug
choices would be most likely to exacerbate the choices would be most likely to exacerbate the
pulmonary condition? pulmonary condition?
A. A. Atenolol Atenolol
B. B. Nifedipine Nifedipine
C. Hydrochlorothiazide C. Hydrochlorothiazide
D. D. Captopril Captopril
E. E. Verapamil Verapamil
2
Which of the following Which of the following antihypertensives antihypertensives would would
exacerbate COPD or asthma by thickening the exacerbate COPD or asthma by thickening the
airway mucous, thereby obstructing the airway mucous, thereby obstructing the
airways? airways?
A. A. Atenolol Atenolol
B. B. Nifedipine Nifedipine
C. C. Hydrochlorothiazide Hydrochlorothiazide
D. D. Captopril Captopril
E. E. Verapamil Verapamil
Compared with Compared with nifedipine nifedipine, , diltiazem diltiazem and and
verapamil verapamil: :
A. are suitable for use in conjunction with a A. are suitable for use in conjunction with a
beta beta- -blocker or blocker or digoxin digoxin
B. cause more reflex tachycardia B. cause more reflex tachycardia
C. C. produce a greater slowing of AV nodal produce a greater slowing of AV nodal
conduction conduction
D. cause significant D. cause significant venodilation venodilation leading to leading to
profound orthostatic hypotension profound orthostatic hypotension
E. produce more significant positive E. produce more significant positive ionotropic ionotropic
effects effects
Compared to Compared to captopril captopril, , losartan losartan: :
A. Has a higher incidence of A. Has a higher incidence of bronchospasm bronchospasm and and
hyperuriciemia hyperuriciemia
B. is B. is prefered prefered for managing hypertension during for managing hypertension during
pregnancy pregnancy
C. C. doesn doesn t inhibit synthesis of t inhibit synthesis of angiotensin angiotensin II II
D. blocks catecholamine D. blocks catecholamine- -mediated mediated
vasoconstriction vasoconstriction
E. should only be used after other drug classes E. should only be used after other drug classes
like calcium channel blockers and beta like calcium channel blockers and beta- -blockers blockers
have been tried and found to be ineffective have been tried and found to be ineffective
A 57 year A 57 year- -old man with CHF being treated with old man with CHF being treated with
digoxin digoxin, , furosemide furosemide and and captopril captopril now presents now presents
with a with a- -fib. Serum electrolytes are normal and fib. Serum electrolytes are normal and
the the digoxin digoxin level is at the upper end of the level is at the upper end of the
normal range. After electrical conversion, he is normal range. After electrical conversion, he is
started on anticoagulant therapy, together with started on anticoagulant therapy, together with
an anti an anti- -arrhythmic agent, arrhythmic agent, quinidine quinidine. What is the . What is the
most likely outcome of the last addition? most likely outcome of the last addition?
A. development of A. development of quinidine quinidine toxicity toxicity
B. B. development of development of digoxin digoxin toxicity toxicity
C. inhibition of C. inhibition of furosemide furosemide renal activity renal activity
D. increased D. increased angiotensin angiotensin levels levels
Angiotensin Angiotensin- -converting enzyme inhibitors are converting enzyme inhibitors are
associated with a relatively high incidence of: associated with a relatively high incidence of:
A. hepatitis A. hepatitis
B. B. hypokalemia hypokalemia
C. C. agranulocytosis agranulocytosis
D. D. proteinuria proteinuria
E. E. hirsutism hirsutism
Do not administer this drug to patients with Do not administer this drug to patients with
second second- -degree or greater heart block or degree or greater heart block or
administer with other drugs that produce heart administer with other drugs that produce heart
block. block. To which of the following would such a To which of the following would such a
warning justifiably apply? warning justifiably apply?
A. A. Captropril Captropril
B. B. Losartan Losartan
C. C. Nifedipine Nifedipine
D. Nitroglycerin D. Nitroglycerin
E. E. Verapamil Verapamil
3
A 43 A 43- -year year- -old man asks his physician for a old man asks his physician for a
prescription for prescription for sildenafil sildenafil [Viagra] to enhance [Viagra] to enhance
his sexual performance. Due to life his sexual performance. Due to life- -threatening threatening
hypotension, this drug should not be used in hypotension, this drug should not be used in
patients receiving which of the following drugs? patients receiving which of the following drugs?
A. ACE inhibitor A. ACE inhibitor
B. Beta B. Beta- -blocker blocker
C. C. Nitrosovasodilator Nitrosovasodilator
D. D. Thiazide Thiazide diuretic diuretic
E. AT E. AT- -1 blocker 1 blocker
Diuretic Diuretic- -induced induced hypokalemia hypokalemia can have can have
significant clinical consequences. Which of the significant clinical consequences. Which of the
following is least likely to produce this following is least likely to produce this
condition? condition?
A. A. Amiloride Amiloride
B. B. Bumetanide Bumetanide
C. Hydrochlorothiazide C. Hydrochlorothiazide
D. D. Metolazone Metolazone
E. E. Torsemide Torsemide
Amiloride Amiloride and and triamterene triamterene produce their produce their
potassium potassium- -sparing effects by: sparing effects by:
A. A. blocking tubular Na+ channels and therefore blocking tubular Na+ channels and therefore
Na+/K+ exchange Na+/K+ exchange
B. enhancing the binding of B. enhancing the binding of aldosterone aldosterone to its to its
receptors receptors
C. Hastening metabolic inactivation of C. Hastening metabolic inactivation of
aldosterone aldosterone
D. Inhibiting proximal tubular Na+/K+ D. Inhibiting proximal tubular Na+/K+- -ATPase ATPase
E. E. supressing supressing cortisol cortisol and and aldosterone aldosterone release release
from the adrenal cortex from the adrenal cortex
Most diuretics (not osmotic diuretics) can Most diuretics (not osmotic diuretics) can
significantly increase the toxicity of: significantly increase the toxicity of:
A. A. cholestyramine cholestyramine
B. B. lithium lithium
C. C. nifedipine nifedipine
D. D. phenylephrine phenylephrine
E. E. statin statin- -type anti type anti- -lipemic lipemic agents agents
A patient who is being treated with A patient who is being treated with furosemide furosemide
and and digoxin digoxin develops signs and symptoms of develops signs and symptoms of
digoxin digoxin toxicity, although a check of levels toxicity, although a check of levels
reveals that they are reveals that they are within normal limits. within normal limits.
Which of the following likely accounts for the Which of the following likely accounts for the
development of toxicity? development of toxicity?
A. A. Digoxin Digoxin displacement from plasma protein displacement from plasma protein
binding sites binding sites
B. B. Hypocalcemia Hypocalcemia
C. C. Hypokalemia Hypokalemia
D. D. Hyponaremia Hyponaremia
E. Reduction in E. Reduction in digoxin digoxin metabolism metabolism
A patient with CHF has a 3 A patient with CHF has a 3- -year history of year history of
successful treatment with successful treatment with digoxin digoxin and and furosemide furosemide. .
Following the development of Following the development of osteo osteo- -arthritis, he arthritis, he
begins high begins high- -dose therapy with a non dose therapy with a non- -specific (COX specific (COX- -
1 & 2) non 1 & 2) non- -steroidal steroidal antiinflammatory antiinflammatory agent. Which agent. Which
of the following is the most likely outcome? of the following is the most likely outcome?
A. A. Hyperchloremic Hyperchloremic acidosis, indicative of acute acidosis, indicative of acute
diuretic toxicity diuretic toxicity
B. Dramatic increase in B. Dramatic increase in furosemide furosemide s s potassium potassium- -
sparing effect sparing effect
C. C. Edema, weight gain and other signs/symptoms of Edema, weight gain and other signs/symptoms of
reduced reduced diuresis diuresis
D. Rapid onset of D. Rapid onset of digoxin digoxin toxicity due to reduce toxicity due to reduce
drug elimination drug elimination
E. Reduced E. Reduced digoxin digoxin activity because of competition activity because of competition
with the NSAID at the with the NSAID at the myocyte myocyte receptor receptor
4
A patient on which of the following drugs is A patient on which of the following drugs is
most likely to develop most likely to develop hyponatremia hyponatremia? ?
A. A. Bumetanide Bumetanide
B. B. Furosemide Furosemide
C. C. Hydrochlorothiazide Hydrochlorothiazide
D. D. Torsemide Torsemide
E. E. Mannitol Mannitol
0 0 0 0 D. D.
0 0 0 0 C. C.
0 0 B. B.
0/ 0/ A. A.
HCO HCO
3 3
- -
Cl Cl
- -
Mg Mg
2+ 2+
Ca Ca
2+ 2+
K K
+ +
Na Na
+ +
DRUG DRUG
Which of the following drugs produces the
qualitative change in urinary electrolyte profile
shown in line B? shown in line B?
A. A. Triamterene Triamterene
B. B. Furosemide Furosemide
C. Hydrochlorothiazide C. Hydrochlorothiazide
D. D. Acetazolamide Acetazolamide
E. E. Amiloride Amiloride
Rx for Angina
1. Nitrates: Nitroglycerin
! ! NO ! "cGMP ! "PKG ! relaxation of VSMC
! FX:
Venodilation! #preload (do NOT affect afterload!)
! *higher doses (e.g. IV) can ! arterial vasodilation*
Coronary Vasodilation
#Pulm Vasc R
slight #CO
BP ~same
HR ~same
! Side Fx:
Hypotension
! Reflex symp stim: tachycardia, "contractility
! #coronary perfusion
! paradoxical worsening of angina pectoris
! *** do NOT take w/ Sildenafil (Viagra) or ! HYPOtension
! Preparations (to help w/ rapid absorp & 1
st
pass metab): see slide 14 & 15!
! Tolerance avoid by having 8-12 hrs w/o Rx each day.
! Anginal Rebound do NOT stop IV suddenly or ! coronary vasospasm.
2. B-blockers: *slide 31 chart
Propranolol, Timolol cardioprotective
Naldolol water soluble
Pindolol, Labetolol ISA
Acebutolol ISA; B
1
selective
Esmolol B
1
selective
Metoprolol B
1
selective; cardioprotective
Atenolol B
1
selective; cardioprotective; water soluble
FX:
! *Tx exertional angina #HR & inotropy response to stress; #myocard O
2
demand
! Tx post-MI
! CNS fx ! #afterload (NOT preload)
! Do NOT prevent coronary vasospasm ineffective in vasospastic angina!
Side Fx: (mostly non-cardiac fx, B
2
)
! Bronchospasm, hypoglycemia, CNS fx, alopecia
! * Contraindications:
Asthma, labile type II diabetes, depression
COPD, PVD may use B
1
-selective
Sinus bradycardia, SA/AV block, decompensated CHF
! Do NOT suddenly w/draw ! rebound tachycardia ! unstable angina or MI!
3. Ca
2+
-Channel Blockers: ! L-type Ca
2+
channels only. *Slide 24
ALL PREGNANCY CATEGORY C
* B-blockers considered 1
st
choice for angina! Use CCB when pt cant tolerate BB, or BB +
nitrate does not work.
Non-DHP: use-dependent, i.e. access in the open state of the channel target CARDIAC
! Verapamil
Reduces clearance of Digoxin
Constipation
! Diltiazem
! FX of Both: (Verapamil > Diltiazem)
#HR; slow AV cndxn; #contractility do NOT use w/ CHF pts!
! # myocardial O
2
demand
arteriolar vasodilation ! #afterload (NOT preload do not relax vv)
Coronary vasodilation ! prevent or reverse vasospasm
! Side FX of Both:
* Bradycardia, asystole, SA/AV block do NOT use w/ B-blockers!
CHF
* CYP3A4 metabolized by and inhibit CYP3A4! see slide 27 for drug interaxn.
Dihydropyridines: voltage-dependent, i.e. access @ certain membrane potential target VSMC
! Nifedipine, Amlodipine, Nicardipine
! Felodipine longer t
1/2
than others.
! Isradipine - *use in pts w/ CHF (no negative inotropy); also longer t
1/2
than others!
! FX:
[More potent vasodilators ! more indirect fx. ! overall fx more subtle than non-DHP]
* #Afterload & coronary vasodilation ! main antianginal fx
! use w/ angina + left-sided valvular insufficiency
HR & contractility: overall no change.
[b/c reflex symps ! "contractility, tachycardia]
All DHP better in pts w/ CHF than non-DHP (esp. Isradipine)
! Side Fx:
excessive vasodilation ! hypotension
periph edema (b/c precap aa dilation)
paradox. exacerbation of angina b/c less blood to heart
4. Combos:
*BB + Nitrate*
! BB prevents reflex tachycardia & contractility from Nitrate hypoT
! Nitrates prevent coronary vasospasms & increased LV EDV (preload) from BB
! Both: #myocardial O
2
consumption & "subendocardial blood flow
(diff mechs)
*BB + DHP* - (slow-release or long-acting DHPs)
! DHPs prevent coronary vasospasm & ! #systemic vasc R (#afterload)
! BB prevents reflex tachycardia of DHPs
BB + non-DHP dont do it! marked fatigue; extreme bradycardia; AV block!
1
Anti-Arrhythmic Drugs Assessment 5
Clinical approach to tx arrhythmias:
1. Assess the Rhythm and Symptoms
2. Identify and Treat underlying cause of arrhythmia (caffeine, CHF, hypokalemia, drugs)
3. Then assess need for drugs/AICD.
1.) Class 1: Na+ Channel Blockers
Action: decrease membrane responsiveness by binding to open & inactivated channels
o ! rate of rise of phase 0 depolarization (tilted) " ! conduction velocity
o fewer Na+ Channels " delayed recovery " # ERP (effective refractory period)
Side Efx: Torsades de Pointes, reports of #mortality post-MI
Those with (T) < 1sec. (super fast!) $no interference with normal fxns, but will interfere
with tachycardia by interrupting re-entry.
o Lidocaine (Xylocaine) ! automaticity in ventricles only
lipid soluble $toxicity usu. manifests w/ CNS problems
IV only (short half-life and very high 1
st
pass metabolism)
o Mexilitine (Mexitil) same, except orally effective w/ GI distress $! use
Those with (T) > 1sec. (fast) prolong AP overall bad side efx $! use
o Quinidine (Quinidex) tx chronic/outpatient arrhythmias.
o Procaineamide (Procan-SR) IV only, use limited to acute control of
arrhythmias b/c bad side efx long term (SLE, GI intolerance, hyperkalemia).
o Disopyramide (Norpace)
Those with (T) > 10 sec. (eh, not so fast) - !conduction velocity $ prolong QRS
o Flecainide (Tambocor) cardiac depressant $many bad side efx.
Clinical use limited to: WPW, supraventricular arrhythmias w/out any
structural heart disease.
o Propafenone (Rhythmol) limited use in atrial arrhythmias.
2
2.) Class 2: %-Blockers
Reduce mortality post-MI (by tx sx like ischemia + Vfib)
o Adrenergic blocking " !conduction velocity and #ERP of AV node
o ! automaticity in all conducting heart tissues (if caused by Ach or ischemia)
specific for anti-arrhythmias b/c they are cardio-protective.
o Used to tx DAD (delayed after-depolarizations, ie, intracellular Ca++ overload)
o Can tx Torsades de Pointes
Metoprolol - %1 selective; use for arrhythmias is off-label use, but common.
Propanolol -
Timolol -
3.) Class 3: K+ Channel Blockers prolong repolarization " #ERP + suppress reentry
o Pacemaker rhythm of SA + AV nodes is mediated by special K+ channels
undergoing automaticity.
o Hierarchy of Pacemakers (backup plan): SA > Atrial > AV > Purkinje > Ventricular
o Common bad side efx: Torsades de Pointes
Amiodarone (Cordorone) has class 1 and 3 actions!!!!!! And some class 2 actions.
o Tx: acute life-threatening (ex: Vtach) or chronic Afib, Vfib
o drug of choice in cardiac rescuscitation. Most effective in maintaining rhythm
after Afib, BUT pts still have 80% recurrence within 1 yr.
o Half-life is 20-200 DAYS (accumulates in tissues)
o Side efx: Inhibits CYP3A4, pulmonary fibrosis, hypo- & hyper-thyroidism,
blindness, !liver
o Good: Torsades de Pointes is rarer b/c of BB + Na+B effects.
Sotolol (Betapace) mostly class 3, but has some non-selective %-Blocker effects.
o Overall, a good drug choice. Tx A + V arrhythmias.
o Contraindicated in: COPD, renal insufficiency, overt CHF, AV block, bradycardia
o Side efx: BB (bradycardia, bronchospasm). Can be used with other BBs but
watch HR carefully.
Bretylium (Bretylol) emergency IV; inhibits NE release " profound orthostatic
HTN (last resort drug).
Ibutilide (Convert) IV for acute Vfib
Dofetilide (Tikosyn)
3
4.) Class 4: Calcium Channel Blockers (CCBs)
Verapamil and Diltiazem
Actions: SA + AV depolarization is Ca++ dependent, so CCBs slow conduction velocity
specifically in the AV node " # ERP
o Good for preventing re-entry.
o Wouldnt this also cause bradycardia b/c slowing of SA node, too?? No, b/c the
drug is AV node specific. Handy.
Side Efx:
o SA, AV block
o Impaired contractility
o Hypotension
o No significant protection post-MI
o Contraindicated in WPW pts
When would you use them?
o Tx atrial arrhythmias in Pts with normal LV function, or who cant tolerate BBs
5.) Digoxin
Vagal stimulation " !conduction velocity and #ERP of AV node only
o Also !SA node automaticity
o Mechanism of Action: blocks Na/K ATPase
Side Efx: atrial fibrillation (paradoxical effect)
o Paradoxical Effect: vagal stimulation in atrium " shorter AP, # conduction
velocity, and !ERP in the atrial cells. Thats why AFib is a common side efx.
o Contraindicated in WPW pts b/c # conduction through 3
rd
pathway. !
6.) Adenosine
Tx: acute PSVT by blocking AV node
Short half-life (10 seconds)
Side Efx: tight chest, flushing, recurrence of fib.
Interactions
o Methylxanthines (like caffeine) blocks adenosine receptors
o Dypyridamole prevents uptake so effect potentiated.
o Contraindicated in WPW pts.
7.) Implantable Defibrillators: AICD. Effective chronic tx of arrhythmias.
Studies show 50% reduction in mortality.
Drug therapy may accompany AICD to reduce frequency of discharge.
4
Review:
- Good drug class for tx automaticity (DAD): %-Blockers
- Good drugs classes for tx re-entry: Class 1 (Na+ Blockers) and Class 3 (K+ blockers)
- Good drugs to tx paroxysmal supraventricular tachycardia (re-entry @AV node):
Ca++ Blockers, Digoxin, %-Blockers, and Adenosine.
- Good drug for stopping Torres des Pointes? First MgSO4 (then maybe BB.)
Treatment of Choice: the final chart from the Anti-Arrhythmia lectures.
Arrhythmia Drug/Device of Choice Alternatives
Atrial Fibrillation (Afib)
(Rate Control)
CCB, BB, Digoxin None
Atrial Fibrillation
(conversion to SR)
DC Cardioversion IV procaineamide or
ibutilide,
Oral propafenone or
flecainide.
Atrial Fibrillation
(Maintinence of SR)
Amiodarone, Sotolol,
Flecainide, Propafenone,
Dofetilide
Quinidine, procaineamide,
disopyramide
Supraventricular Tachy.
(SVT, acute termination)
IV adenosine or CCB IV esmolol, some other BB,
or digoxin
SVT
(long-term suppression)
BB, CCB, flecainide,
propafenone, amiodarone,
sotolol, or digoxin
Quinidine, procainamide or
disopyramide
Ventricular Premature
Contractions (VPC)
If asymptomatic, no drugs. BB for pts with symptoms
Ventricular Tachycardia
(SCD or post-MI with ! EjF)
AICD Amiodarone, sotolol,
procainamide, mexilitine
Cardiac Glycoside-induced
Ventricular Arrhythmias
Dogoxin immune Fab Lidocaine, Phenytoin
Torsades de Pointes
(Drug-Induced)
IV magnesium sulfate
(and remove offending drug!)
Cardiac Pacing, isoproterenol
Hyperuricemia and Gout
1. Hyperuricemia = >7mg/dL uric acid in plasma
Causes:
! 1. Metabolic (10%)
Primary: specific enzyme abnls
Secondary: synth too much purine
! certain blood disorders
! chemo- or radiation Tx
! 2. Renal (90%)
Primary: kidney Dz (renal failure)
Secondary:
! long-term diuretic Tx
! toxemia of pregnancy
2. Purine Metabolism:
3. Tx Goals & Rx:
Acute attack terminate
! Colchicine, Indomethacine
Acute gouty arthritis prevent recurrence
! Colchicine
Ureate crystal deposition reverse/ prevent complications
! Allopurinol; Probenecid, Sulfinpyrizone
Kidney stones prevent formation
! Allopurinol
Other assocd factors prevent
4. Colchicine
Hypoxanthine guanine
phosphoribosyl transferase
(HGPRT)
Xanthine Oxidase (X.O.)
Xanthine Oxidase (X.O.)
PRPP synthase
MECH: depolymerizes m-i-c-r-o-t-u-b-u-l-e-s
TX: only against gouty arthritis
! Terminate acute attacks of gout
! Prevent recurrence of gouty arthritis
! Familial Mediterranean fever
SIDE FX:
! GI acute
! Blood dyscrasias chronic
note: dyscrasia = a morbid general state resulting from the presence of abnl material
in the blood, usu applied to diseases affecting blood cells or platelets.
5. Indomethacine
PHARM:
! COX inhibitor
! Analgesic, antipyretic
! Inhibit leukocyte motility
TX: acute attack
PK: 50mg, 3x/day
SIDE FX(toxic):
! GI: N/V, ulcers (b/c COX inhibitor!)
! CNS: severe frontal headache
! Hematopoietic disorders
! Antagonizes Furosemide & HCTZ
6. Allopurinol
MECH:
! Competitively inhibits X.O.
! ! Oxypurinol non-competitively inhibits X.O.
FX:
! " UA in plasma and urine
! # xanthine & hypoxanthine in plasma and urine i.e. oxypurine precursors
! ! dissolve UA crystals in joints and kidneys
! prevent UA kidney stone formation
* TX:
! 1
o
Hyperuricemia:
gout due to enzyme abnls
children w/ familial juvenile hyeruricemic nephropathy
! 2
o
Hyperuricemia:
hematologic disorders (e.g. multiple myeloma)
chemo-Tx
SIDE FX:
! #acute gout incidence
! Hypersensitivity rxns: Dermatitis (2%), Exfoliative dermatitis
Desensitize w/ Low dose of allopurinol OR substitute Oxypurinol
! Liver fnxn fx
! 6-mercaptopurine interaxn ! "dose to 25%
! Ampicillin (& related antibiotics) contraindicated!!
7. Uricosuric Agents (Probenecid & Sulfinpyrizone)
Renal Handling of UA (pic below)
! 1. Filtered in glomerulus
! 2. Reabsorbed in PT (= pre-secretory reabsorption)
! 3. Secreted
! 4. Partially reabsorbed (= post-secretory reabsorption)
Probenecid
! MECH:
Inhibits transport of organic anions across epith barriers
Interferes w/ UA reabsorp by organic acid transporter (brush border of PT)
! FX:
#UA excretion if pt excretes <1g/day
! Dissolve UA crystals in joints
! [Note: given w/ adequate hydration to pt w/ good renal fnxn]
! SIDE FX:
Salicylates inhibit uricosuric action e.g. aspirin!
Sulfinpyrizone
! MECH: (same as Probenecid)
! FX:
More potent than Probenecid in mobilizing UA crystals
(otherwise same)
! SIDE FX:
GI fx
Blood dyscracias
Inhibits metab of oral hypoglycemics ! hypoglycemia
# platelet lifespan
Antihistamines (not included: slides 1-18)
I. First Generation
A. Drugs: --- * see slide 24 for comparison
1. Ether or ethanolamine derivatives:
a) Diphenhydramine (Benadryl)
b) Deminhydrinate (Dramamine)
c) Clemastine (Tavist)
2. Alkylamine derivatives:
a) Chlorpheniramine (Chlor-Trimeton)
b) Brompheniramine (Dimetane)
c) Triprolidine (Actidil)
3. Phenothiazine derivatives: *the most sedative & antiemetic
a) Promethazine (Phenagren)
4. Piperazine derivatives:
a) Cyclizine (Marezine)
b) Meclizine (Antivert)
c) Hydroxyzine (Atarax)
5. Ethylenediamine derivatives:
a) Tripelennamine (Pyrabenzamine Citrate)
B. Properties:
1. based on histamine structure
2. often short-lived -- multiple dosing -- piperazines can last longer (4-24hrs)
3. highly sedative lots of rings, not very polar ! cross BBB ! inhib H1 in hypothalamus
4. anti-cholinergic side fx (bind to muscarinic R ! potent antiemetic)
5. GI cramps (+ /++)
6. NOT anti-asthmatic (*asthmatics should not use these drugs)
7. do NOT inhibit Histamine release
C. Tx:
1. s/s - allergy & hayfever (rhinits & urticaria)
2. s/s - insect bites/ stings; contact flora
3. * motion sickness & vertigo specific to 1
st
gen.
a) CN VIII (Musc R) ! vomit center ! chemoreceptor trigger zone ! emesis
D. Side FX:
1. *sedation, decreased alertness, slowed rxn time; insomnia (? slide 41)
2. impaired cognition, confusion, dizziness
3. dystonia
4. potentiation of nasal congestion
II. Second Generation
A. Drugs --- *slide 31 compares
1. Piperidine derivatives
a) Loratadine (Claritin)
b) Terfenadine (Seldane)
(1) Taken off the market due to cardiotoxicity: when combod w/ macrolide
antibiotics or imidazole antifungals (hepatic metabolism) ! increase serum
Seldane ! bind heart K
+
channels ! severe arrhythmias
(2) Developed Fexofenadine (Allegra) active metabolite of Seldane.
(a) Excreted by kidney w/o hepatic metabolism ! avoid Rx interaxns
(b) all of the newer 2
nd
generation antiH also have much lower affinity
for K
+
channels!
c) Astemizole (Hismanal)
(1) same problems as Seldane!
2. Alkylamine derivatives
a) Acrivastine (Semprex)
b) Telemastine
3. Piperazine derivatives
a) Cetirizine (Zyrtec) [! appetite stimulation]
B. Properties:
1. Structures divergent, diff from Histamine
2. Longer duration of axn -- single/ multiple dosing; ! better compliance
3. limited or non-sedating structures more polar, limited ability to cross BBB
4. limited or no anti-cholinergic fx NOT antiemetic
5. Anti-asthmatic (++) not prescribed as antiasthmatics, but safe for asthmatics to use
6. NOT sedative; NOT anti-cholinergic; do NOT cause GI cramps; do NOT inhib H release
C. Tx:
1. s/s - allergy & hayfever (rhinits & urticaria)
2. s/s - insect bites/ stings; contact flora
D. Side FX:
1. mild cognitive disturbance
2. appetite stimulation Zyrtec
III. Other may consider in 2
nd
gen, but different
A. Desloratadine (Clarinex)
1. more specific
a) H1: 14-17x greater binding than Loratadine (Claritin)
b) Muscarinic: 15-50x lower affinity than for H1
2. rel long t
1/2
= 27 hrs
B. Olopatadine (Patanol)
1. *inhibits release of Histamine from mast cells the ONLY H1 blocker that does this.
2. more selective for H1 than other ocular anti-H: ketotifen, levocabastine, antazoline,
pheniramine
3. Tx: ocular rhinitis
C. Levocabastine (Livostin)
1. *more specific for H1 than anything else!
a) 1250x more potent than 1
st
gen (chlorpheniramine)
2. low side fx even w/ 40,000x effective dose; ocular application does not bother eyes;
nasal application ! fast release of s/s (minutes)
3. Tx: ocular rhinitis
D. Azelastine (Astelin)
1. inhibits histamine, leukotriene, and PAF activity
2. long t
1/2
3. Tx: rhinitis & hay fever
a) Can use in asthma pts!
b) * not used to treat asthma directly
4. Side FX:
a) Somnolence, bitter taste, nasal burning, sore throat, dry mouth
b) Teratogenic w/ high doses avoid in Pg
* Slide 41 good review of 1
st
gen vs. 2
nd
/3
rd
Names:
1
st
gen:
-amine
-zine except Cetirizine (Zyrtec) which is 2
nd
gen
Also: Deminhydrinate (Dramamine), Clemastine (Tavist), & Triprolidine (Actidil)
2
nd
gen & other:
-adine
-astine except Clemastine (Tavist) which is 1
st
gen
Remember Cetirizine (Zyrtec) is 2
nd
gen
Astemizole (Hismanal) too which is no good anyway b/c of cardiotoxicity w/ Rx interaxns
Asthma and COPD
Note: slides 5-9, 18, 33, 38 not included here
I. Adrenergic Agonists: Bronchodilators
A. Non-Specific: all have hyperT & cardiac fx
1. Epinephrine B
1
B
2
!
1
!
2
lasts 30-90min
2. Ephedrine - B
1
B
2
,
some !
3. Isoproterenol - B
1
B
2
B. B
2
specific fast: Metaproterenol, Albuterol, Terbutaline
1. relievers
2. quick onset + intermed dur (3-6hr)
C. B
2
specific slow: Salmeterol, Formoterol
1. preventers commonly for nighttime or exercise-induced asthma
2. slower onset + long dur (12+ hr)
D. FX:
1. B-agonists stim Adenylyl Cyclase ! "cAMP ! bronch dilation (pic slide 11)
2. Other:
a) some inhib of release of mediators from mast cells
b) some inhib of microvasc perm
c) slight promotion of mucociliary transport
E. FX:
1. nausea, vomiting, headache
2. #BP, "HR, cardiac arrhythmias
3. #PaO
2
! CNS toxic fx: agitation, convulsions, coma, respiratory & vasomotor
collapse
II. Cholinergic Antagonists: Bronchodilators
A. Atropine
B. Ipratropium
1. quarternary cpd poorly absorbed no systemic fx
C. FX of BOTH:
1. (cause competitive Ach-muscarinic blockade)
2. #airway smooth m constrxn
3. #mucous secretion
4. "B
2
-mediated bronchodilation
D. SIDE Fx:
1. on contact: pupillary dilation & cycloplegia (loss of fnxn of ciliary m)
NOTE: Combivent = Albuterol + Ipratropium (combined B
2
agonist + Muscarinic antag) ! greater
improvement in lung fnxn than either alone. --- Tx: COPD
III. Methylxanthines: Bronchodilators and Anti-Inflammatory
Aminophylline, Theophylline
A. Mech and 1
o
FX: - (pic slide 16)
1. inhibit PDE ! "cAMP ! bronchodilation
2. block muscle adenosine receptors ! bronchodilation
3. #release of mediators ! anti-inflamm
B. Other FX:
1. + chronotropic, + ionotropic
2. "CNS activity, gastric acid secretion, diaphragm m strength
3. weak diuretic effect
C. SIDE Fx:
1. 10-20ug/mL serum ! nausea, vomiting, nervousness, headache, insomnia
2. >20ug/mL serum ! vomiting, hypoK, hyperglycemia, tachycardia, arrhythmias,
tremor, neuromuscular irritability, seizures
IV. Cromolyns: Anti-Inflammatory Cromolyn, Nedocromil
A. FX:
1. alter Cl
-
channel activity
2. mast cells in lung inhib degranulation
3. eosinophils inhib inflamm response
4. airway nn inhibit cough
5. #bronchial hyperactivity assocd w/ exercise- and inhaled Agn-induced asthma
B. SIDE Fx:
1. (No systemic toxicity)
2. bad taste (inhaled Nedocromil)
3. irritation of trachea ! cough, bronchospasm after inhalation
4. Rarely: chest pain, restlessness, hypoT, arrhythmias, nausea, vomiting, CNS
depression, seizures, anorexia
V. Corticosteroids: Anti-Inflammatory
A. Inhaled Beclomethasone, Budesonide, Triamcinolone, Fluticasone
1. Side Fx:
a) Oropharyngeal candidiasis, hoarseness, dry mouth
b) #bone density in premenopausal women
c) #growth rate in children
B. Oral Prednisone, Prednisolone
1. Side Fx: (prolonged use)
a) Glc intolerance
b) "BP and weight
c) Bone demineralization
d) Cataracts
e) Immunosuppression
f) #growth in children
C. FX of BOTH:
1. DNA binding/activation ! "anti-inflamm proteins (this also ! side fx!)
2. Inhib transcription ! #prdxn of inflamm proteins (cytokines, enzymes, adhesion
molecules, etc)
3. #mucus secretion
4. #bronch hyperactivity
5. "fx of B
2
agonists
D. Cushingoid Syndrome:
1. weight gain: abdomen, moon face, buffalo hump
2. leg/arm muscle weakness and thinning
3. thin skin easily bruised, stretch marks
4. women: "acne, facial hair, #scalp hair
5. ruddy complexion, neck skin darkening (acanthosis)
6. child obesity, poor growth
7. high BP
NOTE: Advair = Fluticasone + Salmeterol (combined glucocorticoid + B
2
agonist)
BG on Luekotrienes (LT)
- (*slide 25 diagram)
- Memb Phospholipids ! (PLA
2
) ! AA ! (5-LO) ! LTA4 ! LTB4 & LTC4, LTD4,
LTE4 ! receptors
- LTB4 = neutrophil chemoattractant
- LTC4 & LTD4 mimic asthma symptoms bronch hyperreactivity, bronchocnstrxn,
mucosal edema, "mucus secretion
VI. Leukotriene Receptor Blockers: Anti-Inflammatory
A. Monteleukast side fx:
1. GI disorders, laryngitis, pharyngitis, nausea, otitis, sinusitis (2% freq of viral infxn;
more in pediatric pts)
2. NOT tumorigenic in rodents
B. Zafirleukast
1. GI disturbances, mild headache, "liver enzymes in some pts
2. cancer risk: high doses in rodents ! hepatic & bladder cancer, hisocytic
carcinoma
C. Mech of BOTH:
1. block LTD4 receptors
D. FX of BOTH (oppo. of axns of LTD4):
1. #bronch reactivity and bronchocnstrxn
2. #mucosal edema and hypersecretion
3. #airway inflamm
E. Tx: aspirin-induced asthma (do not give COX inhibitors to asthma pts)
VII. Leukotriene Syn Inhibitors: Anti-Inflammatory Zileuton
A. Mech: inhibits 5-lipoxygenase ! inhibits LT formation (LT-B,C,D,E-4)
B. FX:
1. #smooth m cntrxn
2. #blood vessel perm, #leukocyte migration to damaged area
C. SIDE Fx:
1. "hepatic enzymes reqs LFTs (liver fnxn tests)
2. metabd by and inhibits CYP1A2 interaxn w/ theophylline (& others)
VIII. Anti-IgE Monoclonal Aby: Anti-Inflammatory Omalizumab
A. Mech: binds IgE ! prevents IgE-mediated release of inflamm mediators ! decreases
allergic response.
B. FX:
1. #severity & freq of asthma attacks
2. #req of inhaled corticosteroids; improves long-term asthma control
C. SIDE Fx:
1. ***Anaphylaxis: difficulty breathing, closing of throat, swelling of face, lips, or
tongue, hives *do not give unless pt is under medical supervision*
2. Other: bruising, warmth, burning, stinging, itching, pain or inflamm @ injxn site;
sore throat, cold symptoms
3. Tumors reported in some pt's
D. Contraindications no known drug interaxns, but avoid concurrent agents w/o consulting
physician (like Rx, OTC, vitamins, herbal supplemements)
Stepwise Approach to Treatment:
Asthma vs. COPD
Contraindicated in
Airway Dz:
- sedatives
- BBs
- COX inhibs (aspirin)
- ACE inhibs
- Local anesthetics
COPD Tx Options:
- Smoking cessation w/ nicotine
replacement (Bupropion +/- patch)
- Bronchodilators: incl. Terbutaline,
Ipratropium, Formoterol, Salmeterol
- Combo of Bronchodilators
- Theophylline, Aminophylline
- Corticosteroids (poor response)
- O
2
Tx; mucolytics, KI, Guaifenesin,
N-acetylcysteine
- Surgery, lung vol rdxn, lung
transplant
Immunosuppressants
BG info slides 1-18, 40 not included.
NOTE: Slides 19, 48, 51 = muy tiles.
*trend to reduce exposure to calcineurin inhibitors & limit steroids, to use more specific Rx.
1. Polyclonal Abys (ATG = anti-thymocyte globulin)
Horse ATGAM adverse rxns in many pts
Rabbit rATG used much more than horse
BOTH:
! FX: NONSPECIFIC binding to T-cells ! lose 80-90% of T-cells; recover in 2 mos.
! Uses:
Bone marrow transplant
Organ transplant
Aplastic anemia
! * ~ TOLERANCE i.e. w/ repeated use develop neutralizing Abys to these Abys!
so used to initially "T-cells in induction.
! Side Fx:
Fever
Chills
hypoT
thrombocytopenia ("platelets)
2. Anti-CD52 Aby: Alemtuzumab
(humanized, mono-clonal)
CD52: esp on B & T (also on NK, monocytes, macros, platelets, male repro.)
FX:
! B & T most sensitive to lysis; cellular- or complement-mediated
! Affect esp. blood & bone marrow; less in spleen & lymph nodes
! Profound, long-term lymphopenia - *antibiotic prophylaxis necessary
Side Fx: Infusion rxns common (chills, rigors, nausea/vomiting)
3. Co-stimulatory Molecules: Muromonab CD3
= IV mouse anti-CD3 Aby
FX:
! On CD3
+
,4
+
,8
+
T-cells in peripheral blood & tissues
! Reversible; normalize w/in 1 week
*~TOLERANCE pts can develop human-mouse Abys; no good if titer> 1:1000
Side Fx:
! Acute hypersensitivity w/in minutes b/c can activate immune system do NOT use
this Rx again.
! @ 30-60 min, symptoms cytokine-mediated (a lot of symptoms slide 22)
! * minimize w/ high-dose steroid pretreatment
4. Calcineurin Inhibitors:
Cyclosporine
! Hirsutism/hypertrichosis
! Gingival hyperplasia
Tacrolimus 100x potency of Cyclosporine!
! Neurotoxicity
! CYP3A5 SNPs
Pimecrolimus
FX for all:
! Inhibit 1
st
phase of T-cell activation by blocking NFAT-P ! NFAT by calcineurin
Inhibit activation of T (IL-2, IF!) and B (IL-4)
Side Fx for all: Calcineurin is widely expressed ! affect many other tissues.
! *Renal toxicity even though it may be given for renal transplant!
due to renal vasocnstrxn
# serum creatinine, BUN, K
+
, MAP
difficult to distinguish from graft rejection (20% have both)
stop drug see contd deterioration in renal fnxn. specific fx slide 24.
! Mild-moderate hyperT: #symp tone; renal vasocnstrxn
! Various infxns
! 2
o
malignancies lymphomas & skin cancers
5. Corticosteroids: Methylprednisolone
Recall these have cytoplasmic receptor, then to nucleus for fx takes hours.
FX:
! Low Dose: " inflamm cytokine transcrip
! High Dose: # anti-inflamm gene transcrip
! T & B inhibited; "monocytes, "eosinophils, #neutrophils
Side Fx:
! CNS confusion; psychosis can happen in 2 wks, may be b/c of w/drawal
! HPA suppression (hypothalamic pituitary adrenal axis) in 5 days w/ high dose; long
Rx use ! 1 year recovery.
! Steroid withdrawal sydrome mood swings, arthralgias, etc
Must TAPER off dosing to prevent all of these!
! w/ prolonged dosing above physio levels: protein metab dysfnxn (myopathy,
osteoporosis, fractures, stunted growth), #infxn, Cushings, hyperglycemia, DM
aggravation, menstrual irreg, hypercholesterol, atherosclerosis, fat embolism,
thrombosis, thromboembolism, phlebitis, neuro fx (insomnia, depression, anxiety), skin
fx (atrophy, impaired healing) wow.
6. CD25 Inhibitors:
Daclizumab and Basiliximab
FX: Block IL-2R" (CD25) on activated T-cell surface
! Impairs immune response to Agn challenge
! * does NOT change lymphocyte # or phenotype just prevents upreg
Long elimination t
1/2
weeks
Side Fx: severe acute hypersensitivity; no increase in 2
o
malignancies
7. mTOR Inhibitors: Sirolimus
binds same thing as Tacrolimus (hence the name) BUT presents in different location
FX: inhibits mTOR (mammalian target of rapamycin)
! Inhibits 2
nd
phase of T-cell activation (signal transduction & clonal prolif) ! G
1
arrest
! Prevents B-cell differentiation into Aby-producing cells
"IgM, IgG, IgA
! Synergistic w/ Cyclosporine but Sirolimus itself does not affect calcineurin!
! Affects prolif of non-immune cells too, but no signif fx.
Side Fx:
! Hyperlipidemia monitor
! azotemia (=uremia), #serum creatinine, "GFR monitor kidney fnxn.
! Tumors
! [Others slide 31]
CYP3A4 & P-glycoprotein fx
8. Cell Cycle Disruptors:
Mycophenolate mofetil
! FX: inhibits IMPDH (inosine monoP deHase)
IMPDH: IMP ! GMP; necessary in all tissues in S phase, BUT lymphocytes
IMPDH is much more sucsceptible to MM.
Affects mostly T & B cells inhibits prolif b/c cannot make enough GMP
Advantages:
! Blocks 2
o
Aby responses of memory B cells
! Selective on lymphocyte prolif unlike Azathioprine, Methotrexate
! no chrom breaks
! Side Fx: typical (GI fx, infxns, tumors)
! Enterohepatic recirculation
! [also: has been shown to reduce anti-A, anti-B RBC Abys in ABO incompatible pts]
Azathioprine
! FX: an S phase-specific purine antagonist
Lymphocytes must rely on de-novo purine synthesis
Principal fx mediated by 6-thioguanine triphosphate inhibits RAC1 blocks
CD28 costimulation promotes apoptosis, esp of memory T cells
! Side Fx:
Pregnancy category D; also avoid in lactation
#risk skin cancer, esp w/ UV
! Other:
*many other side-paths that ! toxic/radical products
! pt w/ low TPMT ! increased toxic products, must decrease dose
e.g. on 5-aminosalicylates, which inhibit TPMT activity
! high TPMT, must increase dose
Allopurinol ! #Aza toxicity
Decreased Warfarin levels
! * Before/during use: TPMT test, Pg test, skin exams
Cyclophosphamide
! prodrug
! FX: lymphopenia, B > T (! greatest effect is suppression of humoral immunity)
! Side Fx:
Hematologic pancytopenia (leuko-, neutro-, thrombocyto-, anemia) is dose-limiting.
Acrolein (metabolite of cyclophosphamide) ! hemorrhagic cystitis
Tx w/ hydration & MESNA
Menstrual irreg/ amenorrhea; *infertility
infxns
Methotrexate
! FX: S-phase specific inhibition of cell cycle; inhibits tetrahydrofolate reductase
Cofactor depletion ! inhibits thymidylate & purine synth
Also undergoes polyglutamation ! MTX-PGs & DHFA-PGs ! inhibit thymidylate
synth & enzymes in purine synth
! Side Fx:
Rapidly dividing cells most sensitive ! serious toxicity & increased cytotoxicity
* GI: severe nausea & vomiting
! pretreat w/ 5HT3-antagonist & corticosteroid
Hematologic toxicity pancytopenia
Hepatotoxicity
Infxns; neurologic syndrome
* Teratogen
9. Co-stimulator Blockers:
Recall full T-cell activation reqs MHC-TCR stim & co-stim signal.
! lack of 2
o
signal ! apoptosis
Abatacept, Belatacept fusion protein
! FX: blocks engagement of CD28
"T-cell prolif and prdxn of cytokines (e.g. TNF", IF!, IL-2).
! Side Fx:
R.A.
Headache, dizziness, hyperT, GI
infxns
Efalizumab monoclonal Aby
! FX: binds T-cell LFA-1 "-subunit (CD11") - prevents binding to ICAM-1
"inflamm & rejection
Prevent binding of T-cell to endoth prevent T migration to inflamm sites
! CD11" also on B-cells, monocytes, neutros, NK, other may affect their
activation, adhesion & migration
Tx Psoriasis
! Side Fx:
Mild-moderate 1
st
dose rxn
Pain, flu-like S/S, arthralgia, asthenia, periph edema
URT infxns
2
o
malignancies skin, solid tumors
Alefacept fusion protein
! FX: binds to T-cell CD2 & simult to Ig receptors on cytotoxic T-cells.
* CD2 mostly on memory effector T-cells; nave T-cells largely unaffected!
Simult binding ! granzyme-mediated apoptosis
Tx Psoriasis
! Side Fx:
Lymphopenia 6-8 wks after start
2
o
malignancy skin
Serious infxns
Hypersensitivity rxns urticaria & angioedema
! (the most signif problem w/ these more specific protein drugs)
NSAIDS and DMARDS
NSAIDS
Salicylates Para-aminophenol derivatives COX-2
inhib
Acetylslicyclic acid (Aspirin) acetaminophen (Tylenol) celecoxib (Celebrex)
Indomethacin
Heteroaryl acetic-acid der. Propionic acid derivatives Enolic acid der
Ketorolac Ibuprofen (Advil, Motrin, Nuprin) piroxicam
Diclofenac Naproxen (Aleve, Naprosyn) meloxicam
Anthrotec Oxaprozin
Pathophys:
Osteoarthritis
Damage to cartilage w/ increased amts of ECM components of cartilage (PG and collagen)
Bone tissue under cartilage stiffens ! can cause osteocytes (outgrowths)
Cartilage debri and osteocytes in jt space cause pain and inflamm response
Rheumatoid Arthritis
Immune mediated
o Intense lymphocytic inflamm infiltrate in synovium
o Synovial macrophages and fibroblasts proliferate and secrete proteolytic enzyes
o Macro and lympho secrete cytok (IL-1 and TNF) ! cause array of cell responses
like cell death and release of lysosomal enzymes
o Later in disease, irrev cartilage damage, bony erosion
Symptoms (can last for many years)
o Redness of affected joint, some fever, tender, warm, swollen joints
o Symmetrical pattern, affected jts not nec weight bearing
o Fatigue, maybe fever, malaise
o Pain stiffness >30 mintes in morning/after long rest
Tx needs: decrease pain, maintain mobility, minimize disability, decrease inflamm, preserve
fxn
Use of NSAIDS: inflammation (anti-inflamm), pain (analgesic), fever (anti-pyretic)
PG synthesis
not stored in cells/tissues
COX-1 constitutively expressed; COX-2 inducible by cytokines, serum factors, GFs
**NSAIDS not inhibit lipoxygenase (Leukotrienes-chemotactic)
o Overproduction of Leukotrienes may be involved w/ aspirin hypersensitivity
PGI2 &PGE2 -
o potent vasodilation, potentiate vasc perm due to bradykinin,
o bronchodilation,
o stomach- protect GI mucosa from acid by decreasing gastric acid secretion,
increasing mucosal blood flow
PGE2
o Produce bone reabsorption! possible contribution to bone/jt damage assoc w/ RA
o Produce fever (leukocytes release polypeptide that acts on hypothal to release PGE)
o Produce pain ! potentiates effects of agents like bradykinin and histamine
PGF2a
o Stim uterine contractions (too much ! dysmenorrheal)
o Role in parturition! NSAIDS may delay onset of labor
o PGI2 maintain patent DA ! NSAIDS may lead premature closure in late pregs
TXA2
o Rapidly converted to inactive thromboxane B2
o Vasoconstriction
o Inducer of platelet aggregation
Leukotrienes- LT C4, D4, E4
o Bronchoconstriction
o Increase vasc perm and chemotactic
o Imp in inflamm and allergic rxns ! blocking cyclooxygenase path will reduce by
NOT eliminate inflamm
NSAIDS
Common Properties
-Mechanism of Action
NSAIDS inhibit enzymatic production of PGs via inhibition of COX-1 AND COX-2
Dont inhibit formation of Leukotrienes (diff enzyme- lipoxygenase)
Synth of LT from arachidonic acid may be accelerated by COX inh
-Therapeutic Activities of NSAIDS:
Analgesic effective against low-to-moderate pain, pain due inflamm well controlled
Antipyretic NSAIDS decrease body temp in febrile states
Antiinflammatory used to treat minor injuries, RA, OA, ankylosing spondylitis
Other Uses:
Closing of ductus arteriosus in neonates (PG maintain patency)
o Indomethacin and related agents will close DA in neonates when remained patent
Treat headache, muscle aches, dysmenorrheal
Protection from CV disease ! aspirin
Prevent colon cancer frequent use of aspirin/NSAIDS assoc w/ decrease risk colon cancer
Shared Side FX:
Most common: gastric or intestinal ulceration
o Caused by local irritation by orally administered drugs allows back diffusion of acid
into the gastric mucosa! inducing tissue damage
o Inhibition of biosynthesis of protective PGs (esp PGI2 and PGE2)
o All NSAIDS except acetaminophen tend cause GI Fx
" Coadminister PGE1 analog misoprostol to help prevent gastric ulceration
increase bleeding time due disturbances decreased formation in the platelets of TXA2
Prolongation of gestation or spontaneous labor
Changes in renal fxn: decrease renal BF and glomerular filtration in CHF, retain Na and H20
Intolerance of aspirin and most NSAIDS
Contraidications for NSAIDS
History of GI ulcers
Bleeding disorders or on anticoags
Pregnant patients - NSAIDS delay onset of labor o cause premature closing of DA in fetus
Hypersensitivity to aspirin - may also demonstrate hypers to other NSAIDS
Renal disorders
Salicylates and Aspirin
Mechanism of action
Aspirin covently modifies both COX-1 and COX-2, irreversibly inhibiting cyclooxygenase
activity ( a unique property to aspirin)
Aspirin acetylates COX enzymes (ALL other NSAIDS are reversible inhibitors)
Inhibits platelet aggregation for the life of the platelet
Platelets have no capacity for protein biosynthesis and cant regenerate the COX enzyme
Therapeutic Uses
Treat inflammation in rheumatoid and other arthritis, musculoskeletal injury, acute
rheum fev
Alleviate fever, pain and other signs of inflamm
Relieve types of pain like headache, arthritis, dysmenorrheal, neuralgia, myalgia
Large doses (3-6 g/day) can treat RA
Metabolism
Administered orally and absorbed rapidly in stomach and upper GI
Rapidly converted to salicyclic acid in liver
o Salicyclic acid a reversible inhibitor of COX enzymes
o Salicyclic acid reduces PG synthesis in vivo
Half life- 15 minutes, salicylate 2-3 hours @ low doses w/ 12 hours at anti-inflamm doses
Salicylates are subject to hepatic metab and renal excretion
Routes of admin:
Oral
Topical Asper Cream (15% trolamine salicylate), ICY hot (2% menthol, 29% methyl
salicyte) patches and sleeves
Side Fx:
GI Ulceration- misoprostol use in conjuction
Tinnitus (ringing) and hearing loss w/ higher doses
Hepatic injury over time, not acute
Reyes Syndrome in children infected w/ chicken pox or form of influenza virus
Asprin Induced asthma
Prolonged bleeding time single dose aspirin inhibit platetel COX for life of plately (8-11
days) in as little as 40 mg to produce this effect
o Decreased platelet agg useful in patients who have had their first MI
Contraindication
Bleeding disorders (hemophiliacs) or taking oral anti-coag
Para-aminophenol derivatives
Acetominophen (Tylenol)
Mechanism of Action
Weak inhibitor of COX 1 and 2
Also a strong inhibitor of COX-3 (expressed in the brain)- not sure of therapeutic actions
Therapeutic Actions
Analgesic and antipyretic effects similar to aspirin (acetaminophen present in over 200
generic and prescribed meds)
NOT!! A useful agent to treat inflammatory conditions
o Only WEAK antiinflamm FX (NOT an NSAID), not useful in RA
Useful for patients in whom aspirin is contraindicated
Metabolism
Oral admin, peak blood levels 30-60 min, half life ! 2 hours
Hepatic metabolism:
o Hepatotoxicity may occur after ingestion of single dose of 10-15 g w/ doses of 20-
25 g potentially fatal
o Acetaminophen normally converted in liver to acetaminophen-glucuronide or sulfate
o Also formed is highly reactive intermediate N-acetyl-para-benzoquinonimine which is
conjugated w/ glutathione (GSH)
o In overdose, hepatocellular levels of GSH are depleted and hepatic protein
modification occurs
o Hepatocytes susceptible to oxidant injury
Tx:
o Gastric lavage (has own risks)
o Measure serum drug levels > 4 hours after ingestion
o If >150 mcg/mL @ 4 hr OR 75 mcg/mL @ 8 hr ! give sulfhydryl compounds which
replenish hepatic stores of glutathione N-actelycysteine
o Most effective treatment begin <8-10 hours following ingestion (efficacy decrease)
Side Fx:
DO NOT produce GI irritation or bleeding at therapeutic doses
NO effects on platelets or excretion of uric acid
Hepatic toxicity (excess acetaminophen leading cause of hepatotoxicity whether accident
or intentional)
OTC Drugs: anacin, Excedrin (slides 41- 42)
Combo of NSAIDS and opioids for pain relief (also marketed w/ ibuprofen)
Propoxyphene/Acetominophen
o Propoxyphene (Darvon)- opioid analgesis
o Used for relief moderate pain
o Combo more effective than either alone
o 2 mechs of pain relief- central and peripheral
o Reduce opiate exposure
o Sedation, respiratory depression, habit forming
Oxycodone/acetaminophen (Percocet)
o Oxycodone (Oxycontin) opioid analgesis
Hydrocodone/acetaminophen (Vicodin)
Butalbital/aceta/caffeine (Fioricet)
Butalbital/aspirin/caffeine (Fiorinal)
Indomethacin
Mech of action: one of the more potent inhitors of COX enzymes
Therapeutic actions:
Antiiflammatory, analgesic, antipyretic
Useful to treat gout, arthritis
Side Fx:
GI irritation common
CNS effects: headache, dizziness, depression, esp w/ elderly patients
Renal dysfxn
CA in pregnancy
Heteroaryl Acetic Acid derivatives
Ketorolac
Potent analgesic but only moderately effective anti-inflam
o Use for short term (5 days or less) for severe pain
o Approved for parenteral admin (IM or orally)
Therapeutic uses:
Postoperative pain and inflamm following surgery (IM or oral)
Topical use for inflamm conditions of the eye (allergies)
Side Fx: similar other NSAIDS
Diclofenac
Inhibitor of COX, potency greater than inodmethacin, naproxen
Therapeutic uses: RA, OA
Side Fx:
GI effects
Not recommended pregs
Elevation of hepatic aminotransferase activies in 15% of patients (do liver tests)
Anthrotec (diclofenac and misoprotol)
Will provide gastric protection
Misoprostol PGE1 analog
Propionic Acid derivates
Ibuprofen, naproxen, oxaprozin, ketoprofen, flurbiprofen, fenoprofen
Pharm properties of all:
All COX inhibitors (reversible)
All alter platelet fxn and prolong bleeding time
All anti-inflamm, antipyretic, analgesic
All cause GI irritation, usually less severe than with aspirin
Ibuprofen (advil, motrin, nuprin)
Uses:
For RA, w/ daily dose 3200 mg/day
For mild/moderate pain (400 mg, 4-6 hours as needed)
Pharmacokinetics: oral admin, w/ half life 2 hours
Side fx:
GI intolerance, although less than other NSAIDS
Not to be used in pregnant women
Naproxen
half life 14 hours (2 x daily dosing)
Oxaprozin
antiinfalmm, analgesic, antipyretic
long half life 40 hours (single day dose)
Side Fx: GI
Enolic Acids
Piroxicam
anti-inflamm, analgesic, anit-pyretic
equiv aspirin, indomethacin, or naproxen
long t1/2 ! 50 hours (allow singe dosing)
Side Fx: GI and renal adverse rxns (high risk)
Drug: may reduce renal excretion of lithium
Meloxicam
more selective COX -2 (will also inhibit COX-1)
single dose day
Treat OA, RA
Side Fx:
o sim other NSAIDS (lower GI adverse rxns)
DRUG Interactions: Slide 59 PASTE
Selective COX-2 inhibitors
Celecoxib (Celebrex)
Mechanism of Action: selective COX-2 inhibitor/not affect COX-1
Therapeutic uses:
anti-inflamm, antipyretic, analgesic
OA, RA, acute pain, dysmenorrheal
Side Fx:
Potential CV probles
Less GI ulceration, but still possible
Dyspepsia, diarrhea, GI discomfort
Fewer antiplatelet effects
Fewer CV effects than Vioxx or Bextra
Inhibition induction of labor
Alterations renal function
Hypersensitivity rxns
Drug Interactions:
Sulfonamide (Bactrim, Septra D.S) ! Celebrex has sulfonamide side chain can cause
allergic symptoms
Coumadin potential for increased bleeding time
Interactions when administered w. drugs that inhibit P450 2C9 (that is the main way it is
metabolized in the liver) ! so would cause increased levels of celecoxib
Interactions w/ fluconazole and lithium
DMARDS
DMARDS
Methotrexate (Rheumatrex), Leflunomide, Sulfasalazine, Hydroxychloroquine, Gold
Etanercept, Infliximab, Adalimumab, Anakinra
Abatacept, Rituximab
Methotrexate
Mech of action: inhibitor of dihydrofolate reeducates (DHFR) and interferes w/ de novo purine
biosynth
Uses:
Very common for RA
o Low doses improve
o Therapeutic effects seen 4-6 wks
o Admin orally w/ folic acid
o Can be co-admin w/ glucocorticoids
High doses used in leukemias
Psoriasis
Immune suppressor (can be used in organ transplant)
o Decrease serum levels Igs (IgA, G, M)
o Inhibits activity pro-inflam cyto: (TNF, IL-1, IL-6)
CA/Side Fx:
Liver disease or alcohol use (signif)
Certain infections more common with immunosuppression
Renal excretion, so toxicity more likely in poor renal fxn
NSAIDS will decrease methotrexate clearance
Teratogenic
Co-admin w/ leflunomide can cause liver toxicity
Combo therapy:
Patients w/ refractory RA to methotrexate alone may be treated w/ methotrexate,
sulfalazine, and hydroxycholorquine
Addn of etanercept, infliximab, or anakinra may provide relief
Leflunomide
Mech: oral pyrimidine synthesis inhibitor
Tx: slow progression of mild RA
Side Fx:
Diarrhea, skin rash, hepatic toxicity
Teratogenic (not use pregs)
o Use cholestyramine (questram) to bind and eliminate leflunomide (can take 1-2 yrs to
clear)
Hydroxychloroquine
Anitmalarial
2
nd
line agent for mild RA
3-6 months onset of effects, well tolerated
Side FX:
Nausea, epigastric pain
Hemolysis w/ glucose -6- P DHG def
Retinal damage/vision monitored
Sulfasalazine
Prodrug; colonic bacteria release (5ASA ! therapeutic benefit)
Uses:
RA, mild to moderative ulcerative colitis, Crohns
Side Fx: GI disturbances, drop WBC (rare)
Gold (myochrysine)
Primary for RA
Produces gradual reduction of symptoms of inflamm in RA (suppresses, not cure)
Unknown mech of action
Administer IM (injectable more effective than oral)
SIDE FX:
Toxic effects involve skin, mucous membranes, usually mouth (15%)
Kidney fxn may be affected
Blood dyscrasias (severe)
High incidence of side effects
TNF Inhibitors
TNF
Role in pathology of RA ! stimulates macrophages which produce TNF IL-1, IL-6
TNF, Il-1, IL-6 induce chondrocytes, osteoclasts, and fibroblasts
Elevated TNF levels found in synovial fluid in RA patients
Goals of inhibitors:
Reduce circulating levels of TNF-a and block interaction of TNF-a with its receptor
Etanercept
Mech of action: dimeric fusion protein of ligand-binding portion of the human 75 TNF receptor
Produced in CHO cells
Action: to decrease TNF-a levels
Administration
Once (50 mg) or twice (25 mg) a week by Subcutaneous injection
Half life 3-4 days
Onset of actions 2-4 weeks
Therapeutic Uses:
For active RA in patients who have had inadequate response to other DMARDS
Can be used in comob w/ methotrexate, NSAIDS, or other agents
Infliximab
MEch of action: inhibits binding of TNF-a w/ its receptor
Administration:
IV infusion
Administerd 0 and 2 weeks (every other month)
Uses: RA and Crohns disease
Tables 82?
Adalimumab
Mech of action:
human monoclonal TNF-a antibody,
clears soluble and membrane bound TNF
Administration:
SC injection, every other week
Can be admin w/ other DMARDS or NSAIDS
Side Effects of TNF Inhibitors (etanercept, infliximab, adalimumab)
Injection site reactions common (usually mild w/ redness, itching, pain, swell)
Infections
Auto-Ab
Expensive compared to NSAIDS
Interleukin-1 Receptor Antagonists
Anakinra
Recombo, nonglycosylated form of human IL-1 receptor antag (one aa diff than IL-1
Mecho of action: blocks biologic activity of IL-1 by competitively inhibiting IL-1 binding to IL-1
type I receptor
Uses:
Moderately to severely active RA, in patients who have failed 1 or more DMARDS
Admin:
Used alone or in combo w/ DMARDS
Not used with TNF blocking agents
Admin SC daily
Combo therapy:
Side Fx: most commonly injection site reactions
Abatacept
Mech of action:
T-cell costim blocker
Has extracellular domain of CTLA4 conjugated w/ human IgG
CTLA4 binds CD28 on T cell and diminishes T cell response and inflamm cytokine secretion
(TNF)
Administration:
IV at 0,2,4 weeks and once a month
Onset of action 3 months
Rituximab
MEch of action: deplete B cells
Monoclonal Ab against CD20 on B cells! leads decrease cytokines and B/T interact
Administration:
2 IV infusions 2 weeks apart
Onset action 3 months for RA
Uses: in US for RA patients who fail resond to TNF antags
Corticosteroids/Glucocorticoids
Predinisolone or Triamcinolone
MEch of action:
Decreased numer circ lymphocytes, eosinophils, monocytes, basophils
Inhibit production of cytokines
Inhibit cytokines (IL 1,2,3,6) and TNF-a
Uses:
Anti-inflammm and immunosuppression
Provide relief until other, slower acting anti RA durgs (methotrexate) take effect
Side Fx:
Osteoporosis, Mood changes, Fragile skin, bruising, Fluid retention, Weight gain, muscle
weakness, worsening of diabetes, cataracts, increased risk of infection
1
Opioids
Assessment 6
1) Foundation
Mechanism of Action
o Stimulate endogenous opioid receptors ! analgesia
! Types of opioid receptors:
a. Mu (MOR) - "respiration, "GI activity
b. Delta GI regulation, autonomics
c. Kappa (KOR)- hallucinations
! Activated receptors
a. block ascending pain pathways (ie, spinothalamic tract)
b. activate descending pain inhibitory pathways (from peri-aqueductal
gray in midbrain
o
o
o
o
o
o
o
o
o
o
o
o
o
o CNS Actions of Opioids
! " Respiration " respiratory acidosis
a. eventual tolerance develops BUT narrow therap. window initially
! " cough
! miosis no tolerance develops
! nausea/vomiting
! euphoria
! sedation/drowsiness
! seizures/myoclonus high doses
! Endogenous Peptides:
large precursor protein
cleaved to form:
" Enkephalins
" Endorphins
" Dynorphin
2
o Peripheral Axns of Opioids
! Constipation no tolerance develops
! # histamine
a. cardiovascular " vasodilatioin
b. skin " urticaria
! contracts sphincter of bladder (acute) " urgency + retention
! " uterine muscle excitability " impair labor (unless intraspinal dose)
o Drug Interactions w/ opioids:
! Sedatives, Hypnotics, Alcohol, Barbiturates " "" respiration
! Sympathomimetics " ##analgesia
a. Opioids + Sympathomimetic = good combo for enhancd pain relief
! Anti-histamines " ##analgesia
! MAO-inhibitors " LETHAL with Meperidine
a. Toxic metabolite of Meperidine accumulates " seizures + death
b. Morphine and Fentanyl safe
o Pharmacokinetics
! Extensive 1
st
pass metabolism " parenteral dosing preferred
! Some are inactive pro-drugs and must be activated
a. Codeine, Heroin, LAAM
o Tolerance
! Inevitably develops with repeated dosing
a. Cellular changes at first dose
b. " analgesia after several days
! Cross-tolerance if acting on same receptor (may be incomplete)
o Dependence and Addiction
! Withdrawal Symptoms
a. 6-12hr restless, sweating, lacrimiation
b. 12-24hr irritable, tremor, dilated pupils
c. 24-72hr weak, depressed, nausea, vomiting, cramps, chills, flushes,
aches, pains, #HR, #BP, dehydration " can be fatal!
d. 7-10 days physical recovery but behavioral cravings persist
! Physical Dependence $ Addiction!
a. Addiction has a lot to do with brain re-wiring " cravings
b. Physical Dependence is a pain but most patients recover without
developing an addiction.
! Never undermedicate out of fear of causing abuse!
3
2) Opioid Receptor Agonists
Morphine*
o Axn: MOR agonist
! Active and has active metabolite: M-6-glucaronide = 100x potency
o Tx: dull, diffuse, continuous pain
! Half-life = 4hr
! Dosing: parenteral best; intrathecal, epidural; oral but 70% 1
st
pass metab.
o Side efx: tolerance, constipation, renally cleared
! Contraindicated in asthmatics b/c can # histamine " use Fentanyl instead
Codeine
o Axn: low affinity for MOR but 1
st
pass metab. 10% converted to Morphine
! Oral or parenteral
! Renal clearance
o Tx: mild analgesia
! cough suppressant (use only if not responsive to dextromethorphan)
Meperidine
o Active and has toxic metabolite: normeperidine = long ! life + seizure risk
! Thus Meperidine is bad for chronic usage.
o Benefits: no miosis, less seizures, " constipation, only 50% 1
st
pass metab.
o Side Efx:
! Renal clearance " watch out for toxic metabolite accumulation!
! Lethal if combined with MAO-inhibitors
! Contraindicated in children (toxicity)
Fentanyl - 80x potency than Morphine
o Transdermal patch for chronic pain
o Initial anesthesia IV b/c rapid onset + short duration
Methadone - Tx withdrawal
o slower onset, lower peak
o treats craving; may be used indefinitely
Propoxyphene
o 4hr duration
o renally cleared " toxic metabolite norproproxyphene " cardiac tocicity
Heroin - Equal efficacy as morphine; illegal
Others Briefly Mentioned
o MS Contin - Morphine with a longer half-life (8-12 hr)
o Hydromorphone oral and parenteral
o LAAM very long half-life
o Pemifentanil
o #$%&'(')*
4
3) Mixed Agonist/Antagonist
Pentazocine and Butorphanol
o Axn:
! Bind but do not activate MOR
! Bind and activate KOR
o Efx (compared to Morphine)
! Slight " analgesic affect (still OK for moderate pain)
! No constipation
! "" respiratory depression
! " abuse potential
4) Partial Agonist
Buprenorphine
o Axn: low MOR ativation
o Tx: addiction
! Suboxone = Buprenorphine + Naloxone
a. Supposed to take sublingual (naloxone ineffective)
b. If bad pt tries to inject, Naloxone will kill effects of Buprenorphine
o Side Efx: abstinence syndrome
5) Opioid Receptor Antagonist say No to opioids
Naloxone
o Axn: Bind but do not activate ORs (non-selective)
! IV only: rapid onset (1-2 min), short duration (1-2hr)
o Tx: opioid OD " respiratory depression
! Beware withdrawal syndrome " start with low dose!
Nalmefene tx opioid OD " longer duration (4hr)
Naltrexone
o Longer-er duration (24hr)
o Oral efficacy
o Tx Alcohol abuse: " craving and relapse
6) Other agents derived from Opiates
Loperamide
o No CNS axn b/c does not penetrate BBB
o Tx: diarrhea
! peripherally " GI motility, peristalsis, & secretion " # absorption time
Dextromethorphan
o Tx: cough suppressant
o Axn: non-opioid receptors
o Does NOT cause GI, respiratory ", or analgesia
5
7) Adjuvant agents for pain = drugs that # analgegsic effect of the opioid
o Ideal for # relief without # opioid side efx
Mild/Moderate Pain with milder opioids
o Acetaminophen + codeine
o Acetaminophen + propoxyphene (Darvocet)
o Aspirin + codeine
Moderate Pain
o Acetaminophen + hydrocodone (Lortab)
o Acetaminophen + oxycodone (Percocet)
o Aspirin + oxycodone
Other Adjuvants
o Clonidine
o Hydroxyzine
o Desipramine
If you want to treat Combine opioid with
o Bone Metastasis Pain NSAIDS or Calcitonin
o Neuropathic Pain tricyclic anti-depressants or anticonvulsants
(finicky dosing)
o Nerve Compression Corticosteroids
8) When do you use what?
Mild Pain Moderate Pain Severe Pain Addiction
NSAIDs
Propoxyphene
Opioid + NSAID + Adjv
Codeine
Hydrocodone
Oxycodone
Dihydrocodeine
Tramadol
Morphine
MS Contin
Fentanyl
Hydromorphone
Oxymorphone
Meperidine
Methadone (clinics)
Buprenorphine
Buprenorph + Naloxone
LAAM
1) Cyclosporine is effective in organ transplantation. The actions of this drug are to:
A) Activate natural killer (NK) cells
B) Block the tissue response to inflammatory mediators
C) Increase catabolism of Increase catabolism of IgG antibodies
*) Inhibit gene transcription of interleukins
E) Interfere with antigen recognition by T cells
1) Azathioprine
A) Binds to cytoplasmic immunophilin
B) Blocks formation of tetrahydrofolic acid
C) Is a precursor of cytarabine
*) Produces hematotoxicity and causes skin neoplasms
E) Is a metabolite of mercaptopurine
3) Your previously diagnosed asthma patient complains of feeling fatigued and unable to
always obtain a good nights sleep owing to awakening with breathlessness. The drug of
choice for this medical condition is:
A) terbutaline [Brethine]
B) epinephrine
C) albuterol [Proventil]
*) formoterol [Foradil]
E) metaproterenol [Alupe
4) Which of the following drugs is a nonselective parenteral bronchodilator that is
effective in treating bronchospasm?
A) Cromolyn [Intal]
B) Terbutaline
C) Zileuton [Zyflo]
*) Epinephrine
E) Prednisone
5) Which of the following is effective only as a prophylactic treatment by mast cell
stabilization?
A) Albuterol [Proventil]
B) Zafirlukast [Accolate]
*) Nedocromil [Tilade]
D) Prednisone
E) Terbutaline
6) The major clinical use of second-generation antihistamines is:
A) coughs and colds
B) insomnia
*) hay fever
D) motion sickness
7) A long distance truck driver complains of serious allergic rhinitis. Which of the
following would be the best antihistamine to prescribe for him?
A) Diphenhydramine [Benadryl]
*) Fexofenadine [Allegra]
C) Meclizine [Antivert]
D) Promethazine
E) Chlorpheniramine [Chlor-Trimeton]
8) Which of the following statements correctly describes H1 antihistamines and their
clinical utility?
A) Agents that are useful for allergic rhinitis also inhibit gastric acid secretion
B) Antihistamines are generally useful for the control of asthma
C) Antihistamines are the drugs of choice in treating anaphylaxis
*) Second-generation drugs have fewer anticholinergic effects than first-generation
agents
9) In the ER, the administration of large doses of terbutaline s.c. have failed to dilate the
airways of an asthmatic but instead caused tachycardia. In addition to the provision of
oxygen, what else should be done to manage the bronchoconstriction and restore the
activity of the beta-adrenergic drug?
A) Give inhaled cromolyn [Intal]
*) Give a parenteral corticosteroid
C) Give parenteral diphenhydramine
D) Switch to epinephrine
E) Switch to isoproterenol
10) Which of the following is NOT an effect of first generation antihistamines?
A) Reduction in urinary bladder tone
B) Local anesthetic effects if injected
C) Reduction in motion sickness
*) Increase in total peripheral resistance
E) Sedation
11) A 9 year-old boy suffers from severe asthma. The wheezing and other symptoms
have been inadequately controlled by the present treatment regimen. Combination
therapy with drugs chosen to target different mechanisms of action is indicated. Which of
the following would inhibit the increased parasympathetic bronchoconstrictor tone?
A) Cromolyn [Intal]
*) Ipratropium [Atrovent]
C) Nedocromil [Tilade]
D) Theophylline [Theo-Dur]
E) Zafirlukast [Accolate]
13) Olopatadine [Patanol] is unique among the second generation H1-antagonists in its
ability to:
A) block H1 and H3 histamine receptors with potency
*) block histamine release from mast cells
C) block H1 receptors only in the peripheral vasculature
D) be effective in blocking H1 receptors without causing sedation
E) effectively blunt acute asthmatic attacks
14) Through which of the following actions does morphine produce analgesia?
A) Activation of neuronal adenylyl cyclase
B) Increase pre-junctional neurotransmitter release
C) Reduction of post-junctional neuronal potassium conductance
*) Reduction in pre-junctional neuronal calcium conduction
15) Which of the following adverse effects of opiate therapy is least likely to become
tolerized upon chronic therapy?
A) Respiratory depression
B) Nausea and vomiting
C) Analgesia
D) Sedation
*) Constipation
16) Which of the following agents would produce salivation, lacrimation, urination,
defecation, depression and autonomic hyper-activity in an opioid addict?
A) Morphine
B) Oxycodone
C) Alfentanyl
*) Naloxone
E) Methadone
17) Meperidine and morphine are alike in many way, but meperidine does possess one
effect that is not observed with morphine or indeed the other opiates. That unique effect
is:
A) Constipation and paralytic ileus
B) Heightened pain perception (hyperalgesia)
C) Intense biliary tract spasm
*) Psychoses and possible seizures
E) Respiratory depression, apnea and ventilatory arrest
18) Which of the following opioid agonists is metabolized to a more potent analgesic?
A) Clonidine
*) Codeine
A) Meperidine
B) Naloxone
C Oxycodone
19) Which of the following agents possesses antipyretic and analgesic properties, BUT
NOT anti-inflammatory or anti-thrombotic effects?
*) Acetaminophen
B) Aspirin
C) Ibuprofen
D) Ketoprofen
E) Naproxen
20) Which of the following agents is contraindicated in infants suffering from chicken
pox or influenza virus?
A) Acetaminophen
*) Aspirin
C) Ibuprofen
D) Ketoprofen
E) Naproxen
21) Which of the following drugs produces its pharmacologic effects through the specific
inhibition of cyclooxygenase-2?
A) Amitryptyline
*) Celecoxib
C) Caffeine
D) Phenytoin
E) Ketoprofen
22) Ibuprofen, Naproxen and Indomethacin all reduce the production of:
A) cyclooxygenase (COX)
*) prostaglandins
C) arachidonic acid
D) phopholipase A2
23) With regard to inflammatory conditions, which of the following is specifically
inhibited by pharmacologic doses of glucocorticoids?
A) Cyclooxygenase-1 & 2
B) Histidine decarboxylase
C) 5-lipoxygenase
*) Phospholipase A2
E) Xanthine oxidase
24) Which of the following drugs would be administered to close the ductus arteriosus in
a premature infant suffering from blood gas and hemodynamic problems?
A) Histamine
B) Cimetidine
C) Diphenhydramine
*) Indomethacin
E) Prostaglandin E1 [alprostadil]
25) A 67 year-old woman with rheumatoid arthritis has been placed on high dose
indomethacin treatment by her physician. Which of the following additional drugs would
be most likely used to prevent drugs would be most likely used to prevent
gastroesophageal ulceration?
A) Celecoxib
B) Cimetidine
C) Diphenhydramine
*) Misoprostol
E) Sumatriptan
26) Aspirins inhibition of platelet aggregation arises from:
A) inhibiting thrombin and activating antithrombin III
B) blocking platelet aggregation by preventing bridging between glycoprotein between
glycoprotein IIb IIb/IIIa IIIa receptors on neighboring platelets
C) blocking platelet ADP receptors
*) inhibiting thromboxane A2 synthesis
E) stimulating fibrinogen synthesis and enhancing thrombolysis
27) Which of the following is a classical early sign of aspirin toxicity?
A) Constipation
B) Cough
C) Hypertension
D) Myopia
*) Tinnitus
28) Which of the following signs/symptoms would you expect to observe in a patient
suffering from a massive aspirin overdose?
A) Hypothermia
B) Metabolic alkalosis
C) Respiratory acidosis
*) Metabolic acidosis
E) Ventilatory depression
29) Concerning rheumatoid arthritis, which of the following correctly describes the
significant difference between methotrexate, gold salt and penicillamine versus aspirin or
indomethacin?
A) Activate immune/inflammatory responses
B) Are primary therapies for gout, gouty arthritis and hyperuricemia hyperuricemia
C) Are remarkably free of serious toxicities
D) Provide much quicker relief of arthritis signs and symptoms symptoms
*) Slow, stop and possibly reverse joint pathology in rheumatoid arthritis
Ancillary Drugs in Anesthesia
*note: all of these are covered elsewhere w/ other fnxns!
Pre-anesthetic medication:
A. psych & pharm prep; relieve anxiety, sedation, amnesia
B. dry secretions (bad w/ intubation), !autonomic responses (esp in kids); !gastric fluid, "gastric pH
C. antiemesis
D. !anesthetic reqs; facilitate indxn
E. prophylaxis against allergic rxn
F. there is no best drug or combo use tradition & experience
G. Timing is everything! as important as drug selection (b/c these are mostly oral/i.m)
1. oral 60-90min before OR
2. i.m. >20min, pref. 30-60min before OR
H. Children vs. Adults:
1. psych prep
2. more easily induced vagal reflex to airway manipulation
3. greater use of rectal route of admin in kids
4. intranasal drip, fentanyl lollipop, etc.
Typical Drug sequence
A. pre-op visit + interview
B. night before surgery:
1. BZ p.o.
C. 1-2 hr before surgery [this lecture tells us what these are all for]
1. BZ p.o., 150mL water
2. opioid i.m. for analgesia
3. Scopolamine for amnesia & sedation
4. Cimetidine &/or Metoclopramide p.o.
5. Glycopyrrolate or atropine i.m.
D. transfer to surgery:
1. 8-10 addl drugs; idea of balanced anesthesia
Sedation, amnesia, anxiolysis
A. Benzodiazepines: sedative effects, amnesic, calming; NO analgesia
1. act on GABA receptors in CNS to prolong binding of GABA
2. notice diff. durations of fx
B. Barbiturates: sedative effects, NO analgesia
1. act on GABA receptor in CNS to "its activity
2. !pre-op use b/c:
a) lower Tx index than BZs
b) tolerance & substance abuse
C. Butyrophenones: inhibit dopamine in CNS; NO analgesia alone
1. for anxiety that accomps psychoses; less effective against situational anxiety
2. Uses:
a) Innovar (Droperidol + Fentanyl) to # neurolept-analgesia
b) antiemesis
D. Phenothiazines: anti-dopamine/cholinergic/histamine fx; sedative; antiemetic
1. act on Dopamine, Cholinergic, and Histamine receptors in the CNS
2. side effect: !threshold for seizures do not use in pt w/ epilepsy
E. Antihistamine: bronchodilator, sedative, anxiolytic, AND analgesic
F. H
1
vs. H
2
Antagonists:
Notice only H
1
antagonists have:
- sedative effect
- cholinergic antag
useful to dry airways
useful for anti-tussive
(also to Tx extra-pyramidal s/s in Parkinsonism)
- anti-emesis
usu. to Tx motion sickness, not w/ anesth N/V
Analgesia
A. Opioids: act on ORs in CNS & spinal cord
1. Problems:
a) orthostatic hypoT, epigastric distress, constipation (anti-diarrheal), "sphincter tone
b) N/V via chemoreceptor trigger (Dopamine antag.) + delay of GI transit + "GI secretions
c) * morphine esp # N/V!
B. NSAIDs: COXII inhibitors; a large class some examples:
1. [alternatives to opioids for analgesia; avoid opioid side fx]
2. post-op may use PCA + opioid; progress to NSAID
3. inhibit PG syn, may # inhibition of platelet aggregation, inhibited ossification
a) Post-surgical bleeding outside GI tract: esp. surgery of GU, cardiac, oral cavity
(1) most other surgery NOT signifly impacted by NSAID-reduced hemostasis
b) Fracture healing: COXII inhibitors inhibit ossification
(1) clinical impact on bone healing unclear
(2) other risk factors: smoking, DM, periph aa occlusive dz
Aspiration pneumonitis
A. recall protective reflexes may be lost w/ anesthetic agents one of those reflexes protects the lungs from
aspiration of stomach contents, which can # Aspiration pneumonitis
B. factors that can influence risk: (DNTM!) abdominal tumor, drugs/EtOH, anesthesia, anxiety, cardiac arrest,
unconsciousness, diabetes, emergency abdominal surgery, very young age, hiatal hernia, intracranial P,
nasogastric tube, ascites, day surgery, seizures, trauma
C. Gastric pH
1. nl values: pH<2.5; >25mL
2. "pH & !volume # reduce incidence of aspiration pneumonitis if aspiration does occur
3. secretion of gastric acid impacted by many different receptors (gastrin, M
3
, H
2
, somatostatin, PG)
4. anticholinergic agents
5. H
2
receptor antagonists: more signif effect; no CNS sedation!
a) no consistent effect on volume that already exists
b) no effect on existing content pH only on prdxn of more acid
6. Side fx: headache; confusion, seizures, agitation in elderly(?)
7. Antacids: neutralize existing contents (no lag time waiting to change acid secretion)
a) particulate: [not on list!] may not be good to introduce particulates into stomach
b) non-particulate: (liquid)
D. Gastric Volume
1. Gastrokinetic agent: accel emptying
a) Fx:
(1) sensitizes upper GIT to Ach fx # "gastric emptying/peristalsis
(a) * only provided that Ach receptor system is working!
(b) Anticholinergics /narcotics will antag axn of Metoclopramide!
(2) central fx: Dopamine antag fx # sedation, lowers seizure threshold*
b) alters bioavail of oral drugs +/
2. Water: 150mL?? this stimulates stretch receptors to stim natural emptying
N/V Anti-emetics
A. myltiple stimuli of emesis:
[CTZ = chemo trigger zone]
B. w/ N
2
O or opiates in regimen, "N/V!
C. N/V esp troubling w/ day surgery b/c need to get rid of pt.
D. need for routine prophylaxis? no consensus
1. wide choice of agents
2. costs vary: cost-effectiveness?
E. Mech: Antagonists of: dopamine, histamine, Ach-muscarinic, serotonin receptors all acting on CTZ on CNS
1. serotonin (5-HT) receptor antagonists $$$ - reserved for extreme emesis e.g. w/ chemoTx
2. Dopamine antagonists - $$
(1) recall Metoclopramide also stims gastric emptying
b) Cholinergic antagonist:
(1) blocks pathways from inner ear
(2) recall very commonly for motion sickness prophylaxis
Prophylaxis of Allergic Rxn
A. many drugs & additives
B. often preTx w/ Cimetidine & Diphenhydramine (H
2
+ H
1
blocker) to prevent the consequences of the
rxn, not to prevent Histamine release
C. *not always effective
Prophylaxis of Infection
- avoid vancomycin resistance, not routine
A. antimicrobials # !risk infection, esp @ surgical site weigh against risk of rxn & producing resistant bac
1. esp in surgery of GU and GI
B. prophylaxis aimed @ most likely infxs agent, not every potential pathogen
C. Long pre-op hospitalization # "risk infxn for any pt; trend to day surgery
Anticholinergics
(antisialogogue effect = dry secretions)
A. pre-op use
B. lack specificity, use as needed
C. Uses:
1. Tx reflex bradycardia
2. block muscarinic fx of anticholinesterases (e.g. Neostigmine), which is used to reverse NMB,
and can # cholinergic stim @ M & N receptors
a) typical side fx of Neostigmine = N/V, diarrhea, miosis, hypersalivation, sinus bradycardia,
bronchospasm, & "bronch secretions
b) very common to give w/ Atropine when NMB reversal is done
3. drying of secretions recall some inhaled anesths can # "secretions
4. only Scopolamine # sedation & amnesia
D. Why might drugs be needed here to Tx reflex bradycardia?
Rapid Sequence Intubation: immed before surgery, initial O
2
to pt so
O
2
stays high while intubating. O
2
stays high several min. (graph)
Also pretreat highrisk pts before intubation with other drugs (chart).
High risk pts:
- those who cant tolerate increased ICP
- reactive airway dz
- CV dz
- children respond to intubation w/ profound bradycardia.
PreTx drugs are given & then wait 3 min to let drugs take effect before
proceeding w/ Succinylcholine.
IV push of sedative, then NMB (usu. Succinylcholine)
Post-anesthetic Period
A. ~25% pts have complications (%)
1. N/V (10)
2. resp depression - i.e. need airway support (7)
3. hypoT (3)
4. disrhythmia (2)
5. hyperT (1)
6. altered mental status (<1)
B. ~Risk factors:
1. ASA class II
2. 2-4 hr procedure
3. type of surgery: abdominal, orthopedic
4. hypothermia
5. smoking
C. Airway Support:
1. central resp depression seen w/ ANY anesthetic, but esp narcotics & NMBs
2. narcotic antags reverse resp depression of narcotics (e.g. Naloxone, Nalmefene)
a) small doses
b) t
1/2
problems if diff bet agonist & antag
c) in high doses, pain returns # symp stim # "HR & BP
3. NMBs failure to reverse # inadequate resp mm. fnxn; seen in
a) renal failure # inadeq excretion
b) use w/ gentamycin, neomycin, clindamycin or furosemide
c) hyperMg
2+
or hypothermia
D. Cardiac Support:
1. HypoT:
a) fluids
b) i.v. Dopamine 1-3ug/kg/min (! effect on heart + renal perfusion preservation)
c) Phenylephrine (!
1
agonist) or ephedrine (indirect causes presyn NE release)
(1) hypoT often seen w/ spinal or epidural anesthesia
2. HyperT:
a) often due to pain, hypercapnia, hypoxemia, hypervolemia
b) most resolved <4 hrs can use short-term drugs
(1) long-acting drugs are unnecessary
c) rapid-acting drugs e.g. Nitroprusside
(1) vasodilator, arterioles & venules
d) Trimethaphan (ganglion blocker) # !symp tone and # vasodilation
(1) prevents reflex effects on heart
E. Wake up!!
1. most common reason pt wont wake up = residual anesthetics & ancillary drugs
2. Reversal aimed @ most likely agent:
a) Narcotic or BZ antag likely give respective antagonist
b) Physostigmine can reverse fx of some other sedatives & inhaled anesths
c) discount NM agents if no signif resp depression
d) rarely Lidocaine OD can # unconsciousness
e) old age in itself does not # delayed awakening
F. Post-op N/V
1. no strong evidence implicates one anesth technique more, except:
a) Propofol anesthesia has lower incidence of NV even compared w/ others
b) N
2
O is assocd w/ N/V: evaluate its use if want low chance of N/V
G. Delerium & Cognitive Decline: (slides 31-32) DNTM
1. drugs & other factors very complex. Just know it may happen.
H. Drug-related Complications
1. more drugs are administered for a surgery than at any other time
a) 8-10 pre-op + 8-10 during surgery + any other meds pt is on
2. Admin errors
a) wrong drug!
b) inadvertent soln!
(1) most anesths relatively aq insoluble
(2) rely on pH (e.g. Thiopental pH 10) or formulation as salt of acid or base
(3) may req surfactant for solubility
(4) problems w/ extravasational or i.a. precipitation
3. incorrect site choice e.g. some # irritation if injected
4. incorrect admin rate
a) e.g. Histamine release w/ opioids when give too much too rapidly
5. allergic/immune rxns
6. drug-drug interaxn:
a) "chance w/ "drugs taken
b) other anesthetics, ancillary meds, longstanding meds unreld to surgery
7. genetic predisposition to unusual rxn
8. Peri-operative Drug Withdrawal (slide 36) - DNTM but know that it is often more imp to
continue w/ regular drug Tx and manage that w/in the combo than it is to suspend it for surgery.
9. Anaphylaxis in Anesthesia
a) 1/5000 1/25,000 incidence; mortality 3.4%
b) many anesths are known to assocd w/ Anaphylactic rxns:
(1) anesthetic indxn agents
(a) cremophor solubilized drugs, barbiturates, etomidate
(2) para-amino benzoic ester type local anesthetics
(3) muscle relaxants
(a) succinylcholine, gallamine, pancuronium, d-tubocurarine, metocurine,
atracurium
(4) Narcotics
(a) meperidine, morphine, fentanyl
(5) Others:
(a) antibiotics, bone cement, drug additives, radiocontrast dye
(b) protamine, blood products, colloid volume expanders
c) the problem is release of inflamm mediators, primarily Histamine, which # resp, CV, & cut. fx
d) Respiratory:
(1) cyanosis, wheezing, "peak airway P
(2) acute pulm edema, bronchospasm (23%)
e) CV:
(1) tachycardia, dysrhythmias, pulm hyperT
(2) !SVR, CV collapse (>68%)
(3) cardiac arrest (11%)
f) Cutaneous:
(1) urticaria, flushing
(2) perioral/ periorbital edema
g) Anaphylaxis Mgmt:
(1) Initial:
(a) stop drug admin, discont. anesthesia if possible difficult to det what is the
cause w/ so many drugs
(b) give O
2
(c) give Epi stim CV, vasoconstrict against hypoT
(d) i.v. volume expansion (e.g. isotonic crystalloid)
(2) Secondary:
(a) antihistamine e.g. diphenhydramine does not prevent H release, but
blocks H
1
receptors
(b) catecholamines e.g. Epi, norepi, isoproterenol
(c) aminophylline use w/ persistent bronchospasm # bronchodilation
(d) corticosteroids e.g. hydrocortisone, methylprednisolone antag
inflamm fx of LTs, PGs, kinins released by mast cells
(e) NaHCO
3
w/ acidosis of anaphylaxis
!"#$%&'(')*+ %)"-&.
/0 1234536789:;<96=
a) 1hree effecLlve rouLes: Loplcal, sysLemlc, or lnLraleslonal rouLes
l) 1oplcal drug peneLraLlon ls deLermlned by drug lonlzaLlon, hydrophlllclLy and molecular welghL.
(1) WaLer-soluble lons/polar molecules do noL peneLraLe well.
(2) urug upLake ls depend on a [] gradlenL across skln
b) 1he lnLacL (normal) skln blocks exLenslve drug absorpLlon buL ls more permeable
l) ln varlous body areas (scroLum, face, axllla, scalp)
ll) AL Lhe exLremes of age (preLerm lnfanLs and elderly)
c) ercuLaneous absorpLlon:
l) ^ln eczema (broken surface), j ln psorlasls (Lhlckened epldermal plaques)
d) urug may reslde ln Lhe dermal layers and acL as a naLural susLalned release" mechanlsm.
e) urug vehlcle lmp ln: drug dellvery, skln healLh (molsLurlzlng), provldlng sLable yeL easlly releasable
envlronmenL for acLlve lngredlenLs, ease of appllcaLlon/removal nonlrrlLaLlng, cosmeLlcally pleaslng
l) lmproved peneLraLlon ls achleved wlLh uMSC, propylene glycol & urea formulaLlons
>0 &7?963@ %:<9A97<96=
a) ackaged as mulLlple anLlbloLlcs aL well above Lhreshold dose ln Loplcal preparaLlons Lo provlde broad
coverage and delay Lhe emergence of drug reslsLance.
b) &BC
l) revenL clean wound lnfecLlon, early 1x of lnfecLed ermaLoses/wounds, prevenL SLaph
colonlzaLlon of nares, 1x Acne vulgarls, axlllary deodorlzaLlon
ll) 2
o
lnfecLed dermaLoses, dlaper ermaLlLls, oLlLls exLerna and lmpeLlglnlzed eczema
lll) used ln comblnaLlon w/ corLlcosLerold
60 17@D5DB9:
l) .9E; FBC lf sysLemlcally absorbed!neuroLoxlc and nephroLoxlc
(1) Avold ln open wounds or denuded skln
E0 );:<35969:
l) .9E; FBC lf sysLemlcally absorbed!neuroLoxlc, nephroLoxlc, and oLoLoxlc
ll) LlmlLed ln Loplcal usage Lo j emergence of reslsLance
;0 &;<436D6@9:;=
l) 8arely phoLoLoxlc
ll) ConLralndlcaLed ln pregnancy, renal and hepaLlc dz.
G0 &7?963@ %:<9HI:J3@ %J;:<=-well LoleraLed wlLh few problems: eg. ConLacL dermaLlLls
a) %K7@; E;49L3<9L;= MN3K7@;0
l) $;62C lnh 14 o-demeLhylase! j converL lanosLerol Lo ergosLerol ! j fungal cell wall lnLegrlLy
990 +@7<4953K7@;-C?3A4 lnLeracLlon
9990 "67:3K7@;
9L0 O;<767:3K7@;
L0 $967:3K7@;-lf used lnLravaglnally, j efflcacy of spermlcldal drugs
L90 'B967:3K7@;
L990 .I@67:3K7@;
A0 %@@D@359:;= MNH9:;0
l) $;62C lnh squalene monooxygenase (key enz ln sLerol synLh)!^squalene!jsLrucLural lnLegrlLy
990 -3H<9H9:;
9990 &;4A9:3H9:;
9L0 PI<;:3H9:;
60 &297634A353<;=
90 &7@:3H<3<; Q&9:36<9:R
E0 17@D;:;=
90 $;62C blnd Lo ergosLerol
990 -D=<3<9: Q$D67=<3<9:R
9990 %5?27<;4969: P QFI:J9K7:;R
e) Addlng azole w/ polyene does noL add effecL b/c Lhe Lwo mech work agalnsL each oLher
S0 '43@ %:<9HI:J3@ 3J;:<=-^ drug-drug lnLeracLlon due Lo ^ sysLemlc levels
a) )49=;7HI@L9: QFI@L969:R
l) $;62C dlsrupLs fungal mlLoLlc splndle sLrucLure! meLaphase arresL
(1) may also produce defecLlve unA ! lnh repllcaLlon
ll) ulLramlcronlzed" drug formulaLlons have greaLly lmproved bloavallablllLy.
lll) .9E; FBC
(1) Leukopenla and proLelnurla
(a) 8ouLlne hepaLlc, renal, hemaLopoleLlc monlLorlng advlsed).
(2) Slgnlf lnLeraxns due Lo changes ln meLabollsm
(a) j anLlcoagulanL effecL of +7I5349: & T34H349:, may manlfesL laLe (12 weeks)
(b) j conLracepLlve effecL wlLh oral agenLs
(c) j +D6@7=?749:; serum levels! j lmmunosuppresslon ! ^ organ re[ecLlon
(d) ^ "<23:7@ effecLs: Lachycardla, dlaphoresls, flushlng
b) &2; U%K7@;=V
l) $;62C see Loplcal azole
ll) O;<767:3K7@;Q-9K743@R-Cral/Loplcal/shampoo
(1) lnh LesLosLerone synLh ln hlgh []
(2) lnh C?2C19 & 3A4, 3, 7
lll) F@I67:3K7@; Q!9H@I63:R-Cral
(1) nC LesLosLerone effecL aL LherapeuLlc []
(2) lnh C?2C9
lv) *<4367:3K7@; Q.?743:7BR-Cral/parenLeral
(1) More poLenL Lhan keLoconazole
(2) lnh C?3A4, 3, 7
v) W74967:3K7@; QWF"-!R-Cral/parenLeral
(1) Lnhanced poLency and specLrum of acLlvlLy
(2) lnh C?286, 2C9, 2C19, 3A4
vl) ConLralndlcaLlons due Lo C?430 lnhlblLlons
(1) S1A1lnS: 3<74L3=<3<9:X 6;49L3=<3<9:X @7L3=<3<9:X =95L3=<3<9:
(a) SubsLanLlally ^ rlsk of myopaLhy, rhabdomyolysls, and acuLe renal fallure.
(l) lnLeraxn unllkely wlLh H@IL3=<3<9:, ?43L3=<3<9:X 47=IL3=<3<9: b/c noL C?3A4
meLabollzed?
(2) 8LnZCulAZLlnLS: 59E3K7@35X <493K7@35, 3@?43K7@35 and ;=<3K7@35
c) &;4A9:3H9:; M(359=9@0
l) .9E; FB: lnh C?2u6
(1) j converslon of codelne Lo morphlne
(2) ^ [Lheophylllne] (C?1A2 meLabollzed)-mech for lnLeraxn unknown
Y0 +74<967=<;479E=
a) lmmunomodulaLory, anLl-lnflammaLory, anLlprurlLlc (anLl-lLch), vasoconsLrlcLlve
b) $;62C lnduce llpocorLln ! j phosphollpase A2 acLlvlLy ! j breakdown of leukocyLe lysosomal
membranes and release arachldonlc acld ! j formaLlon and release of endogenous lnflammaLory
medlaLors: prosLaglandlns, klnlns, hlsLamlne, llposomal enzymes, Lhe complemenL sysLem.
60 &7?963@ J@I67674<9679E=
l) lf ^ cuLaneous blanchlng, Lhen ^ poLency
ll) oLenL /very poLenL drugs for acuLe conLrol, lesser poLency drug for malnLenance
lll) Plgh poLency drugs should nLvL8 used on face or lnLerLrlgenous areas (neck, groln) and only for
shorL perlods on Lrunk or exLremlLles
9L0 .9E; FBC
(1) Worsenlng and spread of Lhe lnfecLlon
(2) SLrlae & skln aLrophy locally wlLh glaucoma & caLaracLs lf Lhe drug ls used on eyellds
(3) Long-Lerm use!PlrsuLlsm acne and deplgmenLaLlon
(4) oLenL glucocorLlcosLerolds on face! 'perloral dermaLlLls'
(3) Long-Lerm sysLemlc exposure!Cushlngold feaLures
(6) Ampllfled by:
(a) occluslve dresslngs
(b) wlde area of appllcaLlon
(c) long duraLlon of exposure
(d) hlgh poLency drugs
(e) skln damage, lnflammaLlon, occluslon, or Lhln sLraLum corneum
(f) mosL commonly ln lnfanLs & young chlldren
v) ZDE47674<9=7:; 0.1, 0.3, 1, 2.3-mlld
vl) P;<35;<23=7:; L3@;43<; 0.023-moderaLe
vll) PIE;=7:9E; 0.023-poLenL
vlll) +@7A;<3=7@ ?47?97:3<; 0.03-very poLenL
d) *$ J@I67674<9679E=- acuLe 1x of LranslenL lllnesses or llfe-LhreaLenlng dermaLoses.
l) $;<2D@?4;E:9=7@7:; Q.7@IN$;E47@R-Large lv dally doses
(1) &BC reslsLanL pyoderma gangrenosum, organ-LhreaLenlng SLL & dermaLomyoslLls
e) *W may ! hypo-/hyper1, hyperglycemla, hypo-/hyperkalemla, anaphylaxls, acuLe psychosls and CPl
l) 1apered wlLhdrawal!psorlasls L may suffer pusLular flare
ll) WlLhdrawal of hlgh dose 1x may ! arLhralglas, myalglas & [olnL effuslons
6) *55I:7=I??4;==3:<=
a) +3@69:;I49: A@768;4=
l) &BC aLoplc dermaLlLls
ll) $;62C
(1) lnh calclneurln ! dehos of nl-A1-nuclear facLor of acLlvaLed LranscrlpLlon ! prevenL nl-
A1 from LranslocaLlng Lo Lhe nucleus !
(a) jregulaLe lnLerleukln (lL)-4 and Cu40 llgand ! lnh 8-cell acLlvaLlon
(b) jregulaLe lL-2 and lln-y ! lnh 1-cell acLlvaLlon
(2) May blnd Lo cell surface sLerold recepLors ! jregulaLe enLlre lnflammaLory cascade
lll) uo noL lnh collagen synLh or cause skln aLrophy
lv) noL as effecLlve as hlgh-poLency sLerolds
v) &3647@95I= Q147<7?96R[Loplcal/oral
(1) $;62C blnd Lo lk-blndlng proLeln ! lnh calclneurln
(2) .9E; FBC meLab by C?3A4 !mulLlple drug-drug lnLeracLlons
vl) 195;647@95I= Q"@9E;@R-Loplcal only
(1) .9E; FBC ulsulflram-llke rxn w/ alcohol has been reporLed.
vll) +D6@7=?749:; Q-;743@R-oral
(1) &B: severe, plaque-Lype psorlasls ln lmmuno-compeLenL paLlenLs who falled aL leasL one
sysLemlc Lherapy (e.g., uvA, reLlnolds, meLhoLrexaLe)
(a) Cr ln L for whom oLher sysLemlc Lheraples are conLralndlcaLed or cannoL be LoleraLed
(2) $;62C blnds Lo cyclophllln ! lnh calclneurln
(a) uoes noL affecL suppressor 1-cells or 1-cell lndependenL, Ab-medlaLed lmmunlLy
(3) .9E; FBC
(a) uose- and duraLlon-dependenL nephroLoxlclLy (^serum creaLlnlne and k
+
, ^arLerlal 8)
(l) due Lo renal vasoconsLrxn
(ll) ^ S creaLlnlne and 8un (azoLemla) may progress Lo lrreverslble renal dysfnxn
(lll) uncommon ln 1x for skln dz b/c low doses (max 3mg/kg) used
(b) Skln cancer-ln all lmmunosuppressanLs, Avold sun, uv8 or uvA Lherapy
vlll) *59\I957E Q%@E343R-Loplcal
(1) &B: Lemporary sympLomaLlc rellef of exLernal genlLal or perlanal warLs caused by Pv
(a) uoes noL ellmlnaLe Pv and warLs may reappear
(2) $;62C unknown
(a) Locally lnduces m8nA encodlng cyLoklnes llke lln-o
(b) Slgnlf j PvL1, m8nA and Pv unA
lx) %@;H36;?< Q%5;L9L;R[lv/lM fuslon proLeln
(1) &BC mod-severe chronlc plaque psorlasls
(2) $;62C modulaLes Cu2 recepLor medlaLed lmmune response and lnduces cellular-medlaLed
apopLosls of Cu2+ cells.
(3) .9E; FBC
(a) Lymphopenla
(b) 2 basal or squamous cell mallgnancles (due Lo lmmunosuppresslon)
(c) AnLl-alefacepL Ab formaLlon reporLed (3) buL noL correlaLed w/ lx or slde lx
x) "H3@9KI53A Q#3?<9L3R-monoclonal Ab
(1) &B: psorlasls
7) .63A9;= 3:E 1;E96I@7=9= &4;3<5;:<=
a) (9:E3:; Q.63A;:;R- y-hexachlorocyclohexane, 8x only llquld agenL
l) &B: edlculosls humanls caplLls (head llce), Lhlrus publs (crab llce), SarcopLes scablel (scables)
(1) Cnly used lf cannoL LoleraLe or falled 1
sL
llne 1x
ll) $;62: absorbed lnLo Lhe paraslLes and Lhelr ova
lll) .9E; FB:
(1) Selzures and deaLhs w/ prolonged appllcaLlon
(2) CnS sLlmulanL lf absorbed sysLemlcally ! adverse effecLs slmllar Lo uu1 (block CA8A axn)
b) +47<359<7: Q+47<7:R[cream or loLlon (10)
l) $;62C unknown
ll) Avold lnflamed skln or raw or weeplng skln surfaces
c) 1;45;<249: Q%6<969:, C1C as -9B]
l) &B of cholce for pedlculosls caplLls (head llce)
(1) Q"@959<;R-3 Loplcal cream: 1x of scables
ll) $;62: na
+
channel dlsrupLor ! paralysls and deaLh of Lhe paraslLes (llce, Llcks, fleas, mlLes)
lll) 8esldual ovlcldal acLlvlLy perslsLs afLer rlnslng
lv) 8eslsLance Lo 1;45;<249: has been documenLed
v) .9E; FBC none
(1) Mln percuLaneous absorpLlon
(2) lnacLlvaLed by esLer hydrolysls lf drug absorbed lnLo sysLem
d) $3@3<297: Q'L9E;R
l) &BC Llce reslsLanL Lo ;45;<249: or 1D4;<249:=
ll) $;62: lnh lnsecL aceLylchollnesLerase (AChL)
lll) .9E; FB:
(1) noL assoc w/ slgnlf Loplcal chollnerglc acLlvlLy
(2) Cral/pulmonary lngesLlon produces chollnerglc lx
(a) 1x w/ 3<47?9:; and ?43@9E7B95;
8) #;<9:79E=-derlvaLlves of vlLamln A
a) lnLracrlne and paracrlne medlaLors of cell dlfferenLlaLlon and prollferaLlon, apopLosls, reproducLlon
b) 8lnd Lo all reLlnold recepLors: reLlnold x recepLors (8x8s) vs. reLlnolc acld recepLors (8A8s)
l) 8oLh Lypes have o, , y subLypes, each has many lsoforms
(1) 8A8-o ! acuLe promyelocyLlc leukemla
(2) 8A8- ! squamous cell cancers
(1) 8A8-y ! reLlnold effecLs on mucocuLaneous Llssues and bone
c) &BC lnflammaLory dlsorders, hyperprollferaLlve dlsorders, skln mallgnancles, phoLo-aglng eLc.
l) 1oplcal appllcaLlon can normallze dlsordered skln keraLlnlzaLlon ln sebaceous folllcles and can
enhance Lhe peneLraLlon of oLher Loplcal agenLs
ll) Lsp effecLlve lf used w/ A;:K7D@ ?;47B9E;/Loplcal anLlbloLlcs
d) $;62 for derm
l) 8lnd Lo skln reLlnolc acld recepLors (8A8) & y and ^regulaLe skln prollferaLlon (^ 8nA
polymerase acLlvlLy, ^ CL2, ^ unA Lhymldlne lncorporaLlon) ! jepldermal cell coheslon,
^epldermal cell Lurnover
e) .9E; FBC
l) Slmllar Lo vlL A LoxlclLy: dry skln, nose bleeds, con[uncLlvlLls and halr loss
ll) ^ LumorlgenlclLy of uv llghL
lll) ^effecLs of phoLosenslLlzlng agenLs (all #;<9:79E=) ]I9:7@7:;= (parLlcularly .?34H@7B369:),
12;:7<293K9:;=, .I@H7:359E;=, .I@H7:D@I4;3=, &;<436D6@9:;=, and &293K9E; dlureLlcs
lv) C8AL 8L1lnCluS A8L C1Ln1 1L8A1CCLnS
(1) lx may perslsL for several years beyond cessaLlon of Lherapy
f) urug examples
l) 1
sL
gen: &4;<9:79: 4;<9:796 369E Q#;<9:N%R-oral/Loplcal, *=7<4;<9:79: Q%66I<3:;R-oral
ll) 2
nd
gen: %69<4;<9: Q.7493<3:;R-oral
lll) 3
rd
gen: %E3?3@;:; Q!9HH;49:RX &3K347<;:; Q&3K7436R-Loplcal
g) LaLer gen have more rlgld chemlcal sLrucLures ! more speclflc and less prone Lo produce adverse lx
9) P;:K7D@ ?;47B9E; - Loplcal
a) &B: !" $%&'( ln sebaceous folllcles and comedones (blackheads)
b) $;62C
l) 8elease free-radlcal C
2
specles ! oxldlze bacLerlal proLelns
ll) urylng and desquamaLlve (keraLolyLlc) effecL !j !" $%&'( levels, llplds, and free faLLy aclds ln Lhe
skln folllcle ! acne resoluLlon
c) .9E; FBC
l) xerosls, eryLhema, skln lrrlLaLlon, mlld sLlnglng
ll) hyslcal lncompaLlblllLles wlLh Loplcal reLlnolds & anLlbloLlcs ! ^ rlsk of skln lrrlLaLlon
lll) 1oplcal ZDE47\I9:7:; and P;:K7D@ ?;47B9E; on Lhe same skln ! LranslenL dark sLalnlng due Lo
oxldaLlon of ZDE47\I9:7:;
10) O;43<7@D<96=
a) .3@96D@96 %69E-Loplcal (3-6 = keraLolyLlc, >6 = desLrucLlve)
l) $;62C solublllzaLlon of cell surface proLelns.
ll) .9E; FBC
(1) Sallcyllsm: rlnglng ln ears, nausea/vomlLlng
(a) &BC hemodlalysls
(2) Allerglc rxn: urLlcarla, anaphylaxls, eryLhema mulLlforme
(3) ueaLh
lll) 147?D@;:; )@D67@[Loplcal, may be formulaLed w/ 6 .3@96D@96 369E
(1) LffecLlve keraLolyLlc agenL alone aL 40-70
(2) .9E; FBC allerglc conLacL dermaLlLls
11) &49627J;:96 ^ %:<9<49627J;:96 %J;:<= ME4IJ= 3HH;6<9:J 2394 J47_<20
a) $9:7B9E9@ Q#7J39:;R[Loplcal, relaLed Lo (7:9<;:-poLenL oral vasodllaLor
l) &BC halr loss
ll) $;62 for halr regrowLhC unknown
(1) lnh uL ! [cAM] ! Sm m conLrxn
(2) May acLlvaLe Lhe halr folllcle dlrecLly or sLlmulaLe folllcular mlcroclrculaLlon
(3) May also alLer local androgen meLabollsm
lll) .9E; FBC SysLemlc absorpLlon ! hypo1
(1) Mln percuLaneous absorpLlon
(2) Skln abraslon or lrrlLaLlons, eg. excorlaLlons, psorlasls, sunburn, ^sysLemlc absorpLlon
b) F9:3=<;49E; Q147?;693R[oral
l) &BC halr loss [ 1 mg/day, 8P [ 3 mg/day
ll) $;62C 8lock 3-alpha-dlhydroLesLosLerone (uP1) producLlon ! j scalp and serum [uP1]
(1) no lx on corLlsol, esLradlol, prolacLln, 1SP, Lhyroxlne, cholesLerol or 1P-axls
lll) .9E; FBC Low lncldence, malnly sexual dysfuncxn
(1) .3_ ?3@5;<<7 M.;4;:73 4;?;:=0 and H9:3=<;49E; have a slmllar pharmacologlc mech
(a) ConcurrenL use ls noL recommended
c) "H@74:9<29:; QW3:9\I3R-Loplcal
l) &B: unwanLed faclal halr ln women by j halr growLh
(1) used ln faclal and chln areas only, do noL apply around eyes or Lo mucous membranes
(2) noL a depllaLory (ablllLy Lo remove halr)
(3) arenLeral drug used by WPC Lo LreaL proLozoal lnfecLlons
ll) $;62 of reducLlon of unwanLed halrC unknown buL relaLed Lo skln CuC levels
(1) Speclflc lrreverslble lnhlblLor of ornlLhlne decarboxylase (CuC) !j polyamlnes, j nuclelc
acld synLh, j cell dlvlslon & dlfferenLlaLlon
lll) LlmlLed percuLaneous absorpLlon
12) 19J5;:<3<97: %J;:<=
a) &49N(I53-comblnaLlon of F@I769:7@7:;, ZDE47\I9:7:;, and &4;<9:79:
l) &B: 1emp rellef of faclal skln darkenlng by hormonal changes, pregnancy, oral conLracepLlve or
hormone replacemenL Lherapy
ll) F@I769:7@7:;: AnLl-lnflammaLory acLlons of corLlcosLerolds
lll) ZDE47\I9:7:;: lnh melanocyLe enzymaLlc oxldaLlon of Lyroslne Lo 3,4-dlhydroxyphenylalanlne
(uCA) ! j melanln formaLlon
(1) CLher melanocyLe processes are also lnhlblLed
lv) &4;<9:79:: ModulaLe skln growLh and plgmenLaLlon
(1) ^keraLlnocyLe sheddlng from Lhe reLlnold-LreaLed epldermls ! jepldermal melanln conLenL
b) $;<27B=3@;: Q`N5;<27BD?=743@;:abW%!"cR[oral/Loplcal
l) &BC
(1) vlLlllgo (smooLh whlLe spoLs on skln)
(2) w/ uvA for sympLomaLlc rellef of psorlasls
(3) w/ phoLopheresls for cuLaneous 1-cell lymphoma (mycosls fungoldes), alopecla areaLa,
lnflammaLory dermaLoses, eczema, and llchen planus.
ll) $;62 for vlLlllgo: sLlm melanocyLes ln halr folllcle
lll) .9E; FBC
(1) When acLlvaLed by uv radlaLlon (320-400 nm), lL ls a poLenL eryLhemogenlc, melanogenlc,
and cyLoLoxlc Lherapy
(a) Con[ugaLe and cross-llnk w/ unA
(2) Lxposure Lo uvA + meLhoxsalen ! cell ln[ury and lnflammaLlon
(3) uelayed eryLhema followed over several weeks by ^epldermal melanlzaLlon and Lhlckenlng
of Lhe sLraLum corneum
(4) eak phoLosenslLlvlLy wlLhln 1-2 hours, can perslsL for days
/G0 &7?963@ %:<9L943@ %J;:<=
30 %6D6@7L94 Qd7L943BRX W3@36D6@7L94 QW3@<4;BRX 1;:696@7L94 Q!;:3L94RX F35696@7L94 QF35L94R
l) &BC mlnor herpes slmplex vlrus lnfecLlons, herpes lablalls or herpes flbrllls
ll) Mln percuLaneous absorpLlon
lll) .9E; FBC
(1) lrrlLaLlon (mlld paln, sLlnglng)
(2) Alopecla
(3) LryLhema mulLlforme
(4) hoLosenslLlvlLy rash
(3) rurlLus
14) &7?963@ %:<929=<359:;=
a) &BC acuLe and chronlc urLlcarla, local allerglc rxn, llke lnsecL blLes.
b) +;<949K9:; QdD4<;6RX !;=@743<9E9:; Q+@349:;BRX (743<3E9:; Q%@3L;4<R
l) non-sedaLlng agenLs
ll) $;62C block effecLs of hlsLamlne on P1 recepLors, buL don'L affecL hlsLamlne release
/Y0 %@8D@3<9:J %J;:<= 3:E %:<95;<3A7@9<;=
a) Covered ln anLl-cancer lecLures
Inhalation Anesthesia
Definitions:
1. analgesia = relief of pain without intentional production of altered mental state
2. anxiolysis = decreased apprehension with no change in the level of awareness
3. conscious sedation = dose-dep; protective reflexes are maintained; have
independent maintenance of airway, oxygen sat., and ventilation; response to
physical or verbal stimuli
4. deep or unconscious sedation = profound effects with loss of 1 or more
components above
5. general anesthesia = sensory, mental, reflex, and motor blockade; concurrent
loss of all protective reflexes
Drug List: Currently Approved Agents
GASES: Nitrous Oxide
LIQUIDS: Halothane
Enflurane
Isoflurane
Desflurane
Sevoflurane
*Methoxyflurane
* now withdrawn due to the fact that 50% of the drug undergoes sig. metabolism
liberating F ions and transforming into a reactive metabolic intermediate that causes
cumulative impairment of RENAL FXN.
General Anesthetics:
Agents that can produce REVERSIBLE depression of neuronal fxn , loss
of ability to perceive pain, etc.
Depression of spontaneous ventilation or a drug-induced NM Blockade
often requires maintaining a patent airway and + pressure ventilation
DOSING = INHALATION and INTRAVENOUS preferred. WHY??
They offer a more immediate control over dose and t/f DOA. Oral drugs
offer no such control over depth of consciousness of pt.
*Father of Anesthesia = Crawford Long
Indicated use of chloroform in childbirth.
MECHANISM OF ACTION:
UNKNOWN!!! We still dont completely understand how they work.but we do
know a lot about what affects their onset of action, etc.
Myer-Overton Hypothesis: (see graph of MAC vs. Oil:Gas partition coefficient)
MAC = minimum alveolar concentration = the concentration of the drug
needed to produce immobilization to stimulus in 50% of patients; defines the
potency of inhaled agents lower the MAC, more potent the drug (ie less []
needed to see effect in 50% of pts.)
Oil:Gas Partition Coefficient = measure of a drugs lipid solubility; higher the
PC, the more lipid soluble the rx
Activity of agent/pharmacological potency is linked to LIPID
SOLUBILITY!!!
The more lipid soluble, the more easily it passes to the CNS and a lower dose is
t/f needed to produce unconsciousness.
LS is NOT the only component important because we can chemically alter Rxs to
make them more lipid soluble, but they have LESS pharmacological act.
Dose-Response Curves of Inhalation Anesthetics:
Normal Curve for a Rx and receptor system is SIGMOID, meaning as you
increase the dose, you increase the effect over a range of [].
Anesthetics drugs receptor interaction is still unknown.
IA curve is much steeper ie a slight increase in [] of the rx you go from no effect
to 100% effect quickly. Not a classical rx:r interaction.
*These agents dissolve within the lipid bilayer of membranes, affecting the lipid
components and the transmembrane ion channels. These ion channels are responsible for
neuronal activity and can be INHIBITED to get CNS depression.
*Agents can also dissolve in more specific areas of TM proteins, affecting the flexibility
of the protein and inhibiting it from carrying out its intended fxn.
Spinal Cord as Mediator of Immobility:
Immobility DOES NOT correlate to EEG act, rather to suppression of motor
neuron activity.
2 Distinct Pharmacological Effects of IA:
1. ENHANCE = inhibitory effectors in CNS
GABA
Glycine
2. INHIBIT = excitatory agents that arouse neuronal activity
Ach
Serotonin
Glutamate
How do both above conflicting actions occur in a single rxn???
1. Inhibitory Synapse: Normally, GABA release opens Cl channels to change
neuronal polarity and activity. Anesthetic agents bind to a site on a 5
transmembrane protein to cause changes with how GABA interacts with its
receptor system = ENHANCES GABA act.
2. Excitatory Synapse: Ach release opens Na channels on post-synaptic neuron
to stimulate it and increase neuronal act. In this rxn., the agent does not bind
to the TM protein itself, but IN the ion channel to prevent the easy passage of
Na = INHIBITING ACH POST-SYN NEURONAL ACT.
Recent Hypothesis = agents use a wide range of receptors, and they dont
necessarily act directly on the receptor system but also accessory proteins ie
PDZ that is responsible for internal signaling of receptor act. These proteins are
common to many post-synaptic receptor systems.
So, anesthetics have a DIRECT EFFECT on the anesthetic site of action, and an
INDIRECT EFFECT at sites where the agents can modulate anesthetic effect.
Guedel Stages of Anesthesia:
1. Delerium no surgery - ! RR, ! BP, irritation of tracheo-bronchial, mydriasis,
! muscle tone
2. Plane 1 dental/thoracic surgery
3. Plane 2 abdominal surgery
4. Plane 3 deep abd. Surgery
5. Plane 4 no surgery
6. Medullary Paralysis/Death
As ! depth and uptake of agent into CNS, there is a progressive " RR and
breathing fxn, "BP, loss of protective reflexes, papillary constriction then
dilation, and prolonged " muscle tone.
There is also different responsiveness of parameters in CNS to the agent being
used. Low [] of agents elicit no response in explicit memory and perceptive
awareness first. It then takes higher []s to inhibit movement and then even higher
to blunt autonomic axns. (See graph slide 23)
Structure of Volatile Agents:
Simple, diverse, containing HALOGENS!!!
Halogens contribute to organ toxicity so why include them in the Rx?? To "
flammability that is inherent in many of these agents.
Have an asymmetric C atom so exist in RACEMIC MIXTURES. It is thought that
one isomer has a higher potency than the other.
Absorption of Inhalation Agents:
In mixture of gases, the partial pressure or tension of a gas is proportional to its []
in the overall mixture.
ADMIXTURE = 70% nitrous oxide, 25% O2, 5% halothane
All partial pressures add up to atm. P = 760 mmHg.
Blood/Gas Partition of Halothane:
The inhaled agent must pass the alveolar wall once inhaled to get from the gas
into the blood, and from there then distributed into organ systems.
EX: of Halothane [] of 2 Vol. % in gas corresponding to a PP of 15.2 mmHg. It
must reach equilibrium between the alveolar and blood and for the PP to be the
same, the vol % has to be 4.6%. Need this level to get the PP equilibriated.
Halothane in the blood dissolves in the lipid components and is not free to be a
gas to pass biological membranes into the next system. Is sort of analogous to the
protein binding of other Rxs in blood. FREE Rx is only one that passes
membranes and exerts effects.
Comparison of Inhalation Agents: See slide 27 for actual #s and 33 for chart.
HALOTHANE = older Rx
side fxn: arrhythmias and hepatoxicity halothane hepatitis
most often occurs in obese females with previous exposure to
the Rx. It is converted into a reactive metabolic intermediate
that binds to liver proteins eliciting and immune response
ISOFLURANE = irritant, muscle relaxation
ENFLURANE = irritant, muscle relaxation, seizures only in susceptible ind.
SEVOFLURANE = newer Rx
DESFLURANE = newer Rx; irritant
NITROUS OXIDE = incomplete anesthetic given alone it cannot render the
pt. unconscious [note MAC value of 105!!!] VERY low potency but does add to
the overall admixture.
-low [] produce analgesia
- give alone, you have maintenance of protective reflexes
- TOXICITY??? teratogen in animals, ! risk spontaneous abortion?, myelin
sheath degeneration in infants due to chronic exposure, inhibit vitamin B12
synthase; med facilities have expensive N2O scavenging air systems to " ambient
air levels of N2O.
- SECOND GAS EFFECT = high vol. of N2O and relative insolubility = leads
to rapid uptake of gas from alveoli including any accompanying anesthetic agent
or O2 (ie. ! rate of uptake of volatile agent with coadminstration of N2O.)
- DIFFUSIONAL HYPOXIA = administer O2 to maintain oxygenation in
immediate post-anesthetic phase because large quantities exiting via exhalation
can " O2 tension in lungs
- SOLUBILITY 34xs that of nitrogen so in some spaces in the body can
displace it. Not a problem in places that have adequate compliance to
accommodate such as the bowels, etc. But an !in P in middle ear can rupture the
eardrum.
- WHY DO WE USE N2O??? cheaper!
1. Vapor sparing effect reduced requirement for expensive volatile agent
2. Reduced inspired volatile concentration - " repiratory depression and CV
effects, smoothens anestheic procedure (" consequences of other agents to spare
protective reflexes)
3. Mild analgesic properties
- USE of N2O Alone: produces drowsiness, dizziness, vertigo, dysphoria, panic,
amnesia, inappropriate laughing (laughing gas), parasthesias
- IMPORTANT 70-75% of overall admixture is N2O high volume, that is
relatively insoluble in blood and rapidly taken up across alveolar walls. BUT this
also " component of O2, and low levels of O2 have been shown to have adverse
effects on the patient on surgical wound infections and post-op recovery.
XENON = inert gas thought to be used eventually in anesthesia due to its
extremely low PC of blood:gas and rapid equilibration
[Isoflurane, Desflurane, and Sevoflurane are current agents of choice.]
Regardless of muscle relaxation or pain relieving qualitites, it is customary to
administer a neuromuscular blocking drug and an analgesic such as nitrous oxide
or an opiod.
*Lower MAC = more potent the drug
( #s for this value are not imp. Just recognize that they are all very potent Rxs a low %
in the admixture can elicit vast effects. EXCEPTION Nitrous Oxide see above)
*Partition Coefficient = low PC signifies that the Rx equilibrates rapidly between
compartments. Low blood:gas PC means that you after administer it, it renders the pt.
unconscious faster because it equilibriates faster. Halothane was once the prime inhaled
agent with a relatively low blood:gas PC, however, the newer, sevoflurane and
desflurane were created and have an even lower PC and are currently used. Newer drugs
are taken up faster into brain too and t/f have a more rapid onset of action.
*LIPOPHILICITY These agents are very lipophilic and would very much like to
distribute into fat but they are not delivered there very readily because fat has a " blood
supply. T/f no sig. accumulation here in short term administation.
*Most common route of exit from the body = EXHALATION.
Give mask inhaled blood brain leave via exhalation after anesthesia stopped.
Some % of drugs are metabolically coverted to metabolites and extreted.
OLD DRUGS = higher conversion
NEW DRUGS = lower conversion due to less time in the body
OVERALL TREND = New drugs (Sevo and Des) accumulate and equilibrate faster
than halothane. In addition, they are exhaled more rapidly than halothane allowing
the patient to recover consciousness quicker.
Factors Affecting Uptake: see graph slide 30
Dependent upon the blood supply to the organ.
Ex: brain has high blood supply so they rapidly accumulate here
Concentration of Inspired Gas = variable that anesthetist has direct control
over; this value is ! in the induction phase to ![] gradient, ! passage of drug to
body and speed up the process of unconsciousness, then " back down to
maintenance levels
Solubility - partition coefficient
Rate of blood flow to lungs
Cardiac Output
Tissue Distribution
*High blood flow tissues see a higher [] faster, and also are cleared of it faster. Fat, on the
other hand, has a less rapid uptake and tends to hang on to the agent for longer as well.
Respiratory Effects of Inhaled Agents:
! RR and "TV = regular rhythmic shallow breathing
" respiratory fxn with ! depth of consciousness
Reflex response to PaCO2 is blocked by all but nitrous oxide. So, as !PaCO2, no
stimulation of repiratory center to !RR and blow off excess CO2.
Result = !PaCO2 with ! depth unconsciousness.
Cardiovascular Depression by Inhaled Agents:
" in BP with ! depth of consciousness this is due to a " in CO overall trend,
not true for desflurane or isoflurane
overall effect is dep. On the individual patient and their concurrent pathology,
cardioactive drugs, and mechanical ventitlation
Could have Pharmacological effect by:
-direct depression
- "sympathetic outflow
- peripheral ganglion blockade
- " adrenal catecholamine release
- BR attenuation
- "Ca2+ flux
- vagal stimulation
Nitrous oxide has no significant CV effects when given alone. With ! in opioid,
nitrous oxide produces CV depression suggesting a sympathomimetic action.
i.v. Anesthetics
omitted: slides 38-40
I. Review slides 6-17 Key ideas:
A. Balanced anesthesia
B. formulation problems (b/c lipophilic in aq soln)
1. * except Methohexital & Ketamine (will dissolve in aqueous soln)
C. complex structures ! specific Rs (e.g. sites on GABA receptor; Ketamine on Glu
-
receptor)
D. * slide 12 pic of sites of axn
E. TMN signalling in wakefulness w/ Histamine "vs! VLPO signalling in non-REM sleep w/ GABA
F. * slide 15 graph of time course of i.v. anesthetics
1. * waking ! drug metabolized! just redistributed out of CNS to mm & skin, then fat
2. elim t
1/2
s are hrs for all, but wake up ~15-30min
G. majority of these drugs do NOT ! analgesia (pain relief), so must add opiate.
1. exception: Ketamine, a potent i.m. analgesic, acting on Glu
-
receptor
II. Induction Agents: Barbiturates Thiopental, Thiamylal, & Methohexital
A. Mech: prolong binding of GABA to the GABA receptor
1. * linear #in depression of CNS w/ # dose easier to die w/ OD than BZs
(i.e. a dose-dependent response see graph slide 11)
2. widespread depression of brain activity (rat images)
B. Side Fx:
1. NOT analgesic in low conc actually #sensation of pain
a) Must add Rx for analgesia here, opiates
2. * Dose-dep resp depression: ! death w/ OD
3. Can ! broncho- and laryngospasm @ beg while Rx admind
4. Usu no signif CV fx, but...
a) * caveat: Slide 19 other factors affect CV response to i.v. anesthetics
(1) ANS
(2) Rx e.g. BBs, vasodilators
(3) CV pathology
C. Other Problems:
1. Cerebral vasocnstrxn
2. Hypovolemia, BBs, central anti-hyperTs (e.g. Clonidine) all can affect CV stability w/ Rx
3. Enzyme indxn & tolerance barbiturates induce CYP450 & enlargement of liver due to protein syn
4. Non-aq formulation
5. Allergic rxn
6. Porphyria (demyelination of nn due to drug axn)
III. Induction Agents: Propofol
A. looks like skim milk
B. Mech:
1. enhance GABA activity + direct activation of GABA R
2. ALSO: inhib Glu
-
R
C. *Rapid compd to Thiopental
1. recovery is 10x faster
2. only Desflurane is faster
D. FX:
1. NO analgesia
2. lower doses ! conscious sedation
3. antiemetic very low incidence of N/V
4. resp & CV fx = barbiturates (i.e. well-tolerated)
5. * $intraocular P
6. some m. relaxation
a) but if req signif m relax for surgery, would use nm blockers
E. Problems:
1. pain on injection
The initiating drugs we talk about are relatively
well-tolerated i.e. no major side fx common, but
can have these bothersome side fx
Notice that:
Propofol very low incidenc of N/V.
Methohexital & Thiopental higher incidence
of N/V; may req addl antiemetic drugs.
IV. Induction Agents: Etomidate
A. Mech: enhances GABA axn
1. may displace endog inhibs of binding
B. FX:
1. CV & Resp depression: rare when used alone well tolerated
a) resp depression w/ inhalational agents or opioids
2. direct, potent cerebral vasoconstrictor
a) can be advantageous in some cases
C. Problems:
1. pain on injection
2. * inhib of steroidogenesis pts showed inhib of hypothal-pit-adrenal axis ! failure to thrive ! death
a) ACTH-unresponsive
b) NOT used in ICU!!
V. Ketamine
A. Mech: inhibits *Glu
-
*
(acts on Glu
-
receptor) [no direct effect on GABA]
1. diff pattern of depressed CNS activity (specific areas) vs. global fx of barbiturates (rat images)
B. useful IM when IV impractical
C. FX:
1. * potent analgesic
2. Symp stim activity:
a) #muscle tone
b) open eyes (may resemble catatonic state) eyes open, but unconscious & pain-free
c) #BP, #myocard O
2
consump, minimal resp depression
d) #intracranial P, #intraocular P may need to avoid according to circumstance
3. Intact pharyngeal/ laryngeal reflexes
4. * Potent bronchodilator Tx refractory bronchospasm; facilitates good resp fnxn in anesthesia
D. Side Fx:
1. Hallucinations (?)#or$ using other drugs too
a) young women w/ h/o vivid dreams most susceptible
b) may need to give pt short-acting BZ e.g. Midazolam (Versed) to control hallucinations
while pt emerging from unconsciousness
VI. Benzodiazepines Diazepam (Valium), Lorazepam, Midazolam (Versed)
A. Mech: bind & ! allosteric change in GABA receptor activity ! #activity of receptor w/ less GABA
(i.e. shift D-R curve to the left)
1. dose vs. CNS depression: max effect levels out graph @ increasing doses;
much more difficult to ! death w/ OD than barbiturates unless combo w/ EtOH.
B. FX:
1. NO analgesia (if need analgesia, use as part of drug combo.)
2. anticonvulsant 1
o
use
3. anterograde amnesia pt doesnt remember surgery or immed prior to surgery
4. use w/ opioids suggests sympathomimetic effect *slide 26 graph
a) has direct depressive CV effect but balanced by its symp stim ! no net CV effect
b) unless used w/ e.g. opiates, which block symp output ! reveal direct depressive CV fx
(1) recall: same thing happens w/ N
2
O + opiates
5. wide Tx safety margin
6. * Flumazenil specific antagonist for BZ given i.v. to rapidly antag negative fx of BZs; only when
necessary b/c has its own side fx
C. Problems:
1. Diazepam:
a) 1
o
drug & active metabolites ! prolonged sedation
b) * vs. Midazolam :
(1) water soluble
(2) very rapid distribution & metabolism short duration, rapid recovery
VII. Chloral Hydrate (Aquachlor) NOT on drug list! may be w/drawn from market soon.
A. oral/rectal alternative to BZs
B. ! Conscious Sedation: dental procedures & perioperative for antianxiety/sedation
C. Common side fx: vomiting, behavioral changes
1. resp depression possible, esp combod w/ EtOH
D. Habit forming: w/drawal ! seizures, delerium, & death (!) if untreated
E. (alc. dehyd.) ! Trichloroethanol active product (GABA)
1. trichloracetic acid suspected renal toxin & carcinogen
VIII. Opioids
A. MuORs in thalamic & spinal cord areas Mu is involved in dulling pain
1. most effective against dull, poorly localized pain
2. difficult to reliably predict reqd effective dose due to:
a) CO, age, smoking, alcohol
b) morphine conjugates have pharm activity
c) acute tolerance
B. Arguments for/against using opioids as sole anesthetic agent:
1. For:
a) pain relieved but pt arousable
b) NO direct effect on heart
c) maintain nl regional blood flow autoreg
d) $airway reflexes (facilitates intubation)
e) NOT toxic to organs no malignant hyperthermia
2. Against (it is not used alone now):
a) incomplete amnesia pt could remember events from surgery
b) CV instability
(1) bradycardia
(2) hypoT (direct) or hyperT (insufficient block of pain ! symp stim in surgery)
(3) addn of N
2
O! CV depression
c) #blood reqs
d) prolonged resp depression in ICU
e) histamine-induced rxns
C. Side Fx:
1. [Assocd w/ speed of injection, high conc, & presence of other cardioactive Rx]
2. Bradycardia via vagus or direct axn on SA/AV nodes
3. Hypotension 2
o
to histamine release
4. Hypertension:
a) perhaps due to activation of renin-angio system
b) intense pressor effect w/ Naloxone catecholamine release?
5. * Resp depression = major side effect (*see graph slide 33 worse w/ anesthetic + opioid)
a) $responsiveness of carotid bodies to rising PaCO
2
do not respond to #ventilation
b) breathing driven by hypoxic drive no O
2
admin!! will get rid of their only drive to breathe
c) reverse w/ opiate antagonists: Naloxone, Nelmefene
(1) * shorter t
1/2
than opiate agonist! so must monitor pt for recurrence of resp depression
d) entero-hepatic recirc of opioid
6. muslce rigidity wooden chest syndrome
7. #intracranial blood flow & P may need to avoid in pt
8. N/V, constipation, miosis
9. * opiate OD classic s/s = pinpoint pupils, $resp, coma
D. Relative narcotic potency:
1. Meperidine 0.1x morphine
2. Morphine is the standard @ 1 it is used most b/c cheaper
3. Alfentanyl 0.1-0.2x Fentanyl Fentanyl 75-125x Sufentanyl 5-10x Fentanyl
a) synthetic, more $$
E. Opioid Combinations:
1. Innovar ! neurolept-analgesia; combo of...
a) Droperidol ! state of indifference, anti-emetic, anti-convulsant
b) Fentanyl ! analgesia
c) useful for radiology, endoscopy, to change burn dressings
2. + N
2
O (65%) ! neurolept-anesthesia
a) pt is now unconscious + pain free + indifferent
b) diff in t
1/2
(D 3-6hr; F 1/2hr)
3. other: Atropine + Morphine/Meperidine
F. Remifentanil a new class of opioids
1. very short-acting
2. very potent analgesic activity
3. rapid onset & peak (~1min); short t
1/2
10-20min
a) effects not cumulative b/c so rapid
4. rapid recovery when discontinue admin but so does the analgesia! must consider & give other drug
for analgesia beforehand so it can take effect
G. Choosing an opioid:
1. Long-lasting analgesia: Morphine prototypical, very commonly used.
a) poor penetration of BBB (<1%)
b) pain relief correlates w/ CSF drug level
c) peak relief 15-30min
d) N/V is a classical side effect
2. Short-acting: Fentanyl
a) 20-min drug for 20-min procedure
b) more lipid soluble
c) onset < 30sec!
d) peak relief 2-3min
e) N/V rare unlike morphine!
IX. Pre-op Drug Sequence *skipped to talk a/b more w/ ancillary drugs
A. pre-op visit + interview
B. night before surgery:
1. BZ p.o.
C. 1-2 hr before surgery:
1. BZ p.o., 150mL water
2. opioid i.m. for analgesia
3. Scopolamine for amnesia & sedation
4. Cimetidine &/or Metoclopramide p.o.
5. Glycopyrrolate or atropine i.m.
D. transfer to surgery:
1. 8-10 addl drugs in anesthetic regimen
X. Malignant Hyperthermia
A. Mech:
1. causative agent ! intracell Ca
2+
release from SR (sarcoplasmic reticulum) !
#metabolic activity & mm cntrxn
B. Dx:
1. #2-3x in end tidal CO
2
2. total body rigidity (mm cntrxn)
3. unexpected tachycardia, tachypnea
4. resp & metab acidosis
5. can ! unexpected cardiac arrest
a) * primarily in young males w/ unDxd myopathy ! 50% mortality
C. Causative Agents:
1. Succinylcholine (nm blocker) now labeled NOT for routine use in children
2. other triggers:
a) ALL volatile anesthetic agents! incl. Desflurane, Sevoflurane
D. Safe Drugs:
1. N
2
O, local anesthetics, barbiturates, narcotics, tranquilizers, catecholamines, new muscle relaxants (e.g.
Mivacurium, Doxacurium)
E. Tx:
1. Dantrolene (not on list; will be discussed in Tx of mm spasticity) ! repackaging of Ca
2+
into SR
2. stop trigger agent; avoid CCBs (Ca
2+
channel blockers)
3. hyperventilate w/ O
2
4. correct hyperK
+
& acidosis
5. cool core temp
Local Anesthetics
Amide-type:
(infiltration/injection)
Lidocaine
Mepivacaine
Prilocaine
Bupivacaine
Levobupivacaine (discontd)
Ropivacaine
Ester-type:
(infiltration/injection)
Procaine
Chloroprocaine
Tetracaine
Cocaine
*Articaine amide & ester bonds
Topical use only:
Benzocaine (ester-type)
Dyclonine
Dibucaine (amide-type)
Pramoxine
EMLA
TAC
I. Local Anesthetics Reversible blockade
A. Ideal agent:
1. lipophilic and hydrophilic
2. low toxicity
3. short onset t.
4. completely reversible fx
5. active by topical, injection, & infiltration
B. Pros: simple, safe w/in dosing limits, cheap
C. Cons: unsuitability for some procedures, unpredictable surgery, prejudice (pt. & doc)
D. Mech:
1. block voltage-gated Na
+
channels ! prevent neuronal cndxn
a) increase refractory period of nerve; longer t for Na
+
to reconfig
b) most bind w/in channel
c) Benzocaine acts w/in memb ! memb swells ! occlusion of channel
2. NO effect on resting memb potential, only on depolarization
3. other explanation: Disruption of surface charge of memb by local anesthetics ! impairs nl depolar
mech this prob. adds to overall activity of these drugs
E. Differential Blockade i.e. does not block all nerve fibers to the same extent
1. fiber diameter smaller fibers blocked more easily
2. myelination must block 3 successive nodes of Ranvier to have complete blockade of cndxn, or
impulse just skips over
3. position in nerve bundle
4. nerve activity change in ion concs affect rel polarity of memb ! change frequency of Na
+
channel
activity and avail to bind a frequency-dependent blockade
a) "effect in hyperK
+
- in pts given Lidocaine for cardiac arrhythmias; hyperK
+
! "penetration
b/c Na
+
channels more freq avail
in less polarized memb ! heart
block ! death!
b) #effect in hyperCa
2+
- b/c memb
more polarized, less activity of
Na
+
channels to gain access
5. Drugs affect pain & temp before other
fnxns
a) pain in type A! & type C fibers
most sensitive to local anesth
II. Partitioning of local anesthetic:
A. local anesths are weak bases have 3
o
amine; most can be ionized: pH pK
a
= log (unionized/ionized)
1. all else equal, drugs w/ pKa closest to local pH ! fastest, strongest block!
B. *Ion pooling may occur in inflamed extraneural tissue (more acidic) w/ same amt drug applied, much less
effective & shorter duration (b/c the extraneural drug doesnt just stay there, and then more drug comes
back out)
C. Interneural space pH rel constant pH = 7
*recall: only the unionized form crosses the membrane.
III. Anatomical Aspects of Nerve Block:
A. Nerve bundle:
1. outer fibers go to proximal areas
2. inner fibers go to more distal areas
B. Drug applied outside nerve bundle
1. Anesthetic diffuses down conc gradient from outer to inner nn. block runs proximal ! distal
2. Diffusion, dispersion, dilution, absorption
3. Conc grad now reversed highest in center, lowest outer; drug diffuses again back out of n return
of sensation runs distal ! proximal
IV. Structure of Local Anesths: need to understand!
- 3
o
Amine: imp for axn of the drug
- Aromatic ring: gives lipophilicity to penetrate membs into n. fiber
- Intermediate portion two groups: ester & amide
* if drug name has i" anywhere before caine it is an Amide!
* if name does not have i before -caine it is an Ester!
- Changes of this baseline structure: DNTK them, but their purpose is to change pK
a
,
lipophilicity, dynamics of absorp into n. fiber & mech of fx
* Articaine has thiophene ring instead of benzene ring of the others
has both amide & ester linkage
rapidly metabd ! articainic acid (inactive); so very short-acting
V. Amide-type: Hepatic Metabolism tend to have longer duration
A. affected by:
1. CV status
2. liver dz, can ! accum & "systemic toxicity
3. toxemia of Pg
4. cimetidine
5. volatile anesthetics
6. BBs
B. elim as urinary metabolites
VI. Ester-type: NON-Hepatic Metabolism by plasma Pseudocholinesterase shorter duration
A. esterase affected by:
1. liver dz
2. Pg
3. chemoTx some #efficacy of pseudocholinesterase
4. atypical enzyme activity genetic - "systemic toxicity
B. elim as urinary metbolites
VII. Systemic Toxicities:
A. prepare for toxicity when:
1. approaching max dose
2. there is a potential for direct i.v. injections
B. Drug systematization:
note: some goes into blood stream rate of this systemization is crucial
C. 1
st
= avoidance!
D. ask pt to report s/s of minor toxicity:
1. ringing in ears
2. metallic taste
3. numbness of lips/tongue
4. if reported, stop injection immediately!
E. if no warning & high systemic conc,1
st
sign of toxicity = Seizures
1. Tx:
a) protect airway
b) admin Thiopental or Diazepam
c) Succinylcholine may be needed if severe protects airway & #metabolic acidosis
2. prompt Tx ! no long-term brain damage
3. delay ! potential permanent neuro deficit
F. CV less sensitive than CNS, but w/ rapid i.v. large dose ! Cardiac toxicity (ventric dysrhythmias or
fibrillations)
1. worst w/ Bupivacaine b/c bind Na
+
channel for long t
2. possible w/ all local anesths
3. Tx:
a) secure airway, 100% O
2
, artificial circ
b) EPI + defibrillate
c) Bretylium (antiarrhythmic) 5mg/kg to 30mg/kg
G. Vasoconstrictors: mimize drug systemization
1. w/o vasoconstrictor:
a) drug diffuses from site of application, to n. bundle & removed to blood
2. w/ vasoconstrictor:
a) local blood supply constricted - "chance for drug to go to n. bundle
b) "duration & intensity of blockade
VIII. Complications & Additives:
A. Epinephrine or Levonordefrin common (vasoconstrictors! "duration & intensity)
1. Toxic rxns may be evident:
a) in small children & w/ large doses for deep parenteral sedation
b) exaggerated responses w/ other sedating agents
2. Epinephrine interaxn possible w/:
a) BBs, TCAs (Imipramine), halothane (sensitizes myocard to Epi)
b) also w/ hyperT, heart block, cerebral vasc insufficiency, uncontrolled hyperthyroidism
3. Aspiration test: pull back on the barrel of the syringe to make sure you havent penetrated the vasc.
a) avoid vasc injxn of local anesth & Epi (signif CV fx)
b) but will not always show i.a. placement
B. Ester-type: more likely to ! allergy
1. rxn to para-aminobenzoic acid (metabolite) a well-known allergen
2. cross-sensitivity among, not between, esters & amides
C. Rxn to preservatives (sulphites)
1. w/ allergic patient, e.g. asthmatic, use preservative free!
a) 1% diphenhydramine 1:100,000 epi limited success b/c has 3
o
amine
D. True allergic rxns are rare (<1%)
1. rash, verticaria, laryngeal edema, bronchospasm
2. usu inadvertent i.a. admin
E. Most complications are psych, due to injection anxiety, not pharm:
1. pallor, unrest, sweating, fatigue, palpitations, N/V
2. Vasovagal reaction:
a) s/s sweating, faintness, pulse changes
b) may ! cerebral hypoxia, seizures, CV catastrophe
c) Tx is critical: place in recumbent position & give immed. supportive measures
IX. Vial Info:
A. drug conc given as %soln (for anesthetic)
1. e.g. Lidocaine Hydrochloride 2% = 2g/100mL = 2000mg/100mL, 20mg/mL
B. 1:X dilution (for vasoconstrictor)
1. e.g. Epinephrine 1:100000; 1:1 = 1g/mL; 1:1000 = 1mg/mL; 1:100000 = 10ug/mL
Onset slow/rapid:
- speed somewhat due to pK
a
, amt ionized at
physiological pH
- drugs w/ less non-ionized form have slower onset b/c
conc of avail unionized drug is reduced (e.g.
Bupivacaine)
Potency
- all based on Procaine (1)
- note those similar & much more potent
Duration short/intermed/long:
- long based partly on kinetics of binding to Na
+
channel
R i.e. bind and inactivate it for a longer t
DNTM these #s, but know drugs are sepd according to
onset t, potency, & duration of axn
note long-acting drugs clinically important
X. Common Ester Anesthetics:
A. Cocaine:
1. topical use only ENT
2. Fx: potent vasocnstrxn only local anesth that does this
3. Side fx:
a) w/ chronic sniffing, vasoconstrict ! ischemia & gangrene in nasal passages
b) potentiates cardiac arrhythmias, esp w/ Epi present
B. Procaine:
1. slow onset, short duration preferrable in some situations
2. this is the standard to measure the others potency
C. Chloroprocaine
1. short plasma t
1/2
2. this minimizes fetal exposure in OB
D. Tetracaine
1. long axn; slow metab
2. very potent
3. potentially very toxic due to long blockade & "potency
XI. Common Amide Anesthetics:
A. Lidocaine:
1. most commonly used local anesthetic
2. more rapid onset, longer duration & intensity vs. Procaine
B. Mepivacaine:
1. resembles axn of Lidocaine, but
2. no topical effect
C. Prilocaine
1. lower acute toxicity than Lidocaine, but
2. toxic metabolite (orthotoluidine) ! methemoglobinemia
a) Ferrous ! Ferric ion in Hb ! #O
2
carrying capacity of Hb ! low O
2
in pts predisposed, e.g.
w/ COPD
b) blue lips & nail beds
c) antidote: Methylene blue (or ascorbic acid): Ferric ! Ferrous
D. Bupivacaine & Ropivacaine
1. slow onset
2. long activity (up to 24hrs!) useful in post-op anesthesia around wound
3. more potent & more cardiotoxic than Lidocaine or Mepivacaine b/c of long binding
4. Ropivacaine has #d cardiotoxicity
XII. Topical Local Anesthetics
A. only topical due to poor aq solubility &/ localized toxicity w/ infiltration (irritate local tissue if injected)
1. some of these penetrate w/ low enough conc when used topically to not ! irritation
B. locations for use: skin & mucus membs (some exceptions); mouth, pharynx, larynx, trachea, esophagus,
urethra
C. Benzocaine
1. assocd w/ Methemoglobinemia (also seen w/ Prilocaine)
2. skin, NOT mucus membs
D. Dyclonine
1. skin, NOT mucus membs
E. Dibucaine
F. Pramoxine
G. EMLA (Eutectic Mixture of Local Anesthetics)
1. 2.5% Lidocaine + 2.5% Prilocaine, cream
2. apply, wrap, wait, wipe off ready for procedure
H. TAC (Topical Anesthesia thru Cut skin)
1. liquid applic to lacerations that req stitches
a) ineffective when applied to intact skin
b) rapidly absorbed thru mucus membs
2. widely used in pediatric emergency rooms
XIII. Regional Anesthesia: Infiltration
A. inject adjacent to nerve or nerve bundle
B. duration determines agent
1. recall: Epi prolongs fx of all drugs
C. area dictates dose
1. large surf A ! large volumes of dilute soln
a) e.g. Lidocaine - MTD 5mg/kg: MED 0.3-0.5% - so use 1 mL of 2% soln or 4 mL of 0.5% soln
D. Injection Technique: local anesthetics can be injected w/ little/no pain!
1. use smallest needle
2. inject subQ before raising wheal subQ tissue can stretch more than dermis
3. solns are acidic ! stinging pain on injection
a) neutralize w/ NaHCO
3
0.1-0.2 mEq/mL ! #pain & may improve onset
(1 mEq/ 10mL of 1.5%Lidocaine)
b) dont come like that b/c of drug stability! mix immed before use
4. body temp solns better tolerated
XIV. Regional Anesthesia: Tumescent
A. mostly commonly in plastic surgery liposuction
B. subQ perfusion of large volumes of saline w/ dilute local anesth + Epi (33-55mg/kg)
C. very good outcomes reported, but
1. comp to Lidocaine infiltration (above), conc much higher b/c then suctioned out w/ fat
2. but have seen plasma peaks ~8-12 hrs later
3. unexpected deaths in CA attributed to this technique
D. *addl local anesth by any route not recommended for 12-18hrs may get CNS & cardiotoxicity w/ too much
XV. Regional Anesthesia: i.v. Lidocaine
A. 1
o
for upper limb surgery
B. also short-duration foot procedures
C. tourniquet applied to occluded limb
1. entire limb loses sensation
2. tourniquet left on to allow absorp of anesth from the vasc
3. when removed, what is left goes systemic and is metabd
XVI. Regional Anesthesia: Central Nerve Block (Spinal or Epidural)
A. duration dep on: agent, dose, concurrent vasoconstrictor
B. hyper-, hypo-, or isobaric soln i.e. additives in vial to make soln more, less, or equally dense than CSF
1. allows migration of drug down/up after injection
C. + Epi: has "
2
axn ! inhibit Substance P release ! #pain transmission
D. + Clonidine: also has "
2
axn
E. application of drug can have complications
1. esp w/ higher than nl epidural dose must monitor closely
2. * Sympathetic Blockade w/ migration of drug up spinal cord:
a) Heart: symp innerv starts ~T12 chain ganglia; block will not stop heart (has parasymps too),
but ! #CO!
b) Resp ~same lower level as heart (T12) ! respiratory depression
c) Brain higher ! profound depression & death
XVII. Systemic Uses for Local Anesthetics low levels of i.v. Lidocaine:
A. [ineffective orally due to big 1
st
pass effect; given i.v. by divided bolus dose + infusion]
B. Suppress Grand Mal seizures
1. inhib hyper-excited neurons
C. #Intracranial P
1. cerebral vasocnstrxn w/ less hypoT than Barbiturates
D. Analgesia
1. for post-op pain
2. #need for opioids/ inhaled anesth
a) (*ceiling effect)
E. Suppress Cough
1. used peri-op
F. Antiarrhythmic: Tx Cardiac Dysrhythmias
G. Orally active congeners of Lidocaine (same mech but have oral bioavail):
1. Tocainide
2. Procainamide
3. Flecainide
H. other info:
a) Na
+
channels modulated @ 50-100uM
b) many other effects @ 1-5000x lower conc area of research
XVIII. Single Enantiomer Drugs:
A. BG: most syn drugs are 1:1 racemic mixtures; removal of inactive enantiomer ! improve Tx index; may
#side fx
B. Ropivacaine: pure S-enantiomer
Migraine
not included: slides 5-9
Acute Migraines: Principles
A. use only safe agents
B. choose based on severity of attack
1. mild-mod ! OTC
2. severe ! triptans or DHE most effective
C. use MTD before say that Tx does not work
D. w/ N/V, route of admin imp injection/nasal spray better than oral
E. treat when mild! ! greater efficacy
1. only if <2 headaches / wk
2. >3d / wk ! "risk analgesic overuse syndrome
[CSD = cortical spreading depression]
note:
- many different receptor systems involved
- targeting ! or H3 does NOT ! signif clinical fx
NSAIDs inhibit COX I & II ! #PG
Triptans activate:
5-HT
1B
! vasocnstrxn
5-HT
1D
! block Ca
2+
into neuron ! # release of
CGRP & SP
Acute Migraine Therapy
A. Analgesics: oral
1. NSAIDs single agent: Aspirin, ibuprofen, naproxen
a) Mech: inhib COX I & II ! #syn of pro-inflamm mediators
b) take sooner vs. later!
c) Side fx:
(1) chronic use ! irritate gastric mucosa ! potentiate migraine-assocd N/V
(2) * additive nephrotoxicity! monitor renal fnxn.
(a) inhib COX! #PGE
2
, PGI
2
! #renal blood flow & "ET-1
d) Drug interaxns:
(1) attenuate diuretics, BBs, ACEIs, vasodilators, central !
2
agonists, periph !
1
& Angio II
blockers
(2) adjust dose in pts on NSAIDs
(3) elderly at "d risk
2. NSAID combinations: Acetaminophen/Aspirin/Caffeine + Butalbital = Fioricet, Fiorinal
a) G6PD deficieny: imp w/ chronic high doses b/c aspirin ! hemolytic anemia in these pts
b) Butalbital (a barbiturate)
(1) Mech: thalamic GABA enhancement ! sedative-hypnotic fx
(2) Fx: drowsiness, sedation, #cerebral fnxn
(3) Side fx:
(a) * analgesic overuse syndrome strongly linked!
(b) enzyme inducer (CYP450)
(c) CNS & respiratory depression
(d) Porphyria (demyelination of nn due to drug axn)
(4) Contraindicated w/ ethanol & sedatives
c) Caffeine
(1) ! cerebral vasocnstrxn
(2) useful esp in caffeine w/drawal
(3) Side fx: potential CV interaxns (stimulant)
B. Triptans: oral; sooner is better!
1. Sumatriptan (oral, nasal, or S.C.) does not cross BBB, but active against migraine!?
a) may have axn outside CNS?
b) migraine pts may have compromised BBB! so maybe it does cross the BBB.
2. Zolmitriptan
3. Naratriptan ! inactive products, so has least problem w/ side fx
4. Rizatriptan
5. Newer analogs ! oral dosing, #onset t, "CNS penetration, "duration
6. Mech: triple axn! (also see pic above)
a) selective intracranial/extracerebral vasocnstrxn
b) inhibit trigeminal n. activation by vasoactive peptides
c) inhibit trigeminal cervical complex activation
d) note: 5-HT
1B
& 5-HT
1D
specific axns contrast w/ ergots! (chart slide 18)
(1) i.e. the K
i
values for 5-HT
1B
& 5-HT
1D
are much lower than w/ any other Rs
(2) fnxnl activity (50% efficacy) varies slightly by analog
7. Metabolism:
a) by MAO: Suma-, Zolmi-, & Riza- interaxns w/ MAOIs!
b) by CYP450: Nara- interaxns w/ anything that inhibits CYP450!
8. * Tx: first line for moderate/severe attacks & non-responders!
a) * max usage = 2d/wk
9. Side fx: [only signif problem: Side fx ! #d compliance]
a) sleepiness/tiredness (50%)
b) difficulty thinking (25%)
c) racing HR (25%)
d) dizziness (20%)
e) can ! coronary & periph vasospasm
(1) * contraindicated in: coronary or periph vasc dz, uncontrolled hyperT, or IBD
(ischemic bowel dz)
(2) vasospastic fx additive w/ ergot alkaloids do not give w/in 24 hrs:
2 triptans or triptan + ergot
C. Ergot alkaloids: parenteral (S.C., I.M., I.V.) or I.N.
1. Drugs:
a) Ergotamine
(1) moderate doses ! contrxn of smooth muscle (e.g. in small aa); used to
(a) control hemorrhage
(b) promote uterine cntrxn
(c) Tx migraine headaches!
(2) large doses ! paralyze motor n. ending of symp. NS (ergotism)
(a) s/s = mental disorientation, convulsions, m. cramps, dry gangrene of
extremities
b) Dihydroergotamine (DHE)
2. * Tx: limited to severe migraines use other less toxic Rx for milder migraines
3. Mech: agonist on 5-HT
1 & 2
, !
1 & 2
, D
2
(specific K
i
s slide 18)
4. Hepatic metabolism ! renal elimination
a) metab by CYP450 so, caution w/ impariment or concurrent CYP3A4 inhibitors
(1) SSRIs fluvoxamine
(2) HIV drugs saquinavir
(3) azoles intraconazole
5. Fx: Complex
a) central (5-HT) & peripheral (!) vasocnstrxn + amine reuptake inhibition
(1) * contraindicated w/ any vasospastic predisposing condition:
periph vasc dz, CAD, sepsis, MI, uncontrolled hyperT, etch
b) BP fx unpredictable
(1) capacitance >> resistance vessels
(2) dose-dependent fx
(3) ! antagonist w/ "" dose
6. Side fx:
a) many drug interaxns!
(1) do not use w/in 24hrs of triptans additive vasospastic fx
(2) do not use w/ sympathomimetic vasoconstrictors
(3) do not use w/ tobacco (vasoconstricts)
(4) do no use w/ Propranolol blocks vasodilation
(5) antagonizes: nitrates, BBs, CCBs
b) Catogory X! do not use in lactation! excreted in milk, affects infants CV/BP
c) chronic use ! valvular heart dz
D. Narcotics (Opiates): Butorphanol I.N.
1. Mech:
a) all 3 ORs (mu, delta, kappa) agonist/antagonist in spinal cord & higher CNS centers
b) hyperpolarizes endplate; #cAMP
(1) blocks release of SP from n. ending
2. Side fx:
a) Respiratory depression, bradycardia, histamine release, QT prolongation, constipation (recall:
no tolerance to this effect)
b) CYP3A4 substrate ! signif hepatic drug-drug interaxns
c) N/V common (as w/ all opiates)
(1) ! avail w/ promethazine (anti-emetic)
3. * special consideration: severe migraines do NOT need narcotics!
a) 80% of migraines ! allodynia (hypersensitivity to touch & other sensations)
Triptans are ineffective for this type of migraine.
b) >50% of ppl who go to ER for migraine receive a narcotic analgesic!
c) Ketorolac is an injectable NSAID
(1) effective & avoids narcotics (habit-forming)
(2) (also used in ancillary anesthesia for analgesia)
d) Narcotics should only be given as a last resort!
E. Migraine & Pregnancy
1. common, most in 1
st
trimester * when fetus @ greatest risk for abortifacent & teratogenic
drugs!!
a) Acetaminophen mainstay for 1
st
trimester attacks
b) Opioids may be added for migraines in later trimesters
2. DHE: contraindicated
3. other classes used only when unavoidable
4. chronic migraine is rare and most difficult to treat
F. Antiemetics: Metoclopramide, Prochlorperazine, Promethazine, Chlorpromazine I.V.
1. Emesis:
a) assocd w/ migraines &/ ergot use
2. Mech work in 1/3 ways:
a) block signals to & from vomit center
b) block gut receptors that trigger nausea in the brain
c) act directly on stomach ! "rate of emptying
3. Metoclopramide
a) cheapest, most common
b) Mech:
(1) central D
2
blockade
(2) "Ach release from post-gang fibers peripherally
(a) stimulates gastric emptying
c) Side fx:
(1) CNS: drowsiness, fatigue, confusion, restlessness
(2) "PL secretion (D
2
pituitary effect) ! gynecomastia
(3) oral drug interactions: e.g. "aspirin, tetracycline, lithium, & #digoxin
4. Prochlorperazine & Chlorpromazine
a) Mech:
(1) D
2
block in CTZ(chemoreceptor trigger zone) & adverse extrapyramidal effects
(2) Ach & !-adrenergic block
(a) sedation, muscle relaxation, hypoT, headache
b) Side fx:
(1) D
2
block ! tardive dyskinesia avoid in Parkinsonism
(2) !
2
block ! hypoT caution w/ CV dz & elderly
(3) Ach block ! glaucoma, urinary retention, prostatic hypertrophy
(4) additive fx w/ CNS drugs e.g. sedatives, anti-seizure, anticholinergic
(5) #seizure threshold in predisposed pts
5. Promethazine (Phenergan)
a) Mech:
(1) H
1
antag (GI, uterus, smooth m.)
(2) weak D
2
antag
(3) central Ach antag in CTZ
b) Side fx:
(1) * fatal respiratory depression <2 yoa!
(2) Ach antag ! glaucoma, urinary retention, prostatic hypertrophy
(3) D
2
antag ! drowsiness, "seizure risk, Parkinson-like symptoms
Chronic Preventive Migraine Therapy
Note: preventive Tx is controversial
when? how long? which drugs? always required? how many migraines per month indicate need?
A. Considerations:
1. recurrent migraine interfering w/ daily routine despite acute Tx
2. very frequent headaches w/ risk of rebound
3. acute meds: failure, contraindication, or signif side fx; overuse
4. special: hemiplegic migraine, risk of perm neuro injury
5. patient preference
B. How to procede:
C. Amitriptyline (a TCA)
1. Mech:
a) inhibit reuptake of NE & Serotonin
(1) metabolite Nortriptyline also inhibits NE reuptake
b) strong anti-cholinergic axn
2. Side fx typical anticholinergic:
a) aggressiveness, irritability, sedation
b) tachycardia, palpitations
c) cycloplegia
d) xerostomia, constipation, urinary retention
e) endocrine dysfnxn, weight gain
D. Divalproex (Depakote) & Valproic Acid (Depacon)
1. anticonvulsant; multiple mechs
a) inhibit voltage-gated Na
+
channels
b) #GABA metabolism/ reuptake
2. Side fx:
a) highly protein bound displacement can "[free drug] & toxicity
b) CYP2C9 substrate potential interaxns, e.g. warfarin, losartan, phenobarbital
c) * Teratogen
d) other: N/V, indigestion; pancreatitis or hepatotoxicity; sedation; derm rxns; "/#weight
E. BBs: Timolol & Propranolol
1. 50-70% effective to prevent migraine
2. Fx:
a) prevent aa dilation; inhibit renin secretion
b) block catecholamine-induced lipolysis ! #AA syn ! #PG prdxn
c) "O
2
delivery to tissues
3. Side Fx:
a) lethargy, GI upset, exercise intolerance
4. Contraindications:
a) asthma, AV block, sinus bradycardia, diabetes mellitus
F. Topiramate (Topamax)
1. 50% effective to prevent migraine
2. Antiepileptic agent blocks spread of seizures
3. Complex Mech
a) block voltage-gated Na
+
channels
b) enhance GABA axn
c) inhibit Glutamate axn
4. PKs:
a) long duration of action
b) narrow therapeutic window: #metab and/or #excretion ! "toxicity
c) limited hepatic metab (CYP450)
(1) interaxns w/ CYP450 inhibitors
d) renal excretion
(1) decreased renal fnxn ! "toxicity
G. Botox
1. Tx: spasticity, cervical dystonia, blepharospasm, strabismus, 1
o
hyperhydrosis
2. Speculated mech: direct #release of mediators or indirect #mm. activation of nn.
3. Admin: symmetrical injxn into glabellar frontalis & temporalis mm
4. Fx: #incidence & severity of all headaches
a) no adverse fx!! no vascular or systemic fx!!
b) But, high placebo rate
H. Cafergot (=Caffeine + Ergotamine) oral/ rectal
1. act synergystically
2. Mech:
a) additive cerebral vasocnstrxn? (both do this)
b) * enhanced GI absorp of ergotamine tartrate
(1) ! "absorp rate & peak plasma levels
3. PKs:
a) rectal bioavail 20x oral
b) T
max
~2 hrs post-oral admin
c) relief w/in 1-2 hrs of admin
Analgesic Overuse Syndrome
A. Fulfiling
Headache for >15 days/month (char depends on the drug)
+ headaches began/progressed in severity while taking meds
+ headache resolves or reverts to previous pattern w/in 2 mos after discontinuation of chronic drugs
B. Regular medication overuse >3 mos
1. Ergotamin, Triptans, Opioids, & combination NSAIDs >10 days/month
2. Simple analgesics (NSAIDs: aspirin, ibuprofen, naproxen) >15 days/month
3. Note:
a) mean duration of drug overuse can be years
b) monthly doses highest for least expensive agents analgesics
C. Trigeminovascular system sensitization
1. due to incomplete initial drug Tx, or
2. by direct drug-effects on modulatory pathways in CNS
D. drug-induced # in 5-HT levels ! 5-HT
2
receptor upregulation
E. Cellular adaptation changes to already aberrant internal signaling
F. Free radical damage in periaqueductal grey
1. * may be irreversible if extensive
G. Level of Association of drugs w/ analgesic overuse syndrome:
H. Three-Facet Approach:
1. Transition or bridging program (60-90% success)
a) 1
st
control migraines themselves w/ Ergotamine; prophylaxis w/ Propranolol
2. Biofeedback therapy
3. Prophylaxis to #incidence of migraines:
a) TCA (Amitriptyline), SSRI, BBs (Timolol, Propranolol), anti-epileptics (Divalproex,
Valproic acid, Topiramate), NSAIDs (Aspirin, Ibuprofen, Naproxen)
I. Overuse of medicine accounts for the majority of chronic dz headaches
1. need to raise physician awareness
2. avoid the syndrome in the 1
st
place!
Prior to surgery, a 37 year-old patient receives
ranitidine to:
A) Produce sedation
B) Reduce tracheobronchial secretions
C) Empty the stomach
D) Reduce vagal stimulation
E) Reduce stomach acid secretion
Which of the following produces vasospasm and is
contraindicated in a migraineur with uncontrolled
hypertension or coronary artery disease?
A) Butalbital
B) Valproic acid
C) Ibuprofen
D) Dihydroergotamine
E) Butorphanol
Anti-Cancer Agents Assessment 8
"
Principles of Cancer Cell Growth
Cancer is the clinical manifestation of carcinogenesis
Carcinogenesis is the dz
o Caused by dysregulation of the cell cycle (ex: multiple mutations)
o Oncogenes = encode proteins that tell the cell to divide
o Tumor Suppressor Genes = proteins that detect damage ! repair or apoptosis.
Cell-Kill Hypothesis (from Skippers Model)
o Chemo follows log-kill model: constant % cells killed regardless of tumor size
" First-order kinetics
" Ex: if there are 10
10
cells and chemo has a log-kill power of 4, how many
cells will be left? Answer: 10
6
o Skipper failed to take into account vascularization or drug resistance.
Growth # as size $ - a sigmoidal relationship (Gompertzian Model). Why? b/c tumor
outgrows blood and nutrient supply.
Vascularization: - Good: more effective drug delivery
- Bad: $ risk of metastasis
Drug Resistance: the major obstacle to successful cancer chemo. (Goldie-Coldman)
o Acquired via random mutation (NOT b/c of response to drug).
o Tx with combination chemotherapy to achieve cell-kill and avoid drug resistance
o Beware Narrow Therapeutic Window!
Treatment Options
o Best Tx is surgery remove it all. (Easier said than done)
o Systemic adjuvant or neoadjuvant chemo to de-bulk tumor before surgery.
o Systemic chemo if dz is disseminated (ex: leukemia, metastasis)
o Evolving Drug Choice
" Older drugs interact with DNA ! inhibit synthesis ! cell death
" Newer drugs target specific molecular targets
IMPORTANT GENERAL TOXICITIES OF ANTINEOPLASTIC CHEMOTHERAPY
o Myelosuppression ! thrombocytopenia
o Secondary Malignancies all that DNA damage $ risk for another tumor
o Nausea/Vomiting + Diarrhea
o Organ toxicity
o Tumor Lysis Syndrome lysis of tumor cells releases purine, K
+
, etc ! kidney
is overwhelmed ! uric acid & calcium phosphate deposition ! RENAL FAILURE
" Tx: Hydration
" Allopurinol blocks xanthine oxidase (cf gout lecture)
" Rasburicase $urate oxidase (converts uric acid ! soluble allatoin)
Anti-Cancer Agents Assessment 8
#
Alkylating Agents
What are Alkylating Agents?
o Have chlorethyl (alkyl) group that reaches out and binds DNA
o Usu @ N7-Guanine
o The binding causes miscoding and DNA strand breakage ! G
2
Block
" Thus, replicating cells are the most susceptible, like
Cancer cells
Bone Marrow
GI ! diarrhea
Hair ! allopecia
" Cells in earlier cell cycle stages may have time to repair damage.
O6-alkylguanine-DNA alkyltransferase (AGT) is an endogenous
enzyme that takes the alkyl grp off the DNA (suicide enzyme).
o General/Common Side Efx of Alkylating Agents
" N/V ! Tx with Ondansetron (serotonin antagonist)
" Lung fibrosis (progressive, may show up years later)
" Secondary Malignancies
" Teratogen
Nitrogen Mustards
o Cyclophosphamide
" MOA: chlorethyl group alkylates DNA
Prodrug coverted in liver + kidney to aldophosphamide (active)
Alternate use: immunosuppression (transplants + stubborn RA)
" Common Side Efx plus:
Renal Failure
Urotoicity ! severe hemorrhagic cystitis + bladder tumors
o Tx with Mesna conjugates toxic acrolein (metabolite)
o Ifosfamide
" Renal Failure
" Urotoxicity ! tx w/ Mensa
" CNS toxicity: altered mental status, ataxia, seizures, coma
o Mechlorethamide
Busulfan (an alkyl sulfonate)
o MOA: same as cyclophosphamide, just different structure
" Oral or IV ! hepatic metabolism
o Common Side Efx plus:
" Addison-Like efx: asthenia, hypotension, normal corticosteroid levels.
" Hepatic Toxicity ! veno-occlusive liver dz (see below)
Anti-Cancer Agents Assessment 8
$
Nitrosoureas only alkylators for brain tumors b/c lipophylic ! can cross BBB
o BCNU (Carmustine)
" 2 MOAs: (parenteral)
Alklates O6-Guanine ! DNA breakage
Isocyanate protein metabolite ! inhibits DNA repair
" Side Efx:
Injection site rxn
Pulmonary Fibrosis
CNS toxicities! 1) endocrine dysfunxn (hypothyroidism, etc)
2) seizures, dementia, encephalopathy
Hepatic Toxicity veno-occlusive dz
o $ alk.phosphatase, transaminase, + hyperbilirubenemia
b/c endothelial damage !
o Sx: abdominal pain, hepatomegaly, jaundice
o Treat with Defibrotide.
o CCNU (Lomustine)
" MOA: alklator
Thiotepa
o MOA: polyfunctional alkylater (IV, IVe, or IC)
" Rapidly metabolized in liver to TEPA ! loses an aziridine group !
forms interstrand DNA cross-links
o Side Efx:
" Neurotoxic symptoms: seizure, coma
" Injection site rxn
" Local bladder toxicities if IVe: dysuria, retention, hemorrhagic cystitis
Mitomycin C (antibiotic)
o MOA: bio-reductive alkylator
" Also generates free radicals
" Comes from Streptomyces
" Metabolically activated (! vulnerable to reistance)
o Side Efx: myelosupression, injection site rxn, hemolytic anemia
o Overall, this drugs effectiveness in recent trials has been disappointing. %
Anti-Cancer Agents Assessment 8
%
Drugs with Platinum (and Chloride atoms) that Alkylate
o Cisplatin
" MOA: alkylates intrastrand DNA links; 1 at N7-Guanine.
IV only; renal elimination
" Side Efx:
Ototoxic
Nephrotoxic ! tx with Amifostine.
N/V pretty bad ! tx with Ondansetron
Progressive neuropathy (motor + sensory) even after stop drug
Secondary Malignancy: AML (acute myeloid leukemia)
o Carboplatin
" MOA: same; also IV only
" Much less reactive than Cisplatin ! # severity of side efx
(myelosuppresion is still dose-limiting factor)
Dacarbazine
o MOA: methylates DNA at O6-Guanine. (does not use Cl
-
)!
" Metabolically activated; IV only
" Temozolomide is similar oral form
o Common Side Efx. (myelosuppression, N/V, etc)
Procarbazine
o MOA: methylates DNA at O6-Guanine
" Prodrug activated in liver (CYP)
" Resistance rapidly develops when used alone!
o Side Efx:
" Myelosuppression
" Weak MAO inhibitor ! beware drug-drug interaxns!!!!
" Disulfriam-like actions (pt feels malaise if they drink alcohol)
Review Alkylation Agents:
o Which two drugs can cause fatal liver toxicity?
o Which drugs have CNS side efx? (name at least 4)
o Which alkylator is not synthetic?
o Which drugs methylate instead of using chloride as the alkylator?
o Which drugs favor O6-Guanine instead of the N7 one? (name at least 3)
Anti-Cancer Agents Assessment 8
&
Anti-Metabolites
! mimic RNA + DNA (get inserted) but difference in structure foils transcription.
Folic Acid Analogs
o Methotrexate our DMARD friend
" MOA:
inhibits DHFR (which is necessary for folic acid to be able to
provide carbon groups for purine synthesis).
inhibits thymidylate synthase
When active drug enters cell, it gets polyglutamated
o This form is active, too
o Cant get out of cell
doesnt cross BBB
" Resistance: #uptake, $efflux, #polyglutamation
" Toxicity: & Bone marrow hemorrhage
o Renal Toxicity
o Pneumonitis
" Rescue with Leucovorin a reduced folate that doesnt need DHFR.
o Pemetrexed (Alimta)
" Strongly inhibits GART: glycinamide ribonucleotide formyltransferase
" Good to tx mesothelioma
o Trimetrexate (Neutrexin) - $BBB crossing, tx Pneumocystis carinii.
Pyrimidine Analogs (Cytosine, Thymine, & Uracil)
Mnemonic? Pyramid Cytings of Gems, Capes, and Fluorine?
o Fluorouracil (5-FU) IV only
" MOA: inhibits thymidylate synthase (TS)
! requires a triple complex: enzyme + reduced folate + FdUMP
! Leucovorin enhances the enzyme part ! $potency of 5-FU!
" Resistance: #5-FU activation; $ TS synthesis
" Toxicity:
Angina
Myelosuppression
Hand-Foot syndrome: erythema + desquamation
o Capecitabine oral precursor of 5-FU ! Hand-Foot more frequent
Anti-Cancer Agents Assessment 8
'
o Cytarabine
" MOA: interferes w/ base stacking ! inhibits chain elongation
Prodrug converted to ARA-CTP (active)
S-phase specific
" Resistance: #conversion to ARA-CTP or $ARA-UMP (inactive)
" Toxicity: potent myelosuppression
o Gemcitabine
" MOA: locks up cell division (similar to Cytarabine but not S-phase
specific)
" Toxicity: & myelosuppression
o *flu-like syndrome
o $liver transaminases
o interstitial pneumonitis
Purine Analogs and Friends (Guanine, Adenine)
o 6-Mercaptopurine (Purinethol) - oral
" MOA: ???
" Resistance: #HGPRT, $alkaline phosphatase, #uptake, $efflux, etc.
" Toxicity
Myelosuppression
$ hepatic enzymes ! jaundice
You MUST do genotyping to check for lack of TPMT! (slide 52,54)
DRUG INTERACTION: Allopurinol slows deactivation! Reduce
dose of Mercaptopurine.
o Thioguanine similar to 6-MP; no allopurinol conflict
o Pentostatin parenteral
" MOA: inhibits adenosine deaminase ! apoptosis
" Myelosuppression is dose-limiting.
o Cladribine and Fludarabine
" MOA: oral prodrugs metabolized by deoxycytidine kinase to active
triphosphate ! apoptosis
" Resistance: #deoxycytidine kinase activity
" Toxicity: myelosuppression, lingering immunosuppression (>1yr)
Anti-Cancer Agents Assessment 8
(
Natural Products (plant alkaloids and molds) (Slide 57ff)
! do not assume that similar drug structure = same spectrum of activity.
! a lot of these guys have a huge structure ! good for taking up space
Vinca Alkaloids
o Vinblastine - IV
" MOA: bind "-tubulin, preventing polymerization
! metaphase arrest
! hepatic metabolism
" Resistance: P-glycoprotein or binding site of "-tubulin mutation
" Toxicity:
Neurotoxicity (neural microtobules): numbness, #reflexes,
weakness ! $dose has seizures + irreversible coma
Alopecia and local cellulitis
o Vincristine and Vinorelbine
" MOA: same as Vinblastine
" Toxicity: Leukopenia, alopecia, local cellulitis
Camptothecin analogs The Happy Tree
o Topotecan
" MOA: bind and inhibit Topoisomerase 1 ! strand breakage
Hepatic metabolism via glucaronidation; renal elimination.
" Resistance: $ eflux, change in Topo-1 expression, or $Topo-2
! this is why you give concurrent Topo 1+2 inhibitors!!!
" Toxicity:
*Gilbert Syndrome: pt cant glucaronidate anything ! cant
metabolize the drug ! toxicity
Neutropenia, diarrhea, N/V
$ hepatic enzymes
o Irinotecan
" MOA & Resistance: same (inhibit Topo-1)
" Toxicity:
Same as Topotecan, plus
*Acetylcholinesterase inhibition ! Ach efx, including acute
diarrhea that doesnt respond to Loperamide (give Atropine!)
Anti-Cancer Agents Assessment 8
)
Podophyllotoxins (slide 68 Mandrakes)
o Etoposide (Toposar)
" MOA: inhibits Topo-II (forms ternary complex with it)
prevents re-sealing of normal DNA break ! inappropriate
breakage of DNA
Oral
Renal elimination (dose correction for creatinine clearance)
" Resistance: typical: $efflux, mutation
" Side Efx: myelosuppression, alopecia
o Teniposide (Vumon)
" MOA: inhibits Topo-II (same)
IV
Extensive metabolism, then renal elimination (no dose fix)
" Side Efx: myelosuppression, N/V
Taxanes (from the Western Yew)
o Paclitaxel (Taxol)
" MOA: bind "-tubulin, preventing de-polymerization
! mitosis arrest
Needs surfactant for solubility
If the cell isnt cycling, paclitaxel has no efx.
Hepatic metabolism
" Side Efx:
Cremaphor EL (surfactant) ! microembolism ! chest pain
o Tx prophylactically with antihistamines + steroids!!!
Myelosuppression
*Stocking-glove sensory neuropathy
! b/c efx microtubules in nerves
! Cisplatin has similar side efx; do NOT give in combo!
o Docataxel (Taxotere)
" Semi-synthetic taxol
" more potent than paclitaxel
" less surfactant problems b/c uses Polysorbate 80 instead.
" Side Efx:
Neutropenia
Fluid retention ! perif + pulmonary edema
! Tx prophylactically with oral Dexamethasone
Anti-Cancer Agents Assessment 8
*
Anthracyclines -rubicin
o Doxorubicin (Adriamycin)
" MOA:
Inhibits Topo-2 (large planar ring structure gets in groove)
Makes free radicals
Apoptosis (via p53, caspases, FAS)
" Resistance: typical
" Toxicity
Myelosuppression, alopecia
Etravasational necrosis
Cardiac toxicity ! cumulative
o Acute is reversible
o Chronic is irreversible ! CHF
o PROTECTION with Dexrazoxane (iron chelator that
binds up free radicals, preventing cardio damage)
Red urine (not toxic, just weird)
o Daunorubicin (Cerubidine) same as Doxorubicin
o Epirubicin (Ellence) less cardiotoxic ', but less effective anti-cancer %.
o Valrubicin (Valstar) - non-cardiotoxic; used IVe for bladder carcinoma.
o Idarubicin (Idamycin)
o Mitoxantrone (Novantrone) (the only one without rubicin but it has anthr in it)
" MOA:
Inhibits Topo-2
Binds cytoskeleton protein (cytokeratin 8)
Not enough free radicals for anti-tumor efx
! but still enough for cardiotoxicity
" IV dosing, hepatic elimination
" Blue urine
Anti-Cancer Agents Assessment 8
"+
Bleomycin (Blenoxane)
o MOA: drug-Fe complex causes oxidative damage to the deoxyribose
" effectively same as if blocking Topo ! DNA breaks
" IV or IM ! high drug levels in skin + lung
o Resistance: typical
o Toxicity
" Pulmonary fibrosis + dry cough (may be latent)
" Cutaneous toxicity: hyperpigmentation, hyperkeratosis, etc.
Actinomycin-D (aka: Dactinomycin, Cosmegen)
o MOA: intercalates DNA (ie, inserts itself between a G-C base pair)
" Single strand DNA breaks via Topo-2 axn
" IV dosage
o Toxicity:
" Pancytopenia, anorexia, N/V, diarrhea, alopecia
" Extravasational necrosis
" Dermatalogical manifestations, subject to X-ray (erythema,
desquamation, inflammation).
Asparaginase (Elspar) from E. coli
o MOA: # protein synthesis
o Toxicity:
" # protein synthesis
Beware drug interaxns
Immunosuppression
# insulin ! hyperglycemia
" Pancreatitis (note that amlase and lipase levels may be normal!)
" Hypersensitivity (10% have a potentially fatal rxn)
Review
o Which drugs inhibit Topo-1? Which ones inhibit Topo-2?
o Factoid: Mandrakes come from the same plant family as Atropa belladonna
(Atropine), tomatoes, potatoes, and eggplant. (thank you, Wikipedia).
o Which drug group requires prophylactic steroid tx? Why?
o Which drugs can cause neurotoxicities?
Anti-Cancer Agents Assessment 8
""
Drugs with Specific Molecular Targets
Hydroxyurea (Hydrea)
o MOA: interferes with conversion of ribonucleotides ! deoxyribonucleotides
by stealing the free radical from ribunocleotide reductase.
" Rate-limiting step in DNA synthesis.
" Oral
" Resistance: $reductase
o Toxicity
" Desquamative interstitial pneumonitis
" Myelosuppression ! used against various myeloproliferative disorders.
Thalidomide (Thalomid)
o MOA:
" $ NK cells (via $ IL-2 + IFN-#)
" inhibits anti-apoptosis (ex: NF-$B)
" # angiogenesis
" prevents tumor cell adhesion
o Side Efx:
" Sedation
" Constipation
" peripheral sensory neuropathy
" teratogen!
Tretinoin
o Specifically tx Acute Promyelocytic Leukemia (APL)
! also used for acne + psoriasis b/c promotes desquamation
o MOA: promotes differentiation and disrupts the chimeric gene being over-
expressed in APL.
" Oral
" Hepatic metabolism
o Toxicity
" Retinoic Acid Syndrome: fever, dyspnea, wt gain, pleural effusion
" Teratogen
" $ liver enzymes
Glucocorticoids: Dexamethasone and Prednisone
o MOA: anti-inflammatory + immunosuppressive via #synth of PG + leukotrienes
" Small, lipophilic, with cytoplasmic receptor ! gene transcription
" High doses suppres T-cells (and B-cells)
Anti-Cancer Agents Assessment 8
"#
Antibodies: biological response modifiers
! they all cause apoptosis and ADCC (antibody-dependent cell cytotoxicity)
o Rituximab (Rituxan)
" MOA: binds CD-20 ! B-cell depletion
Directly binds & dimerizes cell surface receptors ! apoptosis
Fc region provides target for complement ! Big MAC
Fc region provides target for macrophages
" Tx cancer and RA
o Alemtuzumab (Campath)
" Binds CD-52 ! T-cell depletion
o Trastuzumab (Herceptin)
" Monoclonal Ab binds EGFR-2 and Her-2/NEU
" Tx breast cancer (30% have the aggressive Her-2 mutation)
" Side Efx: Cardiomyopathy
o Cetuximab (Erbitux)
" Binds EGFR-1 and Her-1
" Tx colorectal cancer
o Bevacizumab (Avastin)
" Monoclonal Ab that blocks VEGF ! anti-angiogenesis
Note: does not target/kill tumor cells, just limits its growth
" Side efx: $$ HTN ! CHF + pulmonary hemorrhage + GI perf.
o Interferon-%2a (Roferon)
" MOA: acts like endogenous INF ! antiviral + anti-neoplastic
Cell cycle arrest in G
0
Apoptosis
$ cytotoxic T-cells + NK cells
pegylated form needs hepatic metabolism; renally eliminated.
" Toxicity:
*Neuropsychiatric
*Flu-like sx
CYP450 inhibition
Anti-Cancer Agents Assessment 8
"$
Tyrosine Kinase Inhibitors
o Gefitinib (Iressa) and Erlotinib (Tarceva)
" MOA: prevent EFGR TK from phosphorylating ! no signal passed on
Cell cycle arrest + inhibits angiogenesis
Oral w/ hepatic metabolism
" RAPID RESISTANCE via expansion of clones w/ mutated targeted TK
" Side Efx: fatiue, rash, N/V, anorexia, diarrhea
o Imatinib (Gleevec) and Dasatinib (Sprycel)
" MOA: oral TK inhibitor
" Resistance to Imatinib is high; Dasatinib is 2G drug w/ different
binding site
o Bortezomib (Velcade)
" MOA: inhibits the ubiquitin-proteasome pathway
prevents degradation of I$B%
o I$B% restrains NF$B (who is a pro-proliferation guy)
o Result: no proliferation '
Activates caspases
Inhibits binding of myeloma cell to stroma
# angiogenesis
inhibits cytokine interactions
o Tocicity: Thrombocytopenia, Peripheral neuropathy
Drug Associations
(randomly inserted here b/c there was room)
Oncology Agent Concurrent Agent Consequence
Tumor Lysis Syndrome Allopurinol, Rasburicase # uric acid ! renal protect
Cyclophosphamide Mensa Protect from acrolein
Cisplatin Amifostine Cytoprotection
MTX Leucovorin Metabolic Rescue
5-FU Leucovorin Enhanced action!
6-MP Allopurinol INCREASES TOXICITY
Anthracyclines Dexroxazone Iron chelator !#cardiotox
Bone Metastasis Pamidronate, Zoledronate #bone pain & fractures
Anti-Cancer Agents Assessment 8
"%
Hormones as anti-tumor agents
Leuprolide (Lupron) and Goserelin
o MOA: GnRH agonists ! initial hyperstimulation! desensitization (castration)
" Avoid initial flair with AR blockers
o Side Efx: sweat, #libido, hot flashes, nausea
Neilutamide and Flutamide
o inhibit androgen binding (but circulating levels remain high)
o Side Efx: gynecomastia
Estramustine
o MOA: alkylating agent that targets cells with estrogen receptors
" binds microtubules ($ disassembly), DNA breakage, apoptosis
o Side Efx: N/V + diarrhea is dose-limiting
Anti-Estrogen Therapy
o Fulvestrant Selective Estrogen Receptor Downregulator (SERD)
" MOA: completely suppresses ER genes
" Resistance: molecular cross-talk b/t ER + growth factor signals
o Tamoxifen and Raloxifene Selective Estrogen Receptor Modulator (SERM)
" MOA:
Estrogen agonist @bone
Estrogen antagonist @ mammary tissue
" Side Efx: endometrial hypertrophy ! endometrial cancer
o Aromatase Inhibitors 3
rd
Generation drugs
" Non-Steroidal: Anastrozole and Letrozole competitively inhibit
aromatase
" Steroidal: Exemestane irreversibly binds aromatase
" Oral w/ hepatic metabolism
" Side Efx:
*more arthralgia & diarrhea than Tamoxifen, but fewer
gynecological symptoms
no affect on adrenal steroids or other hormones.
Nuscle Relaxants Assessment 8
1
Note how the bouy hanules the uiug (hepatic metabolism, etc)
Note othei !"#$$%$ of uiugs that have potential inteiactions.
Review the table on the back page of the hanuout.
ueneial Siue Effects
- impaiieu balance especially in the elueily
- opeiation of motoi vehicles
- auuitive CNS uepiession when useu with othei CNS uepiessants (go figuie).
- anti-cholineigic actions (!secietions, uiinaiy ietention, bluiieu vision)
- potential uiug uepenuency " stopping uiug can cause iebounu pain!
Tx of Spacticity
!"#$%&'( *+,%-'."$/
o N0A0 12!2 "3%(,.4 " 567'-7%$"-,8"4,%( " ! 9:.#$' 4'(.,%(
# also inhibits Substance P
# oial oi intiathecal uosing
# ienally eliminateu
o FBA Inuications: multiple scleiosis, muscle spasm, spasticity, coiu tiauma
o Biug Inteiactions & Siue Efx.
# Renal failuie
# $ bloou glucose (bewaie anti-uiabetics!)
# uiowsiness, confusion, uizziness
;"(4-%$'(' *;"(4-,:9/
o N0A: <$%#=. -6"(%>,(' -'#'74%- %( ."-#%7".9,# -'4,#:$:9 "
7-'?'(4. @"
AA
-'$'".' " -'.4%-'. @"
AA
<"$"(#' <6 "$$%B,(3 -'7"#="3,(3
" ! 9:.#$' "C(
# 0ial oi Iv (neeus suifactant)
# Bepatic metabolism
o FBA Inuications: Nalignant Bypeitheimia, Neuioleptic Nalignant Synuiome,
multiple scleiosis, anu of couise spasticity.
o Biug Inteiaxns anu Siue Efx
# *Livei toxicity, esp. w estiogens " iegulai livei fxn tests
# *Injection site phlebitis
# *Ciosses placenta " floppy baby synuiome
# Bo N0T use with Ca
++
channel blockeis " v-fib
# Raiely: seizuies, peiicaiuitis, pulmonaiy euema
Nuscle Relaxants Assessment 8
2
D,8"(,>,(' *E"("&$'C/
o N0A0 7-'F.6("74,# !G -'#'74%- "3%(,.4
# ! muscle tone but N0T muscle stiength!
# Efficacy to tx spasticity = Baclofen B0T.
Noie seuation
Less auveise muscle weakness
# Efficacy to tx BTN << Cloniuine
o FBA Inuications: NS, spasticity, spinal coiu tiauma
o Siue Efx
# Bon't use with othei anti-BTN uiugs bc " hypotension
# !2 stuff: weakness, xeiostomia, uizziness, seuation
H:,(,('
o N0A: $iefiactoiy peiiou anu !motoi enu plate excitability
# Also gieat anti-piotozoal
o 0ses: tx Nalaiia, tx noctuinal leg ciapms
0thei Biugs fiom 0thei Lectuies
o Cloniuine
o uabapentin
o Biazepam
o !%4:$,(:9 4%C,( - clips v-snaies " pievents 2#5 vesicle ielease at NN}
! pt may uevelop antibouies against it; just switch type A" B.
These uiugs just tx Spasm (ie, uiugs that ielax skeletal muscle) - most act in the CNS
@"-,.%7-%>%$ *I%9"/
o N0A: @JI "C( %( -'4,#:$"- "#4,?"4,(3 .6.4'9 ,( .7,("$ #%->
# No uiiect effect on peiipheial neives, muscle excitability, etc
# 0ial
# Bepatic metabolism (CYP2C19) " uiinaiy elimination
o Siue Efx:
# Biug inteiaxn: Rifampin will ! potency; Ketoconazole will $ potency
# CNS efx: uiowsiness, uizziness, insomnia, veitigo, ataxia
# Nyuiiasis
# 0ithostatic hypotension
@5$%-8%C"8%(' *K"-"&$'C/
o N0A: CNS - unknown
# 0ial
# *No anticholineigic axns
o Siue Efx:
Nuscle Relaxants Assessment 8
S
# Bepatic toxicity " monitoi livei enzymes anu avoiu acetaminophen
@6#$%<'(8"7-,(' *L$'C'-,$/
o N0A: CNS at level of biain stem
# oial
# (fibiomyalgia off-label use)
o Siue Efx:
# Significant anticholineigic efx: uiowsy, xeiostomia, uizziness,
constipation, Nv, bluiieu vision
# Caiuiac efx " falling
M'4"C%$%(' *I='$"C,(/
o N0A: CNS " geneial seuative axn anu alteieu pain peicption
# 0ial
# Bepatic metabolism " monitoi enzyme levels!
# (uiinaiy elimination)
o Siue Efx
# Fatty meals $ plasma uiug levels
# Typical stuff: auuitive CNS uepiession, Nv, uI upset, uiowsiness
# Beauache, iiiitability
M'45%#"-<"9%$ *M"-<"C,(/
o N0A: same as Netaxolone but can be given oial, Iv, oi IN
# Can tx muscle spasm anu tetanus
o Siue Efx
# Phlebitis bc of suifactant foimulation (piopylene glycol)
# Typical stuff
N-75'(">-,(' *L$'C%O'#4/
o N0A: geneializeu seuative axn in meuulla anu ceiebial motoi centeis
! Similai stiuctuie to uiphenhyuiamine (Benauiyl)
analgesia + local anesthetic
milu anti-cholineigic axns
anti-histamine
# Also useu off-label to tx Paikinsonism
# 0ial, Iv, IN
# Bepatic metabolism
o Siue Efx: anti-cholineigic stuff
Tx of Fibiomyalgia - K-'3"<"$,( *+6-,#"/
N0A: 12!2 "("$%3:' "4 !G# .:<:(,4. %& @"
AA
#5"(('$.
o ! neuional calcium cuiients " ! neuiopathic pain + anxiety
o ienal elimination, viitually unchangeu
Siue Efx:
Nuscle Relaxants Assessment 8
4
o iebounu woisening withuiawal
o swelling of hanus + feet, uizziness, xeiostomia, seuation, wt. gain
GI Drugs Assessment 9
"
Laxatives
Note: laxative abuse & overuse can lead to thorough constipation.
Bulk-Forming Laxatives
o Methyl psyllium (Metamucil) and Methyl cellulose (Citrucel)
! MOA: dissolve in water " form a gel.
In intestines, they attract water and swell ! #H
2
O in stool.
Side efx: reduce absorption of other drugs and nutrients.
o Polycarbophil (Mitrolan) (not on drug list)
Surfactant Laxatives
o MOA: Stool softener
! $ water tension b/t stool and GI tract " reduce strain of defecation
! Do not use long-term b/c of mucosal irritation
o Docusate sodium (Colace, Surfak) anionic surfactant
o Poloxamer 188 non-ionic surfactant
o Castor oil anionic surfactant AND stimulates myenteric plexus (peristalsis)
! Converted to active form (ricinoleic acid) in small bowel
! Used for catharsis (complete bowel evacuation)
! Can induce uterine contraction in pregnancy
Stimulant Laxatives
o Most Potent Class of Laxatives
o 3 MOAs:
! # permeability of intestinal mucosa " allow back diffusion
! stimulate myenteric plexus " # peristalsis
! # prostaglandin synthesis and intestinal secretions
o Bisacodyl (Dulcolax and Modane) - prodrug, converted by enteric bacteria
o Sena (Senekot)
! Natural product; more gentle than Dulcolax.
! Promotes colonic motility
! Pink urine
GI Drugs Assessment 9
#
Osmotic Laxatives
o Laxatives with Magnesium
! 2 MOAs:
non-absorbable " osmotic effect " retains water in lumen
cause release of CCK " # intestinal motility and secretion
! Magnesium sulfate (Epsom salt)
! Magnesium hydroxide (Milk of Magnesia)
! Magnesium citrate (Citroma) cathartic
o Laxatives with Phosphate
! Buffered phosphate (Fleet Enema or oral) cathartic
o Nondigestible sugars and alcohols
! Lactulose (Cephulac)
2 MOAs:
o osmotic (non-absorbed semi-synthetic disaccharide)
o Fecal acidifier (acidic metabolism products via enteric
bacteria)
! can help liver failure pt excrete ammonia.
! Glycerine osmotic and lubricant effects; suppository.
! (Golytely) polyethylene glycol electrolyte solution (not on drug list)
Nasty: dissolve into 4L and drink for complete evacuation.
Other Laxatives
o Cascara sagrade extract (not in lecture)
o (Haleys) Mineral Oil penetrates and softens stool
o Lubiprostone (Amitiza) (not on drug list)
! # secretions by activating Cl
-
channels, which also causes #motility.
! Great for tx chronic idiopathic constipation (ex: IBS).
GI Drugs Assessment 9
$
Anti-Diarrheals
Tegaserod (Zelnorm) on quiz but not in lecture
o 5-HT
4
antagonist " motility stimulant
o withdrawn from US market in 2007 (but can be acquired for emergencies)
Metamucil (also see above)
o In intestines, they attract water and swell ! #H
2
O in stool, except this time
somehow, this encourages stool to form instead of being a laxative. ???
Bismuth subsalicylate (Pepto-Bismol)
o Adsorbs harmful bacteria, viruses, and/or toxins
Attapulgite (Kaopectate) same as Pepto Bismol
Opiates as Anti-Diarrheals
! 4 MOAs of opioids:
$ secretions
# muscle tone " stiff " anti-spasmotic (tx cramps)
" # sphincter tone " $ urgency
$ motility " # contact time
does not cross BBB ! $$CNS efx ! specific for diarrhea
o Paregoric camphorated extract of opium (0.04% morphine)
o Diphenoxylate + atropine (Lomotil) atropine added to thwart abuse
o Loperamde (Imodium) binds calmodulin
Anti-Cholinergics as Anti-Diarrheals
o MOA: block Ach from Vagus N. ! block signals for GI motility + secretion.
! Note that doses high enough to block these signals would be toxic.
*These drugs are use as anti-spasmodics to alleviate cramps.
! Dont cross BBB ! $$ CNS efx
o Propantheline (Pro-Banthine) not on drug list; also tx urinary incontinence
o Dicyclomine (Bentyl) not on drug list
o [a different anti-cholinergic] + Benzodiazepine = (Librax) " sedative
GI Drugs Assessment 9
%
Anti-Emetics
Review: CNS involvement in the vomiting reaction (slide 24 + 25)
Scopolamine (Scop-Dur) - anti-cholinergic
o MOA: blocks muscarinic receptors on CN VIII as it travels to CTZ (?)
o Tx: prophylaxis for motion sickness
o Dose: transdermal patch behind ear
o Side Efx: sedation, drowsiness, dry mouth
Anti-Histamines as Anti-Emetics
! Remember: 1
st
Gen. H
1
blockers also exhibit anti-cholinergic efx.
! MOA: anti-cholinergic part can act at any of the M
1
receptors in the diagram.
o Dimenhydrinate (Dramamine) OTC prophylaxis for motion sickness
o Cyclizine (Marezine) - OTC prophylaxis for motion sickness
o Meclizine (Antivert) requires Rx
! Tx Vertigo and Menieres Dz b/c has depressant efx on ear labyrinth
o Promethazine (Phenergan) - #potency; tx severe N/V or use pre-surgery
GI Drugs Assessment 9
&
Anti-Dopaminergics as Anti-Emetics
o Chlorpromazine (Thorazine)
! 2 MOAs: anti-dopaminergic + anti-cholinergic
! low doses highly effective for N/V and intractable hiccups
o Prochlorperazine (Compazine) not on drug list
o Thiethylperazine (Torecan) not on drug list; used at hospitals b/c injectable
o Droperidol (Inapsine) - Blocks D2 receptors in CTZ; Tx Post-op N/V
o Metoclopromide (Reglan)
! 2 MOAs:
Blocks D2 receptors
# gastric emptying (prokinetic)
! Tx chemo-induced & Post-op N/V.
o Trimethylbenzamide (Tigan) - extrapyramidal side efx ! use short-term
Serotonin Antagonists as Anti-Emetics
! MOA: 5-HT
3
antagonist (see above figure)
block receptors in GI
block receptors in CTZ
*Most effective anti-emetics " allow # chemo dosing
*Potency # even more if co-administered with dexamethasone
o Ondansetron (Zofran) class rep; IV, oral
o Granisetron (Kytril) more potent; oral
o Dolasetron (Asemet) longer t!
Miscellaneous Anti-Emetics and Adjuvants
o Delta 9 THC (Dronabinol) marijuana derivative
! Tx intractable N/V in chemo pts (only in CA)
o Corticosteroids: Dexamethazone and Methylprednisolone
! Anti-emetic AND reduce side efx of other drugs via $ prostaglandins
o Aprepitant (Emend) substance P antagonist; crosses BBB to act on CTZ
o Lorazepam (Ativan) benzodiazepine, used for anticipatory vomiting
GI Drugs Assessment 9
'
Great drugs to tx Peptic Ulcer Dz
Antacids
Magnesium-aluminum Hydroxide (Maalox)
o MOA: weak bases that neutralize HCl ! prevent pepsin activation
o Uses: simple reflux, or adjunct w/ H
2
Blockers and/or PPIs.
o Side Efx: drug interactions b/c " pH; Frequent dosing is inconvenient
Mg-Al Hydroxide + alginic acid (Gaviscon)
o alginic acid is a floating gel to help prevent reflux
Calcium Carbonate (Tums)
o Side efx: acid reflux (b/c pH # so fast " reflex acid secretion #)
H
2
Antagonists
Ranitidine (Zantac)
o MOA: comptetitively inhibit H
2
receptors (in stomach) !$ acid secretion
Famotidine (Pepcid AC) most popular b/c most Potent and Longest t!
Niatidine (Axid) comparable to Famotidine
Cimetidine (Tagamet) not on drug list. No reason to ever give it b/c its least
potent, shortest t! and side efx (CYP450) can be avoided using the other 3.
Proton Pump Inhbitors (PPIS)
MOA: covalently bind & inhibit hydrogen ion pump (90% effective!).
o Irreversible modification of sulfydryl group on H/K-ATPase on parietal cells
o Requires acidic pH for activation
o Drug trapping (b/c covalent)
o Best to use short-term b/c long-term efx unknown
Omeprazole (Prilosec) oral, long t!
Esomeprazole (Nexium) - oral, long t!
Lansoprzole (Prevacid) less effective
Rebperazole (Aciphex) - metabolized less by CYP450 ! lasts longer in pts
taking other Rxs.
GI Drugs Assessment 9
(
Cytoprotective
Bismuth subsalicylate (Pepto Bismol)
o 4 MOAs:
! # secretion of mucous and HCO
3
! inhibits pepsin
! forms protective barrier at base of ulcer
! inhibits H. pylori
o Uses: GERD, PUD, and diarrhea
Sucralfate (Carafate)
o Forms sticky viscous gell at base of ulcer
o Requires acid pH (prevent pneumonia in nocosomial chronic users)
Misoprostol (Cototec) PGE
1
analog
o # secretion of mucous and HCO
3
o Side efx: intolerable (ex: diarrhea)
Antibiotics (for attacking H. pylori)
! a multi-drug regimen (slide 30): PPI + 2 Abx
Clarithromycin - Macrolide that inhibits microbe protein synthesis
Metronidazole synthetic abx for obligate anaerobes (resistance is a problem)
Tetracycline second-line drug (stagger dosing if w/ Bismuth)
o Not much resistance problem, but it turns kids adult teeth brown
Amoxicillin for G- bacilli
Furazolidine nitrofuran that is antibacterial and antiprotozoal
Drugs for portal HTN and Encephalopathy
Lactulose (Cephulac) see laxatives; acidification of stool $ systemic NH
4
Neomycin give enema to $ colonic bacteria
GI Drugs Assessment 9
)
Drugs to Tx GERD
Two-pronged approach to Tx GERD:
1) postural & dietary therapy (smaller meals, no mexican food, elevate bed)
2) prokinetic drugs to enhance peristalsis (keep that food down!)
(Note: anti-secretory drugs (H
2
-R + PPI) can be used to #healing, but do not affect LES pressure)
D
2
Receptor Blockers
Metoclopramide (Reglan)
o MOA: anti-D
2
removes inhibition ! # local Ach (5HT
4
can now signal) "
smooth muscle stimulation (Slide 39).
! * accelerate gastric emptying
! * # LES pressure
! # esophageal peristalsis amplitude
o Side Efx: other D
2
Rs get blocked (tardive dyskinesia) ! use only 1-2 wks
Domperidone (motilium) same as Metoclopramide
Drugs to Tx Inflammatory Bowel Dz
Local Anti-Inflammatory Agents
Sulfsalazine (Azulfidine)
o MOA: prodrug that is broken down into two metabolites
! 5-ASA " active
! sulfapyridine " side efx: anemia, rash, impotence
ASA-Dimer (Rowasa)
o MOA: prodrug that is metabolized to two molecules of 5-ASA
o Fewer side efx but weaker anti-inflammatory
Glucocorticoids: Prednisone
Antibodies for TNF#
Infliximab (Remicade) - monoclonal IgG Aby for TNF# " bind TNF#
Etanercept (Enbrel) - MOA: soluble TNF# receptor " bind TNF#
Endocrine Drugs Assessment 10
"
Pituitary: Natural Hormones and Associated Drugs
Somatotropic Hormones (slide 9 & 10) pulsatile release
o Growth Hormone (GH)
! stimulates liver et al (via tyrosine kinase) to release IGF-1 ! growth
! deficiency ! pituitary dwarfism
! excess ! gigantism or Acromegaly
! Dx deficiency: hypoglycemia (insulin-induced) "GH; high glucose #GH
$ Somatropin (Serstim, Genotropin, Humatrope, etc) same as hGH
$ Somatrem (Protropin) = GH + methionine
(Methionine added at terminal end of GH peptide to extend patent)
$ Sermorelin acetate (Geref)
the first 29aa of GHRH (44 total)
for testing, not for replacement therapy
$ Side Efx
Less in children but include: leukemia, "ICP, nausea
Adults: carpal tunnel, peripheral edema, arthralgia, myalgia
o IGF-1 (Insulin-like Growth Factor)
! deficiency looks like #GH BUT does not respond to hGH. Tx with:
$ Mecaserin (Increlex) IGH binding protein combo (1+3)
Provides the IGF binding protein AND " t!.
! excess causes Acromegaly. Tx with:
$ Pegvisomant (Somavert) GH Receptor antagonist ! # IGF-1
covalently bound polyethylene glycol (PEG) # renal clearance !" t!
o Prolactin (PRL) no therapeutic use, but
o Dopamine Receptor Agonists to "DA ! # prolactin ! tx hyperprolactin-
emia from pituitary adenomas
$ Pergolide (Permax) - 1 tx Parkinsons. Least expensive.
$ Cabergoline (Dostinex) - "affinity, "t!
$ Quinagolide [not in US]
$ Bromocriptine (Parlodel)
Somatostatin Analogs
! Somatostatin normally negatively regulates secretion of GH + TSH
! excess GH = Gigantism or Acromegaly. Best tx is surgery; drugs are 2.
o Octreotide (Sandostatin) short t! (3x daily injxn)
$ Side Efx: diarrhea, nausea, abdominal pain
o Lanreotide (Somatuline LA) long acting, slow release, same side efx
Endocrine Drugs Assessment 10
#
Glycoprotein Hormones
o Thyrotropin (TSH)
o Luteinizing hormone (LH) ovulation occurs 36 hrs after LH surge
o Follicle-Stimulating Hormone (FSH)
$ Menotropin (Pergonal, Humagon, Repronex) give IM
urine from post-menopausal women; contains FSH + LH
tx female infertility
$ Recombinant FSH give SubQ - also tx female infertility
Follitropin " (Gonal-F) or Follitropin # (Puregon, Follistim)
o Chorionic Gonadotropin (hCG)
$ Diagnostic kits target hCG-#
$ Human excreted CG (Pregnyl, Profasi)
From pregnant womens urine. Mimic LH ! tx female infertility
$ Menotropin same as above
o RISK of multiple pregnancy with gonadotropins!
Pro-opiomelanocortin (POMC)-derived Hormones
o Corticotropin (ACTH)
o "-MSH & #-MSH (melanocyte stimulating hormones)
Posterior Pituitary Hormones: Oxytocin, Vasopressin (ADH), Desmopressin
Hypothalamus: Releasing Hormones
Gonadotropin Rleasing Hormone (GnRH)
! stimulates FSH + LH ! stimulate gonads ! necessary for fertility
o Synthetic GnRH (Factrel, Lutrepulse) - t! = 2-4 min
$ Use Factrel to DDx pituitary vs. hypothalamic defect when pt has
hypogonadotropism
$ Use Lutrepulse (pulsating IV) to tx male infertility (try androgens 1
st
).
o Analogues of GnRH longer t!
! tx prostate cancer & precocious puberty by surge ! downregulation
$ Goserelin acetate (Zoladex), Triptorelin (Trelstar), Leuprolide (Lupron)
$ Histrelin (Supprelin) & Nafarelin (Synaral)
o Cetrorelix (Cetrotide) and Ganirelix (Antagon) = GnRH Antagonists
$ used to delay LH surge ! delay ovulation to allow collection of ova for
use in in vitro fertilization
Growth Hormone Releasing Hormone (GHRH) ! stimulates AP to release GH
Thyrotropin Releasing Hormone (TRH) (Protirelin) used for diagnostics (slide 37)
Corticotropin Releasing Hormone (CRH) used for diagnostics (Cushings vs. ectopic)
Endocrine Drugs Assessment 10
$
Adrenocorticosteroids
ACTH
o Natural (HP Acthar Gel) from animal sources (POMC peptide)
o Cosyntropin (Cortrosyn) synthetic (aa 1-24), preferred
$ Major clinical use is to test integrity of HPA axis (negative feedback to
hypothalamus & pituitary, slide 10) does pt need supplemental steroids?
Glucocorticoids ! gluconeogenesis & anti-inflammatory (block Phospholipase A2)
o Cortisol = Hydrocortisone short t!
o Cortisone Acetate short t!
o Prednisone (Deltasone) & Prednisolone medium t!
o Methylprednisolone medium t!
o Dexamethasone (Decadron) long t!
o Betamethasone long t!, tx asthma
o Triamcinolone long t!, tx asthma
o Budesonide (Pulmicort) tx asthma or IBD
o Side Efx of Glucocorticoids
$ *Suppression of ACTH and TSH production ! dont stop tx abruptly!
$ " lipolysis, redistribute fat (Cushing-oid)
$ " diabetes risk (b/c opposes insulin)
$ peptic ulcers ! perforation risk b/c steroids suppress the pain
$ CNS ! arousal, euphoria, insomnia
$ Blood: " Hgb + RBC + PMNs; # lymphocytes + eosinophils
$ In MEN: hypogonadism
$ In WOMEN: stop ovulation, dysmenorrhea, osteoporosis
$ In CHILDREN: inhibit IGF-1, osteoporosis
Mineralocorticoids ! Na+ Retention
o Aldosterone
$ Stimulated by 1) angiotensin II & 2) "K+
$ Axn: distal convoluted tubule ! Na+ resorption; K+ & H+ secretion
$ Side Efx: edema, HTN, cardiomyopathy, CHF, hemorrhage
o Fludrocortisone synthetic aldosterone
o Spironolactone aldosterone antagonist.
Inhibitors of Adrenocorticoids
o Aminoglutethimide inhibits CYP450 in synthetic pathway ! inhibits
overproduction of cortisol ! tx Cushings.
o Ketoconazole anti-fungal; also inhibits CYP450 ! tx Cushings.
" potency
b/c no efx on
mineralocorticoid
receptors
Endocrine Drugs Assessment 10
%
Gonadal Hormones
Estrogen ! birth control (BC) & tx prostate cancer
$ Bones: closes epiphysial plates; # osteoclasts (tx osteoporosis)
$ Cancer Risk: stimulates whats already there ! breast, endometrial
$ " hepatic protein synthesis ! clotting factors ! thromboembolism
$ " HDL, # LDL (good)
o Natural Estrogens "" 1
st
pass metab
$ Estradiol most potent; principal ovarian steroid
$ Estrone like estradiol, it is made from androgen via aromatase.
$ Estriol least potent; principal placental steroid
o Ethinyl Estradiol & Mestranol synthetic 17" bonds allow #
1st
pass metab.
$ oral use for contraception
o Estrogen Esters: conjugated (Premarin), from estradiol (Delestrogen et al)
$ IM injection to tx menopause (Premarin = Pregnant Mare Urine)
o Estropipate (Ogen) crystalline estrone sulfate
o Non-steroidal Estrogens avoid 1
st
pass efx
$ Diethylstilbesterol (DES) - teratogenic
$ Clorotrianisene
o Selective Estrogen Receptor Modulators (SERM) ! tissue selective
$ Tamoxifen, Raloxifene, & Toremifene
agonist in bone, brain, + liver
antagonist in breast + endometrium (! tx breast cancer)
o Anti-Estrogens: Clomiphene & Fulvestrant
$ antagonist in all tissues (bind ER"+#)
$ Axn: block feedback inhibition ! "GnRH !! induce ovulation
Progestin ! estrogen Precursor, maintains Pregnancy
$ Norethindrone
$ Norgestrel
$ Levonorgestrel
o Anti-Progestins
$ Mifepristone RU 468 blocks P receptor; morning-after pill (49 days)
$ Onapristone more pure antagonist
o Selective Progesterone Receptor Modulator Asoprisnil experimental
o Aromatase Inhibitors ! tx breast cancer (after Tamoxifen fails) (slide 32)
$ Anastrozole & Letrozole
# HDL, " LDL (bad) ! CHD
thickens cervical mucus & # oviduct motility
tx endometrial cancer
morning-after pill (Levonorgestrel)
Endocrine Drugs Assessment 10
&
Androgens
o Testosterone:
$ 3 MOA:
bind androgen receptor
conversion in some tissues to 5"-dihydrotestosterone (DHT),
which is more potent.
conversion to estradiol ! binds estrogen receptor
$ Side Efx: masculinize females, feminize men, " risk CHD, hepatic
carcinoma
o Testosterone Derivatives (slide 53)
$ Methyltestosterone
$ Testosterone propionate
$ Testosterone cypionate
$ Testosterone enanthate
$ Fluoxymesterone
$ Danazol tx endometriosis; masculinizing side efx
Androgen Receptor Antagonists
o Cyproterone acetate tx acne + baldness
o Flutamide, Bicalutamide, & Nicalutamide tx prostate cancer
$ Nicalutamide is less hepatotoxic, longer t!
Inhibitors of 5"-Reductase Finasteride blocks testo converstion to DHT
o Tx BPH (benign prostatic hyperplasia) and male-pattern baldness
o Teratogenic
Anabolic Steroids ! athletes abuse em
o Side efx: #Testo levels, #libido, #sperm, "liver toxic, CHD (#HDL+"LDL).
o Oxandrolone less conversion to estrogen (so its better?)
o Androstenedione
Loose Ends (not on drug list)
o Spironolactone aldosterone antagonist competes for testo receptor
o Ketoconazole antimycotic inhibits CYP450 ! inhibits testo synthesis (note
that this is a side effect, NOT therapeutic use)
o SARM: selective androgen receptor modulators experimental
$ Bind androgen receptors to stimulate muscle + bone growth
Review: Use in Cancer Chemotherapy (slide 31)
o Breast Cancer ! tamoxifen, aromatase inhibitors
o Endometrial Cancer ! anti-estrogens, progestins
o Prostate Cancer ! estrogens, anti-androgens
Endocrine Drugs Assessment 10
'
Monomer (no hexamer with zinc)
! faster onset + shorter t!
Pancreatic Hormones and Anti-Diabetic Drugs
Natural Regular (soluble) Insulin for IV injection
o Porcine differs from human by only 1 aa
o Bovine differs by 3 aa
o Ovine (sheep) differs by 3 aa
Modified crystal size insulins (slide 23)
o NPH insulin intermediate axn ! use twice daily (B-fast + Supper)
o Lente insulin (also intermediate axn) = 30% semilente + 70% ultralente
$ Semilente insulin short-acting
$ Ultralente insulin long-acting b/c has larger crystals
Synthetic Insulins slide 31!
o Recombinant DNA Human Insulin (Humulin) made in bacteria/yeast
o Human Insulin made by switching AA of Porcine insulin (Novolin)
o Insulin lispro (Humalog)
o Insulin aspart (NovoLog)
o Insulin glulisine (Apidra)
o Insulin glargine (Lantus) long-acting asparagine 21 replaced by glycine
o Insulin detemir (Levemir) long-acting acidic solution neutralized at injxn !
crystals precipitate ! slow absorption
Sulfonylureas ! promote hypoglycemia by "efx of insulin on glucose uptake
o Metabolized in liver, excreted by kidney, use is controversial.
o Axn is enhanced by NSAIDs
$ 1
st
Gen
Tolbutamide
Chlorpropamide
Tolazamide
Acetohexamide
$ 2
nd
Gen more potent
! all start with Gli ! filled with Glee for being better than 1
st
Gen
Glyburide can be combined w/ Metformin
Glipizide
Gliclazide
Glimepiride
Meglitinides: Repaglinide & Nateglinide ! promote hypoglycemia by " insulin secretn
o short t! ; used to control post-prandial glucose level. (Beware hypoglycemia)
Endocrine Drugs Assessment 10
(
Biguanides ! promote hypoglycemia by # hepatic glucose production
$ Does not affect insulin secretion, ! no hypoglycemia
o Phenformin withdrawn b/c lactic acidosis
o Metformin (Glucophage)
Thiazolidindiones (the glitter zone) ! promote hypoglycemia by binding PPAR$
receptor ! " insulin sensitivity
o Troglitazone withdrawn b/c severe liver toxicity
o Rosiglitazone (Avanida) black box warning
o Pioglitazone (Actos)
"-glucosidase Inhibitors ! promote hypoglycemia by inhibiting "-glucosidase (in
epithelial brush border) ! # carbohydrate absorption
o Acarbose
o Miglitol
Incretins ! " insulin secretion
o Whats an Incretin? Endogenous compounds (GIP & GLP-1) that # post-prandial
blood glucose. Usu secreted w/ oral food intake.
o Exenatide (Byetta) more potent than GLP-1 (from Gila monster venom)
o Sitagliptin Phosphate (Januvia) inhibits inactivation of Incretins
Amylin Analogues Pramlintide augments endogenous amylin
o Whats amylin? Similar axns to GLP-1 but different receptors: slows gastric
emptying, " satiety, inhibits glucagon.
o Benefits: pt loses weight and needs less insulin.
Diazoxide inhibits insulin secretion (but not synthesis) ! tx hypoglycemia
Octreotide long-acting somatostatin analogue ! inhibits insulin, glucagon, GH, &TSH
o Tx insulinomas, glucagonomas, acromegally, etc.
Drug Combinations add it with Metformin for a happy cocktail
o + Glyburide
o + Rosiglitazone
o + Pioglitizone
o + Glipizide
o + Sitagliptin
The Future: Tyrosine Kinase Inhibitors (like Imatinib) to tx Type 1 DM.
Endocrine Drugs Assessment 10
)
Calcium Regulating Hormones
Parathyroid Hormone
o Teriparatide (hPTH 1-34) short t!
o Full-Length hPTH (1-84)
Calcitonin
o Synthetic human calcitonin hCH
o Natural calcitonin from salmon (Calcimar)
$ Abys may develop; use prednisone.
o Use: excess Ca
++
from Hyperparathyroid
(short-term use), Pagets Dz, Osteoporosis
Vitamin D (Calcitriol)
$ Cholecalciferol = Vitamin D
3
(fish liver oils)
$ Ergosterol (similar to cholesterol)
$ Ergocalciferol (after irradiation) = Vitamin D
2
$ 25-OH cholecalciferol
$ Calcipotriol analog of Calcitriol; tx psoriasis
$ Dihydrotachysterol (reduced VitD
2
, DHT)
Less active, but more effective w/ "dose ! good tx osteoporosis
$ Paricalcitol MOA: #PTH secretion
$ 22-Oxacalcitriol MOA: # PTH synthesis
* " plasma Ca
++
(bone, kidney, GI)
* MOA: " cAMP (urine test)
* # plasma Ca
++
* comes from C-cells in thyroid
* opposes efx of PTH
Actions of Calcitriol
* " plasma Ca
++
(GI, kidney, bone)
* synth. in skin
* most important Ca
++
regulating hormone!
Therapeutic Uses:
* hypoparathyroid
* rickets/osteomalacia
* osteoporosis
Endocrine Drugs Assessment 10
*
Bisphosphonates ! inhibit bone resorption
o Tx: Pagets Dz, Osteoporosis, Hypercalcemia (long- term tx for weeks)
o Dose: must take after overnight fast w/ glass of water, no food for 30 min.
o Side Efx: osteonecrosis of the Jaw! (esp w/ 3G)
! gingival swelling and loosening of teeth; surgery makes it worse! %
$ 1
st
Gen Etidronate less effective orally (infusion better to # Ca
++
)
$ 2
nd
Gen more potent
Alendronate (Fosamax) tx osteoporosis
Pamidronate
Ibandronate (Boniva)
$ 3
rd
Gen even more potent! ! Risedronate (Actonel) & Zoledronate
Calcium Sensing Receptor (CaSR) Mimetics (aka: calcimimetics)
o Cinacalcet
$ MOA: binds allosterically to CaSR ! suppresses PTH at lower [Ca++].
$ Tx: hyperparathyroid, PT-carcinoma
Fluoride binds Ca
++
o Cavity prophylaxis (! in our drinking water)
o Prevent blood clotting
o Prevent osteoporosis
o Toxicity: osteosclerosis (but no cancer risk, which is nice).
(one more page!)
Endocrine Drugs Assessment 10
"+
Thyroid and Anti-Thyroid Drugs
The Natural Hormone tx hypothyroidism
$ T
4
= tetraiodothyronine = the form synthesized in the thyroid gland
$ T
3
= triiodothyronine = active form metabolite of T
4
.
$ rT
3
= reverse T
3
, inactive form
$ Axns: growth, " metabolism, "HR
$ Side Efx: monitor levels closely to avoid "/#-thyroidism
o Desiccated animal thyroid preparations (T
4
+T
3
) not preferred b/c " variability
o Levothyroxine (L-T
4
) (Synthroid)
o Liothyronine Sodium (L-T
3
)
o Liotrix (both T
4
+T
3
)
Anti-Thyroid Drugs (Thioureylenes) tx hyperthyroidism
o Propylthiouracil (PTU)
$ 2 MOA:
inhibits I
-
organification ! it cant bind to thyroglobulin
inhibits peripheral conversion of T
4
! T
3
.
$ Side Efx: uncommon (agranulocytosis, rash)
o Methimazole
$ MOA: only inhibits I
-
organification.
$ More potent and longer t! than PTU
$ Side Efx: crosses placenta (bad b/c fetus needs thyroid for happy brain)
o Carbimazole
Iodine & Friends
o Iodine
$ MOA: large doses inhibit iodine metabolism ! rapidly blocks T
4
release
$ Tx: thyroid storm
o Radioactive Iodine (Na
131
I)
$ concentrates in thyroid ! destroys parenchyma
$ Tx: big thyroid (ex: Graves Dz, goiter, carcinoma?)
o Iodinated Contrast Media (off-label use for hyperthyroidism)
$ MOA: inhibit peripheral conversion of T
4
! T
3
$ Diatrizoate
$ Iohexol
Anti-Lipid Drugs Assessment 10
1
Synthetics:
FAR
Drugs that (primarily) Lower LDL Cholesterol (and ! coronary events)
Bile Acid Sequesterants
o MOA: anionic ! bind (-) bile acids in gut " interrupt bile recycling " makes
liver think it needs to excrete more cholesterol
! safe, non-systemic, ok for kids & liver dz
# Colestipol big tablet
# Cholestyramine -
# Colesevelam more potent; forms hydrophilic gel ! drink water!
o Side Efx: unpleasant sandy texture, flatulence, constipation; drug interaxns
Statins = HMG-CoA Reductase Inhibitors
o MOA: up-regulate hepatic LDL-receptors via $ SREBP-2 transcription
! extensive 1
st
pass metabolism BUT ok b/c liver is the target organ! %
o Tx: ! LDL, ! TG
# Simvastatin prodrug, intermediate efx
# Pravastatin safer but w/ low potency, low efficacy
# Fluvastatin - safer but w/ low potency, low efficacy; Gemfibrozil ok
# Atorvastatin $ potency; !!renal clearance
# Rosuvastatin most potent
# Lovastatin prodrug (needs CYP3A4)
o Side Efx:
# Generally well-tolerated, may have GI distress or sleep issues
# CYP3A4 (get out that plastic card) " LOTS of drug interaxns!!!
# Not for renal dz (except Atorvostatin OK)
# Teratogenic
# Rhabdomyolysis: if it gets systemic " $CPK " muscle lysis " acute
renal failure " death.
# Myositis (muscle weakness + incr CPK)
Cholesterol Absorption Inhibitors " Ezetimibe
o MOA: blocks internalization of NPC1L1 (niemann-pick) " inhibits cholesterol
absorption (50%) in small intestine " ! hepatic cholesterol " up-regulates
LDL receptors " ! LDL + TG & $ HDL " biliary excretion.
o Side Efx:
# Usu. well-tolerated (minimal steatorrhea)
# GI distress, fatigue, gallstones
# Plasma Levels $ if: elderly, female, liver insufficency
# Drug interaxns: CYP3A4, bile acid sequesterants, etc (slide 35)
# Pregnancy Category C; excreted in breastmilk ! do not use
Anti-Lipid Drugs Assessment 10
2
Drugs that (primarily) Lower Triglycerides (TG) & Raise HDL-Cholesterol
Fibric Acid Derivatives (Fibrates)
o MOA: activate PPAR-" (FA oxidation). (Note: #-targeted ones are for diabetes)
! $LPL, $ApoA1, but $ bile cholesterol excretion causes $ gallstones
# Gemfibrozil safe (at low doses) for renal + liver dz
side efx: reflux, diarrhea, myopathy if used w/ statins (so
either use Fluvastatin, OR switch to Fenofibrate).
+benefit to !CHD (esp if $TG (go figure) or diabetes)
# Fenofibrate has active metabolite
side efx: $transaminases, !GFR (azotemia) !bad for renal dz
# Clofibrate side efx: gallstones + cancer
o All are Teratogenic
Nicotinic Acid (Niacin)
o Aka: pyridine-3-carboxylic acid = vitamin B3
# Immediate Release (IR) (Niacor) - $ side efx
# Sustained Release (SR) (Slo-Niacin) slow release but $$ hepatitis
# Extended Release (ER) (Niaspan) t! 4-6hrs
# Niaspan + Simvastatin (Simcor)
o MOA: unknown, something about !FFA mobilization
o +benefit to !CHD, esp combined w/ simavastatin.
o Side Efx:
# Hepatotoxicity (! max 2g/day)
# Flushing w/ ants
# Eye issues: conjunctivitis, retinal detachment
# $ insulin resistance " look for acanthosis nigricans
# Other: GI irritation, gout, dry skin, Pregnancy Category C
Omega-3 Polyunsaturated fatty acids (Fish Oil)
o MOA: !TG (nil efx on HDL or LDL)
o +benefit to !CHD " antiplatelet, hypotensive, antiarrhytmic
Investigational HDL-raising Drugs just FYI, not for test. %
Anti-Parasitic Drugs Assessment 10
"
Drugs to Tx Protozoal Infections
*Metronidazole requires metabolic activation
o MOA: block Pyruvate:ferrodoxone oxidoreductase (parasite specific).
! Equally active in dividing and non-dividing cells.
! " bioavailability, BBB penetration, hepatic metabolism
o Tx: amoeba (tissue), giardia, trichomonas, anaerobic bacteria (B.fragilis)
o Side Efx: GI, heatache, metallic taste, dizziness, disulfriam-like
o Contraindications: Lithium, Coumadin
Atovoquone
o MOA: inhibits electron transport ! # pyrimidine synthesis
o Tx: pneumocystis, toxoplamsa, amoeba, trichomonas, P.falciparum.
*Eflornithine
o MOA: inhibits ornithine decarboxylase (a parasite essential)
o Tx: W. trypanosoma
o *Side Efx: anemia, leucopenia, diarrhea convulsions, GI pain, alopecia
Paramomycin
o MOA: aminoglycoside abx
o Tx: amoeba (DOC), tapeworms, leishmanias, (giardia if pregnant)
o Side efx: diarrhea, GI upset, not for renal dz
Iodoquinol MOA unknown
o Tx: tapeworms, amebas (lumen), and maybe anti-protozoal.
o Side efx: diarrhea, iodine toxicity (but no neuropathy)
o Contraindicated for optic neuropathy, renal dz, thyroid dz
Pentamide - MOA unknown, may inhibit DNA
o Tx: 2
nd
line for pneumocystis, leishmania, & trypanosoma (blood stage)
o Side Efx: 50% toxicity = hypoTN, hypoglycemia, blood dyscrasias,
cardiotoxicity, nephrotoxicity
Sodium Stibogluconate
o MOA: interferes with trypanothine redox system (IV or IM)
o Side Efx: overall ok, but pancreatitis, myelosuppression, muscle pain
Melarsoprol
o MOA: arsenic $ inhibit trypanothione reductase (always give IV)
o Tx: trypanosoma brucei (CNS stage)
o Side Efx: toxicity = fever, reactive encephalopathy (5%), neuropathy
! prevent w/ prednisone prophylaxis
! Paramomycin
is preferred
Anti-Parasitic Drugs Assessment 10
#
Drugs to Tx Malaria
Blood schizontocides
o Chloroquine
! MOA: unclear, something about 4-aminoquinolines, or DNA, or heme.
Widely distributed, sloooow clearance (months-years)
! Tx: Plasmodium (except "resistance via efflux pump); non-GI amebas
! Side Efx: high doses $ permanent blurred vision + retinal pigment.
! Q: use for prophylaxis? Hallucinations?
o Quinine
! MOA: block DNA synthesis
! Tx: adult Plasmodium; gametes of P.vivax + P.malariae
! More toxic and less effective than chloroquine; used if resistant bug.
Cinchonism: tinnitus, blurred vision, headache, #hearing
Muscle: # heart, dilate BV and uterus
Rifampin causes faster clearance of Quinine
o Quinidine gluconate
! MOA and Tx parallel Quinine; more effective for falciparum.
! Side Efx: anticholinergic ! A-V Block. Use only for severe falciparum
o Halofantrine
! MOA unknown, but do NOT administer w/ food! ("absorption)
! Tx: multi-drug resistant falciparum
! Side Efx: prolonged QT interval; arrhythmias; long elimination time
o Mefloquine
! MOA ~ like quinine and maybe chloroquine (:-P); excreted in bile.
! Side Efx: Gi, vertigo, insomnia, "-blockers, convulsions
o Artemisinins from Chinese herb
! MOA: free radicals damage macromolecules (like iron) in Plasmodium
! Tx: severe Plasmodium, Leishmania, Toxoplasma, Schistosomiasis
o Lumefantrine effective for falciparum w/ #cardiotoxicity, but expensive.
Anti-Parasitic Drugs Assessment 10
$
Tissue schizontocides (liver stage, esp. vivax & ovale)
o Primaquine
! MOA: unknown, 8-aminoquinoline structure
! Tx: prophylaxis; kill gametes, cure vivax and ovale in liver
! only anti-malarial that kills falciparum gametes
! Side Efx: toxicity w/ chronic use; G6PD deficient $ hemolytic anemia
o *Pyrimethamine + sulfadoxine = Fansidar (never used alone)
! MOA: inhibits DHFR
! Tx: Plasmodium; Toxoplasma gondii.
! Side efx: resistance, megaloblastic anemia, bad skin stuff
Drugs to Tx Helmintic (Worm) Infections
Benzimidazoles
! MOA: inhibits microtubule assembly (affinity for parasite tubulin)
! # larval development and immobilize worm $ let go and fall off
! Teratogenic!!!
o Albendazole erratic absorption
o *Mebendazole oral, broad-spectrum nematodes (whip, pin, hook)
Pyrantel Pamoate
o MOA: bind nicotinic receptors $ depolarizing blocade $ spastic paralysis
! side efx in host minimal b/c so poorly absorbed ! stays in GI lumen.
o Tx nematodes, Ascaris, moniliformis
Ivermectin
o MOA: inhibits Glutamate and GABA $ hyperpolarized nerve $ paralysis
o Oral, no metabolism, long t ! , excreted in feces
o Tx: Strongyloidiasis, River Blindness (onchocerca), other nematodes
o Side Efx: GI, itchy, dizzy, allergic/inflammatory rxn to dying bugs
Diethylcarbamazine
o MOA: unknown
o Tx elephantitis
o Side Efx: mild $ anorexia, nausea, headache
Praziquantel
o MOA: " Ca
++
permeability $ spastic paralysis
! ok for humans b/c ""1
st
pass metabolism (#dose w/ liver dz)
o Tx tapeworms, schistosomiasis (not if ocular), other flukes
o Side Efx: GI pain, diarrhea, headache; hepatic metabolism.
A 57-year-old man is brought to the ER. Vital signs include
temperature 103, BP:190/120, HR:184, SOB, confusion and
delerium. Thyrotoxicosis 2 to a thyroid tumor is diagnosed and
propranolol [Inderal] is administered. The purpose of this is to:
A) block parenchymal cell receptors for thyroid hormone
B) block release of hormone from the thyroid
C) inhibit thyroid hormone synthesis
D) lessen the dangerous 2 signs/symptoms of thyroid hormone
excess
E) lower TSH levels
A 62 year-old woman at high risk from osteoporosis is started
on alendronate [Fosamax] therapy. For this drug and the other
bisphosphonates, a serious adverse effect is:
A) Cholelithiasis
B) Esophagitis
C) Fluid/electrolyte loss from extreme diarrhea
D) Hepatic necrosis
E) Renal calcium deposits
Which of the following endocrine / metabolic disorders is
most likely to arise in some patients taking bisphosphonates
for Pagets disease of the bone?
A) Cushings disease (Cushingoid symptoms)
B) Diabetes insipidus
C) Diabetes mellitus
D) Hyperparathyroidism
E) Hyperthyroidism
Pagets disease of the bone can be successfully
treated with a naturally occurring substance called:
A) Calcitonin
B) Cortisol
C) Etidronate
D) Parathyroid hormone
E) Thyroxine
A 73 year-old diabetic is taking oral medication for this
condition. One day she goes without eating for 18 hours
and is brought to the ER in a critical condition with a
blood glucose level of 48 mg/dL. Which of these
potential oral medications most likely contributed to
her present condition?
A) Acarbose
B) Glyburide
C) Metformin
D) Pioglitazone
E) Rosiglitazone
A 57 year-old retired pilot with TB is developing signs
of severe acute adrenal insufciency. This condition
will most likely produce:
A) a moon face
B) dehydration
C) hyperglycemia
D) hypertension
E) hyperthermia
Which of the following endocrine processes can be tested
by the administration of metyrapone?
A) Pancreatic islet alpha cells
B) Pancreatic islet beta cells
C) Pituitary adrenal axis
D) Testicular Leydig cells
E) TSH effects upon thyroid gland function
A 35 year-old woman with systemic lupus erythematosis
abruptly stops taking here glucocorticoids because she
feels well and doesnt want to gain weight. After several
days she presents at the ER, feelin terrible. Which of the
following results would be found if serum from this patient
was analyzed?
A) Elevated ACTH
B) Elevated cortisol
C) Hypernatremia
D) Hypokalemia
E) Hypoglycemia
Leuprolide is used to treat a 75 year-old man with
prostate carcinoma. This drug works by:
A) inhibiting 5-alpha reductase
B) acting as an antagonist at androgen receptors
C) competitively inhibiting LH
D) acting like GnRH
E) acting like testosterone
A 39 year-old woman with a 2-year history of pulmonary and
extra-pulmonary TB collapses while out shopping and is brought
to the ER. She complains of recent weight loss, increasing fatigue
and muscle weakness. Dark spots have appeared over her
knuckles and in her mouth. Signicant clinical signs include:
hyponatremia, hyperkalemia, low plasma aldosterone, high
plasma renin. She fails to respond physiologically to cosyntropin
challenge. Select the most appropriate long-term management
for this individual.
A) ACTH replacement
B) Albuterol
C) Aldosterone
D) Insulin and a glucose infusion
E) Hydrocortisone plus udrocortisone
An adrenal tumor has resulted in Cushings disease in a
47 year-old man. Which of the following drugs would
most likely reduce the signs and symptoms of this mans
disease?
A) Betamethasone
B) Cortisol
C) Fludrocortisone
D) Ketoconazole
E) Triamcinolone
Which of the following corticosteroids has the highest
anti-inammatory potency?
A) Cortisol
B) Dexamethasone
C) Fludrocortisone
D) Prednisone
E) Triamcinolone
A 55 year-old man with benign prostatic hyperplasia and male
pattern baldness seeks help from his physician who replies
that he can certainly help both problems, and with a single
drug! He is thinking of:
A) cortisone
B) estradiol
C) nasteride
D) gonadotropins
E) testosterone
A man with type-2 diabetes is taking combination oral drug
therapy for his condition. If he become hypoglycemic,
ingesting sucrose (sugar) will work less well and take longer
to restore blood glucose levels if he is taking:
A) acarbose
B) glyburide
C) metformin
D) repanglinide
E) rosiglitazone
Propylthiouracil is prescribed for a 32 year-old woman with
Graves disease, a small goiter and mild-to-moderate
symptoms. The patient needs to be followed closely for
which of the following side effects?
A) Agranulocytosis
B) Cholestatic jaundice
C) Gout
D) Renal tubular necrosis
E) Rhabdomyolysis
A 60 year-old man is given pioglitazone to treat his type 2
diabetes. The ability of this agent to lower blood glucose is
based upon it:
A) increasing insulin secretion
B) causing glycosuria
C) increasing target sensitivity to insulin
D) increasing hepatic gluconeogenesis
E) blocking intestinal carbohydrate absorption
Endometriosis in a 27 year-old woman is treated with
danazol. Which of the following is the most likely adverse
effect for which a physician should be monitoring?
A) Anemia from excessive vaginal bleeding
B) Abnormal liver function tests
C) Psychosis
D) Thrombocytopenia
E) Weight loss
Ritodrine infusion is started in a 22 year-old woman in
imminent danger of delivering a premature infant. Which
other drug should be administered prepartum specically for
the purpose of reducing the risks and complications of the
newborns immature respiratory system development?
A) Albuterol
B) Betamethasone
C) Ergonovine
D) Indomethacin
E) Magnesium sulfate
Many insulin preparations contain modications to the
structure of regular insulin. These include recombinant
modications in amino acid sequence, conjugation with
neutral protamine, or addition of zinc. The common result of
each of these modications is:
A) elimination of allergenicity
B) enabling intravenous and subcutaneous administration
C) selective effects on glucose metabolism but no effects on
lipids
D) reactivation of endogenous insulin synthesis and release
E) modulating onset time and duration
A 31 year-old woman is diagnosed with epilepsy and is started
on phenytoin therapy. For several years she has successfully used
an oral contraceptive (estrogen/progestin). Which of the
following is the most likely consequence of adding the phenytoin?
A) Agranulocytosis or aplastic anemia requiring the abrupt
stopping of both medications
B) Breakthrough seizures from increased phenytoin clearance
C) Rapidly appearing phenytoin toxicity
D) A dramatic increase in craniofacial abnormalities in the
developing fetus
E) Reduced contraceptive efcacy
A 23 year-old woman seeks a prescription for an oral
contraceptive and you have to decide between
recommending an estrogen/progestin combination and a
mini-pill comprised only of progestin. You recall that,
compared to combination products, minipills:
A) Have a higher risk of thromboembolism
B) Have direct spermicidal activity
C) Cause more menstrual irregularities (length,
amenorrhea, spotting, etc)
D) Are more effective contraceptives
E) Must be taken on an irregular cycle, rather than daily, so
compliance is an issue
Which of the following adverse or side effects of oral
contraceptives is due to estrogen excess arising from the
estrogen component?
A) Fatigue
B) Hypertension
C) Hypomenorrhea
D) Increased appetite
E) Weight gain
Your 20 year-old patient would like to take an oral
contraceptive but is concerned about the risks of
thromboembolism. Which of the following drugs could you
prescribe that would carry a lower risk of this adverse effect?
A) A combination drug with high estrogen component
B) A combination drug with high progestin component
C) A combination drug with low estrogen component
D) A combination drug with low progestin component
E) A single component, estrogen only product
A 27 year-old woman has hypercortism. It is important to
determine whether cortisol production is independent of
pituitary gland control so you decide to administer a high
potency glucocorticoid to suppress ACTH. You would select:
A) Dexamethasone
B) Hydrocortisone
C) Methylprednisolone
D) Prednisone
E) Triamcinolone
A 67 year-old man with multiple cardiovascular problems is
receiving multiple drug therapy. He complains of muscle aches
and tenderness. Clinical examination reveals myoglobinuria, a rise
in serum creatinine kinase levels and a decline in creatinine
clearance. Which of the following drugs is most likely responsible
for these ndings?
A) Captopril being taken for hypertension and heart failure
B) Nitroglycerin being taken for exercise-induced angina
C) Procainamide being taken to control atrial brillations
D) Atorvastatin being taken for high LDL cholesterol levels
E) Furosemide as adjunctive therapy for congestive heart
failure
Which of the following is ineffective in reducing plasma
triglyceride levels?
A) Rosuvastatin [Crestor]
B) Nicotinic acid [Niaspan]
C) Cholestyramine [Questran]
D) Fenobrate [Tricor]
E) N-3 fatty acids [Max-EPA]
Which one of the following drugs/foodstuffs does
NOT increase the risk of statin-induced myopathy by
interference with the function of the CYPs responsible for
statin metabolism?
A) Nefazodone [Serzone]
B) Ezetimibe [Zetia]
C) Erythromycin [generic]
D) Grapefruit juice
E) Gembrozil [Lopid]
A 35 year old female is found to have hypercholesterolemia.
Total cholesterol is 270 mg/dL, HDL-C is 85 mg/dL, Triglyceride
120 mg/dL, and LDL-C is 161 mg/dL. Other than a positive family
history of coronary heart disease [father and paternal uncles],
she has no risk factors for coronary disease. Her 10/year risk of a
coronary event is < 1% [or < 0.1% per year] based on the
Framingham study calculations. She plans to have several children
over the next few years. Which of the following would you
recommend as the safest initial therapy of her
hypercholesterolemia. with appropriate modication during
pregnancy and lactation?
A) Pravastatin [Pravachol]
B) Gembrozil [Lopid]
C) Nicotinic acid [Niaspan]
D) Simvastatin [Zocor]
E) NCEP (National Cholesterol Education Program) Phase II diet
A 52-year-old Greek immigrant is to receive
primaquine to treat an active Plasmodium vivax
infection. This drug is generally well tolerated, but you
are concerned for an increased risk in this individual
and test for:
A) a normal electrocardiogram
B) creatinine clearance
C) glaucoma
D) G6PD status
E) nystagmus
Which of the following drugs is most appropriate to treat
the exerythrocytic phase of a Plasmodium vivax infection?
A) Chloroquine
B) Primaquine
C) Pyrimethamine
D) Quinidine
E) Doxycycline
Which of the following drugs produces reactive
encephalopathy as an adverse effect and in consequence is
reserved for late stage E. African trypanosomiasis infection
A) Atovoquone
B) Eornithine
C) Melasoprol
D) Metronidazole
E) Paromomycin
Which of the following drugs requires metabolic
activation under anaerobic conditions?
A) Atovoquone
B) Eornithine
C) Mebendazole
D) Metronidazole
E) Pyrimethamine
Key foi Review 1u (1218u8)
# Answei # Answei
1 B 17 B
2 B 18 B
S B 19 E
4 A 2u E
S B 21 C
6 B 22 B
7 C 2S C
8 E 24 A
9 B 2S B
1u E 26 C
11 B 27 B
12 B 28 E
1S C 29 B
14 A Su B
1S A S1 C
16 C S2 B
Drug Abuse Assessment 11
January 2009
"
Drug Abuse Introduction and Miscellaneous
Definitions
o Addiction = compulsive drug seeking behavior and use
! Can be caused by the drug, the user, or the environment.
! Reinforcement: dopamine reward pathway: VTA " nucleus accumbens
" prefrontal cortex
o Tolerance = need # for intoxication OR $ efx with same dose
o Dependence
Marijuana (Cannabis sativa)
o Endogenous " Anandamide & 2-arachidonyglycerol
o From Plants " THC (tetrahydrocannabinol) - psychoactive
! !
9
-THC is more like anandamide
o Rx " Dronabinol & Nabilone
! MOA: 7TM cannabinoid receptors
CB1: brain (basal ganglia + limbic system) + testes
CB2: immune (spleen)
! receptors activate multiple pathways
o # K
+
extracellularly
o Block Ca
++
entering cell (" # Ca
++
extracellularly)
o $cAMP
! Approved Medical Uses
Antiemetic (cancer)
AIDS wasting syndrome
o Side Efx:
! CNS
Acute: $memory, confusion, depersonalization, #hunger,
$REM, $balance, dry mouth
Chronic: amotivational syndrome (apathy, $judgment,
$concentration + memory, etc)
! Cardiovascular: #HR (dose-dependent) " bloodshot eyes
! Immune: $T-cells " $immune response
! Endocrine: $ LH+FSH " $Testo, testes, + libido; $GH, $Prl,
#ACTH
! Respiratory: acute bronchodilates, but chronic constricts
! Tolerance: $receptors; dependence is mild
Withdrawal sx: irritable, nausea, insomnia, sweating
o Hazards
! Psychotoxicity
! Carcinogenic
! Teratogenic
Drug Abuse Assessment 11
January 2009
#
Hallucinogens
o LSD (lysergic acid diethylamide)
Sympathomimetic
Psychedelic hallucinations (colors, loss of time, etc)
Persistent Adverse Rxn: prolonged psychosis, flashbacks
o Mescaline
! MOA: serotonin and dopamine agonist (from the peyote cactus)
! Efx:
Sympathomimetic
Hallucinations, unusual time perception
Adverse: paranoia & fear
o Phencyclidine (PCP, Angel Dust)
! 3 MOA:
NMDA receptor antagonist
! same MOA as Ketamine (Special K) + dextromethorphan
sigma receptor agonist
dopamine/norepi reuptake inhibitor
! Efx:
Sympathomimetic
#sensitivity to stimuli w/ loss of proprioception; restlessness,
disorientation, detachment, anxiety
Adverse: flashbacks, psychosis, dependence, OD
o Natural Derivatives
! Mushrooms: psilocybin + psilocin " like LSD + panic attacks
! Salvia divinorum (mint family) " dissociation from self
o Drugs with Hallucinogenic Properties
! MDMA (Ecstasy)
MOA: blocks NTM reuptake @ synapse
! Cathinone
Physical Efx: HTN, #HR, arrhythima, MI
CNS: insomnia, cerebral hemorrhage
Psychic: hallucinations (visual + auditory), mania, euphoria,
aggressive, anxiety, emotionally unstable
OTC
o Dextromethorphan (Delsym) - cough suppressant; NMDA receptor antagonist
o Dimenhydrinate (Dramamine) tx motion sickness
! can also cause Disorientation, Delirium, and Delusions
Drug Abuse Assessment 11
January 2009
$
Inhalants
o Options
! Volatile Solvents: paint thiner, dry-cleaning, glue, markers
! Aerosols: spray paint, PAM, etc
! Gases: ether, chloroform, nitrous oxide (laughing gas)
! Nitrites: (sexual enhancers)
o MOA: activate dopamine ("CNS depressants)
o Problems
! Neurotoxicity " demyelination
! Motor incoordination
! $immune system (makes AIDS worse)
! Sudden Sniffing Death " cardiac arrhythmias
! Other causes of death: choking, suffocation, asphyxiation
___________________________________________________________________
Nicotine
Nicotine
o Bolus activates addiction. No bolus, no addiction!
o Neuronal receptors: pentameric, ligand-gated w/ subunits #2-#9, $2-$4
Cigarette tobacco
o ##effective drug delivery system large nicotine bolus in <10 sec.
Nicotine Replacemnt Therapies (NRTs)
o nicotine gum (Nicorette)
! Efficacy: o Short-Term: 24% abstinence @ 6 mo
o Long-Term: 18% abstinence @ 1 yr
! Best if used w/ Buproprion
! Suggested termination of use after 6 mo.
o nicotine transdermal patch (Habitrol, Nicotrol, Nicoderm CQ, ProStep)
! Efficacy: 16.8% (double placebo) @ 24 wks
! Overall well tolerated; may have sleep disturbance or skin irritation.
o nicotine inhaler (Nicotrol NS)
! Efficacy: ~25% (~ double placebo) @12 wks
! Goal: disrupt behavioral associations (best if used in combo).
! Side Efx: nasal irritation
! Use >3 mo = useless (no further change)
o low- or no-nicotine cigarettes (Eclipse, Accord, Quest)
! $exposure to smoke-related toxins by heating tobacco w/o burning it.
! Ineffective overall (b/c smokers dont want to use them)
o Smokeless tobacco (Snus)
! somewhat similar to snuff
! Efficacy: works in Sweden.
Drug Abuse Assessment 11
January 2009
%
Non-nicotine cessation compounds
! Regardless of which drug is used, abstinance > 1 yr is low (~10%)
! In contrast to other drugs, the more times you try to quit, the more successful youll be
o Buproprion (Wellbutrin, Zyban)
! MOA: unknown, but has anti-depressant efx
! Efficacy:
60% abstinence @ 9 wks (double placebo)
24% abstinence @ 1 yr (4x placebo), esp in combo.
! Side Efx: well-tolerated, $potential for abuse, BUT beware CYP450!
Do NOT give w/ $B, tricyclic antidepressant, seizures, anorexia
o Barenicline (Chantix)
o Mecamylamine
! MOA: non-selective antagonist at non-#7-nicotinic cholinergic
receptors " crosses BBB " #risk side efx (in clinical trials)
! Efficacy: inconclusive
o Rimonabant
! MOA: CB1 antagonist
! Efficacy: yes short term, but not more than other tx. Try as 2
nd
line?
! Side Efx: severe depression
o Clonidine our old anti-hypertensive friend; also a 2
nd
line quitter drug
! MOA: #2 agonist; crosses BBB, t! ~ 1hr
o Nortriptyline a Tricyclic Anti-Depressant
! MOA unconfirmed but blocks NorEpi; crosses BBB; long t !
! Efficacy: highest in depressed pts.
o Vaccines
! MOA: Abys trap nicotine in plasma "cant cross BBB to reward center
! Efficacy: lasts just a few months " only tx initial quitting, or relapse.
Therapeutic Potential: Epibatidine " pain reduction
Drug Abuse Assessment 11
January 2009
&
Alcohol
Alcohols
o Ethanol
! MOA: alters ion channels
! Zero-order kinetics
! Metabolized in Liver:
1 = alc. dehydrogenase
2 = ALDH (inactive in 50% of Asians)
! Side Efx:
CNS tolerance develops (but not liver " toxic)
CNS damage:
o BeriBeri/Werkicke-Korsakoff " thiamine deficiency "
peripheral neuropaty
o Cerebellar degeneration " ataxia
o Central Pontine Myelinolysis " dysarthria, confusion
o Marchiafava-Bignami Syndrome " apathy, dementia
o Pellagra = niacin deficiency " Dermatitis, Diarrhea,
Dementia, Dizzyness, and Depression
Hepatomegaly " encephalitis, esophageal varices
Acute vasodilation
Cardiomyopathy
# gastric damage of NSAIDs " ulcers + gastritis
! also sensitizes pt to acetaminophen toxicity.
Pancreatitis
Anemia + Immune suppression
Fetal Alcohol Syndrome (inhibition of cellular proliferation)
Women have $1
st
pass metabolism " # [blood alcohol]
Cross-tolerance w/ barbiturates + benzodiazepines
! Withdrawal:
Early: agitation, confusion, hyperactive autonomics, seizures
Late: delirium tremens " hyperthermia, hallucination, coma
'()* +"," -./(012/342/ +#," -./(0(/ " 5)# 6 *#)
Drug Abuse Assessment 11
January 2009
7
o Methanol (wood alcohol)
! Oxidized like Ethanol but yields formaldehyde
! Result: blindness, irreversible acidosis " death
! Tx: ethanol + dialysis
o Isopropanol (rubbing alcohol)
! Oxidized to acetone (ie, a desperate second choice)
! Result: #CNS toxicity, severe gastritis, nausea, pain
! Tx: hemodialysis
Tx CNS Alcohol Toxicity
o Thiamine "
Tx Chronic Alcoholism
o Naltrexone " opioid receptor antagonist; helps $ relapses
o Ondansetron " 5-HT
3
antagonist; helps $ craving
o Acamprosate " NMDA-R antagonist (no studies in US); helps $ relapses
! Reduce dose w/ renal insufficiency
o Topiramate " AMPA-R antagonist & GABA-R modulator
! Adverse efx " titrate dose
o Disulfiram " acetaldehyde dehydrogenase antagonist " # [acetaldehyde]
" same thing as a bad hangover. (It also blocks NE synthesis)
! Acetaldehyde syndrome: #HR, flushing, hypotension, N/V, headache
! No efx on craving
! Side Efx: hepatotoxicity, depression, psychosis
Tx Alcohol Withdrawal
Rx Tremulousness Sx Seizures Delirium Tremens
Benzodiazepines
% % %
Atenolol
%
%
Clonidine
%
Phenytoin
%
Drug Abuse Assessment 11
January 2009
8
Toxicology
Some general methods of decontamination
o SDAC = Single Dose Activated Charcoal
! Tx oral toxin ingestion via ##SA (protect airway)
! NOTE: no evidence of improved outcome
o Ipecac " promotes emesis; but no evidence of improved outcome.
! Side Efx: dehydration, cardiotoxicity
o Gastric Lavage
! Side Efx: perforation, aspiration
o Whole Bowel Irrigation w/ isotonic fluid " rapid elimination of gut contents
o Hemodialysis " only if toxin is watersoluble
! Ex: methanol, ethylene glycol, salicylates, lithium, sotalol.
o Hemoperfusion = pass blood through charcoal cartridge filter
! Ex: carbamazepine, Phenobarbital, phenytoin, theophylline
How does the poisoned patient die? (slide 31)
Supportive Lab Tests " anion gap = Na Cl HCO
3
Nerve gas carbamate herbicide intoxication ?
National Poison Control Center: 1-800-222-1222
Toxin Antidote
Acetaminophen
Sx: appear after 24hrs " RUQ pain
Death: hepatic failure
N-acetylcystine
When: <10 hrs
MOA: replace liver enzyme (?)
Adverse: N/V, bad taste, anaphylaxis
Aspirin (acetylsalicylic acid)
Sx: N/V, tinnitus, sweating "
lethargy + respiratory failure "
resp.alkalosis " metab.acidosis "
more ASA crosses BBB " worse
Death: neurologic decline
Tx options:
Charcoal (bad choice?)
Fluids + dextrose
Na-Bicarb " ionizes drug " no BBB
Hemodialysis
Benzodiazepines
Sx: drowsy, confused, incoordinated
Death: if taken w/ alcohol
Supportive Care = 1 choice
Flumazenil - not routinely used
N/V, dizzy, panic attack, seizures
Barbiturates
lethargy"" resp. depression + shock
Phenobarbital & Aprobarbital
ABC = airway, breathing, circulation
tx via urinary alkalinization (ion trapping)
Drug Abuse Assessment 11
January 2009
9
$-Blockers & Ca
++
-channel blockers
BB Sx: $HR, hypoTN, QRS widening,
seizure, $resp, hypoglycemia, #K
+
CCB Sx: $HR, AV block (Verap + Dil)
Vasodilation (-pine)
If immediate release " gastric lavage
If sustained release " whole bowel
Atropine for bradycardia
Glucagon reverses $contractility + HR
NorEpi for vasopressor
Digoxin
Sx: malaise, vomiting, abd. pain,
arrythmias
Digibind
Corrects hyperkalemia
but #serum [digoxn] (from tissues)
Opioids (Rx or Street)
Sx: unconscious, resp. depression
Supportive Ventilation = 1 choice
Naloxone reverses resp. depression
but can cause withdrawal sx.
Tricyclic Antidepressants (TCA)
Sx: w/in 2hrs; cardiotoxic, seizures
Charcoal + gastric lavage
Bicarb: #pH displaces drug from Na
+
channels
Vasporessor + IV fluids
Theophylline
Tachycardia, vomiting, hypoTN,
seizures if blood levels really high.
Supportive Care
Aggressive gut decontamination + $B
Hemodialysis if blood levels really high
Anti-Cholinergics
Sx: flushed, dehydrated, delirious,
tachycardia, pupils dilated
Supportive care
Physostigmine (in small doses IV;
beware heart block + seizures)
Intoxication by Gas
Gas Toxicity Sx + Tx
CO Binds Hgb " $O
2
capacity
Sx: headache, N/V, seizures
Tx: 100% O
2
Irritants: chlorine,
ammonia, sulfur dioxide
Corrosive efx on #+$
airways
Sx: cough, stridor, pneumonia
Tx: O
2
+ bronchodilators
Cyanide Blocks O
2
binding Sx: headache, N/V, seizures
Tx: antidote kit (nitrite + thiosulfate)
Hydrogen Sulfide Similar to Cyanide Sx: cyanide + smell of rotten eggs
Tx: nada
Nitrogen oxides Methemoglobinemia Sx: Dyspnea, cyanosis, syncope, seizure
Tx: methylene blue
Hydrocarbons (solvents) Sx: cough/choke, headache, lethargy
Tx: ABCs, supportive care
Drug Abuse Assessment 11
January 2009
:
Insecticides & Herbicides
Insecticides + Nerve Gas
Organophosphates:
o Diazinon
o Malathion
o Parathion
Atropine + Supportive Tx
Pralidoxime (2PAM)
Caustic Acids & Alkalis (slide 66) not on drug list
Heavy Metal Poisoning (slide70)
Lead
Sx: colic, constipation, anemia, $fxn
proximal tubule, encephalopathy
Chelators $ [blood]; do not reverse damage
Succimer " for mild cases
Dimercaprol " for severe cases
Arsenic
Source: herbicide, paint, insecticide,
electrical manufacturing
Acute Sx: N/V, colic, psychosis, rash,
cardiomyopathy, seizures
Chronic Sx: Mees Lines (nails), hair
Dimercaprol (in peanut oil) = 1 choice
nephrotoxic; beware G6PD deficiency
Succimer
hydration important b/c renal exretn
Mercury Succimer
Copper Penicillamine
use $ b/c of toxicities (slide 83)
Iron
MOA: impairs Ox-Phos " cell death
Sx: hematemesis, diarrhea " liver
damage, metabolic acidosis, GI scar
Deferoxamine = 1 choice IV
MOA: chelates iron
Sx: red urine, #HR, hypoTN, fever
Deferasirox: tx transfusion pts w/ #iron
Sx: diarrhea, headache, cough
Venom
Rattlesnake
Dx: fang marks, local tissue damage
Sx: hemorrhage, ecchymosis,
necrosis, inflammation, coagulopathy
Anti-Venom = CroFAB
Brown Recluse Spider
Venom: sphingomyelinase D2
Sx: pain, itchy, enlarging blister
Most bites resolve w/out tx.
(anti-venom use questionable)
Black Widow Spider
Venom: #-latrotoxin binds ion
channels " affects Ach
Sx: hours later muscle cramping,
headache, anxiety, fatigue, insomnia
Tx:
Anti-spasmodics (benzos)
Opiates
Anti-venom (high-risk pts only)
Drug Abuse Assessment 11
January 2009
";
Sedatives & Hypnotics
Vocab Basics
o Sedative = $ excitement
o Hypnotic = # drowsiness
Benzodiazepines, in general:
o MOA: #freq. of Cl
-
channel opening " enhances GABA
A
-receptor-induced
#Cl
-
channel opening " #postsynaptic inhibition.
! Membrane hyperpolarization
! Absorbed rapidly, cross BBB, and do not induce CYP450.
! # anxiolytic; $ fatal CNS depression " high therapeutic index &
! all benzos are equally effective
o Tx: Anxiety Disorders, Panic Disorder, Acute Stress.
o General Efx:
! Sedation
! Anti-convulsant
! Muscle relaxation (via CNS) " not for Myasthenia Gravis pts!
! Amnesia
! Sleep " $awakenings, #stage 2, $stage 3+4, #bizzare dreams
! beware rebound insomnia
! Withdrawal: anxiety, insomnia, irritable, panic, anorexia. (slide 17)
! must taper dose if used many weeks
o Contraindications:
! sleep apnea "
! alcohol consumption " potentiates depression (deadly)
! pregnancy + lactation
! Drugs that # Benzo efx: ($metab.) cimetidine, disulfriam, & estrogen
! Drugs that $ Benzo efx: antacids & rifampin
Short-Acting Benzos " worse chance for rebound anxiety + insomnia
o Midazolam [Versed] full agonist; t! = 2 hr
! no active metabolites
! Use: conscious sedation; adjunct anesthesia; skeletal muscle relax.
! Side Efx: hypotension, headache, amnesia.
o Alprazolam [Xanax]
o Lorazepam [Ativan]
o Oxazepam [Serax]
o Triazolam [Halcion]
! Pros: less daytime sedation b/c fast acting
! Cons: more frequent amnesia & rebound insomnia; hostility at #doses
Drug Abuse Assessment 11
January 2009
""
Long-Acting Benzodiazepines " worse chance for day after hangover
o Diazepam [Valium]
o Chlordiazepoxide [Librium]
o Flurazepam [Dalmane] hypnotic; sedation hangover especially notorious
o Clonazepam [Klonopin]
The Z drugs
! # abuse potential " limit use to 2-3 nights
! reduce dose 50% if elderly or pregnant
o Zolpidem [Ambien]
! MOA: not a benzo! It acts at omega-1 benzo receptor
Short-acting (~2 hr)
No active metabolites (true for all 3 Z drugs)
! Efx:
Hypnotic + sedative
NO anticonvulsant/muscle relaxing efx.
Well tolerated in elderly
# sleep time but NO CHANGE in sleep architecture (<20mg)
worsens sleep apnea
o Zopiclone [Lunesta] "
o Zaleplon [Sonata] "
Discussed but not on drug list (NODL):
o Flumazenil (Romazicon) " benzo competitive antagonist @ GABA-A receptor
! Use: reverse benzo sedation; VERY short t!
o Temaepam (Restoril) " intermediate duration benzo for hypnotic
o Estaolam (ProSom) " intermediate duration hypnotic (slide 30).
Other hypnotics slide 39
o Chloral Hydrate (NODL) only works short term b/c dependency/tolerance
o Diphenhydramine (Benadryl) our anti-histamine friend is also a sedative!
o Doxylamine (Unisom) OTC anti-histamine
o Hydroxyzin (Vistaril) Rx anti-histamine
! causes drowsiness, but not effective for insomnia
o Melatonin (NODL) jet lag, etc
o Valerian (NODL) - ## sedation
Drug Abuse Assessment 11
January 2009
"#
Anti-Depressants and Mood Stabilizers
Pharmacology of Depression: adaptive changes in monoamine signaling (NE, 5-HT)
BLACK BOX WARNING: # risk of suicide in kids + adolescents
Tricyclic Antidepressants (TCA) " gold standard. Newer drugs
! MOA: inhibit reuptake of ("potentiate) NE + 5-HT @ presynaptic terminals
- potentiates NE + 5-HT
- also block mAch, 5-HT, & histamine receptors " side efx.
o #-adrenergic antagonism " othostatic hypotension
o mAch antagonism " tachycardia, confusion, $ fluid (dry eye,
constipation, urinary retention).
o Histamine + #-AR antagonism " sedation
- Other Side Efx: arrhythmia, worse CHF, acidosis, delerium, seizures
- Potentiated by alcohol = bad combo
o Amitriptyline (Elavil)
o Imipramine (Tofranil)
o Nortriptyline (Pamelor)
o Clomipramine (Anafranil)
o Desipramine (Norpamin)
o Doxepin (Sinequan)
o Protriptyline (Vivactil)
o Trimipramine (Surmontil)
Atypical Antidepressants (2
nd
+ 3
rd
generation) heterocyclics
o Amoxamine mixed inhibition of NET>SERT~DAT
! Use for depression in psychotic patients (b/c analog of loxapine)
o Maprotiline (Ludiomil) NorEpi reuptake inhibitor (NRI)
! # risk of seizures
o Bupropion (Wellbutrin) weak blocker; active metabolite blocks NE reuptake
! Side Efx: anxiety, restlessness, seizure; can aid smoking cessation
o Venlafaxine (Effexor) Serotonin & NorEpi Reuptake Inhibitor (SNRI)
! No TCA-like side efx! Does have mild HTN. Short t! (~5 hr).
o Duloxetine (Cymbalta) most potent SNRI
! CYP metabolism; t ! ~12 hr; 95% protein bound
Drug Abuse Assessment 11
January 2009
"$
o Mirtazepine (Remeron) - enhances release of serotonin & NE by
antagonizing presynatpic #2-ARs
! also has anti-histamine axn " sedation
! # wt. gain, but less GI + sexual problems than SSRIs.
o Trazodone (Desyrel) & Nefazodone moderate 5-HT reuptake inhibitors
! use to tx depression w/ sleep disturbance & anxiety
! inhibit CYP3A4
Selective Serotonin reuptake inhibitors (SSRI) " potentiate serotonin
! first-line tx for major depresion
o Efx: initial CNS stimulation, euphoria " after a few weeks, sx improve
! High therapeutic window; overall fewer side efx
Adverse Efx: nausea, $ libido
Bad idea if you take it with a MAOI " Serotonin Syndrome
o Serotonin Syndrome = overstimulation of 5-HT1A in midbrain
! Sx: #temp, hyperreflexia, tremor, myoclonus, agitation, seizures,
confusion, delerium, cardiovascular collapse, coma, death
! Tx: discontinue medication immediately!
o Citalopram (Celexa)
o Fluoxetine (Prozac) t! ~ a week
o Fluvoxamine (Luvox)
o Paroxetine (Paxil) teratogenic!
o Sertraline (Zoloft)
Monoamine Oxidase Inhibitors (MAOI)
! only use if other anti-depressants havent worked, or to tx panic disorder
! Tranylcypromine (Parnate)
! Isocarboxazid (Marplan)
! Phenelzine (Nardil)
o MOA: irreversibly inhibit oxidative metabolosm of monoamines (NE, 5-HT)
! t! = 1-3 weeks!
o Efx: initial CNS stimulation, euphoria " after a few weeks, sx improve
o Adverse Efx: orthostatic hypotension, sleep disturbance; dont eat cheese.
Mood Stabilizers " tx Bipolar (Manic Depression)
o Lithium DOC, but rapid t! w/ NARROW tx window!!
o Valproate (Depacon) anti-convulsant; helps both phases of Bipolar.
o Carbamazepine (Tegretol) anti-convulsant
1. 2.
3. 4.
5. 6.
7. 8.
9. 10.
11. 12.
13. 14.
15. 16.
17. 18.
19. 20.
21. 22.
23. 24.
25. 26.
27. 28.
29. 30.
31. 32.
33. 34.
35.
Different Rx
select for
different
mutations of
reverse
transcriptase
Anti-Virals
Disclaimer: some of these facts were taken from the HIV Micro lecture.
Retrovirus (HIV)
Fusion Inhibitors ! no viral entry into host cell
o Enfuvirtide binds gp41 of viral envelope ! no zipping
" SubQ 2x/day (inconvenient)
" # risk pneumonia
" Resistance develops, but no cross-resistance w/ other drugs
" Only for tx-experienced pts failing HAART
o Maraviroc CCR5 antagonist (a chemokine receptor on macrophages)
" needs CYP3A4 (beware drug interaxns)
" resistance via P-Glycoprotein pump
" works well BUT only against the R5 serotype
" Side Efx: cough, rash, dizziness, liver and cardiac problems.
Nucleoside Reverse Transcriptase inhibitors (NRTI)
! analogs of nucleosides act as competitive inhibitors ! block elongation.
This helps protect uninfected cells (tough luck if already infected)
! all nucleosides must be phosphorylated x3 for efx
" Zidovudine pyrimidine (T), aka AZT; $ perinatal transmission, gets
glucaronidated, avoid fat meal, myelosuppression
" Stavudine pyrimidine (T) worst side efx (above) PLUS
peripheral neuropathy, pancreatitis
" Lamivudine pyrimidine (C)
" Didanosine purine (A,G) dont take w/ food; diarrhea,
peripheral neuropathy, pancreatitis
" Abacavir purine (G) EtOH dehydrog. metab. ! beware genetics
! all can cause GI distress, & lactic acidosis due to mitochondrial toxicity
Non-nucleoside reverse transcriptase inhibitors
! allosteric binding causes conformational change in active site ! no synth.
(Note that this does not require Phosphorylation)
! Side Efx: maculopapular rash
o Delavirdine CYP450 inhibitor.
o Nevirapine CYP450 inducer ! fever, fatigue, nausea, hepatotoxic.
o Efavirenz CYP450 inducer ! neuropsychiatric, teratogenic.
(more anti-retroviral drugs)
Nucleotide Inhibitor ! Tenofovir inhibits reverse transcriptase
o only requires 2 phosphorylations for efx. Oooooh.
o Side Efx: N/V, diarrhea, weakness, GI upset, # liver enzymes
Integrase Inhibitor ! Raltegravir HIV cant get into host genome
o Only for tx-experienced pts
o orally bid (t! = 9hr)
o Metabolism: glucaronidation in liver (not CYP450)
Protease Inhibitors
! most effective ART available! (-navir)
! selective, competitive inhibitors of protease binding site
! no cleavage ! no viral maturation ! no infectious particle
! each drug selects for different mutations in specific protease codons
" General Side Efx:
Hyperlipidemia
GI distress: vomiting, diarrhea
Diabetes
Lipodysrophy = fat wasting and redistribution
Many drug interactions b/c inhibit CYP3A4 (slide 43)
Oral bioavailability varies widely
o Lopinavir just your run-of-the-mill PI - Like other PIs, it has high plasma
protein binding & low renal excretion b/c CYP metabolism
o Atazanavir hyperbilirubinemia ! jaundice + heart block
o Ritonavir potent CYP inhibitor ! used to # plasma [drug] of other ARTs.
" Hepatotoxic at high doses (go figure)
o Saquinavir lowest CYP inhibition maybe best choice for interaxns
o Indinavir alopecia, kidney stones, notorious lipodystrophy
o Nelfinair ## efx if taken w/ meal
o Amprenavir not on drug list and manufacture is discontinued.
Herpesvirus Drugs (Herpes Simplex, Varicella, Cytomegalovirus) ! cyclovir
! acyclic nucleoside analogs that inhibit viral DNA polymerase ! chain termination
! require activation via (P) by viral thymidine kinase = magic bullet
! doesnt work if virus mutates its DNA polymerase or doesnt have TMK.
Acyclovir purine analog headache, nausea, diarrhea (renal+CNS toxic @ #dose)
Valcyclovir purine analog, acyclovir prodrug (orally hydrolyzed)
Ganciclovir w/ Valganciclovir 100x # potency than acyclovir ! tx CMV retinitis
o Take together b/c valganciclovir is a prodrug activated by ganciclovir
o Side Efx: myelosuppression, teratogenic
Famciclovir prodrug form of penciclovir
Penciclovir - guanine analog ! competitive inhibitor ! no chain termination
o Can also be used against HBV post liver transplant
o Best bioavailability (~70%)
Cidofovir cytidine nucleotide analog; use if acyclovir resistant b/c
o worse side efx: Nephrotoxic, neutropenia, carcinogenic
Foscarnet pyrophosphate analog ! inhibits DNA polymerase by blocking cleavage
o Side Efx: nephrotoxic, N/V, anemia, fatigue
Hepatitis B + C
Adefovir nucleotide adenosine analog ! inhibits viral DNA polymerase
o Side Efx:
" rebound hepatitis with discontinuation
" nephrotoxicity (b/c low protein binding ! renal excretion)
" lactic acidosis ! severe hepatomegaly w/ steatosis
Lamivudine use in combo w/ adefovir # potency; ok to use w/ liver problems
Interferons - activates Jak-Stat ! anti-viral, anti-immune, anti-proliferative.
o Also can Tx Kaposi Sarcoma
o Side Efx: myelosuppression, N/V, neurotoxic, # serum creatinine
" Micro says it can also cause alopecia & depression/suicide.
Ribavirin competitively inhibits GTP 5 capping of viral mRNA
o Side Efx: hemolytic anemia, teratogenic.
o Works better with specific HCV genotypes (2+3) (micro)
Influenza Virus
Uncoating Inhibitors ! block HA glycoprotein binding ! no internal acidification
o Amantadine -
o Rimantadine -
" These work on Influenza A only
Viral Release Inhibitors ! inhibit viral neuraminidase ! no cleavage of sialic acid !
no detachment from host cell ! reduce viral spread %
o Zanamivir low oral bioav
o Oseltamivir -
" These work on Influenza A & B.
Review:
Hey, thats handy
- all drugs ending with -fovir are nucleoTIDE analogs
- protease inhibitors (-navir) are SNARLIng ! imagine a mean protein w/
lipodystrophy
Anti-Psychotic Drugs - Used to tx: Psychosis, Depression, Anxiety, and Mania
Typical Anti-Psychotic Drugs
! MOA: inhibition of Dopamine (D2) receptor binding And others, too.
Phenothiazenes
o Chlorpromazine oldest; aliphatic side chain ! low potency
! side efx: anti-diuretic, ! insulin, jaundice
o Triflupromazine - aliphatic side chain ! low potency
o Thioridaine piperdine ring
o Mesoridazine - piperdine ring
o Fluphenazine piperazine group ! "potency
o Trifluroperazine piperazine group ! "potency
Thioxanthenes:
o Chlorprothixene - aliphatic side chain ! low potency
o Thiothixene - piperdine ring
Benzepines: Loxapine potent
Butyrophenones: Haloperidol "" potency
Indolones: Molindone & Oxypertine potent
Other: Butaclamol -
Atypical Anti-Psychotic Drugs
! MOA: " 5-HT2 affinity (low D2 affinity) # inhibition
! " risk Type2 DM (and can " mortality in alzheimers? Slide 9)
Clozapine low potency; beware blood dyscrasis w/ leucopenia prodrome
o Olanzapine
o Quetiapine
Risperidone 5-HT2/D2 antagonist, but limited EPS at low doses
o Only approved agent for children + teens
Paliperidone active metabolite of Risperidone
Ziprasidone 5-HT2A, 5-HT1A, 5-HT2C/D2 antagonist; limited EPS
Aripiprazole 3 MOA (below) with fewer side efx
o D2 partial agonist (! !axn of full agonist)
o 5-HT2A antagonist
o 5-HT1A partial agonist
Pharmacokinetics (slide 30)
lipophilic & protein-bound # "bioav. If IM injection AND crosses placenta/milk
peak efx in ~2 hrs, efx last 24hrs, but elimination ~30hrs ! once daily dosing.
Potential Side Efx
General: Neuroleptic Syndrome
o Suppression of spontaneous movements and complex behaviors
o Reduced initiative + interest in environent
o Decreased manifestations of emotion or affect
o Psychotic symptoms disappear over time
CNS Efx
o Cerebral Cortex: ! seizure threshold (esp !potency phenothiazines)
o Basal Ganglia: (tolerance builds over time)
$ EPS= Extra-Pyramidal Symptoms
Acute Dystonia muscle spasms, facial grimacing, torticollis
Akathesia ants in my pants
Parkinsonian Syndrome - ! movement, masked face, tremor
Neuroleptic Malignant Syndrome rare (slide 39) " mortality
Perioral Tremor rare rabbit syndrome
Tardive Dyskinesia tic-like movements; no tx just stop Rx.
$ " DA metabolism
$ " Ach turnover # Ach sx: dry mouth, blurred vision, constipation,
orthostatic hypotension (see heart)
o Limbic System: site of anti-psychotic effects
o Hypothalamus: " prolactin secretion; no tolerance develops
o Brainstem: respiration OK; ! reflexes; no N/V b/c "DA at CTZ
Renal chlorpromazine may be antidiuretic
Liver may worsen liver dz
Endocrine - " risk of Type 2 Diabetes with Atypical drugs
Heart orthostatic hypotension (yes tolerance)
o More efx: chlorpromazine, thioridazine
o Less efx: haloperidol, loxapine, risperidone
Mild Physical Dependence: malaise, difficulty sleeping
Skin: urticaria, photosensitivity
Weight Gain
Drug Interactions
Drug Choice based on trial-and-error side efx.
Misc. Uses: N/V, alcohol hallucinations, movement disorders (Tourettes, Huntingtons,
intractable hiccups)
Anti-Epilepsy Drugs
! lessen symptoms but do not cure disease
! mono-therapy is recommended (and start w/ low dose) b/c of so many drug interactions
! " suicide risk w/ these drugs
Type of Seizure 1
st
Choice 2
nd
Choice
Partial (simple or complex)
! simple = retain consciousness
! complex = LOC
Carbamazepine Phenytoin, Valproate,
Lamotrigine, Gabapentin,
Zonisamide, Levateracetam
Tonic-Clonic (grand mal) Carbamazepine Phenytoin, Valproate
Absence (petit mal)
! 3 Hz spike
Ethosuximide Valproate, Lamotrigine
Myoclonic, Atonic, Atypical Absence Valproate Lamotrigine, Clonazepam
Status Epilepticus Diazepam (I.V.) Lorazepam, Phenytoin
Refractory generalized seizure Clonazepam
Hydantoins
o Phenytoin stabilizes inactive Na
+
channels.
# Narrow Window: nystagmus, ataxia, arrhythmias ("dose), coarsened
face, hirsutism, gingival hyperplasia, peripheral neuropathy, teratogenic
o Fosphenytoin water-soluble phosphoester of phenytoin ! parenteral
# Arrhythmias, esp in elderly
o Methphenytoin prodrug ! nirvanol (active).
# Worse side efx than Phenytoin.
o Ethotoin use for pts hypersensitive to phenytoin. Less efx.
Barbiturates
o Pehonbarbital
# MOA: prolong opening of GABA receptor ! Cl
-
flux
# Side Efx: sedation, lethargy, nystagmus, rash, megaloblastic anemia (b/c
folate $), VitD $
o Mephobarbital N-methyl Phenobarbital, demethylated in liver to active form
o Primidone rapidly converted to Phenobarb + active metabolite (PEMA).
Iminostilbenes
o Carbamazepine inhibits Na
+
channel recovery
# also used to tx HD
# most likely to reduce clinical efficacy of concurrent Rxs
# Side Efx: blood dyscrasias, N/V, diplopia, ataxia, drug interactions
o Oxcarbamzepine inhibits Na
+
channel recovery
# Less potent (and less toxic) than Carbamazepine.
Succinimides DOC for absence seizures
o Ethosuximide inhibits T-type Ca
++
channels ! prevents 3 Hz spike/wave
# Side Efx: N/V, lethargy, dizziness, euphoria, hiccups, fatigue, tolerance
o Phensuximide
Branched-Chain Carboxyllic Acid = Valproic Acid (Valproate)
o 3 MOA:
# stabilizes inactive Na
+
channels (like Phenytoin)
# $ Ca
++
current (like Ethosuximide)
# stimulates GABA synthesis + inhibits GABA degradation
o Side Efx: nausea, abdominal pain, heartburn, liver toxicity, teratogenic
Benzodiazepines
# MOA: " ease of opening the Cl
-
channel ! potentiate GABA receptor
# Side Efx: sedation, lethargy, tolerance
o Clonazepam - tx refractory generalized seizures
o Diazepam (Vallium) DOC Status Epilepticus
o Lorazepam longer acting than diazepam
Miscellaneous
o Gabapentin " GABA axn (analog). Mild side efx: dizzy, ataxia
o Lamotrigine slows recovery of Na
+
channels; adjunct; 1% get Stevens-Johnson
o Levetiracetam MOA unknown; mild side efx
o Tigabine " GABA b/c inhibits reuptake. May make absence seizures worse.
o Topiramate inhibits Na
+
channels & $ Ca
++
current. Kidney Stones.
o Felbamate " GABA & inhibits NMDA. Adjunct drug. Aplastic Anemia = bad.
o Zonisamide - inhibits Na
+
channels & $ Ca
++
current. Broad spectrum axn.
Comparing Pharmacokinetics its like masochism, only for a grade.
Drug Bioav. Onset t! Albumin Metabolism Drug Interaxns
Phenytoin varies 3-12 hr
12-36
hrs.
High
Dose-Dependent
CYP2C9
Induces CYP 2C + 3A;
Valproate, Warfarin,
Oral Contraceptn $
Barbs
100%,
slowly
5 days 50% CYP2C9
Induces CYP2C +UGT
Oral Contraceptn $
Carbamazepine 100% 6-8 hr 30 hr 70% CYP2C9
Induces CYPs + UGT
MANY INTERAXNS.
Ethosuximide 100% 3-7 hr 40 hr no Glucaronidation Valproate
Valproate 80% 2 hr
9-18
hrs
high
affinity
UGT + oxidation
Inhibits UGT (itself).
Inhibits CYP2C9.
Protein binding.
Benzos Good Rapid 40 hr binds active products
Drugs to Tx Neurodegenerative Disorders
Alzheimers Disease
Problem: not enough Ach (also low levels of 5-HT + NorEpi)
Solution: reversible CNS Acetylcholinesterase inhibitors!
o Tacrine dont use it b/c !bioav. and " side efx: hepatotoxic.
o Donepezil (Aricept) long t! = 70hr
o Rivastigmine short t! = 1.5 hr
o Galantamine medium t! = 7 hr
o Side Efx: N/V, diarrhea, insomnia (wild dreams), bradycardia.
The other Problem: too much glutamate (excitotoxic)
The Solution: block NMDA-type glutamate receptors!
o Memantine (NaMenDA) low affinity for NMDA (100% bioav.)
# allows normal hippocampus activity but blocks excitotoxic levels.
# Side Efx: confusion, headache, insomnia, agitation cystitis, "libido
Huntingtons Disease
Problem: trinucleotide repeat expansion of CAG (more = worse) $ loss of
cholinergic & GABAergic neurons in striatum (basal ganglia) $ "indirect path
! this is, like, the opposite of Parkinsons
Rx for depression
o Fluoxetine (Prozac) & Carbamazepine
Rx for chorea $ anti-pychotics with extra-pyramidal (! parkinsonian) side efx
o Reserpine depletes CNS dopamine stores
o Tetrabenazine degrades DA
o Chlorpromazine DA antagonist
o Haloperidol DA antagonist
Amyotrophic Lateral Sclerosis (ALS)
Problem: impaired glutamate reuptake ! too much
glutamate ! excitotoxicity
Riluzole CYP450 metabolism, t! = 12hr
o Side Efx: nausea, fatigue, sedation, liver dz
Multiple Sclerosis (MS) ! autoimmune abys attack myelin sheath
Interferon "-1# - anti-inflammatory restores BBB ! ! [cytokines] in CNS
Natalizumab anti-inflammatory, more effective than Interferon, BUT
o Side efx: progressive multifocal leukoencephalopathy.
Glatiramer myelin decoy; beware injxn site rxns
Mitoxantrone anti-neoplastic
Alemtuzumab anti-neoplastic - Aby against CD52 on T-cells
3 MOA $ reduce glutamate
1. block inactive Na-channel
2. block activated Ca-channel
3. block NMDA channel
Parkinsons Disease damage to Dopamine-producing cells in the substantia nigra
! less DA ! inhibitory D2 receptors in basal ganglia dont get stimulated
! failure of inhibition ! failure of fine-tuning ! bradykinesia + hyporeflexia
The 5 main strategies for the treatment of Parkinsonism
Dopamine Replacement Tx ! " [DA]
L-DOPA (Levidopa) converted to DA by endogenous L-AAD
o First-line tx for Parkinsons but wait till sx appear cuz only works 3-5 yrs.
o Adverse Efx: N/V, anorexia, orthostatic hypOtension, Afib
L-DOPA + Carbidopa (Sinemet) peripherally inhibits L-AAD (cant cross BBB)
o 75% more effective per gram!
o Adverse Efx: depression, anxiety, delusions, chorea, on-off phenomenon
o Interactions: Vit.B6, MAO-I, glaucoma, psychosis, ulcers
DA Receptor Agonists ! counteract that inhibition failure
o These drugs are best for early Parkinsons Dz tx.
Bromocriptine D2 agonist D1 partial agonist
Pergolide D1/D2 agonist more effective than Bromocriptine
Pramipexole D2 selective free radical scavenger?
Ropinirole D2 selective CYP450 metab.
Enhancement of DA Release
Amantadine antiviral w/ unknown MOA; efx are modest & short-lived.
o Adverse Efx: restless, depression, psychosis seizures, heart failure
Inhbition of DA metabolism
MAO-B inhibitors ! retard breakdown of DA
o Selegiline interacts w/ TCA, SSRIs, meperidine (opioid), & L-DOPA
o Rasagiline new, more potent axns
# Use these in pts w/ $ response to L-DOPA. (Minimal efx used alone).
COMT inhibitors ! prolong axn + bioav. of L-DOPA & prevent its fluctuations
o Entecapone - peripheral only; preferred over Tolcapone
o Tolcapone peripheral + central axn; beware liver failure.
Anti-muscarinics ! alter DA/Ach balance by blocking cholinergic activation of striatum
o Used in early PD or as adjunct to L-DOPA
o Adverse Efx: drowsy, inattention, delusions, hallucinations, Ach dryness.
Benztropine % Diphenhydramine (Benadryl) % Trihexphenidyl
The Future: L-type Ca
2+
channel antagonists.
Anti-Microbials
No single drug is useful for all infections.
cidal vs. static ! both rely on host defenses to aid eliminating bug.
Combination Abx: tx resistant, mixed, or severe infxns; usu not necessary
b/c " cost & " toxicity.
Ideal Abx: obvious things + cidal, narrow spectrum, acid stable, oral, bones
Inhibitors of Bacterial Cell Walls ! all are bactericidal.
1. Penicillins
MOA: bind cell wall enzymes ! !-lactam square & 5-membered ring w/ Sulfur
Pharmacology:
o Hepatic metabolism
o Renal excretion ! glomerular filtration & tubular secretion
Prophylactic use: gonorrhea, syphilis, rheumatic fever, or heart valve dz w/ surgery.
General Side Efx:
o Rash ! delayed rxn " appears in ~2 days. (tx w/ cephalosporin instead)
o Accelerated allergic rxn = within 48 hrs ! hives, wheezing, edema
o Acute allergic rxn ! anaphylaxis, bronchospasm
o Neurotoxicity (worse w/ renal impairment)
Bug Drug Bioav. Side Efx Factors Resistance
Penicillin G
paren-
teral
renal impairmnt add procaine or
benzathine to
prolong t!.
(G+) Naturals
(staph, strep,
spirochetes)
Penicillin V oral
!-lactamase
in staph
Nafcillin p # electrolytes
Oxacillin
Cloxacillin
Penicillinase
Resistant
Staph
Dicloxacillin
o
Ampicillin p/o diarrhea, rash
Amoxicillin
Extended
Spectrum:
G+ & some G- Cyclacillin
o
acid stable
!-lactamase
in G- bugs
Carbenicillin
Ticarcillin # electrolytes
Mezlocillin
(G-) Anti-
pseudomonal
(& influenza)
Piperacillin
o
Combined w/
aminoglycoside if
serious infx
Augmentin =
amox + clav a.
o
N/V, diarrhea,
rash
tx resistant
staph & URIs
Unasyn = ampi +
sulbactam
tx flu, mixed,
comm. pneumo.
Timentin = ticar
+ clav a.
tx anaerobes (B.
fragilis)
Combo:
penicillin with a
!-lactamase
inhibitor
Zosyn = piper +
tazobactam
p
tx G- hospital
infxn, not pseudo
2. Cephalosporins
o MOA: Block cell wall synthesis
$ Chemistry: !-lactam square & 6-membered ring w/ sulfur.
o Renal tubular excretion " delayed excretion w/ probenecid (except Taz)
o General Side Efx:
$ Hypersensitivity similar to penicillins, but less anaphylaxis
$ Diarrhea, phlebitis, IM pain, nephrotoxic, rare superinfections.
First Generation ! similar to ampicillin = G+ cocci, many G- bacilli
o Cefazolin
o Cephalexin
Second Generation ! less G+, more G-
o Cefoxitin
o Cefuroxime
o Cefaclor
Third Generation ! enteric G-, crosses BBB
! Reserve for serious infxns: meningitis, septicemia
o Cefotaxime
o Ceftriaxone hemodialysis OK.
o Ceftazidime excretion via glomerular filtration
o Cefpodoxime (prodrug)
Fourth Generation ! broad spectrum w/ " activity for G+, !-lactamase organisms
! Use to tx Pseudomonas, Klebsiella, E.coli.
o Cefepime
3. Carbapenems
! !-lactam square & 5-membered ring with Carbon and a dbl bond.
! broadest spectrum of any !-lactam abx.
! Gets in CSF only if meninges are inflamed ! convenient?
Imipenem - always give with cilastin to prevent breakdown " renal damage
o Side Efx: seizures, nephrotoxicity, CNS toxicity, & typical penicillin stuff
Meropenem dont need cilastin; # seizures, # efx for G+
Ertapenem dont need cilastin; longer t !, # efx pseudomonas & acinetobactr
4. Aztreonam (Azactam)
MOA: blocks cell wall synthesis by binding PBPs
o A Monobactam = monocyclic bacterially produced !-lactam.
o Narrow spectrum ! G- bacilli only, parenteral only.
o Use in combo w/ broad-spectrum abx.
Side Efx: GI, skin
Renal elimination
5. Vancomycin
MOA: inhibits cell wall synth (cidal), but different site from other !-lactams
Target: G+ bugs, #1 for MRSA.
Resistance: alteration in binding site; plasmid mediated (esp. enterococcus)
Side Efx:
o Does not cross BBB unless meninges are inflamed
o Nephrotoxicity b/c glomerular filtration
o Ototoxicity, esp w/ loop diuretics
o Red Man Syndrome from histamine release ! vasodilation & shock
o Reduced efficacy in patients w/ Multiple Myeloma b/c " [IgA].
6. Fosfomycin
o MOA: blocks formation of cell wall precursors ! cidal
o Pharm: rapid oral, concentrates in urine
o Target: uncomplicated UTI
o Side Efx: generally good; expensive, diarrhea
Daptomycin ! inhibits cell membrane, not cell wall
o MOA: alters charge of cell membrane of G+ bugs b/c it is lipophillic. Cidal.
o Target: G+ bugs unresponsive to other tx.
$ (ex: vanc resistant enterococcus; methicillin-resistant staph)
o Resistance: none
o Side Efx:
$ Muscle pain/weakness ! " serum creatine kinase
$ Interaxns: binds serum albumin (90%); renal elimination.
Rx that Inhibit the Bacterial Ribosome
1. These inhibit the 50s ribosomal subunit ! mostly static.
Dalfopristin-Quinupristin (Synercid) ! 70:30 combo
o MOA: binds ribosome peptidyltransferase " blocks tRNA
o Why together? Alone they are static; together they are cidal.
o Target: Vanc-resistant E. faecium (only).
o Side Efx: inhibits P450; arthralgia, myalgia, " conj. bili
Linezolid (Zyvox)
o Target: Vanc-resist entero. (static @ staph & entero; cidal @ strep.)
o Resitance: pt mutation in 23s RNA of the ribosome
o Side Efx: N/V, diarrhea, pseudomembranous colitis
o Pharmacology: 100% oral bio. OK for liver & kidney BUT inhibits MAO.
$ contains aspartame " bad for phenylketonuria
Macrolides/Ketolides
o Erythromycin
$ MOA: binds reversibly to 50s ribosome " static. (t! = 1.6 hr)
$ Target: G+ bugs when cant use penicillin (narrow spectrum)
DOC for Legionaires
$ Resistance: rapid, via plasmids, " ensure "dose & compliance.
$ Side Efx: Cholestatic hepatitis
o conc. in liver & excreted in bile
o GI pain
o CYP450 inhibitor
o Clarithromycin (t! = 4 hr)
$ Think erythro plus ! better b/c: #GI efx & " acid stable
$ DOC for mycobacterium avium complex (MAC)
o Azithromycin (t! = 40 hr)
$ Think erythro plus ! better b/c: # GI efx & " acid stable
$ DOC for: Legionella, MAC, campylobacter, lyme dz.
o Telithromycin
$ MOA: ketolide that binds ribosome at two sites """ affinity
$ Resistance: low
$ Target: lungs " tx community acquired pneumonia
$ Side Efx: liver toxicity, prolonged QT, inhibits CYP3A4
o Clindamycin
$ Acid stable; slow resistance.
$ Side Efx: pseudomembranous colitis; GI; rash.
Chloramphenicol static
o Resistance: plasmids share inactivation via enzymatic acetylation
o Target: broad spectrum, similar to tetracycline
o Side Efx:
$ Liver: glucaronidation metabolism (t! = 4 hr), but inhibits CP450
$ Renal: filtered & secreted
$ Bone Marrow Toxicity
dose related reversible
aplastic anemia (with " mortality) even months later.
$ Gray baby syndrome
2. And these inhibit the 30s ribosomal subunit ! most are cidal
Tetracyclines ! static
o Tetracycline the drug in the class called tetracyclines.
$ MOA: enter cell via passive diffusion through porin channels
$ Target: broad spectrum " G+ & G-, aerobic & anaerobic
$ Resistance: slow but via # transport in or " efflux out.
$ Side Efx:
Chelates cations (+) easily
o Esp Ca
++
in bone ! discolors teeth if <8 yo.
o Dont give w/ milk/dairy or iron supplements!
Efx gut flora ! avitaminosis or superinfections
Vestibular toxicity ! vertigo
Photosensitivity
Liver toxicity
o Doxycycline - Severe liver damage if parenteral, but # GI pain & ## doses.
o Minocycline prophylaxis for meningitis; bad vomiting & vertigo.
o Demeclocycline - ?
o Tigecycline (not on drug list)
$ MOA & Side Efx: similar to tetracyclines; broad spectrum "tx MRSA
$ Resistance: low b/c it can bind other sites and evade efflux pumps.
Aminoglycosides ! cidal
$ MOA: aminosugars diffuse through porin channel " energy dependent
Not acid stable " dont give it orally or mixed with !-lactams
t! = 30-90 min
$ Resistance: inactivation or #O
2
/energy (ie, doesnt work in anaerobes)
! Note: resistance to one does not mean resistance to all. %
$ Its pretty toxic, so only use for severe aerobic G- bugs
Ototoxicity (irreversible)
Nephrotoxicity (glomerular filtration)
Neuromuscular blockade
o Gentamicin great for enterococcs endocarditis
o Tobramycin great for P. aeruginosa
o Amikacin great for strains resitant to Gentamycin & Tobramycin.
o (Streptomycin 2
nd
line for TB)
Cidal drugs work best in growing microbes. Static drugs inhibit growth.
Concurrent use is counterproductive.
Metabolic Analogs ! prevent folate metabolism
Sulfonamides
$ Resistance is slow
$ Distribute to CSF, placenta, breastmilk
$ Renal excretion
$ Classic allergic rash
$ Crystalline aggregates in urinary tract
o Sulfamethoxazole rapidly absorbed,
o Sulfsoxazole rapidly absorbed, DOC for UTI
o Silver sulfadiazine rapidly absorbed, topical,
tx eye infxns
o Sulfasalazine poorly absorbed " good for IBD
o Sulfadoxine t! = 1 week (not on drug list)
Trimethoprim
o MOA: prevents reduction of di- to tetra-hydrofolate
$ Penetrates CSF; concentrates in prostate & vaginal fluid
$ t! = 11 hr
Bactrim = Trimethoprim + Sulfamethoxazole
o Static alone, cidal together! ! 20:1 ratio (sulfa:trimethoprim)
o Skin rash common
o Targets: UTI, URI, neisseria, influenza, Legionella, P. jiroveci, nocardia
Inhibitors of Nucleic Acid Synthesis (Fluoroquinolones) ! cidal
MOA: inhibit DNA gyrase; t! = 4 hr
o Resistance: # porin proteins or " efflux of drug
Side Efx: Gi, dizzy, photosensitivity, teratogenic, seizures w/ NSAIDs.
Target: alternative for more toxic broad-spectrum drugs.
1
st
Gen Naldixic acid
Cirioxacin
Tx uncomplicated UTI
Rapid resitence
2
nd
Gen Ciprofloxacin
Enoxacin
Grepafloxacin
Lomefloxacin
Norfloxacin
Ofloxacin !
" G- & systemic axn
Improved pharmacokinetics
# side efx BUT
prolong QT & inhibit CYP450
good CSF penetration
3
rd
Gen Gatifloxacin
Levofloxacin
Moxifloxacin
Sparfloxacin
More axn at G+
Broader G- coverage
4
th
Gen Truvafloxacin additional anaerobe axn
"
Hematopoietic Agents
Growth Factor Agonists
Erythropoietin (more RBCs, please)
o Epoetin ! & Darbepoetin !
! MOA: recombinant human erythropoietin " act on committed
progenitor cells to " RBC production. (give IV or SC)
Supplement w/ iron dextran
! Tx: AIDS, chemo, preemies, chronic inflammation, renal failure.
! Side Efx: high dose #heart problems, renal dz, death.
Myeloid Growth Factors (go bone marrow, go!)
o Sagramostin (GM-CSF) - GM = Granulocytes & Monocytes
! Tx: shortens period of iatrogenic neutropenia (transplant, chemo)
! Side Efx:
"" granulocytes # need frequent blood counts
bone pain; rash
flu-like sx, malaise, fever, diarrhea, dyspnea
o Filgrastim (G-CSF) - G = Granulocytes
! Tx: severe neutropenia (iatrogenic or hereditary)
! Side Efx:
"" granulocytes # need frequent blood counts
bone pain; rash
o Pegfilgrastim (Neulasta) like filgrastim w/ a longer t! .
Megakaryocyte (makes platelets)
o Thrombopoietin
! MOA: selective megacaryocytopoiesis # rapid " #platelets
! Tx: improves other anemia therapies (currently in clinical trials).
Basically, always use it w/ a myeloid GF and erythropoietin.
o Oprelvekin
! MOA: recombinant form of IL-11 # "lymphoid & myeloid growth
! Tx: thrombocytopenia
! Side Efx: fatigue, dizziness, dyspnea, arrhythmia, edema
#
Vitamins & Minerals
Iron
o Ferrous Sulfate DOC for iron deficiency anemia; oral
! Others: Ferrous Gluconate, Ferrous fumarate.
! Side Efx: heartburn, nausea, GI discomfort, constipation, diarrhea
! Iron Poisoning: pain, diarrhea, vomiting brown/bloody stomach
contents, pallor/cyanosis, hyperventilation (acidosis), shock.
o Parenteral Iron (Ferric gluconate in sucrose; Iron dextran; Iron sucrose)
! give only if oral not tolerated or absorbed (ex: renal dz w/ Epoetin)
! Side Efx: different from oral iron
Headache, malaise, fever, lymphadenopathy, arthralgia,
urticaria, worsens RA, anaphylactic shock (rare)
o Deferoxamine (iron chelator)
! Tx: iron poisoning; hereditary hemochromatosis
B12 # Cyanocobalamin & Hydroxycobalamin
o Both used to tx Vitamin B12 deficiency (impaired DNA synth #
megaloblastic anemia).
o o/p (injection preferred)
Folic Acid
o Deficiency:
! Classic patients are either pregnant or taking folate-chelating drugs
! Classic complications: neural tube defects, "homocystine,
megaloblastic anemia
o Folic Acid - o/p
! May counteract efx of anti-epileptics
o Folinic Acid F-formyl derivative of tetrahydrofolate
! This is important b/c it can circumvent any inhibition of DHFR (like
methotrexate), so you can keep taking that drug AND fix the anemia.
! Also note that if your chemo drug is an anti-folate drug, this will put
a rather large damper on the efx of that other drug.
General advice:
o Give both B12 and Folate in case the pt needs both.
o Treat the specific deficiency instead of giving a multivitamin.
Dietary Supplements
Massive industry ! 22 million in 2006
Age Range ! highest % use in young children and retired folks.
Problems with Supplements:
o patients think natural = safe (wrong!)
o lower safety/testing standards; active ingredients and potency may vary.
o the manufacturer is responsible for supplements safety
o patients dont always think to tell you theyre taking them ! " risk of drug
interactions (especially elective surgeries)
Supplement Clinical Implications Intended Use
Kava-Kava sleeping aid, anti-anxiety
Comfrey bone + muscle; kidney stones
Germander Wt loss, general tonic
Green Tea Ext.
hepatotoxicity
anti-oxidant, anti-inflamm.
Ephedra cardiovascular toxicity Herbal wt. loss
Chaparral tonic, arthritis, wt. loss
Borage rheumatoid arthritis, HTN
Senna
hepatotixicity
&
carcinogenic Laxative
Licorice Pseudo-aldostronism Peptic ulcers; flavoring
Garlic anti-platelet axn
Ginkgo Biloba
anti-platelet
inhibits CYP1A2 & 2D6
prevent Alzheimers (doesnt
work)
Anise
Celery
Chamomile
Fenugreek
natural coumarin derivatives
Red Clover
natural coumarin derivaative
estrogen-like ! " risk cancer
Meadowsweet
Poplar
Willowbark
natural salicylate
Capiscum hypocoagulability b/c fibrinolytic axn
St. Johns Wort Induces CYP3A4 & CYP1A2
Echinacea
Induces CYP3A4
Inhibits CYP1A2 & 3A4 (intestinal)
Antagonize immunosuppressants
Ginseng
Antagonize immunosuppressants
prolonged bleeding
inhibits CYP2D6
Bitter Orange Inhibits CYP3A4
Pomegranate juice
" mean PSA doubling time
Inhibits CYP3A4
rhabdomyolysis (" risk w/ statins)
Cranberry GI upset, diarrhea urinary tract health
Caffeine stimulant!
In lecture but not on drug list:
Supplement Clinical Implications of excess Intended Use
Vitamin A (retinol)
N/V, blurred vision, birth defcts,
may " mortality (so can E).
Vitamin D
N/V, constipation, arrhythmia,
calcium deposition in soft tissue
Vitamin E & K antagonize warfarin (anticoag.)
fat-soluble vitamins
Vitamin C kidney stones, "iron, GI upset
Vitamin B-3 (niacin) flushing, GI upset
Vitamin B-6 peripheral neuropathy + pain
Note: does not slow cognitive
decline in Alz.
Folic Acid (Vit. B-9) may hide sx if B12 deficient Prevent birth defects
Omega-3 fatty acids
high intake ! bleeding
halitosis
" HDL
Chromium
no proven efx in diabetes or
body wt.
enhance insulin axn & "
metabolism
Selenium improve cancer or HIV antioxidants
Zinc
# diarrhea, " healing of gastric
ulcers, # sickle cell sx.
cofactor in your body
"
Anti-Fungal Agents
Rule of Thumb: if it disrupts the cell membrane, its cidal.
Polyene Anti-fungals
o Amphotericin B
! MOA: binds ergosterol in fungal cell membrane " forms a pore "
K
+
& Mg
++
leak out " cidal.
Lipid-based formulations have # side efx
Give IV, binds to !-lipoprotein
Excreted unmetabolized in urine & bile
Resistance is rare
! Target: deep fungal infxns in pregnant woman
! Side Efx:
Nephrotoxicity dose limiting
Fever, chills, shock-like hypotension
o Nystatin static or cidal, depends on dose.
5-Flucytosine
o MOA: prodrug that inhibits thymidylate synthesis & DNA synthesis
! cidal/static efx are dose dependent
! Give in combo w/ amphotericin B " prolongs t!
o Resistance: lack of permease; defective cytosine deaminase (no activation)
o Side Efx:
! Glomerular filtration " adjust for renal dz
! Hematological toxicity
! Colitis
Azoles
! MOA: inhibit synthesis of ergosterol (" defective membrane)
! Resistance: rapid if used alone
! Side Efx:
All are teratogenic
All inhibit CYP450
o Voriconazole >Itraconazole =Ketoconazole >>Fluconazole
o Fluconazole penetrates CSF; t! = 22 hr; renal excretion
o Itraconazole - needs acid for absorption " H2RBs reduce efx. t! = 36 hr
! Target: broader spectrum than fluconazole
! Side Efx: liver toxicity (excreted in bile), GI disress, CHF
o Voriconazole visual disturbance (transient), photosensitivity, liver toxicity
o Ketoconazole N/V, #testosterone/steroid problems
o Topical Azoles (for mucocutaneous use) " Miconazole & Clotrimazole
#
Terbinafine
o MOA: inhibits squalene epoxidase (needed for ergosterol synthesis)
! Lipophilic " protein bound and concentrates in keratin " hair & nails
o Side Efx: headache, GI, taste changes, cholestatic hepatitis (liver toxicity)
Caspofungin
o MOA: inhibits #(1,3)D-glucan synthesis (integral component of cell WALL).
! IV infusion that takes 1 hr yikes
! Excreted in feces & urine
o Target: 2
nd
line for invasive aspergillus or candida
o Side Efx: Histamine sx; teratogenic
Griseofulvin
o MOA: disrupts mitotic spindle in fungal cells " static.
o Target: dermatophytes
o Side Efx: headache, GI, photosensitivity, $ hepatic metabolism (ex: #OCs)
Anti- Tubercular Agents
! These bugs grow slow, live intracellularly, and develop resistance easily.
First-Line Tx for Mycobacterium (takes ~ 24 wks)
M. tuberculosis M. avium complex
1. Isoniazid
2. Rifampin
3. Pyrazinamide
4. Ethambutol or streptomycin
1. Clarithromycin
2. Ethambutol or clofazimine or
cipro or amikacin
Isoniazid
o MOA: blocks mycolic acid synthiesis " disrupts cell wall " cidal.
! Penetrates to intracellular space and CSF, placenta, & breastmilk
! Efx limited to static if slow-growing or walled off (caseous necrosis).
! Metabolism in liver (n-acetylation); excreted in urine
o Resistance is rapid " never use alone!
o Side Efx: peripheral neuropathy; hepatotoxicity, antacids & corticosteroids
make it less effective.
Rifampin
o MOA: binds ! subunit of RNA polymerase " cidal.
! Penetrates CSF; metabolized in liver & induces CYP450
o Resitance is rapid " never use alone!
o Target: TB, MRSA, meningitis, & best anti-leprosy.
o Side Efx: Orange-red body fluids, GI, fever, hepatotoxic, #OCs
$
Ethambutol
o MOA: unknown maybe block RNA synthiesis? It does require actively
dividing bugs. Regardless, its static. But resistance is latent, so thats nice.
o Side Efx: optic neuritis " #visual acuity
Pyrazinamide
o MOA: bugs convert drug to pyranzinoic acid " #pH " bug cant grow.
! Cidal or Static (dose dependent)
! Resistant bugs are smart and dont convert it to an acid.
! Gets into CSF; metabolized in liver; urine excretion
o Target: bugs in acid environment of lysosome/macrophage (ie, slow-growing).
o Side Efx: hepatotoxicity, hyperuricemia & gout, arthralgia.
Cycloserine
o MOA: analog of D-alanine " blocks cell wall synthesis.
! cidal/static = dose depenent.
! Broad spectrum, but use only when others fail. Renal excretion
o Side Efx: CNS problems (headache, bertigo, confusion, psychosis, seizures)
Capreomycin
o MOA: unknown, but its static. Give IM
o Target: last ditch effort b/c side efx: nephrotoxicity
Ethionamide
o MOA: inhibits peptide synthesis (analog of isoniazid but works different)
! Penetrates CSF
o Target: last ditch effort b/c of toxicity
o Side Efx: GI, hepatic, thyroid
REVIEW: Antimicrobial Sites of Action
Cell Membrane
daptomycin
polymyxins
polyene antifungals
imidazole antifungals
Ribosome (30s) inhibitors
aminoglycosides
tetracyclines
spectinomycin
Cell Wall Synthesis
penicillins
cephalosporins
monobactams
carbapenems
vancomycin
bacitracin
caspofungin
isoniazid
RNA polymerase
rifampin
Folic Acid Metabolism
trimethoprim
sulfonamides
DNA gyrase inhibitors
fluroquiniolones
Ribosome (50s) inhibitors
macrolides
chloramphenical
clinamycin
synercid
linezolid
CNS Stimulants
Indirect Dopamine Agonists
o Amphetamine (Adderall) & Dextroamphetamine (Dexedrine)
! Tx: obesity, narcolepsy, ADHD
! Efx:
Incr BP, arrhythmias, angina, headache
Incr alertness, decr fatigue, incr self-confidence, insomnia
Releases Dopamine in reward pathways " incr risk abuse
Neurotoxic
! OD: convulsions, coma, cerebral hemorrahge, wt loss, schizophrenia
o Methamphetamine (Ice)
! Take a pinch of red phosphorus, a smidgeion of ephedrine, a dash of
iodine and a skosh of lye. Add some distilled water and simmer for a
few hours and hope it doesnt explode and kill you. Voila!
! High CNS stimulation w/ decr. peripheral efx.
o Methylphenidate (Ritalin)
! Think Meth, but milder CNS stimulation. Still has abuse potential.
! Tx uses: narcolepsy, ADHD
o Cocaine
! Stimulates VTA " nucleus accumbens " prefrontal cortex
! t ! = 50 min (but the perceived high is shorter)
! metabolites detectable in urine 2-10 days after use.
! Cocaine + Alcohol " metabolized to cocaethylene
Incr & prolonged euphoria
Incr cardiotoxicity
! Preferable Efx:
Vasoconstriction (b/c blocks noradrenergic transporter)
Local Anesthetic (b/c blocks voltage-gated Na+ channels)
Incr. HR & BP
Incr. arousal, alertness, & Euphoria
! Less desirable Efx:
Efx of Long-Term Use: motor spasms, paranoia, irritability
Tolerance to euphoric efx. #
Heart: arrhythimas, ischemia, myocarditis, aortic dissection
Sex: decr. libido; premature labor (sex makes babies)
Brain: vasoconstriction/ischemia, seizures, paranoia, addictive
o Withdrawal Sx: depression, fatigue, craving, decr. HR
o Mazindol (Sanorex)
! Similar MOA as cocaine but more specific for NorEpi. (not DA?)
! Tx: obesity
! Side Efx: allergic rxn, insomnia, dry mouth/eyes (glaucoma)
And ones like cocaine: arrhythmia, incr. BP, anxiety, impotence.
Drug interaxns: MAO-Is, TCAs, Guanethidine
Phentermine (Adipex, Fastin) - indirect Serotonin Agonist
o Tx: obesity (short-term use only!)
o Good: lower risk of abuse than amphetamine
o Bad: atherosclerosis, HTN, hyperthyroid, hx of drug abuse, MAOIs.
Atomoxetine (Strattera) indirect NorEpi Agonist (ie, reuptake inhibitor)
o Tx: ADHD (only drug specifically approved for adults)
o Low abuse potential
o Side Efx: anorexia, insomnia, incr HR & BP, not as effective as stimulants
Caffeine (methylxanthine)
o MOA: adenosine receptor agonist " incr DA & NE, inhib. Phosdiesterase
! Rapid tolerance
! Mild withdrawal: fatigue, sedation, headaches, nausea
! NOT ADDICTING (according to APA).
Others
o Sibutramine
! MOA: blocks reuptake of dopamine, NorEpi, & Serotonin. (dcr. abuse)
! Tx: obesity
! Contraindicated with: MAOI, Anorexia Nervosa, HTN
! Side Efx: Serotonin Syndrome
o Modafinil
! MOA unknown. T ! = 15 hrs.
! Tx: narcolepsy
! No efx on Dopamine so no abuse potential. No GI or heart side efx.
! Side efx: Induces CYP450, headaches (for a week)
o Ephedrine
! MOA: increase release of DA & NorEpi " potent stimulant.
t ! = 5 hr.
! Tx: narcolepsy, bronchoconstriction, depression
! Side Efx: HTN, stroke, MI, insomnia, tachyphylaxis (rapid desensitization)
o Strychnine
! MOA: glycine receptor antagonist
Disinhibition
Convulsions & impaired respiration " pesticide axns (fatal)
Found in street drugs b/c stimulates all portions of CNS
! Tx: respiratory support & diazepam (anti-convulsant)
No longer on the Market (or your drug list)
o Fenfluramine withdrawn from market b/c cardiac toxicity.
o Pemoline ADHD drug withdrawn from market b/c liver toxicity.
1) A 59 year-old woman is diagnosed with TB. Before prescribing a drug regimen, you
take a careful history because one of the drugs used to treat TB is an hepatic CYP450
inducer. Which drug is it?
A) Ethambutol
B) Isoniazid
C) Pyrazinamide
*) Rifampin
E) Vitamin B6
2) Prior to surgery for a prosthetic heart valve, a 67 year-old man with multiple antibiotic
resistances is given a prophylactic IV dose of antibiotic to protect against endocarditis.
As the drug is infused, the patients skin becomes flushed red over most of his body. The
drug he most likely received is:
A) Erythromycin
B) Gentamicin
C) Penicillin G
D) Tetracycline
*) Vancomycin
3) An intoxicated elderly man is brought to the ER where it is determined that he is in
urgent need of antimicrobial treatment for an infection. You wish to avoid a disulfiram-
like reaction that might precipitate cardiovascular or respiratory sequelae, bearing in
mind his inebriated state. Assuming each of these drugs would be suitable for the
infection, which is most likely to produce the described adverse effect?
A) Amoxicillin
*) Cefotetan
C) Erythromycin
D) Linezolid
E) Penicillin G
4) A 19 year-old is being treated for leukemia when she develops a fever indicative of an
infection. You give her several agents that will cover fungal, bacterial and viral etiology.
After 48-hours, serum creatinine is rising and acute renal failure ensues. Which of the
following drugs is most likely responsible?
A) Acyclovir
*) Amphotericin B
C) Ceftazidime
D) Penicillin G
E) Vancomycin
5) A 21 year-old woman with UTI due to E. coli is prescribed
sulfamethoxazole/trimethoprim [Septra 800/160]. Trimethoprim works by:
A) binding to beta-lactamase
B) binding to the 50s ribosomal subunit
C) inhibiting renal dihydropeptidases
*) inhibiting dihydrofolic acid reductase
E) inhibiting RNA synthesis
6) A 72 year-old man is receiving drug therapy for TB. Two weeks following the
initiation of drug therapy, he returns to his PCP to complain that his sight is going
funny and that his gout is worsening. Which of the following drugs would most likely
produce these symptoms?
*) Ethambutol
B) Isoniazid
C) Pyrazinamide
D) Rifampin
E) Vitamin B6
7) Fungal cytosine deaminase converts flucytosine to:
A) Ergosterol
B) Mycolic acid
*) 5-Fluorouracil
D) Porphyrin
E) Sulfacetamide
8) Azole antifungal agents work by:
A) binding to ergosterol and forming pores in fungal membranes
*) inhibiting P450 14alpha-demethylation of lanosterol
C) binding to the 50s ribosomal subunit
D) inhibits squalene epoxidase
E) inhibits alpha (1,3)-D-glucan synthesis
9) Low hemoglobin and a low hematocrit are found in a G6PD-patient receiving drug
therapy for TB. Which of the following drugs would most likely produce these
symptoms?
A) Ethambutol
*) Isoniazid
C) Pyrazinamide
D) Rifampin
E) Vitamin B6
10) Gynecomastia is a consequence of treatment with:
A) Amphotericin B
B) Caspofungin
C) Griseofulvin
*) Ketoconazole
E) Terbinafine
11) Terbinafine is used to treat which type of fungal infections?
A) Aspergillus
*) Onchomycosis
C) Cryptococcus
D) Histoplasmosis
E) Disseminated Candida albicans
12) Which of the following binds to and inactivates bacterial transpeptidase, thereby
inhibiting cross-linking of peptidoglycan subunits?
A) Clindamycin
B) Levofloxacin
*) Penicillin G
D) Doxycycline
E) Trimethoprim
13) Resistance to beta-lactam antibiotic occurs through a number of mechanisms,
including the production of bacterial beta-lactamases. Which of the following is a beta-
lactam antibiotic that is resistant to beta-lactamase expressing bacteria?
*) Aztreonam
B) Amoxicillin
C) Pipercillin
D) Ampicillin
E) Ticarcillin
14) Which of the following drugs is effective against MRSA, VRSA, and vancomycin-
resistant E. faecium and E. fecalis?
A) Azithromycin
B) Cefaclor
*) Daptomycin
D) Dalfopristin/Quinipristin
E) Oxacillin
15) The class of antimicrobials known as penicillins has many members. Which of the
following is considered to be acid stable with an extended spectrum of activity?
*) Amoxicillin
B) Ticarcillin
C) Cloxacillin
D) Nafcillin
E) Penicillin G
16) Which of the following works by inhibiting bacterial DNA gyrase?
A) Amoxicillin
B) Cefaclor
C) Linezolid
D) Demeclocycline
*) Levofloxacin
Identify the INCORRECT statement regarding herbal remedies.
A) Herbal medications are covered drugs and under DSHEA, manufacturers are not
required to demonstrate efficacy before marketing a particular agent or combination
product
B) There are insufficient clinical studies to document dosing for herbal medications
C) Herbal medications produce pharmacological effects, and thus, may produce drug
interactions and side effects
*) The FDA regulates herbal medications in the same manner that it regulates OTC
products and medical devices.
Which of the following agents was removed from the market because of its association
with hemorrhagic stroke?
A) Echinacea
B) Ginko biloba
C) Garlic
D) Kava
*) Ephedra
Your diabetic patient was previously managing their condition quite well but lately blood
sugar levels have been erratic. In questioning your patient about recent changes in their
life that might explain this development, they tell you that they have recently begun
taking an herbal product. Which of the following is most likely responsible for the effect?
A) Ginkgo
*) Ginseng
C) Red clover
D) Sawtooth palmetto
E) Valerian
Which of the following contains estrogen-like constituents and would therefore be
relatively contraindicated in a woman with hormonally-responsive breast cancer?
A) Ginkgo
B) Ginseng
*) Red clover
D) Sawtooth palmetto
E) Valerian
A 45 year-old woman is pancytopenic following adjunctive chemotherapy for breast
carcinoma. Her physician prescribes a drug that will selectively stimulate megakaryocyte
proliferation to increase her platelet count. Such a drug is:
A) Epoetin alfa [Epogen].
B) Folic acid.
*) Oprelvekin; rh-IL-11 [Neumega].
D) Sargramostim; GM-CSF [Leukine].
E) Vitamin B12.
A 27 year-old vegan has pernicious anemia. Lifetime supplementation is necessary with
which of the following drugs to correct the anemia and to prevent irreversible neurologic
damage?
*) Cyanocobalamin [Berdoz].
B) Deferoxamine [Desferal].
C) Ferrous sulfate.
D) Folic acid.
E) Ferretin.
"
Drugs for the Prevention and Treatment of Arterial Thrombosis
Big Picture:
Anti-platelet drugs (aspirin & clopidogrel) most effective in preventing arterial
thrombosis (stroke, MI, etc); less effective in preventing venous thrombosis.
Anti-coagulants (heparin & warfarin) prevent both arterial and venous thrombosis
(DVT, pulmonary embolism, arterial thrombi).
Thrombolytics (Fibrinolytics) lyse both arterial and venous thrombi.
Anti-Coagulants
Indirect Thrombin Inhibitors (via Anti-Thrombin III)
Heparin
o MOA: activates antithrombin III ! inactivates thrombin (binds Exosite 2)
" Only works for soluble thrombin (clot-bound has hidden binding site)
" Monitor dose w/ PTT
o Side Efx: immune response mounts after 5-10 days of use (b/c platelet 4
binds heparin & abys bind to the new complex) ! thrombocytopenia (HIT).
LMWH (Low Molecular Weight Heparin):
! Enoxaparin, Dalteparin, Ardeparin, & Danaproid
" Smaller, active pieces of heparin with a longer t !. (give SubQ)
" ! # anti-Xa axn & $ anti-platelet axn (! dont need to monitor)
Fondaparinux
o MOA: Factor Xa is the single molecular target of this drug.
#
Direct Thrombin Inhibitors
Hirudin
o MOA: irreversibly binds at the active site and Exosite 1 of thrombin
" Independent of antithrombin III.
" Axn against free (soluble) AND clot-bound thrombin
" Unaffected by factors that neutralize heparin
o Origin: leech spit
o Use: heparin-induced
thrombocytopenia
Lepirudin a recombinant
derivative of Hiruden.
Melagatran/Ximegalatran
MOA: reversibly binds the
active site of thrombin.
Vitamin K Antagonists:
Coumarin/Warfarin
MOA: competes w/ Vitamin K epoxide reductase ! $ fibrin formation
Side Efx: skin necrosis, bleeding
Give heparin while waiting.
aka Prothrombin Time
$
Anti-Platelet Drugs
COX inhibitors
o Aspirin non-selective COX 1&2 irreversible inhibitor (!efx last 4-7 days)
! Antipyretic, anti-inflammatory, analgesic, antiplatelet
" Block COX 1 ! no TxA2 from platelet ! no platelet aggregation
" Block COX 2 ! no PGI
2
from endothelium
" Use: $CHD %
" Side Efx: GI bleed, hemorrhagic stroke, asthma (b/c # leukotrienes)
o Other NSAIDS - non-selective COX 1&2 reversible inhibitor
" Anti-platelet efx not nearly as good as aspirin. (!dont $CHD)
o Celecoxib selective COX-2 ! no anti-platelet efx. (#CHD = bad!)
o Acetaminophen COX-3? (very weak COX 1&2)
" ideal antipyretic/analgesic for pts taking warfarin or heparin.
Drugs that # platelet cAMP
o Phosphodiesterase Inhibitors
" Dypyridamole
MOA: blocks phosphodiesterase (enzyme that degrades cAMP)
! #cAMP ! inhibits aggregation & #adenylate cyclase.
Also a potent vasodilator
Use: makes aspirin better; weak anti-platelet used alone.
Side Efx: headache, dizziness, GI upset
" Cilostazol
MOA: PDE IIIb inhibitor (reversible) & vasodilator.
Not a 1 antiplatelet drug.
o Adenylate Cyclase Activators: Prostacyclin (PGI) & Organic Nitrates
(indirect)
Drugs that Inhibit ADP (! prevent aggregation)
o (Ticlopidine 1stGen neutropenia, TTP, & aplastic anemia. Bad. Off market.)
o Clopidorgrel a thienopyridine prodrug.
" MOA: prevents ADP from activating GP IIb/IIIa Receptor ! no
platelet activation ! no aggregation
Anti-platelet efx = aspirin (but #$$ & dont use em together)
" Side Efx: bleeding (but not those bad ones of Ticlopidine)
Drugs that block GP IIb/IIIa Receptor
o Eptifibidate synthetic peptide, prevents binding of fibrinogen, give IV
o Abciximab Aby for the receptor, give IV
%
Thrombolytic Drugs
! These all convert plasminogen ! plasmin, which degrades fibrin & fibrinogen.
Clot-Busters work in ~60% of coronary thrombosis pts.
! Give aspirin and heparin concomitantly to prevent re-thrombosis.
! beware Systemic Lytic State ! intracranial hemorrhage! (occurs in ~3%)
Sreptokinase
o 1
st
Gen - Comes from hemolytic streptococcus
o MOA: forms activator complex with plasminogen; non-specfic
o Good: cheap; additive efx w/ aspirin.
o Bad: lytic state; triggers immune response ! one-time use only
Urokinase
o 1
st
Gen - Comes from cultured human fetal kidney cells (! not antigenic)
o MOA: serine protease that cleaves plasminogen into plasmin; non-specific
o Use: acute massive unstable PE
o Side Efx: lytic state (b/c non-specific)
tPA
o 2
nd
Gen recombinant endogenous serine protease from vascular endothelium
o MOA: tPA, fibrin, & plasminogen form a ternary complex ! specific axn
against fibrin clot
o Use: MI, PE, or stroke w/out hemorrage.
Reteplase
o r-PA a deletion variant of tPA w/ longer t!.
o works about the same as tPA but #incidence of hemorrhagic stroke (yikes).
When to NOT give these drugs:
- pt >75 yo
- recent surgery, biopsy, or CPR
- uncontrolled HTN
Over the Counter Drugs
General:
! OTC or Rx who decides?
1. FDA decides if drug is safe for direct selling via Non-prescription Drug
Advisory Committee (NDAC).
a) Does the drug in question treat a condition that consumers can
diagnose and manage themselves
b) Is the drug sufficiently safe for use by consumers without direct
supervision by the physician
c) Does the label clearly explain the potential adverse effects and
conditions with clear and understandable directions
d) The variability in decision-making criteria between candidate drugs
calls into question the transparency of the process.
! Rx to OTC switch has allowed Americans a more active role in their healthcare.
! Changing role =
1. Original intention relieve symptoms
2. Now many of them were once rx agents to treat or cure the illness
3. Key to successful use = select correct product but NOT easy must
recognize symptoms, judge severity, choose and assess tx options
! OTC Labels a large % of consumers dont read label!
1. Product name
2. Active Ingredients
3. Purpose antacid, antihistamine, cough suppressant
4. Uses symptoms or dz to be treated
5. Warnings when not to use, to stop, to see a doctor
6. Directions how to take, how much, how long
7. Other info storage conditions
8. Inactive ingredients binders, coloring, flavoring
! Misperception = increasing dose beyond what is recommended, re-dosing earlier,
or taking more drug in a day than recommended brings great and quicker relief.
1. This is NOT true!!
2. This misperception is pervasive across all age groups even with adults.
3. Primary rule of safety for any med = to give right does at right time.
! Significant Problems = drug interactions with food and beverages, potential
problems with dzs, alcohol + OTC = not good, anti-coag tx, CNS acting drugs
might not mix with OTC agents, and careful with NSAID dose
! Prescription drugs were the 3
rd
most used drugs amongst teens in 2005 behind
marijuana and inhalants.
Reasons for OTC Use:
! Typical uses = allergies, arthritis, athletes foot, common cold, constipation,
cough, diarrhea, drowsiness, eye problems, fever, GI, HA, hemorrhoids, jock itch,
menstrual pain, muscle pain, pain, poison, ring worm, scalp itch, skin problems,
sleep disorders, sore throat, ulcer, upset stomach, vomiting
! Analgesics/NSAIDs very commonly used OTC
1. Safe when taken as directed for short-term use (7-10 days)
2. Studies have shown toxicity in kidney, liver and GI tract
3. FDA proposed Label Changes:
a) Products with acetaminophen include warnings for liver tox,
particularly when used in high doses, with other acetaminophen
products, or with 3+ alcohol drinks a day.
b) OTC NSAIDS include warning for stomach bleeding in people
over 60, those who have had ulcers, taken a blood thinner or
more than one NSAID, or those who take them with alcohol or
longer than directed.
c) To help consumers track consumption, FDA also wants
acetaminophen or NSAID to be prominent on the package.
Consumers taking a pain reliever may not know that a cold med
also has the ingredient.
Acetaminophen (Tylenol)
! SE = hepatic toxicity
! Interactions = hepatotoxic drugs (azoles, macrolides,
warfarin), CYP inducers
! Cautions = cirrhosis, poor nutrition, alcohol use, anti-coag
! Dosing = 10-15 mg/kg/dose q4-6 hr with no more than 5
doses in 24 hr; max daily dose = 80 mg/kg/day tox
reported at lower doses
NSAIDS (Bayer, Advil, Naprosyn, Orudis)
! SE = tinnitus, diarrhea, N, gastritis, GI bleed, renal failure
! Interactions = Warfarin, ACEIs
! Cautions = renal failure, CHF, cirrhosis, gout, aspirin
sensitive asthma
! Allergy Meds
1. Anti Histamines runny nose, sneezing, watery eyes
Loratadine (Claritin, Alavert, Zyrtec)
! Marketed as non-sedating
! Push too high and CNS effects will occur
! 1
st
generation drugs used for motion sickness = diphenhydramine,
dimenhydrinate, cyclizine
! Alternative to the sedating agents:
Brompheniramine (Dimetane)
Chlorpheriramine
Diphenhydramine (Benadryl)
Clemastine
2. Coughs and Colds
Anti-Cholinergic Antistamines (Benadryl)
! SE = cognitive dysfxn, hallucinations, insomnia,
xerostomia, constipation, impaired diaphoresis, !
thirst, mydriasis, anuresis, seizures, arrhythmia, heat
stroke
! Interactions = Anti-parkinsonian drugs, TCAs,
phnothiazines, oxybutynin
! Cautions = closed angle glaucoma, dementia
Pseudoephedrine (Sudafed)
! SE = HTN, vasospasm , arrhythmia, stroke, seizure,
hallucinations, chronic Has, insomnia, tremor
! Interactions = BBs, digoxin, MOAIs
! Cautions = CHD, HTN, thyroid dz, diabetes, prostatic
hypertrophy, urinary retention, closed-angle glaucoma
Topical Nasal Decongestants (Afrin, Neo-Synephrine)
! SE = rhinitis medicamentosa, HTN
! Interactions/Cautions = same as for pseudoephedrine
3. Anti-Tussives for dry irritating cough
Benzonatate
! Local anesthetic like action; limited efficacy
! SE = sedation, mild dizziness, and HA, mild GI upset
Codeine, Hydrocodone BY PRESCRIPTION ONLY!!!
! MOA = direct action on the cough center of the medulla
! Suppression is achieved at lower doses than those
producing analgesia
! Drying effect and ! viscosity of respiratory secretions
! NO well controlled studies demonstrate efficacy report
of peds deaths and other adverse SEs
Dextromethorphan found in >125 OTC products
! MOA = binds to non-opiate Rs in cough center
! At normal doses (15-30mg q6-8 hr) has NO sedative,
analgesic, or addictive properties
! Demethylated by CYP2D6 and enzyme deficient in some
individuals leading to rapid acute tox
! Excess = dry mouth and throat, !HR, warm feeling,
inability to concentrate
! With > 2mg/kg (5-10x normal dose) you get phencyclidine
like effects --- out of body state, disorientation,
depersonalization, confusion, somnolence, stupor,
impaired coordination, disorientation of speech,
dissociative anesthesia; addiction is problematic
! Combo products = contain ingredients that limit dosing
(guaifenesin) or have toxicity (chlorpheniramine)
4. Expectorants productive cough, congested
Guaifenesin = only FDA approved OTC agent
! High dose effects = N/V, dizziness, HA, rash
5. Conclusions:
a) Anti-tussives have ? clinical efficacy
b) Centrally acting agents are dangerous, esp in young kids
c) Decongestant/anti-H may " post-nasal drip and " cough
! OTC Products Affecting BP
Ephedrine
Epi
Ibuprofen
Phenylephrine
Pseudoephedrine
Racinephrine
Theophylline
! OTC Stimulants (Diet Aids) Caffeine
Coffee
Decaf
Tea
Cold Remedies
Analgesic Preparations
Stimulants
Weight Loss Aids
a) > 300mg/day ! spontaneous abortion, low birth weight,
metabolizing enzymes absent in newborn
b) Caffeine withdrawal syndrome = HA, sleepiness, drowsiness,
irritability, confusion, etc.
c) At normal doses, no arrhythmogenic link with CV dz.
! Orlistat
a) GI lipase (covalent) inhibitor for obesity management
b) Blocks the absorption of dietary fat -- "calorie intake leads to
negative E balance and weight loss
c) Minimal systemic absorption
d) Adverse effects, esp. with >30% fat calories = flatulence with
discharge, fecal urgency/incontinence, steatorrhea, oily spotting,
oily evacuation
e) Pt. needs to adhere to recommended diet plan
f) Psyllium fiber adjunct can " some GI side effects
g) Hypovitamnosis can be prevented through use of daily mv
that contains fat soluble vitamins
! Benzocaine Gum numbs the taste buds removing the pleasure of eating
! OTC Dyspepsia and Heartburn
1. Antacids [Maalox, Mylanta, Rolaids, Tums]
! SE = electrolyte imbalance, diarrhea, constipation, kidney
stones
! Interactions = Ibuprofen, sulfonylurea drugs, ferrous
sulfate, tetracycline, ciprofloxacin, INH
! Cautions = kidney stones, hyperCa, renal failure, CHF
2. H2 Receptor Antagonists [Tagamet] and PPIs [Prilosec]
! SE = liver dz. tachyphylaxis
! Interactions = a ton
! Cautions = cirrhosis, anti-coag.
Anti-Diarrheals
1. Bismuth Subsalicylate [PeptoBismol, Kaopectate]
! SE = discolored feces and tongue, fecal impaction
! Interactions = warfarin, tetracycline, steroids,
valproic acid, uricosuric drugs, antacids
! Cautions = anti-coag and inf. D
2. Loperamide [Imodium]
! SE = electrolyte imbalance, fluid loss, dehydration,
paralytic ileus
! No interactions
! Cautions = cirrhosis, inf. D
OTC Constipation Products
1. Bisacodyl [Dulcolax] and Senna [Ex-lax]
! SE = electrolyte imbalance, cathartic axn
! No interactions
! No cautions
2. Magnesium Hydroxide [MOM] and Magnesium Sulfate [Epsom salts]
! SE = electrolyte imbalance, edema
! DI = quinolones, azoles, thyroid drugs, digoxin
! Cautions = renal failure, bone dz
Insomnia Sleep Disturbances
! OTC Sleep Aids = have 1
st
gen. anti-histamines
Diphenhydramine, Doxylamine
! Lack of consistency in action tolerance
! Daytime drowsiness, dry mouth palpitations, blurred
vision, urinary retention (problems with an enlarged
prostate)
Special Patient Populations
1. Women
! Transplacental passage occurs in pg. adverse teratogenic
or pharmacological effects possible
! *Acetaminophen is DOC for short-term pain relief
! NSAIDs/Aspirin developmental/delivery problems
! 3
rd
trimester = heartburn is common; chronic antacid
use = hyper, or hypoMg and hyper Ca; H2 blockers have
shown anti-androgenic effect t/f direct patients to antacids
because safety data is stronger
2. Neonate
! Acetaminophen + NSAIDs provide safe pain relief
! Aspirin in milk = rashes and neonatal bleeding
! Anti-Histamines (H1 and H2) eliminated in the
milk H1 = sedation, irritability, crying, sleep
disturbances, " milk production; H2 = AAP accepts
with no risks involved
! Al or Mg antacids dont enter milk
3. Children
! OTC drugs are safe when used appropriately
! Kids are not just small adults follow dosing instructions
and DONT DOUBLE THE DOSE b/c child seems sicker
than last time the OTC product was used
! Acetaminophen = DOC for pain relief
! Avoid aspirin = risk of Reyes syndrome
! Decongestants use correct dose
! Antacids widely used but safety not established
! H2 blockers are safe liquid formulations are not OTC!
4. Fetus see chart slide 35 list of drugs and effects on fetus
5. Elderly
! ! risk NSAIDs and kidney dz/ GI bleeding
! ! risk glaucoma/UT block with pseudoephedrine
! Interactions with anti-histamines may be significant
worsen asthma, narrow angle glaucoma, prostatic
enlargement, confusion, delirium, dizziness (falls and
fractures)
! More susceptible to adverse effects of GI drugs:
(Diarrhea/dehydration (Mg) or constipation (Al)
Mg antacids are best if no remal impairment
Drug interaction with cimetidine most likely
1) Streptokinase is administered as part of the immediate therapy for a patient presenting
with acute MI. The drug works by:
A) Activating the conversion of fibrin to fibrinsplit products
*) Activating the conversion of plasminogen to plasmin
C) Inhibiting the conversion of prothrombin to thrombin
D) Inhibiting the conversion of fibrinogen to fibrin
2) A patient on heparin therapy is bleeding profusely from the i.v. site after treatment is
terminated. Protamine is administered to reverse the effects of heparin. It does this by:
A) hydrolyzing heparin
B) changing the conformation of antithrombin III to prevent heparin binding
C) activating the coagulation cascade, overriding the actions of heparin
*) combining with heparin as an ion-pair, thereby inactivating it
3) Clopidogrel is administered to a 67 year-old man to guard against another stroke.
When employed in this manner, clopidogrel works by:
A) Inhibiting platelet thromboxane production
*) Antagonizing the ADP receptor
C) Antagonizing glycoprotein Iib/IIIa
D) Inhibition of vitamin K-dependent coagulation factor synthesis
E) Activation of plasminogen to plasmin
4) In patients receiving warfarin, the antithrombotic effect is decreased when they are
given which of the following drugs?
A) Chloral hydrate
B) Heparin
C) Aspirin
*) Cholestyramine
E) Clopidogrel
5) Which of the following drug pairings represents a pharmacokinetic drug interaction?
A) Propranolol - Isoproterenol
B) Nalmefene - Morphine
*) Acetaminophen - Ethanol
D) Neostigmine Tubocurarine
6) In the Facts & Comparisons A to Z Drug Facts book, one reads that: "effects of
felodipine [Plendil] may increase if given with grapefruit juice." The mechanism
responsible for this interaction is:
A) increased stomach acidity
*) decreased metabolism in the intestinal wall
C) decreased stomach emptying
D) increased rate of tablet dissolution
E) decreased renal excretion
7) Drug X is a CNS-active product that is converted to a single inactive metabolite by a
CYP: 2C19 (P-450) mediated biotransformation. Which of the following statements
regarding this process is CORRECT?
A) Concurrent cimetidine exposure will shift the dose-response curve of drug X to the
left and increase its half-life
B) Concurrent rifampin exposure will reduce the affinity of drug X for its receptor
C) Concurrent rifampin exposure will shift the dose-response curve of drug X to the right
and decrease its half-life
D) Concurrent cimetidine exposure will increase the affinity of drug X for its receptor
E) Neither cimetidine nor rifampin will have any effect upon the activity of drug X
8) The abuse liability of stimulants is thought to result from:
A) stimulation of norepinephrine transmission
B) inhibition of serotonin transmission
C) simulation of GABA-A receptors
D) inhibition of AMPA receptors
*) stimulation of dopamine transmission
9) Which anti-narcolepsy drug has relatively little abuse liability?
*) Mazindol (Mazanor)
B) Methamphetamine (Ice)
C) Methylphenidate (Ritalin)
D) Amphetamine (Dexedrin)
E) Modafinil (Provigil)
Heparin:
A) has thrombolytic activity
B) has the most prolonged activity when administered orally
*) acts by inhibiting antithrombin
D) inhibits the aggregation of platelets caused by TXA2
E) acts by blocking hepatic vitamin K regeneration
Warfarin:
A) acts rapidly when given orally
B) is potentiated by barbiturates
C) is antagonized by protamine sulfate
*) affects the activity of clotting factors
E) is potentiated by platelet factor 4
The risk of bleeding in patients receiving heparin is increased by concurrent aspirin
treatment because aspirin:
A) inhibits heparin anticoagulant activity
*) inhibits platelet function
C) displaces heparin from plasma protein binding sites
D) inhibits prothrombin formation
E) causes threombocytopenia
When given concurrently, which of the following drugs decreases the antithrombotic
effect of warfarin?
A) Chloral hydrate
B) Heparin
C) Aspirin
*) Cholestyramine
E) Clopidogrel
Aspirin can:
*) prevent TXA2 formation
B) prolong whole blood clotting time
C) shortens bleeding time
D) inhibits fibrinolysis
E) inhibits the effects of warfarin
If bleeding became a problem in a 67 year-old man receiving warfarin for prophylaxis of
a recurrent venous thromboembolism, which of the following would most effectively
reduce the clotting time?
A) Aspirin
B) Heparin
C) tPA
*) Vitamin K
E) Fibrinogen
Alteplase is prescribed for a 54 year-old man with an acute MI. This drug works by:
A) blocking platelet ADP receptors
B) inhibits platelet TXA2 formation
C) blocking the metabolic formation of vitamin K-dependent coagulation factors
D) blocking glycoprotein IIb/IIIa receptors
*) promoting conversion of plasminogen to plasmin
Which of the following tests would show an abnormal value in a patient taking aspirin on
a chronic basis?
A) Activated Partial Thromboplastin Time (APTT)
*) Bleeding time
C) INR (International Normalized Ratio)
D) Platelet count
E) Prothrombin time
OTC Drugs.
1. How are OTC products regulated?
2. When used as directed, what are the side effects or toxicities and possible interactions
with prescription drugs?
In a patient who is self-medicating with NSAIDs for rheumatoid arthritis, which of the
following OTC antidiarrheal agents would give MOST cause for concern of a drug
toxicity?
A) Loperamide
*) Bismuth subsalicylate
C) Kaolin
D) Calcium carbonate
E) Alumina powder
Which of the following OTC drugs is known to reduce milk volume in mothers with
suckling infants?
A) cimetidine [Tagamet]
B) aspirin
*) diphenhydramine [Benadryl allergy sinus]
D) metamucil
E) tums or rolaids
Factors affecting drug action.
1. What factors affect drug action?
2. What impact do they have?
3. Can you manipulate them?
The renal clearance of drug X is <GFR when ammonium chloride is administered
concurrently, but is >GFR when sodium bicarbonate is administered concurrently.
Which of the following BEST characterizes the properties of drug X?
A) Strong organic base
B) Non electrolyte
*) Weak organic base
D) Weak organic acid
E) Strong organic acid
In the Facts & Comparisons A to Z Drug Facts book, one reads that: "effects of
felodipine [Plendil] may increase if given with grapefruit juice." The mechanism
responsible for this interaction is:
A) increased stomach acidity
*) decreased metabolism in the intestinal wall
C) decreased stomach emptying
D) increased rate of tablet dissolution
E) decreased renal excretion
2) Drug X is a CNS-active product that is converted to a single inactive metabolite by a
CYP: 2C19 (P-450) mediated biotransformation. Which of the following statements
regarding this process is CORRECT?
*) Concurrent cimetidine exposure will shift the dose-response curve of drug X to the left
and increase its half-life
B) Concurrent rifampin exposure will reduce the affinity of drug X for its receptor
C) Concurrent rifampin exposure will shift the dose-response curve of drug X to the right
and increase its half-life
D) Concurrent cimetidine exposure will increase the affinity of drug X for its receptor
E) Neither cimetidine nor rifampin will have any effect upon the activity of drug X
Potrebbero piacerti anche
- Growth Hormone (HGH)Documento33 pagineGrowth Hormone (HGH)Juan Solis Quiroz100% (1)
- Fast Facts: Deficiencia de piruvato quinasa: Divulgando el conocimiento sobre esta enfermedad genética raraDa EverandFast Facts: Deficiencia de piruvato quinasa: Divulgando el conocimiento sobre esta enfermedad genética raraNessuna valutazione finora
- Region With Human Constant Regions and Variable FrameworkDocumento2 pagineRegion With Human Constant Regions and Variable FrameworkBigBoosting100% (1)
- Localización en Neurología ClínicaDocumento1 paginaLocalización en Neurología ClínicaDanielGiraldoNessuna valutazione finora
- Pathophysiology of Cardiogenic Pulmonary Edema - UpToDateDocumento9 paginePathophysiology of Cardiogenic Pulmonary Edema - UpToDateRoberto López MataNessuna valutazione finora
- Fisiologia de Los Opioides Epidurales e IntratectalesDocumento13 pagineFisiologia de Los Opioides Epidurales e Intratectalessanjuandediosanestesia100% (5)
- Revista - Medigraphic - 2000 - Hidroterapia en Enfermedades MentalesDocumento6 pagineRevista - Medigraphic - 2000 - Hidroterapia en Enfermedades MentalesGiancarlo Gardella MartínezNessuna valutazione finora
- Criterios Beers 2019Documento8 pagineCriterios Beers 2019Viki BernalNessuna valutazione finora
- Alveoli T IsDocumento15 pagineAlveoli T IsValentina CRNessuna valutazione finora
- Validate Memory Test ChileDocumento13 pagineValidate Memory Test ChileLicAndreaMeleNessuna valutazione finora
- 2020 - Guías KDIGO ERC PDFDocumento115 pagine2020 - Guías KDIGO ERC PDFMarieta ColonioNessuna valutazione finora
- Sistema EndocrinoDocumento59 pagineSistema EndocrinoJuan Ignacio DrovandiNessuna valutazione finora
- Diagnosis and Management of Hyponatremia A ReviewDocumento12 pagineDiagnosis and Management of Hyponatremia A ReviewCynthia Huaman C.Nessuna valutazione finora
- L9 Sympathomimetics Lytics REVISED 2017 PDFDocumento49 pagineL9 Sympathomimetics Lytics REVISED 2017 PDFVea AngelesNessuna valutazione finora
- Drugs Affecting The Adrenergic Nervous SystemDocumento37 pagineDrugs Affecting The Adrenergic Nervous SystemJah SuNessuna valutazione finora
- SY - Medichem i -Drugs acting on ANS (1)Documento83 pagineSY - Medichem i -Drugs acting on ANS (1)KevalNessuna valutazione finora
- List of Drugs Pharmacology 2Documento13 pagineList of Drugs Pharmacology 2Maisarah Ab SamadNessuna valutazione finora
- Assignment On Adrenergic ReceptorDocumento13 pagineAssignment On Adrenergic ReceptoryannaingNessuna valutazione finora
- Faktor Neurobiologi: Qara Syifa Fachrani 1610211039Documento22 pagineFaktor Neurobiologi: Qara Syifa Fachrani 1610211039Qara Syifa FNessuna valutazione finora
- Antipsychotics: Corina Freitas MS, MD, MBA, DABFMDocumento48 pagineAntipsychotics: Corina Freitas MS, MD, MBA, DABFMCorina FreitasNessuna valutazione finora
- PharmacologyDocumento236 paginePharmacologynbde2100% (5)
- Parkinson'sDocumento42 pagineParkinson'sjabari.baraNessuna valutazione finora
- Adrenergic & Antiadrenergic DrugsDocumento54 pagineAdrenergic & Antiadrenergic DrugsUzma KhanNessuna valutazione finora
- Phl211 Sns 14th Lecture SFDocumento10 paginePhl211 Sns 14th Lecture SFALNAKINessuna valutazione finora
- Pharma NewestDocumento131 paginePharma NewestPaolo Montańa EzparasNessuna valutazione finora
- Pharm ANSDocumento45 paginePharm ANSaditya_goel_10Nessuna valutazione finora
- Ketamine Drug SummaryDocumento3 pagineKetamine Drug SummarySydney JenningsNessuna valutazione finora
- CNS 2022Documento8 pagineCNS 2022Kathleen Kate MonsalveNessuna valutazione finora
- Exam 1 Pharmacology II NotesDocumento4 pagineExam 1 Pharmacology II Notessin2begin2Nessuna valutazione finora
- Drenergic AND Anti Adrenergic Drugs: Shabib AkhtarDocumento21 pagineDrenergic AND Anti Adrenergic Drugs: Shabib AkhtarDeepa ShaiekhNessuna valutazione finora
- 11 20 2006 Bio Medical HomeostasisDocumento44 pagine11 20 2006 Bio Medical Homeostasisapi-3696530Nessuna valutazione finora
- Adrenergic Drugs!: Drugs That Affect Catecholamine SYNTHESISDocumento10 pagineAdrenergic Drugs!: Drugs That Affect Catecholamine SYNTHESISDan TadeoNessuna valutazione finora
- Adrenergic DrugsDocumento33 pagineAdrenergic DrugsZsa Zsa FebryanaNessuna valutazione finora
- CHFDocumento11 pagineCHFGwendolyn Talahiban LusaraNessuna valutazione finora
- Adrenergic DrugsDocumento45 pagineAdrenergic DrugsHUZAIFA YAMAANNessuna valutazione finora
- Adrenergic Drugs: Pharmacological Department Medical School - UNPAD Ike HusenDocumento33 pagineAdrenergic Drugs: Pharmacological Department Medical School - UNPAD Ike HusenHendra EfendiNessuna valutazione finora
- ANS RXDocumento23 pagineANS RXLarry TenhoffNessuna valutazione finora
- Written - Year 1 Drugs (6) - 2Documento10 pagineWritten - Year 1 Drugs (6) - 2MariaaaahNessuna valutazione finora
- Chap 5 CNSDocumento106 pagineChap 5 CNSKIDUS YAREDNessuna valutazione finora
- Parkinson's DiseaseDocumento9 pagineParkinson's DiseaseJAMAL WARISNessuna valutazione finora
- Adrenergic PharmacologyDocumento6 pagineAdrenergic Pharmacologyjess6001Nessuna valutazione finora
- Pharm Exam #1Documento19 paginePharm Exam #1Taylor SolomonNessuna valutazione finora
- Cardiovascular Pharmacology - Antihypertensive AgentsCardiovascular Pharmacology - Antihypertensive AgentsDocumento14 pagineCardiovascular Pharmacology - Antihypertensive AgentsCardiovascular Pharmacology - Antihypertensive AgentsAndySatrioTipunkNessuna valutazione finora
- IntroductIon To AutonomousDocumento29 pagineIntroductIon To AutonomousMerve kdkkNessuna valutazione finora
- Dopamine, Serotonine, Epinephrine, and NorephinephrineDocumento28 pagineDopamine, Serotonine, Epinephrine, and Norephinephrinehafshah100% (1)
- Pharma CAL Lab Dog BP Expt.Documento14 paginePharma CAL Lab Dog BP Expt.sibananda palNessuna valutazione finora
- AntidepressantsDocumento38 pagineAntidepressantsjabari.baraNessuna valutazione finora
- Adrenoreceptor Antagonist: Leida Marie P. Alarcon, MD, FPAFPDocumento23 pagineAdrenoreceptor Antagonist: Leida Marie P. Alarcon, MD, FPAFPKenneth NuñezNessuna valutazione finora
- Adrenergic AntagonistsDocumento6 pagineAdrenergic Antagonistsfiena92100% (2)
- Adrenergic Agents SeminarDocumento48 pagineAdrenergic Agents SeminarTheBoss 20Nessuna valutazione finora
- Effects and Uses of Adrenergic Agonists and AntagonistsDocumento120 pagineEffects and Uses of Adrenergic Agonists and Antagonistscoosa liquors100% (1)
- Autonomic Nervous System PharmacologyDocumento7 pagineAutonomic Nervous System Pharmacologydonordarah93Nessuna valutazione finora
- Naplex NotesDocumento226 pagineNaplex NotesløzanNessuna valutazione finora
- Sympathetic Agonist and Antagonist 23Documento12 pagineSympathetic Agonist and Antagonist 23PNessuna valutazione finora
- PharmTest3 StudyGuideDocumento9 paginePharmTest3 StudyGuideTara Bickford ManisNessuna valutazione finora
- Adrenergic AgonistsDocumento22 pagineAdrenergic AgonistsEthar LoveNessuna valutazione finora
- Notes For Diazepam and Other DrugsDocumento1 paginaNotes For Diazepam and Other DrugsVanessa HabajabNessuna valutazione finora
- Autonomic Nervous System AgentsDocumento14 pagineAutonomic Nervous System AgentsRhenier S. Ilado100% (1)
- SympathomimeticDocumento56 pagineSympathomimeticvarish0% (1)
- PharmaDocumento11 paginePharmaGohar KamranNessuna valutazione finora
- Drugs Acting On Renal SystemDocumento98 pagineDrugs Acting On Renal SystemIsmael JaaniNessuna valutazione finora
- Anesthesia Drugs Part 1 and 2 CompiledDocumento20 pagineAnesthesia Drugs Part 1 and 2 CompiledLavNessuna valutazione finora
- Usmle Step1 MCQ Study Online Questions ReviewDocumento13 pagineUsmle Step1 MCQ Study Online Questions ReviewfrabziNessuna valutazione finora
- Pharmacology ReviewerDocumento21 paginePharmacology ReviewerCzairalene QuinzonNessuna valutazione finora
- Genitourinary PharmacologyDocumento11 pagineGenitourinary PharmacologySadia YousafNessuna valutazione finora
- Technichal Siwes ReportDocumento10 pagineTechnichal Siwes ReportBerende AbuhasanNessuna valutazione finora
- Formulation Science & Bioavailability: Pharmacological Parameters Study On Loop Diuretic Drug - FurosemideDocumento3 pagineFormulation Science & Bioavailability: Pharmacological Parameters Study On Loop Diuretic Drug - FurosemidevivianNessuna valutazione finora
- DiureticsDocumento29 pagineDiureticsSaravanan RajagopalNessuna valutazione finora
- CVS: Diuretics GuideDocumento2 pagineCVS: Diuretics GuideCatNessuna valutazione finora
- Fluids Electrolytes PDFDocumento27 pagineFluids Electrolytes PDFAnonymous rDD9I2Nessuna valutazione finora
- Kidney Transplant Nursing CareDocumento1 paginaKidney Transplant Nursing CareAlrhajib Francis AnniNessuna valutazione finora
- Digital Scrapbook - Espina - n1Documento15 pagineDigital Scrapbook - Espina - n1Marie Antionette MondragonNessuna valutazione finora
- FCPS II CardiologyDocumento32 pagineFCPS II CardiologyAamir HamaadNessuna valutazione finora
- KidneyDocumento19 pagineKidneySridharNessuna valutazione finora
- Potassium-sparing diuretics: functions, indications and nursing responsibilitiesDocumento9 paginePotassium-sparing diuretics: functions, indications and nursing responsibilitieschelseyNessuna valutazione finora
- Diuretics MOA, Examples, Effects, and Nursing ConsiderationsDocumento1 paginaDiuretics MOA, Examples, Effects, and Nursing ConsiderationsGrace ButlerNessuna valutazione finora
- DIURETICSDocumento2 pagineDIURETICSLaureece Salm ApduhanNessuna valutazione finora
- State Exams Questions 20 40Documento257 pagineState Exams Questions 20 40Yaoling WenNessuna valutazione finora
- Metabolic Alkalosis: Bicarbonate ExcessDocumento3 pagineMetabolic Alkalosis: Bicarbonate ExcessAllyssa MackinnonNessuna valutazione finora
- Urine FormationDocumento49 pagineUrine FormationMajd HusseinNessuna valutazione finora
- Caffeine Vs Caffeine-Free Sports Drink Effects On Urine Production - Wemple 1997Documento7 pagineCaffeine Vs Caffeine-Free Sports Drink Effects On Urine Production - Wemple 1997Yo Vivo Fit Pablo y KarlaNessuna valutazione finora
- PHINMA Nursing Drug Study on HydrodiurilDocumento1 paginaPHINMA Nursing Drug Study on HydrodiurilArianne Nicole PinuelaNessuna valutazione finora
- Ka-En MimsDocumento7 pagineKa-En MimsMFWPNessuna valutazione finora
- Revision MCQs on Renal Physiology and PharmacologyDocumento6 pagineRevision MCQs on Renal Physiology and PharmacologywiamNessuna valutazione finora
- Nursing Care Plan for Hypertension ManagementDocumento5 pagineNursing Care Plan for Hypertension Managementbhavana100% (1)
- Diuretic DrugsDocumento2 pagineDiuretic DrugsEngku ElisaNessuna valutazione finora
- Hypertention and HypotentionDocumento46 pagineHypertention and HypotentionAmanuel MaruNessuna valutazione finora
- Review of The TheoryDocumento8 pagineReview of The TheoryPriskaCliquersNessuna valutazione finora
- Pharmacotherapy of HypertensionDocumento52 paginePharmacotherapy of HypertensionDrVinod Kumar Goud VemulaNessuna valutazione finora
- Pharmacology Test 3 ReviewDocumento6 paginePharmacology Test 3 ReviewNatalia BortellNessuna valutazione finora